Abstract
The purpose of this study was to compare the effects of three different intervention strategies, postural education (PE) and two corrective exercise programs (CEPs), on the craniovertebral angle (CVA) in young adults with forward head posture (FHP). A prospective four-arm parallel randomized controlled trial with repeated measures was performed. Seventy-nine healthy young adults (55 women, 24 men; mean age: 20.08 ± 2.19 years) with FHP were randomized into four groups: PE group, self-myofascial release + stretching group (SMRS), self-myofascial release + stretching + strengthening group (SMRSS), and a control group (CG). Participant CVA (°) was assessed before and after a 4-week intervention. Seventy-two participants completed the trial. Mean difference comparisons of within-group change in mean CVA revealed an increase in the PE (MD = 3.1, p < .01), SMRS (MD = 3.8, p < .01), and SMRSS (MD = 4.4, p < .01) groups. Mean difference comparison of between-group change in mean CVA supported greater CVA change in the SMRS and SMRSS groups compared to the CG (F(3, 68) = 5.26, p < .01, η2 = .188). All three interventions appear to be effective techniques for improving FHP in young adults, however CEPs may provide superior outcomes than PE alone. A 4-week CEP consisting of self-myofascial release + stretching may yield similar CVA enhancements as a CEP consisting of self-myofascial release + stretching + strengthening. Study findings can assist fitness professionals in designing evidence-based FHP intervention programs for young adults.
Keywords: Photogrammetry, self-myofascial release, strengthening, stretching
INTRODUCTION
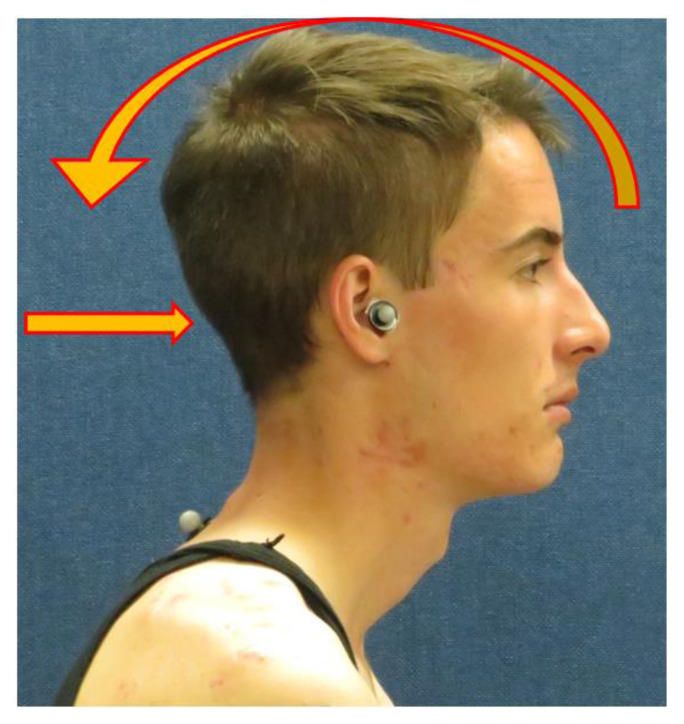
Escalated by technological advancements, the use of computers, laptops, and mobile electronic devices (MEDs), including smartphones and tablets, has dramatically increased over the last 20 years. Studies have reported forward head posture (FHP) prevalence ranging from 52% to 68% in adolescents (63, 78, 79), and from 11.4% to 67% in young adults (36, 48, 60). When using MEDs, 91% of individuals flex their neck to look downward at the device rather than raising it up to eye level (20). Sustained neck flexion facilitates the development of FHP (16, 27, 49, 54, 57, 60). In FHP, the cranium projects anterior to the shoulders, as well as rotates posteriorly in the sagittal plane to enable horizontal optic gaze (Figure 1) (55, 68). Posterior rotation of the cranium can facilitate hyperextension and compression in the suboccipital region (32, 55).
Figure 1.
Mechanism of forward head posture.
Some of the most common ailments associated with FHP include text neck syndrome, generalized neck pain, cervical spine degeneration, myofascial trigger points, headaches, temporomandibular disorders, shoulder abnormalities, and respiratory impairments (18). A need exists for correction of FHP to assist in preventing the onset and chronicity of musculoskeletal conditions (6, 11, 13, 54, 62, 63). If FHP is not addressed during young or middle adulthood, it may persist throughout life as a result of spinal remodeling and degenerative musculoskeletal pathology (16, 57, 71).
The most advantageous methods for professionals to address FHP in their clientele are still up for debate. Two common approaches include postural education (PE) and the implementation of corrective exercise programs (CEPs) (18, 42, 46, 67, 68). PE is a component of ergonomic intervention that incorporates risk factor awareness and postural recommendations when using equipment or devices (42, 66). When individuals possess a greater understanding of health risks associated with FHP it can help improve their proprioception (42). PE also commonly includes topics such as postural guidelines for using computerized technology and recommendations for rest break frequency (42, 46, 56). CEPs are integrated strategies to address an identified neuromuscular dysfunction (18). Once a dysfunction, such as a postural abnormality, has been identified by a qualified professional, corrective exercise techniques and interventions such as self-myofascial release (SMR), stretching, and strengthening exercises are prescribed and implemented (18).
SMR is a technique involving the self-application of mechanical pressure to fascia and muscle tissue for the purpose of enhancing flexibility, reducing muscle soreness, and decreasing neuromuscular overactivity (7, 18). Improvements in FHP, forward shoulder posture, and hyperkyphosis have been observed utilizing a CEP incorporating SMR to the latissimus dorsi, levator scapulae, sternocleidomastoid, thoracic spine, and upper trapezius muscles when combined with a stretching, strengthening, and ergonomic intervention (31).
A stretching program targeting shortened muscles can help restore neutral posture (29, 41, 51, 53, 75). FHP promotes adaptive muscle shortening in the sternocleidomastoid (SCM), upper trapezius (UT), and upper cervical extensors (UCE) (32). In addition, prolonged slouching during MED use also facilitates shortening of the pectoral muscles (PM) in individuals with FHP (35, 39). The most common form of stretching prescribed to address postural abnormalities is static stretching (SS) (18, 29, 53).
FHP also predisposes the development of underactive and overly lengthened muscle groups in the head, neck, and upper thoracic region, contributing to muscle imbalance and the loss of upright head and neck posture (18, 40, 75). Examples include the deep cervical flexors, superficial intrinsic cervical extensors, the upper thoracic/lower cervical erector spinae, and rhomboid muscles (24, 32, 52, 55). Strengthening exercises that engage these muscles can help correct this postural abnormality by improving length-tension relationships and enhancing muscle force production (9, 18, 22, 40).
The majority of studies investigating the effect of corrective exercise programming on FHP incorporate individuals with existing pain or pathology (44, 68). Gaps in the literature exist for knowledge of optimal intervention for the young adult population with FHP who are at risk for developing future pain and/or pathology. It is currently unclear whether PE alone can influence a change in an established clinical measure of head posture, the craniovertebral angle (CVA) (42, 46). The effectiveness of a combined SMR + stretching intervention compared to a CEP incorporating SMR + stretching + strengthening exercises is also presently unknown (21, 53, 64). The purpose of this study was to compare the effects of three different intervention strategies, PE and two CEPs, on the CVA in young adults with FHP. An interrelated objective was to determine which intervention, if any, yields the greatest postural enhancement.
