Abstract
Background:
There is no clinical gold standard for the indications for single-row (SR) versus double-row (DR) repair according to small, large, or massive rotator cuff tear size.
Purpose:
To conduct a meta-analysis to compare the clinical outcomes and retear rates after arthroscopic SR and DR repair for rotator cuff injuries with different tear sizes.
Study Design:
Systematic review; Level of evidence, 3.
Methods:
On the basis of PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) criteria, the PubMed, Embase, Cochrane Library databases, Web of Science, China National Knowledge Infrastructure, and China BioMedical Literature database were searched for relevant studies published before November 1, 2021, using the following search terms: “Rotator Cuff Injuries,” “Rotator Cuff Tears,” “Arthroscopy,” “Arthroscopic Surgery,” “single-row,” and “double-row”; a total of 489 articles were retrieved. Quality evaluation was conducted for all the studies that met the inclusion criteria. This study evaluated the Constant-Murley score, American Shoulder and Elbow Surgeons (ASES) score, University of California, Los Angeles (UCLA) score, and range of motion (ROM) as well as retear rate. A fixed-effects or random-effects model was adopted to calculate the results and assess risk.
Results:
A total of 10 clinical studies were included, with 404 cases of DR and 387 cases of SR. Regarding overall results, DR had better forward elevation ROM (mean difference [MD] = -4.03° [95% CI, -6.00° to -2.06°]; P < .0001; I 2 = 46%) and a lower retear rate (MD = 2.39 [95% CI, 1.40 to 4.08]; P = .001; I 2 = 0%) compared with SR repair. With regard to small tears (<3 cm), there was no noticeable difference on any of the 3 outcome scores between SR and DR. For large rotator cuff tears (≥3 cm), DR repair showed significantly better ASES scores (MD = -3.09 [95% CI, -6.19 to 0.02]; P = .05; I 2 = 73%) and UCLA scores (MD = -1.47 [95% CI, -2.21 to -0.72]; P = .0001; I 2 = 31%) compared with SR repair.
Conclusion:
Our meta-analysis revealed that DR had better UCLA scores, ASES scores, and ROM in forward elevation and lower retear rates. In rotator cuff tears <3 cm, there were no statistical differences in clinical outcome between SR and DR.
Keywords: arthroscopic rotator cuff repair, clinical outcomes, double-row, fixation, rotator cuff injuries, single-row
Arthroscopic single-row (SR) and double-row (DR) rotator cuff repair has been used extensively for multifarious types of rotator cuff tears, especially with advances in surgical techniques and biomaterials. 3,18,32 In recent years, some studies have considered that DR repair may preserve more of the anatomic footprint and has both a better postoperative joint function and a comparatively low tear rate. 1,8,39 Nevertheless, there is controversy about which surgical procedure should be chosen for rotator cuff injuries with dissimilar tear sizes. 10,34,35,42
For a successful rotator cuff repair, it is essential to restore the original anatomic and biomechanical structure as much as possible. 11,36 Some recent biomechanical studies have proved that DR repair can heighten footprint contact, strengthen tendon strength, and expand acromiohumeral distance, which may promote the prognosis of patients with DR repair. 2,14,40 Aside from that, as demonstrated by several previous meta-analyses, DR repairs can tolerate greater failure loads and noticeably lessen gap formation. 12,30 Overall, because of the anatomic and biomechanical factors mentioned above, a higher retear rate has been seen after SR than DR, especially for partial-thickness retears, but there has been no remarkable difference in clinical outcomes between these 2 techniques. 5,37,38,43
Despite the development of these surgical techniques, the risk of complications such as retear of the rotator cuff is still high. Retearing reduces clinical function and strength and may lead to persistent pain. 6 The risk of retear may be associated with preoperative tear size, postoperative rehabilitation, tendon quality, and surgical methods. 13,27
The purpose of this study was to perform a systematic review and meta-analysis to update and report on the outcomes after DR versus SR repair for rotator cuff tears, with particular focus on tears of varying sizes. We hypothesized that the data from more recent studies would indicate that DR repair is superior to SR repair for large rotator cuff tears.
Methods
Literature Search
This study conducted a systematic review and meta-analysis according to PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) standard. 31 From the beginning of the database to November 1, 2021, we searched PubMed, Embase, Cochrane Library databases, Web of Science, China National Knowledge Infrastructure, and China BioMedical Literature database, using search terms “Rotator Cuff Injuries” (Medical Subject Headings [MeSH]) AND “Arthroscopy” (MeSH) AND “single-row” AND “double-row.”
Study Selection
Two authors (Z.G. and S.W.) independently screened the titles and abstracts of relevant research. When differences were encountered, a third reviewer (K.-W.Z.) gave a final opinion. We also retrieved the references of eligible articles to ensure a comprehensive review of all relevant studies.
Study Inclusion and Exclusion Criteria
Studies were included if they fulfilled the following criteria: (1) skeletally mature patients (older than 18 years); (2) randomized studies included needed to compare SR and DR repair; (3) studies with Level 1, 2, or 3 evidence; (4) human clinical research; (5) follow-up was no less than 12 months and reported outcomes included one of visual analog scale score, University of California, Los Angeles (UCLA) score, American Shoulder and Elbow Surgeons (ASES) score, range of motion (ROM), and retear rate.
