Abstract
Background.
The Member States of the European Region (EUR) of the World Health Organization (WHO) have made great progress towards achieving the goal of measles elimination by 2010.
Methods.
Measles surveillance and vaccine coverage data from 2003–2009 reported to WHO were analyzed. A review of feasibility of reaching the elimination goal by the 2010 target date was conducted in 2009.
Results.
From 2003–2009, the measles incidence decreased dramatically and coverage with 2 doses of measles vaccine increased among wide age groups of susceptible persons. With the decrease of disease incidence and the reduction of outbreaks in the eastern part of EUR, the proportion of reported cases in the western part increased. In 2009, outbreaks in 5 countries accounted for 89.6% of reported cases. Challenges to reach the 2010 goal include ongoing outbreaks with reestablished endemicity in some countries, decreased demand for vaccines with an increased focus on the measles vaccine safety, and population groups with limited access to immunization services.
Conclusions.
Measles elimination in EUR is attainable, albeit not by 2010. EUR countries should ensure political commitment and resources to protect the gains made to date and address these challenges to sustain the progress and achieve the elimination goal.
BACKGROUND
After introduction of measles vaccine into routine immunization schedules of the 53 member states of the European Region (EUR) of the World Health Organization (WHO), there was a dramatic decrease in the rate of measles. In 2002, the European Region adopted a goal: elimination of measles and rubella by 2010 [1, 2] using the strategy outlined in Table 1 [3]. Activities are focused on reaching elimination through strengthening immunization systems to achieve high (≥95%) coverage with 2 doses of measles vaccine and at least 1 dose of rubella vaccine through routine immunization services. In countries with large cohorts susceptible to measles virus, one-time catch-up supplementary immunization activities (SIAs) were conducted in wide-target age groups (up to 40 years in some countries). EUR countries generally rely on routine immunization rather than follow up SIAs to maintain high 2-dose coverage in young children. The strategy also includes advocacy efforts, such as European Immunization Week (EIW), to provide health care professionals with accurate and relevant information on measles disease and vaccine safety.
Table 1.
Key Components of the Measles and Rubella Elimination Strategy in the World Health Organization European Region
| Strategies: |
|---|
|
|
| 1. Achieving and sustaining very high (≥95%) coverage with 2 doses of MCV and ≥1 dose of rubella vaccine through high-quality routine immunization services |
| 2. Providing a second opportunity for measles immunization through SIAs to populations susceptible to measles; and using the opportunity provided by SIAs to target populations susceptible to rubella |
| 3. Strengthening surveillance systems by rigorous case investigation and laboratory confirmation of suspected measles cases. |
| 4. Improving the availability of high-quality information for health professionals and the public on the benefits and risks associated with immunization against measles and rubella. |
NOTE. MCV, measles-containing vaccine; SIA, supplementary immunization activity.
Monitoring progress towards achieving the goal of measles elimination relies on quality surveillance and accurate reporting of vaccine coverage. To assess progress, to identify remaining challenges, and to identify approaches to address these challenges, we reviewed data on measles epidemiology, vaccine coverage, and surveillance activities in the European Region during 2003–2009. (For the purpose of this report, the 53 Member States of the European Region were grouped into the following subregions: Western Europe (WE): Andorra, Austria, Belgium, Cyprus, Denmark, Finland, France, Germany, Greece, Iceland, Ireland, Israel, Italy, Luxembourg, Malta, Monaco, the Netherlands, Norway, Portugal, San Marino, Spain, Sweden, Switzerland, Turkey, and the United Kingdom; Central and Eastern Europe (CEE): Albania, Bosnia and Herzegovina, Bulgaria, Croatia, Czech Republic, Estonia, Hungary, Latvia, Lithuania, the Former Yugoslav Republic of Macedonia, Montenegro, Poland, Romania, Serbia, Slovakia, and Slovenia; and Newly Independent States (NIS) of former Soviet Union: Armenia, Azerbaijan, Belarus, Georgia, Kazakhstan, Kyrgyzstan, Republic of Moldova, Russian Federation, Tajikistan, Turkmenistan, Ukraine, and Uzbekistan.)
METHODS
Aggregate counts of measles cases, vaccine coverage, and vaccination schedules submitted annually to the WHO Regional Office for Europe using the WHO/the United Nations Children’s Fund (UNICEF) Joint Reporting Form were reviewed for the period 1991–2009 [4, 5]. Since 2002, countries have been encouraged to report case-based data (eg, age, vaccination status, and laboratory confirmation status for individual measles cases) and data on measles outbreaks on a monthly basis. At national levels, different methods are used to collect information from local health authorities, including aggregate, case-based, and sentinel physician reporting. The European Regional Office uses a computerized information system for infectious diseases (CISID) [6] with monthly reporting of surveillance data by countries. Twenty-seven member states of the European Union and Croatia, Iceland, Norway, Switzerland, and Turkey report to the CISID through EUVAC.NET [7]. The EUR laboratory network for measles and rubella surveillance comprises 51 national laboratories, as of 2009, using standardized diagnostic methods and reagents, and 4 regional reference laboratories providing external quality assurance to the national laboratories and sequencing viruses. Laboratories report measles and rubella testing results and performance diagnostics online each month to the Regional Office and the Regional Office provides feedback to them on their performance using standardized indicators. A quality assessment program, which includes an annual accreditation review and proficiency testing, is in place. Coverage data during SIAs were reported by countries with independent evaluations in 6 countries (Armenia, Azerbaijan, Kyrgyzstan, Tajikistan, Turkmenistan, and Uzbekistan) that confirmed the high coverage achieved in these campaigns.
