Abstract
Two in five African American men have obesity, but they are underrepresented in community-based weight loss interventions. This pilot effectiveness trial examines the acceptability and feasibility of the first weight loss study for African American men that includes randomization and individual tailoring. Using a community-based, cluster-randomized, longitudinal parallel group design, four churches were randomized to a control condition or a weight loss condition. Each church received physical activity equipment, a coordinator, and small group physical activity sessions. A total of 71 African American men (mean age: 58.5) enrolled and received a Fitbit, Bluetooth-enabled scale, a t-shirt, gift cards for participation, and 45 min of small group physical activity led by a certified personal trainer. Men in the weight loss condition also received 45 min of health education and individually tailored SMS text messages. Multiple metrics suggest that Mighty Men was feasible, yet the acceptability of the intervention components was mixed. Participants in both the weight loss and control conditions lost weight between zero and 6 months (p < .001), but body fat (p = .005) and visceral fat percentage (p = .001) of men in the weight loss condition decreased while men in the control condition did not (p < .05). An increase in physical activity was seen among men in the weight loss condition (p = .030) but not among men in the control condition (p < .05). It is acceptable and feasible to conduct a 6-month weight loss intervention with African American men that includes randomization and individually tailored text messages.
Keywords: African American men, men’s health equity, intervention, weight loss, faith-based, obesity, implementation science
For those who have obesity, weight loss through diet and physical activity remains a critical intervention to prevent and modify individual risk for cancers, Type 2 diabetes, coronary heart disease, hypertension, sleep apnea, and other chronic conditions (Abshire et al., 2023; American Cancer Society, 2020; Borek et al., 2018; Schubart et al., 2011). Waist circumference has been identified to be directly associated with all-cause mortality when adjusted for total body fat, suggesting an increased mortality risk related to excess body fat is mainly due to abdominal adiposity (Ross et al., 2020). Men aged 40 and older have a higher rate of obesity than men aged 20 to 39 (Fryar et al., 2020), and men are less likely than women to adopt a healthy lifestyle past age 45, which is yet another reason that men are at greater risk of mortality and cardiovascular disease than women (King et al., 2007).
Regardless of gender, most behavioral interventions include dietary changes, exercise, and a similar set of behavior-change techniques, including tools to promote self-monitoring of behavior and weight (United States Preventive Services Task Force, 2018). While there does not appear to be a difference in the weight loss needs of women and men, men are underrepresented in formal weight control programs or intervention trials (Crane et al., 2017; Robertson et al., 2016). Thus, men are not receiving the health benefits of weight loss intervention participation (Crane et al., 2017). A systematic review of randomized controlled trials of weight management interventions conducted in Australia, Finland, Italy, the Netherlands, the United Kingdom, and the United States for obese men and women found that men are underrepresented in studies open to both sexes (Robertson et al., 2016). Robertson et al. (2016) reported that men and women have different preferences for types of weight management interventions, and there are gender differences in the response to different weight control intervention approaches.
For men, weight loss is best achieved and maintained with the combination of reduced diet, increased physical activity, and behavior change techniques (Robertson et al., 2017). However, there is little evidence that interventions that promote dietary modifications and physical activity changes consider or account for the greater body size or muscle mass of obese men (Robertson et al., 2016). Although some argue that there is little evidence to support different weight loss strategies for men and women, Robertson et al. (2016) argue that the within-study differences found in their review show gender variation in response to interventions and therefore suggest more data are needed to most effectively address the needs of men. While there may not be enough data to conclude what study designs are best for men, or whether weight control, management, and loss interventions should be designed differently for men and women (Robertson et al., 2016), few gender-tailored weight loss interventions seem to have consulted or been informed by the views of men (Robertson et al., 2016, 2017). Men tend to be reluctant to join groups, and it may be important to ensure that groups are designed and tailored specifically to attract, engage, and retain men; however, very few trials reported that they had consulted men during the development of their interventions (Robertson et al., 2017). When compared with women, men are less likely to perceive themselves as overweight, or to report attempting to control or lose weight (Crane et al., 2017). Some data suggest that men may lose more weight when interventions include more individual support or tailored advice, personalized feedback, simple fact-based language, promote a greater sense of personal control, or acknowledge that men’s educational needs may differ from women’s (Robertson et al., 2016).
African American Men’s Health
Non-Hispanic Black men have lower rates of obesity than Hispanic men, Non-Hispanic White men, and Asian men (body mass index [BMI] ≥30+ kg/m2), yet Non-Hispanic Black men have higher rates of severe obesity than Hispanic men, Non-Hispanic White men, and Asian men (BMI ≥40+ kg/m2; Fryar et al., 2020; Hales et al., 2018). Relative to White men, African American women, and other Americans, African American men’s shorter life expectancy and overall poorer health have been documented for more than 100 years (Arias & Xu, 2019; Griffith, 2018, 2020; Griffith, Holliday, et al., 2021). With their rates of obesity and severe obesity, chronic disease, and premature mortality, there is an urgent need to develop weight loss interventions to promote healthier and more active lifestyles for African American men (Abshire et al., 2023; American Cancer Society, 2022; Borek et al., 2018; Griffith & Jaeger, 2020; Griffith, Jaeger, et al., 2021; Powell et al., 2018).
Behavioral Interventions to Improve African American Men’s Health
While African American men’s poor health is well-documented, few reviews of interventions to promote men’s weight loss have considered potential unique patterns and impacts by race (Crane et al., 2017; Lowe et al., 2020; Robertson et al., 2016, 2017), and efforts to reduce obesity among African Americans have historically failed to consider gender (Borek et al., 2018; Crane et al., 2017; Griffith et al., 2018; Lowe et al., 2020; Newton et al., 2014; Whitt-Glover et al., 2014; Whitt-Glover & Kumanyika, 2009). Carr et al. (2022) argue that the Diabetes Prevention Program, Look AHEAD and PREMIER, and other seminal multicenter trials have often failed to meet recruitment, retention, and weight loss goals for African Americans in their studies. Behavioral interventions targeted at African Americans are thought to be gender-neutral, but they typically have included far fewer men than women (Burton et al., 2017; Crane et al., 2017; Newton et al., 2014; Whitt-Glover et al., 2014, 2017). Physical activity, healthy eating, and other weight loss or weight maintenance interventions specifically for African Americans have included few African American men (Borek et al., 2018; Griffith et al., 2018; Lowe et al., 2020; Newton et al., 2014, 2019).
Interventions that were targeted at African American men had a high risk of bias, including participants not being randomized and there being no control group utilized as a comparison (Griffith et al., 2018; Joseph et al., 2022; Newton et al., 2014). Only one study, Joseph et al. (2022), focused on weight loss or weight control and lasted more than 3 months; their intervention lasted 6 months. Joseph et al. (2022) conducted Black Impact, which was an important contribution to the literature as it is one of the first studies to demonstrate the acceptability, feasibility, and impact of an intervention designed for Black men based on weight, BMI, cholesterol, glucose, and diet. The single-arm pilot design of an intervention conducted in recreation and park centers would be considered to have a high risk of bias due to the lack of a comparison group, lack of random assignment of participants, and other factors that would mitigate concerns about reliability, validity, reproducibility, and sustainability. In sum, there are no rigorously designed weight loss studies designed explicitly for African American men that have lasted 6 months or included randomization of participants or study conditions.
The Present Study
The present study is a pilot effectiveness study: a small-scale test of the feasibility and acceptability of the approach, methods, and procedures to be used in a larger-scale study in real-world conditions (National Center for Complementary and Integrative Health, 2022; Porzsolt et al., 2015). The primary goal of this pilot is to assess the logistical feasibility and acceptability of the effectiveness trial protocol for investigators and participants in preparation for a fully powered randomized controlled trial (Czajkowski et al., 2015; Freedland, 2020). The three aims of this pilot study are to (a) evaluate the feasibility of the approach (e.g., rates of completion; ability to recruit, randomize, and retain participants and churches); (b) assess the acceptability of the trial procedures (e.g., quantitative and qualitative feedback from participants, trainers, staff and consultants on the study procedures, components, and length of study); and (c) explore the impact of the intervention (e.g., pre–post changes in anthropometric measures, biomarkers, behavior, and psychosocial mediators). To achieve these aims, we include a control group with an alternative intervention (Freedland et al., 2019) that was acceptable to our community partners (i.e., faith-based organizational leaders) to allow us to test our ability to recruit and randomize churches, enroll and retain participants, and implement the intervention with fidelity (National Center for Complementary and Integrative Health, 2022). In addition, it is unclear whether a randomized design is feasible and acceptable to African American men. Having a randomized design may not always be necessary for pilot studies, but having a comparison group can provide a more realistic examination of recruitment rates, randomization procedures, implementation of interventions, and the potential to assess for differential dropout rates (National Center for Complementary and Integrative Health, 2022). It is also uncertain if individually tailoring SMS text messaging designed for African American men is an acceptable and feasible component of a multilevel community-based intervention for this population. SMS text messaging is ubiquitous, inexpensive, scalable, and familiar to African Americans and others (Perrin, 2021). Using technology that African Americans utilize on a daily basis like SMS text messaging helps overcome access, literacy, and numeracy barriers associated with other forms of communication (Aoun et al., 2012; S. Armstrong et al., 2017; Greaney et al., 2009).
