Abstract
Background:
Evidence for the superiority of surgical versus nonsurgical treatment of Rockwood type 3 acromioclavicular joint (ACJ) dislocation is still lacking.
Hypothesis:
It was hypothesized that surgical treatment will outperform nonsurgical treatment.
Study Design:
Randomized controlled trial; Level of evidence, 1.
Methods:
A prospective randomized trial involving 4 study centers was performed from January 1, 2011, to March 31, 2016. A total of 85 patients with acute Rockwood type 3 ACJ dislocations were allocated randomly to receive either nonsurgical or surgical treatment. A total of 70 patients were treated as allocated, and 8 patients made an early crossover from nonsurgical to surgical treatment, leaving 47 patients treated surgically and 31 patients nonsurgically. All patients were followed up longitudinally, including clinical evaluation using the Constant score and standardized radiographic evaluation, with final follow-up after 2 years.
Results:
At no follow-up time point was there a significant difference in Constant score between the surgically and nonsurgically treated patients. Radiographic analysis showed not only an inferior coracoclavicular distance at all follow-up points for surgical treatment but also a higher incidence of posttraumatic osteoarthritis and heterotopic ossifications, without any negative clinical correlation. With regard to complications, 1 patient (3%) in the nonsurgical group underwent secondary surgical ACJ stabilization. The revision rate after surgical treatment was 17% (P < .001). Neither primary horizontal instability nor younger age were associated with inferior clinical outcomes after nonsurgical treatment.
Conclusion:
Surgical treatment of ACJ Rockwood type 3 injuries did not lead to superior functional outcomes. Neither younger age nor horizontal instability were associated with inferior outcomes after nonsurgical treatment. Surgical treatment led to a slower recovery and to higher complication and revision rates.
Registration:
ISRCTN registry (study ID: ISRCTN92265154).
Keywords: acromioclavicular dislocation, functional outcome, Rockwood type 3, skillful neglect, surgery
Injuries to the acromioclavicular joint (ACJ) account for 4% to 17% of all injuries to the shoulder girdle and represent the second most common sports-related injury of the shoulder. 19,22 The incidence is reported between 1.8 and 4.6 per 10,000 person-years, 9,11 leading to approximately 2.4 million ACJ injuries per year worldwide. In 1984, Charles Rockwood 22 introduced a classification system for ACJ dislocations based on the degree of injured ligamentous structures, and the Rockwood system is used widely in clinical practice to determine the appropriate type of treatment. Currently, the consensus is to treat Rockwood type 1 and 2 ACJ injuries conservatively and type 4 to 6 injuries surgically. 5,26 Therapeutic recommendations for type 3 injuries are still under debate. Although recent indications tend toward nonsurgical treatment, 8,25,30 recent systematic reviews and meta-analyses have not presented any level 1 studies of sufficient sample sizes that focused exclusively on type 3 injuries. 15,18,25 These reviews concluded that studies with higher levels of evidence are needed.
The purpose of this study was to conduct a randomized trial comparing nonsurgical and surgical treatment for isolated acute Rockwood type 3 ACJ injuries. The hypothesis was that surgical treatment of type 3 ACJ dislocations will outperform nonsurgical treatment in terms of functional outcome at 2-year follow-up.
Methods
Before starting this prospective, multicenter, interventional randomized trial, the study protocol received ethics committee approval and was registered and published online on the website of the German National Society for Shoulder and Elbow Surgery. In addition, the protocol was registered on the ISRCTN registry (https://www.isrctn.com/). The manuscript was completed according to the CONSORT (Consolidated Standards of Reporting Trials) guidelines for reporting randomized controlled trials (RCTs). All included patients provided written informed consent to participate in the study.
Patient recruitment lasted from January 1, 2011, until March 31, 2016, with final follow-up in March 2018. Four referral centers for shoulder pathologies participated in this study. The study inclusion criteria were (1) presence of an acute (≤3 weeks after trauma) ACJ injury, 13 (2) Rockwood type 3 ACJ dislocation as defined by an increase in the coracoclavicular (CC) distance of 25% to 100% compared with the contralateral side on panorama stress radiograph with a 10-kg load on the hanging arm, and (3) age between 18 and 65 years. Exclusion criteria were (1) patient’s request for reconstruction out of cosmetic purposes; (2) preexisting shoulder- or ACJ-related pathologies of the affected or contralateral shoulder; (3) acute or chronic infections of the involved joint; (4) neurological or musculoskeletal diseases affecting the shoulder including rotator cuff tears; (5) inadequate compliance regarding the need for postoperative immobilization and physiotherapeutic rehabilitation; (6) inability to participate in the regular follow-up; (7) smoking status or abuse of drugs or alcohol; and (8) workers' compensation claims.