METHODS
Participants
A prospective four-arm parallel randomized controlled trial (ClinicalTrials.gov registration number: NCT05321654) with repeated measures took place on the campus of Liberty University from August to November 2021 in order to compare 3 groups receiving different 4-week interventions to a control group. The institutional review boards of Liberty University (IRB-FY20-21-1073) and Concordia University Chicago (1775403-1) approved this research prior to commencement. Participation in this study was voluntary, and informed consent was acquired from each participant prior to enrollment. This research was carried out fully in accordance with the ethical standards of the International Journal of Exercise Science (47). The authors utilized CONSORT guidelines for reporting parallel group randomized trials and TIDieR checklist and guides for presenting study interventions (26, 43).
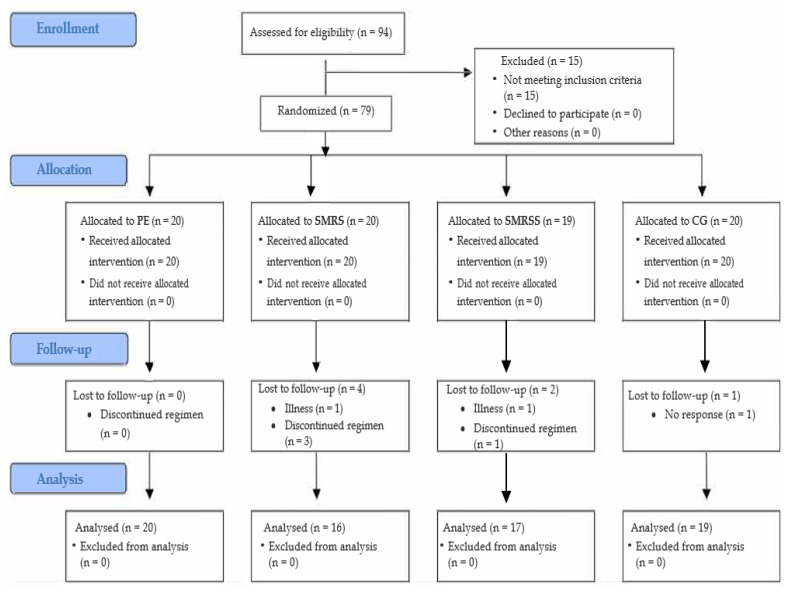
The population consisted of a non-probability sample of convenience to include young adult volunteers between the ages of 18 and 29 years of age (Table 1). A total of 94 participants responded to invitations to participate and completed the 2020 Physical Activity Readiness Questionnaire (2020 PAR-Q+), followed by a questionnaire to rate their current stage of change (SOC) from the transtheoretical model adapted to assess exercise/postural modification behavior change. Participants then underwent a head posture screening in the Liberty University Biomechanics & Motion Analysis Laboratory with the use of photogrammetry. Inclusion criteria were: CVA ≤ 53° (39) and self-identification of SOC stage ≥ 3/5 to indicate their readiness to comply with an assigned exercise prescription or postural guidelines (37). Exclusion criteria consisted of any musculoskeletal injury to the head, shoulders, or spine within the last six months; diagnosis of pathology related to the cervical spine, thoracic spine, or upper extremities; or non-clearance for physical activity based on results of the 2020 PAR-Q+ questionnaire. As depicted in the flow chart of participants through the trial (Figure 2), 79 participants (55 women, 24 men) with mean age of 20.08 ± 2.19 years; mean height of 167.48 ± 8.13 cm;, and mean weight of 70.67 ± 14.32 kg; were initially accepted into the study. Seventy-two participants (51 women, 21 men); mean age: 20.17 ± 2.25 years; mean height: 167.34 ± 8.25 cm; and mean weight: 70.31 ± 14.61 kg completed the trial.
Table 1.
Participant characteristics by group (Mean ± SD).
| Variable | PE (n = 20) | SMRS (n = 16) | SMRSS (n = 17) | CG (n = 19) | p-value* |
|---|---|---|---|---|---|
| Age (Years) | 21.20 ± 3.07 | 20.25 ± 2.05 | 19.59 ± 1.42 | 19.53 ± 1.65 | 0.071 |
| Height (cm) | 167.87 ± 8.52 | 165.73 ± 5.35 | 166.47 ± 8.73 | 168.91 ± 9.71 | 0.676 |
| Weight (kg) | 74.78 ± 15.45 | 66.53 ± 13.06 | 67.34 ± 17.87 | 71.44 ± 10.96 | 0.293 |
SD: Standard deviation; PE: Postural Education; SMRSS: Self-Myofascial Release+Stretching; SMRSS: Self-Myofascial Release+Stretching+Strengthening; CG: Control Group;
p < .05.
Figure 2.
CONSORT flowchart of study design and participant randomization.
The sample size was determined utilizing G*Power software (G*Power, version 3.1.9.7, Germany). Based on calculated results for a repeated measures ANOVA within- and between-factors, a sample size of at least 40 participants was necessary for 80% power (1-β = 0.80) with an effect size of d = 0.5, and an alpha level (type I error) of 0.05. For a one-way ANOVA, a sample size of at least 48 participants was necessary for 80% power (1-β = 0.80) with an effect size of d = 0.5, and an alpha level (type I error) of 0.05. A total of 94 participants initially volunteered to participate in the study. After baseline posture assessment, the researchers excluded 15 individuals from the study due to not meeting inclusion criteria. Out of the 79 participants who began the study, four self-withdrew due to discontinuing the regimen, two withdrew due to illness, and one did not schedule a follow up due to non-response (Figure 2). A total of 72/79 participants completed the study (drop out ratio = 8.9 %). Data sets used during statistical analysis did not include CVA measurements of drop out participants.
Protocol
Participants arrived to the lab wearing either a tank top or t-shirt, as well as had their hair tied back if necessary (63). A digital scale (Health-o-meter Professional, model 500KL, McCook, IL) was used to measure height and weight. The primary investigator (PI), who is a licensed physical therapist with over 20 years of experience, performed posture screening. A 9.5 mm reflective joint marker was placed on the tragus of the participant’s ear, and a 14 mm reflective joint marker was placed over the spinous process of the C7 vertebrae (63). A digital camera (Canon Powershot, model SX540, Tokyo, Japan) was mounted on a tripod (Manfrotto, model 055, Cassola, IT) and leveled utilizing multi-plane circular spirit bubble levels (59). The camera was placed three meters away from the participant (16, 63), orthogonal to the sagittal plane, and adjusted to the height of the C7 spinous process of the participant to aid in lens error reduction (4, 15, 38). Each participant underwent lateral-view postural assessment of their dominant side (33, 63) in the sitting position. Participants sat comfortably on a stool with hands resting approximately two-thirds down their thighs with palms supinated and feet flat on the ground with hips and knees at 90° (62). They performed three repetitions of both neck flexion and extension in their full available pain-free range of motion (34, 80) and then stopped their head to rest in a self-selected “natural” position while looking straight ahead at an opposite wall in the laboratory (16, 33). Once the participant sat motionless for five seconds, a photograph of their head and neck was captured with the digital camera (64). This protocol was repeated without delay to capture a second photograph of the participant’s posture (33). Immediately after data capture, the PI uploaded the image files into Kinovea video analysis software (version 8.15) for CVA assessment.
Randomization of participant group assignments was completed by the PI using a block randomization generator on a website (http://www.randomization.com). Utilizing a sequence created by the block randomizer, the PI placed participants who met inclusion criteria into one of four groups: postural education (PE; n = 20), self-myofascial release + stretching (SMRS; n = 20), self-myofascial release + stretching + strengthening (SMRSS; n = 19), and control group (CG; n = 20). A hard copy of the sequence generator report was kept concealed in a manila folder and was only opened by the PI during group delegation. Participants and researchers were not blinded to group assignment.