Theoretical Foundations of the Present Study
While there have been interventions individually tailored to African American women (Bennett et al., 2013; Herring et al., 2017; Herring et al., 2016), we propose to conduct the first intervention individually tailored to African American men (Griffith & Jaeger, 2020). The present study was anchored in the Social Ecological Framework (McLeroy et al., 1988) of health behavior to highlight environmental constraints (e.g., resources and opportunities to engage in physical activity) that men face, and particularly African American men (Griffith et al., 2011). Elements of Social Cognitive Theory also were included to identify the importance of providing opportunities for goal setting and self-monitoring, skills training and mastery of health behaviors, and self-efficacy to change and maintain health behavior (Bandura, 2004). In addition, we sought to enhance social support to help men develop and grow active social networks that could help them combat time pressures, unhealthy social norms, and other interpersonal barriers to physical activity (Anderson et al., 2007; Israel & McLeroy, 1985). Finally, this study aimed to enhance Autonomous Motivation, a key element of Self-Determination Theory, that highlights the need for men to identify their own sources of motivation, not ones performed due to external or internal pressure or coercion (e.g., pleasing others, fear of disease, avoiding guilt or shame; Fortier et al., 2009). Autonomously motivated individuals not only see the importance of the behavior but also connect changes to their core values and beliefs. These individuals feel competent, are ready to act and persist when faced with obstacles, and have identified meaningful reasons for change (Resnicow et al., 2017; Ryan & Deci, 2000). Thus, Self-Determination Theory was a key aspect of our approach to individually tailoring SMS text messages.
Tailoring health communication entails using information from an individual or population to determine the content, the context surrounding the content, and who and how the information will be delivered (Hawkins et al., 2008). This process has been found to enhance the relevance and impact of health messages (Davis & Resnicow, 2011; Hawkins et al., 2008) and health interventions. In the last 30 years, individual tailoring has been used in myriad studies to increase recipient attention, processing effort, and perceived message salience, thereby outperforming generic or group-targeted messages in promoting health behavior change (Hawkins et al., 2008; Latimer et al., 2010). Tailored messages are customized to each individual (Noar et al., 2009) using strategies and information intended to reach a specific person, based on characteristics that are unique to that person (Kreuter et al., 1999) because these strategies for individualizing messages increase the likelihood that people will view the message as relevant to them and consciously choose to make and sustain healthy behavior changes. The unique tailoring approach tested in this study uses two types of tailoring: one that focuses on the centrality of factors related to identity and a second that focuses on increasing the salience of messages to men’s daily lives on autonomous motivation or helping men overcome modifying factors that constrain opportunities and motivation to engage in healthier behaviors (Griffith, Jaeger, et al., 2021; Ryan & Deci, 2000).
Method
Setting
From 2017 to 2019, we partnered with churches in metropolitan Atlanta, GA: the largest metropolitan statistical area in Georgia and the state’s capital. Approximately half (48.2%) of the city’s population is African American (United States Census Bureau, 2022). When compared with their White counterparts in the state, African Americans in Georgia have higher rates of heart disease and cancer (Centers for Disease Control and Prevention, 2020; National Cancer Institute, 2018). The study was reviewed and approved by the (Vanderbilt University Institutional Review Board; Approval No. 191252). All participants provided written informed consent prior to enrollment in the study.
Study Design and Intervention Components
We randomized four churches to a control condition or a weight loss condition, but participants within each church were not randomized. We chose this pilot design because it preserves independence at the church level, provides the ability to study church-level factors, and prevents cross-subject contamination (e.g., behavior adoption, information sharing) of intervention effects of participants within churches. This design allowed us to intervene both at the individual and at small group levels within each church (Griffith & Jaeger, 2020).
The Mighty Men curriculum also included content from various health education resources and existing curricula (e.g., the Diabetes Prevention Program). We provided physical activity equipment to all churches (i.e., kettlebells, resistance bands, exercise mats, bosu balls, and balance balls) to use during small group sessions. Churches were able to keep the physical activity equipment after the completion of the program. To maximize assessment participation, we gave participants an incentive for the 0-, 3-, and 6-month assessment visits—US$30, US$40, and US$50, respectively.
We recruited churches using methods successfully implemented in previous faith-based studies (Bopp et al., 2012; Lancaster et al., 2014; Resnicow et al., 2002, 2004, 2005). We created a list of churches in the geographic area regardless of Christian denomination. Following sending an initial information packet via postal mail or email, a member of the Mighty Men team called the church to follow up to confirm receipt of the information and to assess interest and eligibility. Simultaneously, we created a video and virtual flyer that we distributed via social media. Next, we set up an appointment to present the project to church leaders and interested members of the leadership team at the church. The process of recruitment, engagement, and agreement for the church to be part of Mighty Men took approximately 3 months. The recruitment process concluded with a designated church leader signing a memorandum of agreement on behalf of the church. Churches were randomized either to the control group or to a weight loss condition (see Table 1). We chose to have a nontraditional control group in this pilot study because this was an effectiveness trial in a community setting that used a community-based participatory research approach (Griffith et al., 2009). We initially planned to have a health education intervention as a control group, but the faith leaders that we collaborated with asked that our control group include something that would be more tangibly beneficial to the participants; thus, we chose to provide participants with 45 minutes of small-group physical activity training led by a certified personal trainer, a Fitbit Charge 2 physical activity tracker, and Bluetooth enabled weight scale devices for participant self-monitoring.
Table 1.
Intervention Components by Condition
| Control Condition | Weight Loss Condition |
|---|---|
| Self-monitoring (via Fitbit and Bluetooth-enabled weight scale) | Self-monitoring (via Fitbit and Bluetooth-enabled weight scale) |
| • 45 min of small group physical activity led by a personal trainer | • 45 min of small group physical activity led by a personal trainer • 45 min of the Mighty Men curriculum |
| No SMS text messages or goal tracking | Tailored SMS text goals/messages—3×/week • Reminder message • Tailored motivational message • Tailored goal-tracking message |
| Educational resources (NIH handouts, list of websites) | Educational resources (NIH handouts, list of websites) |
Note. NIH = National Institutes of Health.
Participants in the weight loss condition received the same equipment and activities as the control condition participants and also received 45 min of health education led by the certified personal trainer, and three SMS text messages a week. The three SMS text messages a week included a small group session reminder, an individually tailored motivational message (Griffith, Jaeger, et al., 2021), and an individually tailored goal-tracking message (Griffith, Jaeger, et al., 2021). Only the goal-tracking SMS message required a response. Our tailoring methodology was informed by previous work that identified manhood and race—and their intersection—as important variables to include to increase health messaging salience (Griffith, Pennings, et al., 2019; Griffith & Cornish, 2018). Participants in the control condition did not receive any motivational or goal-tracking messages, nor did they receive the weight loss education content until after the study was completed. The weight loss education content was a 24-week curriculum designed by our study team.
Church Eligibility Characteristics
To be eligible to participate, each church had to meet inclusion criteria and sign a Memorandum of Understanding indicating the following: (a) the church had not participated in a research study that included discussion of eating, physical activity, or weight loss in the last year; (b) the church leadership and representatives understood that they would be participating in a research study; (c) the church had at least 75 active adult members, most of whom were African American; (d) the church leadership and representatives accepted that this intervention was exclusively for middle-aged and older African American men who met our inclusion criteria; (e) the church agreed to be randomized to either the control condition or the weight loss condition; and (f) the church would receive an honorarium and physical activity equipment in addition to the honoraria and equipment that individual participants received. Following the signing of this agreement, we added each church to the Institutional Review Board application as a study site.
Participant Recruitment and Inclusion Criteria
We recruited men within enrolled churches via the distribution of flyers, word of mouth, and sending emails to the organization with requests to distribute information. We hired a coordinator from within each church to be our primary point of contact. The church coordinator’s role was to distribute recruitment material to potential participants, to help recruit participants, to facilitate the opening and closing of the church facility, and to set up and break down the room in the church where small group sessions would take place. As a study employee, the church coordinator was paid hourly for their work with the study. We recruited churches from November 2017 to April 2018, and we recruited, enrolled, and collected data from participants from April 2018 to May 2019.
We enrolled participants if they: (a) primarily identified as an African American or Black man; (b) were 35–77 years old at the time of enrollment; (c) had a body mass index (BMI) of 27 or greater; (d) weighed less than 400 pounds; (e) did not have any medical conditions that would not allow for them to safely increase their physical activity level (potential participants had to complete the Physical Activity Readiness Questionnaire [PAR-Q] and get written clearance from a medical provider if they answered yes to any of the questions); (f) had a smart phone with SMS text message capability; (g) had no prior or planned bariatric or weight loss surgery; and (h) did not participate in a different obesity, healthy eating, or physical activity program or study in the past 6 months.