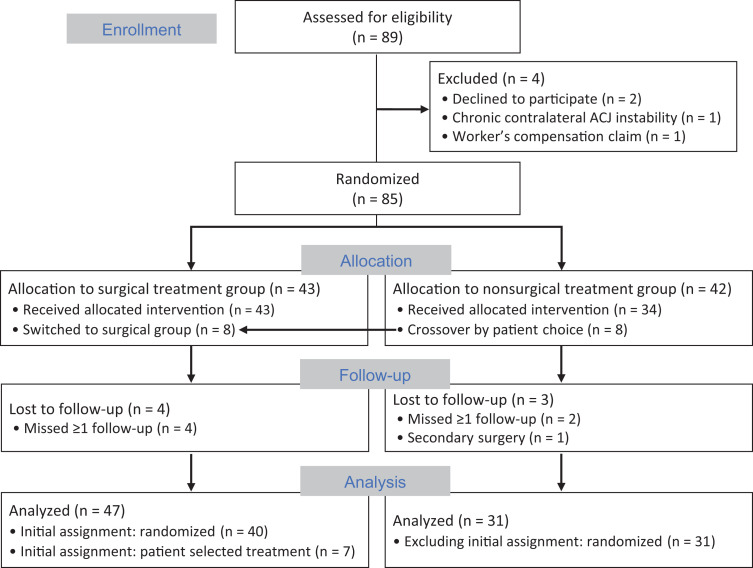
During the study period, 89 patients were recruited, of whom 85 patients were able to be included in the study. A 1-to-1 allocation to either surgical or nonsurgical treatment was performed by the treating surgeon at each center based on a prespecified list generated by the principal investigator using a web-based internet randomizer (https://www.randomize.net/). All 43 patients allocated to the surgical group underwent their treatment per protocol. Of the 42 patients allocated to the nonsurgical group, 8 decided to opt for surgical treatment within 3 weeks after injury. Thus, 85 patients were included: 51 patients in the surgical treatment group and 34 patients in the nonsurgical treatment group. Of these 85 patients, 6 patients were lost to follow-up due to changed contact information without notice, and 1 patient secondarily switched to the surgical group (ACJ reconstruction using a gracilis tendon autograft) 7 months after the injury due to unsatisfying nonsurgical treatment, leaving 78 (92%) patients available for all radiological and clinical analyses: 47 patients in the surgical treatment group and 31 patients in the nonsurgical treatment group (Figure 1).
Figure 1.
CONSORT flow diagram of assignment to the surgical and nonsurgical treatment groups. ACJ, acromioclavicular joint; CONSORT, Consolidated Standards of Reporting Trials.
Treatment Groups
Each of the 4 participating study centers represented 1 of the surgical ACJ stabilization techniques used most frequently according to a survey of trauma and orthopaedic departments in Germany. 3 This approach ensured the surgical generalizability of the comparison between surgical and nonsurgical treatments and the expertise of the participating centers in the respective surgical technique. All surgeries were performed by a single senior shoulder-trained specialist in each center (M.T., L.L., M.S.).
In center 1, a mini-open double TightRope (Arthrex) stabilization was performed in 18 patients and 16 were treated nonsurgically. Center 2 used an arthroscopic double TightRope technique in 12 patients and had 9 patients undergo conservative treatment. Center 3 used the hook plate (DePuy Synthes) for surgical treatment in 11 patients and had 6 patients with nonsurgical treatment, whereas in center 4 an arthroscopic single TightRope device was applied in 10 patients and nonsurgical treatment was performed in 3 patients.
Nonsurgical Treatment
Nonsurgical treatment included adequate pain management using nonsteroidal antirheumatics for several days, accompanied by local ice therapy and immobilization of the injured shoulder using a simple sling. Duration of immobilization was based on the patient’s pain level and lasted between 10 and 14 days. Physical rehabilitation measures were initiated under a physiotherapist’s guidance, performed for 6 to 8 sessions with a frequency of 2 times per week, and continued until full range of motion (ROM) was achieved. The protocol was allowed to be adjusted individually to the pain level of the patient.
Surgical Treatment
All surgeries were conducted after administration of a single dose of intravenous antibiotics with the patient under general anesthesia in the beach-chair position. In the 11 patients in which the hook plate was used, the hook plate was routinely removed after 3 to 6 months to avoid acromial or rotator cuff damage. In all other cases, the TightRope device was used. In 10 cases, it was implanted arthroscopically as a single system. In 12 patients, it was used arthroscopically as a double system, imitating the natural course of the CC ligaments, and in 18 patients a double TightRope system was implanted via a mini-open approach. TightRope implants were removed only if required due to local irritation above the clavicular buttons.
The postoperative protocol was the same for all techniques and included pain management, local ice therapy, and immobilization for 6 weeks in a simple sling. During this period, only passive motion and exercises until 90° of glenohumeral abduction were allowed. Actively assisted shoulder motion in all planes and muscle strengthening followed for the next 6 weeks, with shoulder sports starting after 4 months.
Baseline Evaluation
Clinical examination included inspection and recording of injury signs (eg, hematoma, bruises), local tenderness, and glenohumeral range of motion (ROM). All patients underwent a panorama stress-view radiograph with a 10-kg load on the hanging arm to determine the CC distance in comparison with the contralateral side, as well as bilateral dynamic axillary views 28 or Alexander views to assess horizontal instability. 2 An ultrasound evaluation was performed by a musculoskeletal-trained ultrasound examiner (M.T., L.L., N.K., T.H.) in all patients to exclude rotator cuff injuries.
Clinical Follow-up Evaluation
At 6 weeks postoperatively, general local ACJ pain level on a 10-stage numeric rating scale (NRS; 0 = no pain and 10 = maximum pain) and ROM were assessed. At 3-, 6-, 12-, and 24-month follow-up, outcomes were assessed with the NRS for pain, Constant score, 10 American Shoulder and Elbow Surgeons (ASES) score, 21 the ACJ-specific Taft score, 24 and Acromioclavicular Joint Instability (ACJI) score. 23 The primary outcome measure was the Constant score.