The exclusion criteria for the study were as follows: (1) only 1 technology of SR or DR was reported in the study; (2) non-English or non-Chinese studies; (3) case reports, expert opinions, and narrative review articles; (4) animal or cadaveric studies; (5) no mention of rotator cuff tear size.
Data Extraction
All included randomized studies were comparative studies of SR versus DR. The data extracted contained mainly the following: (1) study information: first author, country of origin, year of publication, study design, level of evidence, and sample size; (2) patient information: mean age, type of interventions, duration of follow-up, and tear size (small, <3 cm, large, ≥3 to 5 cm, massive, >5 cm); (3) outcome measures (mean ± SE): ASES score, UCLA score, Constant-Murley score (CMS), ROM in forward flexion and external rotation, and retear rate.
Methodological Quality Assessment
Based on the Cochrane Handbook for Systematic Reviews and Interventions, 2 authors (Y.Y. and T.R.) independently evaluated the quality and related bias risk of all randomized controlled trials (RCTs). The following parameters were used to evaluate quality: (1) randomness of participation in research, (2) concealment of allocation, (3) blinding method of participating researchers, (4) blinding method of evaluation of outcomes, (5) completeness of outcome data, (6) selectiveness in outcome reporting, and (7) other bias. For nonrandomized studies, the Newcastle-Ottawa Scale was used to assess quality. 41
Data Synthesis and Statistical Analysis
Review Manager Version 5.3 (International Cochrane Collaboration) was used for all data synthesis and analysis. The odds ratio (OR) with 95% CIs was used to analyze all binary variables, and the mean difference (MD) with 95% CI was used to analyze all continuous variables. Heterogeneity was assessed with the I 2 statistic, in which a value of I 2 > 75% is considered to indicate highly significant statistical heterogeneity, suggesting a random-effect modeling estimation. If the I 2 value was <75%, the fixed-effect model was adopted. The outcome parameters (ASES score, UCLA score, CMS, ROM, and retear rate) were compared among the included studies; in addition, we performed a subgroup analysis of the studies according to tear size (small [<3 cm] vs large [≥3 cm]). The results of the comparisons are shown as forest plots. A P value < .05 was set as the threshold for statistical significance.
Results
Final Article Selection
The original search resulted in 489 articles from PubMed, Embase, Cochrane Library, Web of Science, and other databases. After removing duplicates, the titles and abstracts of 259 articles were reviewed, among which 18 articles were considered to meet the screening criteria. Of these 18 articles, 8 were excluded in that 6 of them did not describe tear size and 2 were review articles that did not satisfy the inclusion criteria. Ultimately, the meta-analysis included 10 articles for qualitative and quantitative assessment. A PRISMA flowchart is displayed in Figure 1.
Figure 1.
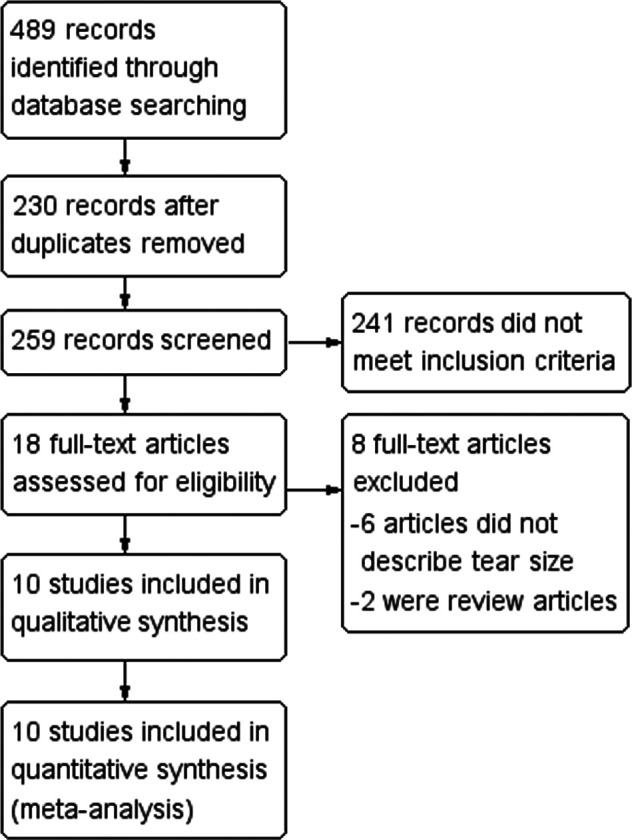
PRISMA flowchart of data extraction. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses
Characteristics of Included Studies
Table 1 summarizes the 10 studies included in our meta-analysis. There were 7 RCTs, 4,6,8,14,21,22,29 1 prospective cohort study, 24 and 2 retrospective studies. 33,37 The 10 studies involved 791 rotator cuff injury cases, of which 387 were SR repairs and 404 were DR repairs. In the DR repair, 75 cases were fixed with a suture bridge, 50 with transosseous-equivalent repair, and the rest were general DR repairs. The mean follow-up time was 55.1 months (range, 24-168 months).
Table 1.
