Abstract
Background
In late 2018, VHA implemented a multi-stage suicide risk screening and evaluation initiative, Suicide Risk Identification Strategy, or “Risk ID,” in primary care settings.
Objective
The main objective of this study was to characterize VHA primary care patient perspectives regarding population-based suicide risk screening through the Risk ID program.
Design
Mixed methods; survey and qualitative interviews.
Participants
Veterans screened for suicide risk using Risk ID in primary care (n = 868) participated in a survey of veteran attitudes about screening (45% response rate); thirty additionally participated in follow-up qualitative interviews.
Main Measures
The quantitative survey consisted of three questions on attitudes about screening for suicidal thoughts in primary care. In qualitative interviews, veterans were asked about their experiences with the Risk ID processes and recommendations for improving Risk ID.
Key Results
Over 90% of veterans reported that it is appropriate for primary care providers or nurses/medical assistants to ask veterans about thoughts of suicide during primary care visits. Approximately half of veterans indicated that veterans should be asked about suicidal thoughts at every visit. Qualitative findings revealed that while most veterans were generally supportive and appreciated VHA screening for suicidal thoughts, they also expressed concern for the potential for inadvertent harm. Participants expressed conflicting preferences for how screening should be handled and delivered.
Conclusions
Findings suggest that most veterans support the integration of standardized suicide risk assessment into routine primary care visits. However, findings also suggest that population-based suicide risk assessment should further consider patient experiences and preferences. Specifically, additional guidance or training for staff conducting suicide risk screening may be warranted to ensure patients feel heard (e.g., eye contact, expressing empathy) and increase patient understanding of the purpose of the screening and potential outcomes. These patient-centered approaches may improve patient experience and facilitate disclosure of suicidal thoughts.
Supplementary Information
The online version contains supplementary material available at 10.1007/s11606-023-08148-w.
KEY WORDS: Suicide, Veterans, Primary care, Patient-centered care
INTRODUCTION
The United States (U.S.) suicide rate increased 30% between 2000 and 2020, and suicide was the 12th leading cause of death for all ages in 2020.1 Veterans are 1.5 times more likely to die by suicide compared to non-veterans,2 and on average, approximately 18 veterans die by suicide each day.3 Although the United States Preventive Services Task Force concluded in 2014 that insufficient evidence existed to recommend universal screening for suicide risk in primary care,4 subsequent relevant research,5–9 clinical practice guidelines,10 and the “zero suicide” initiative11,12 prompted VA and other healthcare systems13–15 to implement routine suicide risk screening. Furthermore, veterans frequently engage with primary care in the months and days prior to suicide death,16,17 with almost half of those who receive care in the 6 months prior to death making contact with their primary care team.17
In late 2018, the Veterans Health Administration (VHA) implemented a multi-stage suicide risk assessment initiative, Suicide Risk Identification Strategy, or “Risk ID.”5 Risk ID is an evidence-informed,10 multi-stage suicide risk assessment process, which includes initial screening (which is what we focus on in this analysis) and subsequent evaluation when indicated. Clinical staff screen all veterans receiving VHA care annually for suicidal ideation and behaviors using the Columbia Suicide Severity Rating Scale Screener (C-SSRS Screener).18 Clinical staff then evaluate those who screen positive on the C-SSRS Screener using VHA’s Comprehensive Suicide Risk Evaluation (CSRE). VHA developed the CSRE for use in clinical settings and is a structured clinical tool addressing suicidal ideation, plan, and intent; suicidal behaviors; and risk and protective factors. Most screening takes place in primary care and mental health specialty settings.
Routine screening for suicide risk may, however, be perceived negatively by patients. Earlier research on VHA’s first iteration of suicide risk screening, implemented a decade ago, suggested that veterans generally accepted the rationale for screening and appreciated that it was straightforward.19 On the other hand, some veterans found the discussions difficult or were unsure or fearful of what might follow disclosure of suicidal ideation. Veterans also reported concerns over a lack of focus on patient priorities, dissatisfaction with repeated questioning, distrust in the healthcare system, or rifts in patient-clinician rapport.19 Recent studies have also found that individuals perceive suicide risk screening or other behavioral health screening to be acceptable overall,13,20–23 but report important drawbacks including mismatch between screening item wording and the patient’s experience (e.g., lack of nuance) and fears of consequences of disclosure (e.g., involuntary hospitalization).13 Furthermore, the extent of patients’ honest disclosure of suicidal thoughts remains unclear and may be affected by how screening is conducted.13,19 That is, although patients accept the rationale for suicide risk screening, they have raised important limitations and concerns with its use.
Population-based (“universal”) suicide risk screening and evaluation processes are increasingly being implemented in primary care settings,5,13–15 and improvements in disclosure that may come from improved delivery could have downstream effects such as better matching of intervention to level of risk.24 It is therefore critical to understand patient attitudes toward routine screening, find ways to reduce potential negative impacts on patients, and learn how to make the screening process more patient-centered.25 The main objective of the current mixed-methods study was to characterize VHA primary care patient perspectives regarding population-based suicide risk screening through the Risk ID program.
METHODS
This study was reviewed and approved by the joint Institutional Review Board of the VA Portland Healthcare System and Oregon Health & Science University, where this study took place. This study was conducted under a waiver of documentation of written consent.
