Abstract
Background
Intrinsic capacity (IC) is a comprehensive indicator of an individual’s positive attributes. The World Health Organization (WHO) recommends a two-step approach to assess IC decline among older people. The first step involves the used of the integrated care for older people (ICOPE) screening tool to identify potential issues, and the second step involves using detailed assessments for confirmation. This study aimed to assess the diagnostic performance of the ICOPE screening tool as a simple preliminary screening to identify IC decline among community-dwelling older people, which has been rarely reported in China.
Methods
This cross-sectional study included 228 community-dwelling older individuals aged ≥ 75 (mean age, 84.0 ± 4.4 years; 131 [57.5%] females) who completed the IC evaluation according to the WHO IC assessment pathway. The diagnostic performance of the ICOPE screening tool was calculated using a 2 × 2 table and a receiver operating characteristic curve.
Results
The proportion of possible IC decline identified by the ICOPE screening tool was 79.4%, whereas the actual IC decline assessed by the detailed assessment was 73.2%, mainly in locomotion. The ICOPE screening tool showed sensitivity and specificity of 94.6% and 62.3%, respectively, with an overall diagnostic accuracy of 86.0%. The diagnostic effectiveness of the ICOPE screening tool was 0.91 (95% confidence interval: 0.87–0.95, p = 0.020). Except for the sensory dimension, the sensitivity of the ICOPE screening tool for diagnosing impairments in each dimension of the IC was the highest in the cognition domain (100%) and the lowest in the vitality domain (51.3%), whereas the specificity was the highest in vitality (94.7%) and the lowest in cognition (55.6%).
Conclusions
The ICOPE screening tool exhibits high sensitivity and can be used as an IC screening tool in community-dwelling older people. However, further improvements are needed in the vitality dimension of the ICOPE screening tool to enhance its sensitivity in identifying individuals at risk of malnutrition.
Keywords: Diagnostic performance, Intrinsic capacity, ICOPE screening tool, Older people
Background
The aging global population is constantly increasing. As a populous country, China faces a severe aging challenge. According to the National Bureau of Statistics of China’s 2022 investigation on population changes [1], the proportion of people aged 60 years and above has reached 19.8%, with those aged 65 years and above accounting for 14.9%, indicating that China has become an aging society. Those born during the second baby boom, between 1962 and 1975, will gradually enter retirement by 2023, further increasing the burden of aging in China. In 2022, the Lancet published a report on China’s path to healthy aging [2], which showed that its life expectancy has gradually approached that of other developed countries.
In 2021, the World Health Organization (WHO) proposed the “Decade of Healthy Aging 2020–2030” [3], which involves the following four areas: (1) providing person-centered integrated care to meet the needs of older people; (2) changing attitudes and behaviors towards aging; (3) supporting community interventions to maintain the intrinsic capacity (IC) of older people [4] and promote functional ability; and (4) providing long-term care for older people in need. Therefore, the concept of healthy aging implies that the medical model for older people should shift from a disease-centered to a function-centered approach [5]. IC is the basis of functional turning.
The concept of IC is an evolution of the International Classification of Functioning, Disability, and Health framework proposed by the WHO in 2001 [6]. Within this framework, the health condition (disease) construct is inadequate to define IC. Only the functional domain aligns with IC, which was proposed in 2015 by the WHO [4]. The WHO [4] defined the concept of IC as a combination of all the mental and physical capacities that an individual can access at any time.
In 2018, Cesari et al. [7] reviewed the literature and proposed the following five dimensions of IC: locomotion, cognition, vitality, psychology, and sensory (hearing and vision). Visual and hearing impairments can affect older people’s activities and cognition, and the presence of both can exacerbate these effects [7]. Therefore, they are generally considered as two capacities within the sensory dimension. Beard et al. [8] verified the validity of this multidimensional model based on the China Health and Retirement Longitudinal Study and found that the individual’s IC could reflect functional ability. Yu et al. [9] in Hong Kong also supported the construction of the five domains of IC using structural equation models. In 2019, the WHO proposed the person-centered assessment and pathways in primary care [10], which contains 5 steps. The first step involves the use of the integrated care for older people (ICOPE) screening tool to identify potential IC decline issues, and the second step involves the use of detailed assessments to confirm individuals with actual IC decline. Based on this assessment, personalized interventions [10] can be provided to older people with IC decline in step 3. Steps 4 and 5 involve monitoring care plans and supporting caregivers, respectively.