Characteristics of Included Studies a
| Lead Author (Year) | Country | Study Design | LOE | Sample Size, SR/DR, n | Age, y, SR/DR b | Intervention | Tear Sizes Included, cm | Clinical Outcomes | Follow-up, mo, SR/DR b |
|---|---|---|---|---|---|---|---|---|---|
| Li (2021) 24 | China | Prosp | 2 | 34/34 | 56.79 ± 10.17/58.27 ± 10.71 | SR/SB-DR | ≤3, >3 | VAS, UCLA, ASES, retear rate, ROM | 39.35 ± 12.37/41.47 ± 12.25 |
| Lapner (2021) 21 | Canada | RCT | 1 | 43/34 | 55.3 ± 8.2/57.2 ± 6.7 | SR/DR | <5 | WORC, ASES, CMS | 120 |
| Plachel (2020) 33 | Germany | Retrosp | 3 | 12/10 | 60 ± 6/62 ± 8 | SR/TOE-DR | <5 | CMS, WORC, SSV, SST, retear rate | 156 ± 12/144 ± 12 |
| Imam (2020) 14 | UK | RCT | 1 | 40/40 | 61.6/60.0 | SR/TOE-DR | <3, >3 | OSS, UCLA, CMS, VAS | 36 |
| Chen (2019) 6 | China | RCT | 2 | 52/53 | 57.5 ± 7.2/56.7 ± 8.0 | SR/DR | <5 | ASES, CMS, ROM, VAS, retear rate | 31 ± 5/29 ± 5 |
| Senna (2018) 37 | Brazil | Retrosp | 3 | 29/27 | 57.5/55.7 | SR/DR | <5 | UCLA, ASES | 37.8/41.0 |
| Gao (2018) 8 | China | RCT | 2 | 39/41 | 57.91 ± 12.83/55.82 ± 13.55 | SR/SB-DR | 1-3 | UCLA, ASES | 49.60 ± 7.23/48.82 ± 6.34 |
| Lapner (2012) 22 | Canada | RCT | 1 | 48/42 | 56.0 ± 8.9/57.8 ± 7.0 | SR/DR | <5 | ASES, CMS, WORC | 24 |
| Ma (2012) 29 | Taiwan, China | RCT | 2 | 27/26 | 60.8/61.6 | SR/DR | <3, >3 | UCLA, ASES, CMS, retear rate | 33.3/33.5 |
| Carbonel (2012) 4 | Spain | RCT | 1 | 80/80 | 55.79 ± 6.3/55.21 ± 5.0 | SR/DR | 1-3, 3-5 | UCLA, ASES, CMS, ROM, retear rate | 24 |
a ASES, American Shoulder and Elbow Surgeons; CMS, Constant-Murley score; DR, double-row repair; FT, full-thickness tear; LOE, level of evidence; OSS, Oxford Shoulder Score; Prosp, prospective cohort study; RCT, randomized controlled trial; Retrosp, retrospective study; ROM, range of motion; SB-DR, double-row suture bridge repair; SR, single-row repair; SST, Simple Shoulder Test; SSV, subjective shoulder value; TOE-DR, transosseous-equivalent double-row repair; UCLA, University of California, Los Angeles; UK, United Kingdom; VAS, visual analog scale; WORC, Western Ontario Rotator Cuff Index.
b Reported as mean or mean ± SD.
Quality Assessment
The risk-of-bias assessment for the 7 RCTs showed that the included studies were of high quality (Figure 2). 4,6,8,14,21,22,29 The quality assessment of the remaining 3 cohort studies indicated that they were of good quality as assessed by Newcastle-Ottawa Scale (Table 2). 24,33,37
Figure 2.
Qualitative assessment of the RCTs included in the review. (A) Risk of bias summary according to study. (B) Graph showing overall risk of bias percentages. RCT, randomized controlled trial.
Table 2.
Qualitative Assessment of the Nonrandomized Studies According to the Newcastle-Ottawa Scale
| Lead Author (Year) | Selection | Comparability | Outcome | Total Score a |
|---|---|---|---|---|
| Li (2021) 24 | 3 | 2 | 2 | 8 |
| Senna (2018) 37 | 3 | 2 | 2 | 7 |
| Plachel (2020) 33 | 3 | 2 | 3 | 8 |
a All studies were considered of good quality: overall score was >6 points, with 2 or 3 points in the selection domain, 2 or 3 points in the comparability domain, and 2 or 3 points in the outcome domain.
Outcomes
ASES Score
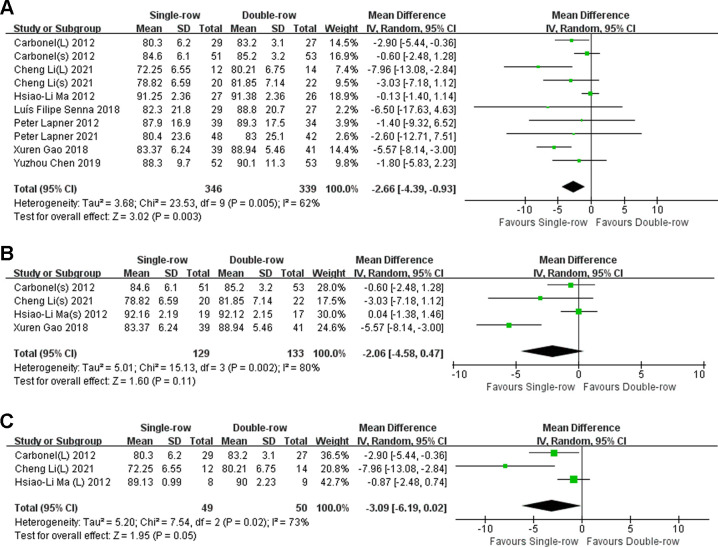
The ASES score was reported in 8 studies, § involving 685 patients. Compared with SR repairs, DR repairs had higher ASES scores (MD = -2.66 [95% CI, -4.39 to -0.93]; P = .003; I 2 = 62%) (Figure 3A). Subgroup analysis according to tear size indicated that for tears <3 cm, there was no statistically significant difference between the 2 groups (MD = -2.06 [95% CI, -4.58 to 0.47]; P = .11; I 2 = 80%) (Figure 3B). For tears ≥3 cm however, the ASES score was significantly better in DR versus SR repair (MD = -3.09 [95% CI, -6.19 to 0.02]; P = .05; I 2 = 73%) (Figure 3C).
