Abstract
OBJECTIVE
To study the relationships between artificial sweeteners, accounting for all dietary sources (total and by type of artificial sweetener) and risk of type 2 diabetes (T2D), in a large-scale prospective cohort.
RESEARCH DESIGN AND METHODS
The analyses included 105,588 participants from the web-based NutriNet-Santé study (France, 2009–2022; mean age 42.5 ± 14.6 years, 79.2% women). Repeated 24-h dietary records, including brands and commercial names of industrial products, merged with qualitative and quantitative food additive composition data, enabled artificial sweetener intakes to be accurately assessed from all dietary sources. Associations between artificial sweeteners (total, aspartame, acesulfame potassium [K], and sucralose) and T2D were investigated using Cox proportional hazard models adjusted for potential confounders, including weight variation during follow-up.
RESULTS
During a median follow-up of 9.1 years (946,650 person-years, 972 incident T2D), compared with nonconsumers, higher consumers of artificial sweeteners (i.e., above the sex-specific medians of 16.4 mg/day in men and 18.5 mg/day in women) had higher risks of developing T2D (hazard ratio [HR] 1.69; 95% CI 1.45–1.97; P-trend <0.001). Positive associations were also observed for individual artificial sweeteners: aspartame (HR 1.63 [95% CI 1.38–1.93], P-trend <0.001), acesulfame-K (HR 1.70 [1.42–2.04], P-trend <0.001), and sucralose (HR 1.34 [1.07–1.69], P-trend = 0.013).
CONCLUSIONS
Potential for reverse causality cannot be eliminated; however, many sensitivity analyses were computed to limit this and other potential biases. These findings of positive associations between artificial sweetener intakes and increased T2D risk strengthen the evidence that these additives may not be safe sugar alternatives. This study provides important insights in the context of on-going reevaluation of artificial sweeteners by health authorities worldwide.
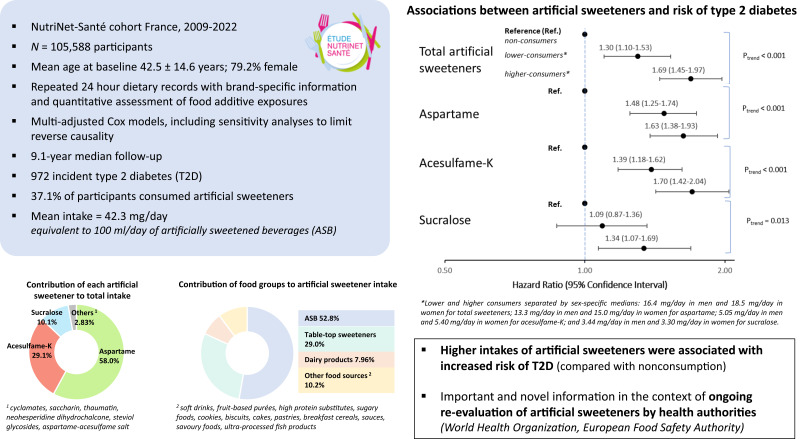
Graphical Abstract
Introduction
Dietary sugars are associated with various health issues, including overweight, obesity, cardiovascular diseases (CVDs), and type 2 diabetes (T2D) (1). Manufacturers have proposed alternatives to reduce added sugars, notably by substituting artificial sweeteners (e.g., aspartame, acesulfame potassium [K], and sucralose) for them. Health-conscious consumers might also shift to artificial sweeteners (1). Those food additives have high sweetening power and low/zero calorie content. They are used in ultraprocessed foods (UPFs), such as artificially sweetened beverages (ASBs) or table-top sweeteners directly added by consumers. One standard can of an ASB (330 mL) contains ∼130 mg of artificial sweeteners (2) and provides 4.3 kcal/standard can versus 138 kcal for a sugar-sweetened version (3).
Artificial sweeteners are present in thousands of products and consumed by millions of individuals. Nonetheless, a growing body of experimental and epidemiological literature suggests they might not be as harmless as expected. Previous findings from the NutriNet-Santé cohort identified positive associations between artificial sweeteners and risk of breast-/obesity-related cancers and CVD (4). The World Health Organization (WHO) recently published a systematic review and meta-analysis of artificial sweeteners-health relationships, based on randomized controlled trials (RCT), prospective, and case-control studies (5). They suggested associations with obesity, CVD, and mortality and identified positive associations with T2D; however, the level of certainty was considered low (5).
T2D represents a major public health issue: 6.3% of the world’s adult population was affected in 2017, and numbers are expected to rise to 7.4% by 2040 (6). T2D is frequently associated with comorbidities of high blood pressure, dyslipidemia, and incidence of cardiovascular events, among others, for which diet is a recognized prevention tool. Artificial sweeteners are notably a marker of UPFs, which have been shown to be associated with T2D (7).
To our knowledge, in previous prospective studies, detailed information on commercial brands and product names was lacking; thus, overall quantitative evaluation of artificial sweetener intakes was not possible. Some studies have nonetheless examined the relationship between ASBs and T2D, and two have investigated the associations with table-top sweeteners (5). Several RCTs have explored the impact of artificial sweeteners versus sugars, sugar-sweetened foods/beverages, or water, on intermediate markers such as blood glucose, glycated hemoglobin, insulin levels, and insulin resistance, with inconclusive results (5), but none have directly investigated T2D risk.
In this context, our objective was to study the associations between artificial sweeteners (i.e., aspartame, acesulfame-K, and sucralose), accounting for all dietary sources for the first time (total and by molecules) and T2D risk, within the NutriNet-Santé cohort.
Research Design and Methods
Study Population and Data Collection
This study was based on the French large-scale population-based NutriNet-Santé prospective cohort, launched in 2009 with the aim of investigating nutrition-health relationships (8). Participants are recruited from the general adult population with Internet access. They are followed using a personal account on the study website (https://etude-nutrinet-sante.fr/), through which they provide detailed information by answering multiple questionnaires. A five-questionnaire inclusion kit collects sociodemographic/lifestyle data (e.g., sex, birthdate, education, and smoking) (9), anthropometry (height and weight) (10,11), health status (e.g., personal and family medical history, prevalence and incidence of diseases, and medical treatments), physical activity level (7-day assessment via the validated International Physical Activity Questionnaire [IPAQ]) (12), and dietary habits (three nonconsecutive 24-h dietary records).
Ethical considerations and authorizations are presented in Supplementary Method 1.
Dietary Assessment
At inclusion and every 6 months thereafter, participants fill out three nonconsecutive 24-h dietary records, randomly assigned over a 2-week period, including 2 weekdays and 1 weekend day (to account for variability in the diet across the week). During those recording days, participants use a dedicated interactive web interface to declare all foods and beverages consumed during the three main meals and any other eating occasion. Using validated portion size photographs and standard containers (13), participants declare quantities consumed for each food/beverage; they can also directly enter the amount (g or mL). For industrial products, participants provide the commercial name and brand. Energy and nutrient intakes are computed using the NutriNet-Santé composition table containing ∼3,500 generic food/beverage items and mixed dishes for which standard French recipes have been defined by nutrition professionals (14). These 24-h web-based dietary records have been validated against interview by a trained dietitian (15) and blood/urinary biomarkers (16,17). Energy underreporters were identified using the basal metabolic rate and the Goldberg cutoff method (18,19) and were excluded from the analyses (additional information available in Supplementary Method 2). Baseline individual dietary intakes were averaged from all 24-h records completed during the first 2 years of follow-up. This represents a reliable estimate of consumption habits, while respective prospective design and guaranteeing sufficient delay between consumption and T2D diagnosis.
