Abstract
Context:
Several studies have compared perceptual responses between resistance exercise with blood flow restriction and traditional resistance exercise (non-BFR). However, the results were contradictory.
Objectives:
To analyze the effect of RE+BFR versus non-BFR resistance exercise [low-load resistance exercise (LL-RE) or high-load resistance exercise (HL-RE)] on perceptual responses.
Data Sources:
CINAHL, Cochrane Library, PubMed®, Scopus, SPORTDiscus, and Web of Science were searched through August 28, 2021, and again on August 25, 2022.
Study Selection:
Studies comparing the effect of RE+BFR versus non-BFR resistance exercise on rate of perceived exertion (RPE) and muscle pain/discomfort were considered. Meta-analyses were conducted using the random effects model.
Study Design:
Systematic review and meta-analysis.
Level of Evidence:
Level 2.
Data Extraction:
All data were reviewed and extracted independently by 2 reviewers. Disagreements were resolved by a third reviewer.
Results:
Thirty studies were included in this review. In a fixed repetition scheme, the RPE [standardized mean difference (SMD) = 1.04; P < 0.01] and discomfort (SMD = 1.10; P < 0.01) were higher in RE+BFR than in non-BFR LL-RE, but similar in sets to voluntary failure. There were no significant differences in RPE in the comparisons between RE+BFR and non-BFR HL-RE; after sensitivity analyses, it was found that the RPE was higher in non-BFR HL-RE in a fixed repetition scheme. In sets to voluntary failure, discomfort was higher in RE+BFR versus non-BFR HL-RE (SMD = 0.95; P < 0. 01); however, in a fixed scheme, the results were similar.
Conclusion:
In sets to voluntary failure, RPE is similar between RE+BFR and non-BFR exercise. In fixed repetition schemes, RE+BFR seems to promote higher RPE than non-BFR LL-RE and less than HL-RE. In sets to failure, discomfort appears to be similar between LL-RE with and without BFR; however, RE+BFR appears to promote greater discomfort than HL-RE. In fixed repetition schemes, the discomfort appears to be no different between RE+BFR and HL-RE, but is lower in non-BFR LL-RE.
Keywords: blood flow restriction therapy, KAATSU training, vascular occlusion, rate of perceived exertion, strength training, vascular occlusion
Low-load resistance training [20-50% 1 repetition maximum (1RM)] programs associated with arterial blood flow restriction (BFR) of the exercised limb can generate neuromuscular adaptations similar to high-load resistance training (80% 1RM) without BFR (non-BFR), and superior to non-BFR low-load nonfailure resistance training.26,69 Therefore, low-load resistance training with BFR can be an alternative for people with limitations in performing high-load resistance training, such as injured athletes 36 or frail elderly. 38 In addition, resistance training with BFR was suggested as a training option for athletes seeking to maximize muscle hypertrophy 57 or for bodybuilders in precompetitive periods when there is a need to train with a high caloric deficit. 1
Low-load resistance exercise (LL-RE) with BFR promotes greater metabolic, neuromuscular, and hormonal changes than non-BFR low-load nonfailure resistance exercise.68,72 In addition, some studies have shown that BFR application increases rate of perceived exertion (RPE) reported in LL-RE.18,73 It is speculated that this increase in RPE is mediated by greater accumulation of fatigue during BFR exercise compared with LL-RE. It is assumed that under these conditions, there is an increase in corollary discharge (a copy of the signal sent to the activated muscle), resulting in activation of a greater number of motor units (MUs), especially high-threshold MUs that contain more type II fibers to maintain force levels. 56 Therefore, the level of effort experienced during BFR exercise may be associated with the chronic adaptations caused by the technique.
A considerable number of studies have evaluated RPE in resistance exercise with BFR; however, results are controversial because some studies have shown a higher,18,73 similar, 71 or even lower 29 RPE in LL-RE with BFR compared with no-BFR LL-RE. When comparing LL-RE with BFR and non-BFR high-load resistance exercise (HL-RE), there are also conflicting results.23,29 For example, Lixandrão et al 29 identified higher RPE in non-BFR HL-RE than in LL-RE with BFR. In contrast, Hollander et al 23 identified similar RPE between LL-RE (30% 1RM) with BFR and non-BFR HL-RE (70% 1RM).
It is worth noting that divergent results extend to studies that analyzed the effect of LL-RE with BFR on other perceptual responses.6,29 Bordessa et al 6 identified higher muscle pain ratings in LL-RE with BFR than in non-BFR HL-RE, whereas Lixandrão et al 29 identified an opposite response, that is, lower pain ratings in low-load exercise with BFR. The divergences presented can be justified by some factors in cuff application and methodology, including occlusion pressure applied in the exercise, 63 repetition schemes (failure versus nonfailure), 60 and device used to generate the BFR.6,45 Understanding the factors that affect perceptual responses in BFR training can be useful for professionals who use the technique in clinical settings, especially when it comes to long-term adherence to the intervention, 56 because exercise intolerance may limit the use of BFR training. Furthermore, analyses of perceptual responses can provide relevant information about the physiological demands of exercise relative to traditional loading approaches. Therefore, this study aims to systematically review and meta-analyze the available evidence on the effect of LL-RE with BFR versus non-BFR resistance exercise (high or low load) on perceptual responses and discuss methodological factors that may contribute to the discrepancies presented about the topic.
Methods
This systematic review was reported in accordance with the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) recommendations. 50 The review methods were established before initiating the research, and protocol registration preceded the search.
Eligibility Criteria
Randomized studies that analyzed the following criteria were eligible for inclusion: population, adults (age ≥18 years); intervention, low-load (≤50% 1RM) resistance exercise with BFR of the exercised limb; comparators, non-BFR LL- or HL-RE (≤50% 1RM or ≥60% 1RM, respectively); outcomes, RPE, perception of discomfort or muscle pain reported during or immediately after exercise, evaluated through psychometric scales.
Reviews, study protocols, case reports, nonrandomized studies, expert opinion, studies that did not include a non-BFR resistance exercise as a control, isokinetic exercise protocols, and elastic resistance exercise protocols were not considered for analysis. In addition, we opted for the exclusion of studies that evaluated people with neurological and rheumatic diseases as well as those with orthopedic issues secondary to injury or postsurgical recovery.
Information Sources
The literature search was conducted in the following databases: CINAHL (via EBSCO), Cochrane Library, National Library of Medicine (PubMed), Scopus (via Elsevier), SPORTDiscus (via EBSCO), and Web of Science (via Clarivate Analytics). The search was conducted after the protocol submission. In addition, the reference list of eligible studies for this review was screened to identify potential studies that were not identified in the consulted databases. Searches were performed on August 28, 2021, and updated on August 25, 2022.
Search Strategy
The search strategy combined the following descriptors and Boolean operators (AND/OR): (“resistance training” OR “resistance exercise” OR “strength training” OR “strength exercise”) AND (“blood flow restriction” OR “vascular occlusion” OR KAATSU OR ischemia) AND (“muscle discomfort” OR “muscle pain” OR exertion OR “physical exertion” OR “physical effort” OR “rating of perceived exertion” OR “perceived exertion” OR “perceptual responses”). No additional filters or search limitations were used.
Selection Process and Data Extraction
The selection process was performed by 2 reviewers (VSQ and RJL) blindly and independently. Disagreements between reviewers were resolved by a third reviewer (IKS). The screening process was divided into 3 stages: (1) elimination of duplicates; (2) reading of titles and abstracts; and (3) reading of full articles. The Rayyan QCRI® (Rayyan QCRI, Qatar Computing Research Institute, HBKU) 49 was used to eliminate duplicates and assist in the screening of titles and abstracts. The Cohen κ statistic was used to assess interreviewer agreement in step 3 of the screening.
After a complete reading of the studies, 2 reviewers (VSQ and RJL) extracted data from the eligible studies. The following information was extracted: sample size, study design, participant characteristics (sex, age, weight, height, resistance training experience), scale used to measure outcomes of interest, exercise(s) tested, and characteristics of exercise [load (1RM%), volume of repetitions, rest interval intersets] and limb BFR(pressure and cuff width). In addition, descriptive data of mean and SD were extracted. When data were reported as median and interquartile range (IQR), the median was considered and the SD estimated from the IQR (SD = IQR/1.35). 21 When results were reported in graphs or were not available in the manuscript, the corresponding author was contacted via email. Data not available were estimated from graphs using the ImageJ software (https://imagej.nih.gov/ij/), as was done in previously published systematic reviews.9,10
Risk of Bias Assessment
The methodological quality of the studies included in this review was assessed by 2 researchers (VSQ, IMF) independently and blindly, using the Cochrane risk of bias tool for randomized clinical trials, version 2 (RoB 2). RoB 2 assesses bias through 5 domains: (1) bias due to the randomization process; (2) bias due to deviations from the intended interventions; (3) bias due to lack of outcome data; (4) bias in the measurement of the result; (5) bias in the selection of the reported result. For crossover studies, the scale has an additional domain, “period and carryover effects.” The judgments of the risk of bias for each domain are “low risk of bias,” “some concerns,” or “high risk of bias.” 64
Data Synthesis and Analysis
Data analyses was performed using Review Manager software, version 5.4 (RevMan 5.4, Cochrane Collaboration). The mean and SD of the final set performed in each training session were chosen for the analyses, as performed in a previously published systematic review. 61 When the study reported both local and overall RPE values, only the overall RPE was considered for the analyses. The standardized mean difference (SMD) and SE were extracted from individual studies and pooled using the generic inverse variance method. SMD outcomes between ≥0.2 and <0.5 were considered small, between ≥0.5 and <0.8 were considered medium, and ≥0.8 were considered large. 67 Random effect models were applied to all analyses. The statistical heterogeneity of treatment effects between studies was assessed using the I2 inconsistency test. Inconsistency was classified as low (<25%), moderate (25-49%), and high (>50%). 22 Values of α ≤ 0.05 were considered statistically significant. The sources of heterogeneity were investigated through sensitivity analyses and subgroup analyses, exploring the effect of the repetition scheme (failure versus fixed repetitions). In addition, we sought to stratify the studies, considering the mode used to generate limb restriction [arterial occlusion pressure (AOP) versus arbitrary pressure]. For sensitivity analyses, outliers, defined by the magnitude and direction of the effect, were removed from the analyses. Publication bias was analyzed by visual inspection of the funnel plot. 65 Asymmetry was tested using the Egger test and was significant when P < 0.05. Risk of bias analyses were limited to meta-analyses with more than 10 interventions. 65 Publication bias analyzes were performed using R software (Version 4.0.1; Foundation for Statistical Computing).