ROM was measured with a goniometer in degrees for forward flexion, abduction, and external rotation. Internal rotation was assessed by determining the spine level the patient could reach with the thumb. Points were accounted to these levels for statistical analysis ranging from 0 to 5 (0 points for leg, 1 point for iliosacral joint, 2 points for L5 vertebra, 3 points for L3 vertebra, 4 points for T12 vertebra, and 5 points for T7 vertebra). Abduction strength measurements were performed using a digital mobile dynamometer (IsoForceControl EVO2, Herkules Kunststoff Oberburg AG) with the arm in the scapular plane at 90° of abduction. Due to the nature of the interventions, no blinding of the participants or observers was possible.
Radiological Follow-up Evaluation
At 3-, 6-, 12-, and 24-month follow-up, a strict radiological protocol was conducted, including panorama views and dynamic functional axillary views or Alexander views. 2,28 At 6-, 12-, and 24-month follow-up, the panorama views were performed under stress with a 10-kg load on the hanging arms. Radiological evaluation was performed by each center and included measurement of the CC distance over time, detection of heterotopic ossifications and identification of posttraumatic ACJ osteoarthritis and/or distal clavicle osteolysis.
Statistical Analysis
We conducted an a priori power analysis based on the Constant score as the primary outcome measure and its minimal clinically important difference of 10.4 points. 17 The calculation was performed with an expected Constant score of 92 ± 16 for surgical treatment (as reported in the literature) and 81.6 for nonsurgical treatment. A continuous endpoint was determined with an alpha value of .05 and a power of 80%. The minimum number of patients required was calculated as 74 patients. A loss to final follow-up of at least 10% was expected, which led to an overall calculated sample size of 85 study patients.
All centers collected data on clinical report forms during the trial, which were later entered into spreadsheets for further analysis. All outcome variables and group characteristics (surgical vs nonsurgical treatment) were tested for normal distribution and were subsequently compared using an unpaired t test (normally distributed data) or a Mann-Whitney U test (nonnormally distributed data) or chi-square test using SPSS Statistics Version 25 (IBM). All tests were 2-tailed, and the threshold value for statistical significance was set to .05.
Due to the very early crossover of patients between groups shortly after allocation, an as-treated analysis was conducted combined with a group comparability assessment. To exclude an important bias due to a broken random assignment, an intention-to-treat versus as-treated analysis was performed in terms of a sensitivity analysis; this analysis showed no significant difference.
Due to the fact that the role of horizontal instability in ACJ injuries is still under debate and the current literature shows weak evidence that persistent horizontal instability is associated with worse clinical outcomes, 4,23 we performed a subanalysis within the nonsurgical treatment group of outcomes according to ISAKOS (International Society of Arthroscopy, Knee Surgery and Orthopaedic Sports Medicine) subclassification of modified Rockwood type 3A and 3B injuries. 6 Type 3A injuries are defined by a stable ACJ without overriding of the clavicle on crossbody adduction radiographic view and without significant scapular dysfunction. Unstable type 3B injuries are further defined by therapy-resistant scapular dysfunction and an overriding clavicle on crossbody adduction/Alexander view. 2 We also performed a subanalysis within the nonsurgical treatment group of outcomes according to age.
Results
Both the surgical and nonsurgical treatment groups showed no significant differences when analyzed using either an intention-to-treat model or an as-treated model (Table 1).
Table 1.
Patient Characteristics According to Intention-to-Treat and As-Treated Models a
| Intention-to-Treat Model | As-Treated Model | |||
|---|---|---|---|---|
| Characteristic | Surgical (n = 39) |
Nonsurgical (n = 39) |
Surgical (n = 47) |
Nonsurgical (n = 31) |
| Age, y | 39.3 ± 13 | 38.4 ± 12 | 40.0 ± 14 | 36.0 ± 14 |
| Male sex | 33 (85%) | 34 (87%) | 40 (85%) | 27 (87%) |
| BMI, kg/m2 | 25.8 ± 2 | 26.0 ± 3 | 25.4 ± 2 | 26.1 ± 2 |
| Dominant side affected | 21 (54%) | 16 (41%) | 24 (51%) | 12 (39%) |
| NRS pain | ||||
| Preoperative | 4.0 ± 3 | 4.3 ± 2 | 4.3 ± 2 | 4.1 ± 2 |
| Postoperative | 0.3 ± 3 | 0.3 ± 2 | 0.4 ± 1 | 0.2 ± 1 |
| Constant score | ||||
| Preoperative | 43.0 ± 13 | 44.2 ± 14 | 41.1 ± 15 | 45.8 ± 13 |
| Postoperative | 92.2 ± 7 | 92.8 ± 5 | 92.8 ± 6 | 92.0 ± 7 |
| ASES score | ||||
| Preoperative | 46.2 ± 14 | 47.6 ± 15 | 47.4 ± 15 | 46.7 ± 13 |
| Postoperative | 96.2 ± 5 | 95.2 ± 4 | 96.5 ± 4 | 96.1 ± 5 |
| Taft score | ||||
| Preoperative | 5.0 ± 1 | 4.9 ± 2 | 4.9 ± 1 | 5.0 ± 2 |
| Postoperative | 11.0 ± 1 | 10.7 ± 1 | 11.2 ± 1 | 10.4 ± 1 |
| ACJI score | ||||
| Preoperative | 30.2 ± 12 | 31.8 ± 14 | 29.3 ± 16 | 32.3 ± 13 |
| Postoperative | 90.8 ± 8 | 84.6 ± 7 | 90.1 ± 8 | 83.2 ± 9 |
| CC distance, mm | ||||
| Injured side | 16.6 ± 3 | 15.8 ± 4 | 17.0 ± 3 | 15.2 ± 3 |
| Uninjured side | 9.7 ± 2 | 9.3 ± 2 | 9.8 ± 2 | 9.1 ± 2 |
| HI (Rockwood type 3B) | 22 (56%) | 20 (51%) | 26 (55%) | 16 (52%) |
a Data are reported as mean ± SD or n (%). There were no significant differences between the groups in either model (P > .05 for all). ACJI, Acromioclavicular Joint Instability; ASES, American Shoulder and Elbow Surgeons; BMI, body mass index; CC, coracoclavicular distance; HI, horizontal instability; NRS, numeric rating scale.