However, what is the diagnostic performance of the ICOPE screening tool in detecting IC decline? There are two published studies, one from Hong Kong, China [11], and the other from Spain [12]; both of them indicate that the ICOPE screening tool has high sensitivity but varying screening effectiveness across different dimensions. Additionally, no relevant studies have been conducted in mainland China.
Therefore, this study aimed to evaluate diagnostic performance, which includes the sensitivity, specificity, and diagnostic accuracy of the ICOPE screening tool to determine whether the screening tool is suitable for community-dwelling older people using step 2 of the detailed assessment of IC as the gold standard.
Methods
Study design and participants
This study used the baseline data of a previous cohort study [13]. This cohort study primarily aimed to explore the trajectory of IC in older people and its predictive value for adverse outcomes. The external environment also influences the functional performance of older people and the occurrence of adverse outcomes [14]. Therefore, to reduce the confounding effects of the external environment and support systems and better explain the impact of individual differences in IC, this study selected residents of a relatively consistent external environment in an elderly friendly community (Taikang Yanyuan) in Beijing as the research participants. This study cohort included community-dwelling older people continuously from July–September 2018. The inclusion criteria were as follows: individuals aged ≥ 75 years and those who had completed the IC assessment. The exclusion criteria were as follows: individuals with acute illness within three months prior to enrollment, including but not limited to acute coronary syndrome, pulmonary infection, and stroke.
Measurements
Sociodemographic data, such as age, sex, height, weight, and education level, were collected. Polypharmacy refers to the use of ≥ 5 medications, including prescription and non-prescription drugs [15].
The Cumulative Illness Rating Scale for Geriatrics (CIRS-G) [16] was used to assess comorbidities. This scale includes the distribution of diseases in 14 systems. Each system is classified into 5 levels based on disease severity, with scores ranging from 0–4. When multiple diseases exist within the same system, the score is based on the highest severity level. The scores of each item are summed to obtain a total score.
Basic activities of daily living (ADL) were evaluated using the physical self-maintenance scale (PSMS) [17], which evaluates basic self-care activities, such as toileting, grooming, feeding, dressing, physical ambulation, and bathing. Each item was scored as 1 point, with a total score ranging from 0–6. A score of < 6 indicated a decline in ADL. Furthermore, instrumental activities of daily living (IADL) were assessed using the Lawton IADL scale [17]. This scale evaluates activities such as telephone use, food preparation, responsibility for own medications, financial management, shopping, housekeeping, laundry, and mode of transportation. Each item was scored as 1 point, with a total score ranging from 0–8. A score of < 8 indicated a decline in IADL.
Intrinsic capacity
This study was based on the WHO IC assessment pathway [10] (Table 1), with step 1 being an IC screening evaluation of the participants using the ICOPE screening tool. The total score ranged from 0–9 points, and a score of ≥ 1 indicated a possible IC decline. Step 2 involved a detailed IC evaluation [18–21] of IC to identify older people with actual IC decline. The total score ranged from 0–6 points, and a score of ≥ 1 indicated actual IC decline. In this study, visual and hearing impairments were defined as impairments impacting daily life during screening and detailed assessment.
Table 1.
2-Step intrinsic capacity assessment: ICOPE screening tool and detailed assessment1
| IC dimensions | ICOPE screening tool | Detailed assessments |
|---|---|---|
| Locomotion | Five times sit-to-stand test ≥ 14 s | SPPB ≤ 9 score |
| Vitality | Loss more than 3 kg of weight in the past 3 months | MNA-SF ≤ 11 score |
| Loss of appetite in the past 3 months | ||
| Cognition | Cannot recall three words | MMSE < 24 score |
| Disorientation in time or space | ||
| Psychology | Depressed or hopeless in the past two weeks | GDS-15 ≥ 5 score |
| Lost interest in activities in the past two weeks | ||
| Sensory (vision) | Vision deteriorated and affected daily life | Same |
| Sensory (hearing) | Hearing deteriorated and affected daily life | Same |
Abbreviations: 1If any problem in the table satisfied is scored 1. The total score of the ICOPE screening tool ranges from 0–9 points, and a score of ≥ 1 indicates possible IC decline. The total score of detailed IC assessments ranges from 0–6 points, and a score of ≥ 1 indicates actual IC decline. IC Intrinsic capacity, SPPB Short physical performance battery, MNA-SF Short-form mini-nutritional assessment, MMSE Mini-mental state examination, GDS-15 15-item geriatric depression scale
Statistical analysis
Baseline data were collected, and normally distributed data were expressed as mean ± standard deviation (x ± s), while non-normally distributed data were expressed as median (interquartile range) [M (IQR)]. Quantitative data were presented as constituent ratios, rates, and absolute numbers. The validity of the ICOPE screening tool for detecting IC decline was calculated using a four-fold table and the receiver operating characteristic curve. All data were analyzed using SPSS26.0 for Windows (IBM Corp. Armonk, NY, USA).