Certainty Assessment
The quality of the evidence was assessed using the Grading of Recommendations, Assessment, Development and Evaluation (GRADE). 20 Initially, GRADE classifies randomized clinical trials as high-quality studies (score 4); the quality of these studies can be lowered according to the identified risk of bias, and can be classified as moderate, low, or very low. The following topics were evaluated: (1) methodological limitations identified in the studies (risk of bias); (2) inconsistency in results (heterogeneity); (3) indirect evidence; (4) imprecision; and (5) publication bias. The evidence was downgraded when 50% of the studies included in the meta-analysis received a rating of “some concerns” on RoB2. For inconsistency, the evidence was downgraded when high and significant heterogeneity was identified in the meta-analysis. The risk of indirect evidence was assessed considering 3 factors: (1) when participants differed from the population of interest; (2) when interventions differed from the specific intervention desired; and (3) when substitute results were used instead of relevant results. For imprecision, the evidence was downgraded when a low number of interventions were included in the meta-analysis (≤5), or when a wide CI that could affect outcomes was identified. The analysis of publication bias was limited to meta-analyses with more than 10 studies.
Results
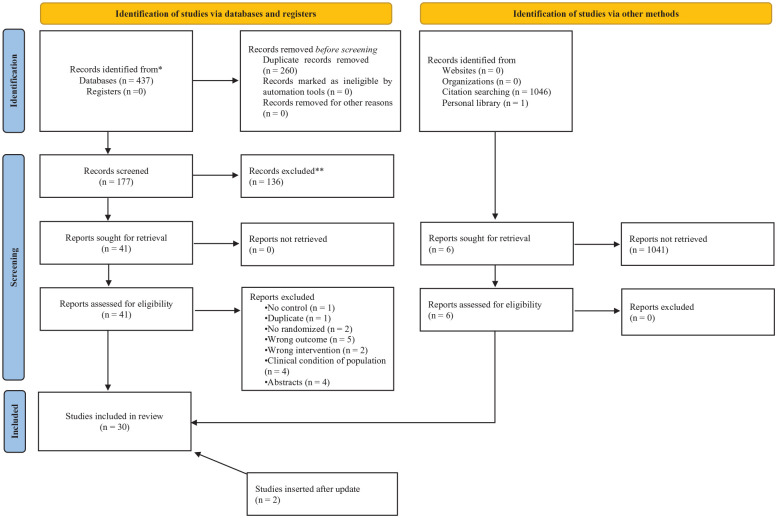
Study Selection
A total of 437 studies were identified in the searched databases (details are provided in Appendix Supplement File 1, available in the online version of this article). Twenty-three studies were considered eligible. Five studies were identified in citation tracking and 1 study was identified based on a survey of the authors in a personal library. Two studies were identified after the review was updated. Therefore, 30 studies were considered eligible for this review. Eighteen studies were included in the meta-analyses. Details of the selection process are reported in Figure 1. Details of excluded studies are reported in Appendix Supplement Files 2 and 3 (available online). Substantial interreviewer agreement was reported in phase 3 of the screening (κ = 0.674; P < 0.01).
Figure 1.
PRISMA 2020 flow diagram for this systematic review, which included searches of databases, registers, and other sources. PRISMA, Preferred Reporting Items for Systematic Review and Meta-Analysis.
Study Characteristics
The studies included a total 573 subjects (females, n = 141; males, n = 432). Sixteen studies (53%) examined women who participated in resistance training programs,3-6,12,23,24,33,34,42,48-50,54,70,71 12 studies (40%) analyzed untrained women,13,18,29,41,43,45,53,58,63,66,73,74 and only 2 studies (7%) did not report information about prior participation in resistance training programs.31,32 Two studies analyzed elderly women,53,58 whereas the other studies analyzed young women. Twenty-two (73.33%) studies adopted a within-subject crossover design, 4 (13.33%) studies adopted a within-subject design comparing contralateral limbs, and 4 (13.33%) studies adopted parallel design (between subjects).
Seven studies tested more than 1 restriction pressure.5,12,33,42,43,63,73 Two studies tested more than 1 intensity.33,70 Practical BFR (ie, BFR generated through elastic bands) was analyzed in 4 studies.3,31,32,45 Three studies tested intermittent and continuous BFR.18,46,47 Ten studies evaluated more than 1 exercise in the same session.3,13,18,23,43,45-48,58 Among the studies that evaluated more than 1 exercise in a session, 3 studies evaluated 2 exercises (leg press and knee extension) for the same muscle group.18,45,58 The characteristics of the participants and studies are presented in detail in Appendix Tables A1 and A2, respectively (available online).
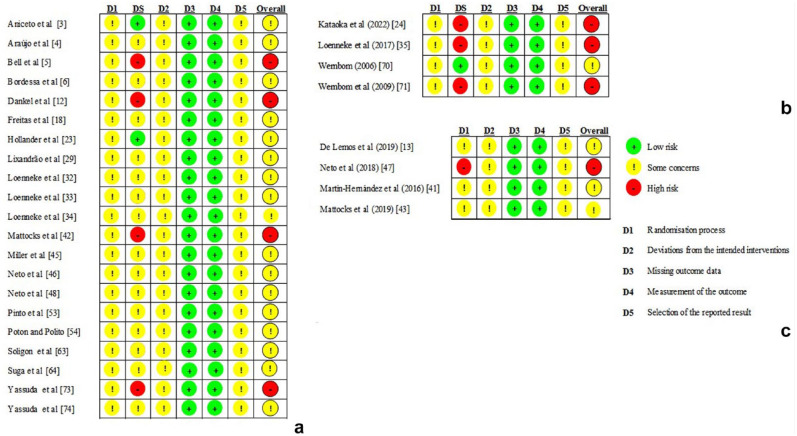
Risk of Bias in Studies
The risk of bias for each study is reported in Figure 2. The studies, in general, had limitations in the randomization process. No analyzed studies reported details about random sequence generation (eg, coin toss or computer-generated numbers sequence) or allocation concealment. In addition, one study with a parallel design 47 identified significant differences between groups in baseline characteristics and was therefore classified with a high risk of bias in domain 1 and in the overall RoB2 score. Seven studies were classified at high risk of bias for the domain S (period and carryover effects) and in the RoB2 classification for crossover studies.5,12,24,34,42,70,73 These specific studies used washout periods shorter than 24 h (single-session assessments). No study reported information about the registration of a research protocol.
Figure 2.
Risk of bias in the included studies: (a) within-subject crossover studies; (b) within-subject contralateral limbs studies; (c) parallel studies.