Artificial Sweetener Intakes
Detailed estimation of food additive exposure, including artificial sweeteners, was obtained through qualitative and quantitative data collection and analyses. Evaluation of food additive exposure has been extensively described elsewhere (20). For each product declared through 24-h dietary records, qualitative composition of the food additives was determined, using three large-scale prospective databases: French food safety agency database Oqali (https://www.oqali.fr/oqali_eng/) (21), Open Food Facts (https://world.openfoodfacts.org/) (22), and Mintel’s Global New Products Database (GNPD) (23). Food additive quantities were then determined by dosages (∼2,700 assays) performed by accredited laboratories and completed with average doses provided by international health authorities: the European Food Safety Authority (EFSA) (24) and the Joint Food and Agriculture Organization (FAO)/WHO Expert Committee on Food Additives (JECFA) (25). Additional information on the evaluation of food additive exposure is available in Supplementary Method 3.
This methodology enabled the assessment of intakes of the following food additive sweeteners: aspartame (European Union food additive identification number: E951), acesulfame-K (E950), sucralose (E955), cyclamates (E952), saccharin (E954), thaumatin (E957), neohesperidine dihydrochalcone (E959), steviol glycosides (E960), and salt of aspartame-acesulfame-K (E962). A “total artificial sweeteners (mg/day)” variable was computed by summing all intakes.
T2D Ascertainment
T2D was assessed using a multisource approach (Supplementary Method 4). Throughout follow-up, participants could report health events, medical treatments, and examinations via biannual health questionnaires or at any time directly via their personal health interface. Besides, linkage of the NutriNet-Santé cohort with the national health insurance system database (Système National d’Information Inter Régimes de l’Assurance Maladie [SNIIRAM]) was performed to collect supplemental information regarding medical treatments/consultations. Linkage to the French national mortality registry (CépiDC) was performed to identify mortality cases.
Statistical Analyses
NutriNet-Santé participants selected for the analyses were those with at least two valid 24-h dietary records at baseline, not underenergy reporters, and with no prevalent type 2 or type 1 diabetes (flowchart of participant selection is presented in Supplementary Fig. 1).
For each artificial sweetener, participants were categorized into three groups: nonconsumers, lower consumers, and higher consumers (sex-specific medians separating the latter two categories). Baseline characteristics were assessed for the overall population and by category of total artificial sweetener intake and compared using χ2 and ANOVA tests for categorical and continuous variables, respectively.
Cox proportional hazard models were computed to study the associations of T2D with total artificial sweeteners and specific artificial sweetener molecules consumed by at least 10% of the study population to ensure sufficient statistical power (i.e., aspartame, acesulfame-K, and sucralose; all others were consumed by <3.5%). Participants contributed person-time until T2D diagnosis, last completed questionnaire, death, or 26 April 2022, whichever occurred first. The three-category model (nonconsumers, lower consumers, and higher consumers, separated by sex-specific medians) was used as the primary analysis to obtain hazard ratios (HRs) and 95% CIs for lower consumers and higher consumers compared with nonconsumers. P for trend was obtained using the ordinal score across each category. Dose-response analyses were also plotted using the restricted cubic spline function with the SAS macro developed by Desquilbet and Mariotti (26), and associations of T2D risk with artificial sweeteners coded as continuous variables were computed. The Cox proportional hazard assumption was verified using the rescaled Schoenfeld-type residual method.
The main model was adjusted for variables suspected or known to be associated with diet and with T2D. These variables pertained to the following domains: sociodemographic (age, sex, and education), lifestyle (baseline physical activity, smoking status, and number of smoked cigarettes), health (family history of diabetes in first-degree relatives and prevalence of CVD, hypertension, or dyslipidemia), number of 24-h dietary records, and weight status (baseline BMI and mean percentage of weight change per year of follow-up [calculated as the difference between end of follow-up weight and baseline-weight divided by baseline-weight, multiplied by 100 and divided by follow-up time]). This variable was chosen for adjustment in the main models since it provided an overview of the weight trajectory across follow-up, to limit potential confounding or reverse causality associated with this key factor. The main model was also adjusted for food groups and nutrients for which a role in T2D etiology has been strongly suggested (27): energy intake without alcohol and daily intakes of alcohol, sugar, sodium, saturated fatty acids, fiber, fruit, vegetables, red/processed meat, and dairy products. Analyses by specific artificial sweeteners (i.e., aspartame, acesulfame-K, and sucralose) were additionally adjusted for other artificial sweetener intakes. Unless stated otherwise, covariables were measured at baseline. Coding for covariates is provided in Supplementary Method 5.
Two additional models were computed to challenge reverse causality, which may be particularly sensitive in this type of study: first, by excluding participants with T2D incidence occurring during the first 6 years of follow-up (subpopulation 1), and second, by further excluding participants with family history of diabetes or prevalence of hypertension, dyslipidemia, or CVD (subpopulation 2) to account for early signs of T2D risk that could have led individuals to replace added sugars with artificial sweeteners. On this latter model, substitution analyses were performed between artificial sweetener and sugar intakes to test whether there could be a benefit of replacing sugars with artificial sweeteners to lower T2D risk. Substitution analyses were performed by including artificial sweetener (converted to a sugar equivalent using sweetening power, ensuring similar order of magnitude) and sugar intakes in the same model. HRs and 95% CIs were estimated using the difference in coefficients obtained from this model. Formal interactions between artificial sweeteners and added sugar intake (by tertile), weight status (BMI <25 or ≥25 kg/m2), and sex (men/women) were tested by entering the product of the two variables into Cox models. Associations between artificial sweeteners and T2D were then computed in each tertile of added sugar intake among nonoverweight and overweight participants and among female and male participants, distinctively.
Other supplementary models tested further adjustments for weight-loss dieting during first 2 years of follow-up, proportion of UPFs, “healthy”/“Western” dietary patterns (derived by principal components analysis, accounting for overall diet quality), a priori dietary score reflecting the level of compliance with the French nutritional recommendations (modified Program National Nutrition Santé Guidelines Score [mPNNS-GS]) (28), total energy intake instead of energy without alcohol, and caffeine intake. Models excluding participants with less than four 24-h dietary records, not adjusting for BMI, additionally adjusting for absolute weight change during follow-up, and adjusting for time-dependent BMI instead of baseline BMI were tested. Analyses based on time-dependent artificial sweetener intakes across the whole follow-up period were also tested. In these models, artificial sweetener intake was estimated for each participant for each year of follow-up so that the exposure variable was updated yearly in Cox models to account for all data collected during follow-up.