Posture Education Group: Immediately after the baseline CVA assessment, PE group members received a one-time 20-minute in-person one-on-one standardized educational session by a research team member in the laboratory. Topics included health risks associated with FHP; postural guidelines for using MEDs, desktop computers, laptop computers, and rest break guidelines (Table 2). At the conclusion of the educational session, each PE group participant was emailed a copy of the presented educational information and guidelines. A weekly email was sent to group members during the 4-week intervention period to provide reminders and encouragement to adhere to postural guidelines. The researchers asked participants not to begin a new exercise program or alter their current physical activity level over the next four weeks.
Table 2.
Summary of the posture education session.
| Topic | Content Outline | References for Educational Content |
|---|---|---|
| Health risks associated with forward head posture |
|
Bayattork et al., 2019 Cuellar & Lanman, 2017 Kalichman et al., 2016 Hansraj, 2014 Lau et al., 2010 |
| Postural guidelines for using mobile electronic devices (MED) |
|
Abdelhameed & Abdelaziem, 2016 Gustaffson, 2012 Syamala et al., 2018 |
| Rest break guidelines for mobile electronic devices (MED) |
|
Kim & Koo, 2016 Neupane et al., 2017 Vate-U-Lan, 2015 |
| Postural guidelines for using desktop computers |
|
NIH, 2021 |
| Postural guidelines for using laptop computers |
|
NIH, 2021 Sahu et al., 2021 |
| Rest break guidelines for computers |
|
Kar & Hedge, 2020 Carter et al., 2018 Engelmann et al., 2011 |
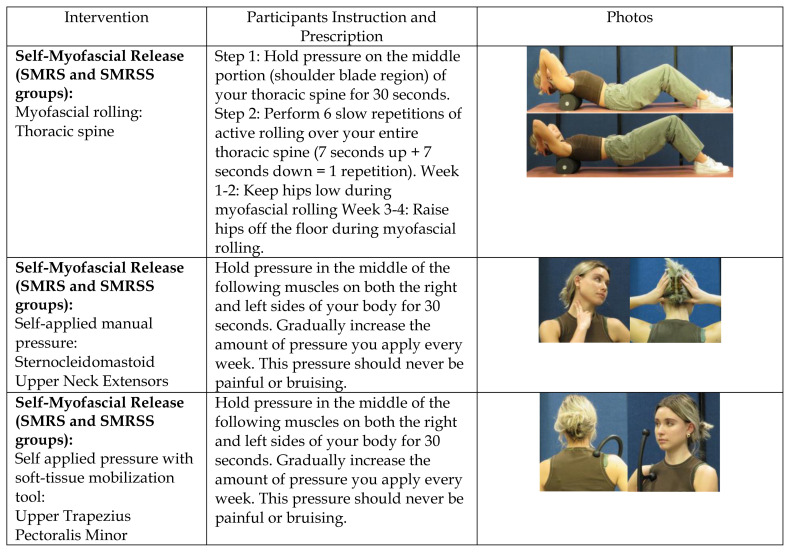
Self-Myofascial Release + Stretching Group: Immediately after the baseline CVA assessment, SMRS group members received a 15-minute in-person one-on-one standardized instructional/training session for the SMRS intervention provided by a research team member in the laboratory (Figure 3). A 12 × 6 × 6 inch high-density myofascial roller (NASM Tool, Cygnet Systems, Dallas, TX) and a 23-inch soft-tissue mobilization tool (STMT) (Therapist’s Choice® Pressure Point Hook Cane, Tampa, FL) was provided to group members at no cost to enable implementation of a 4-week home program. Implemented protocols followed the National Academy of Sports Medicine (NASM) recommendations for inhibitory and lengthening techniques (18). Participants applied SMR to the thoracic spine (TS) using the myofascial roller by holding pressure over the central region of the TS for 30 seconds, followed by six repetitions of active rolling up and down the length of the TS (up + down equaling one repetition) over a 90 second time period to promote mobilization of restricted myofascial tissues and restoration of upright posture (18, 45). Participants applied SMR to the center of the muscle belly in bilateral SCM and UCE using self-applied pressure with fingertips, while the STMT was utilized to administer SMR to center of the muscle belly in bilateral UT and PM for 30 seconds (18). For the first two weeks of the study, participants performed SMR three times per week on nonconsecutive days. During weeks three and four, participants progressed SMR protocol frequency to five days per week. They also performed SS to bilateral SCM, UT, PM, and UCE muscles (Figure 3) after SMR on three non-consecutive days per week. During the first two weeks of the study, participants performed two repetitions of stretches held for 20 seconds, and progressed to three repetitions of 30 seconds, five days per week during weeks three and four. At the conclusion of the training session, each group participant was emailed a copy of instructions for the assigned intervention. A weekly reminder email was sent to group members during the 4-week intervention period to encourage CEP adherence. Researchers asked participants not to begin a new exercise program other than their assigned CEP or alter their current physical activity level during the 4-week intervention period.
Figure 3.
Corrective exercise interventions.
Self-Myofascial Release + Stretching + Strengthening Group: Immediately after the baseline CVA assessment, SMRSS group members received a 20-minute in-person one-on-one standardized instructional/training session provided by a research team member in the laboratory that included the same SMR + stretching protocol as the SMRS group, as well as incorporated strengthening exercises following NASM recommendations for activation and integration techniques (Figure 3) (18). Group participants received a 12 × 6 × 6 inch high-density myofascial roller (NASM Tool, Cygnet Systems, Dallas, TX), a 23-inch soft-tissue mobilization tool (Therapist’s Choice® Pressure Point Hook Cane, Tampa, FL), a 36 inch medium resistance (resistance = 20 lb.) exercise tube with handles (Stroops, model: Slastix Toner, Clearfield, UT), and a 36-inch medium resistance (resistance = 3.7–5.5 lbs.) exercise band (Theraband, Akron, OH) at no cost to enable implementation of the prescribed 4-week home program. Strengthening exercises included the supine chin tuck (SCT), upper thoracic-lower cervical extension (UTLCE), and a single-arm row with trunk rotation (SARTR). The SCT was performed progressed in three phases: Week 1: chin tuck held 2 seconds, 4 second return to start position, repeated five times. Week 2: same as week 1 but incorporated a towel roll placed behind head to enable increased range of motion during the exercise. Week 3 and 4: chin tuck with head lift 1 inch above the towel roll was held for 2 seconds, 4 second return to start position, repeated five times. The UTLCE exercise was performed by placing the resistive exercise band around the back of the head with neck flexed 15–20 degrees. Participants extended their neck to a neutral position against the resistance of the band and held this position for 2 seconds, followed by a 4 second return to the start position. The SARTR exercise was performed by placing one foot forward; completing a single arm row with exercise tubing using the contralateral arm compared to the lead leg; rotating the trunk 90 degrees toward the side of the body performing the row; followed by reversing these movements to return back to start position in a controlled manner. This exercise was performed on both the right and left sides. The UTLCE and SARTR exercises were performed with 1 set of 10 repetitions for weeks 1–2 and progressed to 2 sets of 10 repetitions in weeks 3–4. Participants performed all muscle strengthening exercises three times per week on non-consecutive days throughout the 4-week intervention period. At the conclusion of the training session, each group participant was emailed a copy of instructions for the assigned intervention. A weekly reminder email was sent to group members during the 4-week intervention period to encourage CEP adherence. Researchers asked participants not to begin a new exercise program other than their assigned CEP or alter their current physical activity level during the 4-week intervention period.