Setting
VHA serves 9 million veterans nationally each year at over 1200 facilities. Risk ID is facilitated via a national mandatory clinical reminder within the electronic healthcare record and comprises two stages: the patient is initially screened using the C-SSRS18, and if the patient screens positive (yes response to items 3, 4, 5, or 6b), the VHA Comprehensive Suicide Risk Evaluation (CSRE) is used to further evaluate risk. VHA primary care teams (i.e., health technicians, LPNs, RNs, and PCPs) typically administer the C-SSRS; if the C-SSRS is positive, co-located mental health clinicians, available in most clinic settings, often complete the mandatory same-day CSRE and help to arrange follow-up care as indicated. All clinicians have completed VA mandatory training on the use of these tools.
Sample and Recruitment
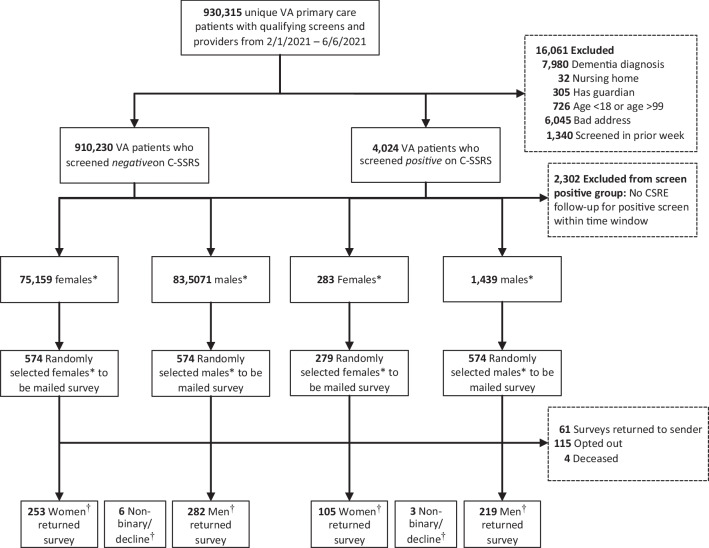
We used national VHA administrative datasets to identify potential participants. These datasets contain healthcare utilization, diagnosis, and demographic data, including Risk ID assessment data (date, results), for all veterans enrolled in VHA care. Data for this study represent all VHA facilities, with one exception: the rollout of VHA’s new electronic health record (EHR) made data from one facility in the Pacific Northwest inaccessible at the time of this study. Between February and October 2021, we sampled veterans aged 18–99 screened with the C-SSRS in primary care settings (Fig. 1). We excluded veterans if they were institutionalized (nursing home, hospice), had a designated guardian, had a dementia or other cognitive disorder diagnosis entered into the EHR in the prior 12 months, or did not receive a CSRE follow-up (same or next day) for a positive C-SSRS screen. We randomly selected veterans from the larger national pool of eligible veterans each week, stratifying by biological sex (female/male) and C-SSRS result (positive/negative) to oversample for female veterans and veterans with positive C-SSRS results. We mailed surveys to 2001 eligible veterans and received 65 surveys returned as undeliverable; 1936 veterans received the survey. Of these, 868 (45%) returned the survey within the study window (up to 2 months following the final reminder mailing). Compared to non-respondents, respondents were more likely to be older (mean age 61 [sd = 16] vs. 54 [sd = 17], p < 0.001), non-Hispanic (91% vs. 86%; p < 0.001), not have been diagnosed with a mental health condition in the prior year (60% vs. 55%; p = 0.03), and have had a negative C-SSRS screen result (62% vs. 54%; p < 0.001).
Figure 1.
Consort diagram. *Biological sex, available in VHA administrative data. †Gender identity, as reported on the survey
We used a modified Dillman approach to recruit eligible veterans to complete the survey. We sent initial mailings within 2 weeks of screening. The initial mailing included an introductory letter, a document detailing elements of informed consent, the paper survey, and a pre-paid return envelope. The survey provided instructions to complete the survey online, if preferred. We sent up to three reminder mailings to non-respondents at 3-week intervals. Survey respondents received $35.
The survey asked veterans if they would be willing to participate in a qualitative interview. Fifty-nine percent of survey respondents (n = 512) expressed interest, comprising our pool of potential interview participants. We then purposively invited veterans to participate in interviews based on demographic characteristics and suicide risk screen result; we sought to obtain an interview sample that was demographically diverse and had approximately equal number of veterans who screened positive and negative for suicidal ideation. We also sought equal numbers of veterans identifying as women and men. We ceased inviting interview participants when the analytic team agreed that additional interviews would not yield new information. Thirty veterans participated in interviews and received an additional $40.
Data Sources
VHA Administrative Data
We used VHA administrative data on participants’ age, urban or rural residence status, prior-year VHA care utilization (yes/no), prior-year mental health diagnoses (anxiety, depression, substance use disorders, post-traumatic stress disorder [PTSD], psychosis), and service connection status (an indicator of an illness or injury incurred or aggravated during active military service).
Survey
The survey gathered self-report information on demographic characteristics (gender, race/ethnicity, marital status, education, employment status). The Kessler-6 non-specific distress scale assessed mental health symptoms.26 A three-item scale from the Well-being Inventory27 measured patient satisfaction with their mental and physical health, and a single item created by the research team (based on research from the Pew Research Center) asked about strength of religious belief rated from 0 (“none whatsoever”) to 7 (“very strong”). “Strong” religious beliefs were defined by a score of 6 or 7. Three questions assessed perceptions of healthcare providers asking about suicidal thoughts. The first two questions had yes/no response options and asked whether (a) primary care providers (e.g., doctors or nurse practitioners) and (b) primary care nurses or medical assistants should ask about thoughts of suicide, respectively. The third question asked respondents how often they thought veterans should be asked about thoughts of suicide, with response options of (0) “Never,” (1) “At each doctor visit,” (2) “Annually,” (3) “Once, when they enroll in care,” and (4) “The frequency should only depend on the veteran’s symptoms.”
