Abstract
Purpose:
Open science that is truly accessible and transparent to all will enhance reproducibility. However, there are ethical and practical concerns in implementing open science practices, especially when working with populations who are systematically excluded from and marginalized in communication sciences and disorders (CSD) research, such as Black, Indigenous, and People of Color (BIPOC) from clinical populations. The purpose of this article was to discuss these concerns and present actionable steps to support open science in CSD research with BIPOC.
Conclusions:
In the movement toward open and reproducible science, the discipline of CSD must prioritize accessibility and transparency, in addition to the implementation of individual scientific practices. Such a focus requires building trust with BIPOC not only as research participants but also as valued leaders of the scientific community.
As clear from the articles in this special issue, open science is an urgent priority. The goals of making science more transparent and universally accessible (Banks et al., 2019; Nosek et al., 2018) can be achieved via data and code sharing, open methodologies, open peer review (i.e., making aspects of the peer review process publicly available pre- or postpublication), and gratis access to scientific publications and educational resources (Munafò et al., 2017; Nosek et al., 2015). These methods enhance reproducibility by providing access to information for replicating and generalizing research (Nosek et al., 2015). However, one underheard perspective in this dialogue is the implications of open science for Black, Indigenous, and People of Color (BIPOC; Sabik et al., 2021). Communication sciences and disorders (CSD) research systematically excludes BIPOC (Clark et al., 2019). Balancing open science with participant rights is critical (Fox et al., 2021). In this viewpoint, we discuss challenges to and strategies for implementing open science in CSD research with BIPOC as aligned with the goals of the American Speech-Language-Hearing Association (2021) and the National Institutes of Health (2021).
We view open science practices through two lenses: ethical principles of research and theory at the intersection of race and disability. The Belmont Report outlines three ethical principles: respect for persons, referring to respecting autonomy while also addressing the special considerations involved in informed consent for vulnerable populations; beneficence, referring to balancing benefits and harms at the individual, community, and societal levels; and justice, referring to ensuring equitable opportunities for all to participate in, access, and conduct research (The National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research, 1979). In turn, the disability studies and critical race theory (DisCrit) posits race and disability are social constructs that reinforce one another and largely involve the reactions of others to individual differences (Annamma et al., 2013). In addition, BIPOC may have intersecting identities that give rise to multiple marginalization (Crenshaw, 1989, 1991).
In the discipline of CSD, exclusion of BIPOC as both researchers and participants provides little precedent on how to conduct research with individuals from these communities (Fox et al., 2021). Such exclusion leads to a biased evidence base for diagnosis and assessment (e.g., Daugherty et al., 2017). For example, Black and Hispanic children are less likely than non–Hispanic White children to be diagnosed as having autism (Wiggins et al., 2020) and are likely to be underdiagnosed as having speech-language impairment (Robinson & Norton, 2019). Though enhancing diversity is a priority, CSD researchers must be thoughtful in their implementation of open science practices.
Challenges and Workable Solutions
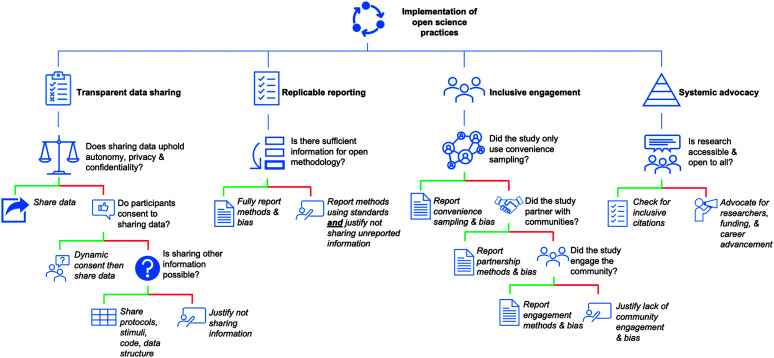
This section presents challenges in the implementation of open science practices (see Figure 1). We also present solutions for incorporating open science practices while increasing accessibility. By following the principles of respect for persons, beneficence, and justice, the field can implement open science practices with BIPOC participants in meaningful ways.
Figure 1.
A flowchart for implementation of open science practices with Black, Indigenous, and People of Color in communication sciences and disorders research.
Transparent Data Sharing
Informed Consent
Data sharing is a central tenet of open science and is often required or encouraged by granting agencies or scholarly journals; sharing requires an informed consent process that is transparent and just. For a participant, data-sharing plans are first mentioned during informed consent. However, for BIPOC from clinical populations, who may distrust the research process for myriad reasons (Shaia et al., 2020), data sharing could cause concern or disengagement from research (Campbell et al., 2019). Indeed, participants report feeling uncomfortable with losing autonomy over how research about them is conducted and disseminated and with not knowing who has received their data (Cummings et al., 2015). Even if participants can withdraw from a study, they cannot reclaim already-shared data. Without transparency in informed consent, open data can erode trust and limit participation for BIPOC from clinical populations.
Privacy and Confidentiality
Even with informed consent, researchers must carefully protect participant confidentiality and privacy, which is a significant concern when participants are scarce in research. For instance, Hurst et al. (1990) published studies describing the KE family, which had a unique monogenic speech disorder. Subsequent research presented highly detailed individual-level descriptions in evaluating genotype–phenotype relationships (Gopnik & Crago, 1991; Lai et al., 2001; Pinker, 2007); the individuals could potentially be identified. Similarly, autistic individuals with intellectual disability are underrepresented in autism research (6% compared with 50% of the population; Russell et al., 2019); thus, even when de-identified, providing geographical information could reveal participants' identities (Sweeney et al., 2017). This risk is further elevated for more minoritized individuals, such as BIPOC autistic individuals with intellectual disability, and in case, dyadic, or pedigree studies providing extensive individual descriptions (McCurdy & Fitchett, 2011). Although data sharing is important for open science, researchers must balance the benefits with these risks (Rocher et al., 2019; Sweeney et al., 2017).