Control Group: Immediately after the baseline CVA assessment, researchers informed CG group members they would not be receiving an intervention and asked them not to begin a new exercise program or alter their current physical activity level over the next four weeks.
Intervention Review Session and Post-Intervention Posture Assessment: On week 2, SMRS and SMRSS group members were asked to return to the laboratory for a 10-minute one-on-one intervention training review session. During the session, participants demonstrated their assigned CEP and received immediate feedback on their technique by a member of the research team. Re-instruction was provided if improper form was observed. After the 4-week intervention period, all study participants returned to the laboratory within a five-day period to undergo follow-up CVA assessment using the same data capture and analysis procedures performed at baseline.
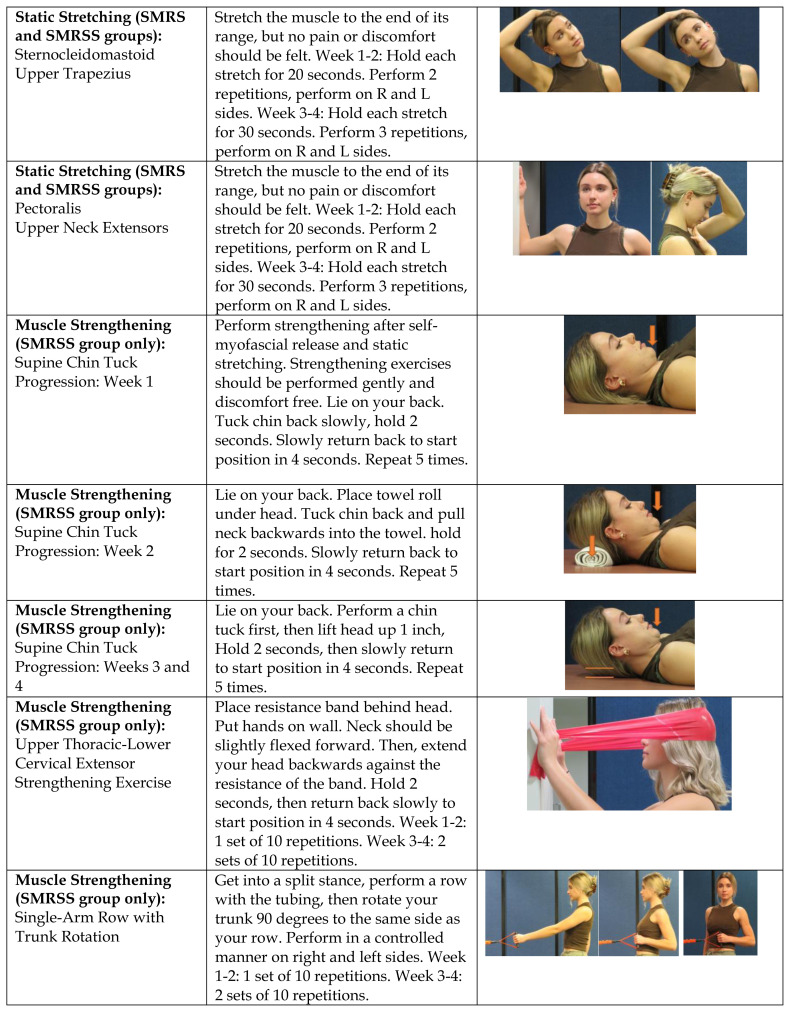
Craniovertebral Angle Assessment: The PI uploaded postural image files into Kinovea video analysis software (version 8.15). This software has been demonstrated to have high validity (r = 1.0 p < .001) and high inter- and intra-tester reliability (ICC (95% CI) > 0.99; p < .001) for joint angle quantification up to 5m from an object compared to AutoCAD engineering software (58). On each image file, the PI assessed participant CVA by measuring the angle between the intersection of two lines: the first line drawn from the tragus of the ear to the spinous process of C7 vertebrae and the second line drawn horizontally through C7 spinous process (Figure 4) (19, 63, 70). The photogrammetric technique for CVA assessment has been found to be valid (r =.89, p < .05) and reliable (ICC (95% CI) = 0.78–0.99, p < .05) compared to radiographic measures (76). A second researcher directly observed the PI perform each CVA assessment, as well as provided verbal agreement with the accuracy of angle measurement. For each participant, the CVA was derived by taking the mean of two CVA measurements that were assessed on the captured photographs (33).
Figure 4.
Craniovertebral angle measurement.
Statistical Analysis
Data analysis was performed using IBM SPSS version 28 for Windows (SPSS Inc., Chicago, IL, USA) and reported with mean and standard deviation. Analysis of descriptive participant characteristics by group was performed using a one-way ANOVA (Table 1). Due to the small sample size, normality of CVA data was assessed using the Shapiro-Wilk test. Mean difference comparison of within-group change in mean CVA measures was completed using a repeated measures ANOVA and the Bonferroni test for adjustment of multiple pairwise comparisons (Table 3). Mean difference comparison of between-group change in mean CVA measures was performed with a one-way ANOVA (Table 4). Due to unequal group sizes, Gabriel’s test was selected for post-hoc comparison. Levene’s test was utilized to assess equality of error variance. Significance level was set at p < .05.
Table 3.
Mean difference comparison of within-group change in mean craniovertebral angle (°).
| Pre | Post | SD | MD | SE | p | ||
|---|---|---|---|---|---|---|---|
|
| |||||||
| M | SD | M | |||||
| PE | 45.1 | 5.9 | 48.1 | 5.9 | 3.1 | 0.64 | <0.001** |
| SMRS | 47.4 | 5.2 | 51.2 | 4.0 | 3.8 | 0.72 | <0.001** |
| SMRSS | 47.1 | 3.9 | 51.4 | 5.4 | 4.4 | 0.70 | <0.001** |
| CG | 46.9 | 4.4 | 47.8 | 5.0 | 0.8 | 0.66 | 0.206 |
M: Mean; SD: Standard Deviation; MD: Mean difference; SE: Standard error; PE: Postural Education; SMRSS: Self-Myofascial Release/Stretching; SMRSS: Self-Myofascial Release/Stretching/Strengthening; CG: Control Group;
p < 0.01.
Bonferroni test utilized for adjustment of multiple pairwise comparisons.
Table 4.
Mean difference comparison of between-group change in mean craniovertebral angle (°).
| Comparison | |||||
|---|---|---|---|---|---|
|
| |||||
| Group | Group | MD | SE | df | p |
| PE | CG | 2.21 | 0.92 | 3.0 | 0.109 |
| SMRS | CG | 2.94 | 0.98 | 3.0 | 0.021* |
| SMRSS | CG | 3.54 | 0.96 | 3.0 | 0.003** |
| PE | SMRS | 0.73 | 0.96 | 3.0 | 0.970 |
| PE | SMRSS | 1.33 | 0.95 | 3.0 | 0.650 |
| SMRS | SMRSS | 0.60 | 1.00 | 3.0 | 0.991 |
MD: Mean Difference; SE: Standard Error; df: Degrees of freedom; PE: Postural Education; CG: Control Group; SMRS: Self-Myofascial Release+Stretching; SMRSS: Self-Myofascial Release+Stretching+Strengthening;
p < .05;
p < .01.
Gabriel post-hoc test utilized for multiple comparisons.
