Abstract
Scar endometriosis is a rare form of endometriosis characterized by the presence of endometrial tissue in the abdominal wall following a cesarean delivery. We present a case report of a 38-year-old female with scar endometriosis and provide a comprehensive review of the literature on its clinical management. The patient presented with intermittent pain and swelling at the site of her previous cesarean section scar. Imaging studies revealed a nodular lesion with characteristic features of scar endometriosis. Fine needle aspiration cytology confirmed the diagnosis, ruling out malignancy. The patient underwent wide surgical resection of the mass, resulting in the resolution of symptoms and no recurrence during follow-up. Our case highlights the diagnostic challenge of scar endometriosis, which can mimic carcinoma, and emphasizes the importance of a multidisciplinary approach involving clinical evaluation, imaging, and histopathological examination for accurate diagnosis and optimal management of this condition.
Keywords: Endometriosis, scar, radiology, gynaecology
Introduction
Endometriosis is a hormone-dependent disorder characterized by the presence of the endometrial gland and stroma outside the normal uterine cavity. 1 It may involve the pelvic organ like the ovary and pelvic peritoneum or the extra pelvic organ like the lung, brain, bowel, and abdominal wall. 2 Scar endometriosis is the most common type of abdominal wall endometriosis, which most commonly occurs following the caesarian delivery of the baby likely due to implantation of the endometrial tissue at the incision site. The endometrial tissue then remains viable and proliferates with the cyclical hormonal aid. 1 Scar endometriosis is rare with an incidence of 0.03%–0.45% and very few cases of malignant transformation are noted. 2 In this article, we present this case report along with a comprehensive review of the existing literature on scar endometriosis and its clinical management.
Case presentation
A 38-year-old female presented with intermittent pain in the lower mid-abdomen, which coincided with her menstrual cycle. She also noticed a swelling at the site of her previous cesarean section scar. Upon reviewing her medical history, it was found that she had undergone a lower segment cesarean section due to fetal distress. Approximately 1 year after the cesarean section, she began to notice the appearance of a mass at the site of pain.
During the physical examination, a tender nodule measuring approximately 3 × 1.5 cm was palpated. The nodule was located on the left paramedian aspect of the lower anterior pelvic wall. It exhibited a hard consistency and immobility, seeming to be fixed to the underlying muscle. Although the overlying skin appeared elevated, there were no apparent color changes or presence of any sinus tracts.
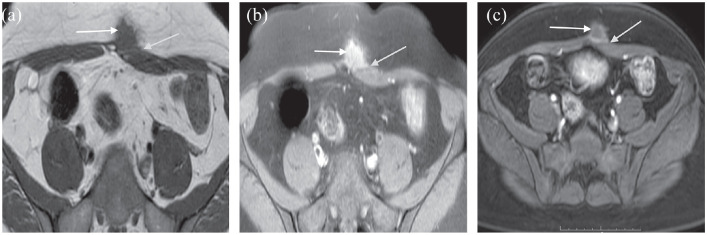
Ultrasound examination showed a heterogeneously hypoechoic irregular nodular lesion in the subcutaneous plane without significantly increased vascularity (Figure 1). The lesion showed T1 low, T2 intermediate, and fat-saturated high signals in MR images (Figure 2(a) and (b)). The lesion shows heterogenous enhancement in post-contrast images and is inseparable from the rectus sheath and rectus abdominis (Figure 2(c)).
Figure 1.

Ultrasound image of the midline lower anterior abdominal wall showing nodular hetero-echoic irregular mass (white arrow) in the subcutaneous plane.
Figure 2.
(a) Axial T1 weighted MRI image showing low signal intensity poorly marginated irregular nodular lesion (white arrow) inseparable from left rectus abdominis and rectus sheath (green arrow). (b) Axial fat-saturated image showing the high signal intensity irregular lesion (white arrow) inseparable from left rectus abdominis and rectus sheath (green arrow). (c) T1 post-contrast axial image showing the irregular nodular lesion (white arrow) showing the heterogenous enhancement and abutting left rectus sheath (green arrow).