Potential Solution: Transparent Data Sharing
Researchers should be transparent about their data-sharing practices with participants, such that participants understand how their data are shared (see Figure 1). For example, the first author explained to a participant that if they shared their data, other researchers who did not know the participant might arrive at their own interpretations of the data (Girolamo & Rice, 2022). That participant consented to take part in the study, but not to data sharing. If providing open data might violate confidentiality and privacy or result in attrition because participants do not consent to sharing data, there are alternatives. Sharing code or methodological information (e.g., stimuli, analysis pipelines, and data structure) allows others to replicate analyses or run simulations (El Emam et al., 2020; Goncalves et al., 2020). Researchers can provide participants with access to publications and other outcomes of the research process, such as community resources, and share information via social media, community presentations, and lay-appropriate summaries to bring the science back to the participants at the end of a study.
When participants consent to data sharing, researchers should use dynamic or graded consent procedures to facilitate participant comprehension of the implications of data sharing. In dynamic consent, consent is an interactive and ongoing process; study procedures and consent, privacy, and confidentiality are thoroughly explained in an accessible register (Brannon et al., 2013; George et al., 2014). Graded consents allow participants control over what is shared (e.g., recordings and transcripts) and where it is shared (e.g., public or restricted databases; Fox et al., 2021; Sabik et al., 2021). Providing examples of identifiable versus de-identified data (e.g., name vs. ID code) and how these are used can fully illustrate these terms. Although open data are a tenet of open science, equally important is transparency in data sharing with participants.
Reporting Standards
As with data sharing, transparent reporting of methodologies raises unique considerations for multiple marginalized participants. Many journals require authors to adhere to reporting standards (American Speech-Language-Hearing Association, n.d.; U.K. Equator Centre, n.d.; see Table 1). However, existing reporting standards for clinical research with human participants are variable in their requirements, potentially leading to methodological underreporting relevant to BIPOC. For example, convenience sampling, which is likely to yield primarily white participants (Maye et al., 2021), is only apparent if authors are required to describe recruitment methods. Authors are also encouraged to provide explanations of efforts to minimize bias (e.g., using community-based methods). Some neurotechnology tools used in CSD research, such as electroencephalography, fail to work equitably on all hair types and skin tones (Choy et al., 2021; Etienne et al., 2020), impact data collection with BIPOC participants; the requirement to show a study flowchart with information about attrition and data loss at each step can clarify such limitations.
Table 1.
Reproducibility criteria in selected recognized standards checklists for designing and implementing clinical studies with human participants and reporting the findings.
| Checklist | Methods |
Limitations |
|||||
|---|---|---|---|---|---|---|---|
| Recruitment methods | Eligibility criteria | Participant demographics | Study flowchart with explanations | Efforts to address bias | Bias in methods | Generalizability | |
| AGREE | Y | Y | |||||
| CARE | N/A | Y | N/A | N/A | |||
| CHEERS | Y | Y | Y | ||||
| COSORT | Y | Y | Y | Y | |||
| COREQ | Y | Y | Y | Y | |||
| ETREQ | N/A | Y | Y | ||||
| MOOSE | N/A | Y | Y | Y | |||
| PRISMA | N/A | Y | Y | Y | Y | Y | |
| SPIRIT | Y | Y | |||||
| SQUIRE | Y | Y | |||||
| SRQR | Y | Y | |||||
| STARD | Y | Y | Y | ||||
| STROBE | Y | Y | Y | Y | Y | Y | |
| TIDIER | |||||||
| TREND | Y | Y | Y | Y | |||
Note. Absence of standard = empty boxes. Checklist: AGREE = AGREE Reporting Checklist: a tool to improve reporting of clinical practice guidelines (Brouwers et al., 2016); CARE = Consensus-Based Clinical Case Reporting Guidelines (Gagnier et al., 2013); CHEERS = Consolidated Health Economic Evaluation Reporting Standards (Husereau et al., 2022); CONSORT = Consolidated Standards of Reporting Trials (Schulz et al., 2010); COREQ = Consolidated Criteria for Reporting Qualitative Research (Tong et al., 2007). ENTREQ = Enhancing Transparency in Reporting the Synthesis of Qualitative Research (Tong et al., 2012); MOOSE = Meta-Analysis of Observational Studies in Epidemiology (Stroup et al., 2000); PRISMA = updated guide for reporting systematic reviews (Page et al., 2021); SPIRIT = Standard Protocol Items for Clinical Trials (Chan et al., 2013); SQUIRE = Standards for Quality Improvement Reporting Excellence (Ogrinc et al., 2015); SRQR = Standards for Reporting Qualitative Research (O'Brien et al., 2014); STARD = Standards for Reporting of Diagnostic Accuracy (Bossuyt et al., 2015); STROBE = Strengthening the Reporting of Observational Studies in Epidemiology (von Elm et al., 2007); TIDIER = Template for Intervention Description and Replication (Hoffmann et al., 2014); TREND = Transparent Reporting of Evaluations With Nonrandomized Designs (Des Jarlais et al., 2004). Y = included in checklist; N/A = not applicable to reporting guidelines.