Assessment Measures
Acceptability
We assessed the acceptability of Mighty Men by capturing the use of self-monitoring devices (Fitbit, scale), the reported intent to continue using self-monitoring devices (Fitbit, scale), the perceived appropriateness of messaging and curriculum, the attrition rate of participants per condition at 3 and 6 months, the evaluation (ratings) of intervention components per condition, and the utilization of Fitbit.
Feasibility
We assessed the feasibility (Arain et al., 2010) of Mighty Men by evaluating the reach, enrollment, and sustainability of the intervention. Using a survey after the 6-month intervention was complete, we captured how much participants reported that they continued or maintained the desired changes 3 months after the study. We also captured the participation rates, attendance at weekly small group sessions, and attendance at outcome assessments by study condition.
Anthropometric Measurements
Our primary outcome was a change in weight at 6 months post-baseline, both in absolute terms as well as percent change from baseline. We hired nurses and other allied health professionals and trained study staff to collect the anthropometric data. We used a high-quality, calibrated digital Tanita scale (Tanita Corporation, 2020) to measure weight (in street clothes without socks or shoes), body mass index (BMI) (calculated as kg/m2), body fat percentage, and visceral fat percentage. We also measured height, neck circumference, waist circumference, and blood pressure.
Blood Markers
Allied health professionals measured total cholesterol, low-density lipoprotein (LDL), high-density lipoprotein (HDL), triglycerides, and blood glucose (nonfasting).
Behaviors
We assessed fruit and vegetable intake during the past month via the Food Attitudes and Behaviors (FABS) questionnaire (Erinosho et al., 2015) validated using multiple 24-hr dietary recalls assessed fruit and vegetable intake (adjusted correlation coefficients ranged from 0.39 to 0.57 for fruit, vegetable, and fruits and vegetables combined; Yaroch et al., 2012). We measured physical activity using the Global Physical Activity Questionnaire (GPAQ; Herrmann et al., 2013) at all survey points including baseline, 3 months (midpoint), and 6 months (final). The GPAQ has shown acceptable test–retest reliability by activity category and modest validity evidence comparable with other subjective physical activity questionnaires such as the International Physical Activity Questionnaire (IPAQ). The GPAQ has the advantage that it captures information in specific physical activity domains (T. Armstrong & Bull, 2006; see Table 2 for more details).
Table 2.
Assessment Measures
| Title | Scale or Measurement Information | Brief Description |
|---|---|---|
| Acceptability | Actual use of self-monitoring devices (Fitbit, scale), intent to continue use of self-monitoring devices (Fitbit, scale), perceived appropriateness of messaging and curriculum | Attrition rate per condition at 3 and 6 months Evaluation (ratings) of intervention components Utilization of Fitbit |
| Feasibility (Arain et al., 2010) | Reach, Enrollment and Sustainability | Continuation or maintenance of desired changes via follow-up survey Participation rate and attendance of weekly small group sessions and at outcome assessments by study condition. |
| Anthropometric measures | ||
| Weight, BMI, body fat percentage, visceral fat percentage | High-quality calibrated digital Tanita Scale© (Tanita Corporation, 2020) | Measurements taken in street clothes without socks or shoes. BMI calculated as kg/m2 Visceral fat note: because of staff error, we did not measure visceral fat percentage at baseline for 10 participants. |
| Height | Measured using a calibrated stadiometer to the nearest 0.1 centimeter | Measured once at baseline, the participant stood shoeless on a firm, level surface, with his head in a horizontal plane. |
| Neck circumference | Measured to the nearest half inch using an anthropometric measuring tape | Measured by placing the measuring tape directly on the skin just below the larynx (Adam’s apple) and extending the tape horizontally around the neck while participants relaxed their shoulders. |
| Waist circumference | Measured to the nearest half inch using an anthropometric measuring tape | Measured with participant standing feet shoulder-width apart, placing the measuring tape about halfway between the bottom of the lowest rib and top of the hip bones, rough in line with the belly button. Participants were then asked to inhale, measurement was taken on the exhale. |
| Blood pressure | Pulse, systolic, and diastolic blood pressure with an automated blood pressure cuff | Cuff placed around the upper part of the participant’s arm to fit smoothly and snugly with the bottom edge one inch above his elbow. A total of three blood pressure and pulse readings were taken with a 5-min break between each reading. |
| Blood markers | ||
| Total cholesterol, LDL cholesterol, HDL cholesterol, blood glucose (nonfasting) | Sample taken from a finger stick blood sample and analyzed using a Cholestech machine (Bastianelli et al., 2017) | Finger prick administered to a clean middle or ring finger using a lancet and captured blood in a capillary tube. The blood sample was dispensed from the tube into the cassette and the cassette was placed in the Cholestech machine to be analyzed. |
| Behaviors | ||
| Global Physical Activity Questionnaire (GPAQ) (Herrmann et al., 2013) | 16 items; four domains • Activity at work • Travel to and from places • Recreational activities • Sedentary behavior |
The main outcome variables from GPAQ analysis include a categorical variable of total physical activity (high, moderate and low); continuous variable of total physical activity within each domain—work, transport, leisure (reported as median MET min/week). |
| “What You Ate in the Last Month”—Foods Attitudes and Behaviors—Section 6” (Erinosho et al., 2015) | 8 items • For each item, (a) frequency (how often) and (b) quantity (how much) responses are captured |
A fruit and vegetable screener that was modified from the National Cancer Institute’s fruit and vegetable screener (Erinosho et al., 2015). Response options included ten frequency categories ranging from never to ≥5 times/day, and four portion size categories ranging from about ¼ cup to more than 2 cups. We converted responses into servings and calculated total fruit and vegetable intake as the sum of all items on the screener, excluding fried potatoes. |
Note. BMI = body mass index; LDL = low-density lipoprotein; HDL = high-density lipoprotein; MET = metabolic equivalent.
Sample Size and Randomization
While churches were the unit of randomization, individuals were the units of analysis. Because weight loss among individuals within the same faith-based organization (FBO) was likely more similar than weight loss among individuals in different FBOs, we had to account for the intra-class correlation (ICC). We adjusted for ICC to cluster randomization by using generalized estimating equation (GEE), although there is limited prior data from which to estimate the ICC. Previous studies suggest the ICC of outcome measures in cluster randomized trials is 0.05 or less. Churches were randomized into a block of four. The randomization was done by the statistician; only the statistician had access to the allocation sequence. Study staff were notified of the outcome of the randomization of churches to the control condition or weight loss condition. We in turn notified church coordinators and then proceeded with participant recruitment. The goal was for each church to enroll a minimum of 20 men.
Data Analytic Approach
The statistician used SPSS version 26 for all statistical analysis, and set the level of statistical significance at p < .05. The statistician evaluated the distributions of the variables and ran descriptive statistics including means and standard deviations of continuous variables and frequencies and percentages of categorical variables. The statistician analyzed health outcomes (i.e., weight, glucose, body fat percentage, visceral fat percentage, and physical activity METs) for changes over time (baseline, 6-month final) using paired-sample t tests for comparison group participants and weight loss participants. Random effects models were not possible to conduct due to the limited number of clusters, which is attributable to the pilot nature of the project. Given the pilot study nature and small sample size, we did not examine between-group differences since not sufficiently powered to detect effects (Freedland, 2020; National Center for Complementary and Integrative Health, 2022).
Results
Participant Characteristics
Descriptive statistics of the 71 African American men who completed the baseline assessment are presented in Table 3. The mean age for participants was 50.4 (SD = 7.9) years, with an age range of 36.8 to 73.2 years. Most of the men were married or in a relationship (n = 55, 77.5%), and more than 40% were unemployed or retired (n = 29, 40.8%). The mean baseline BMI was 37.3 (SD = 5.6) with 95.8% of the men (n = 68) categorized as obese (BMI ≥30).
Table 3.