Figure 3.
Forest plots for the comparison of ASES score (A) overall, (B) for small tears, and (C) for large tears. ASES, American Shoulder and Elbow Surgeons; IV, inverse variance; (L), large tear; (s), small tear.
UCLA Score
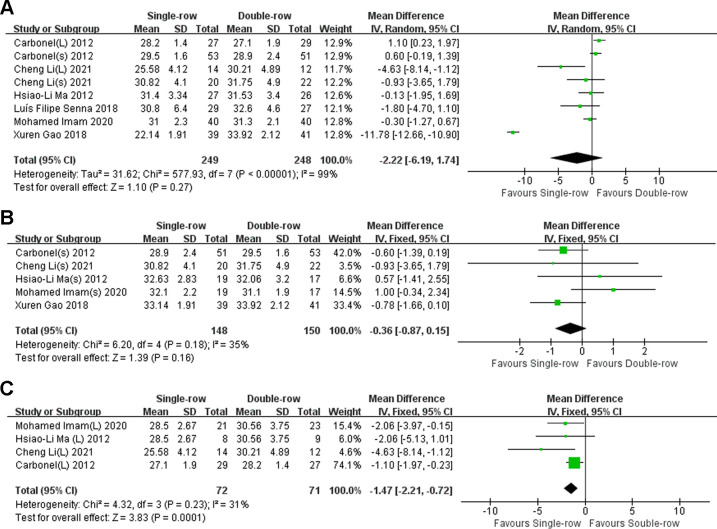
The UCLA score was reported in 4 RCTs, 4,8,14,29 1 prospective cohort study, 24 and 1 retrospective study 37 involving 497 patients. There was no statistical difference between the 2 groups, and heterogeneity between the 2 groups was high (MD = -2.22 [95% CI, -6.19 to 1.74]; P = .27, I 2 = 99%) (Figure 4A). The heterogeneity decreased in both groups after subgroup analysis according to tear size. For tears <3 cm, there was no statistical difference between the 2 groups (MD = -0.36 [95% CI, -0.87 to 0.15]; P = .16, I 2 = 35%) (Figure 4B); however for tears ≥3 cm, the UCLA score was significantly better for DR versus SR repair (MD = -1.47 [95% CI, -2.21 to -0.72]; P = .0001; I 2 = 31%) (Figure 4C).
Figure 4.
Forest plots for the comparison of UCLA score (A) overall, (B) for small tears, and (C) for large tears. IV, inverse variance; (L), large tear; (s), small tear; UCLA, University of California, Los Angeles.
Constant-Murley Score
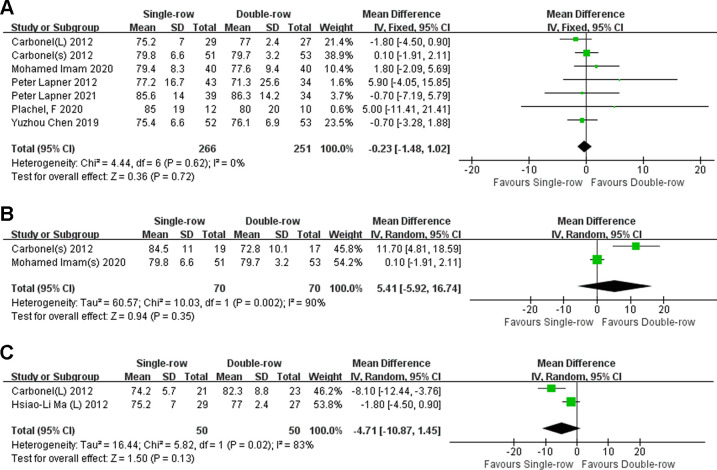
The CMS was reported in 5 RCTs, 4,6,14,21,22,29 and 1 retrospective cohort study, 33 involving 517 patients. There was no statistically significant difference between the groups, and the heterogeneity between the 2 groups was low (MD = -0.23 [95% CI, -1.48 to 1.02]; P = .72, I 2 = 0%) (Figure 5A). There were no significant differences between the groups in the subgroup analysis (for tears <3 cm: MD = 5.41 [95% CI, -5.92 to 16.74]; P = .35; I 2 = 90%; for tears ≥3 cm: MD = -4.71 [95% CI, -10.87 to 1.45]; P = .13; I 2 = 83%) (Figure 5, B and C).
Figure 5.
Forest plots for the comparison of CMS (A) overall, (B) for small tears, and (C) for large tears. CMS, Constant-Murley score; IV, inverse variance; (L), large tear; (s), small tear.