RESULTS
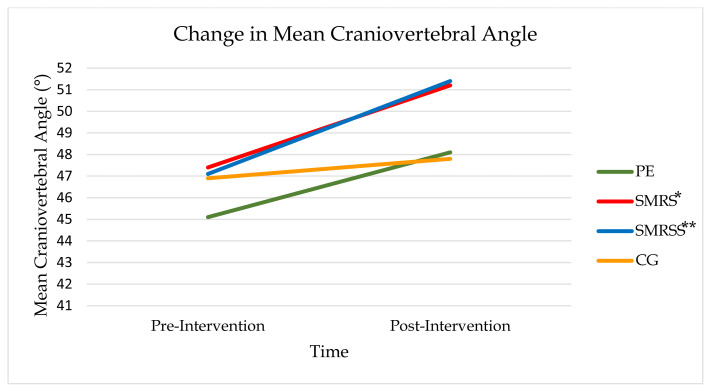
The trial was completed by 72 participants (51 women, 21 men) with a mean age: 20.17 ± 2.25 years; mean height: 167.34 ± 8.25 cm; and mean weight: 70.31 ± 14.61 kg. All participants reported SOC self-rating ≥ 3/5. Figure 2 illustrates a CONSORT flow diagram (8) of participation throughout the study. Pre-intervention analysis revealed no significant difference in participant age (F(3, 68) = 2.45, p > .05), height (F(3, 68) = 0.51, p > .05), or weight (F(3, 68) = 1.27, p > .05) between groups (Table 1). Shapiro-Wilk test, W(72) = .97, p = 0.077, supported normal distribution of CVA data. No significant between-group differences (F(3, 68) = 0.82, p > .05) in baseline CVA were present. Mean difference comparison of within-group change in mean CVA revealed an increase in the PE (MD = 3.1, p < .01), SMRS (MD = 3.8, p < .01), and SMRSS (MD = 4.4, p < .01) groups (F(3, 68) = 5.26, p < .01, η2 = .188, Table 3). Mean difference comparison of between-group change in mean CVA supported greater CVA change in the SMRS (MD = 2.94, p < .05) and SMRSS groups (MD = 3.54, p < .01) compared to the CG (F(3, 68) = 5.26, p < .01, η2 = .188, Table 4, Figure 5).
Figure 5.
Change in mean craniovertebral angle. Change in mean craniovertebral angle was greater in SMRS group* and SMRSS group** compared to CG. *p < .05; ** p < .01.
DISCUSSION
The primary purpose of this randomized control trial was to evaluate the effectiveness of PE or CEP intervention on the CVA in young adults with FHP. The results of this study indicate that fitness professionals who prescribe any of the three intervention protocols used in this study may increase a young adult’s CVA over a 4-week time period, but that CEPs may provide superior postural improvements than PE alone.
To the best of our knowledge, this is the first study to investigate the isolated effects of PE on the CVA. The findings of the present study suggest PE is an effective FHP intervention, as within-group change in mean CVA significantly increased (Table 3) and supports a clinically important difference (5). Studies utilizing checklist rating systems to assess head posture, such as the Rapid Upper Limb Assessment and the Rapid Office Strain Assessment, also support for the use of PE to address FHP (14, 42, 66, 73). In these studies, head posture ratings improved four weeks after one in-person educational session (73), three months after five educational sessions (66), six weeks after six educational sessions (42), and six weeks after 60 minutes of web-based education (14). In the current study, post-intervention CVA significantly increased within the PE group after four weeks, but no difference in CVA change was observed between the PE group and other groups, suggesting PE may be best utilized in conjunction with a CEP rather than a substitute for CEP intervention when addressing FHP in this population.
Although there are examples in the literature where a 4-week CEP consisting of a combined stretching + strengthening intervention yielded CVA improvements (3, 69, 74), to the best of our knowledge, the current study is the first to investigate the effects of a SMR + stretching CEP protocol compared to a SMR + stretching + strengthening CEP protocol on the CVA in young adults with FHP. Three prior studies have utilized a combined SMR + stretching + strengthening CEP to examine potential influences on FHP after 8-week (2) and 12-week (31, 67) durations. In all three studies, researchers reported head posture improvements; however, it should be noted that a different angle than the CVA was utilized to assess head posture, as well as participants in one of the studies (31) received both a CEP and ergonomic educational training concurrently. The results of the present study are in line with the outcomes of these studies, as post-intervention mean CVA change in the SMRSS group was significantly greater than the CG.
One study has been identified that compared the effects of a 12-week muscle strengthening CEP vs a 12-week muscle stretching CEP on FHP in the adolescent population (61). In this study, muscle strengthening intervention was found to be superior to muscle stretching for improving FHP (61). Current study findings suggest that performing SMR immediately prior to static stretching may assist in enhancing stretching effects on CVA improvement, as not only did participants in the SMRS group demonstrate significantly greater CVAs compared to the CG, but no group differences in post-intervention mean CVA change occurred between the SMRS and SMRSS group. These results imply that over the course of four weeks, a SMR + stretching CEP may be just as effective in improving the CVA compared to a SMR + stretching + strengthening CEP.
A primary limitation of the current study was the intervention duration. In attempts to minimize participant drop out due to the COVID-19 pandemic, a 4-week duration was selected. Another limitation was the inability to control for participants’ extra-curricular physical activity level. It is likely that some participants may have been more physically active than others over the 4-week period, which may have influenced outcomes. Other study limitations include the utilization of one team member (the PI) for joint marker placement and CVA assessment, angle measurements in Kinovea software limited to whole numbers (no tenths of degrees), the absence of researcher blinding, and lack of a long-term follow up to evaluate potential lasting effects. Lastly, as this study focused on static posture in young adults without neuromuscular or musculoskeletal pathology, study findings cannot be generalized to dynamic postures, different age groups, or to those with a diagnosed medical condition.
The current study evaluated the effects of PE or CEP intervention on the CVA in young adults with FHP. The results of this study suggest that any of the three intervention protocols utilized in this randomized control trial may increase a young adult’s CVA over the course of four weeks, but that CEPs may yield greater postural improvements than PE. Study outcomes also suggest that clinicians who implement a 4-week CEP consisting of SMR + stretching may yield similar CVA enhancements as a CEP comprised of SMR + stretching + strengthening exercises. To continue to add to the body of research on SMR and its potential benefit on FHP enhancement, it is recommended that future research incorporate longer intervention durations to aid in determining whether SMR may provide additional CVA improvement when combined with stretching compared to a strengthening-only CEP. Comparisons of more intervention combinations, such as SMR + stretching vs stretching only; and a stretching + strengthening protocol with and without SMR; are also suggested to further assist in the determination of optimal CEP programming.
ACKNOWLEDGEMENTS
This study was part of the requirements for completion of a Ph.D. dissertation (Concordia University Chicago) written by Dr. David Titcomb. The authors thank Andrew Fields, Charis Brown, Cassie Brooks, Courtney Green, Theodore Hu, Noah Owens, and Tara Wadford for providing data collection support and intervention instruction. The authors also thank Dr. Kyle Stull for his collaboration, as well as all participants who volunteered for this study. Myofascial rollers and resistive exercise bands used in this study were donated by the National Academy of Sports Medicine (NASM). The Liberty University Center for Research & Scholarship provided funding for the purchase of soft-tissue mobilization tools used in this study [grant number UR2201]. Funding sponsors had no involvement in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit this article for publication.
