Abstract
Background:
Segmental medial meniscal allograft transplantation (MAT) has been shown to restore knee biomechanics; however, stable fixation of the transplantation is critical to avoid extrusion and maximize healing.
Purpose:
To evaluate the degree of meniscal extrusion and biomechanical function of segmental medial MAT performed with meniscocapsular sutures versus repair augmentation with knotless suture anchors.
Study Design:
Controlled laboratory study.
Methods:
Segmental midbody medial meniscectomy and subsequent segmental medial MAT were performed on 10 fresh-frozen cadaveric knees. The knees were then loaded in a dynamic tensile testing machine to 1000 N for 60 seconds at 0°, 30°, 60°, and 90° of flexion, and 4 conditions were tested: (1) intact, (2) segmental defect, (3) inside-out segmental repair, and (4) anchor plus inside-out segmental repair of the medial MAT. Meniscal extrusion was measured using high-fidelity ultrasound imaging. The mean contact area and the mean and peak contact pressures were assessed with submeniscal pressure-mapping sensors. Data from testing conditions were compared with 2-way repeated-measures analysis of variance, with pairwise comparison using the Bonferroni method.
Results:
At 90° of flexion, the segmental defect state showed a higher degree of meniscal extrusion compared with all other states (P ≤ .012). There was no difference in the degree of meniscal extrusion between the intact state and the inside-out repair or anchor plus inside-out segmental repair states at all knee flexion angles (P > .05). There was no significant difference in the mean and peak contact pressures among the 4 states at all flexion angles except that at 0° of knee flexion there was significantly lower peak contact pressure at the medial compartment after anchor plus inside-out segmental repair compared with the segmental defect state (P = .048).
Conclusion:
Meniscal extrusion was not significantly increased at any flexion angle after segmental resection. The addition of knotless anchors did not improve meniscal extrusion or contact pressures/area compared with capsular repair alone. The addition of knotless anchors did improve contact mechanics from the segmental defect state, but only at 0° of flexion.
Clinical Relevance:
The addition of knotless suture anchors to segmental meniscal transplantation increased stabilization of the meniscus at full extension compared with repair with sutures alone. This increased stabilization may lead to better long-term outcomes.
Keywords: knee, meniscus, segmental defect, allograft, transplant, suture anchor
Intact menisci are vital in achieving optimal knee kinematics and loadbearing characteristics. 12 Partial and complete meniscal deficiencies are well-studied diseases. Previous studies have shown that meniscal tissue excision after a meniscal tear subsequently increases the contact stress seen on articular cartilage in the tibiofemoral joint, which often leads to degenerative changes such as osteoarthritis (OA). 6,9,15,18 These consequences are largely attributed to altered biomechanics of the knee joint, the magnitude of which depends on the amount of meniscus removed. 9,12,18 Although partial meniscectomy may provide short-term symptomatic relief, the long-term impacts on articular cartilage in the affected knee joint remain a major problem. 5,6,12,26 Recent efforts for preventing knee arthritis have focused on restoring biomechanical forces and kinematics via meniscal repair or transplantation. 6,15,21,25,28 However, there is conflicting evidence on the efficacy of meniscal allograft transplantations (MATs) for reducing the progression of OA. 28,29
In complete meniscal transplantations, large portions of native meniscal tissue are removed. Previous studies have shown that intra-articular tissues, such as menisci, are able to generate neurosensory signals reaching spinal, cerebellar, and higher central nervous system levels. 2,3 These signals contribute to neuromuscular control and proprioception of the muscles surrounding the knee, helping to maintain normal joint function and tissue homeostasis. 4,8 A potential complication with complete meniscectomy for transplantation is the loss of these meniscal mechanoreceptors. The long-term survival rates for complete meniscal transplantations are 73.5% at 10 years and only around 60% at the 15-year follow-up, raising doubts about the chondroprotective effect of the meniscal transplantations after complete meniscectomy. 20
For patients in whom only the midbody of the meniscus is compromised, segmental meniscal transplantation preserves viable meniscal tissue and has the potential to better restore native biomechanical function. Segmental medial MAT can restore the medial compartment mean contact pressure and area similar to those of the intact medial meniscus. 9,22 The success of segmental medial MAT to restore native knee biomechanics, however, depends on stable fixation. 9,27,31 Suture-only fixation is the most common method for securing medial MAT tissue. 7 Suture-only fixation consists of fixing soft tissue grafts only through the body and meniscal horns, while meniscus roots are fixed via the transtibial suture technique. There have been previous studies looking at biomechanical and clinical differences between suture-only fixation and bone fixation for MATs with varying results. 10,33 However, no studies exist that have reported the long-term clinical outcomes comparing the suture-only technique with the bone fixation technique in MAT, and the decision of fixation types should be made on a case-by-case basis. 7
Extrusion of the entire transplanted medial meniscal allograft suggests a loss of proper mechanical function and has also been associated with poorer outcomes. A retrospective study from Krych et al 14 showed that patients with medial meniscus root tears had a significantly greater age, body mass index, radiographic OA change, and rate of major meniscal extrusion than patients with lateral meniscus root tears. They also pointed out the lower functional outcome after medial meniscus root repair compared with lateral meniscus root repair. 14 Their results may suggest that medial MAT should be performed rather than repair because of major meniscal extrusion and greater OA change. Wang et al 32 recently reported that a MAT had moderate advantages in chondroprotective effects compared with a meniscectomy when the meniscal graft was nonextruded, but grafts with >3 mm of extrusion lost complete function after meniscectomy. There have been no biomechanical evaluations comparing a suture-only technique augmented with knotless suture anchors.
The purpose of this study was to evaluate the degree of meniscal extrusion and biomechanical function of segmental medial meniscal transplantations performed with meniscocapsular sutures alone versus augmentation with knotless suture anchor fixation. We hypothesized that the segmental medial MAT augmentation with intracapsular knotless suture anchor fixation would show significantly improved restoration of meniscal extrusion, contact area, and contact pressure to the native state when compared with the segmental medial MAT performed without the use of suture anchors.
Methods
Specimen Preparation
Ten fresh-frozen cadaveric knees (mean age, 58.5 years; range, 37-65 years; 2 women, 8 men) were tested in this study. The specimens used were donated to a tissue bank for medical research and subsequently purchased by our institution. The use of cadaveric specimens does not require institutional review board approval at our institution. All specimens were prescreened via an arthroscopic examination. Specimens were excluded if there was a chondral lesion greater than grade 2 in the medial or lateral compartment, meniscal lesion, evidence of previous meniscal surgery, excess ligamentous laxity, or gross deformity.