Outcome Details
Most studies reported RPE or muscle discomfort/pain rating for all sets performed. One study reported the highest rating during exercise. 6 Six studies reported the rating reported after the final set performed46-48,54,70,71 and 1 study reported only first set values. 43 Two studies reported the average rating of all sets.41,63 Seven studies reported the median and IQR rating,5,12,33,34,42,70,71 1 study reported mean and CI. 43 The other studies reported the rating in mean and SD. Four studies evaluated local and overall RPE.3,46-48
Results of Synthesis
Low-Load Exercise With BFR Versus Non-BFR Low-Load Exercise
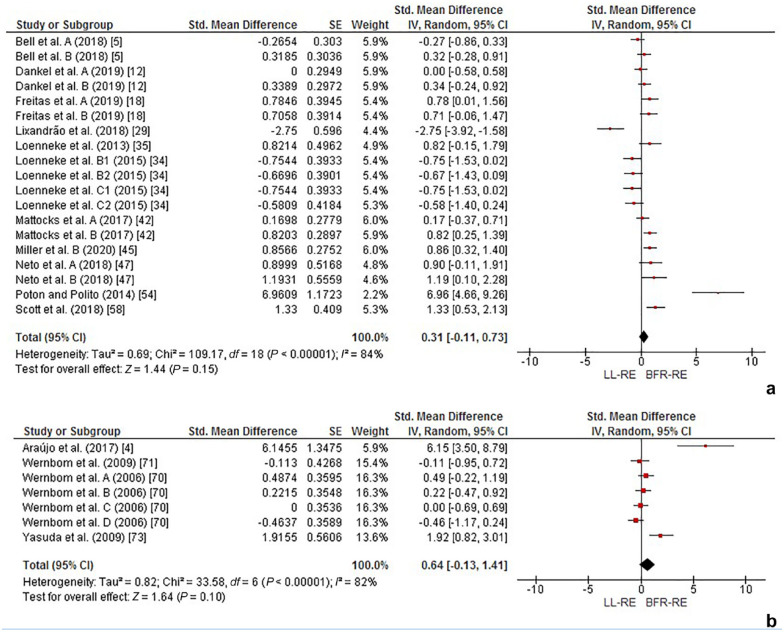
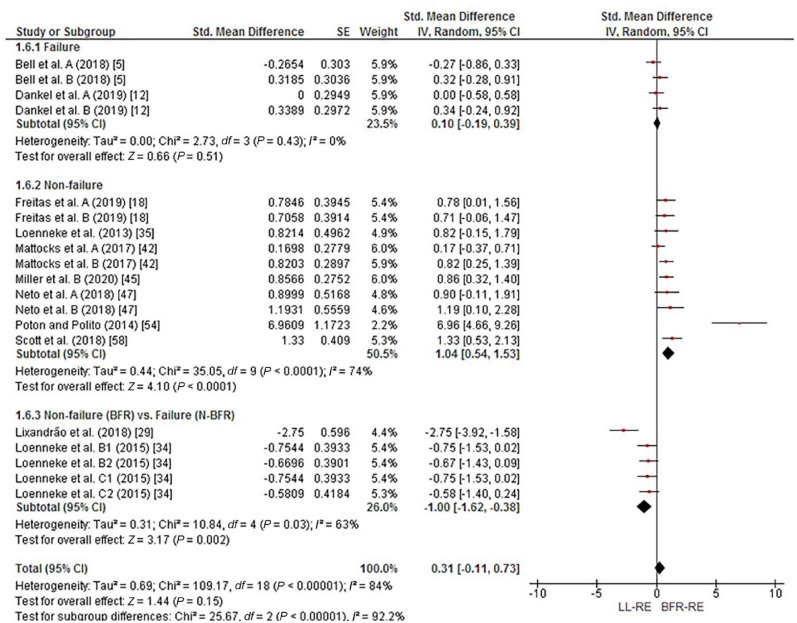
RPE
When considering all available studies, meta-analyses performed for RPE did not indicate differences between low-load exercise with BFR versus non-BFR low-intensity exercise, either in protocols that applied relative pressures [SMD = 0.31 (95% CI = −0.11 to 0.73); P = 0.15; I² = 84%; Figure 3(a)] or arbitrary pressures [SMD = 0.64 (95% CI = −0.13 to 1.41); P = 0.10; I² = 82%; Figure 3(b)]. The subgroup analyses support that this effect seems to be maintained in sets performed to failure [SMD = 0.10 (95% CI = −0.19 to 0.39); P = 0.51; I² = 0%; Figure 4]; however, in fixed repetition schemes, analyses indicated superiority of exercise with BFR [SMD = 1.04 (95% CI = 0.54 to 1.53); P < 0.01; I² = 74%; Figure 4]. Regarding comparisons of fixed repetition BFR exercise versus failure non-BFR exercise, analyses indicated lower RPE for exercise with BFR [SMD = −1.00 (95% CI = −1.62 to −0.38); P < 0.01; I² = 63%; Figure 4]. The details of the GRADE evidence certainty rating for the analyses in question are reported in detail in Appendix Tables A3 and A4 (available online).
Figure 3.
Forest plot demonstrating the effects of low-load exercise with BFR versus non-BFR low-load exercise on RPE: (a) relative pressure; (b) arbitrary pressure. BFR-RE, resistance exercise with blood flow restriction; LL-RE, low-load resistance exercise.
Figure 4.
Forest plot demonstrating the effects of low-load exercise with BFR versus non-BFR low-load exercise on RPE (subgroup analyses). BFR-RE, resistance exercise with blood flow restriction; LL-RE, low-load resistance exercise.
Sensitivity analyses were used to explore the heterogeneity maintained after stratification into subgroups. After we removed 1 study 52 from the analysis of protocols that evaluated fixed repetition schemes, heterogeneity was reduced and the results were maintained [SMD = 0.76 (95% CI = 0.52-0.99); P < 0.01; I² = 0%]. This procedure was performed in the analyses of protocols that compared fixed repetition BFR exercise versus failure non-BFR exercise; after we removed 1 study, 28 heterogeneity was reduced and the results were maintained [SMD = −0.96 (95% CI = −1.08 to −0.30); P < 0.01; I² = 0%]. Similarly, after removing 2 studies4,72 of the comparisons performed for low-intensity exercise with BFR (arbitrary pressure) versus non-BFR low-intensity exercise, the results were maintained and heterogeneity was reduced [SMD = −0.04 (95% CI = −0.29 to 0.36); P = 0.83; I² = 0%].
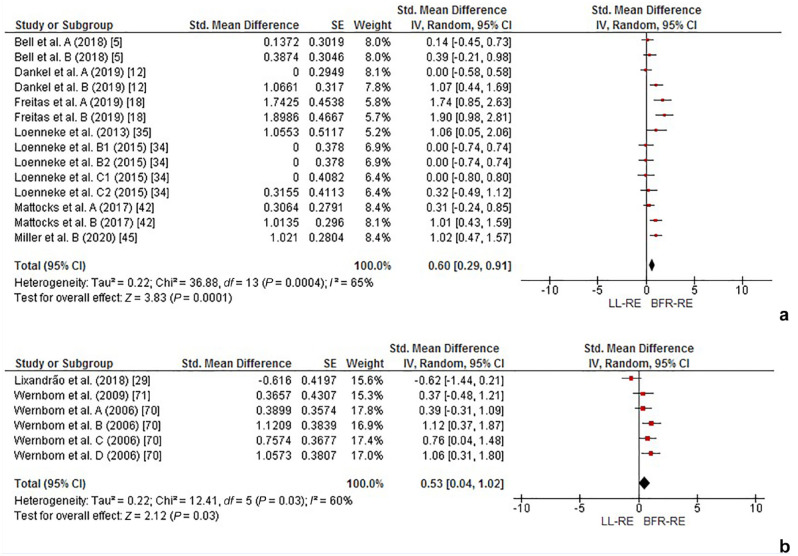
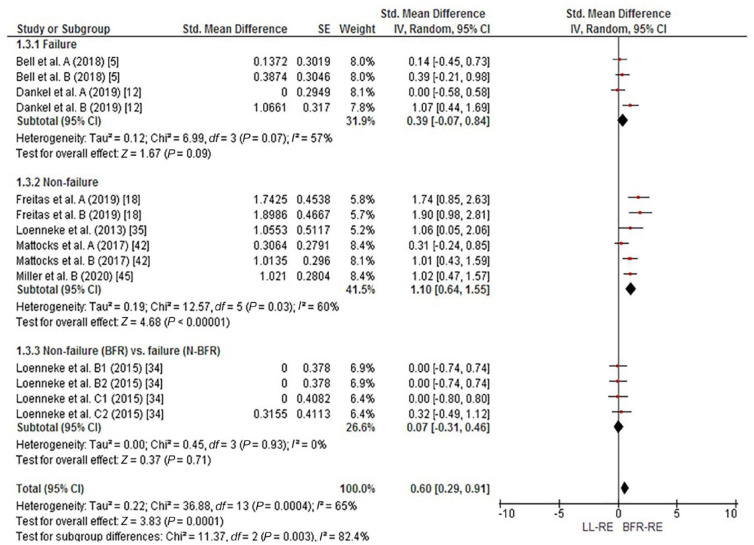
Perception of Discomfort
When considering all available studies, the meta-analysis performed for the perception of discomfort indicated significant differences, with BFR exercise promoting greater discomfort [SMD = 0.60 (95% CI = 0.29-0.91); P = 0.01; I² = 65%; Figure 5(a)]. This effect was maintained after the subgroup analyses, but only for the analyses of studies that adopted fixed repetition schemes [nonfailure; SMD = 1.10 (95% CI = 0.64 to 1.55); P < 0.01; I² = 60%; Figure 6]. There were no differences in meta-analyses performed for protocols performed to failure [SMD = 0.39 (95% CI = −0.07 to 0.84); P = 0.09; I² = 57%; Figure 6] or for the fixed repetition BFR comparisons exercise versus failure non-BFR exercise [SMD = 0.07 (95% CI = −0.31 to 0.46); P = 0.71; I² = 0%; Figure 6].
Figure 5.
Forest plot demonstrating the effects of low-intensity exercise with BFR versus non-BFR low-intensity exercise on (a) perception of discomfort and (b) perception of pain. BFR-RE, resistance exercise with blood flow restriction; LL-RE, low-load resistance exercise.
Figure 6.
Forest plot demonstrating the effects of low-intensity exercise with BFR versus non-BFR low-load exercise on perception of discomfort (subgroups analyses). BFR-RE, resistance exercise with blood flow restriction; LL-RE, low-load resistance exercise.
Sensitivity analyses were used to explore the heterogeneity maintained after stratification into subgroups. After we removed 1 study 41 from the analysis of protocols that evaluated fixed repetition schemes, heterogeneity was reduced and the results were maintained [SMD = 1.24 (95% CI = 0.89 to 1.59); P < 0.01; I² = 12%]. This procedure was performed in the analyses of protocols that compared failure protocols; after we removed 1 study, 12 heterogeneity was reduced and the results were maintained [SMD = 0.17 (95% CI = −0.17 to 0.51); P = 0.32; I² = 0%].
Pain Perception
The meta-analysis performed for perception of pain indicated significant differences, with the BFR exercise promoting greater pain [SMD = 0.53 (95% CI = 0.04-1.02); P = 0.03; I² = 60%; Figure 5(b)]; Results were maintained after removing 1 of the studies 28 included in the analysis, but heterogeneity was reduced [SMD = 0.74 (95% CI = 0.41-1.08); P < 0.01; I² = 0%].