Clinical Outcomes
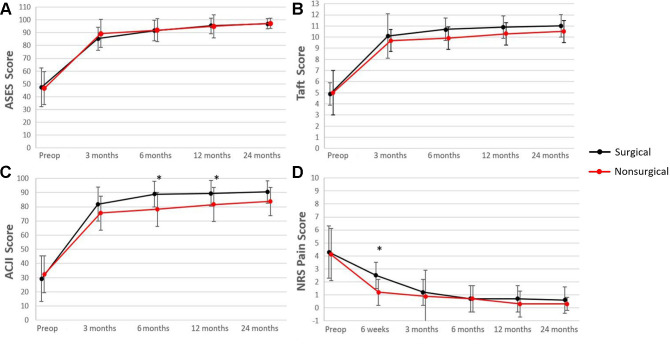
Regarding the primary outcome measure, at no follow-up time point was the Constant score significantly different between the surgical and nonsurgical treatment groups (Figure 2). The nonsurgically treated patients had a significantly faster recovery of ROM within the first 6 postoperative weeks compared with the surgically treated patients (P = .014) (Figure 3).
Figure 2.
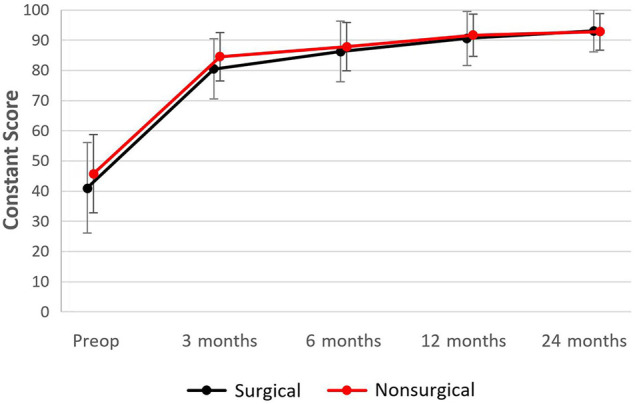
Longitudinal comparison of Constant score (primary outcome measure) between the surgical and nonsurgical treatment groups at different time points. Error bars represent standard deviation. Preop, preoperatively.
Figure 3.
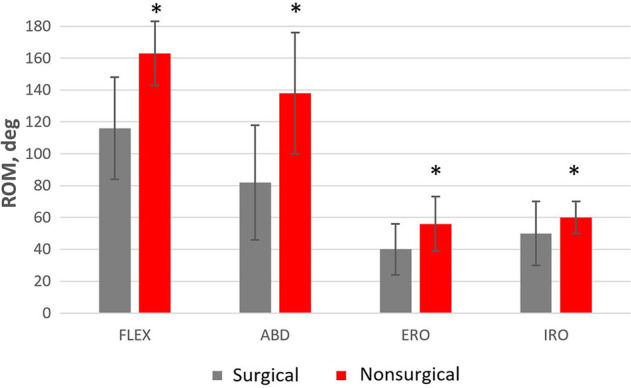
At 6-week follow-up, significantly superior ROM was seen in the nonsurgical treatment group on all ROM planes. Error bars represent standard deviation. *Statistically significant difference between groups (P < .05). ABD, abduction; ERO, external rotation; FLEX, flexion; IRO, internal rotation; ROM, range of motion.
There were no significant differences regarding the secondary outcome measurements including the ASES, Taft, and ACJI scores, as well as pain, at any follow-up time point except for a lower pain score in the nonsurgical treatment group after 6 weeks (P = .01) and a higher ACJI score in the surgical treatment group after 6 and 12 months (P = .023 and .037, respectively) (Figure 4).
Figure 4.
Longitudinal comparison of secondary outcome measurements between surgical and nonsurgical treatment groups at different time points: (A) ASES score, (B) Taft score, (C) ACJI score, and (D) NRS pain score. Error bars represent standard deviation. *Statistically significant difference between groups (P < .05). ACJI, Acromioclavicular Joint Instability; ASES, American Shoulder and Elbow Surgeons; NRS, numeric rating scale; Preop, preoperative.
When comparing the 4 different surgical techniques within the surgical treatment group, no significant difference at final follow-up time point was found, with a certain negative trend for the arthroscopic single TightRope technique. In fact, this surgical technique was stopped after 2 years due to a significantly higher early loss of reduction rate within the first 6 weeks. Clinical outcomes did not differ from the other surgical techniques, which was the reason to include this technique in the final analysis without risk for a relevant bias. Cosmetic intergroup comparison in terms of protrusion of the distal clavicular end was performed according to the subcategories evaluated by the ACJI score, where subjective and objective assessments of the reduction appearance were recorded. Neither subjective (by the patient) nor objective (by the examiner) assessment of the cosmetic outcome showed significant difference at final follow-up.
