Abstract
Scabies is a contagious skin condition caused by Sarcoptes scabiei, and it is always associated with an intense, unbearable, nocturnal deteriorating itch. Its presentations include classic burrows, erythema, pruritic papules, pustules, vesicles, and inflammatory nodules, with diffuse or localized distribution on the finger webs, wrist flexors, elbows, axillae, buttocks, genitalia, and breasts. Nodular scabies is an uncommon clinical variant of scabies. Its management is still challenging for some patients up to date, although topical, intralesional or systemic corticosteroids, topical calcineurin inhibitors, and crotamiton as well as cryotherapy alone or in different combinations are used. We here report five male patients of nodular scabies, aged between 14 and 25 years, who had classical scabies that had been cured by sulfur ointment for at least 4 weeks except for their itching nodules, and their residual pruritic nodules also failed in previous treatments including antihistamines, topical applying and intralesional injection of steroids as well as topical tacrolimus in different combinations before being recruited to this study. The patients were administered tofacitinib 5 mg, twice a day, which led to excellent and rapid improvement for both lesions and symptoms after 1–4 weeks of treatment, respectively, without any associations. During 6 months of follow-up, only one had re-infection of scabies associated with nodules that were cured by sulfur ointment and tofacitinib again. No adverse reaction was observed. The present results suggested that tofacitinib might be a potential agent for nodular scabies with excellent response.
Keywords: Nodular scabies, recalcitrance, refractory, tofacitinib, treatment
Introduction
Scabies is a contagious skin condition caused by Sarcoptes scabiei.1–8 It is transmitted by direct skin-to-skin contact or indirectly by fomite transmission via clothing or bed sheets.1–4 Its presentations often manifest with classic burrows, erythema, pruritic papules, pustules, vesicles, and inflammatory nodules, with diffuse or localized distribution on the finger webs, wrist flexors, elbows, axillae, buttocks, genitalia, and breasts.1–6,9 In rare instances, lesions similar to bullous pemphigoid, impetigo, psoriasis, urticaria, and dermatitis herpetiformis may present.2,5 The patients always associate with an intense unbearable itch which has a night deterioration.1,2,5 The severe itch and the disruptions of the epidermal barrier may lead to a decrease in life quality and secondary complications.1–3,7,9,10
Nodular scabies (NS), occurring in 7–10% of patients and with male preference, is a well-known variant of scabies characterized by inflammatory, itchy, persistent, coarse, firm round nodules of 5–20 mm in size that often present with red, reddish-brown, or livid in color.2,11 The nodules distribute preferentially on the external genitalia and the groins as well as on the axillae, and may last for months even after classical scabies has been successfully treated.2,11,12 Despite the exact mechanisms that remain not fully known, NS is considered to result from a hypersensitivity reaction of deeper penetration of the scabies mite or antigens. 11 Detection of the scabies parasite in nodular lesions had been previously reported.13,14 Treatment for scabies is not difficult; however, management of NS is challenging sometimes for both the patients and physicians. 11 We herein report five male patients of scabies who had residual recalcitrant nodules after being treated successfully with anti-scabies therapy; however, the nodules showed excellent response to tofacitinib. To our knowledge, no similar description has been reported.
Case descriptions
Each patient must fit that he had classical scabies that had been cured for at least 4 weeks except for the residual lesions of NS before he was recruited for this study. Laboratory evaluations including a complete blood count with differentiation, comprehensive metabolic panel, biochemistries, and screening for human immunodeficiency virus and hepatitis B and C before treatment and during the course were tested for each patient. Before administering tofacitinib treatment, a written informed consent was signed by each patient or the guardian for whom the age was under 18 years. All patients were treated with tofacitinib, 5 mg, twice a day, which is the standard dosing for adults and children weighing more than 40 kg. Each patient had been followed up for at least 6 months before we finished the present submission.