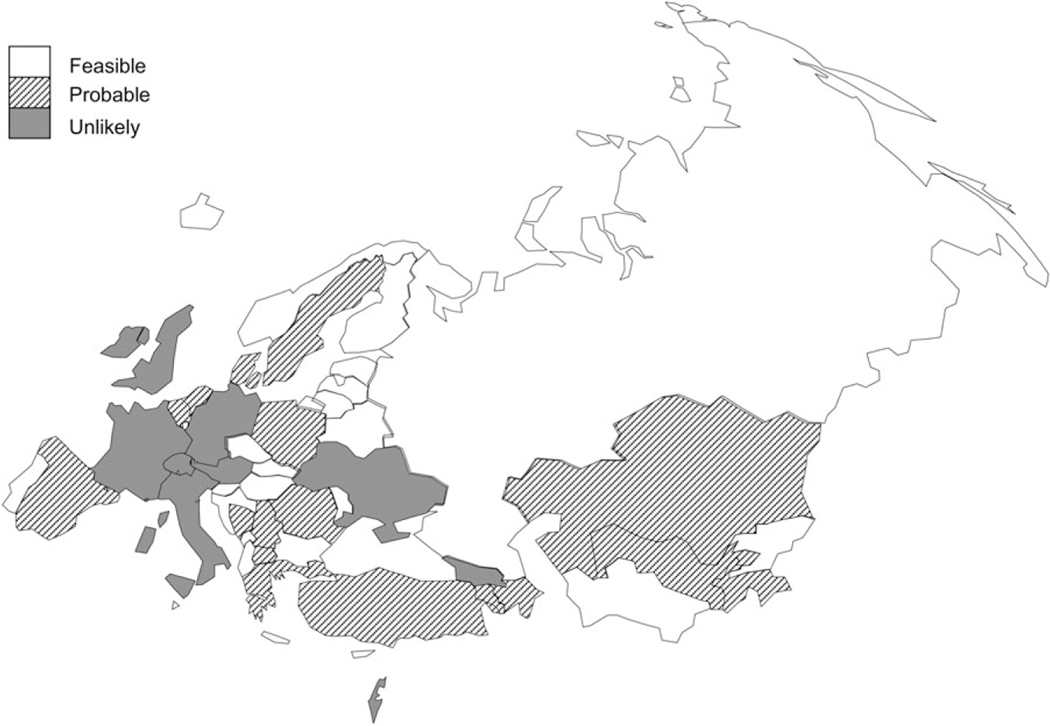
A review of feasibility of reaching the elimination goal by the 2010 target date for the entire region and for each country was conducted in 2009. The likelihood of measles elimination was assessed as “feasible,” “probable,” or “unlikely” on the basis of disease incidence, routine immunization coverage, quality of SIAs, surveillance performance, and overall progress made by each country.
RESULTS
Trends in Measles Incidence
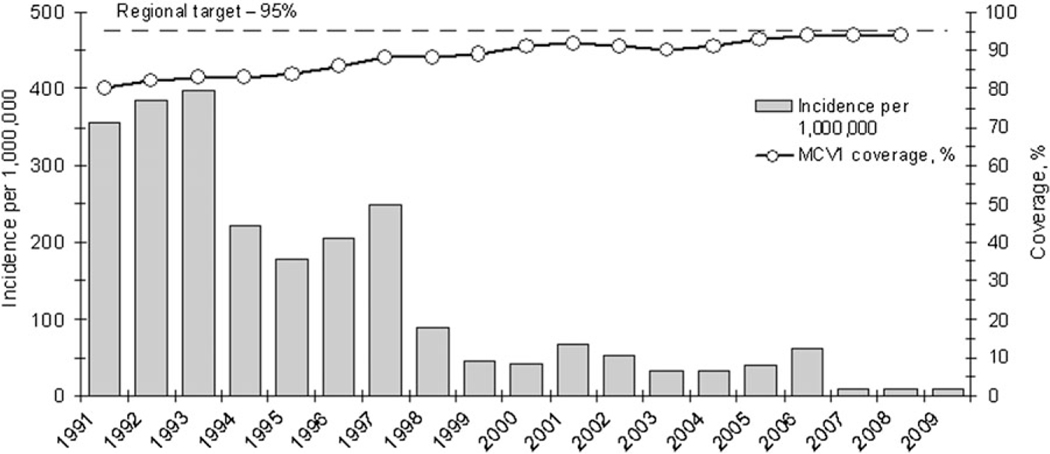
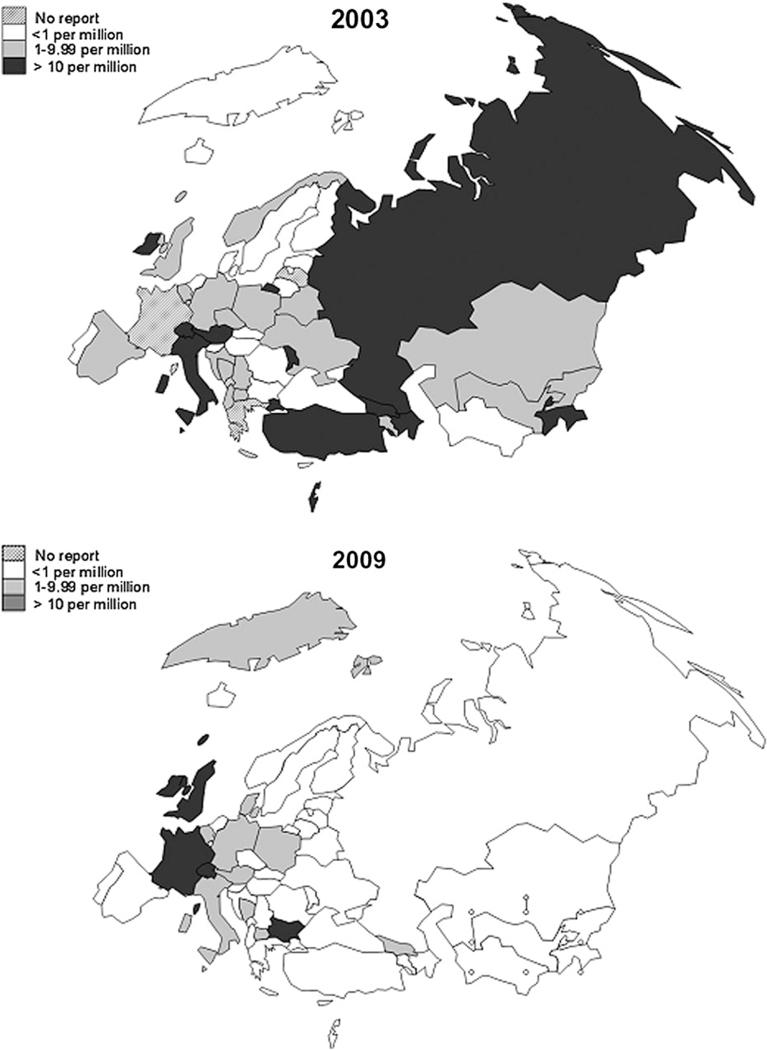
The incidence of measles decreased from almost 400 cases per 1,000,000 population (304,214–342,031 cases) during 1991–1993 to 7.8–10.1 cases per 1,000,000 population (6969–8983 cases) during 2007–2009 (Figure 1). The number of countries with a 0 or low (<1 per 1,000,000) incidence of measles increased from 17 in 2003 to 38 in 2009, including 21 countries with no reported cases of measles (Figure 2). In 2009, only 5 countries (Bulgaria, France, Germany, Switzerland, and the United Kingdom) had high rates of measles incidence (>10 cases per 1,000,000 population), compared with 10–14 countries with high incidence during 2003–2008. These 5 countries accounted for 6475 (89.6%) of the 7375 cases reported in EUR during 2009.