Qualitative Interviews
We used a semi-structured interview guide to ask veterans about their experiences being screened for suicidal thoughts in primary care. The first section of the guide contained questions about participants’ VHA care and their experiences with the Risk ID screening process. The second section of the guide contained questions focused on communication between the participants and their clinicians regarding the suicide risk assessment and care options following the assessment. The final section of the guide asked for participants’ recommendations on improving the Risk ID process or suicide risk assessment and prevention broadly. Interviews occurred over the telephone, were audio recorded, and subsequently transcribed.
Analysis
Survey
We used VHA administrative data to supplement survey data when race/ethnicity or gender was missing. We weighted survey data to represent the population of veterans eligible for the study. Sampling and non-response weights were used to calculate final weights. Sampling weights accounted for the likelihood of being included in the sample within each of the 36 strata created for biological sex, C-SSRS result, and recruitment period combination (although sampling was done for each of the 18 weeks, due to low frequencies of females with positive screens, we created 9 two-week recruitment periods for weighting purposes). We calculated non-response weights using the propensity scores of a logistic regression model adjusting for C-SSRS result, biological sex, recruitment period, age, ethnicity, and the 3-way interaction plus all lower-order interactions between C-SSRS result, biological sex, and recruitment period. Within each of the strata, there were no significant differences in demographics between the population and those sampled.
We summarized the data stratified by C-SSRS result, using weighted statistics (means and standard deviations for continuous variables and percentages for categorical variables). Original (i.e., pre-weighting) sample frequencies are presented for categorical variables. We used the survey package (version 4.0)28,29 in R (version 4.1.2)30 for analyses, which uses a design-based t test for continuous outcomes and the second-order Rao-Scott correction to the Pearson chi-squared test31 for categorical outcomes.
Qualitative Interviews
The interdisciplinary qualitative analyst team consisted of two research assistants and two experienced qualitative researchers (a sociologist and a social psychologist). Using the interview guide and research questions, the analyst team created an initial codebook. Next, implementing a conventional-directed hybrid approach,32 each member of the analytic team independently reviewed transcripts using the codebook followed by a meeting to discuss, update, and refine the codebook.. Atlas.ti was used to assist analysis. Once coding was complete, all analysts reviewed data (i.e., transcript excerpts derived from code reports) relevant to the primary research questions to refine, and come to agreement on, findings. Qualitative data were then considered in light of survey findings to inform study conclusions.
RESULTS
Survey
Table 1 shows the demographic and clinical characteristics of veterans screened using the C-SSRS (weighted for survey non-response, sampling strategy, and time period of recruitment). The average age was 65 (sd = 15.4; 95% CI 63–67) years, and the majority were male (91%; 95% CI 90–92%), white (76%; 95% CI 71–81%), and non-Hispanic (95%; 92–97%). Sixty percent (95% CI 54–66%) reported “strong” religious beliefs. Veterans with a positive C-SSRS were younger and more frequently female, Hispanic, Black, and at least 50% service connected, or had a mental health diagnosis than veterans with a negative C-SSRS. They also more frequently reported “weak” religious beliefs, worse overall health functioning, and higher psychological distress.
Table 1.
Participant Characteristics by C-SSRS Screening Result
| Negative C-SSRS, n = 541 | Positive C-SSRS, n = 327 | Overall, n = 868 | ||||
|---|---|---|---|---|---|---|
| n | Weighted proportion (95% CI) | n | Weighted proportion (95% CI) | n | Weighted proportion (95% CI) | |
| Age, mean, sd | 541 | 64.89 (62.97, 66.80) | 327 | 55.05 (52.98, 57.12) | 868 | 64.87 (62.96, 66.78) |
| Gender | ||||||