Case 1
An 18-year-old man was referred because of severely pruritic nodules. Three months ago, he had intensely pruritic papules, papulovesicles, and nodules over the finger webs, abdomen, thighs, and genitalia, associated with nocturnal exacerbation of itching. Some of his close contacts had similar lesions. The patient was diagnosed with scabies. The itching and papules responded excellently to topical 10% sulfur ointment alone, twice daily for 3 days, a week apart for two cycles. However, the nodules improved mildly with refractory pruritis that also had poor response to systemic antihistamines, topical tacrolimus, and steroids, as well as intra-nodular injection with prednisolone hereafter. Cutaneous examination revealed multiple discrete brown smooth nodules distributed over the thighs, scrotum, and penis [Figure 1(a)]. He then administered tofacitinib 5 mg, twice daily alone, resulting in evident improvement for the pruritis and nodules on day 3. Two weeks later, most nodules had marked relief [Figure 1(b)]. Then tofacitinib was reduced to 5 mg daily, leading to complete remission for the lesions with hyperpigmentation left behind after another 2 weeks of treatment [Figure 1(c)]. In a 6-month of follow-up, the hyperpigmentation disappeared without lesional recurrence [Figure 1(d)].
Figure 1.
Multiple discrete brown smooth nodules distributed over the penis before the treatment (a), most have marked improvement after 2 weeks of treatment of tofacitinib (b), and only hyperpigmentation left behind after 1-month treatment, (c) and the hyperpigmentation disappears 4 months later (d).
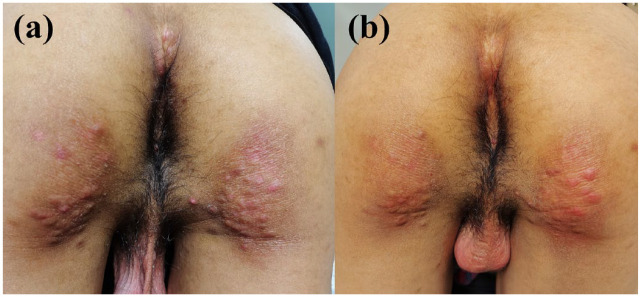
Case 2
A 22-year-old man was referred due to recalcitrant pruritic nodules on his buttocks. Four months ago, the patient presented with intensely pruritic papules and nodules over the lower abdomen, genitalia, and buttocks, the itching had nocturnal exacerbation. He was diagnosed with scabies and administered topical 10% sulfur ointment alone, twice daily for 3 days, 1 week apart for two cycles, which led to excellent remission for the symptoms and signs except for the nodules on the buttocks [Figure 2(a)]. The residual nodules were refractory itching and also showed poor response to systemic antihistamines and steroids as well as topical steroids. Then tofacitinib 5 mg, twice daily, was prescribed, which resulted in evident improvement for the nodules after 1-week treatment [Figure 2(b)]. After 2 weeks of treatment, the lesions were cured with hyperpigmentation left behind. No relapse occurred in a 6-month follow-up.
Figure 2.
Multiple red nodules on the buttocks (a), showing marked improvement after 1 week of treatment with tofacitinib (b).
Case 3
A 24-year-old man was admitted due to intense itchy nodules on the foreskin of his penis. He presented with pruritic papules and nodules on his lower abdomen, thighs, groins, and genitalia associated with nocturnal exacerbation of itching 6 months ago, which was diagnosed as scabies. Three cycles of treatment (a week apart) with topical 10% sulfur cream twice daily for 3 days led to excellent response for the signs and symptoms except for some of the itching nodules over the genitalia. The residual refractory itching nodules also resisted topical and intralesional injection of steroids as well as systemic antihistamines. Then he was administered tofacitinib 5 mg twice daily alone, the itch and nodules showed marked improvement on day 3 and disappeared after 2 weeks of treatment. No recurrence occurred during a follow-up of 6 months.
