ABSTRACT
Background:
Gingival biotype and its relationship to biologic width and alveolar bone thickness may affect surgical periodontal therapy outcomes. Hence, it is vital to assess the gingival biotype prior to any of these treatments for its success.
Aim:
The study aims to compare the thick and thin gingival biotype in the mandibular anterior region concerning biologic width, buccal bone thickness, prevalence and distribution of dehiscence, and fenestration in lower anterior teeth.
Materials and Methods:
A total of 30 patients were selected for the study based on the inclusion and exclusion criteria. The Cone Beam Computed Tomography analysis was performed in the mandibular anterior area to assess gingival thickness (biotype), biologic width, buccal bone thickness, dehiscence, and fenestrations. The data were analyzed using SPSS version 26. An independent t-test was used to assess the relationship between the variables.
Results:
Our study identified an increased biologic width in the thick gingival biotype, a higher frequency of dehiscence in the thin gingival biotype than in the thick biotype, and a greater mean alveolar bone thickness in the thick biotype group.
Conclusion:
A statistical difference was not observed between the groups; however, the thick biotype showed better results than the thinner biotype for the periodontal parameters examined.
KEYWORDS: Alveolar bone, biologic width, dehiscence, fenestration, gingival biotype
INTRODUCTION
Gingival biotype is a term used to describe the thickness of the gingiva in the labiolingual direction. In literature, various gingival biotype (thick and thin) classification has been proposed based on underlying bone and tooth shape,[1] distance from cemento-enamel junction (CEJ) to bone crest,[2] and the thickness and width of keratinized gingival.[3] A varying thickness from 0.7 to 1.5 mm has been suggested for gingival biotype,[4,5] with the gingival thickness ≥1 mm termed as thick, whereas a thin biotype is ≤1 mm.[5] Assessment of gingival thickness previously was carried out by several noninvasive methods for the measurement and classification of gingival thickness–the visual inspection,[6,7] periodontal probe transparency in the gingival sulcus,[8-10] and ultrasound.[11,12]
Cone Beam Computed Tomography (CBCT) has also been used as a noninvasive, promising method of measuring periodontal supporting structures, gingival thickness, and underlying cortical bone and its relation to thick and thin gingival biotype.[13-15]
Evidence from past review suggests that a breach of the biologic width could influence periodontal health by affecting the homeostasis of the periodontal tissues.[1] Several studies observed that gingival recession after surgical and restorative procedures directly correlates with gingival biotype. A thick gingival biotype is usually associated with thick, underlined alveolar bone and is resistant to gingival recession. It also provides better postoperative aesthetic results compared to the thin gingival biotype.[16-18]
Thin gingival biotypes tend to be associated with thin bone over the roots, making them vulnerable to dehiscence and fenestrations and affecting the results of periodontal therapy, root coverage procedures, implant placement, and orthodontic procedures.[19-22]
Identifying alveolar bony fenestrations and dehiscence prior to restorative strategy is helpful for several reasons,[23] as both the types behave differently for inflammatory response and healing response and hence dictate discrete treatment modalities.[24,25]
Many studies observed that visual evaluation, the simplest method, is not considered a reliable assessment, and thin biotypes are usually identified incorrectly.[26,27] In addition, ultrasonographic devices cannot identify minor changes yielding more reliable and repeatable assessments.[28-30]
The purpose of this study is to investigate the relationship between thick and thin gingival biotypes in the mandibular anterior region in relation to biologic width, buccal bone thickness, dehiscence, and fenestration in lower anterior teeth.
MATERIALS AND METHODS
This study was approved by the Institutional Ethical committee and patients requiring CBCT imaging as part of implant or fixed prosthetic treatment plan are included in the study. The inclusion criteria of the study were patients in Qassim province, male, aged from 20 to 50 years, with good periodontal health, systemically healthy, and nonsmokers. Patients who met one of the following criteria were excluded: any systemic disease, smokers, patients who received long-duration antibiotic or antiviral therapy in the last six months, handicapped patients, gingival recession in anterior teeth, and patients who received radiation therapy in the last one year. A total of 60 patients were selected for the study based on the inclusion and exclusion criteria. Primary CBCT examination for gingival thickness was carried out, and finally, 15 patients with thick gingival biotypes and 15 patients with thin biotypes were included for analysis. A total of 180 mandibular anterior teeth (#31, #32, #33 #41, #42, #43), 90 for thick gingival biotype (TkGB1) and 90 for thin gingival biotype (TnGB2), were analyzed using CBCT.