Underreporting of participant characteristics is another salient issue. Following the American Psychological Association (APA, 2020; see also Hammer, 2011), researchers should report (a) inclusion and exclusion criteria; (b) demographics, such as age, sex, ethnicity, and socioeconomic status (SES); and (c) topic-specific characteristics (e.g., variants of a language spoken). However, even CSD research that follows APA guidelines reveals systematic omission of these data. Over 85% of 116 articles on neurological communication disorders published between 1997 and 2007 in the American Journal of Speech-Language Pathology and the Journal of Speech, Language, and Hearing Research failed to report race and ethnicity (Ellis, 2009), with a similar omission rate (> 70%) in 303 articles on aphasia published between 2009 and 2019 (Nguy et al., 2022). Autism research similarly underreports race and ethnicity in parent-implemented interventions (Steinbrenner et al., 2022) and research overall (Pierce et al., 2014). Over one third of 652 articles on pediatric language research published between 2000 and 2015 in Language, Speech, and Hearing Services in Schools; the American Journal of Speech-Language Pathology; and the Journal of Speech, Language, and Hearing Research (Language section) did not report participant SES (Inglebret et al., 2017). In all, underreporting participant characteristics masks who comprises the evidence base and to whom findings may generalize.
Potential Solution: Reporting Standards
Supporting open science requires full reporting of methodology, including the impact of selection criteria and participant flow on participants. Given exclusion of BIPOC as participants, researchers should acknowledge when eligibility criteria tend to exclude multiple marginalized participants, such as autistic BIPOC with intellectual disability (Russell et al., 2019). Indeed, APA (2020) guidelines stipulate reporting participant flow, attrition, and causes for attrition (e.g., inaccessibility of research study times for participants; Brannon et al., 2013).
Participant demographic reporting is critical for multiple reasons, as social determinants of health contribute to racial and ethnic health disparities (Rivera-Figueroa et al., 2022; Singh et al., 2017). Best practices include asking separate questions about gender, sex, and sexuality (National Academies of Sciences, Engineering, and Medicine, 2022), allowing participants to self-report race and ethnicity or including specific rather than broad categories (e.g., Korean vs. Asian; Flanagin et al., 2021), and allowing participants to provide clarification. If reporting detailed participant characteristics threatens privacy and confidentiality, researchers should explain this. Although these recommendations go further than current reporting standards, researchers are responsible for what they report. The standard should be full transparency.
Finally, open methodology includes transparent reporting and justification of analyses. A phenomenon observed in a subset of the population does not necessarily generalize; the real world is heterogeneous (Ellis et al., 2021; Rivera-Figueroa et al., 2022). When sample sizes permit, intersectional analyses can allow testing for differences in outcomes across identities (Bauer et al., 2021). If sample sizes are too small for intersectional analyses, as is common in research with BIPOC from clinical populations, Bayesian approaches may be helpful (McMillan & Cannon, 2019). In all cases, researchers should report sufficient information about selection criteria, participant flow, demographics, analysis, and bias, being mindful of underrepresentation.
Inclusion of Representative Samples
Because CSD research tends to exclude BIPOC, we elaborate on an additional challenge to open science: ensuring that participation in science is accessible to all. Scientists typically aim for a homogenous sample to reduce noise in the data (Munafò et al., 2017). However, this drive for homogeneity can exacerbate exclusion of BIPOC. For example, reviewers of a manuscript suggested that linguistic diversity would be present in BIPOC but not white participants, presenting a confound that should be controlled for in a study (Girolamo et al., 2022). When BIPOC participants are included, they are often a statistical minority, obscuring potentially meaningful differences. This establishes a feedback loop in which research methods, based on homogeneous samples (Fox et al., 2021), result in BIPOC being erroneously viewed as outliers (Lewis & Oyserman, 2016). Although homogenous samples can serve a purpose, the use of such samples should be justified, particularly when it excludes those who are already minoritized.
Efforts to recruit diverse research samples are commendable yet must be realistic and follow research ethics. Grant applications and preregistered reports (i.e., peer-reviewed research proposals that are published or registered prior to data collection) are two contexts in which recruitment methods and participant samples are described prospectively. What is written in these forums is not necessarily what ends up being true of the research study. Researchers may propose to engage BIPOC from clinical populations using community-based methods for recruitment, but the final sample may differ in meaningful ways. Changes may reflect unanticipated limits on access to the targeted population, attrition, lack of effort by the researchers to build community ties, or other factors. Importantly, if researchers enter communities without establishing trust and report with or learning about the challenges of and barriers to data collection in BIPOC communities, this may lead to undersampling or other harm.
Potential Solution: Inclusive Engagement of BIPOC Communities
As ones in charge of designing studies, researchers are ideally situated to convey values and expectations to participants (Lewis & Oyserman, 2016; see Newkirk-Turner & Morris, 2021, for a review on CSD research with the Black speech community). For example, conducting research in BIPOC communities at venues familiar to them and at times when they meet implies the study was built with them in mind. Partnering with BIPOC community stakeholders in community-based participatory research (CBPR) can facilitate the accessibility of research to populations whose voices are often unheard (Ellis et al., 2021; Maye et al., 2021). In CBPR, community members receive research training via long-term partnerships, and research questions are developed in part with the aim of addressing community priorities. When research benefits all partners, it serves to mitigate racial/ethnic disparities (Wallerstein & Duran, 2006). Some journals, such as the British Medical Journal and Autism, now require a statement explaining how researchers engaged community stakeholders (Fletcher-Watson et al., 2021; The BMJ, 2018). Though top-down change is important, researchers should incorporate CBPR practices instead of waiting for organizational change. Inclusive engagement of communities takes time and effort.
No matter the level of community engagement, researchers should justify their study engagement methods (see Figure 1). For example, participants for a study may be recruited by sharing flyers with professional networks; if so, researchers should state who was approached for recruitment (Wendler et al., 2005). In addition, researchers should address any efforts to minimize known barriers to inclusion of BIPOC in research (or list lack of such efforts as a limitation): geographic distance between research sites and participant communities, scheduling conflicts with work, caregiving, and access to transportation (Brannon et al., 2013; George et al., 2014). Such transparency is essential to open science (Fuentes et al., 2022).