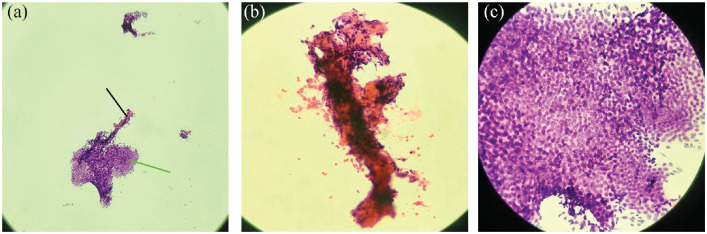
Due to a high degree of suspicion for malignancy, ultrasound-guided fine needle aspiration cytology was performed. The sample was sent for cytopathological examination, revealing clusters of epithelial cells and stromal cells. No suspicious neoplastic cells were identified (Figure 3(a–c)).
Figure 3.
(a) Low power microscopic view showing a cluster of epithelial cells (green line) and aggregate of stromal cells (black line). (b) High-power microscopic view showing the fragment of endometrial stromal cells. (c) High-power microscopic view showing the cluster of endometrial epithelial cells.
Based on these findings, a diagnosis of scar endometriosis was established, and the patient was initially managed conservatively with analgesics and oral contraceptive pills. However, the patient continued to experience persistent pain, and the size of the nodule remained unchanged. Consequently, a decision was made to proceed with wide local excision of the mass. Following the surgical removal of the mass, the patient’s symptoms resolved, and there was no recurrence of the mass.
This case highlights the diagnostic challenge of scar endometriosis, which can mimic carcinoma. By correlating the histopathological findings with the clinical presentation, a proper diagnosis was achieved.
Discussion
Endometriosis is a hormone-dependent disorder characterized by the presence of an endometrial gland and stroma outside the normal uterine cavity. 3 It can affect pelvic organs such as the ovary and pelvic peritoneum, as well as extra pelvic organs including the lung, brain, bowel, and abdominal wall. 4 Scar endometriosis, which commonly occurs following cesarean delivery, is the most prevalent type of abdominal wall endometriosis. This condition arises when endometrial tissue becomes implanted at the incision site and continues growing in response to cyclical hormonal changes. 1 The study carried out by Sengul et al. 5 included three cases of post-cesarean scar endometriosis, and in all instances, there was no recurrence of the nodule following surgical excision.
Scar endometriosis typically presents as a nodule in the lower anterior abdominal wall, accompanied by varying degrees of pain that correlate with the menstrual cycle. 6 Our case aligns with this typical presentation, as the patient experienced severe lower abdominal pain and the presence of a nodular swelling. However, at times, the pain may be noncyclical. Scar endometriosis has several differential diagnoses, including lipoma, granuloma, sebaceous cyst, hematoma, and desmoid tumors. Diagnostic modalities such as ultrasonography (USG), computed tomography, and magnetic resonance imaging (MRI) are used to evaluate the size, location, and volume of the lesion. MRI is particularly preferred for ruling out differential diagnoses. Imaging findings can vary based on the day of the menstrual cycle, the ratio of stromal and glandular elements, the amount of bleeding, and the inflammatory response in peripheral tissue. 7 Although no specific imaging modality has demonstrated high sensitivity in diagnosing scar endometriosis, USG, and MRI have respective sensitivities of approximately 65% and 90%–92% in diagnosing endometrioma. 8
While clinical and imaging findings are often sufficient for making a diagnosis, a biopsy may be necessary in some cases to rule out malignancy. Fine needle aspiration cytology (FNAC) of the mass can be helpful in this regard. Studies reported in the literature by Nigam et al., 9 Pathan et al., 10 and Medeiros et al. 11 have shown 100% sensitivity of FNAC in diagnosing scar endometriosis. FNAC typically reveals glandular epithelial cells, spindle or stromal cells, and hemosiderin-laden macrophages, which aid in the diagnosis. 11 In our case, due to the presence of a nodular mass with irregular margins and low signal intensity on T1-weighted imaging, FNAC of the abdominal wall lesion was advised. The FNAC findings showed clusters, sheets, and fragments of monomorphic cuboidal to columnar epithelial cells and scattered hemosiderin-laden macrophages, suggesting endometriosis.