Missing values were handled with the multiple imputation by chained equations method (15 imputed data sets) (29) for the following covariates: smoking status (0.07% of missing data), level of education (0.85%), physical activity (13.9%), BMI (1.94%), and family history of diabetes (1.13%).
All tests were two-sided, and P < 0.05 was considered statistically significant. The statistical analysis software SAS 9.4 was used for analyses.
Patient Involvement
The research question developed in this article corresponds to a concern expressed by some participants involved in the NutriNet-Santé cohort and of the public in general. Participants in the study are thanked in the Acknowledgments section. The results of the present study will be disseminated to the NutriNet-Santé participants through the cohort website, public seminars, and a press release.
Data and Resource Availability
Researchers from public institutions can submit a collaboration request including information about the institution and a brief description of the project to collaboration@etude-nutrinet-sante.fr. All requests will be reviewed by the steering committee of the NutriNet-Santé study. If the collaboration is accepted, a data access agreement will be necessary, and appropriate authorizations from the competent administrative authorities may be needed. In accordance with existing regulations, no personal data will be accessible.
Results
Descriptive Characteristics
The study sample included 105,588 participants (79.2% women) from the NutriNet-Santé cohort (Supplementary Fig. 1), among which 37.1% were artificial sweetener consumers. Mean intake of artificial sweeteners among consumers was 42.3 ± 72.1 mg/day. This is roughly equivalent to consuming 100 mL/day of an ASB (i.e., approximately one-third of a 330 mL can of soda) (2). Intakes among lower and higher consumers, separated by sex-specific medians among consumers, were 7.40 ± 4.90 and 77.2 ± 88.9 mg/day, respectively. Aspartame, acesulfame-K, and sucralose were consumed by 28.1, 34.5, and 13.9% of the study population, respectively (coconsumption of each artificial sweetener presented in Supplementary Fig. 2). Compared with nonconsumers, higher consumers were more likely to be women, younger, current/former smokers, with higher BMI, and lower physical activity level. They had lower intakes of energy, alcohol, saturated fatty acids, and fiber-containing foods, and consumed more sodium, sugary drinks, unsweetened nonalcoholic drinks, red/processed meats, dairy products, and UPFs. They were also more likely to follow a weight-loss diet (Table 1). Aspartame, acesulfame-K, and sucralose contributed to 97.2% of total artificial sweeteners (58.0, 29.1, and 10.1%, respectively). ASBs, table-top sweeteners, and artificially sweetened dairy products contributed to 52.8, 29.0, and 7.96% of artificial sweetener intakes, respectively. Table-top sweeteners were the main aspartame contributor, whereas ASBs were the main contributors to acesulfame-K and sucralose at baseline (Supplementary Fig. 3). Relative contribution of food groups over time is presented in the Supplementary Results and Supplementary Table 1.
Table 1.
Baseline characteristics of the study population, NutriNet-Santé cohort, France, 2009–2022
| All participants | Categories of artificial sweetener intakes1 | ||||
|---|---|---|---|---|---|
| Nonconsumers | Lower consumers | Higher consumers | P value2 | ||
| Characteristics | N = 105,588 | n = 66,376 | n = 19,569 | n = 19,643 | <0.001 |
| Age, years (mean [SD]) | 42.5 (14.6) | 43.3 (14.8) | 42.3 (14.6) | 40.3 (13.6) | <0.001 |
| Female sex | 83,628 (79.2) | 50,826 (76.6) | 16,367 (83.6) | 16,435 (83.7) | <0.001 |
| Follow-up time, years (mean [SD]) | 8.97 (2.33) | 8.84 (2.35) | 9.30 (2.31) | 9.04 (2.23) | <0.001 |
| Number of 24-h dietary records (mean [SD]) | 5.61 (3.06) | 5.33 (3.02) | 6.84 (3.10) | 5.30 (2.84) | <0.001 |
| BMI, kg/m2 (mean [SD]) | 23.6 (4.33) | 23.3 (4.06) | 23.7 (4.29) | 24.8 (4.97) | <0.001 |
| Weight gain during follow-up, % by year (mean [SD]) | 0.15 (2.87) | 0.11 (2.23) | 0.21 (3.11) | 0.22 (4.22) | <0.001 |
| Family history of diabetes | 14,567 (13.8) | 8,800 (13.3) | 2,689 (13.7) | 3,078 (15.7) | <0.001 |
| Prevalent dyslipidemia | 8,976 (8.50) | 5,261 (7.93) | 1,900 (9.71) | 1,815 (9.24) | <0.001 |
| Prevalent hypertension | 7,974 (7.55) | 4,802 (7.23) | 1,597 (8.16) | 1,575 (8.02) | <0.001 |
| Educational level | <0.001 | ||||
| No higher education | 17,311 (16.4) | 11,214 (16.9) | 3,055 (15.6) | 3,042 (15.5) | |
| Higher education, <2 years | 16,615 (15.7) | 10,521 (15.9) | 2,954 (15.1) | 3,140 (16.0) | |
| Higher education, ≥2 years | 71,662 (67.9) | 44,641 (67.3) | 13,560 (69.3) | 13,461 (68.5) | |
| Smoking status | <0.001 | ||||
| Current | 15,148 (14.4) | 9,549 (14.4) | 2,310 (11.8) | 3,289 (16.7) | |
| Former | 42,606 (40.4) | 26,322 (39.7) | 8,127 (41.5) | 8,157 (41.5) | |
| Never | 47,834 (45.3) | 30,505 (46.0) | 9,132 (46.7) | 8,197 (41.7) | |
| Number of smoked cigarettes, pack-years (mean [SD])3 | 5.26 (11.0) | 5.16 (10.9) | 4.82 (10.3) | 6.06 (12.0) | <0.001 |
| Physical activity level4 | <0.001 | ||||
| Low | 22,229 (21.1) | 13,614 (20.5) | 4,225 (21.6) | 4,390 (22.4) | |
| Moderate | 39,119 (37.1) | 24,366 (36.7) | 7,557 (38.6) | 7,196 (36.6) | |
| High | 29,656 (28.1) | 19,322 (29.1) | 5,192 (26.5) | 5,142 (26.2) | |