Results
Baseline characteristics
Overall, 228 older people were included in this study (Table 2), with a mean age of 84.0 ± 4.4 years. Of them, 131 (57.5%) were female, and 225 (98.7%) had an education level of high school or above. The CIRS-G score was 5 (3–7) points. The ADL score was 6 (6–6) points, indicating a good functional status. Furthermore, the ICOPE screening tool score was 2 (1–4) points, and 181 (79.4%) participants were identified as having a possible IC decline. In the detailed evaluation of step 2 IC, the score was 1 (0–2), indicating that 167 (73.2%) older people had an actual IC decline.
Table 2.
Baseline characteristics of 228 participants
| Variable | Total |
|---|---|
| n = 228 | |
| Age, mean (SD), years | 84.0 ± 4.4 |
| Female, n (%) | 131 (57.5) |
| BMI, mean ± SD, kg/m2 | 24.2 ± 3.4 |
| High school or above, n (%) | 225 (98.7) |
| Polypharmacy, n (%) | 130 (57.0) |
| CIRS-G, M (IQR) | 5 (3–7) |
| ADL, M(IQR) | 6 (6–6) |
| IADL, M(IQR) | 7 (5–8) |
| ICOPE screening tool | 2 (1–4) |
| Possible IC decline, n(%) | 181 (79.4) |
| IC detailed assessment | 1 (0–2) |
| Actual IC decline, n(%) | 167 (73.2) |
Abbreviations: SD Standard deviation, BMI Body mass index, CIRS-G The cumulative illness rating scale for geriatrics, ADL Activities of daily living, ICOPE Integrated care for older people, IQR Interquartile range, IC Intrinsic capacity
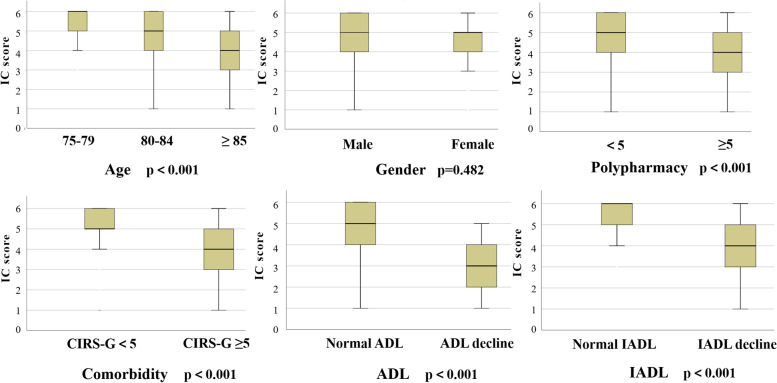
As shown in Fig. 1, we compared the IC scores of different groups and assessed the differences in IC levels between these groups. The results demonstrated that IC levels decline with increasing age. Older people with polypharmacy, a higher burden of comorbidities, and a decline in ADL exhibited lower levels of IC.
Fig. 1.
Comparison of the intrinsic capacity scores among different groups in 228 community-dwelling older people. Abbreviations: IC, intrinsic capacity; CIRS-G, the cumulative illness rating scale for geriatrics; ADL, activities of daily living; IADL, instrumental activities of daily living
Intrinsic capacity
In step 1, the ICOPE screening tool was used to identify possible IC decline among older people, and the proportion identified was 79.4%. The proportions of participants with impaired locomotion, vitality, cognition, psychology, vision, and hearing were 50.0%, 13.2%, 53.9%, 35.1%, 19.7%, and 20.2%, respectively. In Step 2, a detailed evaluation method was used to assess the proportion of older people with actual IC decline (73.2%). The proportions of patients with impaired locomotion, vitality, cognition, and psychology were 60.1%, 17.1%, 17.1%, and 16.2%, respectively (Table 3).
Table 3.