| Woman | 253 | 8.66 (7.81, 9.60) | 105 | 16.18 (15.26, 17.15) | 358 | 8.68 (7.82, 9.61) |
| Man | 282 | 91.15 (90.22, 91.99) | 219 | 83.09 (81.90, 84.22) | 501 | 91.13 (90.21, 91.97) |
| Non-binary/did not identify/unsure/declined | 6 | 0.19 (0.08, 0.43) | 3 | 0.73 (0.22, 2.35) | 9 | 0.19 (0.08, 0.43) |
| Ethnicity | ||||||
| Hispanic | 40 | 5.09 (2.99, 8.52) | 35 | 12.13 (8.34, 17.3) | 75 | 5.1 (3.01, 8.52) |
| Non-Hispanic | 499 | 94.91 (91.48, 97.01) | 292 | 87.87 (82.70, 91.66) | 791 | 94.9 (91.48, 96.99) |
| Race | ||||||
| White | 375 | 76.04 (70.85, 80.55) | 211 | 64.4 (58.51, 69.87) | 586 | 76.02 (70.84, 80.52) |
| Black/African American | 117 | 18.91 (14.75, 23.91) | 69 | 22.26 (17.87, 27.36) | 186 | 18.91 (14.76, 23.91) |
| Asian | 6 | 0.2 (0.09, 0.46) | 4 | 1.9 (0.67, 5.30) | 10 | 0.21 (0.09, 0.46) |
| American Indian or Alaska Native | 5 | 0.67 (0.20, 2.20) | 6 | 1.93 (0.89, 4.15) | 11 | 0.67 (0.20, 2.20) |
| Native Hawaiian/Pacific Islander | 1 | 0.03 (0.00, 0.24) | 3 | 0.64 (0.22, 1.82) | 4 | 0.03 (0.01, 0.23) |
| Multi-racial | 35 | 4.15 (2.52, 6.76) | 30 | 8.88 (5.69, 13.61) | 65 | 4.16 (2.53, 6.76) |
| Marital status | ||||||
| Married or living together | 257 | 60.82 (54.78, 66.55) | 157 | 54.5 (48.47, 60.4) | 414 | 60.81 (54.77, 66.53) |
| Not living together | 239 | 39.18 (33.45, 45.22) | 144 | 45.5 (39.6, 51.53) | 383 | 39.19 (33.47, 45.23) |
| Education | ||||||
| Less than some college | 115 | 29.77 (24.71, 35.37) | 84 | 28.99 (24.19, 34.32) | 199 | 29.77 (24.72, 35.36) |
| Some college or greater | 392 | 70.23 (64.63, 75.29) | 229 | 71.01 (65.68, 75.81) | 621 | 70.23 (64.64, 75.28) |
| Employment | ||||||
| Employed | 157 | 26.73 (21.57, 32.62) | 96 | 33.73 (28.31, 39.61) | 253 | 26.74 (21.59, 32.62) |
| All others | 337 | 73.27 (67.38, 78.43) | 206 | 66.27 (60.39, 71.69) | 543 | 73.26 (67.38, 78.41) |
| Rural/urban | ||||||
| Rural | 195 | 38.56 (33.11, 44.32) | 115 | 34.33 (29.23, 39.81) | 310 | 38.56 (33.11, 44.3) |
| Urban | 346 | 61.44 (55.68, 66.89) | 210 | 65.67 (60.19, 70.77) | 556 | 61.44 (55.70, 66.89) |
| Spirituality/religion strength* | ||||||
| Strong | 300 | 59.83 (53.82, 65.57) | 144 | 44.4 (38.62, 50.34) | 444 | 59.80 (53.8, 65.53) |
| Weak | 193 | 40.17 (34.43, 46.18) | 157 | 55.6 (49.66, 61.38) | 350 | 40.20 (34.47, 46.2) |
| Service connection | ||||||
| At least 50% | 238 | 44.55 (39.00, 50.23) | 178 | 56.96 (51.39, 62.36) | 416 | 44.57 (39.03, 50.25) |
| Below 50% | 116 | 20.42 (16.14, 25.49) | 70 | 21.07 (16.90, 25.95) | 186 | 20.42 (16.15, 25.48) |
| No service connection | 187 | 35.03 (30.11, 40.3) | 79 | 21.97 (17.82, 26.76) | 266 | 35.01 (30.10, 40.26) |
| Prior VA care | 521 | 96.98 (94.22, 98.44) | 314 | 96.52 (93.99, 98.01) | 835 | 96.98 (94.22, 98.44) |
| Any mental health condition† | 154 | 26.65 (21.73, 32.22) | 191 | 57.79 (52.01, 63.36) | 345 | 26.71 (21.80, 32.27) |
| Substance use disorder‡ | 7 | 2.20 (0.82, 5.79) | 15 | 4.93 (2.92, 8.21) | 22 | 2.21 (0.83, 5.78) |
| Health functioning§, mean, sd | 505 | 11.57 (11.22, 11.92) | 308 | 7.67 (7.36, 7.98) | 813 | 11.56 (11.22, 11.91) |
| Psychological distress||, mean, sd | 501 | 10.61 (10.00, 11.22) | 310 | 20.82 (20.24, 21.4) | 811 | 10.63 (10.02, 11.24) |
Weighted values are weighted for survey non-response and week of survey mailing
*Spirituality/religion strength ranges from 0 to 5 for weak and 6 to 7 for strong
†Includes disorders related to anxiety, mood, psychosis, substance use, and alcohol use
‡Includes use of cannabis, cocaine, alcohol, stimulants, hallucinogens, opioids, and sedatives
§Mean score, ranging from 1 to 5 (higher scores indicate higher satisfaction with functioning)
||Mean score, ranging from 1 to 5 (higher scores indicated higher distress)
Table 2 (weighted data) shows that 94% (95% CI 91–96%) of veterans screened using the C-SSRS reported that they think it is appropriate for primary care providers to ask veterans about thoughts of suicide; 92% (95% CI 88–94%) felt it is appropriate for nurses and medical assistants to ask about these thoughts as well. Fifty-three percent (95% CI 47–59%) felt it is appropriate to ask about these thoughts at every doctor’s visit, while 35% (95% CI 30–41%) felt that screening frequency should depend on the veteran’s symptoms. These attitudes did not appear to differ by C-SSRS result.
Table 2.