| Energy intake without alcohol, kcal/day (mean [SD]) | 1,900 (470) | 1,910 (478) | 1,890 (433) | 1,860 (478) | <0.001 |
| Alcohol intake, g/day (mean [SD]) | 7.80 (11.8) | 8.13 (12.3) | 7.61 (10.9) | 6.85 (10.9) | <0.001 |
| Saturated fatty acid intakes, g/day (mean [SD]) | 33.2 (12.1) | 33.6 (12.3) | 33.1 (11.2) | 31.8 (12.4) | <0.001 |
| Sodium intake, mg/day (mean [SD]) | 2,710 (883) | 2,700 (899) | 2,720 (815) | 2,730 (894) | <0.001 |
| Dietary fiber intake, g/day (mean [SD]) | 19.4 (7.20) | 19.8 (7.48) | 19.0 (6.28) | 18.7 (7.01) | <0.001 |
| Total sugar intake, g/day (mean [SD]) | 92.6 (33.1) | 92.1 (33.5) | 94.6 (30.6) | 92.7 (34.2) | <0.001 |
| Added sugar intake, g/day (mean [SD]) | 38.7 (23.7) | 38.4 (23.5) | 40.2 (22.5) | 38.0 (25.5) | <0.001 |
| Energy from added sugar, % (mean [SD]) | 7.98 (4.15) | 7.90 (4.12) | 8.34 (3.93) | 7.91 (4.41) | <0.001 |
| Sugary drinks, mL/day (mean [SD]) | 47.5 (106) | 42.4 (103) | 54.8 (97.6) | 57.5 (123) | <0.001 |
| Unsweetened nonalcoholic drinks, mL/day (mean [SD]) | 1,090 (536) | 1,060 (529) | 1,090 (517) | 1,170 (571) | <0.001 |
| Fruit and vegetable intake, g/day (mean [SD]) | 406 (220) | 410 (223) | 399 (197) | 398 (232) | <0.001 |
| Whole-grain food intake, g/day (mean [SD]) | 34.3 (46.1) | 35.8 (49.3) | 31.5 (38.7) | 31.7 (41.5) | <0.001 |
| Red and processed meat intake, g/day (mean [SD]) | 76.6 (52.7) | 74.7 (53.3) | 76.2 (46.8) | 83.3 (55.9) | <0.001 |
| Dairy product intake, g/day (mean [SD]) | 197 (148) | 185 (145) | 203 (138) | 234 (163) | <0.001 |
| UPF intake, % of the diet in g/day (mean [SD]) | 17.4 (9.89) | 15.9 (9.11) | 17.4 (8.59) | 22.2 (11.9) | <0.001 |
| Weight-loss diet during the first 2 years of follow-up | 18,002 (17.1) | 7,939 (12.0) | 3,710 (19.0) | 6,353 (32.3) | <0.001 |
| Artificial sweetener intake, mg/day (mean [SD]) | 15.7 (48.4) | 0 (0) | 7.40 (4.90) | 77.2 (88.9) | <0.001 |
| Aspartame (E 951) intake, mg/day (mean [SD]) | 9.11 (30.9) | 0 (0) | 3.13 (3.94) | 45.9 (58.6) | <0.001 |
| Acesulfame-K (E 950) intake, mg/day (mean [SD]) | 4.58 (14.9) | 0 (0) | 2.68 (2.76) | 22.0 (28.4) | <0.001 |
| Sucralose (E 955) intake, mg/day (mean [SD]) | 1.59 (16.1) | 0 (0) | 1.08 (1.95) | 7.44 (36.7) | <0.001 |
Values are n (%) unless stated otherwise. 1 kcal = 4.18 kJ = 0.00418 MJ.
Categories of consumption were defined as nonconsumers, lower consumers, and higher consumers separated by the sex-specific median among consumers of 16.4 mg/day in men and 18.5 mg/day in women.
P values for crude comparison between the three categories of sweetener intake by ANOVA or χ2 test where appropriate.
In current or former smokers.
Available for 91,004 participants, categorized into high, moderate, and low categories according to IPAQ guidelines.
Associations Between Artificial Sweetener Intakes and T2D
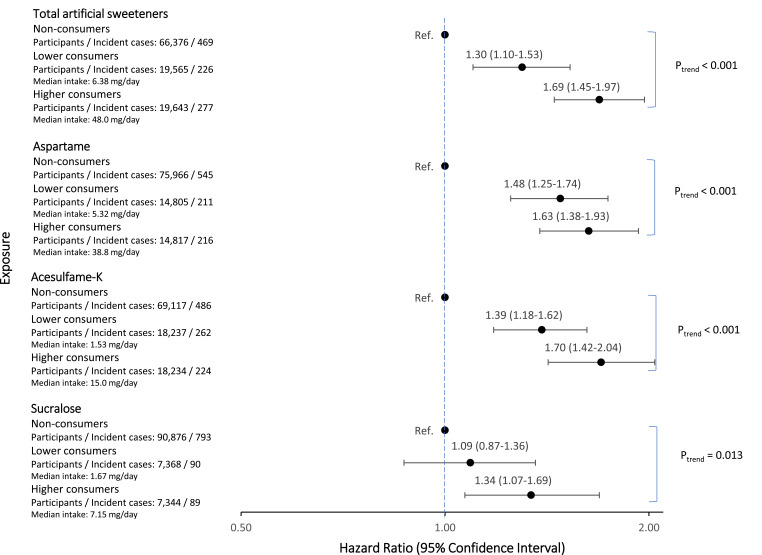
Median follow-up time was 9.13 years (interquartile range 7.63–10.63), for a total follow-up of 946,650 person-years. There were 972 participants diagnosed with T2D after their inclusion in the cohort, at the average age of 59.2 ± 11.4 years. Compared with nonconsumers, higher consumers of artificial sweeteners had higher T2D risk (HR 1.69 [95% CI 1.45–1.97] P-trend <0.001) (Fig. 1). Similarly, positive associations were found for aspartame (HR 1.63 [1.38–1.93] P-trend <0.001), acesulfame-K (HR 1.70 [1.42–2.04], P-trend <0.001), and sucralose (HR 1.34 [1.07–1.69], P-trend = 0.013). Results were similar when artificial sweetener exposures were coded as continuous variables (Table 2), except for sucralose, for which the association was weakened (HRfor 100 mg/day increase 1.06 [0.78–1.43]).
Figure 1.
Association between total artificial sweeteners, aspartame, acesulfame-K, and sucralose intakes and T2D risk, NutriNet-Santé cohort, France, 2009-2022 (N = 105,588). Median follow-up time was 9.13 years (946,650 person-years). Multivariable Cox proportional hazard models were adjusted for (main model) age (time scale), sex, BMI (continuous, kg/m2), mean percentage of weight change per year of follow-up (continuous), physical activity (categorical IPAQ variable: high, moderate, low, missing value), smoking status (categorical: never, former, current smokers), number of smoked cigarettes in pack-years (continuous), educational level (categorical: less than high school degree, <2 years after high school degree, ≥2 years after high school degree), family history of diabetes in first-degree relatives (categorical: yes, no), prevalence of cardiovascular disease (categorical: yes, no), prevalence of hypertension (categorical: yes, no), prevalence of dyslipidemia (categorical: yes, no), number of 24-h dietary records (continuous), energy intake without alcohol (continuous variable: kcal/day), daily intakes (continuous, g/day) of alcohol, sodium, saturated fatty acids, fiber, sugar, fruit and vegetables, red and processed meat, and dairy products. In addition, all models were mutually adjusted for artificial sweetener intake other than the one studied. Sex specific cutoffs among consumers were 16.4 mg/day in men and 18.5 mg/day in women for total artificial sweeteners, 13.3 mg/day in men and 15.0 mg/day in women for aspartame, 5.05 mg/day in men and 5.40 mg/day in women for acesulfame-K, and 3.44 mg/day in men and 3.30 mg/day in women for sucralose.
Table 2.