Figure 1.
Reported measles incidence (per 1,000,000 population) and measles-containing vaccine (MCV) 1 coverage, European Region, 1991–2009
Figure 2.
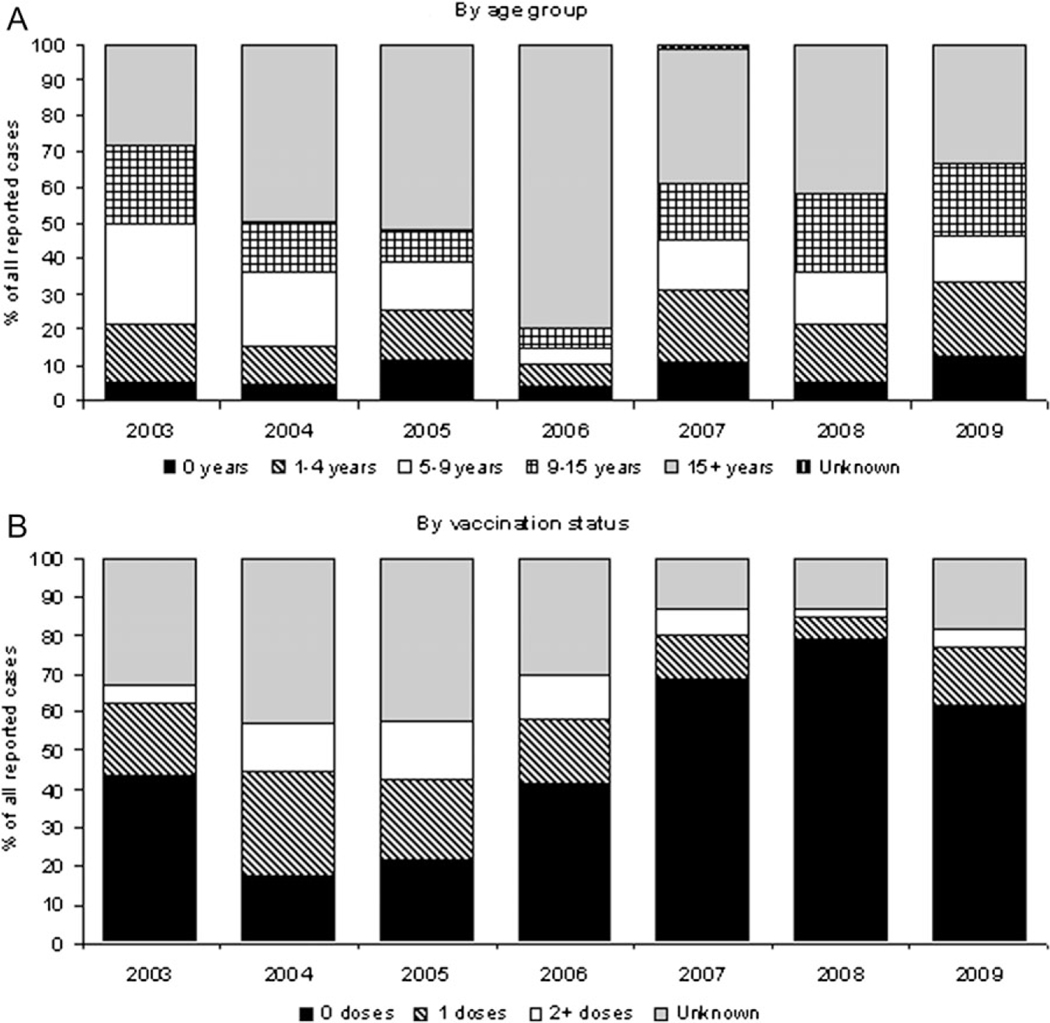
Distribution of reported measles cases by age group and vaccination status, European Region, 2003–2009.
During 2004–2006, 79.5%–96.1% of all measles cases reported annually were from CEE and NIS countries, where large-scale nationwide outbreaks were occurring. Beginning in 2007, the decrease in incidence has been most noticeable in NIS, where <1 case per 1,000,000 population was reported in both 2008 and 2009; and in CEE, where incidence fell to 1.1 case per 1,000,000 population in 2008. In 2007, the outbreaks in the eastern part of EUR subsided, and 58.9%–95.7% of annual cases were reported in western Europe (WE). In western Europe, incidence was substantially higher in 2009 (11.4 cases per 1,000,000) than in 2005 (3.5 cases per 1,000,000) (Table 2). An increase in incidence in CEE from 2008 to 2009 was due to an outbreak in Bulgaria, which accounted for 30.9% (n = 2249) of all reported cases in EUR in 2009. When Bulgaria was excluded, incidence in other CEE countries was 1.0 case per 1,000,000 population.