Attitudes About Being Screened, Survey Responses by C-SSRS Screen Result
| Negative C-SSRS, n = 541 | Positive C-SSRS, n = 327 | Overall | ||||
|---|---|---|---|---|---|---|
| n | Weighted proportion (95% CI) | n | Weighted proportion (95% CI) | n | Weighted proportion (95% CI) | |
| Do you think it is appropriate for primary care providers (e.g., doctors or nurse practitioners) to ask veterans about their thoughts of suicide? | ||||||
| No | 27 | 5.86 (3.61, 9.38) | 22 | 6.72 (4.43, 10.08) | 49 | 5.86 (3.62, 9.37) |
| Yes | 468 | 94.14 (90.62, 96.39) | 289 | 93.28 (89.92, 95.57) | 757 | 94.14 (90.63, 96.38) |
| Do you think it is appropriate for primary care nurses or medical assistants to ask veterans about their thoughts of suicide? | ||||||
| No | 43 | 8.46 (5.68, 12.41) | 32 | 9.05 (6.41, 12.64) | 75 | 8.46 (5.69, 12.40) |
| Yes | 454 | 91.54 (87.59, 94.32) | 275 | 90.95 (87.36, 93.59) | 729 | 91.54 (87.6, 94.31) |
| How often should veterans be asked about thoughts of suicide? | ||||||
| Never | 9 | 2.28 (1.17, 4.42) | 4 | 1.16 (0.48, 2.79) | 13 | 2.28 (1.17, 4.41) |
| At each doctor visit | 284 | 52.74 (46.82, 58.59) | 168 | 55.58 (49.68, 61.33) | 453 | 52.75 (46.84, 58.58) |
| Annually | 37 | 8.19 (5.49, 12.06) | 12 | 4.21 (2.32, 7.51) | 49 | 8.18 (5.48, 12.04) |
| Once when they enroll in care | 7 | 1.73 (0.74, 4.00) | 5 | 1.59 (0.70, 3.59) | 12 | 1.73 (0.74, 3.99) |
| The frequency should depend on the veteran’s symptoms | 174 | 35.06 (29.66, 40.87) | 124 | 37.47 (32.04, 43.23) | 298 | 35.06 (29.67, 40.86) |
Weighted values are weighted for survey non-response and week of survey mailing
Qualitative Interviews
Thirty veterans participated in qualitative interviews (Table 3). Because we selected for a diverse group of interview participants, proportions of women, minorities, and individuals with positive C-SSRS screens were higher than in the main survey sample. The online appendix contains additional participant quotes.
Table 3.
Qualitative Interview Participant Characteristics
| Characteristic | n = 30 |
|---|---|
| Age, mean (sd) | 49 (14) |
| Gender | |
| Woman | 13 (43.3%) |
| Man | 15 (50.0%) |
| Non-binary/did not identify/unsure/declined to answer | 2 (6.7%) |
| Ethnicity | |
| Hispanic | 3 (10.0%) |
| Non-Hispanic | 27 (90.0%) |
| Race | |
| Asian | 3 (10.0%) |
| Black/African American | 7 (23.3%) |
| Multi-racial | 4 (13.3%) |
| White | 16 (53.3%) |
| Marital status | |
| Married or living together | 13 (43.3%) |
| Single/divorced/widowed | 16 (53.3%) |
| Missing | 1 |
| Education | |
| Less than some college | 5 (16.6%) |
| Some college or greater | 25 (83.3%) |
| Employment | |
| Unemployed/retired/unable to work | 17 (56.7%) |
| Employed | 12 (40.0%) |
| Missing | 1 |
| Urban residence | 22 (73.3%) |
| Spirituality/religion strength* | |
| Strong | 17 (56.7%) |
| Weak | 11 (36.6%) |
| Missing | 2 |
| Service connection at least 50% | 15 (50.0%) |
| Prior VA care | 29 (96.6%) |
| Any mental health condition† | 12 (40.0%) |
| Any substance use disorder‡ | 1 (3.3%) |
| Overall health functioning§, mean (sd) | 3.14 (1.14) |
| Psychological distress||, mean (sd) | 2.84 (1.26) |
*Spirituality/religion strength ranges from 0 to 5 for weak and 6 to 7 for strong
†Includes disorders related to anxiety, mood, psychosis, substance use, and alcohol use
‡Includes use of cannabis, cocaine, alcohol, stimulants, hallucinogens, opioids, and sedatives
§Mean score, ranging from 1 to 5 (higher scores indicate higher satisfaction with functioning)
||Mean score, ranging from 1 to 5 (higher scores indicated higher distress)
Opportunity Versus Drawbacks
Veterans felt there was a strong rationale for screening veterans for suicidal thoughts in primary care. Namely, they connected the need for screening to their beliefs of high veteran suicide rates. They also believed screening should continue. However, veterans saw both pros and cons to screening as it is currently being conducted in primary care. On the one hand, veterans saw a welcome opportunity for screening to provide space to discuss suicidal thoughts. For example, some veterans indicated that they personally would not be comfortable discussing suicidal thoughts with family or friends but would with their doctor, and likewise surmised that there are other veterans who could be identified as at risk using this process.
I know from my experience that this is something that I don’t talk to anybody about. I don’t talk to my wife about it. And you know don’t really talk to any friends about it. So, you know I think it is good that people have the opportunity to talk about this, you know something that they maybe wouldn’t tell anyone else. (Gulf war–era veteran, C-SSRS positive)
Veterans also discussed drawbacks of screening. One drawback was that screening could take time away from discussing other health concerns with their doctor and—by extension—may make veterans feel as though their primary health concerns are being dismissed. Repeated screening was also a potential concern; not only could it become annoying or distressing, but veterans also wondered if repeated screening could turn the screening process into “white noise” (Gulf war-era veteran, C-SSRS positive) that providers and veterans would ignore.
Suicide Risk Screening Should Be Handled More Delicately Than Other Screens, but Also Normalized
Veterans made it clear that how they were asked about suicide risk was important to them and that suicide risk screening required more care and attention than other screens delivered in primary care. They noted that question wording, body language, and care team role affected whether the process was a positive or negative experience. Some veterans reported they preferred being asked by their provider rather than the nurse or other assistant. Veterans preferred when the screening was delivered in a direct manner—being calm, straightforward, and not “sugarcoating” (Vietnam-era veteran, C-SSRS positive) the screening. Veterans also preferred direct eye contact with the person conducting the screen.