Range of Motion
Forward elevation and external rotation ROM values were reported in 2 RCTs, 4,6 and 1 prospective cohort study, 24 involving 333 patients. Compared with SR repair, DR repair had significantly higher forward elevation ROM, with moderate heterogeneity (MD = -4.03° [95% CI, -6.00° to -2.06°]; P < .001; I 2 = 46%) (Figure 6A). There was no significant difference between the groups in external rotation ROM, with low heterogeneity between the 2 groups (MD = -0.37° [95% CI, -1.88° to 1.14°]; P = .63; I 2 = 30%) (Figure 6B).
Figure 6.
Forest plots for the comparisons of (A) forward elevation ROM and (B) external rotation ROM. IV, inverse variance; (L), large tear; ROM, range of motion; (s), small tear.
Retear Rate
The retear rate was reported in 3 RCTs, 4,6,29 1 prospective cohort study, 24 and 1 retrospective cohort study, 33 involving 406 patients. Overall, compared with SR repair, DR repair had a lower tear rate (OR = 2.39 [95% CI, 1.40 to 4.08]; P = .001; I 2 = 0%) (Figure 7A). Subgroup analysis based on tear size (reported in 1 study) indicated that for tears <3 cm, 24 there was no statistically significant difference between the 2 groups (OR = 3.00 [95% CI, 0.29 to 31.48]) (Figure 7B); however, for tears ≥3 cm, the retear rate was significantly lower with DR versus SR repair (OR = 13.00 [95% CI, 1.27 to 133.28]; P = .03) (Figure 7C).
Figure 7.
Forest plots for the comparison of retear rates (A) overall, (B) for small tears, and (C) for large tears. (L), large tear; M-H, Mantel-Haenszel; OR, odds ratio; (s), small tear.
Sensitivity Analysis
All the statistically significant results using both the fixed-effects and random-effects models were analyzed for sensitivity. In the UCLA score (MD = -2.22 [95% CI, -6.19 to 1.74]; P < .001; I 2 = 99%), ASES score for small tears (MD = -2.06 [95% CI, -4.58 to 0.47];), ASES score for large tears (MD = -3.09 [95% CI, -6.19 to 0.02]; P = .05; I 2 = 73%), and CMS for large tears (MD = -4.71 [95% CI, -10.87 to 1.45]; P = .13; I 2 = 83%), there were significant differences between the fixed-effects and random-effects models. The rest of the comparison results did not change in any of the models.
Discussion
Our study showed that overall, better forward elevation ROM (P < .0001; I 2 = 46%) and a lower retear rate (P = .001; I 2 = 0%) were seen after DR repair compared with SR repair, and for large rotator cuff tears (≥3 cm), better ASES scores (P = .05; I 2 = 73%), UCLA scores (P = .0001; I 2 = 31%), and retear rate (P = .03) were seen after DR compared with SR repair.
As revealed by previous studies, notwithstanding the fact that no substantial clinical advantage was found for DR over SR, DR increased tendon integrity and had a higher healing rate in long-term follow-up. 22,33 A 2021 study found that DR repair preserved better clinical function and led to better outcome scores than SR repair at up to 10 years of follow-up. 27 DR repair was found to have no prominent advantage for patients with tear length <3 cm, but this method can obtain a more satisfactory score and lower retear rate for patients with tear length ≥3 cm compared with SR repair. 14,24 This result is consistent with the meta-analysis by Zhang et al 44 in 2013.
As with the current study, a meta-analysis conducted by Yang et al 42 in 2016 also demonstrated that DR repair provided more rotator cuff integrity, with higher ASES and UCLA scores. However, the current review includes more recent studies, with a higher level of evidence. As indicated by the latest biomechanical experiments, the better clinical results of DR repair may be correlated with heightening footprint contact, preserving more acromiohumeral distance, and heightening tendon strength. 7,28
As revealed by some previous cadaveric studies, compared with SR repair, the rotator cuff footprint reconstruction of DR repair ameliorated the initial strength and stiffness and lessened the gap formation and strain on the footprint, and the tendon had higher tensile strength. 17,28 As further revealed by recent long-term follow-up multicenter RCTs and biomechanical experiments, regardless of the size of the tear, DR repair retains more shoulder-end humeral distance and better shoulder joint function, and the retear rate of DR repair is lower than that of SR repair, which may provide better long-term results. 15,21 Nevertheless, some of the studies we included exhibited no striking difference in functional outcomes between these DR and SR repair for small tears (<3 cm), whereas for large tears (≥3 and <6 cm), DR repair was superior to SR repair. 4,14,24,29 More RCTs and biomechanical studies with large samples and long-term follow-up are needed to prove this conclusion.
Diminishing the postoperative retear rate and maintaining higher rotator cuff integrity is key to the prognosis of rotator cuff injuries. Results from the 2021 study by Li et al 24 included in this review indicated that, for small tears, the retear rate was not significantly different between DR and SR repair; however, for large tears, the retear rate after DR repair was significantly lower than after SR repair (P = .03). In addition, the 2021 level 1 RCT by Lapner et al 21 concluded that at minimum 10-year follow-up, DR repair had higher rotator cuff integrity according to the Western Ontario Rotator Cuff Index compared with SR repair.