CBCT analysis
CBCT scans of the patients were taken in the radiology clinics of Al-Rass dental college and images were analyzed in the mandibular anterior area for gingival thickness (thick or thin biotype), whether it is thick or thin biotype based on the thickness of the soft tissue with the gingival thickness ≥1 mm termed as TkGB1, whereas ≤1 mm thickness asTnGB2.[5] For measuring the gingival thickness, we used a lip retractor to separate the lip from the gingiva. All the cases were grouped into two groups: Group 1–TkGB1 and Group 2–TnGB2. Both groups were assessed for biologic width, buccal bone thickness, dehiscence, and fenestrations. Gingival and alveolar bone thickness was measured with the sagittal plane view with appropriate magnification. For the assessment of dehiscence and fenestration, we used 3D view. For dehiscence to be considered, the lesion’s vertical distance from the CEJ must be equal to or more than 2 mm. This criterion was intended to prevent counting normal alveolar bone level as a dehiscence, which is usually 1.5 to 2.0 mm below the level of the CEJ.[29] Results of both groups were analyzed and compared. The data were analyzed using SPSS version 26. Quantitative data are expressed as a mean and standard deviation. An independent t-test was used to assess the relationship between the variables. Statistical significance was determined using a P value of 0.05.
RESULTS
Thirty samples of CBCT with a total of 180 teeth were analyzed and divided into TkGB1 (n = 90) and TnGB2 (n = 90).
1. Gingival Biotype Versus Buccal Alveolar Bone Thickness: The demographic data showed the mean of alveolar bone thickness for the TkGB1 was 0.84 mm, while in the TnGB2, it was 0.76 mm.
No statistically significant (P < 0.01) differences were found between the alveolar bone thickness in TkGB1 compared with TnGB2 as shown in Table 1 and Figure 1.
Table 1.
Mean of Alveolar Bone (Buccal) Thickness
| Biotype | n | Mean | Std. Deviation | Std. Error Mean |
|---|---|---|---|---|
| TkGB1 | 90 | 0.8371 | 0.15455 | 0.01629 |
| TnGB2 | 90 | 0.7574 | 0.14277 | 0.01505 |
Figure 1.
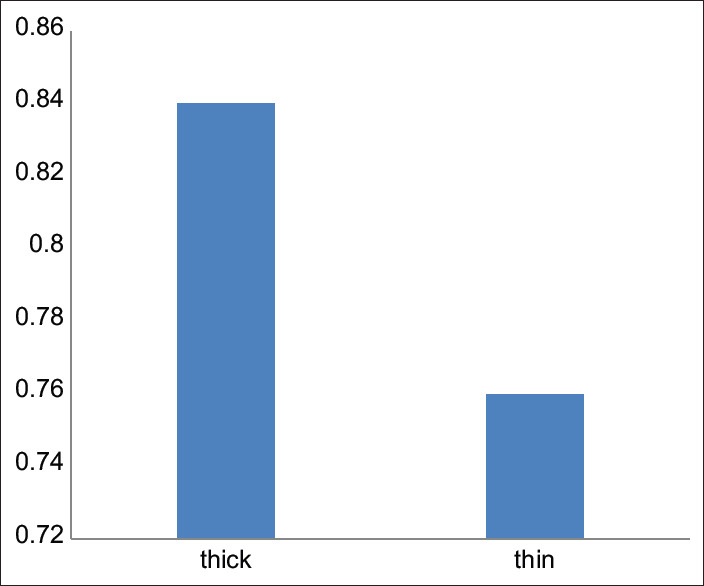
Mean of alveolar bone (buccal) thickness
2. Gingival Thickness and Biologic Width: The result showed a higher value (67.5%) of biologic width of 1 mm–2 mm for TkGB1 compared to 34.2% of TnGB2 of 0.1 mm–1 mm. Also, biological width 0.1 mm–1 mm was found to be 65.8% of TnGB2 compared to a low value of 32.5% of TkGB1 [Table 2 and Figure 2].
Table 2.
Gingival thickness and Biologic width
| Biologic Width (mm) | TkGB1 (n=90) | TnGB2 (n=90) |
|---|---|---|
| 0.1-1 mm | 32.5% (29) | 65.8% (59) |
| 1-2 mm | 67.5% (61) | 34.2% (31) |
Figure 2.