Subgroup Analysis of Nonsurgical Treatment Group
Of the 31 patients in the nonsurgical treatment group, 16 (52%) had a type 3A injury and 15 (48%) had a type 3B injury. No difference was found between these subgroups regarding pain level or clinical outcome scores at final follow-up (Table 2). The subanalysis according to patient age did not reveal a difference in Constant score between patients younger versus older than 35 years (Table 3).
Table 2.
Comparison of Outcomes in the Nonsurgical Group Between Patients with Rockwood Type 3A vs 3B a
| Outcome Measure | Type 3A (n = 16) |
Type 3B (n = 15) |
P |
|---|---|---|---|
| NRS pain | 0.3 ± 0.6 | 0.2 ± 0.4 | .73 |
| Constant score | 92.1 ± 5.4 | 93.3 ± 5.7 | .82 |
| ASES score | 97.3 ± 4.2 | 97.6 ± 2.7 | .92 |
| Taft score | 10.3 ± 1.0 | 10.6 ± 0.7 | .88 |
| ACJI score | 84.7 ± 10.0 | 82.6 ± 10.1 | .77 |
a Data are reported as mean ± SD. ASES, American Shoulder and Elbow Surgery, ACJI, Acromioclavicular Joint Instability; NRS, numeric rating scale.
Table 3.
Comparison of Outcomes in the Nonsurgical Group Between Patients Aged <35 years vs >35 years a
| Outcome Measure | Age <35 years (n = 17) |
Age >35 years (n = 14) |
P |
|---|---|---|---|
| Constant score | 94.1 ± 4.5 | 92.8 ± 5.2 | .81 |
a Data are reported as mean ± SD.
Radiological Outcomes
With surgical treatment the CC distance was able to be reduced, with minimal loss of reduction over time (Figure 5). Interestingly, even after nonsurgical treatment, the CC distance decreased by 8% over time, which was statistically nonsignificant. However, CC distance differed significantly between groups at every follow-up time point in favor of the surgical treatment group. Heterotopic ossifications along the CC ligament complex were present in 26 cases (55%) after surgical treatment and in 4 cases (12.9%) after nonsurgical treatment (P = .001). No influence of heterotopic ossifications on clinical outcomes was observed. Posttraumatic ACJ osteoarthritis or distal clavicle osteolysis was observed in 8 patients (17%) after surgical treatment and in 2 patients (6%) after nonsurgical treatment (P = .013), when compared with the contralateral side. No correlation with clinical outcome scores or pain level was observed.
Figure 5.
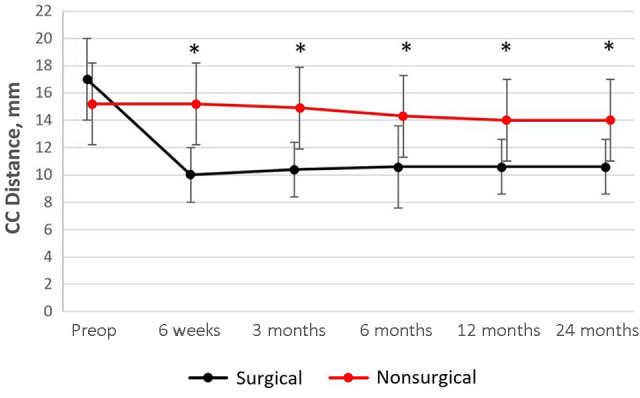
Longitudinal comparison of the coracoclavicular distance at different time points between surgical and nonsurgical treatment groups. Error bars represent standard deviation. *Statistically significant difference between groups (P < .05). Preop, preoperatively; CC, coracoclavicular.
Adverse Events
In the nonsurgical treatment group, there were 8 early failures (19%), with crossover to the surgical group according to patient wishes due to persistent pain or for cosmetic reasons. In addition, 1 late failure (3%) occurred due to persistent pain and instability of the shoulder girdle after nonsurgical treatment. In this patient, secondary ACJ stabilization was performed 7 months after the injury using a gracilis tendon autograft, with satisfying outcome. The patient was excluded from the final follow-up.
In the surgical treatment group, unplanned implant removal was necessary in 7 patients after using the TightRope system due to local subcutaneous implant irritation. This was performed after an average of 11 months. One superficial wound infection occurred 8 days after surgery using the hook plate. Early revision, irrigation and both local and systemic antibiotic therapy achieved infection control allowing the implant to be left in place. Thus, the rate of unplanned secondary surgery encountered after primary surgical treatment was 17%. This was significantly higher compared with the nonsurgical treatment group (P < .001).
Discussion
Based on our results, no significant differences regarding clinical outcomes were observed between surgical and nonsurgical treatment of acute Rockwood type 3 ACJ injuries. Radiologically, as expected, the surgical treatment group achieved a significantly lower CC distance but with a significantly higher incidence of posttraumatic ACJ osteoarthritis and presence of heterotopic ossifications.