IC decline and impairment of each domain in 2-step assessment
| Step1 ICOPE screening tool | Step 2 detailed IC assessments | |
|---|---|---|
| IC decline, n (%) | 181 (79.4) | 167 (73.2) |
| IC domain impairment | ||
| Locomotion, n (%) | 114 (50.0) | 137 (60.1) |
| Vitality, n (%) | 30 (13.2) | 39 (17.1) |
| Cognition, n (%) | 123 (53.9) | 39 (17.1) |
| Psychology, n (%) | 80 (35.1) | 37 (16.2) |
| Sensory (vision), n (%) | 45 (19.7) | 45 (19.7) |
| Sensory (hearing), n (%) | 46 (20.2) | 46 (20.2) |
Abbreviations: IC Intrinsic capacity, ICOPE Integrated care for older people
Validity of the ICOPE screening tool
The ICOPE screening tool had a sensitivity and specificity of 94.6% and 62.3% for identifying IC decline, respectively, with a diagnostic accuracy of 86.0%. Except for the sensory dimension, the sensitivity for detecting impairment in each dimension of the IC using the ICOPE screening tool was the highest for cognition (100%) and the lowest for vitality (51.3%). Regarding specificity, the vitality dimension performed the best at 94.7%, whereas cognition had the lowest specificity at 55.6% (Table 4). As shown in Fig. 2, the diagnostic effectiveness of the ICOPE screening tool was 0.91 (95% confidence interval: 0.87–0.95, p = 0.020).
Table 4.
Sensitivity, specificity and diagnostic accuracy of ICOPE screening tool
| Detailed IC assessment (IC domain impairment) | Possible IC decline by ICOPE screening tool | Sensitivity (%) | Specificity (%) | Diagnostic accuracy (%) | ||
|---|---|---|---|---|---|---|
| Assessment result | Yes | No | ||||
| IC decline | Yes | 158 | 9 | 94.6 | 62.3 | 86.0 |
| No | 23 | 38 | ||||
| Locomotion | Yes | 108 | 29 | 78.8 | 93.4 | 84.6 |
| No | 6 | 85 | ||||
| Vitality | Yes | 20 | 19 | 51.3 | 94.7 | 87.3 |
| No | 10 | 179 | ||||
| Cognition | Yes | 39 | 0 | 100 | 55.6 | 63.2 |
| No | 84 | 105 | ||||
| Psychology | Yes | 27 | 10 | 73.0 | 72.3 | 72.4 |
| No | 53 | 138 | ||||
Abbreviations: IC Intrinsic capacity, ICOPE Integrated care for older people
Fig. 2.
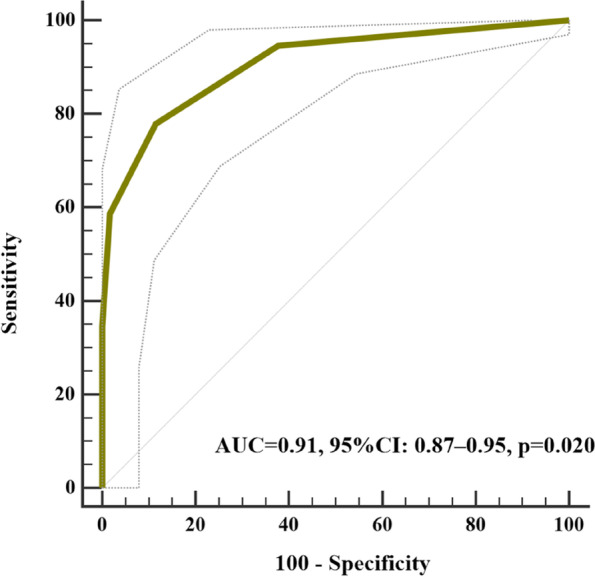
Diagnostic effectiveness of the ICOPE screening tool. Abbreviations: ICOPE, integrated care for older people; AUC, areas under the curve; CI, confidence interval
Body mass index (BMI) < 20 kg/m2 [22] was added to the original ICOPE screening tool for vitality dimension to improve the sensitivity of vitality dimension screening. The vitality domain may be impaired if any of the conditions in the vitality screening question are met. As shown in Table 5, the sensitivity and specificity of the modified ICOPE screening tool were 95.2% and 55.7%, respectively, and the sensitivity of the vitality domain screening increased to 69.2%, with a specificity and diagnostic accuracy of 90.5% and 86.8%, respectively.
Table 5.