Case 4
A 14-year-old boy was referred because of 2 months of itching nodules on his scrotum and hips. Two months ago, the patient presented with itching papules and nodules on the webs of fingers, abdomen, genital regions, and hips, and some of his close classmates had similar lesions. He was diagnosed with scabies and was treated with two cycles of topical 10% sulfur ointment, twice daily for 3 days, 1 week apart, which led to excellent response except for some of the pruritic nodules on the scrotum [Figure 3(a)]. Then topical steroid ointment and repeatedly intralesional injection of triamcinolone acetonide were sequentially applied for the nodules, showing mild improvement and rapid recurrence. Therefore, tofacitinib 5 mg twice daily alone was prescribed for a week, showing excellent response with clearance of nodules [Figure 3(b)]. However, re-infection of scabies with association of new itching nodules occurred a month later, the scabies was cured by sulfur ointment while the nodules responded excellently to tofacitinib again. No relapse occurred in another 6 months of following up.
Figure 3.
Multiple red nodules on the scrotum (a), showing clearance of nodules after 1 week of treatment with tofacitinib (b).
Case 5
A 25-year-old man was admitted to our department because of severe itching nodules on the scrotum and foreskin of the penis. Six weeks ago, he was referred because of pruritic papules and nodules on the webs of fingers, abdomen, and genital regions including scrotum and foreskin, that was diagnosed as scabies and was treated with topical 10% sulfur ointment for two cycles. The treatment resulted in a rapid clearance for the papules except for the pruritic nodules on the scrotum and foreskin. Then he administered systemic antihistamines and topical steroids for 4 weeks, showing poor response yet. Hereafter, he administered tofacitinib 5 mg twice daily alone for 2 weeks, resulting in complete clearance for the nodular lesions. No recurrence occurred in 6 months of follow-up.
The patients’ characteristics and response to treatment are summarized in Table 1, and all had no adverse effects during the treatment and the follow-up.
Table 1.
Patients’ characteristics and outcomes of treatment.
| Case number | Gender | Age (Y) | Distribution of nodules | Before tofacitinib treatment | Tofacitinib dosage, course, and response | Adverse effects | Follow-up | |
|---|---|---|---|---|---|---|---|---|
| Duration (Mo) | Prior treatment and response | |||||||
| 1 | M | 18 | Thighs, scrotum, and penis | 3 | Poor to systemic antihistamines, topical tacrolimus and steroids, and intra-nodular injection with prednisolone | 5 mg, bid. Day 3: improved 2 weeks: marked relief 4 weeks: cured |
None | No recurrence during 6 months |
| 2 | M | 22 | Buttocks | 3 | Poor to systemic antihistamines and steroids as well as topical steroids | 5 mg, bid. 1 week: evidently improved. 2 weeks: cured |
None | No recurrence during 6 months |
| 3 | M | 24 | Foreskin of penis | 6 | Poor to topical and intralesional injection of steroids | 5 mg, bid. Day 3, improved. 2 weeks: cured |
None | No recurrence during 6 months |
| 4 | M | 14 | Scrotum and hips | 2 | Mild improvement with rapid recurrence to topical steroid ointment and intralesional injection of triamcinolone acetonide | 5 mg bid. 1 week: cured |
None | Re-infection after 1 month that is re-cured by sulfur ointment and tofacitinib without recurrence during the latter 6 months |
| 5 | M | 25 | Scrotum and foreskin of the penis | 1 | Poor to systemic antihistamines and topical steroids | 5 mg, bid. 2 weeks: cured |
None | No recurrence during 6 months |
M, male; Mo, month; Y, year;
Discussion
Scabies occurs not only in resource-poor regions but also involves people in high-income societies.2,3,6,9,10 It has been demonstrated that NS has a predominant infiltration of eosinophils and lymphocytes as well as mast cells, mimicking that of pseudolymphoma in histopathology.3,7,11 The exact pathomechanisms for scabies itch are not fully understood yet.1,7 Histamine pathway is not thought the main mediator that contributed to the pathomechanism of sarcoptic itch,4,7 although antihistamines have been used for the treatment of such conditions.1,3,4,7,15,16 However, non-histaminergic pathways such as host–mite interaction including both type I and type IV hypersensitivity reaction, and secondary microbial infection and never sensitization are considered to be the main reasons for scabies pruritis.7,11,15 The recent studies from the animal model showed that transient receptor potential vanilloid-1, transient receptor potential ankyrin 1, protease-activated receptor 2, and tryptase+ cells had played important roles in the non-histaminergic itch of scabies. 