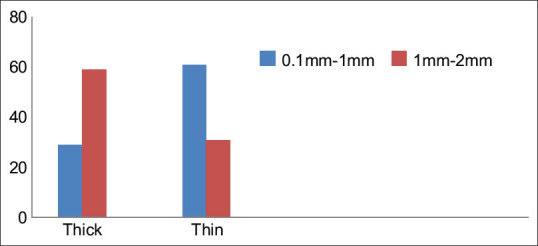
Gingival biotype versus biologic width
This clearly shows the strong association between biologic width upon the nature of the gingival biotype and its correlation with their thickness level.
3. Gingival Biotype Versus Dehiscence: In TkGB1, 23 samples of 90 showed the presence of dehiscence. The mean size of dehiscence was 2.40 mm [Table 3a]. While in TnGB2, 41 teeth of 90 showed the presence of dehiscence. The mean size of dehiscence was 2.68 mm [Table 3b]. When compared for tooth specificity, dehiscence was highest in 31 & 41(10%) for TkGB1 group and highest in 33 & 43 (22%) for TnGB2 group [Figure 3].
Table 3.
(a) Prevalence of Dehiscence in Thick gingiva (b) Prevalence of dehiscence in thin gingiva
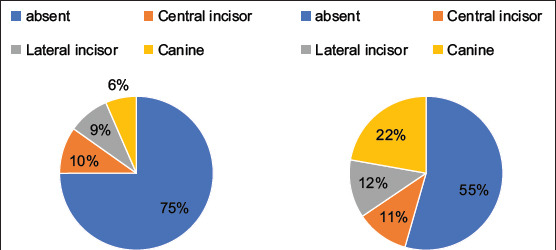
Figure 3.
Gingival Biotypes vs Dehiscence
These results suggest a higher prevalence of dehiscence in the TnGB2 group.
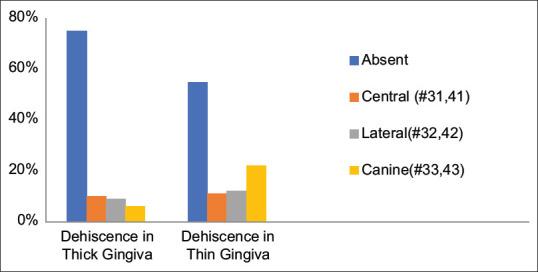
The analysis showed a judicious association for the prevalence of dehiscence in TkGB1 compared with TnGB2, as shown in Table 4 and Figure 4.
Table 4.
Dehiscence Prevalence (number of observations)
| Thick Biotype (n=90) teeth | Thin Biotype (n=90) teeth |
|---|---|
| 25.5% (23) | 45.5% (41) |
Figure 4.
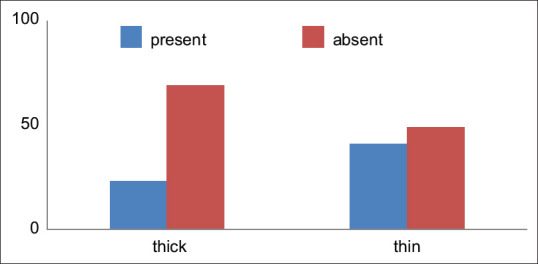
Prevalence of dehiscence and gingival biotype
4. Gingival Biotype Versus Fenestration: In our results, CBCT images of both groups, TkGB1 and TnGB2, did not show any fenestration findings.
DISCUSSION
In our study, we used CBCT to evaluate the gingival thickness in relation to the alveolar bone thickness, biological width, and the prevalence of dehiscence and fenestration.