Association between total artificial sweeteners, aspartame, acesulfame-K, and sucralose intakes coded as continuous variables and T2D, NutriNet-Santé cohort, France, 2009–2022 (N = 105,588 participants; 972 incident cases)1
| Exposure | HR for an increase of 100 mg/day (95% CI) | P value |
|---|---|---|
| Total artificial sweeteners | 1.18 (1.09–1.29) | <0.001 |
| Aspartame | 1.26 (1.08–1.46) | 0.003 |
| Acesulfame-K | 1.62 (1.12–2.33) | 0.010 |
| Sucralose | 1.06 (0.78–1.43) | 0.713 |
Median follow-up time was 9.13 years (946,650 person-years). Multivariable Cox proportional hazard models were adjusted for (main model) age (time scale), sex, BMI (continuous, kg/m2), mean percentage of weight change per year of follow-up (continuous), physical activity (categorical IPAQ variable: high, moderate, low, missing value), smoking status (categorical: never, former, current smokers), number of smoked cigarettes in pack-years (continuous), educational level (categorical: less than high school degree, <2 years after high school degree, ≥2 years after high school degree), family history of diabetes in first-degree relatives (categorical: yes, no), prevalence of cardiovascular disease (categorical: yes, no), prevalence of hypertension (categorical: yes, no), prevalence of dyslipidemia (categorical: yes, no), number of 24-h dietary records (continuous), energy intake without alcohol (continuous variable: kcal/day), daily intakes (continuous, g/day) of alcohol, sodium, saturated fatty acids, fiber, sugar, fruit and vegetables, red and processed meat, and dairy products. In addition, all models were mutually adjusted for artificial sweetener intake other than the one studied.
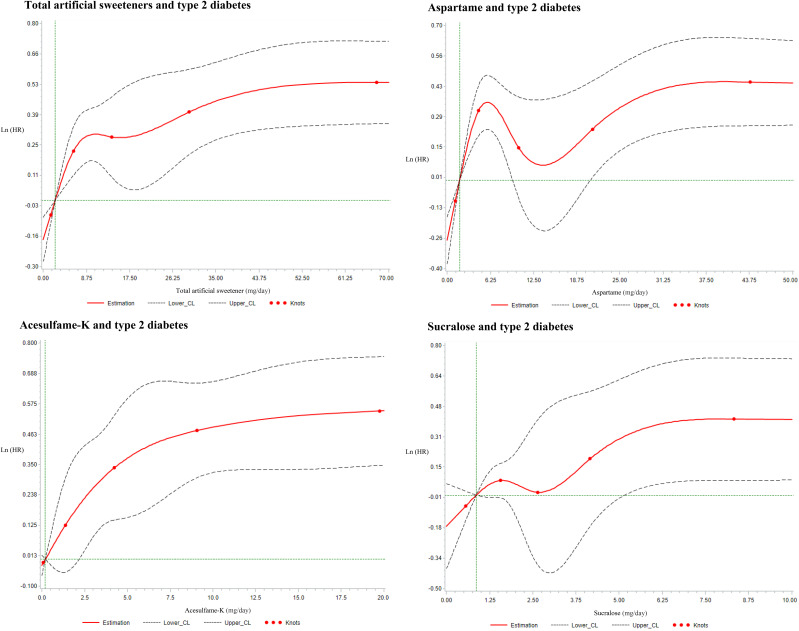
The comparison of the model with three categories versus the model with a linear trend across categories did not provide evidence of nonlinearity (total artificial sweeteners, P = 0.975; aspartame, P = 0.086; acesulfame-K, P = 0.389; and sucralose, P = 0.577). Assumptions of the Cox models were met: dose-response analyses were plotted (Fig. 2), and the proportional hazard assumption was verified (Supplementary Fig. 4).
Figure 2.
Dose-response associations between artificial sweetener intakes and T2D, NutriNet-Santé, France, 2009-2022 (N =105,588). Median follow-up time was 9.13 years (946,650 person-years). Multivariable Cox proportional hazard models were adjusted for (main model) age (time scale), sex, BMI (continuous, kg/m2), mean percentage of weight-change per year of follow-up (continuous), physical activity (categorical IPAQ variable: high, moderate, low, missing value), smoking status (categorical: never, former, current smokers), number of smoked cigarettes in pack-years (continuous), educational level (categorical: less than high school degree, <2 years after high school degree, ≥2 years after high school degree), family history of diabetes in first-degree relatives (categorical: yes, no), prevalence of cardiovascular disease (categorical: yes, no), prevalence of hypertension (categorical: yes, no), prevalence of dyslipidemia (categorical: yes, no), number of 24h dietary records (continuous), energy intake without alcohol (continuous variable: kcal/day), daily intakes (continuous, g/day) of alcohol, sodium, saturated fatty acids, fiber, sugar, fruits and vegetables, red and processed meat, and dairy products. In addition, all models were mutually adjusted for artificial sweetener intake other than the one studied. Restricted cubic splines functions with the SAS macro were developed by Desquilbet and Mariotti (1).
Exclusion of participants with T2D incidence occurring during the first 6 years of follow-up (104,906 participants and 290 cases) or excluding participants with cardiometabolic T2D risk factors (78,455 participants and 109 cases) to challenge reverse causality bias did not substantially modify the findings (Supplementary Table 2), although associations became nonsignificant for acesulfame-K and sucralose. However, in the later model, the statistical power was strongly reduced (e.g., only nine cases in the higher-consumers category for sucralose). Substitution analyses suggest no beneficial effect of replacing sugars by artificial sweeteners regarding T2D risk (HRfor substitution 1.13 [95% CI 0.98–1.29]). No interaction on the multiplicative scale was detected between artificial sweetener intake and weight status (P = 0.943) or sex (P = 0.145), showing similar associations with T2D risk in each subgroup (Supplementary Table 3). Although significant interaction was observed between artificial sweetener and added sugar intakes (P < 0.001), positive associations between artificial sweetener and T2D risk were consistently observed in each tertile of added sugar (Supplementary Table 3).
Lastly, further adjustments for weight-loss dieting, UPFs, dietary patterns, modified Programme National Nutrition Santé Guidelines Score (mPPNS-GS), absolute weight change, time-dependent BMI, total energy intake, and with time-dependent artificial sweeteners provided similar associations, showing the robustness of the results (Supplementary Table 4).
Conclusions
Main Findings
In this large-scale population-based cohort of 105,588 French adults, artificial sweetener intakes were associated with higher risk of T2D. More specifically, positive associations were observed for total sweeteners, aspartame, acesulfame-K, and sucralose. Sensitivity analyses (challenging reverse causality, stratifying by added sugar intake and overweight status, and testing further adjustments) provided similar results, although with a loss of significance for sucralose in some subgroups.