The specimens were thawed for 24 hours before dissection and testing. All skin, subcutaneous tissue, and muscle were dissected down to the capsule, leaving the interosseous membrane, popliteus muscle and tendon, and associated knee ligaments intact. The femur was cut 15 cm proximal to the joint line, and the tibia and fibula were cut 20 cm distal to the joint line. The distal tibia and fibula were then potted in poly(methyl methacrylate) (Fricke Dental International) and fixed in a neutral anatomic position with custom fixtures on an Instron Electropuls 10000.
After this, an oblique, medial femoral condyle osteotomy was performed in order to ensure optimal pressure sensor placement and consistency of the root tear condition. A sagittal saw was used for this procedure on each specimen to facilitate access to the medial compartment per previously established protocol. 9,17 The osteotomy was secured with a removable steel plate and bicortical screws (Figure 1).
Figure 1.
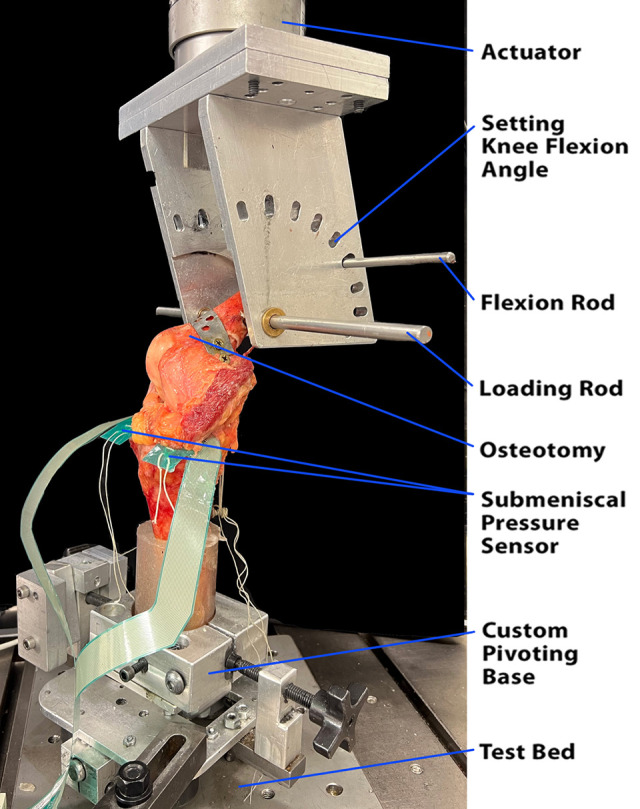
The right cadaveric knee was held at 30° of flexion and loaded in a dynamic tensile machine. Each specimen underwent an oblique medial femoral condyle osteotomy to facilitate access to the medial compartment. The osteotomy was secured with a removable steel plate and bicortical screws. A transepicondylar “loading rod” (10-mm diameter) was placed medial to lateral and acted as the loadbearing axis during testing. An additional “flexion rod” (8-mm diameter) was passed medial to lateral through the proximal femur and allowed for changes to the knee flexion angle from 0° to 90° of flexion in 30° increments. The potted distal tibia was rigidly fixed to a custom pivoting base that allowed for freedom of motion in the transverse plane and for adjustment of the tibial orientation to standardize varus and valgus positioning.
Experimental Testing States
Each specimen underwent biomechanical testing in 4 states: (1) intact medial meniscus, (2) segmental defect, (3) inside-out segmental repair (inside-out), and (4) anchor plus inside-out segmental repair (anchor plus inside-out). The compartment contact area, mean contact pressure, peak contact pressure of both the medial and lateral compartments, and medial meniscal extrusion were recorded for each state.
Surgical Techniques
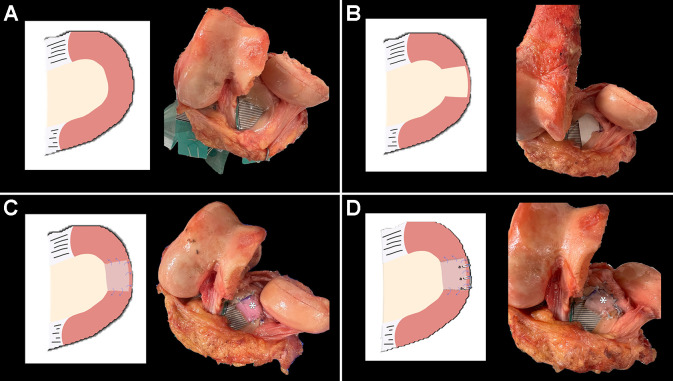
The intact meniscal state is shown in Figure 2A. The remaining 3 states are described below.
Figure 2.
Illustration and photograph of the medial meniscus of a right cadaveric knee in each testing state. (A) Intact state. (B) Segmental defect with a 15-mm tear of the midbody medial meniscus. (C) Inside-out segmental repair. A size-matched medial meniscal allograft was used on each specimen and secured in the anatomic position. Four sutures were passed at the anterior and posterior margins (2 in each margin) of the graft and secured with the remnant of the native meniscus in a horizontal mattress fashion. Then, 3 sutures were passed at the peripheral portion of the graft and repaired to the capsule 4 mm apart in a vertical mattress fashion (inside-out–type repair). (D) Anchor plus inside-out segmental repair. Segmental meniscal allograft transplantation (MAT) was augmented with 3 intracapsular knotless suture anchors placed at the rim of the medial tibial plateau 4 mm apart from each anchor. *Segmental MAT.
Segmental Defect
A 15-mm tear of the midbody medial meniscus measured from the center point of each medial meniscus was created using a No. 11 blade, resulting in a segmental tear of the medial meniscus (Figure 2B).
Inside-Out Segmental Repair
A medial meniscal allograft from a cadaveric donor source (JRF Ortho) was used on each specimen and secured in the anatomic position. A single surgeon (P.G.) performed the size matching of the medial meniscal allograft by direct measurement (width, length, and depth) compared with the native meniscus. A total of 7 No. 2-0 FiberWire sutures (Arthrex) were used to secure the segmental allograft. Four sutures were passed at the anterior and posterior margins of the graft (2 sutures in each margin) and secured with the remnant of the native meniscus (anterior and posterior horn menisci) in a horizontal mattress fashion (side-to-side native meniscus). Then, 3 sutures were passed at the peripheral portion of the graft and repaired to the capsule 4 mm apart in a vertical mattress fashion (inside-out–type repair) (Figure 2C).
Anchor Plus Inside-Out Segmental Repair
Segmental MAT was augmented with 3 intracapsular knotless suture anchors (Knotless FiberTak soft anchors; Arthrex). The anchors were placed at the rim of the medial tibial plateau with 4 mm between each anchor (Figure 2D).