As far as biologic width is concerned, our study showed that TkGB1 has a higher tendency for biologic width of 1 mm–2 mm (67.5%) compared to TnGB2, where most teeth showed biologic width of 0.1 mm-1 mm (65.8%). These results indicate that TkGB1 will have better biologic width; hence, the prognosis for periodontic preprosthetic therapy is enhanced.[31]
In terms of buccal cortical bone thickness, the present study revealed that TkGB1 showed higher alveolar bone thickness than TnGB2 group, but the mean alveolar bone thickness was not statistically significant as TkGB1 demonstrated a mean alveolar bone thickness of 0.76 mm, whereas TnGB2 demonstrated a mean alveolar bone thickness of 0.76 mm. These results are similar to previous study results where the correlation between the gingival biotype and alveolar bone thickness was nonsignificant in anterior teeth, except for maxillary canine, which can serve as correlation indicators.[29] Our findings indicated that irrespective of the thick or thin gingival biotype, the mandibular anterior teeth present insufficient cortical bone thickness, which is of great concern during aesthetic gingival surgical procedures. This observation is in consensus with previous studies of Ghassemian M et al. (2012) and Zekry A et al. (2014) where they reported maxillary and mandibular anterior teeth to exhibit a thin buccal bone plate.[32,33] Cook et al. (2010) found that periodontal biotype was significantly correlated with alveolar bone thickness and crestal bone level.[34] Since buccal cortical bone loss and gingival recession are quite common after surgical procedure in the lower anterior for aesthetic surgical procedures or implant placement, care should be taken for the selection of procedure, atraumatic surgery/extraction, option for delayed implant placement, or soft/hard tissue augmentation to minimize post-treatment gingival recession.[20,35]
Concerning prevalence of dehiscence and fenestrations, our study demonstrated a greater prevalence of dehiscence in the TnGB2 (45.5%) compared to TkGB1 (25.5%) with highest for canine teeth (22%) and least for central incisors (11%). Hence, before the periodontal soft-tissue surgical procedures or orthodontic therapy, care should be taken to evaluate for dehiscence in thin gingival tissue. The present study was unable to establish the relation between thick and thin gingival biotype to prevalence of fenestration as both the groups did not show any cases with fenestration. Smaller sample was a limitation of this study and hence larger samples would help to find fenestration and its association with Gingival biotypes. So, it is anticipated that gingival biotypes alone may not cause fenestration. Other factors such as angulation of roots, prominence of teeth, occlusal trauma, the thickness of cortical bone, periapical pathology, and orthodontic movement play an essential role in influencing the presence of fenestration.[36-39]
This study has limitation due to small sample size; we are unable to find a statistical difference between alveolar bone thickness in thick and thin gingival biotype.
CONCLUSION
The present study observed that the thick biotype is associated with increased biologic width and decreased prevalence of dehiscence compared to the thin biotype. Moreover, the thick biotype had a greater mean proportion of alveolar bone thickness than the thin biotype. Due to a close gap between the distinction of thick and thin biotypes, no statistically significant difference was found for alveolar bone thickness in the thick biotype compared with the thin gingival biotype and as well no identification of fenestration in our study.
Financial support and sponsorship
Research and manuscript are self-funded.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Ochsenbein C, Ross R. A Periodontal Point of View:A Practical Expression of Current Problems Integrating Basic Science with Clinical Data. Springfield, IL: Charles C. Thomas Publishing, Co; 1973. A Concept of Osseous Surgery and its Clinical Application; pp. 276–323. [Google Scholar]
- 2.Kois JC. The restorative-periodontal interface:Biological parameters. Periodontology 2000. 1996;11:29–38. doi: 10.1111/j.1600-0757.1996.tb00180.x. [DOI] [PubMed] [Google Scholar]