Table 2.
Reported Measles Incidence, by Country Group, European Region, 2003–2009
| 2003 |
2004 |
2005 |
2006 |
2007 |
2008 |
2009 |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Characteristic | No. of countries | Incidence | No. of countries | Incidence | No. of countries | Incidence | No. of countries | Incidence | No. of countries | Incidence | No. of countries | Incidence | No. of countries | Incidence |
|
| ||||||||||||||
| Member states in the region | 53 | 32.0 | 53 | 33.4 | 53 | 42.2 | 53 | 60.8 | 53 | 7.8 | 53 | 10.1 | 53 | 8.2 |
| Countries, by MCV coverage | ||||||||||||||
| Coverage rate of ≥95% for both MCV1 and MCV2 | 16 | 8.7 | 18 | 14.9 | 18 | 76.5 | 13 | 160.3 | 20 | 3 | 16 | 0.6 | 15 | 5.11 |
| Coverage rate of ≥95% for either MCV1 or MCV2 | 12 | 21 | 8 | 93.1 | 10 | 21.8 | 10 | 13.1 | 9 | 13.8 | 8 | 42.8 | 17 | 14.79 |
| Coverage rate of <95% for both MCV1 and MCV2 | 10 | 44.1 | 12 | 36 | 8 | 30.9 | 13 | 12.4 | 10 | 5.7 | 18 | 7.1 | 14 | 12.23 |
| Countries includeda | 38 | 38 | 36 | 36 | 39 | 42 | 46 | |||||||
| Subregions | ||||||||||||||
| Western Europe | 24 | 37.8 | 24 | 15.2 | 24 | 3.5 | 24 | 11.7 | 24 | 9.9 | 24 | 20.8 | 24 | 11.4 |
| Central and eastern Europe | 17 | 30.3 | 17 | 46.2 | 17 | 58.3 | 17 | 14.8 | 17 | 3.2 | 17 | 1.1 | 17 | 12.4 |
| Newly independent states | 12 | 25.9 | 12 | 52.1 | 12 | 83.6 | 12 | 171.4 | 12 | 8.0 | 12 | 0.6 | 12 | 0.5 |
| Countries, by income levelb | ||||||||||||||
| High | 25 | 34.6 | 25 | 15.1 | 25 | 3.5 | 27 | 11.4 | 29 | 9.3 | 30 | 19.4 | 30 | 10.5 |
| Upper middle | 8 | 1.3 | 10 | 39.3 | 11 | 38.4 | 13 | 12.3 | 12 | 2.4 | 13 | 0.7 | 13 | 7.7 |
| Lower middle | 16 | 30.2 | 14 | 85.8 | 14 | 171.8 | 10 | 507.2 | 9 | 14.3 | 7 | 1.4 | 7 | 0.7 |
| Low | 4 | 56.4 | 4 | 2.2 | 3 | 42.8 | 3 | 21.9 | 3 | 23.0 | 3 | 0.5 | 3 | 0 |
NOTE. Incidence was the no. of cases per 1,000,000 population. Coverage data for 2009 were not available at the time of writing this report.
MCV, measles-containing vaccine.
Only countries for which both MCV1 and MCV2 data for the given year were available are included in this analysis.
According to the World Bank classification [http://data.worldbank.org/about/country-classifications] accessed 04/21/11.
The greatest progress was seen in low-income countries, which had incidence rate of 0.5 cases per 1,000,000 population in 2008 and no cases reported in 2009 (Table 2). The rates among lower-middle income countries were higher than in the other income groups during 2004–2006 but have since decreased to low levels (ie, <1 case per 1,000,000 population) of measles incidence. The 2009 outbreak in Bulgaria reversed the decrease in the incidence observed in upper-middle income countries. The highest rates during 2008–2009 were reported in upper-income countries (Table 2).
The measles incidence was lowest for countries with ≥95% coverage for both measles-containing vaccine (MCV) 1 and MCV2, and highest for countries with <95% coverage for both MCV1 and MCV2 (Table 2). However, during 2005–2006, the majority of cases were reported in CEE and NIS among older children and adults—age groups that were not targeted through current routine immunization programs (Figure 1) and for which access to 2 doses of measles vaccine was not part of countries’ recommendation in the past.
Each year during 2003–2009, older children (ie, those aged 10–14 years) and adults (age, ≥15 years) accounted for most measles cases (50.5% in 2003 and 84.9% in 2006) in EUR (Figure 3a). The highest proportion of unvaccinated cases was observed for years when the most cases occurred in western Europe, whereas the proportion of partial or fully vaccinated cases was observed during 2003–2006, when most cases were seen in CEE and NIS (Figure 3b).
Figure 3.
Incidence of measles (per 1,000,000 population) in the European Region, 2003 vs 2009.
During 2003–2006, data on hospitalization status were provided for 9.9%–22.0% of reported cases, and at least 2.0%–21.0% of all reported cases annually required hospitalization. Completeness of reporting hospitalization status improved during 2007–2009 to 73.9%–99.1% of all cases, and 16.2%–38.1% of reported measles cases required hospitalization. In general, the proportion of hospitalized patients was higher in NIS and CEE, where patients with measles are routinely hospitalized; in other countries, patients with more severe cases are generally hospitalized. During 2003–2009, 52 measles-related deaths were reported from 16 countries. Nearly onehalf (47%) of the deaths for which age was reported occurred in persons aged ≥10 years, whereas 44% were reported among children aged <5 years. Furthermore, 83% of the persons who died had received never been vaccinated (n = 40) or received 1 dose (n = 3) of a MCV.