Sensitivity, specificity and diagnostic accuracy of modified ICOPE screening tool
| Detailed IC assessment (IC domain impairment) | Possible IC decline by ICOPE screening tool | Sensitivity (%) | Specificity (%) | Diagnostic accuracy (%) | ||
|---|---|---|---|---|---|---|
| Assessment result | Yes | No | ||||
| IC decline | Yes | 159 | 8 | 95.2 | 55.7 | 84.6 |
| No | 27 | 34 | ||||
| Vitality | Yes | 27 | 12 | 69.2 | 90.5 | 86.8 |
| No | 18 | 171 | ||||
Abbreviations: IC Intrinsic capacity, ICOPE Integrated care for older people
Discussion
This study verified the feasibility of the ICOPE screening tool among community-dwelling older people in China based on the WHO proposed assessment pathway for IC in older people. The ICOPE screening tool demonstrated a high sensitivity, specificity, and diagnostic accuracy of 94.6%, 62.3%, and 86.0% in identifying older people with IC decline, respectively. It can be used as a simple and effective screening tool for promotion and application in the community.
The ICOPE screening tool showed varying diagnostic effectiveness for different IC dimensions. The highest sensitivity was observed in the cognitive domain, reaching 100%, whereas the lowest sensitivity was noted in the vitality domain, at 51.3%. A possible reason for the poor sensitivity in vitality is that, in the nutrition screening question, weight loss is defined as “unintentional weight loss ≥ 3 kg in the past 3 months”, while some older people may have lost ≤ 3 kg. Furthermore, for some underweight older people, weight loss may not be significant; however, they may still be at risk of malnutrition. These factors may increase the false-negative rate of the screening tool, leading to a decrease in sensitivity.
Given that a screening tool should have high sensitivity, one method to improve the sensitivity is to lower the weight threshold in the vitality dimension screening question, although the specific value requires further research and discussion. Moreover, adding BMI screening to the screening questions can increase sensitivity. Based on the Global Leadership Initiative on Malnutrition diagnostic criteria recommended for Asians [22] aged ≥ 70 years, a BMI < 20 kg/m2 indicates BMI reduction. In this study, the proportion of older adults with a BMI reduction was 10.1% (23 cases). By including BMI reduction in nutritional screening, the proportion of older adults who may be at risk of malnutrition increased to 19.7% (45 cases). Using the short-form mini-nutritional assessment as the gold standard, the sensitivity of the vitality screening tool increased to 69.2% with a specificity of 90.5% (Table 5). This study provides a reference for future improvements in the ICOPE screening tools. Additionally, the screening question used for the locomotion domain in the ICOPE screening tool was whether the time for the five-time sit-to-stand test (FTSST) was ≥ 14 s. This study mainly included older people of advanced age. We used a short physical performance battery score of ≤ 9 points as the gold standard for impairment in the locomotion domain. Receiver operating characteristic analysis was used to determine that the optimal threshold for the FTSST in this study population was 13.9 s, which was consistent with the recommended threshold in the ICOPE screening tool. However, this threshold may be low in the young age of older people, leading to a decrease in sensitivity. Different age groups may have different FTSST thresholds. Therefore, further sample expansion is required to explore and establish appropriate screening thresholds for the locomotion domain.
The cognitive domain had the lowest specificity among all screening tools (55.6%). In this study, among older people with abnormal cognitive screening results, 95.9% had a decrease in word recall ability, while only 39.0% had impairments in time and space orientation. This suggests that many older people may only experience a decline in word recall ability, whereas memory decline is common in older people and may be unrelated to cognitive impairment. This may be a reason for the low specificity of the cognitive dimension-screening tool.
A study in Spain [12] enrolled 207 older people aged ≥ 70 years, based on the WHO IC assessment pathway, including screening and detailed evaluation of vision and hearing. The results revealed that among all dimensions, the cognitive domain had the highest sensitivity (0.889), with the other dimensions ranging from 0.438–0.557. Among them, vision (0.438), hearing (0.452), and vitality (0.455) domains showed poor sensitivity. The specificities of all dimensions were reasonable, with the vitality domain being the best (0.960), and that of the other domains ranging from 0.682 to 0.953. Overall, their results were similar to those of our study, and some dimensional issues of the ICOPE screening tool require improvement. Another study [11] conducted in Hong Kong, China, included 304 community residents aged ≥ 60 years and found that the sensitivity and specificity of the ICOPE screening tool were 95.0% and 57.6%, respectively. This is consistent with the results of our study. However, the sensitivity of each IC dimension was the highest in the vitality domain, reaching 100%. This difference may be because the study population was relatively younger, and there may have been fewer weight loss individuals, with a lower proportion of actual malnutrition risk or malnourished individuals and a lower false-negative rate.