- 3.Müller HP, Eger T. Gingival phenotypes in young male adults. J Clin Periodontol. 1997;24:65–71. doi: 10.1111/j.1600-051x.1997.tb01186.x. [DOI] [PubMed] [Google Scholar]
- 4.Fu JH, Lee A, Wang HL. Influence of tissue biotype on implant esthetics. Int J Oral Maxillofac Implants. 2011;26:499–508. [PubMed] [Google Scholar]
- 5.Kan JYK, Morimoto T, Rungcharassaeng K, Roe P, Smith DH. Gingival biotype assessment in the esthetic zone:Visual versus direct measurement. Int J Periodontics Restorative Dent. 2010;30:237–43. [PubMed] [Google Scholar]
- 6.Ochsenbein C, Ross S. A reevaluation of osseous surgery. Dent Clin North Am. 169:87–102. 13. [PubMed] [Google Scholar]
- 7.Seibert J, Lindhe J. Textbook of Clinical Periodontology. 2nd ed. Munksgaard, Copenhangen: Denmark; 1989. Esthetics and Periodontal Therapy; pp. 477–514. [Google Scholar]
- 8.De Rouck T, Eghbali R, Collys K, De Bruyn H, Cosyn J. The gingival biotype revisited:Transparency of the periodontal probe through the gingival margin as a method to discriminate thin from thick gingival. J Clin Periodontol. 2009;36:428–33. doi: 10.1111/j.1600-051X.2009.01398.x. [DOI] [PubMed] [Google Scholar]
- 9.Kan JY, Rungcharassaeng K, Umezu K, Kois JC. Dimensions of peri-implant mucosa:An evaluation of maxillary anterior single implants in humans. J Periodontol. 2003;74:557–62. doi: 10.1902/jop.2003.74.4.557. [DOI] [PubMed] [Google Scholar]
- 10.Eghbali A, De Rouck T, De Bruyn H, Cosyn J. The gingival biotype assessed by experienced and inexperienced clinicians. J Clin Periodontol. 2009;36:958–63. doi: 10.1111/j.1600-051X.2009.01479.x. [DOI] [PubMed] [Google Scholar]
- 11.Sönmez G, Kamburoğlu K, Gülşahı A. Accuracy of high-resolution ultrasound (US) for gingival soft tissue thickness mesurement in edentulous patients prior to implant placement. Dentomaxillofac Radiol. 2021;50:20200309. doi: 10.1259/dmfr.20200309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Muller HP, Barrieshi-Nusair KM, Könönen E. Repeatability of ultrasonic determination of gingival thickness. Clin Oral Investig. 2003;11:439–42. doi: 10.1007/s00784-007-0125-0. [DOI] [PubMed] [Google Scholar]
- 13.Sayed AJ, Shaikh SS, Shaikh SY, Hussain MA. Inter radicular bone dimensions in primary stability of immediate molar implants-A cone beam computed tomography retrospective analysis. Saudi Dent J. 2021;33:1091–7. doi: 10.1016/j.sdentj.2021.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Amid R, Mirakhori M, Safi Y, Kadkhodazadeh M, Namdari M. Assessment of gingival biotype and facial hard/soft tissue dimensions in the maxillary anterior teeth region using cone beam computed tomography. Arch Oral Biol. 2017;79:1–6. doi: 10.1016/j.archoralbio.2017.02.021. [DOI] [PubMed] [Google Scholar]
- 15.Al-Rawi B, Hassan B, Vandenberge B, Jacobs R. Accuracy assessment of three-dimensional surface reconstructions of teeth from cone beam computed tomography scans. J Oral Rehabil. 2010;37:352–8. doi: 10.1111/j.1365-2842.2010.02065.x. [DOI] [PubMed] [Google Scholar]
- 16.Small PN, Tarnow DP, Cho SC. Gingival recession around wide-diameter versus standard-diameter implants:A 3-to 5-year longitudinal prospective study. Pract Proced Aesthet Dent. 2001;13:143–6. [PubMed] [Google Scholar]
- 17.Kao RT, Fagan MC, Conte GJ. Thick vs thin gingival biotypes:A key determinant in treatment planning for dental implants. J Calif Dent Assoc. 2008;36:193–8. [PubMed] [Google Scholar]
- 18.Jung RE, Sailer I, Hammerle CH, Attin T, Schmidlin P. In vitro color changes of soft tissues caused by restorative materials. Int J Periodontics Restorative Dent. 2007;27:251–7. [PubMed] [Google Scholar]
- 19.Fu JH, Yeh CY, Chan HL, Tatarakis N, Leong DJ, Wang HL. Tissue biotype and its relation to the underlying bone morphology. J Periodontol. 2010;81:569–74. doi: 10.1902/jop.2009.090591. [DOI] [PubMed] [Google Scholar]
- 20.Claffey N, Shanley D. Relationship of gingival thickness and bleeding to loss of probing attachment in shallow sites following nonsurgical periodontal therapy. J Clin Periodontol. 1986;13:654–7. doi: 10.1111/j.1600-051x.1986.tb00861.x. [DOI] [PubMed] [Google Scholar]