Veterans desired the screening process to be more personal and conversational, and tailored to the individual. For many veterans, especially those screening negative, the screening process currently feels too rote and “cookie cutter” which borders on feeling insensitive. One veteran noted that the rote nature of the screening was especially problematic for those who have lost a loved one to suicide.
I mean if you ask an Iraq, Afghan veteran who’s lost a friend or two to suicide, I guess you might think you want to not be insensitive by making it sound like it’s a canned, scripted question. (Vietnam-era veteran, C-SSRS negative)
Despite expressing specific ways in which the suicide risk screening process should be handled more carefully than other screening, veterans simultaneously desired the suicide risk screening process to feel like a normalized, routine part of care.
So, it’s good that it’s being asked for sure. I mean it should be something that’s part of normal mental health. You know mental health should be accepted…people have mental health problems. It should be considered normal and not something to be ashamed of, I guess I’m trying to say. (Gulf war–era veteran, C-SSRS positive)
Expectations of Provider or Healthcare System Response Affect Disclosure of Suicidal Thoughts
Veterans’ expectations of providers’ responses played a role in whether they felt they could disclose suicidal thoughts. Trust and “feeling heard” were commonly reported as essential for being honest about their mental health status. Importantly, sensing that the person asking the questions cares about the answer to the screening questions and them as a person supported honest disclosure of suicidal thoughts. When veterans reported being dishonest during screening, they commonly noted this was due to fear of staff overreacting, and that they particularly feared being involuntarily hospitalized. For some patients, previous experiences with screening had been distressing, and they wish to avoid similar experiences in the future. One veteran described his experience following a recent screening where his autonomy was challenged; and he feared being hospitalized:
I went a few months ago…I kept telling him that I didn’t wanna talk about it. He actually Baker Acted [involuntarily hospitalized] me. Or tried to have me Baker Acted. But when the psychiatrist spoke with me, I was released within I’d say an hour or two. I was talking about something that bothered me, or had been bothering me, but it wasn’t bothering me at that particular time. And I didn’t wanna talk about it because there was no need at that time to discuss it. (Vietnam-era veteran, C-SSRS negative)
Some veterans reported hesitancy in being honest during screening due to previously facing identity-based discrimination within Department of Veterans Affairs (VA) systems. For example, a Black female veteran reported that encountering racial discrimination when filing her VA benefits claim (i.e., not receiving the same level of service connectedness as her White counterparts with similar injuries) led her to feel like the care system is not interested in helping her. As a result, she is less willing to be honest when screened for suicide risk.
It’s one of the main reasons why when I do go in, they don’t get an honest response. Or they don’t get anything from me because I feel that you’re not for me, you’re not trying to help me, you don’t wanna help me, and why even go through it, go through the motions it seems. So, I can come in feeling suicidal and I leave out feeling suicidal then. (Gulf war–era veteran, C-SSRS positive)
DISCUSSION
In this national, mixed-methods study, we examined veterans’ perspectives of VHA’s universal suicide risk screening process, Risk ID, in primary care settings. Most veterans were supportive of screening in primary care, regardless of screening result, and approximately half of survey respondents indicated that veterans should be asked about suicidal thoughts at every healthcare visit. Qualitative findings revealed some caveats to their support of Risk ID processes; participants expressed some concerns regarding potential drawbacks to screening for suicide risk. They also expressed conflicting preferences for how screening should be handled and delivered. Finally, veterans noted that honest disclosure of suicidal thoughts frequently depended on the response they expected from their provider or the healthcare system—with increased trust, caring, and an otherwise stronger clinician-patient relationships supporting disclosure.
Overall, veterans felt it was appropriate for primary care providers and teams to frequently ask about suicidal thoughts at healthcare visits. As noted in the qualitative interviews, this endorsement may derive from an awareness of veteran suicide rates and a desire to ensure their fellow veterans are taken care of. Prior research on suicidal ideation assessments in VHA found a similar sentiment among veteran participants, who believed the systematic assessment was necessary to prioritize care for those who most needed it.19 Qualitative findings in the current study further suggested that veterans believe screening provides a chance for care teams to identify veterans who need additional support and gives patients the opportunity to talk about suicidal thoughts with someone who could help. Other research from a rural community mental health clinic found similarly high acceptance of screening as well as similar rationales for accepting universal suicide risk screening; for example, screening is about saving lives, can facilitate disclosure of suicidal thoughts, and provides help to those at risk.20 Furthermore, veterans expect to be asked about suicidal thoughts, as screenings in the military and VHA have been used in various forms for some time. Together, these findings suggest that reinforcing the potential broader population-level benefits of suicide risk screening may further increase individual patient acceptance of screening. For non-veteran patient populations, wherein awareness of suicide rates may not be as prevalent, patient education about suicide rates during the screening process may provide beneficial context.