7 Cytokines including interleukin (IL)-4, IL-13, IL-31, and complement 3a/4a/5a, major basic protein, and eosinophil cationic protein were the important factors for the chronic pruritis of NS, and IL-31 seems to be one of the major factors for its pruritus.1,4,7,8 Moreover, some authors considered that mast cell seems not to be a pruritogenic factor for sarcoptic itch because no significant increase in mast cells was detected in the scabies lesion. 15 However, none of the pathomechanisms for scabies itch has been proven conclusively. We support the opinion that the severe sarcoptic itch might be triggered by multiple and complex immune pathways, and the pruritogens include the direct action of the scabies mite and the immune response toward the mite itself.1,7,8
The strategic treatments for NS and its itch are limited and remain challenging sometimes, which include potent topical, intralesional, and systemic corticosteroids, topical calcineurin inhibitors and crotamiton, cryotherapy, surgical excision of the lesions, and even injection of intralesional botulinum toxin A used alone or in a different combination, showing various response with possibility of recurrence.1,7,11,15,16 The effect of antihistamines for scabies is limited, however, which can be used to improve the patient’s somnus and help alleviate pruritus.1,3,4,7,15,16 In rare instances, the sarcoptic nodules are difficult to eradicate as in the present. Tofacitinib is a selective Janus kinase 1/3 inhibitor and specifically blocks Th1-, Th2- and Th17-associated cytokines and the activation of signal transducer and activator transcription (STAT) families, 17 leading to decreases in the pro-inflammatory type I and II cytokines, including IL-6, IL-7, IL-15, IL-21, interferon alpha (IFN-α), and IFN-β, 7 thus reducing both an inflammatory response and inflammation-induced damage caused by dysregulated activation of the immune system. Tofacitinib has been approved for rheumatoid arthritis, ulcerative colitis, and psoriatic arthritis,17,18 its diverse off-label indications have been reported in more than 20 kinds of diseases including alopecia areata, atopic dermatitis, etc., and the vast majorities showed excellent response with no or mild adverse effects. 18 However, tofacitinib has been reported to increase the risk of infection such as herpes zoster and urinary tract infection, other adverse effects include anemia, leukopenia, gastrointestinal perforation, hyperlipidemia, cardiovascular disease, diarrhea, nasopharyngitis, headache, etc. 19 The present results suggested that tofacitinib is a good potential agent for NS with rapid working and few adverse effects although re-occurrence of NS might occur. The mechanisms for treating NS, we speculated, are that tofacitinib inhibits the type 2 inflammatory cytokines, via suppressing IL-4, IL-13, IL-31, etc., leading to improvement for NS lesions and the pruritus. On the other hand, the daily drug cost of tofacitinib 5 mg, twice a day is about only $50 cents for the Chinese-made agent, suggesting that the domestic drug is a potentially cost-effective agent for the treatment of NS in China. The reason for no adverse effects occurred in this study, we considered, is that only five patients were studied and the treatment course was also short. Because different patients might have different responses to tofacitinib as the present study showed, the dosage and treatment course of tofacitinib might be adjusted based on the response as we had done. If possible, more data should be collected to evaluate an optimal dosage and treatment course in the future study. Based on the published off-label data, we also speculated that tofacitinib might be a potential agent for some inflammatory dermatological conditions, even those that resisted conventional therapies. Of course, further studies are necessary to clarify the efficacy and utility of tofacitinib, as well as its safety and adverse effects.