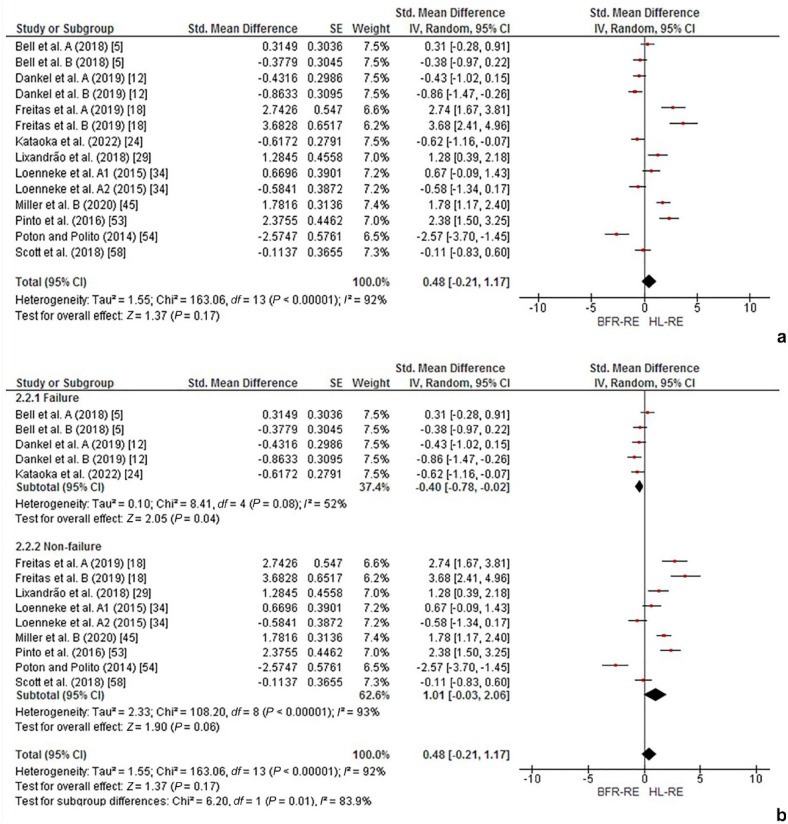
Low-Load Exercise With BFR Versus Non-BFR High-Load Exercise
Rate of Perceived Exertion
When considering all available studies, meta-analyses performed for RPE did not indicate differences between low load with BFR versus non-BFR high load [SMD = 0.48 (95% CI = −0.21 to 1.17); P = 0.17; Figure 7(a)]. The subgroup analyses for studies that tested failure protocols showed differences between the training models tested (lower RPE at high load), but with high heterogeneity [SMD = −0.34 (95% CI = −0.81 to 0.14); P = 0.16; I² = 61%; Figure 7(b)]. After removing 1 study 5 of the analyses, the results were maintained and a heterogeneity reduction [SMD = −0.57 (95% CI = −0.86 to −0.28); P < 0.01; I² = 0%] was observed. Similarly, subgroup analyses for studies that tested fixed repetition schemes did not show differences between the training models tested [SMD = 1.01 (95% CI = −0.03 to 2.06); P = 0.06; I² = 93%]; however, these results appear to have been influenced by individual studies. After removing 1 study 54 which presented greater disparity in relation to the others, it was possible to identify significant differences between the training models, with the no-BFR high-intensity exercise promoting higher RPE [SMD = 1.42 (95% CI = 0.51-2.34); P < 0.01; I² = 90%].
Figure 7.
Forest plot demonstrating the effects of low-intensity exercise with BFR versus non-BFR high-intensity exercise on RPE: (a) general analyses; (b) subgroups analyses. BFR-RE, resistance exercise with blood flow restriction; HL-RE, high-load resistance exercise.
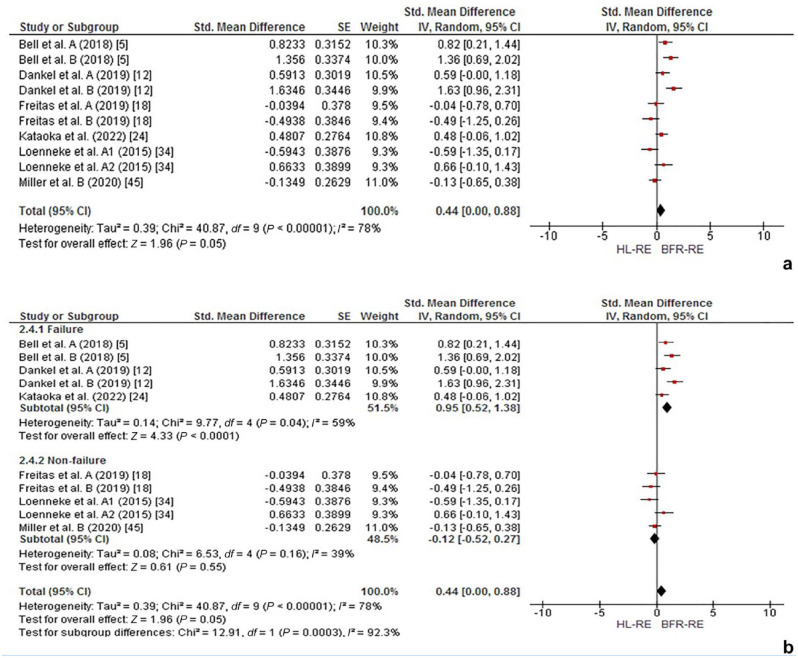
Perception of Discomfort
When considering all available studies, meta-analyses performed for perception of discomfort did not indicate differences between low load with BFR versus no-BFR high load [SMD = 0.44 (95% CI = 0.00-0.88); P = 0.05; I² = 78%; Figure 8(a)]. Subgroup analyses of studies that tested protocols of sets performed to voluntary failure indicated differences between exercise models, with exercise with BFR promoting greater discomfort [SMD = 0.95 (95% CI = 0.52-1.38); P < 0.01; I² = 59%; Figure 8(b)]. In contrast, subgroup analyses for studies that analyzed fixed repetition schemes (nonfailure) did not indicate significant differences between the exercise models tested [SMD = −0.12 (95% CI = −0.52-0.27); P = 0.55; I² = 39%; Figure 8(b)].
Figure 8.
Forest plot demonstrating the effects of low-intensity exercise with BFR versus non-BFR high-intensity exercise on perception of discomfort: (a) general analyses; (b) subgroup analyses). BFR-RE, resistance exercise with blood flow restriction; HL-RE, high-load resistance exercise.
Sensitivity analyses were used to explore the heterogeneity maintained after stratification into subgroups. After we removed 1 study 33 that evaluated fixed repetition schemes, heterogeneity was reduced and the results were maintained [SMD = −0.27 (95% CI = −0.60-0.06); P = 0.11; I² = 0%].
Publication Bias
Publication bias was analyzed in meta-analyses with more than 10 studies. According to Egger’s test, there was no evidence of publication bias in the analyses (P ≥ 0.05). Details of risk of bias analyses are provided in Appendix Supplemental Material 4 (available online).
Discussion
The aim of this systematic review and meta-analysis was to analyze the acute effect of low-load resistance training with BFR versus non-BFR resistance training (high and low load) on RPE and perceived discomfort/muscle pain. The analyses performed showed that in arbitrary (fixed) repetition scheme, exercise with BFR promotes greater RPE and discomfort than non-BFR low-load exercise, but this effect was not identified in sets performed to failure. For comparisons between nonfailure exercise with BFR versus failure low-load exercise without BFR, it was found that the discomfort was similar, but the RPE was lower in the exercise with BFR. For comparisons between exercise with BFR and high-load exercise without BFR, no significant differences were identified for RPE; for sets to failure, the perceived discomfort and RPE was higher in exercise with BFR.
Rate of Perceived Exertion
RPE has been defined in the literature as “the conscious sensation of how hard, heavy and strenuous a physical task is.” 39 Thus, RPE is distinctly different than other perceptual responses such as muscle discomfort and pain that may be influenced through other sensory-related processes.7,51 RPE during exercise is thought to be related to the magnitude of corollary discharge (a copy of the motor signal sent to the activated muscle called motor-related cortical potential) from voluntary motor control centers initiating movement. 14 When muscle force requirements are greater (eg, during heavy lifting), RPE is generally elevated compared with lighter loads 27 to recruit additional muscle fibers needed to meet the demands of the task, resulting in higher muscle excitation (evidenced by surface electromyography). 14 As fatigue accumulates during exercise, the amplitude of motor-related cortical potentials increases to compensate 14 to further recruit available muscle fibers to produce the necessary force, elevating RPE. For low-load exercise with or without BFR, RPE is low during nonfatiguing resistance exercise 11 but significantly elevates approaching failure. 60
Thus, monitoring RPE may provide a surrogate measure for the relative demands of an exercise and its potential to elicit hypertrophy during longitudinal training programs. This is especially true considering low-load BFR exercise has been shown to produce superior hypertrophy when compared with work-matched low-load exercise alone and similar hypertrophy to high-load training.28,35 The accelerated fatigue experienced in the working muscle during low-load BFR exercise is thought to enhance the perceptual experiences of the exerciser due to a proximity to failure from the restricted blood flow attenuating oxygen delivery compared with free-flow exercise.56,57 Therefore, low-load exercise with BFR may be expected to increase the RPE response compared with low-load exercise.
Low-Load BFR Exercise Versus Low-Load Non-BFR Exercise: RPE
In contrast to our hypothesis that BFR would elevate RPE during exercise, the results of our meta-analysis indicate that no significant differences were reported for low-load exercise with BFR compared with low-load exercise without BFR, albeit with high heterogeneity. Based on the high heterogeneity within the included studies in our analysis, caution is warranted in extrapolating these findings. Thus, subgrouping was implemented considering protocols to ascertain the sources of heterogeneity.