Biomechanical Testing
Equilibrated electronic pressure sensors (K-scan Model 4000; 1500 psi; Tekscan Inc) were installed under the meniscus in the lateral and medial compartments, and the anterior and posterior ends of the sensors were sutured and tethered to screws anchored to the tibia to ensure consistent placement of the sensors during all trials and to ensure reproducibility of pressure measurements. The pressure-mapping sensors were calibrated by performing manufacturer-defined calibrations at 20% of the expected maximum pressure and 80% of the expected maximum pressure. At each loading value, a cork (3-mm thickness) cylinder with a contacting surface area of 314 mm2 and capped with a layer of silicone was applied to the pressure sensor, and a power calibration was performed per the manufacturer’s specifications. The sensors allowed the measuring of pressures from 0.1 to 172 MPa with an accuracy of 0.1 MPa. The sensor model is 0.1 mm thick and comprises 2 measuring fields, each with an area of 33 × 22 mm and a spatial resolution of 0.1 mm.
Each testing state was mounted to a biaxial materials testing machine (Instron Electropuls 10000). The potted portions of the distal tibia and fibula were oriented vertically and rigidly secured into a custom pivoting base. The potted portion of the femur was rigidly attached to a custom fixture mounted on the end of the actuator using a transepicondylar rod (10-mm diameter), which acted as the loadbearing axis throughout testing. An 8-mm rod was passed through the proximal femur and secured at various positions on the custom fixture to set knee flexion angles to 0°, 30°, 60°, or 90°. The specimen was initially loaded and held at 20 N of compression. The applied load was then ramped to 1000 N over 10 seconds and held at 1000 N for 60 seconds, and a snapshot of the Tekscan pressure map was captured. This protocol was used in the previous study by Haber et al. 9 The applied load was then decreased to 20 N over a 20-second period. This loading protocol was repeated at each flexion angle. The order of tests at each flexion angle for each state was randomized using a MATLAB (Version R2021a; The MathWorks) script.
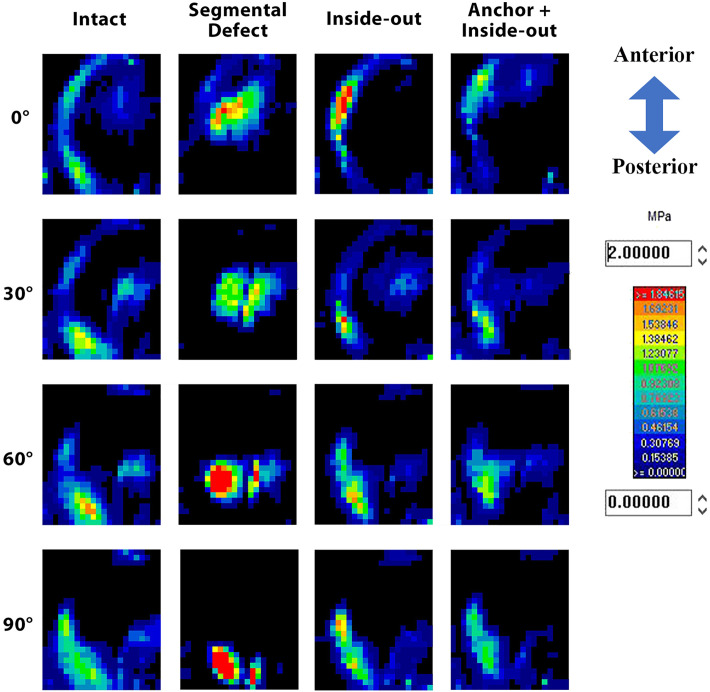
The snapshots of the Tekscan pressure maps were exported for each specimen at each flexion angle (0°, 30°, 60° and 90° of flexion) and analyzed using a custom MATLAB script. Three primary outcomes were computed for the medial compartment: mean contact pressure (mean of all nonzero Tekscan cells), mean peak contact pressure (mean of the highest 20% of pressure sensors), and contact area (Figure 3).
Figure 3.
Tekscan pressure sensor readout of a single specimen at all 4 states and all 4 knee flexion angles. The color bar on the right corresponds to the color and pressure (MPa). Inside-out, inside-out segmental repair.
Meniscal Extrusion Measurements
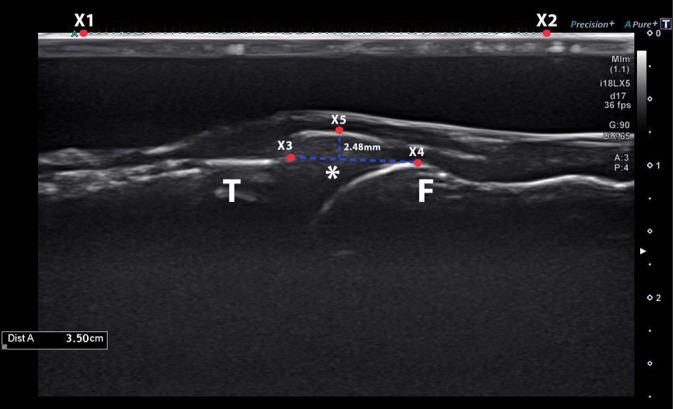
During the 1000-N compression load exerted on the specimen, the medial meniscus was examined for extrusion using ultrasound imaging (Aplio i800, with an 18-MHz transducer i18LX5 [PLI-1205BX]; Canon Medical Systems) by a board-certified orthopaedic surgeon (M.J.F.). First, a stand-off pad was positioned between the medial meniscus and the ultrasound transducer to improve image quality. The transducer was positioned at the medial aspect of the knee using longitudinal sections parallel to the medial collateral ligament. A custom sleeve was secured to the ultrasound transducer such that K-wires could be drilled through the sleeve and into the tibia. Once the medial meniscal margin, proximal tibia, and distal femur were clearly visible in the resulting ultrasound image, K-wires were drilled through the custom sleeve and into the tibia to maintain the desired position and orientation of the transducer relative to the meniscus. Three ultrasound images were captured in this position at each flexion angle for each state.
Medial meniscal extrusion was defined as the maximum distance between the medial margin of the meniscus and the line connecting the medial margin of the distal femur to the medial margin of the proximal tibia, which was calibrated by the line measurement with the ultrasound machine 11,19,23 (Figure 4). The medial meniscal extrusion was measured for all 3 ultrasound images across each testing state by 3 independent observers with varying levels of medical education (B.W.F., medical student; P.G. and M.J.F., board-certified orthopaedic surgeons) using a custom MATLAB imaging script. The final extrusion values were the mean of the values from the 3 observers. Using another MATLAB script, the intraobserver and interobserver reliabilities of the measurements were calculated with the intraclass correlation coefficient (ICC) based on the 2-way, mixed-effects, single-measure, absolute-agreement ICC format as outlined by Koo and Li. 13 Agreement, based on the 95% CIs of the ICC estimates, was classified as poor (0-0.49), moderate (0.50-0.74), good (0.75-0.89), or strong (0.90-1.00). 13
Figure 4.