Systemic Advocacy
At a broader level, the implementation of open science in CSD research requires systemic advocacy to mitigate exclusion of BIPOC from the academy (see Figure 1). We encourage scientists to reflect on how their research practices include or exclude voices in all parts of research and to mitigate systemic racism in the research enterprise (Gilpin & Taffe, 2021; Medin et al., 2017). Institutions must shift to explicitly value diversity (Hruschka et al., 2018). Organizations must recognize that diverse researchers lead to theoretical advances (e.g., understanding mechanisms in identity development; Spencer, 2014) and scientific innovation that strengthens the quality of science by making it more inclusive (e.g., partnering with Black hairstylists to develop equitable fNIRS methods; Parker & Ricard, 2022). Diversifying academia will facilitate the engagement of BIPOC as research participants, as BIPOC researchers can build on existing community ties and insider knowledge (Medin et al., 2017), while also challenging existing paradigms based on primarily white (vs. more diverse) participant bases. One approach to valuing diversity at the university level is to evaluate active participation in and contribution to diversity, equity, and inclusion activities as part of annual faculty reviews. At the organizational level, journals can establish a preregistered report option to encourage open science practices that effectively require researchers to have sound research methods before entering communities (Storkel & Gallun, 2022). There are many ways in which to address underrepresentation in science through systemic advocacy.
Conclusions
Our aim in this article is to move the research enterprise toward greater accessibility and transparency by discussing challenges and solutions for implementing open science in research with BIPOC from clinical populations. Ultimately, open science requires changes in scientific conduct. Diversifying participants, labs, and researchers are all necessary aspects of open science that will benefit the field of CSD.
Acknowledgments
Teresa Girolamo and Inge-Marie Eigsti were supported by T32DC017703 (Co-Directors: Eigsti & Myers). Inge-Marie Eigsti was supported by R01MH112687 (PIs: Eigsti & Fein). Saamntha Ghali was supported by, T32DC000052 (Director: Rice). Alison Hendricks was supported by R21DC018355 (PI: Hendricks).
Funding Statement
Teresa Girolamo and Inge-Marie Eigsti were supported by T32DC017703 (Co-Directors: Eigsti & Myers). Inge-Marie Eigsti was supported by R01MH112687 (PIs: Eigsti & Fein). Saamntha Ghali was supported by, T32DC000052 (Director: Rice). Alison Hendricks was supported by R21DC018355 (PI: Hendricks).
References
- American Psychological Association. (2020). Publication manual of the American Psychological Association: The official guide to APA style (7th ed.).
- American Speech-Language-Hearing Association. (2021). Strategic objective highlights. https://www.asha.org/about/strategic-objective-highlights/
- American Speech-Language-Hearing Association. (n.d.). Guidelines for reporting your research. https://academy.pubs.asha.org/asha-journals-author-resource-center/manuscript-preparation/guidelines-for-reporting-your-research/
- Annamma, S. A. , Connor, D. , & Ferri, B. (2013). Dis/ability critical race studies (DisCrit): Theorizing at the intersections of race and dis/ability. Race Ethnicity and Education, 16(1), 1–31. https://doi.org/10.1080/13613324.2012.730511 [Google Scholar]
- Banks, G. C. , Field, J. G. , Oswald, F. L. , O'Boyle, E. H. , Landis, R. S. , Rupp, D. E. , & Rogelberg, S. G. (2019). Answers to 18 questions about open science practices. Journal of Business and Psychology, 34(3), 257–270. https://doi.org/10.1007/s10869-018-9547-8 [Google Scholar]
- Bauer, G. R. , Churchill, S. M. , Mahendran, M. , Walwyn, C. , Lizotte, D. , & Villa-Rueda, A. A. (2021). Intersectionality in quantitative research: A systematic review of its emergence and applications of theory and methods. SSM—Population Health, 14, 100798. https://doi.org/10.1016/j.ssmph.2021.100798 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bossuyt, P. M. , Reitsma, J. B. , Bruns, D. E. , Gatsonis, C. A. , Glasziou, P. P. , Irwig, L. , Lijmer, J. G. , Moher, D. , Rennie, D. , de Vet, H. C. W. , Kressel, H. Y. , Rifai, N. , Golub, R. M. , Altman, D. G. , Hooft, L. , Korevaar, D. A. , & Cohen, J. F. (2015). STARD 2015: An updated list of essential items for reporting diagnostic accuracy studies. Clinical Chemistry, 61, 1446–1452. https://doi.org/10.1136/bmj.h5527 [DOI] [PubMed] [Google Scholar]
- Brannon, E. E. , Kuhl, E. S. , Boles, R. E. , Aylward, B. S. , Benoit Ratcliff, M. , Valenzuela, J. M. , Johnson, S. L. , & Powers, S. W. (2013). Strategies for recruitment and retention of families from low-income, ethnic minority backgrounds in a longitudinal study of caregiver feeding and child weight. Children's Health Care, 42(3), 198–213. https://doi.org/10.1080/02739615.2013.816590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brouwers, M. C. , Kerkvliet, K. , Spithoff, K. , & AGREE Next Steps Consortium. (2016). The AGREE Reporting Checklist: a tool to improve reporting of clinical practice guidelines. BMJ, 352. https://doi.org/10.1136/bmj.i1152 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell, R. , Goodman-Williams, R. , & Javorka, M. (2019). A trauma-informed approach to sexual violence research ethics and open science. Journal of Interpersonal Violence, 34(23–24), 4765–4793. https://doi.org/10.1177/0886260519871530 [DOI] [PubMed] [Google Scholar]