To date, there have been 2 systematic reviews and 1 meta-analysis comparing nonsurgical with surgical treatment of Rockwood type 3 injuries. 15,18,25 No significant difference was found regarding general pain, posttraumatic osteoarthritis, nonsatisfying function, or clinical outcome scores, thus favoring nonsurgical treatment. However, possible advantages for high-demand patients such as manual workers or athletes could not be excluded. The main flaws of these systematic reviews were the underlying inhomogeneous patient groups, the lack of exclusive focus on type 3 injuries, and the low levels of evidence. To date, only 3 RCTs comparing surgical and nonsurgical treatment of ACJ injuries have been reported, and none of these studies exclusively focused on Rockwood type 3 injuries. 8,14,30
The Canadian Society of Orthopaedics and Trauma compared surgical and nonsurgical treatment of acute type 3 to 5 injuries in a multicenter RCT involving 83 patients (40 surgical, 43 nonsurgical therapy) with a follow-up of 2 years. 8 For surgical stabilization, the hook plate device was used in all cases. A shorter rehabilitation period for the nonsurgical group was shown with better radiological results for the hook plate group. The clinical outcomes (Constant scores of 91 in the nonsurgical group vs 95 in the surgical group) and subjective evaluation of the cosmesis were comparable after 2 years. An analysis according to the injury subtypes described by Rockwood was not performed.
Joukainen et al 14 reported the long-term results of an RCT (level of evidence, 2) comparing surgical and nonsurgical treatment of acute type 3 and 5 injuries. Surgery consisted of open reduction with direct CC ligament repair and temporary K-wire fixation, which was removed after 6 weeks. No difference was found according to the evaluated clinical outcome scores (Constant, University of California, Los Angeles, Larsen and Simple Shoulder Test). Nonsurgically treated patients were better regarding subjective ACJ instability, local tenderness, and crossbody test, although statistically not significant. The surgical group showed better cosmetic results. However, the number of included patients with type 3 injury (n = 11; 7 surgical, 4 nonsurgical group) was very small.
The most recent single-center RCT included 61 patients with an acute ACJ dislocation Rockwood type 3 (30 patients underwent surgical stabilization using the hook plate, 31 patients had conservative treatment). 30 In addition, 60 patients with Rockwood type 5 injury were included. The reported Constant score as the main outcome measurement did not yield statistical significance between groups (91 for the surgical group and 88 for the nonsurgical group, respectively) at final follow-up after 2 years and was comparable with our results. However, no differentiation between subtypes 3A and 3B was considered. Six patients with a type 3 injury assigned to nonoperative treatment (20%) underwent surgery within 19 months, which is much higher when compared with our study (3%).
According to the results of the current study, the clinical outcome after surgical or nonsurgical treatment of isolated Rockwood type 3 ACJ injuries is comparable after a follow-up of 2 years. Therefore, the study hypothesis was rejected. Both treatment approaches achieved close-to-full recovery of function when considering the Constant and ASES scores as outcome parameters. Furthermore, there were no differences in outcome scores after nonsurgical treatment between patients with modified Rockwood type 3A (horizontally stable) versus 3B (horizontally unstable) injuries, indicating that horizontal instability might not be the decisive criterion for surgery in type 3 injuries. Similarly, there were no significant differences in Constant score after nonsurgical treatment between patients younger than versus older than 35 years, indicating that age might not be the decisive criterion for surgery either. After nonsurgical treatment, a quicker recovery from pain and reachievement of ROM was observed after 6 weeks but not at 3 months. This means that a period of up to 3 months is needed until the pain and functional drawback after surgery is recovered. In contrast to the other outcome scores, the surgical group performed significantly better regarding the ACJI scores at 6 and 12 months but not at 24 months. This is explainable due to the inclusion of radiological parameters in the score and the superior reduction of the ACJ after surgical treatment.
The radiological outcomes showed a significantly lower CC distance in the surgically treated group, which might hint at a better cosmetic result, always keeping in mind the scars produced by surgery. Interestingly, the conservatively treated group also showed a small reduction of the CC distance over time. This can likely be explained by the fact that all measurements were made on panorama stress views, which might have more effect in the acute phase than at the later time points where ligament healing advances.
Despite the fact that 8 of 42 patients (19%) chose an early crossover to the surgical group, only 1 patient (3%) required secondary crossover to the surgical group due to unsatisfactory outcome. No other complications were found in this study group. After primary surgical treatment, 8 complications (17%) occurred requiring revision surgery. Together with the routinely scheduled implant removal of the hook plate after 3 to 6 months, the overall secondary surgery rate was 37% of all patients undergoing surgical stabilization, including the crossover patients. Importantly, this comparison has to be seen against the background of an equal clinical outcome, which hardly justifies surgical treatment.
Clinical Implications
Based on these results, the first line of treatment for acute, isolated Rockwood type 3 ACJ injuries should be nonsurgical, except for patients with definitive wish for surgical restoration of ACJ integrity despite counseling regarding the negligible difference in clinical outcome. In the case of persistent complaints after nonsurgical treatment, ACJ ligament reconstruction using tendon grafts can be performed with satisfying clinical results. 7,12,16,27,29 This treatment strategy might also have a relevant positive socioeconomic effect since not only can several surgical procedures be avoided but also rehabilitation times become much shorter allowing the patients a faster return into their working environment. Few data are available regarding costs. In 2019, Putnam et al 20 reported a mean 2-year reimbursement of US $23,096 for surgically treated ACJ dislocations in the United States, considering a revision rate of 67.5%. Also in a 2019 study, Abdelrahman et al 1 calculated US $2,441 for arthroscopic and US $1,573 for open ACJ repair, respectively. Thus, a significant cost reduction can be achieved, if the primary treatment approach of Rockwood type 3 injuries is nonsurgical.