An ultrasound image from a single specimen in the segmental defect state and at 60° of knee flexion. Medial meniscal extrusion was defined as the maximum distance between the medial margin of the meniscus (X5) and the line connecting the medial margin of the distal femur (X4) to the medial margin of the proximal tibia (X3), which was calibrated by the line measurement (X1 to X2) with the ultrasound machine. *Medial meniscus. F, distal femur; T, proximal tibia.
Statistical Analysis
In this study, the primary outcome was meniscal extrusion in millimeters. Secondary outcomes included the mean medial and lateral contact pressures (mm), medial and lateral contact areas (mm2), and peak medial and lateral pressures (MPa). Continuous data were reported as mean and standard deviation. Two-way repeated-measures analysis of variance (ANOVA) was used to evaluate (1) whether there was a significant interaction between meniscal states (ie, intact, segmental defect, inside-out, and anchor plus inside-out) and knee flexion angles (0°, 30°, 60°, and 90°) on the outcome variables and (2) the effects of meniscal states and flexion angles on the outcome variables. If the P value was ≤.05, a pairwise comparison of the means was determined using the Bonferroni method.
The required sample size was calculated under experimental conditions of small effect size (0.26), a mean correlation of 0.8, and an alpha of .05. A minimum of 10 specimens was needed to show a significant difference in the outcome variables with a power of 80%. 24
Statistical analysis was performed and graphs were created using the statistical software SPSS for Windows Version 18.0 (SPSS Inc) and R Version 4.2.1 (The R Foundation for Statistical Computing), respectively. A P value <.05 was considered statistically significant.
Results
Meniscal Extrusion
When the medial meniscus alone (where segmental transplantation occurred) was examined, 2-way repeated-measures ANOVA showed that the meniscal extrusion was mainly affected by the meniscal states (P < .001), the degree of meniscal extrusion was greater with increased knee flexion angles (P < .001), and there was no statistically significant interaction when considering both meniscal states and flexion angle effects on the meniscal extrusion (P = .32). The degree of meniscal extrusion decreased from segmental defect, inside-out, and anchor plus inside-out to the intact state. In addition, the overall degree of meniscal extrusion increased from 0°, 30°, and 60° of flexion to 90° (Table 1, Figure 5A).
Table 1.
Parameter Measurements for the 4 Meniscal States at Each Knee Flexion Angle a
| Parameter | 0° of Flexion | 30° of Flexion | 60° of Flexion | 90° of Flexion |
|---|---|---|---|---|
| Medial meniscal extrusion, mm | ||||
| Intact | 1.02 ± 0.86 | 1.69 ± 0.67 | 1.80 ± 0.62 | 1.99 ± 0.67 |
| Segmental medial defect | 2.08 ± 0.78 | 2.32 ± 0.96 | 2.48 ± 0.96 | 2.86 ± 0.66 |
| Inside-out | 1.55 ± 0.49 | 1.96 ± 0.54 | 1.95 ± 0.46 | 2.17 ± 0.57 |
| Anchor + inside-out | 1.44 ± 0.76 | 1.67 ± 0.76 | 2.01 ± 0.62 | 2.06 ± 0.56 |
| Medial Meniscus | ||||
| Mean contact pressure, mm | ||||
| Intact | 0.49 ± 0.15 | 0.49 ± 0.27 | 0.47 ± 0.16 | 0.60 ± 0.21 |
| Segmental medial defect | 0.65 ± 0.23 | 0.66 ± 0.23 | 0.72 ± 0.23 | 1.00 ± 0.44 |
| Inside-out | 0.53 ± 0.19 | 0.44 ± 0.25 | 0.45 ± 0.20 | 0.68 ± 0.36 |
| Anchor + inside-out | 0.53 ± 0.22 | 0.51 ± 0.30 | 0.50 ± 0.25 | 0.68 ± 0.33 |
| Contact area, mm2 | ||||
| Intact | 499.52 ± 97.78 | 422.42 ± 76.85 | 431.13 ± 72.52 | 360.32 ± 69.18 |
| Segmental medial defect | 384.19 ± 101.78 | 297.26 ± 110.11 | 281.77 ± 104.75 | 247.42 ± 78.63 |
| Inside-out | 417.42 ± 103.50 | 355.32 ± 86.94 | 359.03 ± 71.02 | 321.61 ± 77.91 |
| Anchor + inside-out | 386.45 ± 96.44 | 337.74 ± 96.00 | 341.61 ± 80.03 | 313.06 ± 56.54 |
| Peak pressure, MPa | ||||
| Intact | 3.37 ± 2.08 | 1.92 ± 1.11 | 1.76 ± 0.58 | 3.34 ± 1.88 |
| Segmental medial defect | 4.10 ± 2.63 | 2.81 ± 1.85 | 3.23 ± 2.17 | 4.23 ± 2.24 |
| Inside-out | 3.05 ± 1.73 | 1.74 ± 1.09 | 1.81 ± 0.70 | 3.24 ± 1.92 |
| Anchor + inside-out | 3.05 ± 1.85 | 2.17 ± 1.52 | 2.84 ± 2.98 | 3.87 ± 3.66 |
| Lateral Meniscus | ||||
| Mean contact pressure, mm | ||||
| Intact | 0.52 ± 0.18 | 0.37 ± 0.10 | 0.45 ± 0.12 | 0.64 ± 0.16 |
| Segmental medial defect | 0.66 ± 0.27 | 0.67 ± 0.38 | 0.86 ± 0.57 | 1.01 ± 0.52 |
| Inside-out | 0.47 ± 0.09 | 0.30 ± 0.09 | 0.45 ± 0.22 | 0.60 ± 0.21 |
| Anchor + inside-out | 0.43 ± 0.21 | 0.34 ± 0.11 | 0.47 ± 0.21 | 0.61 ± 0.27 |
| Contact area, mm2 | ||||
| Intact | 520.81 ± 66.28 | 461.77 ± 63.74 | 441.45 ± 46.57 | 380.48 ± 57.10 |
| Segmental medial defect | 387.58 ± 57.34 | 330.64 ± 145.70 | 320.97 ± 141.72 | 275.32 ± 110.55 |
| Inside-out | 422.10 ± 87.92 | 450.81 ± 65.98 | 401.77 ± 90.44 | 343.23 ± 54.24 |
| Anchor + inside-out | 445.32 ± 72.76 | 436.93 ± 68.26 | 417.90 ± 80.23 | 343.39 ± 61.95 |
| Peak pressure, MPa | ||||
| Intact | 2.17 ± 1.09 | 1.47 ± 0.71 | 2.09 ± 1.28 | 2.57 ± 1.26 |
| Segmental medial defect | 2.79 ± 1.61 | 2.19 ± 1.25 | 3.39 ± 2.77 | 4.27 ± 2.98 |
| Inside-out | 1.85 ± 0.42 | 1.54 ± 0.62 | 1.97 ± 1.20 | 2.63 ± 1.37 |
| Anchor + inside-outs | 2.06 ± 1.06 | 1.93 ± 1.27 | 2.00 ± 1.21 | 2.92 ± 2.09 |
a Data are reported as mean ± SD. Inside-out, inside-out segmental repair.