Preoperative factors such as subscapularis fat infiltration; duration of symptoms; bone mineral density; anatomic factors such as tear length, tear width, tear size area, and retraction; and dissimilar intraoperative technical details such as diverse footprint coverage and fixation intensity are among the many reasons for the variation in retear rates. Aside from that, a higher rate of retear may be seen in a high-risk group prone to retear, regardless of the repair modality. 9,25,26,45 A further consideration is that surgical repair of large full-size tears is often performed at a late stage, where undesirable quality and remarkable retraction of the tendon may not allow the surgeon to perform the repair using a DR repair technique. As a result, the only viable option in this case is SR repair, partially covering the impression, which was shown to lead to a noticeably higher tear rate in the current review.
Different postoperative rehabilitation methods affect the prognosis after rotator cuff repair, and the timing of rehabilitation is important to preserve the integrity of the repaired tendon and prevent stiffness. Conventional rehabilitation is through early passive ROM, followed by delayed active activity, and finally strengthening exercises. There was no significant difference in final clinical function between patients treated with early onset active exercise and delayed exercise protocols. 16,19 Aggressive stretching should also be avoided during early activities, and magnetic resonance imaging shows a higher rate of retears after aggressive manual stretching and unrestricted self-directed stretching. 23 In patients with large tears (≥3 cm) after rotator cuff repair, the benefits of immobilization for tendon healing may be more important, as increasing the duration of immobilization may not lead to a greater risk of shoulder stiffness 20 ; in patients with small tears (<3 cm), early exercise can accelerate shoulder motion gain and functional recovery without compromising tendon healing but also requires consideration of age. 15
Limitations
There are some limitations to our review. First and foremost, there were no uniform standards for DR repair technology included in the literature. The current review included 2 studies that used DR suture bridge fixation, 8,24 2 studies that used transosseous-equivalent DR repair, 14,33 and others that used simple DR repair. As a result, optimal normalization is needed to estimate the true pooled estimation effects. In addition, there is no uniform follow-up time for the included studies, for the reason that the cooperation degree of discharged patients is inconsistent.
In the meta-analysis, heterogeneity was high for the overall comparison of UCLA and ASES scores; however, it decreased markedly in both DR and SR groups after subgroup analysis. The high heterogeneity values we found may be on account of the difference in tearing degrees and the diverse techniques that were included in each category. We adopted the random-effects model to cope with the problem of high heterogeneity, which has been proven to deal with this issue.
With regard to tear sizes, a meta-analysis of massive rotator cuff tears was not performed in this study. The subgroup analysis of retear rate according to tear size only included the 2021 study by Li et al. 24 Studies with larger sample sizes and longer-term follow-ups are still needed to investigate the clinical efficacy of SR and DR repair for massive rotator cuff tears and to standardize the assessment of retears after SR versus DR repair. Finally, the cost-effectiveness of SR versus DR repair was not addressed in this review.
Conclusion
Our meta-analysis revealed that DR repair had better ASES scores, UCLA scores, and ROM of forward elevation and lower retear rates compared with SR repair. In rotator cuff tears <3 cm, there were no statistical differences in clinical outcome between SR and DR. Further high-quality biomechanical studies and multicenter, large-sample RCTs are needed to validate this finding and to assess the clinical effectiveness and cost-effectiveness of both techniques.
NOTES
Footnotes
Final revision submitted February 6, 2023; accepted March 9, 2023.
The authors have declared that there are no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Aleem AW, Syed UA, Wascher J, et al. Functional outcomes after bilateral arthroscopic rotator cuff repair. J Shoulder Elbow Surg. 2016;25(10):1668–1673. [DOI] [PubMed] [Google Scholar]
- 2. Anderson K, Boothby M, Aschenbrener D, van Holsbeeck M. Outcome and structural integrity after arthroscopic rotator cuff repair using 2 rows of fixation: minimum 2-year follow-up. Am J Sports Med. 2006;34(12):1899–1905. [DOI] [PubMed] [Google Scholar]
- 3. Avanzi P, Giudici LD, Capone A, et al. Prospective randomized controlled trial for patch augmentation in rotator cuff repair: 24-month outcomes. J Shoulder Elbow Surg. 2019;28(10):1918–1927. [DOI] [PubMed] [Google Scholar]