Demographic Characteristics of Overall Sample and by Group
| Demographic Characteristic | Total | Intervention | Control | p | |||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Demographic variables | |||||||
| Age (M, SD) | 50.4 | 7.9 | 51.3 | 8.0 | 49.6 | 7.9 | 0.352 |
| Race—African American or Black | 71 | 100% | 29 | 40.8% | 42 | 59.2% | |
| Married/in relationship | 55 | 77.5% | 23 | 69.7% | 32 | 84.2% | 0.144 |
| Number of children | 0.781 | ||||||
| None | 7 | 9.9% | 4 | 12.1% | 3 | 7.9% | |
| One | 14 | 19.7% | 5 | 15.2% | 9 | 23.7% | |
| Two | 22 | 31.0% | 11 | 33.3% | 11 | 28.9% | |
| Three or more | 28 | 39.4% | 13 | 39.4% | 15 | 39.5% | |
| Education | 0.716 | ||||||
| No college degree | 21 | 29.6% | 11 | 33.3% | 10 | 26.3% | |
| Associate’s/bachelor’s | 23 | 32.4% | 11 | 33.3% | 12 | 31.6% | |
| Master’s/doctorate/professional | 27 | 38.0% | 11 | 33.3% | 16 | 42.1% | |
| Employment status | 0.829 | ||||||
| Employed, full-time or part-time | 42 | 59.15% | 12 | 28.57% | 30 | 71.43% | |
| Unemployed/retired | 29 | 40.85% | 17 | 58.62% | 12 | 41.38% | |
| Income | 0.743 | ||||||
| Less than 50K | 16 | 23.2% | 9 | 27.3% | 7 | 19.4% | |
| 50K–<100K | 20 | 29.0% | 9 | 27.3% | 11 | 30.6% | |
| 100K+ | 33 | 47.8% | 15 | 45.5% | 18 | 50.0% | |
| Health variables | |||||||
| BMI (M, SD) | 37.3 | 5.6 | 37.7 | 5.6 | 37.0 | 5.7 | 0.629 |
| Obese | 68 | 95.8% | 32 | 97.0% | 36 | 94.7% | 0.641 |
| Regular Physical Activity in past 6 months? (%Yes) | 36 | 50.7% | 16 | 48.5% | 20 | 52.6% | 0.727 |
| Currently Physical Activity (%Yes) | 42 | 59.2% | 20 | 60.6% | 22 | 57.9% | 0.817 |
| Free time engagement in Physical Activity (%Yes) | 31 | 43.7% | 17 | 51.5% | 14 | 36.8% | 0.214 |
| Intend to engage in regular Physical Activity in next 6 months? (%Yes) | 69 | 97.2% | 32 | 97.0% | 37 | 97.4% | 0.919 |
| Sedentary (>3 hr/day) | 55 | 77.5% | 24 | 72.7% | 31 | 81.6% | 0.373 |
| Intend to eat more fruits and vegetables in the next month? (%Yes) | 69 | 97.2% | 32 | 97.0% | 37 | 97.4% | 0.919 |
Note. BMI = body mass index.
A comparison of the 43 men who completed the final assessment at 6 months and the 28 who did not complete the 6-month final assessment is included in Table 4. Results show that participants who completed the study (M = 61.29, SD = 8.55) were significantly older than those who did not (M = 54.26, SD = 9.18, p = .002). There were no other significant differences in demographics or in the primary outcomes of weight, percent body fat, and waist circumference between completers and noncompleters (p > .17).
Table 4.
Means and Standard Deviations of Weight Loss Condition and Control Condition at Baseline and 6-Month Final Timepoints With Group Differences and 95% Confidence Intervals (CI)
| Measure | N | Baseline | Final (6 months) | Difference between baseline and 6 months | t | p |
|---|---|---|---|---|---|---|
| M (SD) | M (SD) | M [95% CI] | ||||
| Anthropomorphic measures | ||||||
| Weight | ||||||
| Weight loss cond. | 21 | 232.30 (40.92) | 225.16 (46.37) | −7.14 [−11.87, −2.40] | 3.14 | .005 |
| Control cond. | 22 | 238.10 (50.37) | 232.99 (47.95) | −5.11 [−8.48, −1.75] | 3.16 | .005 |
| Total | 43 | 235.27 (45.55) | 229.16 (46.79) | −6.10 [−8.88, −3.33] | 4.44 | <.001 |
| Body fat a | ||||||
| Weight loss cond. | 21 | 32.76 (5.83) | 30.39 (7.55) | −2.37 [−3.92, −0.82] | 3.19 | .005 |
| Control cond. | 22 | 31.43 (7.84) | 31.25 (6.81) | −0.18 [−1.25, 0.88] | 0.36 | 0.726 |
| Total | 43 | 32.08 (6.88) | 30.83 (7.11) | −1.25 [−2.21, −0.30] | 2.64 | 0.012 |
| Waist circumference | ||||||
| Weight loss cond. | 21 | 44.98 (4.48) | 44.26 (5.80) | −0.71 [−1.88, 0.45] | 1.28 | 0.217 |
| Control cond. | 21 | 44.38 (6.13) | 43.81 (5.33) | −0.57 [−1.50, 0.36] | 1.29 | 0.213 |
| Total | 42 | 44.68 (5.31) | 44.04 (5.51) | −0.64 [−1.36, 0.07] | 3.14 | 0.076 |
| Biometrics | ||||||
| Blood glucose | ||||||
| Weight loss cond. | 20 | 112.15 (24.99) | 112.80 (27.59) | 0.65 [−13.64, 14.94] | 0.10 | 0.925 |
| Control cond. | 22 | 111.14 (46.28) | 121.27 (60.86) | 10.14 [−2.38, 22.66] | 1.68 | 0.107 |
| Total | 42 | 111.62 (37.23) | 117.24 (47.63) | 5.62 [−3.54, 14.77] | 1.24 | 0.222 |
| Systolic blood pressure a | ||||||
| Weight loss cond. | 21 | 133.76 (18.98) | 138.10 (15.82) | 4.33 [−4.85, 13.52] | 0.98 | 0.337 |
| Control cond. | 22 | 140.55 (13.61) | 129.05 (10.09) | −11.50 [−16.84, −6.16] | 4.48 | <0.001 |
| Total | 43 | 137.23 (16.61) | 133.47 (13.81) | −3.77 [−9.36, 1.83] | 1.36 | 0.181 |
| Diastolic blood pressure | ||||||
| Weight loss cond. | 21 | 82.38 (12.66) | 84.62 (9.58) | 2.24 [−4.69, 9.16] | 0.67 | 0.508 |
| Control cond. | 22 | 87.00 (10.29) | 81.95 (7.38) | −5.05 [−8.49, −1.60] | 3.04 | 0.006 |
| Total | 43 | 84.74 (11.61) | 83.26 (8.53) | −1.49 [−5.31, 2.33] | 0.79 | 0.436 |
| HDL cholesterol | ||||||
| Weight loss cond. | 21 | 44.43 (13.48) | 48.14 (14.04) | 3.71 [−2.8, 10.23] | 1.19 | 0.248 |
| Control cond. | 21 | 51.67 (18.85) | 49.71 (16.89) | −1.95 [−6.16, 2.25] | 0.97 | 0.344 |
| Total | 42 | 48.05 (16.59) | 48.93 (15.36) | 0.88 [−2.93, 4.7] | 0.47 | 0.643 |
| Total cholesterol | ||||||
| Weight loss cond. | 21 | 169.71 (64.37) | 159.57 (46.59) | −10.14 [−22.98, 2.7] | 1.65 | 0.115 |
| Control cond. | 22 | 177.86 (39.69) | 177.64 (29.39) | −0.23 [−17.6, 17.15] | 0.03 | 0.979 |
| Total | 43 | 173.88 (52.7) | 168.81 (39.35) | −5.07 [−15.61, 5.47] | 0.97 | 0.337 |
| Triglycerides | ||||||
| Weight loss cond. | 21 | 160.43 (58.55) | 130.9 (77.26) | −29.52 [−59.47, 0.42] | 2.06 | 0.053 |
| Control cond. | 22 | 183.95(148.48) | 169.77 (140.04) | −14.18 [−70.64, 42.27] | 0.52 | 0.607 |
| Total | 43 | 172.47(113.12) | 150.79 (114.17) | −21.67 [−52.8, 9.45] | 1.41 | 0.167 |
| Pulse rate | ||||||
| Weight loss cond. | 21 | 72.57 (17.53) | 73.27 (13.54) | 0.70 [−4.95, 6.35] | 0.26 | 0.799 |
| Control cond. | 20 | 74.70 (12.50) | 74.05 (9.89) | −0.65 [−5.65, 4.35] | 0.27 | 0.789 |
| Total | 41 | 73.61 (15.14) | 73.65 (11.76) | 0.04 [−3.58, 3.66] | 0.23 | .982 |
| Health behavior | ||||||
| Fruits and vegetables (no fried potatoes) | ||||||
| Weight loss cond. | 23 | 0.62 (0.59) | 0.43 (0.39) | −0.19 [−0.42, 0.04] | 0.73 | .476 |
| Control cond. | 22 | 0.81 (0.83) | 0.71 (0.69) | −0.11 [−0.42, 0.21] | 1.71 | .101 |
| Total | 45 | 0.72 (0.72) | 0.57 (0.57) | −0.15 [−0.34, 0.04] | 1.62 | .113 |
| Fried potatoes | ||||||
| Weight loss cond. | 23 | 0.0154 (0.0350) | 0.0035 (0.0060) | −0.0119 [−0.0271, 0.0033] | 1.63 | .117 |
| Control cond. | 21 | 0.0046 (0.0103) | 0.0019 (0.0048) | −0.0027 [−0.0075, 0.0021] | 1.16 | .258 |
| Total | 44 | 0.0103 (0.0266) | 0.0027 (0.0055) | −0.0075 [−0.0156, 0.0006] | 1.88 | .067 |
| Physical activity (moderate+ vigorous MET) | ||||||
| Weight loss cond. | 16 | 1,912.50 (1,475.87) | 3,506.25 (2,769.29) | 1,593.75 [256.53, 2,930.97] | 2.54 | .023 |
| Control cond. | 19 | 3,650.53 (3,583.31) | 3,315.79 (3,374.96) | −334.74 [−1,947.37, 1,277.90] | 0.44 | .668 |
| Total | 35 | 2,856.00 (2,920.68) | 3,402.86 (3,069.66) | 546.86 [−520.52, 1,614.23] | 1.04 | .305 |
Note. Out-of-range readings: HDL cholesterol had 2 readings <15 at baseline which were assigned values of 14. Total cholesterol had 4 readings <100 at baseline and 3 readings <100 at 6 months which were assigned values of 99. Triglycerides had one reading of >650 at baseline which was assigned a value of 651 and two readings <45 at 6 months which were assigned values of 44. Sensitivity analysis of HDL cholesterol, triglycerides, and cholesterol (comparison group only) with these values removed showed the same pattern of significance. Total cholesterol for the intervention group showed a significant decrease when these values were removed (baseline: M = 186.12, SD = 60.64; 6 months: M = 170.94, SD = 44.21; N = 17, t = 2.20, p = .043) due to two participants with <100 readings at baseline showing substantial increases at 6-months. HDL = high-density lipoprotein; MET = metabolic equivalent.