- Chan, A. W. , Tetzlaff, J. M. , Gøtzsche, P. C. , Altman, D. G. , Mann, H. , Berlin, J. A. , Dickersin, K. , Hróbjartsson, A. , Schulz, K. F. , Parulekar, W. R. , Krleza-Jeric, K. , Laupacis, A. , & Moher, D. (2013). SPIRIT 2013 explanation and elaboration: Guidance for protocols of clinical trials. BMJ, 346. https://doi.org/10.1136/bmj.e7586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choy, T. , Baker, E. , & Stavropoulos, K. (2021). Systemic racism in EEG research: Considerations and potential solutions. Affective Science, 3(1), 14–20. https://doi.org/10.1007/s42761-021-00050-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark, L. T. , Watkins, L. , Piña, I. L. , Elmer, M. , Akinboboye, O. , Gorham, M. , Jamerson, B. , McCullough, C. , Pierre, C. , Polis, A. B. , Puckrein, G. , & Regnante, J. M. (2019). Increasing diversity in clinical trials: Overcoming critical barriers. Current Problems in Cardiology, 44(5), 148–172. https://doi.org/10.1016/j.cpcardiol.2018.11.002 [DOI] [PubMed] [Google Scholar]
- Crenshaw, K. (1989). Demarginalising the intersection of race and sex: A Black feminist critique of antidiscrimination doctrine, feminist theory and antiracist politics. University of Chicago Legal Forum, 140, 25–42. https://doi.org/10.4324/9781315582924-10 [Google Scholar]
- Crenshaw, K. (1991). Mapping the margins: Intersectionality, identity politics, and violence against women of color. Stanford Law Review, 43(6), 1241–1499. https://doi.org/10.2307/1229039 [Google Scholar]
- Cummings, J. A. , Zagrodney, J. M. , & Day, T. E. (2015). Impact of open data policies on consent to participate in human subjects research: Discrepancies between participant action and reported concerns. PLOS ONE, 10(5), e0125208. https://doi.org/10.1371/journal.pone.0125208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daugherty, J. C. , Puente, A. E. , Fasfous, A. F. , Hidalgo-Ruzzante, N. , & Pérez-Garcia, M. (2017). Diagnostic mistakes of culturally diverse individuals when using north American neuropsychological tests. Applied Neuropsychology: Adult, 24(1), 16–22. https://doi.org/10.1080/23279095.2015.1036992 [DOI] [PubMed] [Google Scholar]
- Des Jarlais, D. C. , Lyles, C. , Crepaz, N. , & Trend Group. (2004). Improving the reporting quality of nonrandomized evaluations of behavioral and public health interventions: The TREND statement. American Journal of Public Health, 94(3), 361–366. https://doi.org/10.2105/AJPH.94.3.361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- El Emam, K. , Mosquera, L. , & Bass, J. (2020). Evaluating identity disclosure risk in fully synthetic health data: Model development and validation. Journal of Medical Internet Research, 22(11), e23139. https://doi.org/10.2196/23139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellis, C. (2009). Does race/ethnicity really matter in adult neurogenics? American Journal of Speech-Language Pathology, 18(4), 310–314. https://doi.org/10.1044/1058-0360(2009/08-0039) [DOI] [PubMed] [Google Scholar]
- Ellis, C. , Jacobs, M. , & Kendall, D. (2021). The impact of racism, power, privilege, and positionality on communication sciences and disorders research: Time to reconceptualize and seek a pathway to equity. American Journal of Speech-Language Pathology, 30(5), 2032–2039. https://doi.org/10.1044/2021_AJSLP-20-00346 [DOI] [PubMed] [Google Scholar]
- Etienne, A. , Laroia, T. , Weigle, H. , Afelin, A. , Kelly, S. K. , Krishnan, A. , & Grover, P. (2020). Novel Electrodes for Reliable EEG Recordings on Coarse and Curly Hair. Annual International Conference of the IEEE Engineering in Medicine and Biology Society. IEEE Engineering in Medicine and Biology Society. [DOI] [PubMed] [Google Scholar]
- Flanagin, A. , Frey, T. , Christiansen, S. L. , & the AMA Manual of Style Committee. (2021). Updated guidance on the reporting of race and ethnicity in medical and science journals. JAMA, 326(7), 621–627. https://doi.org/10.1001/jama.2021.13304 [DOI] [PubMed] [Google Scholar]
- Fletcher-Watson, S. , Bölte, S. , Crompton, C. J. , Jones, D. , Lai, M.-C. , Mandy, W. , Pellicano, L. , Stahmer, A. , Taylor, J. , & Mandell, D. (2021). Publishing standards for promoting excellence in autism research. Autism, 25(6), 1501–1504. https://doi.org/10.1177/13623613211019830 [DOI] [PubMed] [Google Scholar]
- Fox, J. , Pearce, K. E. , Massanari, A. L. , Riles, J. M. , Szulc, Ł. , Ranjit, Y. S. , Trevisan, F. , Soriano, C. R. R. , Vitak, J. , & Arora, P. (2021). Open science, closed doors? Countering marginalization through an agenda for ethical, inclusive research in communication. Journal of Communication, 71(5), 764–784. https://doi.org/10.1093/joc/jqab029 [Google Scholar]
- Fuentes, M. A. , Zelaya, D. G. , Delgado-Romero, E. A. , & Butt, M. (2022). Open science: Friend, foe, or both to an antiracist psychology? Psychological Review. https://doi.org/10.1037/rev0000386 [DOI] [PubMed] [Google Scholar]