In this study, 181 (79.4%) older people exhibited a possible IC decline when screened using the ICOPE screening tool; 167 (73.2%) had actual IC decline when assesses using detail assessment. Ma et al. [23] assessed 376 hospitalized older people (68.7 ± 11.4 years) using the ICOPE screening tool and found that 260 (69.1%) individuals exhibited a possible IC decline. Other studies have reported varying proportions of IC decline ranging from 43.0–64.5% [5, 24]. The higher proportion of IC decline in this study may be attributed to the older age of the participants. This study also found that older age, polypharmacy, a higher burden of comorbidities, and a decline in ADL were associated with lower IC levels. These findings are consistent with the results reported by Ma et al. [23]. Additionally, Christine et al. [25] found that cognitive, visual, and hearing impairments were independently associated with ADL decline based on data from the Health and Retirement Study. Furthermore, Sarwat et al. [26] reported that impairments in locomotion (hazard ratio [HR] = 3.03, p < 0.001), cognition (HR = 1.62, p < 0.001), vision (HR = 1.52, p < 0.001), and mental health (HR = 1.71, p < 0.001) were independently associated with an increased risk of ADL decline based on data from the Cardiovascular Health Study with a 7-year follow-up. These studies collectively indicate a close relationship between IC levels and functional status in older people.
Strength and limitation
IC decline is commonly observed in older people and is associated with adverse outcomes [27–32]. Adopting a screening-before-assessment model can utilize community resources more efficiently. The main strength of this study is that few studies have validated the diagnostic performance of the ICOPE screening tool. This enriches the research foundation in this field, provides theoretical references for promoting the ICOPE screening tool in the community, and suggests methods to improve its sensitivity. However, this study also has some limitations. First, this was a single-center, small-sample study, and further sample expansion is needed to validate and extrapolate the conclusions. Second, the screening and detailed evaluation of sensory dimensions in this study were both self-assessment questionnaires. However, considering the limitations of community resources, the evaluation of sensitivity and specificity for sensory screening may be insufficient. Therefore, objective indicators should be used for further evaluation of the sensory domain in future studies.
Conclusion
The ICOPE screening tool has high sensitivity and can be used as an IC screening scale in community-dwelling older people. However, further improvements are needed in the vitality domain of the ICOPE screening tool to enhance its sensitivity in identifying individuals at risk of malnutrition.
Acknowledgements
We are grateful to all the participants in this study. We thank Dr. Guifen Liu, Dr. Xinxiu Yu, Dr. Liang Han, Dr. Jin Zhang, and other medical workers from the Taikang Yanyuan community for their support.
Abbreviations
- ADL
Activities of daily living
- BMI
Body mass index
- CIRS-G
The cumulative illness rating scale for geriatrics
- FTSST
Five-time sit-to-stand test
- GDS
Geriatric depression scale
- ICOPE
Integrated care of older people
- IC
Intrinsic capacity
- IADL
Instrumental activities of daily living
- MMSE
Mini-mental state examination
- MNA-SF
Short-form mini-nutritional assessment
- PSMS
Physical self-maintenance scale
- SPPB
Short physical performance battery
- WHO
World health organization
Authors’ contributions
All authors made a significant contribution to the work reported. The study design was performed by Fei Lu and Xiaohong Liu. Material preparation and data collection were performed by Fei Lu, Shuo Liu, Jiaojiao Li and Xueying Wang. Material analysis was performed by Fei Lu. The first draft of the manuscript was written by Fei Lu. The manuscript was revised by Xiaohong Liu and Xiaohong Sun. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript and agree to be accountable for all aspects of the work.
Funding
National High Level Hospital Clinical Research Funding (2022-PUMCH-B-132). Chongqing Science and Health Joint Medical Research Project (2020FYYX127).
Availability of data and materials
The datasets analyzed in the current study are available from the corresponding author upon request.
Declarations
Ethics approval and consent to participate
We confirm that all methods were performed in accordance with the Declaration of Helsinki and relevant regulations and guidelines. Ethical approval for this study was obtained from the Research Ethics Committee of Peking Union Medical College Hospital (PUMCH, JS2002). Informed consent was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.National Bureau of Statistics of China. Population decreased slightly while urbanization continues to increase. Beijing: National Bureau of Statistics of China; 2023. http://www.stats.gov.cn/zt_18555/zthd/lhfw/2023/sjjd/202302/t20230219_1913346.html. Accessed 22 June 2023.
- 2.Chen X, Giles J, Yao Y, Yip W, Meng Q, Berkman L, et al. The path to healthy ageing in China: a Peking University-lancet commission. Lancet. 2022;400:1967–2006. doi: 10.1016/S0140-6736(22)01546-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization. Decade of healthy ageing baseline report. Geneva: World Health Organization; 2021. https://www.who.int/publications/i/item/9789240017900. Accessed 22 June 2023.