Findings also demonstrated continuing concerns among veterans about repeated screening for suicide risk, insensitive or uncaring screening delivery, and fears over involuntary hospitalizations, consistent with earlier research.13,19 In our interviews, some veterans relayed negative screening experiences that made them feel unheard, took valuable time away from their ability to address other care concerns with their provider, or resulted in unwanted hospitalizations. This suggests that, despite changes to the structure of suicide risk assessments taking place over the past decade, more work is needed to ensure that patients have positive experiences of care following initial screening. Specifically, screening frequency may need to be tailored for certain patients based on histories of suicidal thoughts or behavior to ensure adequate time for patients’ other health concerns. Also, more needs to be done to ensure that patients understand the potential outcomes of screening and under what conditions hospitalization is warranted (i.e., that hospitalization is not the default response to patients who report suicidal ideation). On the provider side, increasing provider skill in screening delivery and response to patient-reported suicide risk (i.e., matching level of response to risk level) also deserves additional attention. In fact, the patient experiences reported here align with other qualitative work examining staff experiences with the Risk ID process.33 Staff reported challenges balancing the time required to complete Risk ID components with other patient care needs, and they felt additional guidance or training would be helpful to reduce unnecessary escalations of patient care (e.g., hospitalizations, requesting mental health follow-up) and improve care coordination between primary care and mental health providers.
There are some limitations to this study. First, this study was conducted within the VHA with veterans, which may limit applicability to other care systems and patient populations. However, VHA’s Risk ID process (i.e., a brief screen followed by additional assessment) is similar to what happens in other health systems and is consistent with zero suicide recommendations.11,12,15,34 Participants may have been more interested in participating if they held strong feelings about the Risk ID process, which might have influenced the degree of acceptance of the screening both on the survey and in qualitative interviews. Survey findings were weighted for non-response, however, and qualitative interview participants were invited from a large pool of potentially interested participants (more than half of survey respondents). It is also possible that veterans who screened negative on the C-SSRS had thoughts of suicide they did not disclose at the time of screening or previously had screened positive for suicide risk on the C-SSRS, which would affect comparisons of veterans with positive and negative C-SSRS results. In qualitative interviews, it was apparent that both situations may exist, but quantitative data suggested few differences in experiences and opinions of Risk ID between these two groups.
Nearly a decade after VHA implemented its first version of suicide risk assessment, the new suicide risk assessment process (Risk ID) is more developed, more uniformly implemented across the healthcare system, and administered across the VA patient population.5 Findings here suggest that while veterans are supportive of routine suicide risk screening in primary care, these improvements have not fully addressed patient preferences related to suicide risk screening. Additional guidance or training for staff conducting suicide risk assessment is warranted; delivering screens in ways that ensure patients feel heard (e.g., eye contact, expressing empathy) and that increase patient understanding of the purpose and potential outcomes of screening may improve patient experience and facilitate disclosure of suicidal thoughts.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
This material is based upon work supported by the United States Department of Veterans Affairs, Veterans Health Administration, and VA Health Services Research & Development Service (HSR&D) project IIR19-215. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or US government.
Data Availability
Data are not available due to institutional regulations.
Declarations
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Garnett MF, Curtin SC, Stone DM. Suicide mortality in the United States, 2000–2020. NCHS Data Brief. 2022;433:1–8. [PubMed] [Google Scholar]
- 2.Office of Mental Health and Suicide Prevention . VA national suicide data report 2005–2015. Washington DC: U.S. Department of Veterans Affairs; 2018. [Google Scholar]
- 3.Office of Mental Health and Suicide Prevention . National veteran suicide prevention annual report. Washington DC: U.S. Department of Veterans Affairs; 2020. [Google Scholar]
- 4.LeFevre ML, U.S. Preventive Services Task Force Screening for suicide risk in adolescents, adults, and older adults in primary care: U S Preventive Services Task Force recommendation statement. Ann Intern Med. 2014;160(10):719–726. doi: 10.7326/M14-0589. [DOI] [PubMed] [Google Scholar]
- 5.Bahraini N, Brenner LA, Barry C, et al. Assessment of rates of suicide risk screening and prevalence of positive screening results among US veterans after implementation of the veterans affairs suicide risk identification strategy. JAMA Network Open. 2020;3(10):e2022531–e2022531. doi: 10.1001/jamanetworkopen.2020.22531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Simon GE, Rutter CM, Peterson D, et al. Does response on the PHQ-9 depression questionnaire predict subsequent suicide attempt or suicide death? Psychiatr Serv. 2013;64(12):1195–1202. doi: 10.1176/appi.ps.201200587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Simon GE, Coleman KJ, Rossom RC, et al. Risk of suicide attempt and suicide death following completion of the patient health questionnaire depression module in community practice. J Clin Psychiatry. 2016;77(2):221–227. doi: 10.4088/JCP.15m09776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Louzon SA, Bossarte R, McCarthy JF, Katz IR. Does suicidal ideation as measured by the PHQ-9 predict suicide among VA patients? Psychiatr Serv. 2016;67(5):517–522. doi: 10.1176/appi.ps.201500149. [DOI] [PubMed] [Google Scholar]
- 9.Mann JJ, Michel CA, Auerbach RP. Improving suicide prevention through evidence-based strategies: a systematic review. Am J Psychiatry. 2021:appi. ajp. 2020.20060864. [DOI] [PMC free article] [PubMed]
- 10.Department of Veterans Affairs and Department of Defense . VA/DoD clinical practice guideline for the assessment and management of patients at risk for suicide. Washington DC: Author; 2019. [DOI] [PubMed] [Google Scholar]
- 11.U.S. Surgeon General, National Action Alliance for Suicide Prevention. 2012 national strategy for suicide prevention: Goals and objectives for action: a report of the U.S. surgeon general and of the national action alliance for suicide prevention. Washington DC: Author; 2012.