Initially, we stratified all included studies that adopted a personalized (eg, 40-100% AOP) or arbitrary (eg, 100-200 mmHg) pressure in comparison with low-load exercise without BFR. No significant differences were reported in these analyses. This is an interesting finding considering how RPE is elevated with increasing proximity to failure and that BFR exercise accelerates volitional fatigue in an exercise task by as much as 43%. 25 The heterogeneity of the included studies within our analyses likely produced our findings because RPE is similar (eg, near maximal) during failure training regardless of the application of BFR, 32 necessitating additional subgrouping according to repetition scheme (eg, fixed versus failure).
Subgroup analyses performed in the meta-analysis of the personalized pressure protocols indicated that in fixed repetition schemes, low-load exercise with BFR induces a significantly higher RPE than exercise with similar training volume performed without BFR with slightly less heterogeneity (I² = 74%) in the dataset. Upon removal of 1 outlier, 54 heterogeneity was reduced (I2 = 0%) and the results were maintained. The study in question 54 utilized an 18-cm-wide cuff at 100% AOP for their leg extension exercise, likely heightening the perceptual response as higher pressures have been shown to augment RPE responses during BFR training 63 and the pressure applied is not recommended for use in clinical practice. 52 The results of this subgroup analysis are clinically relevant because many practitioners use fixed repetition schemes in their BFR training programs. 52 When exercise is performed to failure with or without BFR, no identifiable differences were observed regardless of applied pressure (Figure 4). This mostly aligns with the existing literature on failure training indicating near maximal levels of exertion when exercise is taken to failure, with29,60 or without BFR.29,55
Last, we compared a fixed repetition scheme using low-load BFR with non-BFR low-load exercise to failure and found that RPE was significantly greater in non-BFR low-intensity exercise to failure with moderate-to-high heterogeneity (I2 = 63%; Figure 4). This is a somewhat expected finding as comparing failure with nonfailure exercise during traditional training 15 and low-load training with BFR 60 has produced similar results (eg, RPE is elevated during the failure condition). To reduce heterogeneity, we removed 1 study, 29 decreasing our I2 to 0%, maintaining the same conclusion and narrowing the CIs (from −1.62 to −0.38 to −1.08 to −0.30; P < 0.01). Whereas Loenneke et al 32 utilized a clinically recommended fixed repetition scheme of 30-15-15-15 at 20% to 30% 1RM using 50% to 60% AOP, Lixandrão et al 29 implemented fewer repetitions (15-15-15-15) at a similar pressure (50% AOP), and both studies performed 4 sets to voluntary fatigue as a comparator. Thus, Lixandrão et al 29 likely compared RPE further from failure than Loenneke et al, 33 skewing the results of the subgroup analysis and creating the observed heterogeneity. Withdrawing Lixandrão et al 29 better reflects the difference in RPE between protocols while keeping the same conclusions.
Low-Load BFR Exercise Versus High-Load Exercise: RPE
The results of our analysis indicate that low load with BFR exercise produces similar RPE levels as HL-RE (≥ 65% 1RM) with high heterogeneity (I2 = 92%; Figure 7). Proximity to failure in low load with BFR exercise likely varies significantly depending on the employed protocol. Without subgrouping for particulars in comparison variables, it is difficult to predict proximity to failure between protocols when comparing different loading and repetition schemes (as in this meta-analysis) and as a result, provides inconsistent RPE values between studies. Therefore, subgrouping was needed to elucidate the potential differences between studies.
In our first subgroup comparing exercise to failure with low-intensity BFR compared with high-load exercise, differences were observed between protocols (lower RPE at high load), but with high heterogeneity (P = 0.04; I² = 52%). After removing 1 outlier (effect estimate in the opposite direction to the other studies), 5 heterogeneity was reduced (I² = 0%), producing a significantly greater RPE in the BFR condition compared with high-load exercise (P < 0.01). In this study, when compared with high-load exercise, a greater training volume was achieved in the BFR condition, whereas in the other interventions included in the meta-analysis, the training volume was similar 5 or less in the BFR condition. 12 These data suggest that the training volume does not seem to be the main determinant of RPE, but the level of fatigue, as proposed previously. 12
Our second subgroup analysis also showed no differences between low-intensity BFR exercise and high-load exercise when using fixed repetition (eg, nonfailure) exercise protocols with very high heterogeneity (I2 = 93%; P = 0.06). For example, 6 of the 9 (66.6%) included interventions18,29,33,45,53 in our nonfailure subgrouping favored high-load exercise producing significantly greater RPE values than BFR exercise, whereas only 1 clearly favored BFR exercise. 54 The variations between the protocols likely explain the observed RPE responses particularly as it is impossible to understand proximity to failure between them. For example, Freitas et al 18 compared 4 sets of 10 repetitions of 70% 1RM leg extension and leg press exercise to 4 sets (30-15-15-15) of low-load BFR exercise performed at 20% 1RM at 50% AOP. Thus, the differences between protocols with respect to proximity to failure are likely significantly larger than other included studies in this subgroup such as that by Loenneke et al 33 that utilized leg extensions at 70% 1RM but at 30% 1RM in the BFR condition. The results of Loenneke et al 33 indicate similar RPE response as high-load exercise due largely in part to the higher percentage of the 1RM employed in the fixed repetition protocol. Studies implementing loads that are widely divergent (eg, 20% 1RM BFR versus 80% 1RM) between experimental conditions (such as in Poton and Polito 54 ) and pressures not recommended in clinical practice (eg, 100% AOP) likely increased the differential RPE responses. As such, we removed Poton and Polito 54 to reduce heterogeneity. After removing this study, our significance between groups changed in favor of high-load exercise [SMD = 1.42 (95% CI = 0.51-2.34); P < 0.01; I² = 90%].
Nonetheless, despite the very large heterogeneity still present in our subgroup analysis, it can be stated that the BFR-related prescription factors (eg, pressure, repetitions performed per set, and load used) as well as the protocols for high-intensity strength training (eg, varying between 3-4 and 8-10 at 65-80% 1RM in the included studies) prevent further reduction of heterogeneity as many of the protocols included likely induced RPE values secondary to different proximities to failure. As load tends to drive RPE when volume is equal, 63 not equating volume decreases the likelihood of a heterogeneity reduction.
Rate of Perceived Discomfort/Rate of Perceived Pain
Discomfort during exercise is a fundamentally different sensation than exertion, and researchers have called to distinguish it from RPE when monitoring the perceptual demands of an exercise task. 51 Whereas exertion encompasses how strenuous a task is, discomfort is related to the perception of physiological and unpleasant sensations associated with exercise that may include pain. 40 Researchers assess discomfort frequently utilizing scales such as the Borg’s Discomfort Scale [Category Ratio-10 Scale (CR10+)] and visual analog scale (VAS)8,62 and report it as rate of perceived discomfort (RPD) and rate of perceived pain (RPP) when pain is the main outcome variable of interest.
There is considerable debate as to what mechanisms are underpinning exercise-induced discomfort. 51 However, the most commonly accepted mechanism producing exercise-induced discomfort and pain is related to stimulation of the nociceptive group III and IV afferents. 44 As metabolites accumulate from increased exercise intensity (eg, proximity to failure), the afferents communicate to the central nervous system where processing of information generates conscious awareness of a subjective experience of exercise-induced discomfort/pain. 37 As exercise progresses and proximity to failure increases, metabolite concentrations rise causing a greater magnitude of central nervous system signaling. 19 Once discomfort exceeds a particular variable individual threshold that depends on multiple factors (eg, motivation), it begins to influence performance, ultimately producing cessation of the task (eg, “sensory tolerance limit”). 2 Exercise that induces significant metabolite accumulations with prolonged time under tension (eg, LL-RE performed to failure) is thought to enhance the discomfort/pain experienced during exercise compared with shorter duration exercise (eg, further away from failure) and/or using heavier loads with less time under tension per set.
RPD/RPP are important to understand during BFR exercise because of their association with potentially negative exercise-related side effects that if too severe, may compromise long-term adherence to the modality.56,62 Understanding the relative differences between the RPD/RPP associated with low-load BFR exercise in comparison with low-load and high-load exercise alone in different repetition schemes carries high clinical relevancy. The following sections discuss available comparisons between conditions using RPD and RPP (when available).
Low-Load BFR Exercise Versus Low-Load Non-BFR Exercise: RPD Responses
Our meta-analysis results indicate that low-load BFR exercise produces significantly higher exercise-induced discomfort (RPD) than low-load exercise alone with high levels of heterogeneity (I2 = 65%). However, due to the heterogeneity observed, subgrouping was performed according to repetition scheme (eg, fixed versus failure).
When we subgrouped according to a fixed nonfailure repetition protocol typical of clinical practice, low-intensity BFR exercise was still found to induce more discomfort than low-intensity exercise [I2 = 60%; Figure 6(b)]. To reduce study heterogeneity, we removed 1 study. 42 In addition to the repetition scheme adopted, the study removed applied a BFR pressure equal to or close to most of the interventions included in the meta-analysis (50-60% of AOP); however, the study in question tested an elbow flexion because, whereas the other interventions tested knee extension. This aspect must be considered, since a perception of discomfort resulting from the ischemic stimulus may be more pronounced in the lower limbs than in the upper limbs. 59 Thus, the same relative pressure applied to the upper limbs can promote a lower perception of discomfort than the lower limbs possibly due to the larger muscle mass of the lower limbs (eg, quadriceps) producing elevated metabolite accumulations, justifying the divergent result of the removed outlier.