- 4. Carbonel I, Martinez AA, Calvo A, Ripalda J, Herrera A. Single-row versus double-row arthroscopic repair in the treatment of rotator cuff tears: a prospective randomized clinical study. Int Orthop. 2012;36(9):1877–1883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Chen M, Xu W, Dong Q, Huang Q, Xie Z, Mao Y. Outcomes of single-row versus double-row arthroscopic rotator cuff repair: a systematic review and meta-analysis of current evidence. Arthroscopy. 2013;29(8):1437–1449. [DOI] [PubMed] [Google Scholar]
- 6. Chen YZ, Li H, Qiao Y, et al. Double-row rotator cuff repairs lead to more intensive pain during the early postoperative period but have a lower risk of residual pain than single-row repairs. Knee Surg Sports Traumatol Arthrosc. 2019;27(10):3180–3187. [DOI] [PubMed] [Google Scholar]
- 7. Endo A, Hoogervorst P, Safranek C, et al. Linked double-row equivalent arthroscopic rotator cuff repair leads to significantly improved patient outcomes. Orthop J Sports Med. 2020;8(7):2325967120938311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Gao X, Liang Z, Chen Y, et al. Arthroscopic suture bridge double-row and SCOI single-row sutures comparison of efficacy in repairing medium-sized rotator cuff tears. Chin J Orthop. 2018;26(22):4. [Google Scholar]
- 9. Harada N, Gotoh M, Ishitani E, et al. Combination of risk factors affecting retear after arthroscopic rotator cuff repair: a decision tree analysis. J Shoulder Elbow Surg. 2021;30(1):9–15. [DOI] [PubMed] [Google Scholar]
- 10. Hein J, Reilly JM, Chae J, Maerz T, Anderson K. Retear rates after arthroscopic single-row, double-row, and suture bridge rotator cuff repair at a minimum of 1 year of imaging follow-up: a systematic review. Arthroscopy. 2015;31(11):2274–2281. [DOI] [PubMed] [Google Scholar]
- 11. Heuberer PR, Pauzenberger L, Gruber MS, et al. Delaminated rotator cuff tears showed lower short-term retear rates after arthroscopic double-layer repair versus bursal layer-only repair: a randomized controlled trial. Am J Sports Med. 2020;48(3):689–696. [DOI] [PubMed] [Google Scholar]
- 12. Hohmann E, König A, Kat CJ, Glatt V, Tetsworth K, Keough N. Single- versus double-row repair for full-thickness rotator cuff tears using suture anchors. A systematic review and meta-analysis of basic biomechanical studies. Eur J Orthop Surg Traumatol. 2018;28(5):859–868. [DOI] [PubMed] [Google Scholar]
- 13. Houck DA, Kraeutler MJ, Schuette HB, McCarty EC, Bravman JT. Early versus delayed motion after rotator cuff repair: a systematic review of overlapping meta-analyses. Am J Sports Med. 2017;45(12):2911–2915. [DOI] [PubMed] [Google Scholar]
- 14. Imam M, Sallam A, Ernstbrunner L, et al. Three-year functional outcome of transosseous-equivalent double-row vs. single-row repair of small and large rotator cuff tears: a double-blinded randomized controlled trial. J Shoulder Elbow Surg. 2020;29(10):2015–2026. [DOI] [PubMed] [Google Scholar]
- 15. Kaya T, Haluk Ç, Cenk K, Çağatay Ö. Increased acromiohumeral distance in a double-row arthroscopic rotator cuff surgery compared to a single-row surgery after 12 months. J Orthop Surg Res. 2021;16(1):385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Keener JD, Galatz LM, Stobbs-Cucchi G, Patton R, Yamaguchi K. Rehabilitation following arthroscopic rotator cuff repair: a prospective randomized trial of immobilization compared with early motion. J Bone Joint Surg Am. 2014;96(1):11–19. [DOI] [PubMed] [Google Scholar]
- 17. Kim DH, Elattrache NS, Tibone JE, et al. Biomechanical comparison of a single-row versus double-row suture anchor technique for rotator cuff repair. Am J Sports Med. 2006;34(3):407–414. [DOI] [PubMed] [Google Scholar]
- 18. Kim SH, Yang SH, Rhee SM, et al. The formation of perianchor fluid associated with various suture anchors used in rotator cuff repair: all-suture, polyetheretherketone, and biocomposite anchors. Bone Joint J. 2019;101-B(12):1506–1511. [DOI] [PubMed] [Google Scholar]
- 19. Kjær BH, Magnusson SP, Henriksen M, et al. Effects of 12 weeks of progressive early active exercise therapy after surgical rotator cuff repair: 12 weeks and 1-year results from the CUT-N-MOVE randomized controlled trial. Am J Sports Med. 2021;49(2):321–331. [DOI] [PubMed] [Google Scholar]
- 20. Koo SS, Parsley BK, Burkhart SS, Schoolfield JD. Reduction of postoperative stiffness after arthroscopic rotator cuff repair: results of a customized physical therapy regimen based on risk factors for stiffness. Arthroscopy. 2011;27(2):155–160. [DOI] [PubMed] [Google Scholar]
- 21. Lapner P, Li A, Pollock JW, et al. A multicenter randomized controlled trial comparing single-row with double-row fixation in arthroscopic rotator cuff repair: long-term follow-up. Am J Sports Med. 2021;49(11):3021–3029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Lapner PLC, Sabri E, Rakhra K, et al. A multicenter randomized controlled trial comparing single-row with double-row fixation in arthroscopic rotator cuff repair. J Bone Joint Surg Am. 2012;94(14):1249–1257. [DOI] [PubMed] [Google Scholar]
- 23. Lee BG, Cho NS, Rhee YG. Effect of two rehabilitation protocols on range of motion and healing rates after arthroscopic rotator cuff repair: aggressive versus limited early passive exercises. Arthroscopy. 2012;28(1):34–42. [DOI] [PubMed] [Google Scholar]