REFERENCES
- 1.Abdelhameed AA, Abdel-Aziem AA. Exercise training and postural correction improve upper extremity symptoms among touchscreen smartphone us. Hong Kong Physiother J. 2016;35(1):37–44. doi: 10.1016/j.hkpj.2016.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Abdolahzade M, Daneshmandi H. The effect of an 8-week NASM corrective exercise program on upper crossed syndrome. J Sport Biomech. 2019;5(3):156–167. [Google Scholar]
- 3.Abdollahzade Z, Shadmehr A, Malmir K, Ghotbi N. Effects of 4 week postural corrective exercise on correcting forward head posture. J Mod Rehabil. 2017;11(2):85–92. [Google Scholar]
- 4.Alizadehkhaiyat O, Roebuck MM, Makki AT, Frostick SP. Postural alterations in patients with subacromial impingement syndrome. Int J Sports Phys Ther. 2017;12(7):1111–1120. doi: 10.26603/ijspt20171111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arnold BL, Schilling BK. Evidence-based practice in sport and exercise. Philadelphia, PA: FA Davis; 2017. [Google Scholar]
- 6.Bayattork M, Seidi F, Minoonejad H, McClure P, Mozafaripoor E. Intra-rater and inter-rater reliability and agreement of the scapular dyskinesis test in young men with forward head and round shoulder posture. J Rehab Sci Res. 2019;6(4):169–173. [Google Scholar]
- 7.Beardsley C, Škarabot J. Effects of self-myofascial release: A systematic review. J Bodyw Mov Ther. 2015;19(4):747–758. doi: 10.1016/j.jbmt.2015.08.007. [DOI] [PubMed] [Google Scholar]
- 8.Bethell D, Saunders D, Jongkaewwattana A, Kramyu J, Thitithayanont A, Wiboon-ut S, Yongvanitchit K, Limsalakpetch A, Kum-Arb U, Uthaimongkol N, Garcia JM, Timmermans AE, Peiris M, Thomas S, Engering A, Jarman RG, Mongkolsirichaikul D, Mason C, Khemnu N, Tyner SD, Fukuda MM, Walsh DS, Pichyangkul S. CONSORT 2010 flow diagram. PloS One. 2015 [Google Scholar]
- 9.Brody LT, Hall CM. Therapeutic exercise: Moving toward function. 4th ed. Philadelphia, PA: Wolters Kluwer; 2018. [Google Scholar]
- 10.Carter SE, Draijer R, Holder SM, Brown L, Thijssen DH, Hopkins ND. Regular walking breaks prevent the decline in cerebral blood flow associated with prolonged sitting. J Appl Physiol. 2018;125(3):790–798. doi: 10.1152/japplphysiol.00310.2018. [DOI] [PubMed] [Google Scholar]
- 11.Cortese S, Mondello A, Galarza R, Biondi A. Postural alterations as a risk factor for temporomandibular disorders. Acta Odontol Latinoam. 2017;30(2):57–61. [PubMed] [Google Scholar]
- 12.Cuellar JM, Lanman TH. “Text neck”: An epidemic of the modern era of cell phones? Spine J. 2017;17:901–902. doi: 10.1016/j.spinee.2017.03.009. [DOI] [PubMed] [Google Scholar]
- 13.Dağ C, Demirel A, Özalp N. Can temporomandibular joint disorders be diagnosed beforehand by assessment of postural irregularities? Pediatr Res. 2019;6(2):104–109. [Google Scholar]
- 14.Dalkilinc M, Kayihan H. Efficacy of web-based [e-learning] office ergonomics training: A test study. J Musculoskelet Pain. 2014;22(3):275–285. [Google Scholar]
- 15.Diab AA, Moustafa IM. The efficacy of forward head correction on nerve root function and pain in cervical spondylotic radiculopathy: A randomized trial. Clin Rehabil. 2012;26(4):351–361. doi: 10.1177/0269215511419536. [DOI] [PubMed] [Google Scholar]
- 16.Dimitriadis Z, Podogyros G, Polyviou D, Tasopoulos I, Passa K. The reliability of lateral photography for the assessment of the forward head posture through four different angle-based analysis methods in healthy individuals. Musculoskelet Care. 2015;13(3):179–186. doi: 10.1002/msc.1095. [DOI] [PubMed] [Google Scholar]
- 17.Engelmann C, Schneider M, Kirschbaum C, Grote G, Dingemann J, Schoof S, Ure BM. Effects of intraoperative breaks on mental and somatic operator fatigue: A randomized clinical trial. Surg Endosc. 2011;25(4):1245–1250. doi: 10.1007/s00464-010-1350-1. [DOI] [PubMed] [Google Scholar]
- 18.Fahmy R. NASM Essentials of corrective exercise training. 2nd ed. Burlington, MA: Jones & Bartlett Learning; 2022. [Google Scholar]
- 19.Gadotti IC, Armijo-Olivo S, Silveira A, Magee D. Reliability of the craniocervical posture assessment: Visual and angular measurements using photographs and radiographs. J Manipulative Physiol Ther. 2013;36(9):619–625. doi: 10.1016/j.jmpt.2013.09.002. [DOI] [PubMed] [Google Scholar]
- 20.Gold J, Driban J, Thomas N, Chakravarty T, Channell V, Komaroff EG. Postures, typing strategies, and gender differences in mobile device usage: An observational study. Appl Ergon. 2012;43(2):408–412. doi: 10.1016/j.apergo.2011.06.015. [DOI] [PubMed] [Google Scholar]
- 21.Gupta BD, Aggarwal S, Gupta B, Gupta M, Gupta N. Effect of deep cervical flexor training vs. conventional isometric training on forward head posture, pain, neck disability index in dentists suffering from chronic neck pain. J Clin Diagn Res. 2013;7(10):2261. doi: 10.7860/JCDR/2013/6072.3487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gurudut P, Welling A, Chodankar A. Effect of self-care exercises in forward head posture on craniovertebral angle and craniocervical flexion endurance: A pilot study. Indian J Phys Ther Res. 2020;2:1–25. [Google Scholar]
- 23.Gustafsson E. Ergonomic recommendations when texting on mobile phones. Work. 2012;41(1):5705–5706. doi: 10.3233/WOR-2012-0925-5705. [DOI] [PubMed] [Google Scholar]
- 24.Han JW, Kim KH, Bae TS, Blaikie K. Biomechanical analysis of chin tuck exercise with a subject-specific neck model for the forward headed. Int J Precis Eng Manuf. 2018;19(4):587–592. [Google Scholar]
- 25.Hansraj KK. Assessment of stresses in the cervical spine caused by posture and position of the head. Surg Technol Int. 2014;25:277–279. [PubMed] [Google Scholar]
- 26.Hoffmann TC, Glasziou PP, Boutron I, Milne R, Perera R, Moher D, Michie S. Better reporting of interventions: Template for intervention description and replication (TIDieR) checklist and guide. BMJ. 2014;348:g1687. doi: 10.1136/bmj.g1687. [DOI] [PubMed] [Google Scholar]