Subgrouping protocols performed to failure indicates that discomfort experienced in either condition is similar with high heterogeneity [I2 = 57%; Figure 6(a)]. After removing the outlier 12 that used 80% AOP in knee extension, heterogeneity reduced (I2 = 0%) and the results were maintained. Considering that all studies adopted sets to failure, the disparate results of the current study can be explained by the application of high pressure in a single-joint lower limb exercise. This subgroup analysis supports clinical practice observations and recommendations that low-intensity exercise taken to failure with or without BFR produces significant discomfort, 62 likely due to the similar levels of metabolites produced32,74 stimulating the afferents.
We also subgrouped exercise repetition protocols comparing fixed repetition low-load BFR exercise with failure low-load exercise. The results of our subgroup analysis indicate no significant differences between RPD with no heterogeneity (I2 = 0%). This is a somewhat expected finding considering BFR elevates the perceptual demands of exercise. 62 The protocols used within the subgroup compared 4 sets of BFR leg extension exercise (30-15-15-15) at either 20% or 30% 1RM using 50% to 60% AOP compared with 20% to 30% 1RM low-load exercise to failure. Despite the significantly different volumes lifted between conditions, RPD was similar. 33 These findings suggest that while longitudinal outcomes in hypertrophy may be equivocal when exercising to failure,16,17 discomfort during exercise is similar to low-load failure exercise when using BFR exercising in a protocol and loading range (20-30% 1RM) frequently recommended in practice. It appears that the addition of BFR to low-load exercise augments the perceived discomfort responses to similar levels as traditional low-load exercise carried to volitional fatigue, indicating similar perceptual demands.
Low-Load BFR Exercise Versus Low-Load Exercise: RPP Responses
Exercise-induced muscle pain (eg, RPP) is associated with RPD but is a more focused estimation of the metabolite-related effects of exercise. 14 RPP has been qualified in studies by asking participants to rate the perceptual demands with respect to the “worst lactic acid pain [experienced in the] quadriceps” 70 or asking participants to anchor their response with “[their] worst experiences of pain.” 29 RPP has been described using similar CR-10 Scales. RPP values are important to consider because if an exercise protocol is too painful, long-term compliance may be compromised. 56
In our only subgroup comparison, low-intensity BFR exercise was shown to produce greater RPP than low-intensity exercise. The greater perception of pain evidenced in the exercise with BFR can be partially explained by the metabolic alterations resulting from the exercise and by the discomfort induced by the compression of the limb through the cuff. A moderate-to-high heterogeneity was evidenced in this analysis (I2 = 60%); after removing Lixandrão et al, 29 heterogeneity was reduced (I2 = 0%) and results were maintained. Unlike the other studies, Lixandrão et al 29 had participants exercise using 4 sets of 15 repetitions with BFR compared with low-intensity and high-intensity exercise to failure, whereas Wernbom et al’s studies70,71 were 4 sets to volitional fatigue using low-intensity exercise with and without BFR. Thus, comparisons in the exercise prescriptions between protocols can explain the divergent findings. In the study of Lixandrão et al, 29 the RPP was significantly lower in BFR exercise than in low- and high-load exercise performed to failure. Based on this, the authors speculate that the participants were able to distinguish between muscle pain and discomfort of cuff pressure.
Low-Load BFR Exercise Versus High-Load Exercise: RPD Responses
Our meta-analysis results indicate that low-intensity BFR exercise produces similar levels of exercise-induced discomfort (RPD) as high-intensity exercise with large heterogeneity (I2 = 78%). However, due to the heterogeneity observed, subgrouping was performed according to repetition scheme (eg, fixed versus failure) to further clarify RPD responses.
When subgrouping according to fixed (nonfailure) repetition schemes, no significant differences in exercise-induced discomfort was observed between conditions with low-to-moderate heterogeneity (I2 = 39%). After removing 1 study 33 deemed an outlier, heterogeneity was further reduced (I2 = 0%) while maintaining the initial conclusions. Loenneke et al 33 employed 4 sets of nonfailure BFR exercise using a commonly recommended 30-15-15-15 at 30% 1RM at 40% AOP. Although this prescription is within guidelines, load has been discussed as the main driver for driving perceptual demands of BFR exercise given a minimum amount of pressure. 33 Nonetheless, our subgroup analysis is challenging to interpret given the included studies.
For exercise to failure, our subgroup analysis indicates low-load BFR produces larger RPD than high-load strength training with high heterogeneity (I2 = 54%). Elevated RPD in low-intensity BFR exercise likely arises from greater time under tension, exposing the exerciser to elevated levels of metabolites for longer periods of time, heightening the afferent feedback. Most interventions included in this subgroup used 15% 1RM during upper (unilateral elbow flexion) and lower (unilateral leg extension) exercise at 40/80% AOP compared with 70% 1RM high-load exercise. In this paradigm, higher applied pressures (80% AOP) at lighter loads (20% 1RM) have been shown to produce equivocal hypertrophy in a longitudinal training program as heavier loading schemes (40% 1RM) 30 but at the expense of elevated RPD. 63 Most interventions included in this subgroup were exercising with loads below 20% 1RM, likely prolonging time under tension and, subsequently, RPD compared with heavier loads (eg, 20-30% 1RM). Thus, some caution is warranted given the conclusions within this subgroup as the loads analyzed in the BFR exercise condition are not within recommended clinical practice guidelines. 52
Limitations
There are major limitations to this study. For example, there was high heterogeneity (I² ≥ 65%) in the main analyses performed, suggesting a certain level of variability among the studies included in these meta-analyses. However, subgroup analyses and sensitivity analyses were introduced to isolate the differences and identify factors responsible for the different effects. We emphasize that the results were maintained in almost all meta-analyses after excluding outliers and heterogeneity was reduced. In comparisons between low-load exercise with BFR and high-load exercise, high heterogeneity was maintained in the comparisons of studies that adopted a fixed-repetition scheme (subgroup), and the results of this analysis were strongly influenced by individual studies. Therefore, these results must be interpreted with caution. In addition, the quality of evidence was low and moderate for the meta-analyses and the studies had certain methodological limitations related to the randomization process and allocation secrecy, in addition to the absence of prospective registers.
Clinical Implications
Low-load BFR exercise produces greater levels of exertion and discomfort/pain compared with low-intensity work-matched exercise while inducing lesser (in fixed repetition schemes only), similar, or greater perceptual experiences compared with high-load exercise. Therefore, during load compromised periods in early rehabilitation (eg, postsurgical precautions/contraindications), low-load exercise with BFR may be used to provide a superior muscle sparing stimulus to work-matched low-load exercise. 52 However, as BFR generates significantly more exercise-induced discomfort/pain, patient education may be an important component of long-term compliance to the modality. 56
Conclusion
In a fixed-repetition scheme, LL-RE with BFR promotes greater perceptual demands than low-load exercise without BFR, but this effect is null in sets to voluntary failure. In relation to HL-RE, in a fixed-repetition scheme, the RPE is greater in high-load exercise, but it is similar when both are conducted to voluntary failure. For discomfort, in sets to voluntary failure, LL-RE with BFR promotes greater discomfort, but this effect is null in a fixed-repetition scheme.
Supplemental Material
Supplemental material, sj-docx-1-sph-10.1177_19417381221131533 for Acute Effect of Resistance Training With Blood Flow Restriction on Perceptual Responses: A Systematic Review and Meta-Analysis by Victor Sabino de Queiros, Nicholas Rolnick, Ísis Kelly dos Santos, Ingrid Martins de França, Rony Jerônimo Lima, João Guilherme Vieira, Rodrigo Ramalho Aniceto, Gabriel Rodrigues Neto, Jason Azevedo de Medeiros, Jeferson Macedo Vianna, Breno Guilherme de Araújo Tinôco Cabral and Paulo Moreira Silva Dantas in Sports Health: A Multidisciplinary Approach
Footnotes
The following author declared potential conflicts of interest: NR is the founder of THE BFR PROS, a BFR education company that provides BFR training workshops to fitness and rehabilitation professionals across the world using a variety of BFR devices. NR has no financial relationships with any cuff manufacturers/distributors.
Contributor Information
Victor Sabino de Queiros, Graduate Program in Health Sciences, Federal University of Rio Grande do Norte (UFRN), Natal-RN, Brazil.
Nicholas Rolnick, The Human Performance Mechanic, CUNY Lehman College, Bronx, New York, USA.
Ísis Kelly dos Santos, Graduate Program in Health Sciences, Federal University of Rio Grande do Norte (UFRN), Natal-RN, Brazil; Graduate Program in Physical Education, State University of Rio Grande do Norte (UERN), Mossoró-RN, Brazil.
Ingrid Martins de França, Graduate Program in Physiotherapy, Federal University of Rio Grande do Rio Grande Norte (UFRN), Natal-RN, Brazil.
Rony Jerônimo Lima, Graduate Program in Physical Education, Federal University of Rio Grande do Norte (UFRN), Natal-RN, Brazil.
João Guilherme Vieira, Graduate Program in Physical Education, Federal University of Juiz de Fora (UFJF), Juiz de Fora-MG, Brazil; Strength Training Research Laboratory, Federal University of Juiz de Fora (UFJF), Juiz de Fora-MG, Brazil.
Rodrigo Ramalho Aniceto, Study and Research Group in Biomechanics and Psychophysiology of Exercise, Federal Institute of Education, Science and Technology of Rio Grande do Norte, Currais Novos-RN, Brazil.
Gabriel Rodrigues Neto, Faculty Nova Esperança (FAMENE/FACENE), Coordination of Physical Education, Nursing and Medical Schools, João Pessoa, Brazil; Coordination of Physical Education, University Center for Higher Education and Development (CESED/UNIFACISA/FCM/ESAC), Campina Grande, Brazil.
Jason Azevedo de Medeiros, Graduate Program in Health Sciences, Federal University of Rio Grande do Norte (UFRN), Natal-RN, Brazil.