Widespread nationwide outbreaks reported during 2004–2006 primarily occurred in NIS and CEE countries (eg, Romania, Ukraine, and Georgia) and involved a high proportion of older persons and previously vaccinated persons (Figure 3). Most of the outbreaks since 2007 have been focused in unvaccinated or undervaccinated (ie, recipients of only 1 dose of MCV who were eligible for 2 doses) persons from susceptible subgroups, such as persons who object to vaccination on religious or philosophical grounds or because of safety concerns or vulnerable populations with problems with access to health services. Outbreaks in the general population due to long-term low measles, mumps, and rubella (MMR) uptake, sometimes spanning over several years, have occurred in western Europe (eg, the United Kingdom, Ireland, and Switzerland).
Reaching and Sustaining High Coverage With 2 Doses of MCV
Since 2002, all EUR countries have adopted a 2-dose MCV schedule for routine childhood vaccination programs. Fifty-two member states use MMR vaccine, and Tajikistan uses a measles and rubella vaccine. As of 2009, the earliest recommended age for MCV1 administration was 11–12 months in 33 countries and 13–18 months in 20 countries. The recommended age for MCV2 administration is ≤6 years in 39 countries and 7–12 years in 14 countries.
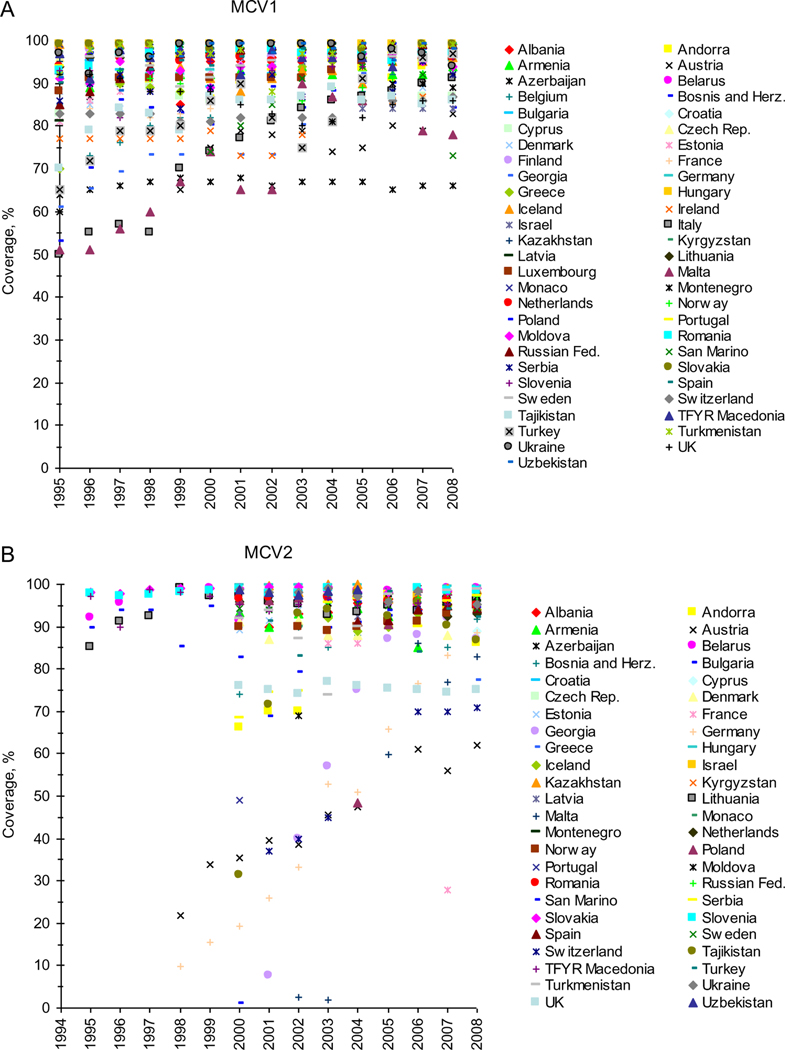
Regional MCV1 coverage rates increased from 90% in 2003 to 94% in 2008 (Figure 1). During 2003–2008, the number of countries reporting ≥95% coverage for MCV1 ranged from 29 in 2003 to 35 in 2007. The number of countries reporting ≥95% coverage for MCV2 ranged from 18 (in 2006) to 23 in 2007 and 2008. However, MCV1 and MCV2 coverage varied widely across the region (Figure 4). Each year during 2003–2008, 11–16 countries reported <90% nationwide MCV1 coverage, including 1–4 countries where the rate of MCV1 coverage was <80%. Similarly, 4–12 countries each year reported a MCV2 coverage rate <90%, including 3–7 countries with <80% MCV2 coverage. Each year, 11–17 countries did not report their MCV2 coverage during this period.
Figure 4.
Measles-containing vaccine (MCV) 1 and MCV2 coverage, European Region, 1995–2008.
In 2008, six countries had a rate of MCV1 coverage ≥95%, and 18 countries had a rate of MCV1 coverage ≥90% in all districts. The number of countries that had districts with <80% MCV1 coverage decreased from 10 in 2004 to 6 in 2008.
Providing a Second Measles Vaccination Opportunity Through SIAs
SIAs involving wide age range (up to 40 years) have been conducted throughout the region and are discussed in detail elsewhere [8, 9]. During 2003–2009, nationwide catch-up SIAs were conducted in Armenia, Azerbaijan, Croatia, Georgia, Ireland, Kazakhstan, Kyrgyzstan, Republic of Moldova, Russian Federation, Serbia, Tajikistan, Turkey, Turkmenistan, and Uzbekistan, achieving ≥94% coverage in all countries except Ireland (70.8% coverage), and Georgia (50.3%) and reaching >55 million persons. Combination vaccines containing both measles and rubella components were widely used, allowing rubella susceptibility to be addressed as well. Unfounded vaccine safety concerns affected 2 SIAs in 2008, leading to the suspension of the SIA in Ukraine and low (50.3%) coverage in the SIA in Georgia. Substantial decreases in measles incidence were observed in all countries after the SIAs. In 2009, the overall measles incidence in countries where SIAs were successfully implemented was at an all-time low, with Armenia, Kazakhstan, Kyrgyzstan, Republic of Moldova, Tajikistan, Turkmenistan, and Uzbekistan reporting no measles cases and Azerbaijan, Croatia, Russian Federation, Serbia, and Turkey having <1 reported case per 1,000,000 population.