- 27.Jung SI, Lee NK, Kang KW, Kim K, Do YL. The effect of smartphone usage time on posture and respiratory function. J Phys Ther Sci. 2016;28(1):186–189. doi: 10.1589/jpts.28.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kalichman L, Bulanov N, Friedman A. Effect of exams period on prevalence of myofascial trigger points and head posture in undergraduate students: Repeated measurements study. J Bodyw Mov Ther. 2017;1:11–18. doi: 10.1016/j.jbmt.2016.04.003. [DOI] [PubMed] [Google Scholar]
- 29.Kang JI, Jeong DK, Park SK, Yang DJ, Kim JH, Moon YJ, Baek SY. Effect of self-stretching exercises on postural improvement in patients with chronic neck pain caused by forward head posture. Korean Soc Phys Med. 2020;15(3):51–59. [Google Scholar]
- 30.Kar G, Hedge A. Effects of a sit-stand-walk intervention on musculoskeletal discomfort, productivity, and perceived physical and mental fatigue, for computer-based work. Int J Ind Ergon. 2020;78:102983. doi: 10.1016/j.apergo.2020.103211. [DOI] [PubMed] [Google Scholar]
- 31.Karimian R, Rahnama N, Ghasemi G, Lenjannejadian S. Photogrammetric analysis of upper cross syndrome among teachers and the effects of National Academy of Sports Medicine exercises with ergonomic intervention on the syndrome. J Res Health Sci. 2019;19(3):e00450. [PMC free article] [PubMed] [Google Scholar]
- 32.Khayatzadeh S, Kalmanson OA, Schuit D, Havey RM, Voronov LI, Ghanayem AJ, Patwardhan AG. Cervical spine muscle-tendon unit length differences between neutral and forward head postures: Biomechanical study using human cadaveric specimens. Phys Ther. 2017;97(7):756–766. doi: 10.1093/ptj/pzx040. [DOI] [PubMed] [Google Scholar]
- 33.Kim BB, Lee JH, Jeong HJ, Cynn HS. Effects of suboccipital release with craniocervical flexion exercise on craniocervical alignment and extrinsic cervical muscle activity in subjects with forward head posture. J Electromyogr Kinesiol. 2016;30:31–37. doi: 10.1016/j.jelekin.2016.05.007. [DOI] [PubMed] [Google Scholar]
- 34.Kim EK, Kim JS. Correlation between rounded shoulder posture, neck disability indices, and degree of forward head posture. J Phys Ther Sci. 2016;28(10):2929–2932. doi: 10.1589/jpts.28.2929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kim SY, Koo SJ. Effect of duration of smartphone use on muscle fatigue and pain caused by forward head posture in adults. J Phys Ther Sci. 2016;28(6):1669–1672. doi: 10.1589/jpts.28.1669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kiruthika S, Rekha K, Preethy G, Abraham M. Prevalence of postural dysfunction among female college students-A qualitative analysis. Biol Med. 2018;10(1):421. [Google Scholar]
- 37.Kuroda Y, Sato Y, Ishizaka Y, Yamakado M, Yamaguchi N. Exercise motivation, self-efficacy, and enjoyment as indicators of adult exercise behavior among the transtheoretical model stages. Glob Health Promot. 2012;19(1):14–22. doi: 10.1177/1757975911423073. [DOI] [PubMed] [Google Scholar]
- 38.Lau KT, Cheung KY, Chan MH, Lo KY, Chiu TTW. Relationships between sagittal postures of thoracic and cervical spine, presence of neck pain, neck pain severity, and disability. Man Ther. 2010;15(5):457–462. doi: 10.1016/j.math.2010.03.009. [DOI] [PubMed] [Google Scholar]
- 39.Lee DY, Nam CW, Sung YB, Kim K, Lee HY. Changes in rounded shoulder posture and forward head posture according to exercise methods. J Phys Ther Sci. 2017;29(10):1824–1827. doi: 10.1589/jpts.29.1824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lee KJ, Han HY, Cheon SH, Park SH, Yong MS. The effect of forward head posture on muscle activity during neck protraction and retraction. J Phys Ther Sci. 2015;27(3):977–979. doi: 10.1589/jpts.27.977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Malmström EM, Olsson J, Baldetorp J, Fransson PA. A slouched body posture decreases arm mobility and changes muscle recruitment in the neck and shoulder region. Eur J Appl Physiol. 2015;115(12):2491–2503. doi: 10.1007/s00421-015-3257-y. [DOI] [PubMed] [Google Scholar]
- 42.Mani K, Provident I, Eckel E. Evidence-based ergonomics education: Promoting risk factor awareness among office computer workers. Work. 2016;55(4):913–922. doi: 10.3233/WOR-162457. [DOI] [PubMed] [Google Scholar]
- 43.Moher D, Hopewell S, Schulz KF, Montori V, Gøtzsche PC, Devereaux P, Elbourne D, Egger M, Altman DG. CONSORT 2010 explanation and elaboration: updated guidelines for reporting parallel group randomized trials. J Clin Epidemiol. 2010;63(8):e1–e37. doi: 10.1016/j.jclinepi.2010.03.004. [DOI] [PubMed] [Google Scholar]
- 44.Na JG, Lee HS, Park SW. Effects of exercise type on neck disability, pain, and postural changes in subjects with forward head posture: Systematic review and meta-analysis. Korean Soc Phys Med. 2018;13(3):121–132. [Google Scholar]
- 45.Nakamaru K, Aizawa J, Kawarada K, Uemura Y, Koyama T, Nitta O. Immediate effects of thoracic spine selfmobilization in patients with mechanical neck pain: A randomized controlled trial. J Bodyw Mov Ther. 2019;23(2):417–424. doi: 10.1016/j.jbmt.2018.05.008. [DOI] [PubMed] [Google Scholar]
- 46.Namwongsa S, Puntumetakul R, Neubert MS, Chaiklieng S, Boucaut R. Ergonomic risk assessment of smartphone users using the Rapid Upper Limb Assessment (RULA) tool. PloS One. 2018;13(8):e0203394. doi: 10.1371/journal.pone.0203394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Navalta JW, Stone WJ, Lyons TS. Ethical issues relating to scientific discovery in exercise science. Int J Exerc Sci. 2019;12(1):1–8. doi: 10.70252/EYCD6235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Naz A, Bashir MS, Noor R. Prevalence of forward head posture among university students. Rawal Med J. 2018;43(2):260–262. [Google Scholar]
- 49.Neupane S, Ali UI, Mathew A. Text neck syndrome-systematic review. Imp J Interdiscip Res. 2017;3(7):141–148. [Google Scholar]
- 50.National Institutes of Health. Health and wellness: Prevention. 2021. Available at: https://www.ors.od.nih.gov/sr/dohs/HealthAndWellness/Ergonomics/Pages/prevention.aspx#Computers.