Significant Time × Group interactions for body fat: F(1,41)=5.97, p = .019 and systolic BP: F(1,41)=9.87, p = .003. Significant change over time shown in bold.
We completed a survey at 9 months, post-baseline that included 32 men: 18 intervention and 14 control. This survey was to collect selected data about the maintenance of behaviors 3 months after the completion of the intervention. Unfortunately, we did not collect demographic data during the 9-month assessment.
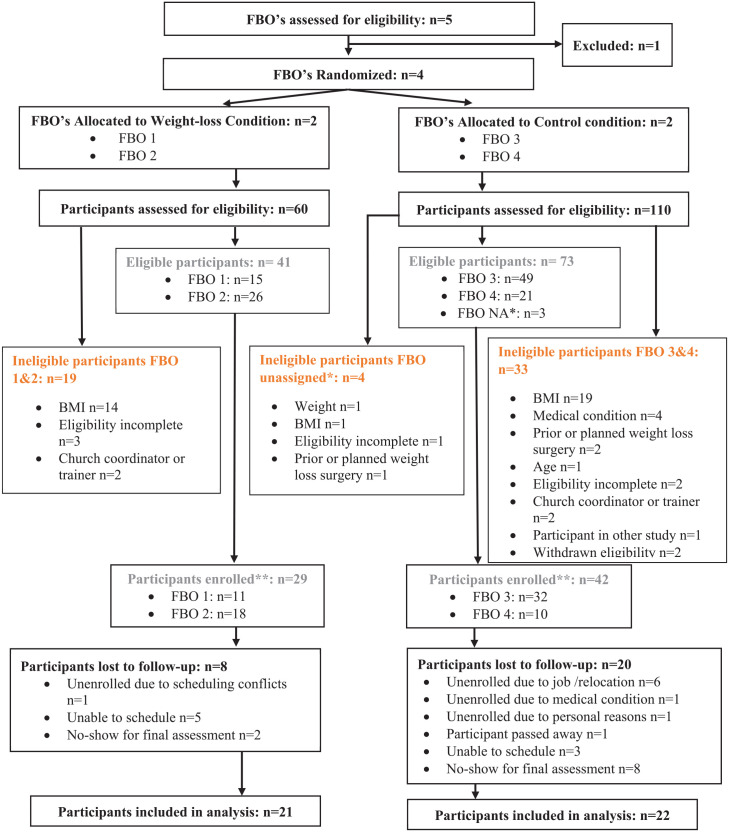
Acceptability and Feasibility
Figure 1 documents participant flow and cluster flow through the eligibility and enrollment process of this intervention as outlined by the CONSORT statement (Montgomery et al., 2013). Based on responses to evaluation survey questions and informal follow-up conversations, churches and participants were receptive to all intervention components, and we successfully completed the 6-month study. However, given the length of the intervention and the level of commitment involved, the recruitment of participants was a challenge. While we did not capture the number of men approached versus those assessed for eligibility, there was consensus among our team and among our church partners that many men were reluctant to make such a time-intensive commitment, despite understanding the potential long-term benefits.
Figure 1.
Mighty Men Atlanta—Enrollment Flowchart
*Participants from other congregations were allowed to participate at one of the established Mighty Men churches. A few participants were screened but never indicated the church they wished to participate with. All of these individuals were ineligible and they are included in the numbers of the comparison group for reporting purposes.
**Participants who were eligible but not enrolled were primarily unable to be contacted after eligibility screening for baseline scheduling or did not show up to their scheduled baseline assessment time.
Attrition
A total of 71 men completed the baseline assessment and were enrolled in the study (control n = 42; weight loss n = 29). Throughout the study, 10 men were unenrolled from the study due to relocation, scheduling conflicts and/or job obligations, personal reasons, health issues, and one death of a participant for reasons unrelated to study participation (control n = 9; weight loss n = 1). A total of 46 men completed the midpoint assessment (control n = 23; weight loss n = 23) for a 3-month attrition rate of 35.2% (control = 45.2%; weight loss n = 20.6%), and 43 men completed the final assessment (control = 22; weight loss n = 21) for an attrition rate of 40% (control = 47.6%; weight loss n = 27.6%) at 6 months. Thirty-two men completed a survey at 9 months post-baseline (control = 14; weight loss n = 18) to capture preliminary data on maintenance of behaviors 3 months after the completion of the intervention.
Evaluation of Intervention Components
Participants at intervention churches received text messages regarding meeting reminders, goal-tracking, and tailored motivational messages. Feedback was gathered from participants on this intervention component at the midpoint (n = 23) and final assessments (n = 21). Participants were asked to rate their experience with the SMS text message component of Mighty Men on a scale of 1 to 4, with 1 being Strongly Disagree and 4 being Strongly Agree. Of those who responded at the midpoint assessment, the majority of participants (82.6%) liked receiving the text messages as part of Mighty Men, found the text messages motivating and helpful (65.2%), agreed message timing reinforced topics covered during small group sessions (60.9%), and helped them focus on their goals throughout the week (69.2%). During the final assessment, most participants Strongly Agreed (24%) or Agreed (48%) that the motivational messages were effective and helpful.
Three months into the program, of the 46 men who completed the mid-point assessment, 43 participants (93.48%) self-reported wearing the Fitbit at least 5 days a week. Of the 43 men who completed the 6-month final assessment, 36 (85.71%) participants self-reported wearing the Fitbit at least 5 days a week, and 26 (81.25%) of the 32 men who completed the 9-month survey continued to wear their Fitbit at least 5 days a week 3 months after the program.
Evaluation of Small Group Sessions
Intervention participants were asked seven questions on the midpoint survey (n = 21) and 10 questions on the follow-up survey related to small group session feedback. During the 3-month assessment, all intervention participants surveyed felt they increased their knowledge about their health, and all but one participant agreed they know how to set SMART goals and overcome barriers to those goals. Session topics intervention participants (n=18) found most useful included: Pay attention to what and how much you eat, Go-Slow-Whoa Foods, Setting SMART physical activity goals and defining stress, remaining motivated to maintain an active lifestyle, and What is your “WHY”? At the 6-month final assessment, intervention participants (n = 18) agreed the skills they learned in the small group sessions and the knowledge gained about physical activity and healthy eating helped them maintain their goals. Only 2 participants who answered the follow-up survey did not feel committed to pursuing their physical activity goals after the intervention. All participants surveyed felt committed to pursuing their healthy eating goals. Eleven of the 18 intervention participants who completed the follow-up survey indicated that SMART Goals (61.1%) was the most helpful skill they learned. At 9 months, half of the intervention participants rated Go-Slow-Whoa (50%) and Workout Plans (50%) as particularly helpful skills learned from the small group intervention. One third (33.3%) of the intervention participants noted that one of the most useful skills they learned was the MyPlate session that teaches the “plate method” of using a plate as a rough guide to determine the proportion of vegetables, protein, and carbohydrates men should have in a given meal.
Impact
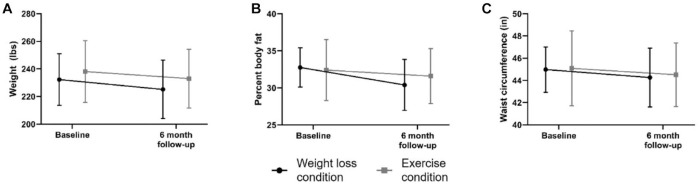
In Table 4, we report baseline and final 6-month means for the anthropomorphic measures (weight, body fat, and waist circumference), biometric measures (blood glucose, systolic blood pressure, diastolic blood pressure, HDL cholesterol, total cholesterol, triglycerides, pulse rate), and health behaviors (fruit and vegetable consumption, fried potato consumption, physical activity moderate + vigorous METS). Using paired-sample t tests, we found significant decreases in weight for both the weight loss condition (M∆ = −7.14, 95% confidence interval, CI = [−11.87, −2.40], t = 3.14, p = .005) and control condition (M∆ = −5.11, 95% CI = [−8.48, −1.75], t = 3.16, p = .005) as well as in the full sample (M∆ = −6.10, 95% CI = [−8.88, −3.33], t = 4.44, p < .001). The weight loss condition participants also had a significant decrease in body fat (M∆ = −2.37, 95% CI = [−3.92, −0.82], t=3.19, p = .012). The raw means are plotted in Figure 2 for the biometric measures of (A) weight, (B) percent body fat, and (C) waist circumference.