Ensuring High Quality Surveillance
Case-based surveillance for measles, introduced in 2002, was adopted by 40 countries in 2009. The proportion of confirmed cases increased from 2.2% in 2003 to 68.2% in 2009. Since 2004, countries began to report on the number of discarded cases (reported by 14 countries in 2009). However, during 2007–2009, the region did not meet the ≥80% target for several indicators of high-quality surveillance, such as proportion of suspected cases with adequate investigation, with blood specimens collected, and with results of laboratory testing reported ≤7 days after the arrival of specimens to laboratory. In 2009, 43 countries (81%) reported surveillance data to the Regional Office; 28 (53%) of countries reported on time.
In 2009, 51 national laboratories the Regional Laboratory Network for measles and rubella tested 18,266 specimens for measles, of which 3133 (17.2%) yielded positive results. By comparison, in 2003, 46 national laboratories tested 2789 specimens, of which 831 (29.8%) yielded positive results. During 2007–2009, measles virus genotyping from reported outbreaks in the region increased from 41% (14 of 34) in 2007 to 75% (12 of 16) in 2009. The most commonly detected genotypes of measles virus in the region were D4 and D5; other identified genotypes included B3, D8, D9, and H1. Genotype D6, a predominant genotype during 2004–2006, has not been detected since 2007 [10].
Improving Available Vaccine Information Through EIW
To strengthen political commitment to immunization programs, mobilize communities, and provide high quality reliable information about vaccination, the annual EIW was established in 2005. The WHO European Regional Office facilitates member states’ efforts to advocate for and strengthen awareness among political leaders, health care professionals, and the general population about measles and rubella elimination through the protection of children through immunization [11]. Participation in EIW has grown from 6 countries in 2005 to 36 countries in 2009. conducting catch-up immunization and increasing awareness of vaccine safety of health care professionals through training and workshops.
Feasibility of Measles Elimination by the 2010 Target Date
The likelihood of measles elimination by 2010 was assessed as “feasible” for 23 countries (ie, Albania, Andorra, Belarus, Bulgaria, Croatia, Czech Republic, Estonia, Finland, Hungary, Iceland, Kyrgyzstan, Latvia, Lithuania, Luxembourg, Republic of Moldova, Monaco, Montenegro, Norway, Portugal, Russian Federation, Slovakia, Slovenia, Turkmenistan; the assessment was performed before the outbreak in Bulgaria); 7 countries were in western Europe, 11 were in CEE, and 5 were NIS), as “probable” for 20 countries (ie, Armenia, Azerbaijan, Belgium, Bosnia and Herzegovina, Cyprus, Denmark, Greece, Kazakhstan, Malta, the Netherlands, Poland, Romania, San Marino, Serbia, Spain, Sweden, Tajikistan, the Former Yugoslav Republic of Macedonia, Turkey, and Uzbekistan; 9 countries were in western Europe, 6 were in CEE, and 5 were NIS), and as “unlikely” for the remaining 10 countries (ie, Austria, France, Georgia, Germany, Ireland, Israel, Italy, Switzerland, UK the United Kingdom, and Ukraine; 8 were in western Europe, and 2 were NIS).
DISCUSSION
Evidence shows that it is technically feasible to eliminate measles from a geographic area [12]. Since adoption of the elimination goal in the WHO European Region, the number of reported measles cases has dramatically decreased. During 2007–2009, measles incidence in the region decreased to historically low levels of ≤10 cases per 1,000,000 population. The number of countries with no reported measles cases or low (<1 per 1,000,000 population) incidence has been increasing. The de- crease in measles cases is a result of high immunization coverage with 2 doses of MCV and of implementation of SIAs targeting remaining susceptible age cohorts, which reached >55 million persons during 2003–2009. Surveillance for measles has also been strengthened by improving case investigation procedures and expanding case-based reporting, including laboratory testing. The establishment of the measles and rubella regional laboratory network, modeled on that for poliomyelitis, provides data for timely confirmation of cases and monitoring circulating measles virus genotypes.
Although there have been many achievements, challenges still exist in reaching the elimination goal, as evidenced by the ongoing measles outbreaks, which have led to unnecessary illness and death. Moreover, ongoing transmission in western Europe has been linked to multiple introductions of measles virus into other regions, including the Americas, which have eliminated indigenous measles [13, 14].
The major challenge to achieving the regional measles elimination goal by 2010 is failure to vaccinate on time or the decision not to immunize. Although national measles immunization coverage estimates remain high, coverage at the sub-national level and among high-risk and vulnerable populations in many countries has been revealed to be much lower than the recommended ≥95% or higher for 2 doses. Challenges to ensuring strong immunization services are present both in countries undergoing health care reform and in those with stable and well-funded primary health care systems. Resulting pockets of susceptible individuals can support disease transmission and cause outbreaks of measles, as was the case with the resurgence of measles cases in western Europe and CEE countries [7, 15, 16].
Most outbreaks are in unimmunized populations (eg, hard-to-reach, vulnerable populations and groups with vaccine safety concerns or with religious, philosophical, or cultural beliefs against immunization) in both high and low socioeconomic strata [7]. These countries must focus their efforts on immunizing these groups, especially the high-risk and vulnerable populations that have limited access to primary health care services for geographical, cultural, ethnic, or socioeconomic reasons. To minimize the risk of acquiring measles, particularly in countries with ongoing outbreaks, optimal timing of routine MCV administration should be ensured by implementing evidence-informed routine immunization schedules for measles. Countries should consider targeted supplementary immunization activities. Although these are not common practice in the western part of the region, catch-up vaccination campaigns among groups and individuals who have not been vaccinated can dramatically close the immunity gaps. With continued outbreaks and increasing incidence in some countries, it is not advisable to delay administration of MCV1 until after 12 months of age or to delay administration of MCV2 until after 6 years of age, as is the current policy in many countries of the region. In addition, every effort should be made to ensure that parents and health care workers adhere to existing immunization schedules and that children receive vaccines on time.