- 24. Li C, Zhang H, Bo X, et al. Arthroscopic release combined with single-row fixation or double-row suture bridge fixation in patients with traumatic supraspinatus tear and adhesive capsulitis non-responsive to conservative management: a prospective randomized trial. Orthop Traumatol Surg Res. 2021;107(4):102828. [DOI] [PubMed] [Google Scholar]
- 25. Liu T, Zhang M, Yang Z, Zhang B, Jiang J, Yun X. Does the critical shoulder angle influence retear and functional outcome after arthroscopic rotator cuff repair? A systematic review and meta-analysis. Arch Orthop Trauma Surg. 2023;143(5):2653–2663. [DOI] [PubMed] [Google Scholar]
- 26. Lobo-Escolar L, Ramazzini-Castro R, Codina-Grañó D, Lobo E, Minguell-Monyart J, Ardèvol J. Risk factors for symptomatic retears after arthroscopic repair of full-thickness rotator cuff tears. J Shoulder Elbow Surg. 2021;30(1):27–33. [DOI] [PubMed] [Google Scholar]
- 27. Longo UG, Carnevale A, Piergentili I, et al. Retear rates after rotator cuff surgery: a systematic review and meta-analysis. BMC Musculoskelet Disord. 2021;22(1):749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Ma CB, Comerford L, Wilson J, Puttlitz CM. Biomechanical evaluation of arthroscopic rotator cuff repairs: double-row compared with single-row fixation. J Bone Joint Surg Am. 2006;88(2):403–410. [DOI] [PubMed] [Google Scholar]
- 29. Ma HL, Chiang ER, Wu HT, et al. Clinical outcome and imaging of arthroscopic single-row and double-row rotator cuff repair: a prospective randomized trial. Arthroscopy. 2012;28(1):16–24. [DOI] [PubMed] [Google Scholar]
- 30. Millett PJ, Warth RJ, Dornan GJ, Lee JT, Spiegl UJ. Clinical and structural outcomes after arthroscopic single-row versus double-row rotator cuff repair: a systematic review and meta-analysis of level I randomized clinical trials. J Shoulder Elbow Surg. 2014;23(4):586–597. [DOI] [PubMed] [Google Scholar]
- 31. Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Peng L, Yue J, Ouyang K, et al. Arthroscopic repair of the medium-size rotator cuff tear with the novel technique of the point union bridge: a minimum 2-year follow-up cohort study. J Shoulder Elbow Surg. 2021;30(9):2056–2064. [DOI] [PubMed] [Google Scholar]
- 33. Plachel F, Siegert P, Ruttershoff K, et al. Long-term results of arthroscopic rotator cuff repair: a follow-up study comparing single-row versus double-row fixation techniques. Am J Sports Med. 2020;48(7):1568–1574. [DOI] [PubMed] [Google Scholar]
- 34. Prasathaporn N, Kuptniratsaikul S, Kongrukgreatiyos K. Single-row repair versus double-row repair of full-thickness rotator cuff tears. Arthroscopy. 2011;27(7):978–985. [DOI] [PubMed] [Google Scholar]
- 35. Quigley RJ, Gupta A, Oh JH, et al. Biomechanical comparison of single-row, double-row, and transosseous-equivalent repair techniques after healing in an animal rotator cuff tear model. J Orthop Res. 2013;31(8):1254–1260. [DOI] [PubMed] [Google Scholar]
- 36. Rossi LA, Rodeo SA, Chahla J, Ranalletta M. Current concepts in rotator cuff repair techniques: biomechanical, functional, and structural outcomes. Orthop J Sports Med. 2019;7(9):2325967119868674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Senna LF, Ramos MRF, Bergamaschi RF. Arthroscopic rotator cuff repair: single-row vs. double-row- clinical results after one to four years. Rev Bras Ortop. 2018;53(4):448–453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Sheibani-Rad S, Giveans MR, Arnoczky SP, Bedi A. Arthroscopic single-row versus double-row rotator cuff repair: a meta-analysis of the randomized clinical trials. Arthroscopy. 2013;29(2):343–348. [DOI] [PubMed] [Google Scholar]
- 39. Sugaya H, Maeda K, Matsuki K, Moriishi J. Repair integrity and functional outcome after arthroscopic double-row rotator cuff repair. A prospective outcome study. J Bone Joint Surg Am. 2007;89(5):953–960. [DOI] [PubMed] [Google Scholar]
- 40. Wall LB, Keener JD, Brophy RH. Double-row vs single-row rotator cuff repair: a review of the biomechanical evidence. J Shoulder Elbow Surg. 2009;18(6):933–941. [DOI] [PubMed] [Google Scholar]
- 41. Wells G, Shea B, O’Connell J. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa Health Research Institute. July 2014. Accessed December 15, 2022. https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp
- 42. Yang J, Jr, Robbins M, Reilly J, Maerz T, Anderson K. The clinical effect of a rotator cuff retear: a meta-analysis of arthroscopic single-row and double-row repairs. Am J Sports Med. 2017;45(3):733–741. [DOI] [PubMed] [Google Scholar]
- 43. Zafra M, Uceda P, Muñoz-Luna F, Muñoz-López RC, Font P. Arthroscopic repair of partial-thickness articular surface rotator cuff tears: single-row transtendon technique versus double-row suture bridge (transosseous equivalent) fixation: results from a prospective randomized study. Arch Orthop Trauma Surg. 2020;140(8):1065–1071. [DOI] [PubMed] [Google Scholar]
- 44. Zhang Q, Ge H, Zhou J, Yuan C, Chen K, Cheng B. Single-row or double-row fixation technique for full-thickness rotator cuff tears: a meta-analysis. PLoS One. 2013;8(7):e68515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Zhao J, Luo M, Pan J, et al. Risk factors affecting rotator cuff retear after arthroscopic repair: a meta-analysis and systematic review. J Shoulder Elbow Surg. 2021;30(11):2660–2670. [DOI] [PubMed] [Google Scholar]