Comparison With Epidemiological Literature
To the best of our knowledge, our cohort study is the first to have quantified artificial sweetener intake from the overall diet. So far, cohort studies investigating incident T2D in relation to artificial sweetener exposure only used proxies, which were either ASBs or table-top sweeteners considered separately as presented in the recent WHO systematic review and meta-analysis (5). The detailed list of references included in this report and discussed thereafter regarding ASBs/artificial sweeteners and T2D risk is provided in Supplementary Table 5. Results from these studies were contrasted. A study based on the European Prospective Investigation into Cancer and Nutrition (EPIC) cohort suggested that a one-can increase of an ASB per day was associated with higher T2D risk; however, after adjustment for BMI, the association became nonsignificant. Similarly, in the EPIC-Norfolk, Health Professionals Follow-Up Study (HPFS), and Black Women’s Health Study (BWHS) cohorts, nonsignificant associations were found between ASBs and T2D after adjusting for BMI. In contrast, later studies identified positive associations among women in the Nurses’ Health Study (NHS) and NHS II between ASB intake and higher T2D risk when analyses were adjusted for BMI. Results from another American cohort suggested a significant association between daily consumption of ASBs and a higher risk of incident T2D compared with nonconsumers, independent of adiposity. Associations between ASBs and T2D risk were also found in a cohort of Japanese men, after adjustment for BMI. In the Women’s Health Initiative (WHI), the associations were also positive for higher consumers (≥2 servings/day) compared with lower consumers (never or <3 servings/month). Similarly, the French E3N (Etude Epidémiologique auprès de femmes de la Mutuelle Générale de l’Education Nationale) study (>66,000 women) suggested an association between ASBs and risk of diabetes for higher consumers (>603 mL/week) compared with nonconsumers, and the associations, although slightly attenuated, remained significant after adjustment for BMI. In the same cohort, it was also suggested that usual sweetener intake in the form of table-top sweeteners (sachets or tablets) was also associated with T2D risk. Jensen et al. (30) tested a research question very similar to the present study. The authors considered intakes of both table-top sweeteners and ASBs and investigated their associations with incident diabetes and early markers of insulin and glucose homeostasis. No significant associations were observed for fasting insulin and glucose analyses. However, in line with results from the present study, consumers of ASBs and table-top sweeteners had higher risks of diabetes compared with nonconsumers.
Findings from these prospective studies have been subjected to several reviews and meta-analyses (5,31,32). The meta-analysis by Azad et al. (31), involving nine cohorts and >400,000 participants, showed a positive association (risk ratio 1.14 [95% CI 1.05–1.25]) for highest versus lowest ASB intake. Qin et al. (32) also identified a direct association between ASBs and T2D (relative risk 1.15 [1.05–1.26]). The latest was the systematic review and meta-analysis from the WHO (5) in 2022, which identified higher T2D incidence in relation with ASB (HR 1.23 [1.14–1.32]) and table-top sweetener (HR 1.34 [1.21–1.48]) consumption. Overall, results from prospective studies observed higher risk of T2D, even after adjusting for BMI status in most cohorts, but associations were lost in models additionally adjusted for BMI in some studies (5). Lastly, regarding RCTs, according to the recent WHO review (5), 21 have studied intermediate factors, such as fasting glucose (16 RCTs), fasting insulin (10 RCTs), glycated hemoglobin (6 RCTs), and insulin resistance (11 RCTs), with inconsistent findings. Results of a recent meta-analysis revealed no significant associations (5). To our knowledge, no RCT has previously specifically investigated the impact on T2D risk (hard end point), probably due to ethical reasons since potential adverse effects are suspected.
Mechanistic Plausibility
Results from the cross-sectional Maastricht Study, including 2,240 participants, suggested that ASB consumption could be associated with disturbances in glucose metabolism, with decreased β-cell sensitivity and lower insulin secretion (33). Artificial sweeteners, including acesulfame-K and sucralose, may also be involved in increased adipogenesis and reduced lipolysis, as suggested by experimental studies in vitro (34). In fact, artificial sweetener consumption could promote a pro-oxidant environment and influence fat-based stem cells differentiation (35). Additionally, Suez et al. (35) suggested that disturbances from artificial sweeteners could include alterations in the gut microbiota, in mice and healthy human subjects, which could then be involved in the etiology of T2D (36). In fact, a recent RCT in healthy adults suggested person-specific effects of artificial sweeteners on the microbiome inducing elevated glycemic responses (35). The authors notably observed specific microbial features in relation with artificial sweetener intake, such as increased levels kynurenine, a diabetes-specific metabolite, during aspartame consumption or overrepresentation of biosynthetic pathways associated with T2D (35). Additionally, the WHO identified positive associations in three cohort studies between artificial sweeteners and high fasting blood glucose, which contributes to metabolic syndrome and, as a prediabetes condition, can translate to T2D (5). Nonetheless, the effects of artificial sweeteners on glucose metabolism remain unclear (37), and further experimental studies are needed to clarify the underlying mechanisms.
Strengths and Limitations
Strengths of this study rely on its prospective design, large sample size, and detailed assessment of artificial sweetener exposure. In fact, if several studies have investigated the associations between ASB and T2D, none had previously considered artificial sweetener exposure from the overall diet. Using 24-h dietary records collecting names and brands of commercial products, allowing for date-to-date dynamic matching with composition data, this study was the first to precisely assess artificial sweetener intakes overall and by molecules, accounting for all dietary sources. In addition, models were adjusted for a wide range of dietary, lifestyle, anthropometric, and sociodemographic confounding variables, which considerably limited residual confounding, although causality cannot be established from one observational study.
It has been suggested that positive associations observed in previous studies may be due to reverse causality, i.e., people at higher risk of T2D, such as participants with overweight/obesity, might be more likely to consume ASBs instead of sugar-sweetened beverages, for instance (38). In fact, results from several prospective studies were nonsignificant after adjustment for BMI (5). Nonetheless, other studies showed significant associations, independently of body weight (5). Thus, we extensively challenged potential reverse causality bias in sensitivity analyses by excluding cases occurring during the first 6 years of follow-up, and results remained similar in this restricted study sample. Additionally, observing the associations among individuals with no early sign of prediabetes (i.e., normal weight status and no prevalence of cardiometabolic disorders, hypertension, or dyslipidemia) further supported the fact that reverse causality is not likely to entirely explain the observed findings.
Next, extrapolating the results should be done cautiously since women and participants with higher educational level were overrepresented in the cohort (39). NutriNet-Santé participants had lower artificial sweetener intakes than the amounts estimated for the French general population (0.51/0.38 mg/kg of body wt/day for aspartame among women/men in NutriNet vs. 0.81/1.08 mg/kg/day in France) (40). This might be because participants who voluntarily enrolled in this cohort were more health conscious (41) and tend to consume less artificially sweetened foods and beverages. This would suggest that associations could be underestimated in the present study compared with what would be observed in a more representative sample of the French population due to reduced contrast between compared categories of sweetener intakes.
In addition, popularity and consumption trends of artificial sweeteners differ among other countries (41); for example, in North America, sucralose is the most important artificial sweetener (by volume), and the highest increase in demand for artificially sweetened products is expected in Latin America and China (41). There are also various assessment methods of artificial sweetener exposure, which makes it difficult to compare intakes between countries (41). Thus, results from the present study should be interpreted and extrapolated cautiously. Studies in other population settings are needed to adequately identify region-specific consumption, trends, and risks associated with artificial sweeteners.
Last, residual confounding cannot be excluded. However, a large range of potential confounding factors were accounted for in main models and sensitivity analyses.