There is a need to restore the public’s trust in immunization and to strengthen the understanding of the value of immunizations. In the near-absence of disease, immunization can lose priority, and perceived vaccine safety fears may outweigh concerns about risks of disease [7, 17]. As a result, there is a shift in public perception from the risk, implications, and severity of the disease to the vaccines safety issues. This has been exacerbated by misinformation about immunizations and the influence of anti-vaccination groups.
Communication initiatives should be developed by countries targeting the concerns of the nonimmunized or underimmunized people. Strategies for creating demand for immunization among identified populations need to be developed and implemented. The WHO European Regional Office will provide guidance on implementing behavioral models to address identified reasons for the failure to immunize. Countries need to employ a multisectoral approach with partners, including the use of civil society organizations to address their main challenges, including vaccine refusals. A focus on strengthening the knowledge of immunizations and vaccinology among health care professionals who are the trusted health advisers for many individuals will increase the opportunity for immunization. Where countries identify specific age cohorts susceptible to measles, additional immunization efforts, including wide-scale SIAs, will need to be considered to ensure they are immunized.
To monitor progress towards the elimination goal and document its achievement, national surveillance systems must be able to rapidly detect and confirm cases. High-quality case-based surveillance is critically important as the foundation for detection, laboratory diagnosis, and classification of all cases and contact tracing. Although surveillance systems for measles are functional in most countries, and although reporting to WHO on a monthly basis has been implemented, the completeness and timeliness of reporting measles cases are at times suboptimal. To further strengthen surveillance and to better monitor indicators of system performance, case-based surveillance must be used in all countries. Measles virus sequencing, a critical tool for monitoring circulating genotypes and documenting the interruption of indigenous transmission, has been widely implemented in the region. This practice needs to be sustained and further expanded. Implementation of recently published updated guidelines of surveillance for measles and rubella in the European Region, adapted for the final stages of measles and rubella elimination efforts in the region [18], is expected to contribute substantially to further improvement of surveillance.
The regional strategy and tools for measles and rubella elimination are effective if implemented fully and appropriately, as evidenced by the progress made towards measles and rubella elimination in the region, with some member states (eg, Finland, Iceland, and Norway) [19] likely having sustained interruption of endemic transmission of one or both of the diseases.
The regional elimination goals are attainable, albeit not by the present target date of 2010 (Figure 5). Recently, in September 2010, the European Regional Committee revised the target date for elimination to 2015 [20]. The European Region is at a point where measles rates are low, but at a time when increased political commitment, financial resources, and efforts are needed. With additional accelerated actions (Table 3), countries will be able to interrupt indigenous transmission, and the region can achieve the elimination goal by 2015. It is urgent that countries renew their political commitment at all levels and ensure that societal support to the elimination goals is strengthened. In addition, countries must mobilize the required human and financial resources to reach the goal. The WHO European Regional Office will provide leadership and guidance on placing greater emphasis on leveraging global and regional resources and opportunities through existing partnerships and other sources of global and regional expertise. To achieve the rubella elimination goal, it must also be integrated with the measles immunization strategy and surveillance system.
Figure 5.
Feasibility of meeting the measles elimination goal by countries in the World Health Organization European Region by the end of 2010.
Table 3.
Remaining Activities Needed to Achieve the Measles and Rubella Elimination Goal in the World Health Organization (WHO) European Region
| For member states | For the WHO Regional Office for Europe |
|---|---|
|
| |
| Review and reinforce political commitment and human and financial resources required to accelerate actions to achieve the goals of measles and rubella elimination | Provide leadership, strategic direction, and technical guidance to member states, and coordinate the annual European Immunization Week to achieve the regional immunization goals |
| Achieve high (≥95%) immunization for 2 doses of measles- and rubella-containing vaccine) at subnational levels and monitor progress towards targets through the following | |
| Strengthening routine immunization services and conducting supplementary immunization activities, as needed, focusing on high-risk and vulnerable populations using proven risk communication | Engage in global and regional partnerships to advocate for commitment and resources to strengthen and sustain immunization services and to prevent and control vaccine-preventable diseases |
| Ensuring quality vaccines administered through safe injection practices; and | |
| Using European Immunization Week as an advocacy tool | Establish a regional measles and rubella verification commission in order to review Member States′ documentation and verify elimination of measles and rubella in the region |
| Engage in partnerships, public and private, to ensure that the measles and rubella elimination goals are met | |
| Achieve measles and rubella elimination through the following | Facilitate the exchange of best practices and experiences among member states on measles and rubella elimination; and to use standardized indicators to monitor progress towards elimination targets; and |
| Implementing and strengthening case-based surveillance | |
| Developing or revising national elimination plans to address all components of the measles and rubella elimination strategy | Monitor and evaluate the progress of member states in reaching immunization targets through assessments and surveys to validate the quality of immunization coverage data |
| Establishing a national measles and rubella elimination verification committee to document progress towards measles and rubella elimination and report to a Regional verification commission | |
The recent polio outbreak in the WHO European Region, which had been polio-free since 2002 [21], is a sobering reminder how fragile the gains to date are; without sustained efforts, they can be lost quickly. Routine immunization programs are the cornerstone of these eradication and elimination goals, and without strong health systems, the goals will be in jeopardy. If the countries of the European Region are fully committed to eliminating measles, accelerated actions must be taken now to ensure that the gains made to date are sustained, so that the goal can be achieved.
Acknowledgments
We acknowledge the 53 Member States of the WHO European Region of the World Health Organization. Data for EU Member States are collected by EUVAC.NET. Measles SIAs in the European Region have been funded by the Measles Initiative, a partnership of the United Nations Foundation, American Red Cross, the Centers for Disease Control and Prevention, WHO and UNICEF.
Supplement sponsorship: This article is part of a supplement entitled “Global Progress Toward Measles Eradication and Prevention of Rubella and Congenital Rubella Syndrome,” which was sponsored by the Centers for Disease Control and Prevention.