- 4.World Health Organization. World report on aging and health. Geneva: World Health Organization; 2015. https://apps.who.int/iris/handle/10665/186463. Accessed 22 June 2023.
- 5.Zhao J, Chhetri JK, Chang Y, Zheng Z, Ma L, Chan P. Intrinsic capacity vs. multimorbidity: a function-centered construct predicts disability better than a disease-based approach in a community-dwelling older population cohort. Front Med (Lausanne) 2021;8:753295. doi: 10.3389/fmed.2021.753295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Health Organization. International classification of functioning, disability and health. Geneva: World Health Organization; 2001. http://www.who.int/classifications/icf/en/. Accessed 22 June 2023.
- 7.Cesari M, de Araujo Carvalho I, AmuthavalliThiyagarajan J, Cooper C, Martin FC, Reginster JY, et al. Evidence for the domains supporting the construct of intrinsic capacity. J Gerontol A Biol Sci Med Sci. 2018;73:1653–1660. doi: 10.1093/gerona/gly011. [DOI] [PubMed] [Google Scholar]
- 8.Beard JR, Jotheeswaran AT, Cesari M, de Araujo Carvalho I. The structure and predictive value of intrinsic capacity in a longitudinal study of ageing. BMJ Open. 2019;9:e026119. doi: 10.1136/bmjopen-2018-026119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yu R, Amuthavalli Thiyagarajan J, Leung J, Lu Z, Kwok T, Woo J. Validation of the construct of intrinsic capacity in a longitudinal chinese cohort. J Nutr Health Aging. 2021;25(6):808–815. doi: 10.1007/s12603-021-1637-z. [DOI] [PubMed] [Google Scholar]
- 10.World Health Organization. Integrated care for older people (icope): guidance for person-centred assessment and pathways in primary care. Geneva: World Health Organization; 2019. https://apps.who.int/iris/handle/10665/326843. Accessed 22 June 2023.
- 11.Leung AYM, Su JJ, Lee ESH, Fung JTS, Molassiotis A. Intrinsic capacity of older people in the community using WHO integrated care for older people (ICOPE) framework: a cross-sectional study. BMC Geriatr. 2022;22:304. doi: 10.1186/s12877-022-02980-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rojano I, Luque X, Blancafort-Alias S, Prat Casanovas S, Forné S, Martín Vergara N, Fabregat Povill P, et al. Identification of decreased intrinsic capacity: performance of diagnostic measures of the ICOPE Screening tool in community dwelling older people in the VIMCI study. BMC Geriatr. 2023;23:106. doi: 10.1186/s12877-023-03799-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lu F, Liu S, Liu X, Li J, Jiang S, Sun X, et al. Comparison of the predictive value of intrinsic capacity and comorbidity on adverse health outcome in community-dwelling older adults. Geriatr Nurs. 2023;50:222–226. doi: 10.1016/j.gerinurse.2023.02.001. [DOI] [PubMed] [Google Scholar]
- 14.Lu S, Liu Y, Guo Y, Ho HC, Song Y, Cheng W, et al. Neighbourhood physical environment, intrinsic capacity, and 4-year late-life functional ability trajectories of low-income Chinese older population: a longitudinal study with the parallel process of latent growth curve modelling. EClinicalMedicine. 2021;36:100927. doi: 10.1016/j.eclinm.2021.100927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Halli-Tierney AD, Scarbrough C, Carroll D. Polypharmacy: evaluating risks and deprescribing. Am Fam Physician. 2019;100(1):32–38. [PubMed] [Google Scholar]
- 16.Miller MD, Towers A (1991). A Manual of Guidelines for Scoring the Cumulative Illness Rating Scale for Geriatrics (CIRS-G).1991. https://www.anq.ch/wp-content/uploads/2017/12/ANQ_Modul_23_CIRS_Manual. Accessed 31 Mar 2023.