- 51.Olszewska E, Tabor P, Czarniecka R. Magnitude of physiological curvatures of the spine and the incidence of contractures of selected muscle groups in students. Biomed Hum Kinet. 2018;10:31–37. [Google Scholar]
- 52.Page P, Frank CC, Lardner R. Assessment and treatment of muscle imbalance: The Janda approach. Windsor, ON: Human Kinetics; 2010. [Google Scholar]
- 53.Park JH. A study on the impact of continuous antagonist strengthening and Evjenth-Hamberg stretching on the cervical mobility in forward head posture subjects. J Int Acad Phys Ther Res. 2013;4(2):633–639. [Google Scholar]
- 54.Park J, Kim J, Kim J, Kim K, Kim N, Choi I, Lee S, Yim J. The effects of heavy smartphone use on the cervical angle, pain threshold of neck muscles, and depression. Adv Sci Tech Lett. 2015;91(3):12–17. [Google Scholar]
- 55.Patwardhan AG, Khayatzadeh S, Havey RM, Voronov LI, Smith ZA, Kalmanson O, Sears W. Cervical sagittal balance: A biomechanical perspective can help clinical practice. Eur Spine J. 2018;27(1):25–38. doi: 10.1007/s00586-017-5367-1. [DOI] [PubMed] [Google Scholar]
- 56.Pereira M, Comans T, Sjøgaard G, Straker L, Melloh M, O’Leary S, Johnston V. The impact of workplace ergonomics and neck-specific exercise versus ergonomics and health promotion interventions on office worker productivity: A cluster-randomized trial. Scand J Work Environ Health. 2019;45(1):42–52. doi: 10.5271/sjweh.3760. [DOI] [PubMed] [Google Scholar]
- 57.Pop MS, Mihancea P, Debucean D. Posture optimization-Is it the key to myofascial neck pain relief? Arch Balk Med Union. 2018;53(4):573–579. [Google Scholar]
- 58.Puig-Diví A, Escalona-Marfil C, Padullés-Riu JM, Busquets A, Padullés-Chando X, Marcos-Ruiz D. Validity and reliability of the Kinovea program in obtaining angles and distances using coordinates in 4 perspectives. PLoS One. 2019;14(6):e0216448. doi: 10.1371/journal.pone.0216448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Quek J, Pua YH, Clark RA, Bryant AL. Effects of thoracic kyphosis and forward head posture on cervical range of motion in older adults. Man Ther. 2013;18(1):65–71. doi: 10.1016/j.math.2012.07.005. [DOI] [PubMed] [Google Scholar]
- 60.Ramalingam V, Subramaniam A. Prevalence and associated risk factors of forward head posture among university students. Indian J Public Health Res Dev. 2019;10(7):775–780. [Google Scholar]
- 61.Ranjbar M, Madialagan DS. Analysis of strength training corrective exercise and stretch training corrective exercise for cervical curvature angle in secondary high school students. Int J Multidiscip Educ Res. 2020;9(4):147–156. [Google Scholar]
- 62.Richards KV, Beales DJ, Smith AJ, O’Sullivan PB, Straker LM. Neck posture clusters and their association with biopsychosocial factors and neck pain in Australian adolescents. Phys Ther. 2016;96(10):1576–1587. doi: 10.2522/ptj.20150660. [DOI] [PubMed] [Google Scholar]
- 63.Ruivo RM, Pezarat-Correia P, Carita AI. Cervical and shoulder postural assessment of adolescents between 15 and 17 years old and association with upper quadrant pain. Braz J Phys Ther. 2014;18(4):364–371. doi: 10.1590/bjpt-rbf.2014.0027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Ruivo RM, Pezarat-Correia P, Carita AI. Effects of a resistance and stretching training program on forward head and protracted shoulder posture in adolescents. J Manipulative Physiol Ther. 2017;40(1):1–10. doi: 10.1016/j.jmpt.2016.10.005. [DOI] [PubMed] [Google Scholar]
- 65.Sahu M, Sundari KG, David A. Recent ergonomic interventions and evaluations on laptop, smartphones, and desktop computer users. In: Arockiarajan A, Duraiselvam M, Raju R, editors. Advances in industrial automation and smart manufacturing. New York, NY: Springer; 2021. [Google Scholar]
- 66.Sanaeinasab H, Saffari M, Valipour F, Alipour HR, Sepandi M, Al Zaben F, Koenig HG. The effectiveness of a model-based health education intervention to improve ergonomic posture in office computer workers: A randomized controlled trial. Int Arch Occup Environ Health. 2018;91(8):951–962. doi: 10.1007/s00420-018-1336-1. [DOI] [PubMed] [Google Scholar]
- 67.Seidi F, Rajabi R, Ebrahimi I, Alizadeh MH, Minoonejad H. The efficiency of corrective exercise interventions on thoracic hyper-kyphosis angle. J Back Musculoskel Rehabil. 2014;27(1):7–16. doi: 10.3233/BMR-130411. [DOI] [PubMed] [Google Scholar]
- 68.Sheikhhoseini R, Shahrbanian S, Sayyadi P, O’Sullivan K. Effectiveness of therapeutic exercise on forward head posture: A systematic review and meta-analysis. J Manipulative Physiol Ther. 2018;41(6):530–539. doi: 10.1016/j.jmpt.2018.02.002. [DOI] [PubMed] [Google Scholar]
- 69.Singh V, Singh S, Kaushal K. Effect of exercise program on forward head posture and chest expansion in students of Adesh University. Int J Health Sci Res. 2020;10(3):168–171. [Google Scholar]
- 70.Singla D, Veqar Z, Hussain ME. Photogrammetric assessment of upper body posture using postural angles: A literature review. J Chiropr Med. 2017;16(2):131–138. doi: 10.1016/j.jcm.2017.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Stone MA, Osei-Bordom DC, Inman RD, Sammon C, Wolber LE, Williams FM. Heritability of spinal curvature and its relationship to disc degeneration and bone mineral density in female adult twins. Eur Spine J. 2015;24(11):2387–2394. doi: 10.1007/s00586-014-3477-6. [DOI] [PubMed] [Google Scholar]
- 72.Syamala KR, Ailneni RC, Kim JH, Hwang J. Armrests and back support reduced biomechanical loading in the neck and upper extremities during mobile phone use. Appl Ergon. 2018;73:48–54. doi: 10.1016/j.apergo.2018.06.003. [DOI] [PubMed] [Google Scholar]
- 73.Syazwan AI, Azhar MM, Anita AR, Azizan HS, Shaharuddin MS, Hanafiah JM, Kasani A. Poor sitting posture and a heavy schoolbag as contributors to musculoskeletal pain in children: An ergonomic school education intervention program. J Pain Res. 2011;4:287–296. doi: 10.2147/JPR.S22281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Szczygieł E, Sieradzki B, Masłoń A, Golec J, Czechowska D, Węglarz K, Golec E. Assessing the impact of certain exercises on the spatial head posture. Int J Occup Med Environ Health. 2019;32(1):43–51. doi: 10.13075/ijomeh.1896.01293. [DOI] [PubMed] [Google Scholar]
- 75.Thigpen CA, Padua DA, Michener LA, Guskiewicz K, Giuliani C, Keener JD, Stergiou N. Head and shoulder posture affect scapular mechanics and muscle activity in overhead tasks. J Electromyogr Kinesiol. 2010;20(4):701–709. doi: 10.1016/j.jelekin.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 76.Van Niekerk SM, Louw Q, Vaughan C, Grimmer-Somers K, Schreve K. Photographic measurement of upper-body sitting posture of high school students: A reliability and validity study. BMC Musculoskelet Disord. 2008;9(1):1–11. doi: 10.1186/1471-2474-9-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Vate-U-Lan P. Text neck epidemic: A growing problem for smart phone users in Thailand. Int J Comput Internet Manage. 2015;23(3):551–556. [Google Scholar]
- 78.Verma SL, Shaikh J, Mahato RK, Sheth MS. Prevalence of forward head posture among 12–16 year old school going students: A cross sectional study. Appl Med Res. 2018;4(2):18–21. [Google Scholar]
- 79.Wiguna NP, Wahyuni N, Indrayani AW, Wibawa A, Thanaya SAP. The relationship between smartphone addiction and forward head posture in junior high school students in North Denpasar. Jurnal Epidemiol Kesehatan Komunit. 2019;4(2):84–89. [Google Scholar]
- 80.Yip CHT, Chiu TTW, Poon ATK. The relationship between head posture and severity and disability of patients with neck pain. Man Ther. 2008;13(2):148–154. doi: 10.1016/j.math.2006.11.002. [DOI] [PubMed] [Google Scholar]