Conclusions, Perspectives, and Policy Implications
This large-scale prospective cohort with detailed dietary data investigated, for the first time, the relationships between artificial sweetener exposure, accounting for all food/beverage sources and risk of T2D. Results suggest positive associations between total artificial sweeteners and main types (aspartame and acesulfame-K, in particular) and higher T2D risk. Of note, results for sucralose appeared to be less robust to sensitivity analyses and warrant further investigation. Although they will benefit from replication in future epidemiological studies, these findings are consistent with those of previous prospective cohorts that used ASBs as a proxy and with experimental evidence regarding plausible mechanisms. They provide key insights in the context of ongoing reevaluation by public health authorities of these substances found in many foods/beverages and ingested daily by millions of individuals worldwide. This new piece of evidence complements recent mounting scientific literature suggesting potential adverse effects of artificial sweeteners on several other chronic diseases (4,5). Altogether, this suggests that artificial sweeteners should not be recommended for a massive consumption as safe alternatives to sugar and that an overall reduction of sugary taste in occidental diets should rather be targeted.
Article Information
Acknowledgments. The authors thank Thi Hong Van Duong, Régis Gatibelza, Jagatjit Mohinder, Aladi Timera, and Rizvane Mougamadou (computer scientists); Julien Allegre, Nathalie Arnault, Laurent Bourhis, and Nicolas Dechamp (data-manager/statisticians); Paola Ivroud (health event validator); and Maria Gomes and Mirette Foham (Nutrinaute support) (all affiliated with University of Paris Cité [CRESS]) for their technical contribution to the NutriNet-Santé study. The authors sincerely thank all the volunteers of the NutriNet-Santé cohort. This project was awarded the NACRe (French network for Nutrition And Cancer Research) Partnership Label.
Funding. The NutriNet-Santé study was supported by the following public institutions: Ministère de la Santé, Santé Publique France, INSERM, Institut national de recherche pour l’agriculture, l’alimentation et l’environnement (INRAE), Conservatoire National des Arts et Métiers (CNAM), and Université Sorbonne Paris Nord. C.D. was supported by the French Institut National du Cancer (grant no. 2019-158). E.C. was supported by a Université Sorbonne Paris Nord Doctoral Fellowship to Galilée Doctoral School. This project has received funding from the European Research Council under the European Union’s Horizon 2020 Research and Innovation Program (Consolidator Grant agreement no. 864219), the French Institut National du Cancer (INCa_14059), the French Ministry of Health (arrêté 29.11.19), the IdEx Université de Paris Cité (ANR-18-IDEX-0001), and a Bettencourt-Schueller Foundation Research Prize 2021.
Researchers were independent from funders. Funders had no role in the study design, the collection, analysis, and interpretation of data, the writing of the report, and the decision to submit the article for publication.
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. C.D. drafted the manuscript and performed statistical analysis. C.D., M.D.-T., E.Ch., B.S., and M.T. designed the study. C.D. and M.T. had full access to all the data in the study. M.D.-T., B.S., and M.T. supervised statistical analysis. E.Ch., N.D.-P., Y.E., and M.T. supervised this technical work. N.D.-P. and Y.E. contributed to global technical work. N.D.-P., Y.E., F.S.d.E., C.A., A.D.S., R.L., and M.T. developed the additives composition database and matched consumption/composition data. F.S.d.E. contributed to data management work. C.A. coordinated dietitian work. M.T. supervised the writing. C.D., M.D.-T., E.Ch., L.S., N.D.-P., Y.E., F.S.d.E., C.A., A.D.S., R.L., C.J., E.K.-G., B.A., P.G., S.H., I.H., E.Co., S.T., B.S., and M.T. contributed to the data interpretation and revised each draft for important intellectual content. All authors read and approved the final manuscript. M.T. is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Clinical trial reg. no. NCT03335644, clinicaltrials.gov
This article contains supplementary material online at https://doi.org/10.2337/figshare.23600688.
The authors alone are responsible for the views expressed in this article and they do not necessarily represent the decisions, policy, or views of the International Agency for Research on Cancer/World Health Organization.
This article is featured in a podcast available at diabetesjournals.org/care/pages/diabetes_care_on_air.
References
- 1. Mooradian AD, Smith M, Tokuda M. The role of artificial and natural sweeteners in reducing the consumption of table sugar: a narrative review. Clin Nutr ESPEN 2017;18:1–8 [DOI] [PubMed] [Google Scholar]
- 2. U.S. Food and Drug Administration . Aspartame and Other Sweeteners in Food. 2018. Accessed 2 March 2018. Available from https://www.fda.gov/food/food-additives-petitions/additional-information-about-high-intensity-sweeteners-permitted-use-food-united-states
- 3. Agence nationale de sécurité sanitaire de l'alimentation, de l'environnement et du travail. Ciqual Table de composition nutritionnelle des aliments. Accessed 8 February 2021. Available from https://ciqual.anses.fr/
- 4. Debras C, Chazelas E, Sellem L, et al. Artificial sweeteners and risk of cardiovascular diseases: results from the prospective NutriNet-Santé cohort. BMJ 2022;378:e071204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Rios-Leyvraz M, Montez J. Health effects of the use of non-sugar sweeteners: a systematic review and meta-analysis. Geneva: World Health Organization, 2022. Accessed 27 April 2022. Available from https://www.who.int/publications/i/item/9789240046429
- 6. Khan MAB, Hashim MJ, King JK, Govender RD, Mustafa H, Al Kaabi J. Epidemiology of type 2 diabetes – global burden of disease and forecasted trends. J Epidemiol Glob Health 2020;10:107–111 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Srour B, Fezeu LK, Kesse-Guyot E, et al. Ultraprocessed food consumption and risk of type 2 diabetes among participants of the NutriNet-Santé prospective cohort. JAMA Intern Med 2020;180:283–291 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Hercberg S, Castetbon K, Czernichow S, et al. The Nutrinet-Santé Study: a web-based prospective study on the relationship between nutrition and health and determinants of dietary patterns and nutritional status. BMC Public Health 2010;10:242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Vergnaud AC, Touvier M, Mejean C, et al. Agreement between web-based and paper versions of a socio-demographic questionnaire in the NutriNet- Santé study. Int J Public Health 2011;56:407–417 [DOI] [PubMed] [Google Scholar]
- 10. Lassale C, Péneau S, Touvier M, et al. Validity of web-based self-reported weight and height: results of the Nutrinet- Santé study. J Med Internet Res 2013;15:e152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Touvier M, Méjean C, Kesse-Guyot E, et al. Comparison between web-based and paper versions of a self-administered anthropometric questionnaire. Eur J Epidemiol 2010;25:287–296 [DOI] [PubMed] [Google Scholar]