- Gagnier, J. J. , Kienle, G. , Altman, D. G. , Moher, D. , Sox, H. , & Riley, D. (2013). The CARE guidelines: Consensus-based clinical case reporting guideline development. Journal of Medical Case Reports, 7(1), 1–6. https://doi.org/10.1186/1752-1947-7-223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- George, S. , Duran, N. , & Norris, K. (2014). A systematic review of barriers and facilitators to minority research participation among African Americans, Latinos, Asian Americans, and Pacific Islanders. American Journal of Public Health, 104(2), e16–e31. https://doi.org/10.2105/AJPH.2013.301706 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilpin, N. W. , & Taffe, M. A. (2021). Toward an anti-racist approach to biomedical and neuroscience research. Journal of Neuroscience, 41(42), 8669–8672. https://doi.org/10.1523/JNEUROSCI.1319-21.2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Girolamo, T. , Castro, N. , Kasambira Fannin, D. , Ghali, S. , & Mandulak, S. (2022). Inequity in peer review in communication sciences and disorders. American Journal of Speech-Language Pathology, 31(4), 1898–1912. https://doi.org/10.1044/2022_AJSLP-21-00252 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Girolamo, T. , & Rice, M. L. (2022). Language impairment in autistic adolescents and young adults. Journal of Speech, Language, and Hearing Research, 65(9), 3518–3530. https://doi.org/10.1044/2022_JSLHR-21-00517 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goncalves, A. , Ray, P. , Soper, B. , Stevens, J. , Coyle, L. , & Sales, A. P. (2020). Generation and evaluation of synthetic patient data. BMC Medical Research Methodology, 20(1), 108. https://doi.org/10.1186/s12874-020-00977-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gopnik, M. , & Crago, M. B. (1991). Familial aggregation of a developmental language disorder. Cognition, 39(1), 1–50. https://doi.org/10.1016/0010-0277(91)90058-c [DOI] [PubMed] [Google Scholar]
- Hammer, C. S. (2011). The importance of participant demographics. American Journal of Speech-Language Pathology, 20(4), 261. https://doi.org/10.1044/1058-0360(2011/ed-04) [DOI] [PubMed] [Google Scholar]
- Hoffmann, T. C. , Glasziou, P. P. , Boutron, I. , Milne, R. , Perera, R. , Moher, D. , Altman, D. G. , Barbour, V. , Macdonald, H. , Johnston, M. , Lamb, S. E. , Dixon-Woods, M. , McCulloch, P. , Wyatt, J. C. , Chan, A. W. , & Michie, S. (2014). Better reporting of interventions: Template for intervention description and replication (TIDieR) checklist and guide. BMJ, 348. https://doi.org/10.1136/bmj.g1687 [DOI] [PubMed] [Google Scholar]
- Hruschka, D. J. , Medin, D. L. , Rogoff, B. , & Henrich, J. (2018). Pressing questions in the study of psychological and behavioral diversity. Proceedings of the National Academy of Sciences, 115(45), 11366–11368. https://doi.org/10.1073/pnas.1814733115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurst, J. A. , Baraitser, M. , Auger, E. , Graham, F. , & Norell, S. (1990). An extended family with a dominantly inherited speech disorder. Developmental Medicine & Child Neurology, 32(4), 352–355. https://doi.org/10.1111/j.1469-8749.1990.tb16948.x [DOI] [PubMed] [Google Scholar]
- Husereau, D. , Drummond, M. , Augustovski, F. , de Bekker-Grob, E. , Briggs, A. H. , Carswell, C. , Caulley, L. , Chaiyakunapruk, N. , Greenberg, D. , Loder, E. , Mauskopf, J. , Mullins, C. D. , Petrou, S. , Pwu, R.-F. , & Staniszewska, S. (2022). Consolidated Health Economic Evaluation Reporting Standards 2022 (CHEERS 2022) statement: Updated reporting guidance for health economic evaluations. International Journal of Technology Assessment in Health Care, 38(1). https://doi.org/10.1017/S0266462321001732 [DOI] [PubMed] [Google Scholar]
- Inglebret, E. , Bailey, S. , Clothiaux, J. A. , Skinder-Meredith, A. , Monson, K. , & Cleveland, L. (2017). Reporting of socioeconomic status in pediatric language research. American Journal of Speech-Language Pathology, 26(3), 1042–1052. https://doi.org/10.1044/2017_AJSLP-16-0229 [DOI] [PubMed] [Google Scholar]
- Lai, C. S. L. , Fisher, S. E. , Hurst, J. A. , Vargha-Khadem, F. , & Monaco, A. P. (2001). A forkhead-domain gene is mutated in a severe speech and language disorder. Nature, 413(6855), 519–523. https://doi.org/10.1038/35097076 [DOI] [PubMed] [Google Scholar]
- Lewis, N. A., Jr. , & Oyserman, D. (2016). Using identity-based motivation to improve the nation's health without breaking the bank. Behavioral Science & Policy, 2(2), 24–38. https://doi.org/10.1353/bsp.2016.0013 [Google Scholar]
- Maye, M. , Boyd, B. A. , Martínez-Pedraza, F. , Halladay, A. , Thurm, A. , & Mandell, D. S. (2021). Biases, barriers, and possible solutions: Steps towards addressing autism researchers under-engagement with racially, ethnically, and socioeconomically diverse communities. Journal of Autism and Developmental Disorders, 52(9), 4206–4211. https://doi.org/10.1007/s10803-021-05250-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCurdy, D. B. , & Fitchett, G. (2011). Ethical issues in case study publication: “Making our case(s)” ethically. Journal of Health Care Chaplaincy, 17(1–2), 55–74. https://doi.org/10.1080/08854726.2011.559855 [DOI] [PubMed] [Google Scholar]
- McMillan, G. P. , & Cannon, J. B. (2019). Bayesian applications in auditory research. Journal of Speech, Language, and Hearing Research, 62(3), 577–586. https://doi.org/10.1044/2018_JSLHR-H-ASTM-18-0228 [DOI] [PubMed] [Google Scholar]