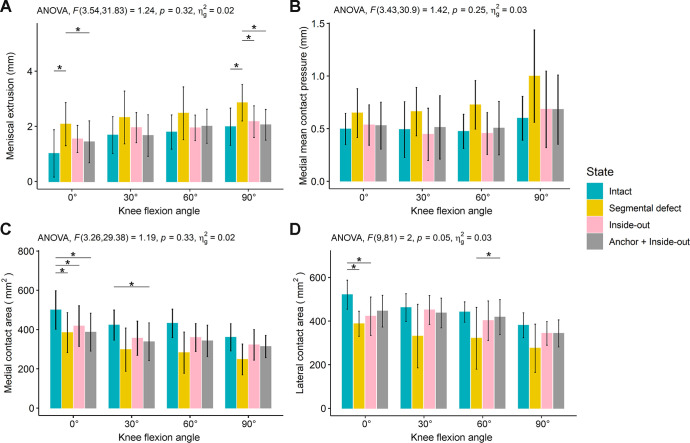
Figure 5.
Bar charts showing the (A) medial meniscal extrusion, (B) medial mean contact pressure, (C) medial contact area, and (D) lateral contact area among the different meniscal states at each knee flexion angle. Bars indicate mean values, and error bars indicate standard deviations. *Statistically significant difference between 2 states (P < .05, Bonferroni test for pairwise comparison). Inside-out, inside-out segmental repair. ANOVA, analysis of variance.
The pairwise comparisons demonstrated that at 0° of flexion, the segmental defect showed a statistically significantly higher degree of meniscal extrusion (2.08 ± 0.78 mm) compared with intact (1.02 ± 0.86 mm; P = .039) and anchor plus inside-out (1.44 ± 0.76 mm; P = .044). The segmental defect state also showed a higher degree of meniscal extrusion compared with other states (intact, inside-out, and anchor plus inside-out) at 90° of flexion (P = .0003, .0001, and .012, respectively) (Table 2, Figure 5A). The degree of meniscal extrusion in the intact state was not significantly different from that of the inside-out state or anchor plus inside-out state at all knee flexion angles (P > .05). There was also no significant difference in the degree of meniscal extrusion between the inside-out and anchor plus inside-out states at all knee flexion angles (P = .9).
Table 2.
Bonferroni P Values for Pairwise Comparisons of All Parameters Between Meniscal States at Different Knee Flexion Angles a
| Medial Meniscus | Lateral Meniscus | ||||||
|---|---|---|---|---|---|---|---|
| Pairwise Comparison b | Meniscal Extrusion, mm | Mean Contact Pressure, mm | Contact Area, mm2 | Peak Pressure, MPa | Mean Contact Pressure, mm | Contact Area, mm2 | Peak Pressure, MPa |
| 0° of Flexion | |||||||
| (1) vs (2) | .039 | .059 | .003 | .99 | .80 | .003 | .99 |
| (1) vs (3) | .085 | .99 | .008 | .99 | .99 | .013 | .99 |
| (1) vs (4) | .46 | .99 | .015 | .99 | .99 | .13 | .99 |
| (2) vs (3) | .082 | .34 | .99 | .20 | .48 | .99 | .33 |
| (2) vs (4) | .044 | .50 | .99 | .048 | .32 | .19 | .91 |
| (3) vs (4) | .9 | .99 | .99 | .99 | .99 | .99 | .99 |
| 30° of Flexion | |||||||
| (1) vs (2) | .2 | .30 | .058 | .51 | .11 | .059 | .33 |
| (1) vs (3) | .6 | .49 | .062 | .99 | .77 | .99 | .99 |
| (1) vs (4) | .9 | .99 | .017 | .99 | .99 | .94 | .99 |
| (2) vs (3) | .9 | .098 | .29 | .079 | .059 | .13 | .66 |
| (2) vs (4) | .052 | .28 | .99 | .98 | .098 | .089 | .96 |
| (3) vs (4) | .9 | .99 | .99 | .99 | .99 | .99 | .96 |
| 60° of Flexion | |||||||
| (1) vs (2) | .052 | .082 | .051 | .41 | .23 | .17 | .54 |
| (1) vs (3) | .9 | .99 | .24 | .99 | .99 | .99 | .99 |
| (1) vs (4) | .9 | .99 | .061 | .99 | .99 | .99 | .99 |
| (2) vs (3) | .1 | .16 | .29 | .51 | .089 | .40 | .35 |
| (2) vs (4) | .8 | .098 | .99 | .99 | .15 | .03 | .34 |
| (3) vs (4) | .9 | .99 | .99 | .99 | .99 | .99 | .99 |
| 90° of Flexion | |||||||
| (1) vs (2) | .0003 | .086 | .095 | .93 | .30 | .13 | .53 |
| (1) vs (3) | .7 | .99 | .36 | .99 | .99 | .55 | .99 |
| (1) vs (4) | .9 | .99 | .24 | .99 | .99 | .18 | .99 |
| (2) vs (3) | .0001 | .38 | .42 | .78 | .084 | .56 | .13 |
| (2) vs (4) | .012 | .10 | .41 | .99 | .23 | .34 | .67 |
| (3) vs (4) | .9 | .99 | .99 | .99 | .99 | .99 | .99 |
a Boldface P values indicate a statistically significant difference between comparisons (P < .05).
b (1) = intact state; (2) = segmental defect state; (3) = inside-out segmental repair state; (4) = anchor plus inside-out segmental repair state.
The overall intra- and interrater reliabilities of meniscal extrusion measurements for the 3 observers are listed in Table 3. Three observers showed good to strong intrarater reliabilities for 3 meniscal states (intact, segmental defect, and anchor plus inside-out) and moderate to strong intrarater reliabilities for inside-out repair state measurement. With regard to the interrater reliabilities of the extrusion measurement, the ICC values demonstrated moderate-to-strong reliabilities for the intact (ICC, 0.72-0.90) and segmental defect (ICC, 0.62-0.94) states. There was moderate-to-good agreement in the anchor plus inside-out state (ICC, 0.60-0.78) but a moderate agreement for the inside-out state (ICC, 0.56-0.59).
Table 3.