- 12. Craig CL, Marshall AL, Sjöström M, et al. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exerc 2003;35:1381–1395 [DOI] [PubMed] [Google Scholar]
- 13. le Moullec N, Deheeger M, Preziosi P, et al. Validation du Manuel-photos utilisé pour l’enquête alimentaire de l’étude SU.VI.MAX. Cah Nutr Diét 1996;31:158–164 [Google Scholar]
- 14. Unité de recherche en épidémiologie nutritionnelle (Bobigny) . Table de composition des aliments, Etude NutriNet-Santé [Food composition table, NutriNet-Santé study]. [in French]. Paris: Les éditions INSERM/Economica, 2013 [Google Scholar]
- 15. Touvier M, Kesse-Guyot E, Mejean C, et al. Comparison between an interactive web-based self-administered 24 h dietary record and an interview by a dietitian for large-scale epidemiological studies. Br J Nutr 2011;105:1055–1064 [DOI] [PubMed] [Google Scholar]
- 16. Lassale C, Castetbon K, Laporte F, et al. Correlations between fruit, vegetables, fish, vitamins, and fatty acids estimated by web-based nonconsecutive dietary records and respective biomarkers of nutritional status. J Acad Nutr Diet 2016;116:427–438 [DOI] [PubMed] [Google Scholar]
- 17. Lassale C, Castetbon K, Laporte F, et al. Validation of a web-based, self-administered, non-consecutive-day dietary record tool against urinary biomarkers. Br J Nutr 2015;113:953–962 [DOI] [PubMed] [Google Scholar]
- 18. Black AE. Critical evaluation of energy intake using the Goldberg cut-off for energy intake: basal metabolic rate. A practical guide to its calculation, use and limitations. Int J Obes Relat Metab Disord 2000;24:1119–1130 [DOI] [PubMed] [Google Scholar]
- 19. Goldberg GR, Black AE, Jebb SA, et al. Critical evaluation of energy intake data using fundamental principles of energy physiology: 1. Derivation of cut-off limits to identify under-recording. Eur J Clin Nutr 1991;45:569–581 [PubMed] [Google Scholar]
- 20. Chazelas E, Druesne-Pecollo N, Esseddik Y, et al. Exposure to food additive mixtures in 106,000 French adults from the NutriNet-Santé cohort. Sci Rep 2021;11:19680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Observatoire de l’alimentation (Oqali) . Accessed 22 Oct 2020. Available from https://www.oqali.fr/oqali_eng/
- 22. Open Food Facts . The free food products database. Accessed 22 Oct 2020. Available from https://world.openfoodfacts.org/discover
- 23. Global New Products Database (GNPD) . Banque de données mondiale de nouveaux produits, suivi des tendances nouveaux produits et innovations. Accessed 22 Oct 2020. Available from https://www.gnpd.com/sinatra/anonymous_frontpage/
- 24. EFSA Panel on Food Additives and Nutrient Sources added to Food (ANS) . Scientific opinion on the re-evaluation of aspartame (E 951) as a food additive. EFSA J 2013;11:3496 [Google Scholar]
- 25. Food and Agriculture Organization/World Health Organization (FAO/WHO) . Codex General Standard for Food Additives (GSFA, Codex STAN 192-1995). Codex Alimentarius Commission, 2019. Accessed 19 September 2018. Available from https://www.fao.org/gsfaonline/docs/CXS_192e.pdf
- 26. Desquilbet L, Mariotti F. Dose-response analyses using restricted cubic spline functions in public health research. Stat Med 2010;29:1037–1057 [DOI] [PubMed] [Google Scholar]
- 27. Khan TA, Field D, Chen V, et al. Combination of multiple low-risk lifestyle behaviors and incident type 2 diabetes: a systematic review and dose-response meta-analysis of prospective cohort studies. Diabetes Care 2023;46:643–656 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Estaquio C, Kesse-Guyot E, Deschamps V, et al. Adherence to the French Programme National Nutrition Santé Guideline Score is associated with better nutrient intake and nutritional status. J Am Diet Assoc 2009;109:1031–1041 [DOI] [PubMed] [Google Scholar]
- 29. Sterne JAC, White IR, Carlin JB, et al. Multiple imputation for missing data in epidemiological and clinical research: potential and pitfalls. BMJ 2009;338:b2393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Jensen PN, Howard BV, Best LG, et al. Associations of diet soda and non-caloric artificial sweetener use with markers of glucose and insulin homeostasis and incident diabetes: the Strong Heart Family Study. Eur J Clin Nutr 2020;74:322–327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Azad MB, Abou-Setta AM, Chauhan BF, et al. Nonnutritive sweeteners and cardiometabolic health: a systematic review and meta-analysis of randomized controlled trials and prospective cohort studies. CMAJ 2017;189:E929–E939 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Qin P, Li Q, Zhao Y, et al. Sugar and artificially sweetened beverages and risk of obesity, type 2 diabetes mellitus, hypertension, and all-cause mortality: a dose-response meta-analysis of prospective cohort studies. Eur J Epidemiol 2020;35:655–671 [DOI] [PubMed] [Google Scholar]
- 33. den Biggelaar LJCJ, Sep SJS, Mari A, et al. Association of artificially sweetened and sugar-sweetened soft drinks with β-cell function, insulin sensitivity, and type 2 diabetes: the Maastricht Study. Eur J Nutr 2020;59:1717–1727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Kundu N, Domingues CC, Patel J, et al. Sucralose promotes accumulation of reactive oxygen species (ROS) and adipogenesis in mesenchymal stromal cells. Stem Cell Res Ther 2020;11:250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Suez J, Cohen Y, Valdés-Mas R, et al. Personalized microbiome-driven effects of non-nutritive sweeteners on human glucose tolerance. Cell 2022;185:3307–3328.e19 [DOI] [PubMed] [Google Scholar]
- 36. Qin J, Li Y, Cai Z, et al. A metagenome-wide association study of gut microbiota in type 2 diabetes. Nature 2012;490:55–60 [DOI] [PubMed] [Google Scholar]
- 37. Romo-Romo A, Aguilar-Salinas CA, Brito-Córdova GX, Gómez Díaz RA, Vilchis Valentín D, Almeda-Valdes P. Effects of the non-nutritive sweeteners on glucose metabolism and appetite regulating hormones: systematic review of observational prospective studies and clinical trials. PLoS One 2016;11:e0161264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Pang MD, Goossens GH, Blaak EE. The impact of artificial sweeteners on body weight control and glucose homeostasis. Front Nutr 2021;7:598340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Andreeva VA, Salanave B, Castetbon K, et al. Comparison of the sociodemographic characteristics of the large NutriNet- Santé e-cohort with French Census data: the issue of volunteer bias revisited. J Epidemiol Community Health 2015;69:893–898 [DOI] [PubMed] [Google Scholar]
- 40. Agence nationale de sécurité sanitaire de l'alimentation, de l'environnement et du travail (Anses) . Evaluation des bénéfices et des risques nutritionnels des édulcorants intenses Maisons-Alfort: Anses; January 2015. (Avide de l’Anses). Accessed 12 February 2021. Available from https://www.anses.fr/fr/system/files/NUT2011sa0161Ra.pdf
- 41. Martyn D, Darch M, Roberts A, et al. Low-/no-calorie sweeteners: a review of global intakes. Nutrients 2018;10:357. [DOI] [PMC free article] [PubMed] [Google Scholar]