- Medin, D. , Ojalehto, B. , Marin, A. , & Bang, M. (2017). Systems of (non-)diversity. Nature Human Behaviour, 1(5), 0088. https://doi.org/10.1038/s41562-017-0088 [Google Scholar]
- Munafò, M. R. , Nosek, B. A. , Bishop, D. V. M. , Button, K. S. , Chambers, C. D. , Percie du Sert, N. , Simonsohn, U. , Wagenmakers, E.-J. , Ware, J. J. , & Ioannidis, J. P. A. (2017). A manifesto for reproducible science. Nature Human Behaviour, 1(1), 0021. https://doi.org/10.1038/s41562-016-0021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine. (2022). Measuring sex, gender identity, and sexual orientation. The National Academies Press. https://doi.org/10.17226/26424 [PubMed] [Google Scholar]
- National Institutes of Health. (2021). NIH-wide strategic plan for fiscal years 2021–2025. https://www.nih.gov/sites/default/files/about-nih/strategic-plan-fy2021-2025-508.pdf
- Newkirk-Turner, B. L. , & Morris, L. R. (2021). An unequal partnership: Communication sciences and disorders, Black children, and the Black speech community. In Critical perspectives on social justice in speech-language pathology (pp. 180–196). IGI Global. [Google Scholar]
- Nguy, B. , Quique, Y. M. , Cavanaugh, R. , & Evans, W. S. (2022). Representation in aphasia research: An examination of U.S. treatment studies published between 2009 and 2019. American Journal of Speech-Language Pathology, 31(3), 1424–1430. https://doi.org/10.1044/2022_AJSLP-21-00269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nosek, B. A. , Alter, G. , Banks, G. C. , Borsboom, D. , Bowman, S. D. , Breckler, S. J. , Buck, S. , Chambers, C. D. , Chin, G. , Christensen, G. , Contestabilea, M. , Dafoe, A. , Eich, E. , Freese, J. , Glennerster, R. , Goroff, D. , Green, D. P. , Hesse, B. , Humphreys, M. , … Yarko, T. (2015). Promoting an open research culture. Science, 348(6242), 1422–1425. https://doi.org/10.1126/science.aab2374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nosek, B. A. , Ebersole, C. R. , DeHaven, A. C. , & Mellor, D. T. (2018). The preregistration revolution. Proceedings of the National Academy of Sciences, 115(11), 2600–2606. https://doi.org/10.1073/pnas.1708274114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Brien, B. C. , Harris, I. B. , Beckman, T. J. , Reed, D. A. , & Cook, D. A. (2014). Standards for reporting qualitative research: A synthesis of recommendations. Academic Medicine, 89(9), 1245–1251. https://doi.org/10.1097/ACM.0000000000000388 [DOI] [PubMed] [Google Scholar]
- Ogrinc, G. , Davies, L. , Goodman, D. , Batalden, P. , Davidoff, F. , & Stevens, D. (2015). SQUIRE 2.0 (Standards for QUality Improvement Reporting Excellence): Revised publication guidelines from a detailed consensus process. American Journal of Critical Care, 24(6), 466–473. https://doi.org/10.4037/ajcc2015455 [DOI] [PubMed] [Google Scholar]
- Page, M. J. , McKenzie, J. E. , Bossuyt, P. M. , Boutron, I. , Hoffmann, T. C. , Mulrow, C. D. , Shamseer, L. , Tetzlaff, J. M. , Akl, E. A. , Brennan, S. E. , Chou, R. , Glanville, J. , Grimshaw, J. M. , Hróbjartsson, A. , Lalu, M. M. , Li, T. , Loder, E. W. , Mayo-Wilson, E. , McDonald, S. , McGuinness, L. A. , … Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. Systematic Reviews, 10(1), 1–11. https://doi.org/10.1186/s13643-021-01626-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Parker, T. C. , & Ricard, J. A. (2022). Structural racism in neuroimaging: Perspectives and solutions. The Lancet Psychiatry, 9(5), e22. https://doi.org/10.1016/S2215-0366(22)00079-7 [DOI] [PubMed] [Google Scholar]
- Pierce, N. P. , O'Reilly, M. F. , Sorrells, A. M. , Fragale, C. L. , White, P. J. , Aguilar, J. M. , & Cole, H. A. (2014). Ethnicity reporting practices for empirical research in three autism-related journals. Journal of Autism and Developmental Disorders, 44(7), 1507–1519. https://doi.org/10.1007/s10803-014-2041-x [DOI] [PubMed] [Google Scholar]
- Pinker, S. (2007). The language instinct. Harper Perennial Modern Classics. [Google Scholar]
- Rivera-Figueroa, K. , Marfo, N. Y. A. , & Eigsti, I.-M. (2022). Parental perceptions of autism Spectrum disorder in Latinx and Black sociocultural contexts: A systematic review. American Journal on Intellectual and Developmental Disabilities, 127(1), 42–63. https://doi.org/10.1352/1944-7558-127.1.42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robinson, G. C. , & Norton, P. C. (2019). A decade of disproportionality: A state-level analysis of African American students enrolled in the primary disability category of speech or language impairment. Language, Speech, and Hearing Services in Schools, 50(2), 267–282. https://doi.org/10.1044/2018_lshss-17-0149 [DOI] [PubMed] [Google Scholar]
- Rocher, L. , Hendrick, J. M. , & de Montjoye, Y.-A. (2019). Estimating the success of re-identifications in incomplete datasets using generative models. Nature Communications, 10(1), 3069. https://doi.org/10.1038/s41467-019-10933-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell, G. , Mandy, W. , Elliott, D. , White, R. , Pittwood, T. , & Ford, T. (2019). Selection bias on intellectual ability in autism research: A cross-sectional review and meta-analysis. Molecular Autism, 10(1), Article No. 9. https://doi.org/10.1186/s13229-019-0260-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sabik, N. J. , Matsick, J. L. , McCormick-Huhn, K. , & Cole, E. R. (2021). Bringing an intersectional lens to “open” science: An analysis of representation in the reproducibility project. Psychology of Women Quarterly, 45(4), 475–492. https://doi.org/10.1177/03616843211035678 [Google Scholar]