Direct financial support was not received for the work presented. Measles and rubella surveillance laboratory testing and capacity building in the World Health Organization European Region is partially supported by the US Centers for Disease Control through the World Health Organization, Geneva
Footnotes
Potential conflicts of interest: none reported.
References
- 1.World Health Organization (WHO). Health 21: the health for all policy framework for the WHO European Region. Vol 6. Copenhagen, Denmark: WHO Regional Office for Europe, 1999. (European Health for All Series). [Google Scholar]
- 2.World Health Organization (WHO). EUR/RC55/7. Strengthening national immunization systems through measles and rubella elimination and prevention of congenital rubella infection in WHO’s European Region with a target date of 2010. In 55th Session of the Regional Committee for Europe, Bucharest, Romania, 12–15 September, 2005. WHO, 2005. http://www.euro.who.int/_data/assets/pdf_file/0010/87877/RC55_edoc07.pdf. Accessed 21 April 2011. [Google Scholar]
- 3.World Health Organization (WHO). Strategic plan for measles and congenital rubella infection in the WHO European Region. Vol 2009. Copenhagen, Denmark: WHO Regional Office for Europe, 2003. http://www.euro.who.int/__data/assets/pdf_file/0008/79028/E87772.pdf. Accessed 21 April 2011. [Google Scholar]
- 4.World Health Organization (WHO). WHO/UNICEF joint reporting process. http://www.who.int/immunization_monitoring/routine/joint_reporting/en/index.html. Accessed 21 April 2011. [Google Scholar]
- 5.World Health Organization (WHO). Surveillance guidelines for measles and congenital rubella infection in the WHO European Region. In: Organization WH, ed. Copenhagen, Denmark: World Health Organization, 2003; 1–66. [Google Scholar]
- 6.World Health Organization. Computerized information system for infectious diseases (CISID). http://data.euro.who.int/cisid. Accessed 21 April 2011. [Google Scholar]
- 7.Muscat M, Bang H, Wohlfahrt J, Glismann S, Molbak K. Measles in Europe: an epidemiological assessment. Lancet 2009; 373:383–9. [DOI] [PubMed] [Google Scholar]
- 8.Khetsuriani N, Deshevoi S, Goel A, Spika J, Martin R, Emiroglu N. Supplemental immunization activities to achieve measles elimination: experience of the European. RegionJ Infect Dis 2011; doi: 10.1093/infdis/jir074. [DOI] [PubMed] [Google Scholar]
- 9.Khetsuriani N, Imnadze P, Baidoshvili L, et al. Impact of unfounded vaccine safety concerns on the nationwide measles-rubella immunization campaign, Georgia, 2008. Vaccine 2010; 28:6455–62. [DOI] [PubMed] [Google Scholar]
- 10.Mankertz A, Mulders M, Shulga S, et al. Molecular genotyping and epidemiology of measles virus transmission in the WHO European Region, 2007–2009. J Infect Dis 2011; doi: 10.1093/infdis/jir101. [DOI] [PubMed] [Google Scholar]
- 11.World Health Organization Regional Office for Europe. European Immunization Week 2008: progress towards regional goal. Euro Surveill 2008; 13. http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId=18836. Accessed 21 April 2011. [Google Scholar]
- 12.De Quadros CA, Izurieta H, Carrasco P, Brana M, Tambini G. Progress toward measles eradication in the region of the Americas. J Infect Dis 2003; 187(Suppl. 1):S102–10. [DOI] [PubMed] [Google Scholar]
- 13.EUVAC.NET. Report of the 6th annual meeting. Copenhagen, 29–30 May 2008. Copenhagen, Denmark; Statens Serum Institut, 2009. http://www.euvac.net/graphics/euvac/pdf/meeting_2008.pdf. Accessed 21 April 2011. [Google Scholar]
- 14.Centers for Disease Control and Prevention. Update: measles –- United States, January–July 2008. MMWR Morb Mortal Wkly Rep 2008; 57:893–6. [PubMed] [Google Scholar]
- 15.Centers for Disease Control and Prevention. Progress toward measles elimination–European Region, 2005–2008. MMWR Morb Mortal Wkly Rep 2009; 58:142–5. [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention. Progress toward elimination of measles and prevention of congenital rubella infection-European Region, 1990–2004. MMWR Morb Mortal Wkly Rep 2005; 54:175–8. [PubMed] [Google Scholar]
- 17.Salathe M, Bonhoeffer S. The effect of opinion clustering on disease outbreaks. J R Soc Interface 2008; 5:1505–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.World Health Organization. Surveillance guidelines for measles, rubella and congenital rubella syndrome in the WHO European Region. Copenhagen, Denmark: WHO, 2010. http://www.euro.who.int/_data/assets/pdf_file/0018/79020/E93035.pdf. Accessed 21 April 2011. [PubMed] [Google Scholar]
- 19.Peltola H, Jokinen S, Paunio M, Hovi T, Davidkin I. Measles, mumps, and rubella in Finland: 25 years of a nationwide elimination programme. Lancet Infect Dis 2008; 8:796–803. [DOI] [PubMed] [Google Scholar]
- 20.World Health Organization. European Regional Office, Copenhagen, Denmark. Renewed commitment to elimination of measles and rubella and prevention of congenital rubella syndrome by 2015 and Sustained support for polio-free status in the WHO European Region. 60th Session of the Regional Committee for Europe, Moscow, Russian Federation, 13–16 September, 2010. WHO, 2010. http://www.euro.who.int/__data/assets/pdf_file/0016/122236/RC60_eRes12.pdf. Accessed 21 April 2011. [Google Scholar]
- 21.World Health Organization Country Office/Tajikistan, WHO Regional Office for Europe, European Centre for Disease Prevention and Control. Outbreak of poliomyelitis in Tajikistan in 2010: risk for importation and impact on polio surveillance in Europe? Euro Surveill 2010; 15: 1–3. http://www.eurosurveillance.org/ViewArticle.aspx?ArticleId519558. Accessed 21 April 2011. [DOI] [PubMed] [Google Scholar]