Figure 2.
Means and 95% Confidence Intervals of Weight, Percent Body Fat, and Waist Circumference From Baseline to 6 Months
We found no significant changes over time in the weight loss condition participants biometric measures, although the control condition participants did show significant decreases in systolic (M∆ = −11.50, 95% CI = [−16.84, −6.16], t = 4.48, p < .001) and diastolic blood pressure (M∆ = −5.05, 95% CI = [−8.49, −1.60], t = 3.04, p = .006) over time. For health behaviors, we found a significant increase in physical activity (moderate + vigorous METS) between baseline and final (M∆ = 1,593.75, 95% CI = [256.53, 2,930.97], t = 2.54, p = .023) only in the weight loss condition participants. We found no significant changes in fruit and vegetable consumption (excluding fried potatoes) or in fried potato consumption in either group. There were no harms or unintended effects among participants or churches reported in relation to this study.
Discussion
Mighty Men was a pilot acceptability and feasibility effectiveness trial to inform a fully powered intervention to produce weight loss at 6 months in overweight and obese African American men. To our knowledge, this is the first 6-month trial of an intervention designed to achieve weight loss in African American men that included either randomization or individual tailoring of SMS text messaging; this study included both. Our application of individual tailoring built from our qualitative efforts to hear and learn from African American men and to incorporate those findings and lessons in the intervention takes a novel approach Griffith, Jaeger, et al., 2021).
Acceptability was measured based on feedback and evaluation tools related to the use and maintenance of self-monitoring devices, receipt of SMS text messages, the usefulness of the Mighty Men curriculum, and study attrition rate. Feasibility was measured based on study reach, enrollment, and perceived sustainability. Similar to prior research (Dean et al., 2018; Newton et al., 2019), participants found wearing and using the Fitbit Charge 2 device acceptable and feasible as a self-monitoring tool. One of the features of the self-monitoring Fitbit devices that was underutilized was the social connectivity platform to facilitate social support and accountability as well as healthy competition against individuals and groups. In a future iteration of this study, we plan to enhance this aspect of the intervention to see if we can increase the use of the Fitbit platform or some other form of social media to augment the Fitbit platform to promote social connectedness, social support, and accountability. We recognize, however, that with a participant mean age of almost 60 years old, some participants may be less comfortable using or less interested in social connectivity technology. This suggests that continuing to explore ways to conduct in-person interventions for this middle-aged and older age group may be important to continue despite the COVID-19 endemic and advances in technology. Finally, although technology-based social connectivity was underutilized, these middle-aged and older African American men found our individually tailored SMS text messages acceptable. Weight loss condition participants liked how the motivational messages aligned with and reinforced the small-group content.
We had several interruptions for holidays, busy times on the church calendar, and due to project staffing changes; however, interruptions were expected given the length of the program. While program buy-in from church coordinators and leadership varied by site, the investment from the sites did not seem to be associated with either the control condition or the weight loss condition. Unsurprisingly, coordinators and supporters of the program who were more vocal and engaging may have facilitated recruitment, retention, social connectedness, and participation.
Limitations
Despite the success of this acceptability feasibility pilot as the first randomized trial of an individually tailored intervention for African American men, our study had limitations. While our intervention assessments, components, and procedures (i.e., recruitment, randomization, treatment, and assessment) were feasible and acceptable to the sites and to the participants, our control group was not deemed acceptable. The control group served primarily to test our ability to randomize intervention participants, and we explicitly did not compare intervention and control group findings. While we anticipated that we may have more loss to follow-up in the control group when compared with the intervention group, the loss of 45% (45.2%) of control group participants at 3 months and almost half of control group participants at 6 months (47.6%) suggests we need to employ a different comparator for our weight loss condition (Freedland et al., 2019).
Lessons Learned Regarding Acceptability and Feasibility
Overall, it appears that our approach was acceptable and feasible, but it will be important for future iterations of Mighty Men to include a different comparator or a different study design. The control condition components were not enough to keep some men engaged in the study, those control condition participants who remained active in the program and did complete the final assessment lost five pounds from their baseline weight, and had significant decreases in their systolic blood pressure and diastolic blood pressure. Although these intervention components were not selected to achieve equipoise with the weight loss condition (Freedland et al., 2019), our findings did demonstrate that the combination of small group exercise, Fitbit, a Bluetooth-enabled scale, and educational materials was effective in creating and sustaining behavior change for some men. This is an important finding as it suggests that some men are looking for cost-effective and convenient opportunities to exercise while others are looking for more.
In hindsight, we could have provided SMS-text messages and a small group educational curriculum to control group participants to isolate the tailoring components of the study, making this a comparative effectiveness trial (Freedland et al., 2019). Because our goal was primarily to test the acceptability and feasibility of the randomization processes and weight loss intervention, we chose a control group selected with our community/ faith-based partners rather than a comparison group. Because of financial and other resource constraints, we were unable to complete a more comprehensive 9-month assessment of behavior and health-change maintenance. We should have completed a demographic survey at the 9-month point, however. Also, it would have been preferable to use data from Fitbit as an objective measure of physical activity, but there were inconsistencies and gaps across the Fitbit data related to wear/usage among the enrolled men. The Fitbit itself was used more predominately as a measure of self-monitoring for participants. Finally, our study was conducted prior to the COVID-19 pandemic. We recognize that future iterations of this study may have to accommodate churches’ and potential participants’ concerns about potential virus transmission from participants being in such close proximity to one another in an enclosed indoor space.
Conclusion
It is feasible to conduct a randomized, individually tailored weight loss intervention for African American men in a community-based setting that lasts 6 months. The utilization of SMS text messaging and wearable devices (e.g., Fitbit) was also acceptable. Utilizing approaches that continue to apply intersectionality and other concepts that facilitate our ability to increase the salience of interventions to specific population groups will continue to be important.
Footnotes
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was funded by the American Cancer Society (RSG-15-223-01-CPPB) and NIH/NIMHD (5U54MD010722-02).
Trial Registration: This study was registered with ClinicalTrials.gov (Identifier NCT03082157).
ORCID iD: Derek M. Griffith  https://orcid.org/0000-0003-0018-9176
https://orcid.org/0000-0003-0018-9176
References
- Abshire D. A., Wippold G. M., Wilson D. K., Pinto B. M., Probst J. C., Hardin J. W. (2023). A qualitative study of ecological and motivational factors to inform weight management interventions for Black men in the rural South of the United States. Social Science & Medicine, 326, Article 115898. 10.1016/j.socscimed.2023.115898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Cancer Society. (2020). Cancer facts and figures 2020. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/annual-cancer-facts-and-figures/2020/cancer-facts-and-figures-2020.pdf
- American Cancer Society. (2022). Cancer facts & figures for African American/ Black people 2022–2024. https://www.cancer.org/content/dam/cancer-org/research/cancer-facts-and-statistics/cancer-facts-and-figures-for-african-americans/cancer-facts-and-figures-for-african-americans-2019-2021.pdf
- Anderson E. S., Winett R. A., Wojcik J. R. (2007). Self-regulation, self-efficacy, outcome expectations, and social support: Social cognitive theory and nutrition behavior. Annals of Behavioral Medicine, 34(3), 304–312. [DOI] [PubMed] [Google Scholar]
- Aoun S., Osseiran-Moisson R., Shahid S., Howat P., O’Connor M. (2012). Telephone lifestyle coaching: Is it feasible as a behavioural change intervention for men? Journal of Health Psychology, 17(2), 227–236. 10.1177/1359105311413480 [DOI] [PubMed] [Google Scholar]