Inter- and Intraobserver Reliabilities of the Medial Meniscal Extrusion Measurements a
| Intraobserver | ||||
|---|---|---|---|---|
| Meniscal State | Observer 1 | Observer 2 | Observer 3 | Interobserver b |
| Intact | ||||
| 0° of flexion | 0.969 (0.914-0.992) | 0.881 (0.705-0.965) | 0.945 (0.853-0.985) | 0.896 (0.732-0.971) |
| 30° of flexion | 0.910 (0.766-0.975) | 0.935 (0.828-0.982) | 0.887 (0.713-0.968) | 0.817 (0.549-0.947) |
| 60° of flexion | 0.877 (0.693-0.965) | 0.897 (0.741-0.971) | 0.842 (0.626-0.953) | 0.872 (0.686-0.963) |
| 90° of flexion | 0.900 (0.741-0.972) | 0.948 (0.861-0.986) | 0.926 (0.802-0.979) | 0.718 (0.394-0.912) |
| Segmental medial defect | ||||
| 0° of flexion | 0.917 (0.787-0.977) | 0.847 (0.622-0.955) | 0.952 (0.868-0.987) | 0.874 (0.655-0.965) |
| 30° of flexion | 0.983 (0.953-0.995) | 0.980 (0.944-0.995) | 0.953 (0.873-0.987) | 0.919 (0.693-0.980) |
| 60° of flexion | 0.939 (0.838-0.983) | 0.935 (0.823-0.982) | 0.937 (0.834-0.982) | 0.939 (0.837-0.983) |
| 90° of flexion | 0.925 (0.801-0.979) | 0.923 (0.799-0.978) | 0.959 (0.883-0.989) | 0.618 (0.269-0.871) |
| Inside-out | ||||
| 0° of flexion | 0.859 (0.650-0.959) | 0.778 (0.507-0.932) | 0.882 (0.705-0.966) | 0.564 (0.195-0.848) |
| 30° of flexion | 0.867 (0.670-0.961) | 0.813 (0.564-0.944) | 0.929 (0.805-0.980) | 0.582 (0.125-0.866) |
| 60° of flexion | 0.704 (0.377-0.906) | 0.749 (0.436-0.923) | 0.788 (0.511-0.936) | 0.589 (0.114-0.871) |
| 90° of flexion | 0.772 (0.496-0.930) | 0.895 (0.733-0.970) | 0.830 (0.598-0.950) | 0.570 (0.095-0.863) |
| Anchor + inside-out | ||||
| 0° of flexion | 0.869 (0.672-0.962) | 0.809 (0.555-0.943) | 0.861 (0.658-0.960) | 0.780 (0.500-0.933) |
| 30° of flexion | 0.903 (0.751-0.972) | 0.900 (0.746-0.971) | 0.903 (0.751-0.973) | 0.772 (0.406-0.934) |
| 60° of flexion | 0.851 (0.640-0.956) | 0.852 (0.645-0.957) | 0.865 (0.673-0.961) | 0.647 (0.214-0.890) |
| 90° of flexion | 0.925 (0.805-0.979) | 0.757 (0.453-0.926) | 0.809 (0.556-0.943) | 0.602 (0.214-0.867) |
a Data are reported as intraclass correlation coefficient (95% CI).
b Interobserver reliability was assessed from the measurements between the 3 observers.
Contact Pressure
For examination of the medial meniscus alone, there were no significant differences in the mean contact pressure and peak contact pressure among the intact, segmental defect, inside-out, or anchor plus inside-out states from the pairwise comparisons at all knee flexion angles (Figure 5B), except at 0° of flexion, in which there was a significantly lower peak pressure at the medial compartment after the anchor plus inside-out state compared with the segmental defect state (3.05 ± 1.85 vs 4.10 ± 2.63 MPa; P = .048) (Tables 1 and 2). When the lateral meniscus alone was examined, there were no significant differences in mean and peak contact pressures in the lateral compartment.
Contact Area
At 0° of flexion, the medial contact area of the intact state was significantly higher than the segmental defect (P = .003), inside-out (P = .008), and anchor plus inside-out (P = .015) states. There was also less medial contact area in the anchor plus inside-out versus the intact (P = .017) state at 30° of flexion (Figure 5C). However, there was no significant difference in terms of medial contact area at 60° and 90° of flexion between each state.
When the lateral meniscus alone was calculated, the lateral contact area of the intact state was significantly higher than the segmental defect (P = .003) and inside-out (P = .013) at 0° of flexion. The lateral contact area after anchor plus inside-out repair was not significantly different from the intact state (P = .13) at 0° of flexion. In addition, anchor plus inside-out repair demonstrated a significantly higher lateral contact area compared with the segmental defect state (P = .03) and no difference between the intact and inside-out states at 60° of flexion (Table 2, Figure 5D).
Discussion
The most important finding of this study is that the addition of knotless anchors did not improve meniscal extrusion or contact pressures or area compared with capsular repair alone. Segmental medial meniscal transplantation with or without intracapsular knotless suture anchors showed a robust repair and restored meniscal extrusion to values measured in the intact state. There was no difference in the degree of meniscal extrusion between the intact and inside-out segmental repair or anchor plus inside-out segmental repair states at all knee flexion angles. Thus, in terms of meniscal extrusion, the knotless anchors provided a limited benefit over inside-out repair. With the addition of knotless anchors, segmental meniscal transplantation mechanics may be improved at full knee extension (a lower peak contact pressure and better restoration of lateral contact area compared with the segmental defect state).