- 12.Brodsky BS, Spruch-Feiner A, Stanley B. The zero suicide model: applying evidence-based suicide prevention practices to clinical care. Front Psychiatr. 2018;9:33. doi: 10.3389/fpsyt.2018.00033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Richards JE, Hohl SD, Whiteside U, et al. If you listen, I will talk: the experience of being asked about suicidality during routine primary care. J Gen Intern Med. 2019;34(10):2075–2082. doi: 10.1007/s11606-019-05136-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Richards JE, Simon GE, Boggs JM, et al. An implementation evaluation of “Zero suicide” using normalization process theory to support high-quality care for patients at risk of suicide. Implement Res Pract. 2021;2:26334895211011769. doi: 10.1177/26334895211011769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Roaten K, Johnson C, Genzel R, Khan F, North CS. Development and implementation of a universal suicide risk screening program in a safety-net hospital system. Jt Comm J Qual Patient Saf. 2018;44(1):4–11. doi: 10.1016/j.jcjq.2017.07.006. [DOI] [PubMed] [Google Scholar]
- 16.Denneson LM, Williams HB, Kaplan MS, McFarland BH, Dobscha SK. Treatment of veterans with mental health symptoms in VA primary care prior to suicide. Gen Hosp Psychiatry. 2016;38:65–70. doi: 10.1016/j.genhosppsych.2015.08.007. [DOI] [PubMed] [Google Scholar]
- 17.Denneson LM, Kovas AE, Britton PC, Kaplan MS, McFarland BH, Dobscha SK. Suicide risk documented during veterans’ last VA healthcare contacts prior to suicide. Suicide Life Threat Behav. 2016;46(3):363–374. doi: 10.1111/sltb.12226. [DOI] [PubMed] [Google Scholar]
- 18.Posner K, Brown GK, Stanley B, et al. The columbia-suicide severity rating scale: initial validity and internal consistency findings from three multisite studies with adolescents and adults. Am J Psychiatry. 2011;168(12):1266–1277. doi: 10.1176/appi.ajp.2011.10111704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ganzini L, Denneson LM, Press N, et al. Trust is the basis for effective suicide risk screening and assessment in veterans. J Gen Intern Med. 2013;28(9):1215–1221. doi: 10.1007/s11606-013-2412-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Christensen-LeCloux M, Weimer M, Bjorkgren K, Booker W, Campo JV. Universal suicide risk screening: views of rural adults on acceptability and implementation in primary care. Gen Hosp Psychiatry. 2021;71:102–107. doi: 10.1016/j.genhosppsych.2021.03.009. [DOI] [PubMed] [Google Scholar]
- 21.Samuels S, Abrams R, Shengelia R, et al. Integration of geriatric mental health screening into a primary care practice: a patient satisfaction survey. Int J Geriatr Psychiatry. 2015;30(5):539–546. doi: 10.1002/gps.4180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zimmerman M, Farber NJ, Hartung J, Lush DT, Kuzma MA. Screening for psychiatric disorders in medical patients: a feasibility and patient acceptance study. Med Care. 1994:603–608. [DOI] [PubMed]
- 23.Lish JD, Kuzma MA, Lush DT, Plescia G, Farber NJ, Zimmerman M. Psychiatric screening in primary care: what do patients really want? J Psychosom Res. 1997;42(2):167–175. doi: 10.1016/S0022-3999(96)00235-8. [DOI] [PubMed] [Google Scholar]
- 24.McCarthy JF, Cooper SA, Dent KR, et al. Evaluation of the recovery engagement and coordination for health–veterans enhanced treatment suicide risk modeling clinical program in the veterans health administration. JAMA Netw Open. 2021;4(10):e2129900–e2129900. doi: 10.1001/jamanetworkopen.2021.29900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gordon JA, Avenevoli S, Pearson JL. Suicide prevention research priorities in health care. JAMA Psychiatry. 2020;77(9):885–886. doi: 10.1001/jamapsychiatry.2020.1042. [DOI] [PubMed] [Google Scholar]
- 26.Kessler RC, Barker PR, Colpe LJ, et al. Screening for serious mental illness in the general population. Arch Gen Psychiatry. 2003;60(2):184–189. doi: 10.1001/archpsyc.60.2.184. [DOI] [PubMed] [Google Scholar]
- 27.Vogt D, Taverna E, Nillni Y, Tyrell F. Manual for the well-being inventory (WBI): a multidimensional tool for assessing key components of well-being. Boston, MA: National center for PTSD; 2018. [Google Scholar]
- 28.Lumley T. Complex surveys: a guide to analysis using R. Hoboken, NJ: John Wiley & Sons; 2010. [Google Scholar]
- 29.Lumley T. Package ‘survey’: analysis of complex survey samples, version 4.0. 2020.
- 30.R Core Team. R: A language and environment for statistical computing. 2018.
- 31.Thomas DR, Rao J. Small-sample comparisons of level and power for simple goodness-of-fit statistics under cluster sampling. J Am Stat Assoc. 1987;82(398):630–636. doi: 10.1080/01621459.1987.10478476. [DOI] [Google Scholar]
- 32.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 33.Dobscha SK, Newell SB, Elliot VJ, et al. Primary care and mental health staff perspectives on universal suicide risk screening and care coordination. Psychiatric Services. 10.1176/appi.ps.20220087. [DOI] [PubMed]
- 34.Etter DJ, McCord A, Ouyang F, et al. Suicide screening in primary care: use of an electronic screener to assess suicidality and improve provider follow-up for adolescents. J Adolesc Health. 2018;62(2):191–197. doi: 10.1016/j.jadohealth.2017.08.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are not available due to institutional regulations.