Abstract
Background
Obesity is a major public health crisis in Latino youth. Mounting evidence implicates stress in the development and maintenance of obesity. This study examined the feasibility and acceptability of having community health workers, i.e., promotoras, deliver Adaptando Dieta y Acción Para Todos (ADAPT)+, a family-based health promotion program integrating mindfulness strategies for stress reduction to underserved Latino families in rural communities.
Methods
In an ORBIT model Phase IIb longitudinal quasi-cluster feasibility study, promotoras delivered the 6-session ADAPT+ intervention and 1-session Enhanced Usual Care (EUC) in rural Florida. Feasibility was assessed via sample size and recruitment, randomization by community, data collection completion, and intervention fidelity. Acceptability was assessed via participant retention and program satisfaction. Effect sizes of differences in parent stress and mindful eating between conditions at baseline, end of treatment, and 3-month follow-up were calculated.
Results
Feasibility and acceptability were demonstrated. The recruitment target was 99% met (n = 95 recruited). Randomization was limited to site level due to coronavirus disease 2019-related challenges. Data collection procedures were feasible (100% completion). Retention was 86% at post-assessment and 82.6% at 3-month follow-up. All sessions were completed (100% fidelity). Mean program satisfaction was 3.91/4.00. ADAPT+ parents reported lower stress (difference = −3.04, medium-to-large effect, d = .70) and more mindful eating (difference = 2.00, medium effect, d = .44) than EUC parents at 3-month follow-up.
Conclusion
Study implementation and intervention delivery to rural Latino families using promotoras were feasible and acceptable. Promising findings regarding parent stress and mindful eating support a larger (ORBIT Phase III) efficacy trial.
Clinical Trial Registration
This trial was registered with ClinicalTrials.gov under identifier NCT04800432.
Keywords: obesity and weight management, pilot/feasibility trial, school-age children, Latinos, rural
Introduction
Obesity remains a major public health crisis, particularly in Latino youth. (Note: we use “Latino” to refer to our target community per their preference.) Compared to non-Latino Black (24.8%) or non-Latino White (16.6%) youth, Latino youth have the highest rates of obesity (26.2%), with rates increasing exponentially among Latino immigrants (Stierman et al., 2021). If these trends persist, an estimated 90% of U.S.-born children of Mexican immigrants will be overweight or obese status by 2030 (Wang et al., 2020). Along with increased obesity, Latino youth face higher risks for metabolic syndrome, type 2 diabetes, and cardiovascular disease (Cruz & Granados, 2019; Min et al., 2021; Paixão et al., 2023).
These trends are even more striking for Latino youth in rural areas, who are 25% more likely to be overweight/obese than Latinos in urban areas (Okobi et al., 2021). Latinos in rural areas often share resources, including food, by consuming more meals with friends and relatives outside the home, making healthy food choices more difficult (Seguin et al., 2014). Lack of access to affordable, healthier foods, fewer community resources, acculturation-related dietary changes (e.g., eating more processed and fast foods; Pena et al., 2012), and poverty are key contributing factors to obesity in rural Latino youth (Lutfiyya et al., 2007; Rodriguez et al., 2011). Children in low-income families have 2.3 times greater odds of developing childhood obesity than children from higher income families (Reis et al., 2020). Yet, Latino rural communities have been largely ignored in health promotion research despite the rising economic, social, and personal burden of obesity, including medical care costs (Bolin et al., 2015).
Targeted obesity interventions for Latino youth are needed, and community-based interventions promote better “buy-in” from Latino families (Cotter & Jones, 2020). One way to deliver a community-based intervention is by using promotoras (i.e., community health workers; Ayala et al., 2010). Promotoras bring community perspectives to the research process (Peacock et al., 2011), bridge the gap between the healthcare system and their community (Rhodes et al., 2007), and can facilitate participant engagement (Falbe et al., 2017). Promotora-led interventions have yielded positive outcomes related to obesity and cardiovascular risk factors among Latino populations (Perez et al., 2013; Viramontes et al., 2017).
Obesity interventions that not only are parent-focused but also involve the entire family show the most promise (Janicke et al., 2014). Three recent family-based obesity interventions for rural Latino children delivered in the community have demonstrated good feasibility and potential for improving weight outcomes (Foster et al., 2022; Rosado et al., 2022; Tucker et al., 2022). Most similar to the current study, the 8-week community health worker (CHW)-led La Vida Buena childhood obesity program showed promise for improving family eating and physical activity (PA) behaviors (Tucker et al., 2022). Notably, parents participating in Salud Immokalee! were hesitant to make dietary changes due to the importance of food to their cultural identity (Rosado et al., 2022).