Limitations
A limitation of this study is that our study protocol focused on short-term outcomes with a follow-up period of 2 years. We cannot draw any conclusion regarding longevity of the treatment effect in both groups. However, from the literature we do not have any indication of clinical deterioration over time for either treatment approach. Another issue might be the fact that the data analysis was carried out by 1 observer, leading to a possible confirmation bias. The fact that all surgeries were performed by expert shoulder surgeons might limit the generalizability of the results; however, it is unlikely that the surgical results would have been superior in the hands of less experienced surgeons. Furthermore, the comparison of 4 different surgical techniques creating inhomogeneity in the surgical group might be seen as drawback. However, the most popular techniques performed in the study country over recent years were included, which makes the study results more generalizable. In this context, we have to mention that we did not look at acute ACJ reconstruction using tendon augmentation, which is popular in some centers. Finally, subanalysis was performed for age and horizontal instability among nonsurgically treated patients but not for sports or occupation, which, in hindsight, would have been of interest. Collection of data on return to work/sports was also missed.
The main strength of the study, other than the randomized design with longitudinal follow-up, is the inclusion of isolated type 3 injuries with very strict adherence to the Rockwood classification parameters following a complete imaging protocol including a panorama stress view and additional functional axillary and Alexander views to detect dynamic horizontal instability.
Due to the crossover of 8 patients and the nature of the interventions, both an intention-to-treat and an as-treated analysis were performed. An as-treated analysis alone would create the risk for a certain selection bias. Analysis of both models showed comparability of the study populations and did not reveal any significant outcome differences. Thus, confidence in the study results is increased. However, the group comparability analysis showed that the effect of the randomization procedure was not significantly affected by the crossover.
Conclusion
No difference was observed in the functional outcome between surgical and nonsurgical treatment of acute Rockwood type 3 ACJ dislocations. Neither younger age nor horizontal instability (Rockwood subtype 3B) were associated with inferior outcomes. A slower recovery, higher complication rate, and increased radiological changes as posttraumatic ACJ osteoarthritis and heterotopic ossifications were present after surgery. Considering these medical findings and potential socioeconomic benefits, patients with acute ACJ dislocations of Rockwood type 3 should primarily undergo nonsurgical treatment.
Acknowledgment
The authors thank the German Society of Shoulder and Elbow Surgery for providing the multicenter platform to account for an important sample size.
Footnotes
Final revision submitted April 15, 2023; accepted April 27, 2023.
The authors have declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Ethikkommission für das Bundesland Salzburg (protocol No. 1277).
References
- 1. Abdelrahman AA, Ibrahim A, Abdelghaffar K, Ghandour TM, Eldib D. Open versus modified arthroscopic treatment of acute acromioclavicular dislocation using a single tight rope: randomized comparative study of clinical outcome and cost-effectiveness. J Shoulder Elbow Surg. 2019;28(11):2090–2097. [DOI] [PubMed] [Google Scholar]
- 2. Alexander OM. Dislocation of the acromioclavicular joint. Radiography. 1949;15(179):260, illust. [PubMed] [Google Scholar]
- 3. Balke M, Schneider MM, Shafizadeh S, Bäthis H, Bouillon B, Banerjee M. Current state of treatment of acute acromioclavicular joint injuries in Germany: is there a difference between specialists and non-specialists? A survey of German trauma and orthopaedic departments. Knee Surg Sports Traumatol Arthrosc. 2015;23(5):1447–1452. [DOI] [PubMed] [Google Scholar]
- 4. Barth J, Duparc F, Andrieu K, et al. Is coracoclavicular stabilisation alone sufficient for the endoscopic treatment of severe acromioclavicular joint dislocation (Rockwood types III, IV, and V)? Orthop Traumatol Surg Res. 2015;101(8 suppl):S297–S303. [DOI] [PubMed] [Google Scholar]
- 5. Beitzel K, Cote MP, Apostolakos J, et al. Current concepts in the treatment of acromioclavicular joint dislocations. Arthroscopy. 2013;29(2):387–397. [DOI] [PubMed] [Google Scholar]
- 6. Beitzel K, Mazzocca AD, Bak K, et al. ISAKOS upper extremity committee consensus statement on the need for diversification of the Rockwood classification for acromioclavicular joint injuries. Arthroscopy. 2014;30(2):271–278. [DOI] [PubMed] [Google Scholar]
- 7. Borbas P, Churchill J, Ek ET. Surgical management of chronic high-grade acromioclavicular joint dislocations: a systematic review. J Shoulder Elbow Surg. 2019;28(10):2031–2038. [DOI] [PubMed] [Google Scholar]
- 8. Canadian Orthopaedic Trauma Society. Multicenter randomized clinical trial of nonoperative versus operative treatment of acute acromio-clavicular joint dislocation. J Orthop Trauma. 2015;29(11):479–487. [DOI] [PubMed] [Google Scholar]