Veraldi et al. 20 suggested that NS should be distinguished from post-scabietic nodules. The nodules of NS occur accompanied by the typical scabietic lesions and are localized mainly on axillae, buttocks, genitalia, and breasts; however, post-scabietic nodules always occur after successful treatment of scabies, present as nodules but might not distribute over the typical locations of scabies, fail in treatment to specific anti-scabies therapy, and show excellent response to anti-inflammatory agents such as steroids. Those are helpful for the diagnosis.
Conclusion
The present results suggested that tofacitinib might be a potential agent for the treatment of NS, even those who resisted to conventional therapies, showing an excellent and rapid improvement.
Acknowledgments
The authors are indebted to the patients as well as the patient and his parents of case 4 to agree to the present publication.
Footnotes
ORCID iD: Di-Qing Luo  https://orcid.org/0000-0001-7922-344X
https://orcid.org/0000-0001-7922-344X
Contributor Information
Yu-Kun Zhao, Department of Dermatology, The East Division of The First Affiliated Hospital, Sun Yat-sen University, Guangzhou, China.
Jing-Fa Lu, Department of Dermatology, The First Affiliated Hospital of Gannan Medical University, Ganzhou, China.
Juan-Hua Liu, Department of Dermatology, The East Division of The First Affiliated Hospital, Sun Yat-sen University, Guangzhou, China.
Hui-Hui Wu, Department of Dermatology, The East Division of The First Affiliated Hospital, Sun Yat-sen University, Guangzhou, China.
Lu-Li Song, Department of Dermatology, The East Division of The First Affiliated Hospital, Sun Yat-sen University, Guangzhou, China.
Chun-Lei Wan, Department of Dermatology, The First Affiliated Hospital of Gannan Medical University, 23 Qingnian Rd., Ganzhou, Jiangxi Province 341000, China.
Di-Qing Luo, Department of Dermatology, The East Division of The First Affiliated Hospital, Sun Yat-sen University, 183 Huangpu Rd. E., Guangzhou 510700, China.
Declarations
Ethics approval and consent to participate: Informed written consents signed by each of the patient as well as his parents of case 4 were obtained before the treatment. The ethics approval was approved by the Institutional Review Boards of the First Affiliated Hospital, Gannan Medical College, China (No: LLSL-2022061403).
Consent for publication: Written informed consent was obtained from the patients and their parents of case 4 for publication of the case report and any accompanying images. The copies of the written consent are available for review by the Editor-in-Chief of this journal.
Author contributions: Yu-Kun Zhao: Conceptualization; Data curation; Formal analysis; Investigation; Project administration; Resources; Validation; Writing – original draft; Writing – review & editing.
Jing-Fa Lu: Conceptualization; Data curation; Formal analysis; Investigation; Project administration; Visualization; Writing – original draft; Writing – review & editing.
Juan-Hua Liu: Conceptualization; Investigation; Project administration; Resources; Visualization; Writing – original draft.
Hui-Hui Wu: Conceptualization; Formal analysis; Methodology; Resources; Validation; Writing – original draft.
Lu-Li Song: Data curation; Investigation; Project administration; Resources; Visualization; Writing – original draft.
Chun-Lei Wan: Conceptualization; Data curation; Investigation; Methodology; Resources; Supervision; Validation; Writing – original draft; Writing – review & editing.
Di-Qing Luo: Conceptualization; Data curation; Formal analysis; Investigation; Methodology; Project administration; Resources; Supervision; Validation; Visualization; Writing – original draft; Writing – review & editing.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Availability of data and materials: Not applicable.