- Schulz, K. F. , Altman, D. G. , & Moher, D. (2010). CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. Journal of Pharmacology and Pharmacotherapeutics, 1(2), 100–107. https://doi.org/10.4103/0976-500X.72352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shaia, W. E. , Nichols, H. M. , Dababnah, S. , Campion, K. , & Garbarino, N. (2020). Brief report: Participation of Black and African American families in autism research. Journal of Autism and Developmental Disorders, 50(5), 1841–1846. https://doi.org/10.1007/s10803-019-03926-0 [DOI] [PubMed] [Google Scholar]
- Singh, G. K. , Daus, G. P. , Allender, M. , Ramey, C. T. , Martin, E. K. , Perry, C. , De Los Reyes, A. A. , & Vedamuthu, I. P. (2017). Social determinants of health in the United States: Addressing major health inequality trends for the nation, 1935–2016. International Journal of MCH and AIDS, 6(2), 139–164. https://doi.org/10.21106/ijma.236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spencer, S. (2014). Race and ethnicity: Culture, identity and representation. Routledge. https://doi.org/10.4324/9780203519165 [Google Scholar]
- Steinbrenner, J. R. , McIntyre, N. , Rentschler, L. F. , Pearson, J. N. , Luelmo, P. , Jaramillo, M. E. , Boyd, B. A. , Wong, C. , Nowell, S. W. , Odom, S. L. , & Hume, K. A. (2022). Patterns in reporting and participant inclusion related to race and ethnicity in autism intervention literature: Data from a large-scale systematic review of evidence-based practices. Autism, 13623613211072593. https://doi.org/10.1177/13623613211072593 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Storkel, H. L. , & Gallun, F. J. (2022). Announcing a new registered report article type at the journal of speech, language, and hearing research. Journal of Speech, Language, and Hearing Research, 65(1), 1–4. https://doi.org/10.1044/2021_JSLHR-21-00513 [Google Scholar]
- Stroup, D. F. , Berlin, J. A. , Morton, S. C. , Olkin, I. , Williamson, G. D. , Rennie, D. , Moher, D. , Becker, B. J. , Sipe, T. A. , & Thacker, S. B. (2000). Meta-analysis of observational studies in epidemiology: A proposal for reporting. JAMA, 283(15), 2008–2012. https://doi.org/10.1001/jama.283.15.2008 [DOI] [PubMed] [Google Scholar]
- Sweeney, L. , Yoo, J. S. , Perovich, L. , Boronow, K. E. , Brown, P. , & Brody, J. G. (2017). Re-identification risks in HIPAA Safe Harbor data: A study of data from one environmental health study. Technology Science, 2017. [PMC free article] [PubMed] [Google Scholar]
- The BMJ. (2018). New requirements for patient and public involvement statements in BMJ Open. Retrieved May 2, 2022, from https://blogs.bmj.com/bmjopen/2018/03/23/new-requirements-for-patient-and-public-involvement-statements-in-bmj-open/
- The National Commission for the Protection of Human Subjects of Biomedical and Behavioral Research. (1979). The Belmont report. https://www.hhs.gov/ohrp/sites/default/files/the-belmont-report-508c_FINAL.pdf
- Tong, A. , Flemming, K. , McInnes, E. , Oliver, S. , & Craig, J. (2012). Enhancing transparency in reporting the synthesis of qualitative research: ENTREQ. BMC Medical Research Methodology, 12(1), 1–8. https://doi.org/10.1186/1471-2288-12-181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong, A. , Sainsbury, P. , & Craig, J. (2007). Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. International Journal for Quality in Health Care, 19(6), 349–357. https://doi.org/10.1093/intqhc/mzm042 [DOI] [PubMed] [Google Scholar]
- U.K. Equator Centre. (n.d.). Enhancing the quality and transparency of health research. Equator Network. https://www.equator-network.org/ [Google Scholar]
- von Elm, E. , Altman, D. G. , Egger, M. , Pocock, S. J. , Gøtzsche, P. C. , & Vandenbroucke, J. P. (2007). The strengthening the reporting of observational studies in epidemiology (STROBE) statement: Guidelines for reporting observational studies. PLOS Medicine, 4(10), e296. https://doi.org/10.1371/journal.pmed.0040296 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wallerstein, N. B. , & Duran, B. (2006). Using community-based participatory research to address health disparities. Health Promotion Practice, 7(3), 312–323. https://doi.org/10.1177/1524839906289376 [DOI] [PubMed] [Google Scholar]
- Wendler, D. , Kington, R. , Madans, J. , Van Wye, G. , Christ-Schmidt, H. , Pratt, L. A. , Brawley, O. W. , Gross, C. P. , & Emanuel, E. (2005). Are racial and ethnic minorities less willing to participate in health research? PLOS Medicine, 3(2), e19. https://doi.org/10.1371/journal.pmed.0030019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiggins, L. D. , Durkin, M. , Esler, A. , Lee, L. C. , Zahorodny, W. , Rice, C. , Yeargin-Allsopp, M. , Dowling, N. F. , Hall-Lande, J. , Morrier, M. J. , Christensen, D. , Shenouda, J. , & Baio, J. (2020). Disparities in documented diagnoses of autism spectrum disorder based on demographic, individual, and service factors. Autism Research, 13(3), 464–473. https://doi.org/10.1002/aur.2255 [DOI] [PMC free article] [PubMed] [Google Scholar]