- 21.Huang LH, Neiva RE, Wang HL. Factors affecting the outcomes of coronally advanced flap root coverage procedure. J Periodontol. 2005;76:1729–34. doi: 10.1902/jop.2005.76.10.1729. [DOI] [PubMed] [Google Scholar]
- 22.Hwang D, Wang HL. Flap thickness as a predictor of root coverage:A systematic review. J Periodontol. 2006;77:1625–34. doi: 10.1902/jop.2006.060107. [DOI] [PubMed] [Google Scholar]
- 23.Schmidt JC, Sahrmann P, Weiger R, Schmidlin PR, Walter C. Biologic width dimensions –A systematic review. J Clin Periodontol. 2013;40:493–504. doi: 10.1111/jcpe.12078. [DOI] [PubMed] [Google Scholar]
- 24.Ferrus J, Cecchinato D, Pjetursson EB, Lang NP, Sanz M, Lindhe J. Factors influencingridge alteration following immediate implant placement intoextraction socket. Clin Oral Implants Res. 2010;21:22–9. doi: 10.1111/j.1600-0501.2009.01825.x. [DOI] [PubMed] [Google Scholar]
- 25.Lindhe J, Berglundh T, Ericcson I, Lilfenberg B, Marinello L. Experimental breakdown of peri-implant and periodontaltissues. A study in the beagle dog. Clin Oral Implants Res. 1992;3:9–16. doi: 10.1034/j.1600-0501.1992.030102.x. [DOI] [PubMed] [Google Scholar]
- 26.Joshi N, Agarwal MC, Madan E, Gupta S, Law A. Gingival biotype and gingival bioform:Determining factors for periodontal disease progression and treatment outcome. Int J Sci Stud. 2016;4:220–25. [Google Scholar]
- 27.Evans CDJ, Stephen T. Chen “Esthetic outcomes of immediate implant placements”. Clin Oral Implants Res. 2008;19:73–80. doi: 10.1111/j.1600-0501.2007.01413.x. [DOI] [PubMed] [Google Scholar]
- 28.Leung CC, Palomo L, Griffith R, Hans MG. Accuracy and reliability of cone-beam computed tomography for measuring alveolar bone height and detecting bony dehiscences and fenestrations. Am J Orthod Dentofac Orthop. 2010;137:S109–19. doi: 10.1016/j.ajodo.2009.07.013. [DOI] [PubMed] [Google Scholar]
- 29.Ten NA. 8. St. Louise, MO: Elsevier; 2013. Cate's Oral Histology: Development, Structure, and Function. [Google Scholar]
- 30.Sanavi F, Weisgold AS, Rose LF. Biologic width and its relation to periodontal biotypes. J Esthet Dent. 1998;10:157–63. doi: 10.1111/j.1708-8240.1998.tb00351.x. [DOI] [PubMed] [Google Scholar]
- 31.Frumkin N, Via S, Klinger A. Evaluation of the width of the alveolar bone in subjects with different gingival biotypes:A prospective cohort study using cone beam computed tomography. Quintessence Int. 2017;48:209–16. doi: 10.3290/j.qi.a37642. [DOI] [PubMed] [Google Scholar]
- 32.Ghassemian M, Nowzari H, Lajolo C, Verdugo F, Pirronti T, D'Addona A. The thickness of facial alveolar bone overlying healthy maxillary anterior teeth. J Periodontol. 2012;83:187–97. doi: 10.1902/jop.2011.110172. [DOI] [PubMed] [Google Scholar]
- 33.Zekry A, Wang R, Chau AC, Lang NP. Facial alveolar bone wall:A cone beam computed tomography study in Asians. Clin Oral Implants Res. 2014;25:194–206. doi: 10.1111/clr.12096. [DOI] [PubMed] [Google Scholar]
- 34.Cook DR, Mealey BL, Verrett RG, Mills MP, Noujeim ME, Lasho DJ, et al. Relationship between clinical periodontal biotype and labial plate thickness:An in vivo study. Int J Periodontics Restorative Denti. 2010;31:345–54. [PubMed] [Google Scholar]
- 35.Nisapakultorn K, Suphanantachat S, Silkosessak O, Ratanamongkolgul S. Factors affecting soft tissues levelaround anterior maxillary single tooth implants. Clin Oral Implants Res. 2010;21:662–70. doi: 10.1111/j.1600-0501.2009.01887.x. [DOI] [PubMed] [Google Scholar]
- 36.Jorgić-Srdjak K, Plancak D, Bosnjak A, Azinović Z. Incidence and distribution of dehiscences and fenestrations on human skulls. Coll Antropol. 1998;22((Suppl)):111–6. [PubMed] [Google Scholar]
- 37.Nimigean VR, Nimigean V, Bencze MA, Dimcevici-Poesina N, Cergan R, Moraru S. Alveolar bone dehiscences and fenestrations:An anatomical study and review. Rom J Morphol Embryol. 2009;50:391–7. [PubMed] [Google Scholar]
- 38.Zawawi KH, Al-Harthi ŞM, Al-Zahrani MS. Prevalance of gingival biotype and its relationship to dental malocclusion. Saudi Med J. 2012;33:671–5. [PubMed] [Google Scholar]
- 39.Garg N, Bhagyalakshmi A, Raghunath N, Shivalinga BM, Avinash BS. Gingival biotype and its relation to incisors'inclination and dentopapillary complex:An in vivo study. Int J Orthod Rehabil. 2017;8:11–8. [Google Scholar]