Jeferson Macedo Vianna, Graduate Program in Physical Education, Federal University of Juiz de Fora (UFJF), Juiz de Fora-MG, Brazil; Strength Training Research Laboratory, Federal University of Juiz de Fora (UFJF), Juiz de Fora-MG, Brazil.
Breno Guilherme de Araújo Tinôco Cabral, Graduate Program in Health Sciences, Federal University of Rio Grande do Norte (UFRN), Natal-RN, Brazil; Graduate Program in Physical Education, Federal University of Rio Grande do Norte (UFRN), Natal-RN, Brazil).
Paulo Moreira Silva Dantas, Graduate Program in Health Sciences, Federal University of Rio Grande do Norte (UFRN), Natal-RN, Brazil; Graduate Program in Physical Education, Federal University of Rio Grande do Norte (UFRN), Natal-RN, Brazil).
References
- 1. Alves RC, Prestes J, Enes A, et al. Training programs designed for muscle hypertrophy in bodybuilders: narrative review. Sports. 2020;8:149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Amann M, Proctor LT, Sebranek JJ, Pegelow DF, Dempsey JA. Opioid-mediated muscle afferents inhibit central motor drive and limit peripheral muscle fatigue development in humans. J Physiol. 2009;587:271-83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Aniceto RR, Robertson R, Silva AS, et al. Is rating of perceived exertion a valid method to monitor intensity during blood flow restriction exercise. Hum Mov. 2021; 22: 68-77. [Google Scholar]
- 4. Araújo AC, Ferreira Junior A, de Oliveira SK, Schamne JC, Okuno NM. Physiological and rating of perceived exertion responses to resistance training sessions with and without vascular occlusion. Isokin Exercise Sci. 2017;25:91-96. [Google Scholar]
- 5. Bell ZW, Buckner SL, Jessee MB, et al. Moderately heavy exercise produces lower cardiovascular, RPE, and discomfort compared to lower load exercise with and without blood flow restriction. Eur J Appl Physiol. 2018;118:1473-1480. [DOI] [PubMed] [Google Scholar]
- 6. Bordessa JM, Hearn MC, Reinfeldt AE, et al. Comparison of blood flow restriction devices and their effect on quadriceps muscle activation. Phys Ther Sport. 2021;49:90-97. [DOI] [PubMed] [Google Scholar]
- 7. Borg GAV. Perceived Exertion Scale. PsycTESTS Dataset. American Psychological Association (APA), 2018. [Google Scholar]
- 8. Capodaglio EM. Comparison between the CR10 Borg’s scale and the VAS (visual analogue scale) during an arm-cranking exercise. J Occup Rehabil. 2001;11:69-74. [DOI] [PubMed] [Google Scholar]
- 9. Centner C, Lauber B. A systematic review and meta-analysis on neural adaptations following blood flow restriction training: what we know and what we don’t know. Front Physiol. 2020;11:887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Cerqueira MS, Maciel DG, Barboza JAM, et al. Low-load blood-flow restriction exercise to failure and nonfailure and myoelectric activity: a meta-analysis. J Athl Train. 2022;57:402-417. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Day ML, McGuigan MR, Brice G, Foster C. Monitoring exercise intensity during resistance training using the session RPE scale. J Strength Cond Res. 2004;18:353-358. [DOI] [PubMed] [Google Scholar]
- 12. Dankel SJ, Jessee MB, Mattocks KT, et al. Perceptual and arterial occlusion responses to very low load blood flow restricted exercise performed to volitional failure. Clin Physiol Funct Imaging. 2019;39:29-34. [DOI] [PubMed] [Google Scholar]
- 13. De Lemos Muller CH, Ramis TR, Ribeiro JL. Effects of low-load resistance training with blood flow restriction on the perceived exertion, muscular resistance and endurance in healthy young adults. Sport Sci Health. 2019;15:503-510. [Google Scholar]
- 14. De Morree HM, Klein C, Marcora SM. Perception of effort reflects central motor command during movement execution. Psychophysiology. 2012;49:1242-1253. [DOI] [PubMed] [Google Scholar]
- 15. Dos Santos WDN, Vieira CA, Bottaro M, et al. Resistance training performed to failure or not to failure results in similar total volume, but with different fatigue and discomfort levels. J Strength Cond Res. 2021;35:1372-1379. [DOI] [PubMed] [Google Scholar]
- 16. Fahs CA, Loenneke JP, Thiebaud RS, et al. Muscular adaptations to fatiguing exercise with and without blood flow restriction. Clin Physiol Funct Imaging. 2015;35:167-176. [DOI] [PubMed] [Google Scholar]
- 17. Farup J, De Paoli F, Bjerg K, Riis S, Ringgard S, Vissing K. Blood flow restricted and traditional resistance training performed to fatigue produce equal muscle hypertrophy. Scand J Med Sci Sports. 2015;25:754-763. [DOI] [PubMed] [Google Scholar]
- 18. Freitas ED, Miller RM, Heishman AD, Aniceto RR, Silva JG, Bemben MG. Perceptual responses to continuous versus intermittent blood flow restriction exercise: a randomized controlled trial. Physiol Behav. 2019;212:112717. [DOI] [PubMed] [Google Scholar]
- 19. Gandevia SC. Spinal and supraspinal factors in human muscle fatigue. Physiol Rev. 2001;81:1725-1789. [DOI] [PubMed] [Google Scholar]
- 20. Goldet G, Howick J. Understanding GRADE: an introduction. J Evid Based Med. 2013;6:50-54. [DOI] [PubMed] [Google Scholar]
- 21. Guo J, Li L, Gong Y, et al. Massage alleviates delayed onset muscle soreness after strenuous exercise: a systematic review and meta-analysis. Front Physiol. 2017;8:747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539-1558. [DOI] [PubMed] [Google Scholar]
- 23. Hollander DB, Reeves GV, Clavier JD, Francois MR, Thomas C, Kraemer RR. Partial occlusion during resistance exercise alters effort sense and pain. J Strength Cond Res. 2010;24:235-243. [DOI] [PubMed] [Google Scholar]
- 24. Kataoka R, Vasenina E, Hammert WB, Ibrahim AH, Dankel SJ, Buckner SL. Muscle growth adaptations to high-load training and low-load training with blood flow restriction in calf muscles. Eur J Appl Physiol. 2022;122:623-634. [DOI] [PubMed] [Google Scholar]
- 25. Kolind MI, Gam S, Phillip JG, et al. Effects of low load exercise with and without blood-flow restriction on microvascular oxygenation, muscle excitability and perceived pain. Eur J Sport Sci. 2022;1-21. doi: 10.1080/17461391.2022.2039781. [DOI] [PubMed] [Google Scholar]
- 26. Laurentino GC, Ugrinowitsch C, Roschel H, et al. Strength training with blood flow restriction diminishes myostatin gene expression. Med Sci Sports Exerc, 2012;44:406-412. [DOI] [PubMed] [Google Scholar]
- 27. Lins-Filho ODL, Robertson RJ, Farah BQ, Rodrigues SL, Cyrino ES, Ritti-Dias RM. Effects of exercise intensity on rating of perceived exertion during a multiple-set resistance exercise session. J Strength Cond Res. 2012;26:466-472. [DOI] [PubMed] [Google Scholar]
- 28. Lixandrao ME, Ugrinowitsch C, Berton R, et al. Magnitude of muscle strength and mass adaptations between high-load resistance training versus low-load resistance training associated with blood-flow restriction: a systematic review and meta-analysis. Sports Med. 2018;48:361-378. [DOI] [PubMed] [Google Scholar]
- 29. Lixandrão ME, Roschel H, Ugrinowitsch C, Miquelini M, Alvarez IF, Libardi CA. Blood-flow restriction resistance exercise promotes lower pain and ratings of perceived exertion compared with either high-or low-intensity resistance exercise performed to muscular failure. J Sport Rehabil. 2019;28:706-710. [DOI] [PubMed] [Google Scholar]
- 30. Lixandrão ME, Ugrinowitsch C, Laurentino G, et al. Effects of exercise intensity and occlusion pressure after 12 weeks of resistance training with blood-flow restriction. Eur J Appl Physiol. 2015;115:2471-2480. [DOI] [PubMed] [Google Scholar]
- 31. Loenneke JP, Balapur A, Thrower AD, Barnes JT, Pujol TJ. The perceptual responses to occluded exercise. Int J Sports Med. 2011;32:181-184. [DOI] [PubMed] [Google Scholar]
- 32. Loenneke JP, Balapur A, Thrower AD, Barnes J, Pujol TJ. Blood flow restriction reduces time to muscular failure. Eur J Sport Sci. 2012;12:238-243. [Google Scholar]
- 33. Loenneke JP, Kim D, Fahs CA, et al. The effects of resistance exercise with and without different degrees of blood-flow restriction on perceptual responses. J Sports Sci. 2015;33:1472-1479. [DOI] [PubMed] [Google Scholar]
- 34. Loenneke JP, Thiebaud RS, Fahs CA, Rossow LM, Abe T, Bemben MG. Blood flow restriction does not result in prolonged decrements in torque. Eur J Appl Physiol. 2013;113:923-931. [DOI] [PubMed] [Google Scholar]
- 35. Loenneke JP, Wilson JM, Marín PJ, Zourdos MC, Bemben MG. Low intensity blood flow restriction training: a meta-analysis. Eur J Appl Physiol. 2012;112:1849-1859. [DOI] [PubMed] [Google Scholar]
- 36. Loenneke JP, Young KC, Wilson JM, Andersen JC. Rehabilitation of an osteochondral fracture using blood flow restricted exercise: a case review. J Bodyw Mov Ther. 2013;17:42-45. [DOI] [PubMed] [Google Scholar]
- 37. Loeser JD, Treede RD. The Kyoto protocol of IASP basic pain terminology. Pain. 2008;137:473-477. [DOI] [PubMed] [Google Scholar]