Surgical resection of the nodule with wide margins is the preferred treatment modality for scar endometriosis, offering the best chance of preventing recurrence. A study by Liang et al. 12 demonstrated a very low risk of recurrence following complete surgical excision. In our case, the patient underwent wide surgical resection, resulting in a significant improvement in her condition. Postoperative follow-up at 6 months revealed no clinical recurrence and normal imaging findings. Postoperative measures such as combined oral contraceptives or hormone suppression with gonadotropin-releasing hormone analogs can be used to reduce the risk of recurrence and prevent new growth. 13 In our patient’s case, only oral contraceptives were prescribed following the surgical removal of the mass. High-intensity focused ultrasound ablation is also an alternative approach to surgery. 14
Conclusion
Scar endometriosis is a rare condition that can resemble a carcinoma, but an accurate diagnosis can be made with a comprehensive diagnostic approach involving clinical, imaging, and histopathological evaluations. Wide surgical resection is the preferred treatment, offering symptom relief and preventing recurrence. Postoperative follow-up and hormonal therapies can further enhance management. Increased awareness among healthcare professionals is essential for early detection and appropriate management. Further research is needed to deepen our understanding of scar endometriosis, including its underlying mechanisms, risk factors, and optimal treatment strategies.
Acknowledgments
None.
Footnotes
Author contribution statement: All authors contributed to the conduct of this research and read and approved the final version of the article. Written informed consent was obtained from the patient party to publish this report by the journal’s “patient consent policy” on the article’s title page.
Data availability: In this case, the data supporting the findings are available upon request to the corresponding author.
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Ethics approval: Our institution does not require ethical approval for reporting individual cases or case series.
Informed consent: Written informed consent was obtained from the patient for her anonymized patient information to be published in this article.
ORCID iDs: Shailendra Katwal  https://orcid.org/0000-0001-7903-8789
https://orcid.org/0000-0001-7903-8789
Sarad Katuwal  https://orcid.org/0000-0002-4130-3329
https://orcid.org/0000-0002-4130-3329
Reference
- 1. Horton JD, Dezee KJ, Ahnfeldt EP, et al. Abdominal wall endometriosis: a surgeon’s perspective and review of 445 cases. Am J Surg 2008; 196(2): 207–212. [DOI] [PubMed] [Google Scholar]
- 2. Sengul D, Sengul I, Soares Junior JM. Caesarean section scar endometriosis: quo vadis? Rev Assoc Medica Bras 2022; 68(1): 1–2. [DOI] [PubMed] [Google Scholar]
- 3. Zhang P, Sun Y, Zhang C, et al. Cesarean scar endometriosis: presentation of 198 cases and literature review. BMC Womens Health 2019; 19(1): 14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Markham SM, Carpenter SE, Rock JA. Extrapelvic endometriosis. Obstet Gynecol Clin North Am 1989; 16(1): 193–219. [PubMed] [Google Scholar]
- 5. Sengul I, Sengul D, Kahyaoglu S, et al. Incisional endometriosis: a report of 3 cases. Can J Surg 2009; 52(5): 444–445. [PMC free article] [PubMed] [Google Scholar]
- 6. Sedhain N, Dangal G, Karki A, et al. Caesarean scar endometriosis. J Nepal Health Res Counc 2017; 15(3): 292–294. [DOI] [PubMed] [Google Scholar]
- 7. Yıldırım D, Tatar C, Doğan O, et al. Post-cesarean scar endometriosis. Turk J Obstet Gynecol 2018; 15(1): 33–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Sachdeva G, Divyashree P, Shailaja N. A non-classical presentation of scar endometriosis during pregnancy: case report and review of literature. JBRA Assist Reprod 2022; 26(3): 563–566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Nigam A, Saxena P, Barla J, et al. Scar endometriosis: the menace of surgery. Case Rep 2014; 2014: bcr2014206693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Pathan ZAAK, Dinesh U, Rao R. Scar endometriosis. J Cytol 2010; 27(3): 106–108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. das Chagas Medeiros F, Cavalcante DIM, da Silva Medeiros MA, et al. Fine-needle aspiration cytology of scar endometriosis: study of seven cases and literature review. Diagn Cytopathol 2011; 39(1): 18–21. [DOI] [PubMed] [Google Scholar]
- 12. Liang CC, Liou B, Tsai CC, et al. Scar endometriosis. Int Surg 1998; 83(1): 69–71. [PubMed] [Google Scholar]
- 13. Pas K, Joanna SM, Renata R, et al. Prospective study concerning 71 cases of caesarean scar endometriosis (CSE). J Obstet Gynaecol 2017; 37(6): 775–778. [DOI] [PubMed] [Google Scholar]
- 14. Xiao-Ying Z, Hua D, Jin-Juan W, et al. Clinical analysis of high-intensity focussed ultrasound ablation for abdominal wall endometriosis: a 4-year experience at a specialty gynecological institution. Int J Hyperthermia 2019; 36(1): 87–94. [DOI] [PubMed] [Google Scholar]