- 17.Lawton MP, Brody EM. Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist. 1969;9:179–186. doi: 10.1093/geront/9.3_Part_1.179. [DOI] [PubMed] [Google Scholar]
- 18.Gómez JF, Curcio CL, Alvarado B, Zunzunegui MV, Guralnik J. Validity and reliability of the Short Physical Performance Battery (SPPB): a pilot study on mobility in the Colombian Andes. Colomb Med (Cali) 2013;44:165–171. doi: 10.25100/cm.v44i3.1181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rubenstein LZ, Harker JO, Salvà A, Guigoz Y, Vellas B. Screening for undernutrition in geriatric practice: developing the short-form mini-nutritional assessment (MNA-SF) J Gerontol A Biol Sci Med Sci. 2001;56:M366–M372. doi: 10.1093/gerona/56.6.M366. [DOI] [PubMed] [Google Scholar]
- 20.Tombaugh TN, McIntyre NJ. The Mini-Mental State Examination: a comprehensive review. J Am Geriatr Soc. 1992;40:922–935. doi: 10.1111/j.1532-5415.1992.tb01992.x. [DOI] [PubMed] [Google Scholar]
- 21.Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, Adey M, et al. Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res. 1982;17:37–49. doi: 10.1016/0022-3956(82)90033-4. [DOI] [PubMed] [Google Scholar]
- 22.Jensen GL, Cederholm T, Correia MITD, Gonzalez MC, Fukushima R, Higashiguchi T, et al. GLIM criteria for the diagnosis of malnutrition: A consensus report from the global clinical nutrition community. JPEN J Parenter Enter Nutr. 2019;43:32–40. doi: 10.1002/jpen.1440. [DOI] [PubMed] [Google Scholar]
- 23.Ma L, Chhetri JK, Zhang Y, Liu P, Chen Y, Li Y, et al. Integrated care for older people screening tool for measuring iIntrinsic capacity: preliminary findings from ICOPE pilot in China. Front Med (Lausanne) 2020;7:576079. doi: 10.3389/fmed.2020.576079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ma L, Chhetri JK, Zhang L, Sun F, Li Y, Tang Z. Cross-sectional study examining the status of intrinsic capacity decline in community-dwelling older adults in China: prevalence, associated factors and implications for clinical care. BMJ Open. 2021;11:e043062. doi: 10.1136/bmjopen-2020-043062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cigolle CT, Langa KM, Kabeto MU, Tian Z, Blaum CS. Geriatric conditions and disability: the health and retirement study. Ann Intern Med. 2007;147:156–164. doi: 10.7326/0003-4819-147-3-200708070-00004. [DOI] [PubMed] [Google Scholar]
- 26.Chaudhry SI, McAvay G, Ning Y, Allore HG, Newman AB, Gill TM. Geriatric impairments and disability: the cardiovascular health study. J Am Geriatr Soc. 2010;58:1686–1692. doi: 10.1111/j.1532-5415.2010.03022.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Charles A, Buckinx F, Locquet M, Reginster JY, Petermans J, Gruslin B, et al. Prediction of adverse outcomes in nursing home residents according to intrinsic capacity proposed by the World Health Organization. J Gerontol A Biol Sci Med Sci. 2020;75:1594–1599. doi: 10.1093/gerona/glz218. [DOI] [PubMed] [Google Scholar]
- 28.Huang CH, Okada K, Matsushita E, Uno C, Satake S, Martins BA, et al. The association of social frailty with intrinsic capacity in community-dwelling older adults: a prospective cohort study. BMC Geriatr. 2021;21:515. doi: 10.1186/s12877-021-02466-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zeng X, Shen S, Xu L, Wang Y, Yang Y, Chen L, et al. The impact of intrinsic capacity on adverse outcomes in older hospitalized patients: A one-year follow-up study. Gerontology. 2021;67:267–275. doi: 10.1159/000512794. [DOI] [PubMed] [Google Scholar]
- 30.Locquet M, Sanchez-Rodriguez D, Bruyère O, Geerinck A, Lengelé L, Reginster JY, et al. Intrinsic capacity defined using four domains and mortality risk: A 5-year follow-up of the SarcoPhAge cohort. J Nutr Health Aging. 2022;26:23–29. doi: 10.1007/s12603-021-1702-7. [DOI] [PubMed] [Google Scholar]
- 31.Sánchez-Sánchez JL, Rolland Y, Cesari M, de Souto BP. Associations between intrinsic capacity and adverse events among nursing home residents: the INCUR study. J Am Med Dir Assoc. 2022;23:872–6.e4. doi: 10.1016/j.jamda.2021.08.035. [DOI] [PubMed] [Google Scholar]
- 32.Yu R, Leung J, Leung G, Woo J. Towards healthy ageing: using the concept of intrinsic capacity in frailty prevention. J Nutr Health Aging. 2022;26:30–36. doi: 10.1007/s12603-021-1715-2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets analyzed in the current study are available from the corresponding author upon request.