- 38. Lopes KG, Bottino DA, Farinatti P, et al. Strength training with blood flow restriction–a novel therapeutic approach for older adults with sarcopenia? A case report. Clin Interv Aging. 2019;14:1461-1469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Marcora SM. Effort: perception of. In: Goldstein EB, ed. Encyclopedia of Perception. Thousand Oaks, CA: SAGE Publications Inc; 2010:380-383. [Google Scholar]
- 40. Marcora S. Perception of effort during exercise is independent of afferent feedback from skeletal muscles, heart, and lungs. J Appl Physiol. 2009;106:2060-2062. [DOI] [PubMed] [Google Scholar]
- 41. Martín-Hernández J, Ruiz-Aguado J, Herrero AJ, et al. Adaptation of perceptual responses to low-load blood flow restriction training. J Strength Cond Res. 2017;31:765-772. [DOI] [PubMed] [Google Scholar]
- 42. Mattocks KT, Jessee MB, Counts BR, et al. The effects of upper body exercise across different levels of blood flow restriction on arterial occlusion pressure and perceptual responses. Physiol Behav. 2017;171:181-186. [DOI] [PubMed] [Google Scholar]
- 43. Mattocks KT, Mouser JG, Jessee MB, et al. Perceptual changes to progressive resistance training with and without blood flow restriction. J Sports Sci. 2019;37:1857-1864. [DOI] [PubMed] [Google Scholar]
- 44. McCord JL, Kaufman MP. Reflex Autonomic Responses Evoked by Group III and IV Muscle Afferents. In: Translational Pain Research: From Mouse to Man, edited by Kruger L, Light AR. Boca Raton, FL:2010. [PubMed] [Google Scholar]
- 45. Miller RM, Galletti BA, Koziol KJ, et al. Perceptual responses: clinical versus practical blood flow restriction resistance exercise. Physiol Behav. 2020;227:113137. [DOI] [PubMed] [Google Scholar]
- 46. Neto GR, Novaes JS, Salerno VP, et al. Acute effects of resistance exercise with continuous and intermittent blood flow restriction on hemodynamic measurements and perceived exertion. Percept Mot Skills. 2017; 124:277-292. [DOI] [PubMed] [Google Scholar]
- 47. Neto GR, Silva HG, Vieira LF, Brasiliano MM, Araújo RC, Cirilo-Sousa MS. Efeito agudo e crônico do treinamento de força com restrição de fluxo sanguíneo contínua ou intermitente sobre as medidas hemodinâmicas e percepção subjetiva de esforço em homens saudáveis. Motricidade. 2018;14:71-82. [Google Scholar]
- 48. Neto GR, Sousa MS, Costa e, Silva GV, Gil AL, Salles BF, Novaes JS. Acute resistance exercise with blood flow restriction effects on heart rate, double product, oxygen saturation and perceived exertion. Clin Physiol Funct Imaging. 2016;36:53-59. [DOI] [PubMed] [Google Scholar]
- 49. Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5:1-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021;88:105906. [DOI] [PubMed] [Google Scholar]
- 51. Pageaux B. Perception of effort in exercise science: definition, measurement and perspectives. Eur J Sport Sci. 2016;16:885-894. [DOI] [PubMed] [Google Scholar]
- 52. Patterson SD, Hughes L, Warmington S, et al. Blood flow restriction exercise: considerations of methodology, application, and safety. Front Physiol. 2019;10:533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53. Pinto RR, Karabulut M, Poton R, Polito MD. Acute resistance exercise with blood flow restriction in elderly hypertensive women: haemodynamic, rating of perceived exertion and blood lactate. Clin Physiol Funct Imaging. 2018;38:17-24. [DOI] [PubMed] [Google Scholar]
- 54. Poton R, Polito MD. Hemodynamic response to resistance exercise with and without blood flow restriction in healthy subjects. Clin Physiol Funct Imaging. 2016;36:231-236. [DOI] [PubMed] [Google Scholar]
- 55. Pritchett RC, Green JM, Wickwire PJ, Kovacs MS. Acute and session RPE responses during resistance training: bouts to failure at 60% and 90% of 1RM. South African J Sports Med. 2009;21. doi: 10.17159/2078-516X/2009/v21i1a304. [DOI] [Google Scholar]
- 56. Rolnick N, Kimbrell K, Cerqueira MS, Weatherford B, Brandner C. Perceived barriers to blood flow restriction training. Front Rehab Sci. 2021;14. doi: 10.3389/fresc.2021.697082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Rolnick N, Schoenfeld BJ. Blood flow restriction training and the physique athlete: a practical research-based guide to maximizing muscle size. Strength Condit J. 2020;42:22-36. [Google Scholar]
- 58. Scott BR, Peiffer JJ, Thomas HJ, Marston KJ, Hill KD. Hemodynamic responses to low-load blood flow restriction and unrestricted high-load resistance exercise in older women. Front Physiol. 2018;9:1324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Sharma V, Cunniffe B, Verma AP, Cardinale M, Yellon D. Characterization of acute ischemia-related physiological responses associated with remote ischemic preconditioning: a randomized controlled, crossover human study. Physiol Rep. 2014;2:e12200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Sieljacks P, Degn R, Hollaender K, Wernbom M, Vissing K. Non-failure blood flow restricted exercise induces similar muscle adaptations and less discomfort than failure protocols. Scand J Med Sci Sports. 2019;29:336-347. [DOI] [PubMed] [Google Scholar]
- 61. Sinclair P, Kadhum M, Paton B. Tolerance to intermittent vs. continuous blood flow restriction training: a meta-analysis. Int J Sports Med. 2022;43:3-10. [DOI] [PubMed] [Google Scholar]
- 62. Spitz RW, Wong V, Bell ZW, et al. Blood flow restricted exercise and discomfort: a review. J Strength Cond Res. 2020;36:871-879 [DOI] [PubMed] [Google Scholar]
- 63. Soligon SD, Lixandrão ME, Biazon TMPC, Angleri V, Roschel H, Libardi CA. Lower occlusion pressure during resistance exercise with blood-flow restriction promotes lower pain and perception of exercise compared to higher occlusion pressure when the total training volume is equalized. Physiol Int. 2018;105:276-284. [DOI] [PubMed] [Google Scholar]
- 64. Sterne JA, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366. doi: 10.1136/bmj.l4898 [DOI] [PubMed] [Google Scholar]
- 65. Sterne JA, Sutton AJ, Ioannidis JP, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomized controlled trials. BMJ. 2011;343. doi: 10.1136/bmj.d4002 [DOI] [PubMed] [Google Scholar]
- 66. Suga T, Dora K, Mok E, et al. Exercise adherence-related perceptual responses to low-load blood flow restriction resistance exercise in young adults: a pilot study. Physiol Rep. 2021;9:e15122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Sullivan GM, Feinn R. Using effect size—or why the P value is not enough. J Grad Med Educ. 2012;4:279-282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68. Takarada Y, Nakamura Y, Aruga S, Onda T, Miyazaki S, Ishii N. Rapid increase in plasma growth hormone after low-intensity resistance exercise with vascular occlusion. J Appl Physiol. 2000;88:61-65. [DOI] [PubMed] [Google Scholar]
- 69. Takarada Y, Takazawa H, Sato Y, Takebayashi S, Tanaka Y, Ishii N. Effects of resistance exercise combined with moderate vascular occlusion on muscular function in humans. J Appl Physiol. 2000;88:2097-2106. [DOI] [PubMed] [Google Scholar]
- 70. Wernbom M, Augustsson J, Thomeé R. Effects of vascular occlusion on muscular endurance in dynamic knee extension exercise at different submaximal loads. J Strength Cond Res. 2006;20:372-377. [DOI] [PubMed] [Google Scholar]
- 71. Wernbom M, Järrebring R, Andreasson MA, Augustsson J. Acute effects of blood flow restriction on muscle activity and endurance during fatiguing dynamic knee extensions at low load. J Strength Cond Res. 2009;23:2389-2395. [DOI] [PubMed] [Google Scholar]
- 72. Wilson JM, Lowery RP, Joy JM, Loenneke JP, Naimo MA. Practical blood flow restriction training increases acute determinants of hypertrophy without increasing indices of muscle damage. J Strength Cond Res. 2013;27:3068-3075. [DOI] [PubMed] [Google Scholar]
- 73. Yasuda T, Brechue WF, Fujita T, Shirakawa J, Sato Y, Abe T. Muscle activation during low-intensity muscle contractions with restricted blood flow. J Sports Sci. 2009;27:479-489. [DOI] [PubMed] [Google Scholar]
- 74. Yasuda T, Fukumura K, Iida H, Nakajima T. Effect of low-load resistance exercise with and without blood flow restriction to volitional fatigue on muscle swelling. Eur J Appl Physiol. 2015;115:919-926. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-sph-10.1177_19417381221131533 for Acute Effect of Resistance Training With Blood Flow Restriction on Perceptual Responses: A Systematic Review and Meta-Analysis by Victor Sabino de Queiros, Nicholas Rolnick, Ísis Kelly dos Santos, Ingrid Martins de França, Rony Jerônimo Lima, João Guilherme Vieira, Rodrigo Ramalho Aniceto, Gabriel Rodrigues Neto, Jason Azevedo de Medeiros, Jeferson Macedo Vianna, Breno Guilherme de Araújo Tinôco Cabral and Paulo Moreira Silva Dantas in Sports Health: A Multidisciplinary Approach