The fundamental purpose of MAT is to restore biomechanics and normal coverage of the tibial plateau. A large amount of meniscal extrusion or decreased size of allograft may decrease the coverage area to the tibial plateau. The most commonly reported classification defines the degree of extrusion as no extrusion, minor extrusion (<3 mm), and major extrusion (>3 mm) regarding the rim of the tibial plateau. 1,28 From the results of our study, most of the medial meniscal extrusions were minor extrusions, even in the segmental defect state. However, the degree of meniscal extrusion appeared to increase over time in an MAT clinical study. 30 In addition, there is still controversy regarding the association between the degree of meniscal extrusion after meniscal transplantation and functional outcome in the literature. A systemic review by Smith et al 28 showed that most studies reported meniscal extrusion after the entire MAT with a mean extrusion between 1.7 and 5.8 mm (at a minimum follow-up of 6 months) or 19.4% and 56.7% (relative percentage of meniscal allograft). They concluded that there was no direct correlation between clinical and radiologic outcomes and the degree of meniscal extrusion after MAT. Long-term clinical and radiologic results after the entire MAT from Verdonk et al 30 demonstrated a 59% rate of progression of meniscal extrusion from the initial study at the final follow-up (mean, 11.9 years) with magnetic resonance imaging (MRI). From their results, the degree of meniscal extrusion after MAT increased with time. However, they found no significant correlation between clinical outcomes, status of cartilage degeneration, and amount of meniscal extrusion. 30 In contrast, a few studies demonstrated poorer clinical outcomes in patients with major meniscal extrusion after MAT. 16,32 Wang et al 32 conducted a long-term cohort study of patients who underwent MAT (mean follow-up time, 11.3 years) and found that the nonextrusion subgroup of MAT (extrusion, <3 mm with coronal MRI) had moderate superiority in chondral protection (less joint space narrowing and increasing cartilage degeneration index [CDI]) compared with meniscectomy. Conversely, the extrusion subgroup of MAT in their cohort (extrusion, >3 mm) showed similar joint space narrowing and CDI to the meniscectomy group, demonstrating that extrusion >3 mm resulted in complete loss of function of the meniscal chondroprotective effect at the long-term follow-up after MAT. 32 A long-term study from Lee et al 16 revealed a greater joint space narrowing in the extrusion group (–1.25 ± 0.78 mm) compared with the nonextrusion group (–0.58 ± 0.66 mm) at >8 years of follow-up (P < .001); however, there was no significant difference in clinical outcome between the groups. Despite that, most of the previous literature has reported both medial and lateral MATs in their outcome studies. The authors believe that the side of the MAT or the repair technique might have an effect on the degree of meniscal extrusion and outcomes. Our study showed that segmental medial MAT with or without intracapsular knotless suture anchor can restore the degree of medial meniscal extrusion to the native state at time zero, which was <3 mm of meniscal extrusion of all knee flexion angles. A longer in vivo study is needed to assess the chondroprotective effect after adding a knotless suture anchor for MAT.
A successful segmental MAT restores native knee biomechanics; however, it depends on stable fixation, especially at peripheral fixation (between the graft and capsule). 25 The graft should be secured and attached to the capsule for improved healing potential and vascularization of the graft. There are various meniscal repair techniques for MAT; however, the systematic review of Rosso et al 25 reported no superiority of one technique over another. Haber et al 9 conducted segmental medial MAT in 10 cadaveric knees and showed that segmental medial MAT can restore the medial compartment contact area and mean contact pressure to values measured in the intact state. The result from their group also demonstrated that the addition of a transtibial pull-out repair to the inside-out repair had a similar biomechanical effect and no advantage compared with the inside-out repair. 9 Our study also showed that segmental medial MAT with or without intracapsular knotless suture anchor had no significant differences in the mean and peak contact pressures in both the medial and lateral compartments and restored medial contact area at 60° and 90° of knee flexion. The results from this study support those of Haber et al, 9 who reported segmental medial MAT restored the medial compartment mean contact pressure and mean contact area to values measured in the intact medial compartment. However, the addition of a knotless suture anchor may offer some benefit at 0° of flexion (lower the medial compartment peak pressure and improve lateral contact area compared with the segmental defect state). However, the contact pressures and area with the additional knotless anchors were not significantly different from capsular repair alone.
Limitations
This cadaveric model included more men (8 knees) than women; therefore, the findings of this study cannot be fully generalized to the general population. Furthermore, all meniscal extrusion measurements in this study were made with ultrasound images, which depended on the operator. To mitigate this error, 1 board-certified orthopaedic surgeon who is well-trained in ultrasound imaging performed all image capture. Furthermore, 3 independent observers measured all meniscal extrusion and calculated for inter- and intrarater reliabilities. However, the effect of reliability on a very small measurement, including beta error, can be anticipated. Additionally, the amount of meniscal extrusion in this study was measured in only 1 coronal plane with ultrasound measurement. MRI can offer the measurement in both the coronal and sagittal planes; however, the meniscal extrusion measured on MRI is often nonloadbearing. On the contrary, extrusion is measured with loadbearing on ultrasound. Therefore, the amount of extrusion in this study may not correlate with that in other clinical studies that utilize MRI. Finally, this study demonstrated the degree of extrusion and biomechanics effect at time zero. The degree of meniscal extrusion appears to increase over time in MAT clinical studies. Additional in vivo studies may be beneficial to understand the effect of knotless suture anchors after segmental medial MAT.
Conclusion
Meniscal extrusion was not significantly increased at any knee flexion angle after segmental resection. The addition of knotless anchors did not improve meniscal extrusion or contact pressures or area compared with capsular repair alone. The addition of knotless anchors did improve contact mechanics from the segmental defect state but only at 0° of flexion.
Acknowledgment
The authors acknowledge the Steadman Philippon Research Institute Digital Media Department for the illustrations and Ms Narumol Sudjai from the Faculty of Medicine Siriraj Hospital, Mahidol University, for statistical analysis.
Footnotes
Final revision submitted March 15, 2023; accepted April 5, 2023.
One or more of the authors has declared the following potential conflict of interest or source of funding: M.J.F. has received education payments from Smith & Nephew. M.T.P. has received education payments from Arthrex; consulting fees from Arthrex, JRF Ortho, and Zimmer Biomet; nonconsulting fees from Arthrex and Arthrosurface; royalties from Anika Therapeutics, Arthrex, and Arthrosurface; and honoraria from Flexion Therapeutics and JRF Ortho. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval was not sought for the present study.