- Arain M., Campbell M. J., Cooper C. L., Lancaster G. A. (2010). What is a pilot or feasibility study? A review of current practice and editorial policy. BMC Medical Research Methodology, 10(1), Article 67. 10.1186/1471-2288-10-67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arias E., Xu J. (2019). United States life tables, 2017, Volume 68, Number 7 (National vital statistics reports). https://stacks.cdc.gov/view/cdc/79487 [PubMed]
- Armstrong S., Mendelsohn A., Bennett G., Taveras E. M., Kimberg A., Kemper A. R. (2017). Texting motivational interviewing: A randomized controlled trial of motivational interviewing text messages designed to augment childhood obesity treatment. Childhood Obesity, 14(1), 4–10. 10.1089/chi.2017.0089 [DOI] [PubMed] [Google Scholar]
- Armstrong T., Bull F. (2006). Development of the World Health Organization global physical activity questionnaire (GPAQ). Journal of Public Health, 14, 66–70. [Google Scholar]
- Bandura A. (2004). Health promotion by social cognitive means. Health Education & Behavior, 31, 143. 10.1177/1090198104263660 [DOI] [PubMed] [Google Scholar]
- Bastianelli K., Ledin S., Chen J. (2017). Comparing the accuracy of 2 point-of-care lipid testing devices. Journal of Pharmacy Practice, 30(5), 490–497. 10.1177/0897190016651546 [DOI] [PubMed] [Google Scholar]
- Bennett G. G., Foley P., Levine E., Whiteley J., Askew S., Steinberg D. M., Batch B., Greaney M. L., Miranda H., Wroth T. H. (2013). Behavioral treatment for weight gain prevention among black women in primary care practice: A randomized clinical trial. JAMA Internal Medicine, 173(19), 1770–1777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bopp M., Peterson J. A., Webb B. L. (2012). A comprehensive review of faith-based physical activity interventions. American Journal of Lifestyle Medicine, 6(6), 460–478. 10.1177/1559827612439285 [DOI] [Google Scholar]
- Borek A. J., Abraham C., Greaves C. J., Tarrant M. (2018). Group-based diet and physical activity weight-loss interventions: A systematic review and meta-analysis of randomised controlled trials. Applied Psychology: Health and Well-Being, 10(1), 62–86. 10.1111/aphw.12121 [DOI] [PubMed] [Google Scholar]
- Burton W. M., White A. N., Knowlden A. P. (2017). A systematic review of culturally tailored obesity interventions among African American adults. American Journal of Health Education, 48(3), 185–197. 10.1080/19325037.2017.1292876 [DOI] [Google Scholar]
- Carr L. T. B., Bell C., Alick C., Bentley-Edwards K. L. (2022). Responding to health disparities in behavioral weight loss interventions and COVID-19 in Black adults: Recommendations for health equity. Journal of Racial and Ethnic Health Disparities, 9(3), 739–747. 10.1007/s40615-022-01269-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2020). Interactive atlas of heart disease and stroke. Georgia summary statistics. https://nccd.cdc.gov/DHDSPAtlas/reports.aspx?state=GA&themeId=2
- Crane M. M., Jeffery R. W., Sherwood N. E. (2017). Exploring gender differences in a randomized trial of weight loss maintenance. American Journal of Men’s Health, 11(2), 369–375. 10.1177/1557988316681221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czajkowski S. M., Powell L. H., Adler N., Naar-King S., Reynolds K. D., Hunter C. M., Laraia B., Olster D. H., Perna F. M., Peterson J. C. (2015). From ideas to efficacy: The ORBIT model for developing behavioral treatments for chronic diseases. Health Psychology, 34(10), 971–982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis R. E., Resnicow K. (2011). The cultural variance framework for tailoring health messages. In Cho H. (Ed.), Health communication message design: Theory and practice (pp. 115–136). Sage. [Google Scholar]
- Dean D. A., Griffith D. M., McKissic S. A., Cornish E. K., Johnson-Lawrence V. (2018). Men on the move–Nashville: Feasibility and acceptability of a technology-enhanced physical activity pilot intervention for overweight and obese middle and older age African American men. American Journal of Men’s Health, 12(4), 798–811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erinosho T. O., Pinard C. A., Nebeling L. C., Moser R. P., Shaikh A. R., Resnicow K., Oh A. Y., Yaroch A. L. (2015). Development and implementation of the National Cancer Institute’s food attitudes and behaviors survey to assess correlates of fruit and vegetable intake in adults. PLOS ONE, 10(2), Article e0115017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fortier M. S., Williams G. C., Sweet S. N., Patrick H. (2009). Self-determination theory: Process models for health behavior change. In DiClemente R. J., Crosby R. A., Kegler M. (Eds.), Emerging theories in health promotion practice and research: Strategies for improving public health (Vol. 2, pp. 157–183). Jossey-Bass. [Google Scholar]
- Freedland K. E. (2020). Purpose-guided trial design in health-related behavioral intervention research. Health Psychology, 39(6), 539–548. https://psycnet.apa.org/doi/10.1037/hea0000867 [DOI] [PubMed] [Google Scholar]
- Freedland K. E., King A. C., Ambrosius W. T., Mayo-Wilson E., Mohr D. C., Czajkowski S. M., Thabane L., Collins L. M., Rebok G. W., Treweek S. P., Cook T. D., Edinger J. D., Stoney C. M., Campo R. A., Young-Hyman D., Riley W. T. (2019). The selection of comparators for randomized controlled trials of health-related behavioral interventions: Recommendations of an NIH expert panel. Journal of Clinical Epidemiology, 110, 74–81. 10.1016/j.jclinepi.2019.02.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fryar C. D., Carroll M. D., Afful J. (2020). Prevalence of overweight, obesity, and severe obesity among adults aged 20 and over: United States, 1960–1962 through 2017–2018 (NCHS Health E-Stats). https://www.cdc.gov/nchs/data/hestat/obesity-adult-17-18/obesity-adult.htm
- Greaney M., Quintiliani L., Warner E., King D., Emmons K., Colditz G., Glasgow R., Bennett G. (2009). Weight management among patients at community health centers: The “Be Fit, Be Well” study. Obesity and Weight Management, 5(5), 222–228. [Google Scholar]
- Griffith D. M. (2018). “Centering the margins”: Moving equity to the center of men’s health research. American Journal of Men’s Health, 12(5), 1317–1327. 10.1177/1557988318773973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffith D. M. (2020). Achieving men’s health equity. In Smalley K. B., Warren J. C., Fernández M. I. (Eds.), Health equity: A solutions-focused approach (pp. 197–215). Springer Publishing Company. 10.1891/9780826177247.0011 [DOI] [Google Scholar]
- Griffith D. M., Bergner E., Cornish E. K., McQueen C. M. (2018). Physical activity interventions with African American or Latino men: A Systematic Review. American Journal of Men’s Health, 12, 1102–1117. 10.1177/1557988318763647 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffith D. M., Citrin T., Jerome N. W., Bayer I., Mebane E. (2009). The origins and overview of the WK Kellogg community health scholars program. Progress in Community Health Partnerships: Research, Education, and Action, 3(4), 335–348. [DOI] [PubMed] [Google Scholar]
- Griffith D. M., Cornish E. K. (2018). “What defines a man?”: Perspectives of African American men on the components and consequences of manhood. Psychology of Men & Masculinity, 19(1), 78–88. https://psycnet.apa.org/doi/10.1037/men0000083 [Google Scholar]
- Griffith D. M., Holliday C. S., Enyia O. K., Ellison J. M., Jaeger E. C. (2021). Using syndemics and intersectionality to explain the disproportionate COVID-19 mortality among Black men. Public Health Reports, 136(5), 523–531. 10.1177/00333549211026799 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffith D. M., Jaeger E. C. (2020). Chapter Nine—Mighty men: A faith-based weight loss intervention to reduce cancer risk in African American men. In Ford M. E., Esnaola N. F., Salley J. D. (Eds.), Advances in cancer research (Vol. 146, pp. 189–217). Academic Press. 10.1016/bs.acr.2020.01.010 [DOI] [PubMed] [Google Scholar]
- Griffith D. M., Jaeger E. C., Semlow A. R., Ellison J. M., Bergner E. M., Stewart E. C. (2021). Individually tailoring messages to promote African American men’s health. Health Communication, 37(9), 1147–1156. 10.1080/10410236.2021.1913837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffith D. M., Metzl J. M., Gunter K. (2011). Considering intersections of race and gender in interventions that address U.S. men’s health disparities. Public Health, 125(7), 417–423. 10.1016/j.puhe.2011.04.014 [DOI] [PubMed] [Google Scholar]
- Griffith D. M., Pennings J. S., Bruce M. A., Ayers G. D. (2019). Measuring the dimensions of African American manhood: A factor analysis. In Griffith D. M., Bruce M. A., Thorpe, Jr. R. J. (Eds.), Men’s health equity (pp. 101–126). Routledge. [Google Scholar]
- Hales C. M., Fryar C. D., Carroll M. D., Freedman D. S., Ogden C. L. (2018). Trends in obesity and severe obesity prevalence in us youth and adults by sex and age, 2007–2008 to 2015–2016. JAMA, 319, 1723–1725. 10.1001/jama.2018.3060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkins R. P., Kreuter M., Resnicow K., Fishbein M., Dijkstra A. (2008). Understanding tailoring in communicating about health. Health Education Research, 23(3), 454–466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herring S. J., Cruice J. F., Bennett G. G., Darden N., Wallen J. J., Rose M. Z., Davey A., Foster G. D. (2017). Intervening during and after pregnancy to prevent weight retention among African American women. Preventive Medicine Reports, 7, 119–123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herring S. J., Cruice J. F., Bennett G. G., Rose M. Z., Davey A., Foster G. D. (2016). Preventing excessive gestational weight gain among African American women: A randomized clinical trial. Obesity, 24(1), 30–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrmann S. D., Heumann K. J., Der Ananian C. A., Ainsworth B. E. (2013). Validity and reliability of the Global Physical Activity Questionnaire (GPAQ). Measurement in Physical Education and Exercise Science, 17(3), 221–235. [Google Scholar]