- 9. Chillemi C, Franceschini V, Dei Giudici L, et al. Epidemiology of isolated acromioclavicular joint dislocation. Emerg Med Int. 2013;2013:171609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;(214):160–164. [PubMed] [Google Scholar]
- 11. Enger M, Skjaker SA, Melhuus K, et al. Shoulder injuries from birth to old age: a 1-year prospective study of 3031 shoulder injuries in an urban population. Injury. 2018;49(7):1324–1329. [DOI] [PubMed] [Google Scholar]
- 12. Fauci F, Merolla G, Paladini P, Campi F, Porcellini G. Surgical treatment of chronic acromioclavicular dislocation with biologic graft vs synthetic ligament: a prospective randomized comparative study. J Orthop Traumatol. 2013;14(4):283–290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Flint JH, Wade AM, Giuliani J, Rue JP. Defining the terms acute and chronic in orthopaedic sports injuries: a systematic review. Am J Sports Med. 2014;42(1):235–241. [DOI] [PubMed] [Google Scholar]
- 14. Joukainen A, Kroger H, Niemitukia L, Makela EA, Vaatainen U. Results of operative and nonoperative treatment of Rockwood types III and V acromioclavicular joint dislocation: a prospective, randomized trial with an 18- to 20-year follow-up. Orthop J Sports Med. 2014;2(12):2325967114560130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Korsten K, Gunning AC, Leenen LP. Operative or conservative treatment in patients with Rockwood type III acromioclavicular dislocation: a systematic review and update of current literature. Int Orthop. 2014;38(4):831–838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kraus N, Hann C, Minkus M, Maziak N, Scheibel M. Primary versus revision arthroscopically-assisted acromio- and coracoclavicular stabilization of chronic AC-joint instability. Arch Orthop Trauma Surg. 2019;139(8):1101–1109. [DOI] [PubMed] [Google Scholar]
- 17. Kukkonen J, Kauko T, Vahlberg T, Joukainen A, Aarimaa V. Investigating minimal clinically important difference for Constant score in patients undergoing rotator cuff surgery. J Shoulder Elbow Surg. 2013;22(12):1650–1655. [DOI] [PubMed] [Google Scholar]
- 18. Longo UG, Ciuffreda M, Rizzello G, Mannering N, Maffulli N, Denaro V. Surgical versus conservative management of type III acromioclavicular dislocation: a systematic review. Br Med Bull. 2017;122(1):31–49. [DOI] [PubMed] [Google Scholar]
- 19. Nordqvist A, Petersson CJ. Incidence and causes of shoulder girdle injuries in an urban population. J Shoulder Elbow Surg. 1995;4(2):107–112. [DOI] [PubMed] [Google Scholar]
- 20. Putnam M, Vanderkarr M, Nandwani P, Holy CE, Chitnis AS. Surgical treatment, complications, and reimbursement among patients with clavicle fracture and acromioclavicular dislocations: a US retrospective claims database analysis. J Med Econ. 2019;22(9):901–908. [DOI] [PubMed] [Google Scholar]
- 21. Richards RR, An KN, Bigliani LU, et al. A standardized method for the assessment of shoulder function. J Shoulder Elbow Surg. 1994;3(6):347–352. [DOI] [PubMed] [Google Scholar]
- 22. Rockwood CA, Jr. Injuries to the acromioclavicular joint: Subluxations and dislocations about the shoulder. In: Rockwood CA, Jr, Green DP, eds. Fracture in Adults. JB Lippincott ; 1984:860–910. [Google Scholar]
- 23. Scheibel M, Droschel S, Gerhardt C, Kraus N. Arthroscopically assisted stabilization of acute high-grade acromioclavicular joint separations. Am J Sports Med. 2011;39(7):1507–1516. [DOI] [PubMed] [Google Scholar]
- 24. Taft TN, Wilson FC, Oglesby JW. Dislocation of the acromioclavicular joint. An end-result study. J Bone Joint Surg Am. 1987;69(7):1045–1051. [PubMed] [Google Scholar]
- 25. Tang G, Zhang Y, Liu Y, Qin X, Hu J, Li X. Comparison of surgical and conservative treatment of Rockwood type-III acromioclavicular dislocation: a meta-analysis. Medicine (Baltimore). 2018;97(4):e9690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Tauber M. Management of acute acromioclavicular joint dislocations: current concepts. Arch Orthop Trauma Surg. 2013;133(7):985–995. [DOI] [PubMed] [Google Scholar]
- 27. Tauber M, Eppel M, Resch H. Acromioclavicular reconstruction using autogenous semitendinosus tendon graft: results of revision surgery in chronic cases. J Shoulder Elbow Surg. 2007;16(4):429–433. [DOI] [PubMed] [Google Scholar]
- 28. Tauber M, Koller H, Hitzl W, Resch H. Dynamic radiologic evaluation of horizontal instability in acute acromioclavicular joint dislocations. Am J Sports Med. 2010;38(6):1188–1195. [DOI] [PubMed] [Google Scholar]
- 29. Tauber M, Valler D, Lichtenberg S, Magosch P, Moroder P, Habermeyer P. Arthroscopic stabilization of chronic acromioclavicular joint dislocations: triple- versus single-bundle reconstruction. Am J Sports Med. 2016;44(2):482–489. [DOI] [PubMed] [Google Scholar]
- 30. Windhamre HB, von Heideken J, Une-Larsson V, Ekstrom W, Ekelund A. No difference in clinical outcome at two-year follow-up in patients with acromioclavicular joint dislocation type III and V treated with hook plate or physiotherapy: a randomized controlled trial. J Shoulder Elbow Surg. 2022;31(6):1122–1136. [DOI] [PubMed] [Google Scholar]