References
- 1. Abat F, Gelber PE, Erquicia JI, et al. Suture-only fixation technique leads to a higher degree of extrusion than bony fixation in meniscal allograft transplantation. Am J Sports Med. 2012;40(7):1591–1596. [DOI] [PubMed] [Google Scholar]
- 2. Assimakopoulos AP, Katonis PG, Agapitos MV, Exarchou EI. The innervation of the human meniscus. Clin Orthop Relat Res. 1992;(275):232–236. [PubMed] [Google Scholar]
- 3. Day B, Mackenzie WG, Shim SS, Leung G. The vascular and nerve supply of the human meniscus. Arthroscopy. 1985;1(1):58–62. [DOI] [PubMed] [Google Scholar]
- 4. Dye SF, Vaupel GL, Dye CC. Conscious neurosensory mapping of the internal structures of the human knee without intraarticular anesthesia. Am J Sports Med. 1998;26(6):773–777. [DOI] [PubMed] [Google Scholar]
- 5. Edd SN, Netravali NA, Favre J, Giori NJ, Andriacchi TP. Alterations in knee kinematics after partial medial meniscectomy are activity dependent. Am J Sports Med. 2015;43(6):1399–1407. [DOI] [PubMed] [Google Scholar]
- 6. Faucett SC, Geisler BP, Chahla J, et al. Meniscus root repair vs meniscectomy or nonoperative management to prevent knee osteoarthritis after medial meniscus root tears: clinical and economic effectiveness. Am J Sports Med. 2019;47(3):762–769. [DOI] [PubMed] [Google Scholar]
- 7. Figueroa F, Figueroa D, Calvo R, Vaisman A, Espregueira-Mendes J. Meniscus allograft transplantation: indications, techniques and outcomes. EFORT Open Rev. 2019;4(4):115–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Fox AJ, Bedi A, Rodeo SA. The basic science of human knee menisci: structure, composition, and function. Sports Health. 2012;4(4):340–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Haber DB, Douglass BW, Arner JW, et al. Biomechanical analysis of segmental medial meniscal transplantation in a human cadaveric model. Am J Sports Med. 2021;49(12):3279–3286. [DOI] [PubMed] [Google Scholar]
- 10. Jauregui JJ, Wu ZD, Meredith S, et al. How should we secure our transplanted meniscus? A meta-analysis. Am J Sports Med. 2018;46(9):2285–2290. [DOI] [PubMed] [Google Scholar]
- 11. Jones LD, Mellon SJ, Kruger N, et al. Medial meniscal extrusion: a validation study comparing different methods of assessment. Knee Surg Sports Traumatol Arthrosc. 2018;26(4):1152–1157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Koh JL, Yi SJ, Ren Y, Zimmerman TA, Zhang LQ. Tibiofemoral contact mechanics with horizontal cleavage tear and resection of the medial meniscus in the human knee. J Bone Joint Surg Am. 2016;98(21):1829–1836. [DOI] [PubMed] [Google Scholar]
- 13. Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. 2016;15(2):155–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Krych AJ, Bernard CD, Kennedy NI, et al. Medial versus lateral meniscus root tears: is there a difference in injury presentation, treatment decisions, and surgical repair outcomes? Arthroscopy. 2020;36(4):1135–1141. [DOI] [PubMed] [Google Scholar]
- 15. Lee BS, Bin SI, Kim JM. Articular cartilage degenerates after subtotal/total lateral meniscectomy but radiographic arthrosis progression is reduced after meniscal transplantation. Am J Sports Med. 2016;44(1):159–165. [DOI] [PubMed] [Google Scholar]
- 16. Lee SM, Bin SI, Kim JM, et al. Long-term outcomes of meniscal allograft transplantation with and without extrusion: mean 12.3-year follow-up study. Am J Sports Med. 2019;47(4):815–821. [DOI] [PubMed] [Google Scholar]
- 17. Marzo JM, Gurske-DePerio J. Effects of medial meniscus posterior horn avulsion and repair on tibiofemoral contact area and peak contact pressure with clinical implications. Am J Sports Med. 2009;37(1):124–129. [DOI] [PubMed] [Google Scholar]
- 18. Muriuki MG, Tuason DA, Tucker BG, Harner CD. Changes in tibiofemoral contact mechanics following radial split and vertical tears of the medial meniscus: an in vitro investigation of the efficacy of arthroscopic repair. J Bone Joint Surg Am. 2011;93(12):1089–1095. [DOI] [PubMed] [Google Scholar]
- 19. Nogueira-Barbosa MH, Gregio-Junior E, Lorenzato MM, et al. Ultrasound assessment of medial meniscal extrusion: a validation study using MRI as reference standard. Am J Roentgenol. 2015;204(3):584–588. [DOI] [PubMed] [Google Scholar]
- 20. Novaretti JV, Patel NK, Lian J, et al. Long-term survival analysis and outcomes of meniscal allograft transplantation with minimum 10-year follow-up: a systematic review. Arthroscopy. 2019;35(2):659–667. [DOI] [PubMed] [Google Scholar]
- 21. Noyes FR, Barber-Westin SD. Long-term survivorship and function of meniscus transplantation. Am J Sports Med. 2016;44(9):2330–2338. [DOI] [PubMed] [Google Scholar]
- 22. Nyland J, Campbell K, Kalloub A, et al. Medial meniscus grafting restores normal tibiofemoral contact pressures. Arch Orthop Trauma Surg. 2018;138(3):361–367. [DOI] [PubMed] [Google Scholar]
- 23. Paletta GA, Jr, Crane DM, Konicek J, et al. Surgical treatment of meniscal extrusion: a biomechanical study on the role of the medial meniscotibial ligaments with early clinical validation. Orthop J Sports Med. 2020;8(7):2325967120936672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Potvin PJ, Schutz RW. Statistical power for the two-factor repeated measures ANOVA. Behav Res Methods Instrum Comput. 2000;32(2):347–356. [DOI] [PubMed] [Google Scholar]
- 25. Rosso F, Bisicchia S, Bonasia DE, Amendola A. Meniscal allograft transplantation: a systematic review. Am J Sports Med. 2015;43(4):998–1007. [DOI] [PubMed] [Google Scholar]
- 26. Salata MJ, Gibbs AE, Sekiya JK. A systematic review of clinical outcomes in patients undergoing meniscectomy. Am J Sports Med. 2010;38(9):1907–1916. [DOI] [PubMed] [Google Scholar]
- 27. Seiter MN, Haber DB, Ruzbarsky JJ, et al. Segmental meniscus allograft transplantation. Arthrosc Tech. 2021;10(3):e697–e703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Smith NA, Parkinson B, Hutchinson CE, Costa ML, Spalding T. Is meniscal allograft transplantation chondroprotective? A systematic review of radiological outcomes. Knee Surg Sports Traumatol Arthrosc. 2016;24(9):2923–2935. [DOI] [PubMed] [Google Scholar]
- 29. Van Der Straeten C, Byttebier P, Eeckhoudt A, Victor J. Meniscal allograft transplantation does not prevent or delay progression of knee osteoarthritis. PLoS One. 2016;11(5):e0156183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Verdonk PC, Verstraete KL, Almqvist KF, et al. Meniscal allograft transplantation: long-term clinical results with radiological and magnetic resonance imaging correlations. Knee Surg Sports Traumatol Arthrosc. 2006;14(8):694–706. [DOI] [PubMed] [Google Scholar]
- 31. Waltz RA, Casp AJ, Provencher MT, Vidal AF, Godin JA. Arthroscopic segmental medial meniscus allograft transplant using three fixation techniques. Arthrosc Tech. 2021;10(11):e2507–e2513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Wang DY, Zhang B, Li YZ, et al. The long-term chondroprotective effect of meniscal allograft transplant: a 10- to 14-year follow-up study. Am J Sports Med. 2022;50(1):128–137. [DOI] [PubMed] [Google Scholar]
- 33. Wang H, Gee AO, Hutchinson ID, et al. Bone plug versus suture-only fixation of meniscal grafts: effect on joint contact mechanics during simulated gait. Am J Sports Med. 2014;42(7):1682–1689. [DOI] [PMC free article] [PubMed] [Google Scholar]