- Israel B. A., McLeroy K. R. (1985). Social networks and social support: Implications for health education. Introduction. Health Education Quarterly, 12(1), 1–4. [DOI] [PubMed] [Google Scholar]
- Joseph J. J., Nolan T. S., Williams A., McKoy A., Zhao S., Aboagye-Mensah E., Kluwe B., Odei J. B., Brock G., Lavender D., Gregory J., Gray D. M. (2022). Improving cardiovascular health in black men through a 24-week community-based team lifestyle change intervention: The black impact pilot study. American Journal of Preventive Cardiology, 9, Article 100315. 10.1016/j.ajpc.2022.100315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- King D. E., Mainous A. G., III, Geesey M. E. (2007). Turning back the clock: Adopting a healthy lifestyle in middle age. The American Journal of Medicine, 120(7), 598–603. [DOI] [PubMed] [Google Scholar]
- Kreuter M. W., Strecher V. J., Glassman B. (1999). One size does not fit all: The case for tailoring print materials. Annals of Behavioral Medicine, 21(4), 276–283. http://mgetit.lib.umich.edu/sfx_local?sid=google [DOI] [PubMed] [Google Scholar]
- Lancaster K. J., Carter-Edwards L., Grilo S., Shen C., Schoenthaler A. M. (2014). Obesity interventions in African American faith-based organizations: A systematic review. Obesity Reviews, 15, 159–176. 10.1111/obr.12207 [DOI] [PubMed] [Google Scholar]
- Latimer A. E., Brawley L. R., Bassett R. L. (2010). A systematic review of three approaches for constructing physical activity messages: What messages work and what improvements are needed? International Journal of Behavioral Nutrition and Physical Activity, 7(1), Article 36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowe D. A., Wu N., Rohdin-Bibby L., Moore A. H., Kelly N., Liu Y. E., Philip E., Vittinghoff E., Heymsfield S. B., Olgin J. E., Shepherd J. A., Weiss E. J. (2020). Effects of time-restricted eating on weight loss and other metabolic parameters in women and men with overweight and obesity: The TREAT randomized clinical trial. JAMA Internal Medicine, 180(11), 1491–1499. 10.1001/jamainternmed.2020.4153 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McLeroy K. R., Bibeau D., Steckler A., Glanz K. (1988). An ecological perspective on health promotion programs. Health Education Quarterly, 15(4), 351–377. [DOI] [PubMed] [Google Scholar]
- Montgomery P., Grant S., Hopewell S., Macdonald G., Moher D., Michie S., Mayo-Wilson E. (2013). Protocol for CONSORT-SPI: An extension for social and psychological interventions. Implementation Science, 8(1), 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Cancer Institute. (2018). Incidence rate report for Georgia by county. https://www.statecancerprofiles.cancer.gov/incidencerates/index.php?stateFIPS=13&areatype=county&cancer=001&race=02&sex=1&age=136&stage=999&year=0&type=incd&sortVariableName=rate&sortOrder=default&output=0#results
- National Center for Complementary and Integrative Health. (2022). Pilot studies: Common uses and misuses. https://www.nccih.nih.gov/grants/pilot-studies-common-uses-and-misuses
- Newton R. L., Jr., Carter L., Romain J. S., Jerrod T., Griffith D. M., Myers V. (2019). Development of a mobile phone app to maintain physical activity in African American men: MobileMen. Mhealth, 5, Article 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newton R. L., Jr., Griffith D., Kearney W., Bennett G. (2014). A systematic review of weight loss, physical activity and dietary interventions involving A frican A merican men. Obesity Reviews, 15, 93–106. [DOI] [PubMed] [Google Scholar]
- Noar S. M., Harrington N. G., Aldrich R. S. (2009). The role of message tailoring in the development of persuasive health communication messages. Annals of the International Communication Association, 33(1), 73–133. [Google Scholar]
- Perrin A. (2021). Mobile technology and home broadband 2021. Pew Research Center. https://www.pewresearch.org/internet/2021/06/03/mobile-technology-and-home-broadband-2021/ [Google Scholar]
- Porzsolt F., Rocha N. G., Toledo-Arruda A. C., Thomaz T. G., Moraes C., Bessa-Guerra T. R., Leão M., Migowski A., Araujo da, Silva A. R., Weiss C. (2015). Efficacy and effectiveness trials have different goals, use different tools, and generate different messages. Pragmatic and Observational Research, 6, 47–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell K. E., King A. C., Buchner D. M., Campbell W. W., DiPietro L., Erickson K. I., Hillman C. H., Jakicic J. M., Janz K. F., Katzmarzyk P. T. (2018). The scientific foundation for the physical activity guidelines for Americans. Journal of Physical Activity and Health, 16(1), 1–11. [DOI] [PubMed] [Google Scholar]
- Resnicow K., Campbell M. K., Carr C., McCarty F., Wang T., Periasamy S., Rahotep S., Doyle C., Williams A., Stables G. (2004). Body and soul. A dietary intervention conducted through African-American churches. American Journal of Preventive Medicine, 27(2), 97–105. http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=15261895 [DOI] [PubMed] [Google Scholar]
- Resnicow K., Jackson A., Blissett D., Wang T., McCarty F., Rahotep S., Periasamy S. (2005). Results of the healthy body healthy spirit trial. Health Psychology, 24(4), 339–348. http://mgetit.lib.umich.edu/sfx_local?sid=google [DOI] [PubMed] [Google Scholar]
- Resnicow K., Jackson A., Braithwaite R., DiIorio C., Blisset D., Rahotep S., Periasamy S. (2002). Healthy body/healthy spirit: A church-based nutrition and physical activity intervention. Health Education Research, 17(5), 562–573. http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=12408201 [DOI] [PubMed] [Google Scholar]
- Resnicow K., Teixeira P. J., Williams G. C. (2017). Efficient allocation of public health and behavior change resources: The “difficulty by motivation” matrix. American Journal of Public Health, 107(1), 55–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson C., Avenell A., Boachie C., Stewart F., Archibald D., Douglas F., Hoddinott P., van Teijlingen E., Boyers D. (2016). Should weight loss and maintenance programmes be designed differently for men? A systematic review of long-term randomised controlled trials presenting data for men and women: The ROMEO project. Obesity Research & Clinical Practice, 10(1), 70–84. 10.1016/j.orcp.2015.04.005 [DOI] [PubMed] [Google Scholar]
- Robertson C., Avenell A., Stewart F., Archibald D., Douglas F., Hoddinott P., Van Teijlingen E., Boyers D. (2017). Clinical effectiveness of weight loss and weight maintenance interventions for men: A systematic review of Men-Only randomized controlled trials (the ROMEO project). American Journal of Men’s Health, 11(4), 1096–1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross R., Neeland I. J., Yamashita S., Shai I., Seidell J., Magni P., Santos R. D., Arsenault B., Cuevas A., Hu F. B., Griffin B. A., Zambon A., Barter P., Fruchart J.-C., Eckel R. H., Matsuzawa Y., Després J.-P. (2020). Waist circumference as a vital sign in clinical practice: A Consensus Statement from the IAS and ICCR Working Group on Visceral Obesity. Nature Reviews Endocrinology, 16(3), 177–189. 10.1038/s41574-019-0310-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ryan R. M., Deci E. L. (2000). Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. American Psychologist, 55(1), 68–78. http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=11392867 [DOI] [PubMed] [Google Scholar]
- Schubart J. R., Stuckey H. L., Ganeshamoorthy M. A., Sciamanna C. N. (2011). Chronic health conditions and internet behavioral interventions: A review of factors to enhance user engagement. Computers, Informatics, Nursing: CIN, 29(2), 81–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanita Corporation. (2020). Tanita InnerScan Pro RD-545Pro. https://www.tanita.com/data/Manuals/RD-545PRO_Manual.pdf?rev=E291
- United States Census Bureau. (2022). QuickFacts. https://www.census.gov/quickfacts/atlantacitygeorgia#qf-headnote-a
- United States Preventive Services Task Force. (2018). Behavioral weight loss interventions to prevent obesity-related morbidity and mortality in adults: US preventive services task force recommendation statement. JAMA, 320(11), 1163–1171. 10.1001/jama.2018.13022 [DOI] [PubMed] [Google Scholar]
- Whitt-Glover M. C., Keith N. R., Ceaser T. G., Virgil K., Ledford L., Hasson R. E. (2014). A systematic review of physical activity interventions among African American adults: Evidence from 2009 to 2013. Obesity Reviews, 15, 125–145. 10.1111/obr.12205 [DOI] [PubMed] [Google Scholar]
- Whitt-Glover M. C., Kumanyika S. K. (2009). Systematic review of interventions to increase physical activity and physical fitness in African-Americans. American Journal of Health Promotion, 23(6), S33–S56. 10.4278/ajhp.070924101 [DOI] [PubMed] [Google Scholar]
- Whitt-Glover M. C., Nwaokelemeh O., Price A. A., Hopkins J. M. (2017). Physical activity among African Americans. In Bopp M. (Ed.), Physical activity in diverse populations (pp. 45–61). Routledge. [Google Scholar]
- Yaroch A. L., Tooze J., Thompson F. E., Blanck H. M., Thompson O. M., Colón-Ramos U., . . .Nebeling L. C. (2012). Evaluation of three short dietary instruments to assess fruit and vegetable intake: The National Cancer Institute’s food attitudes and behaviors survey. Journal of the Academy of Nutrition and Dietetics, 112(10), 1570–1577. [DOI] [PMC free article] [PubMed] [Google Scholar]