References
- 1. Ständer S, Ständer S. Itch in scabies-what do we know? Front Med (Lausanne) 2021; 8: 628392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Sunderkötter C, Wohlrab J, Hamm H. Scabies: epidemiology, diagnosis, and treatment. Dtsch Arztebl Int 2021; 118: 695–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Hengge UR, Currie BJ, Jäger G, et al. Scabies: a ubiquitous neglected skin disease. Lancet Infect Dis 2006; 6: 769–779. [DOI] [PubMed] [Google Scholar]
- 4. Jannic A, Bernigaud C, Brenaut E, et al. Scabies itch. Dermatol Clin 2018; 36: 301–308. [DOI] [PubMed] [Google Scholar]
- 5. Luo DQ, Huang MX, Liu JH, et al. Bullous scabies. Am J Trop Med Hyg 2016; 95: 689–693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Gunning K, Kiraly B, Pippitt K. Lice and scabies: treatment update. Am Fam Physician 2019; 99: 635–642. [PubMed] [Google Scholar]
- 7. Kim HS, Hashimoto T, Fischer K, et al. Scabies itch: an update on neuroimmune interactions and novel targets. J Eur Acad Dermatol Venereol 2021; 35: 1765–1776. [DOI] [PubMed] [Google Scholar]
- 8. Hashimoto T, Satoh T, Yokozeki H. Pruritus in ordinary scabies: IL-31 from macrophages induced by overexpression of thymic stromal lymphopoietin and periostin. Allergy 2019; 74: 1727–1737. [DOI] [PubMed] [Google Scholar]
- 9. Arlian LG, Morgan MS. A review of Sarcoptes scabiei: past, present and future. Parasit Vectors 2017; 10: 297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. El-Moamly AA. Scabies as a part of the World Health Organization roadmap for neglected tropical diseases 2021-2030: what we know and what we need to do for global control. Trop Med Health 2021; 49: 64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Manjhi M, Yadav P, Mohan S, et al. A comparative study of topical tacrolimus and topical triamcinolone acetonide in nodular scabies. Dermatol Ther 2020; 33: e13954. [DOI] [PubMed] [Google Scholar]
- 12. Chouela E, Abeldano A, Pellerano G, et al. Diagnosis and treatment of scabies. Am J Clin Dermatol. 2002; 3: 9–18. [DOI] [PubMed] [Google Scholar]
- 13. Czeschik JC, Huptas L, Schadendorf D, et al. Nodular scabies: hypersensitivity reaction or infection? J Dtsch Dermatol Ges 2011; 9: 840–841. [DOI] [PubMed] [Google Scholar]
- 14. Daye M, Temiz SA, Kılınç F. A case of nodular scabies with atypical course. Dermatol Ther 2020; 33: e13317. [DOI] [PubMed] [Google Scholar]
- 15. Sanders KM, Nattkemper LA, Rosen JD, et al. Non-histaminergic itch mediators elevated in the skin of a porcine model of scabies and of human scabies patients. J Invest Dermatol 2019; 139: 971–973. [DOI] [PubMed] [Google Scholar]
- 16. Lu Y, Qi X, Zhou X, et al. Intralesional botulinum toxin A injection for treating nodular scabies. Dermatol Ther 2020; 33: e14163. [DOI] [PubMed] [Google Scholar]
- 17. Traidl S, Freimooser S, Werfel T. Janus kinase inhibitors for the therapy of atopic dermatitis. Allergol Select 2021; 5: 293–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Tegtmeyer K, Zhao J, Maloney NJ, et al. Off-label studies on tofacitinib in dermatology: a review, J Dermatol Treat 2021; 32: 399–409. [DOI] [PubMed] [Google Scholar]
- 19. He Y, Wong AY, Chan EW, et al. Efficacy and safety of tofacitinib in the treatment of rheumatoid arthritis: a systematic review and meta analysis. BMC Musculoskelet Disord 2013; 14: 298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Veraldi S, Esposito L, Pontini P, et al. Nodular scabies versus postscabies prurigo: a critical review of the literature. Ital J Dermatol Venerol 2021; 156(Suppl. 1): 42–43. [DOI] [PubMed] [Google Scholar]