Stress is central to the development and maintenance of obesity (Tomiyama, 2019) and parent stress specifically influences childhood obesity (Isasi et al., 2017). Latino families are especially subject to specific and burdensome stressors (e.g., economic hardship, fear of deportation) that may predispose them to weight gain and behaviors that increase obesity. Chronic stress is linked with larger waist circumference and higher body mass index (BMI) in youth (Van Jaarsveld et al., 2009), and the incidence of youth obesity increases substantially with the number of caregiver stressors (Isasi et al., 2017). Parent stress is also associated with altered PA, unhealthy eating, and obesity in children and parents (Baskind et al., 2019). Targeting parent stress to positively impact youths’ eating, PA, and other health behaviors may be key to improved outcomes of family-based obesity interventions (Janicke et al., 2014; Leung et al., 2017).
Mindfulness-based programs focus on stress-reducing strategies and can improve weight loss (Rogers et al., 2017), mindful eating, and awareness of hunger and satiety cues (Kristeller & Wolever, 2011). Mindfulness also can improve receptiveness and adherence to healthy eating and PA interventions (Coatsworth et al., 2015), including among Latino young adults (Halperin et al., 2019). While mindfulness-based programs have been successfully delivered to low-income, minority, public school students (Daly et al., 2016; Keck-Kester et al., 2021), few studies have targeted parent stress or Latino families specifically (Cotter & Jones, 2020). Providing preliminary evidence to support targeting parent stress to improve child obesity outcomes, Jastreboff et al. (2018) reported better attendance and a smaller increase in child BMI percentile in the mindfulness intervention group compared to the control group.
To address these gaps, we developed an evidence-informed, theory-based, multi-family, behavioral obesity intervention, Adaptando Dieta y Acción Para Todos (ADAPT), that we successfully delivered to Latino families living in rural communities in Florida (Stern et al., 2021b). Our original intervention did not address parent stress, which is critical to obesity and a top concern of our target population. Parent stress in rural Latino communities has systemic roots, including, but not limited to structural and policy issues related to healthcare, education, economic opportunities, and discrimination (Garcini et al., 2021; Stone et al., 2022). To reduce the experience of stress of Latino parents and improve the eating and PA behaviors of their youth, we incorporated mindfulness-based strategies into our ADAPT program, now called ADAPT+ (Stern et al., 2021a).
We first designed and tested a “proof of concept” (ORBIT Phase IIa; Czajkowski et al., 2015; Soca Lozano et al., 2021). The present article describes our Phase IIb study that tested the feasibility and acceptability of ADAPT+. We examined the feasibility of (1) study sample selection and recruitment; (2) randomization by the rural community; (3) data collection procedures, including collection of a battery of measures from parents and children; and (4) fidelity of intervention implementation by promotoras. We examined the acceptability of the ADAPT+ program via participant retention and program satisfaction ratings. Consistent with the stress-obesity link (Wilson & Sato, 2014), our secondary aim was to measure the preliminary effects of ADAPT+ on parents’ stress and mindful eating based at the end of treatment and 3 months post-treatment to inform a larger clinical trial.
Methods
Study Design, Recruitment, and Randomization Procedures
Study Design
We partnered with a local community-based organization, Hispanic Services Council (HSC), to conduct a longitudinal quasi-cluster study based on the study location in rural central Florida. This study was approved by the University of South Florida Institutional Review Board (Pro39979) and registered at clinicaltrials.gov (NCT04800432).
Study Participants and Procedures
HSC Promotoras trained by research study staff identified and recruited families to the study by phone and in person via (1) HSC’s ongoing educational programming, (2) flyers posted throughout the community (e.g., local stores, churches), and (3) community social networks (e.g., HSC Facebook page). Our study inclusion criteria were that (1) families had children between 8 and 12 years of age with a BMI percentile ≥85 and (2) the participating parent spoke Spanish. Parent exclusion criteria included being non-ambulatory, pregnant, or having a medical condition that might be negatively impacted by PA. Youth exclusion criteria included having a medical or developmental condition that precluded weight loss using conventional diet and PA approaches or having taken antibiotics or steroids in the three months prior to the study.
Participants were recruited from two rural locations in Florida and three cycles of intervention were completed in each location. Informed consent was obtained from all participants prior to their participation in the study. We initially sought to randomize intervention offering at the site level with ADAPT+ or Enhanced Usual Care (EUC) randomly assigned on the first and second cycles, and counterbalanced on the last cycle (Stern et al., 2021a). Due to coronavirus disease 2019 (COVID-19) barriers, including limited community space, the project statistician only was able to randomize which site offered ADAPT+ for the first cycle using a random sequence generator. Intervention delivery remained the same for cycle 2 and was counterbalanced across sites for cycle 3 (Table I). Intervention assignments were concealed from research staff; however, promotoras were aware of the intervention they would be delivering in the community. Participants were recruited in May 2021 (cycle 1: EUC), June 2021 (cycle 1: ADAPT+), September 2021 (cycle 2: EUC), October 2021 (cycle 2: ADAPT+), February 2022 (cycle 3: ADAPT+), and April 2022 (cycle 3: EUC).
Table I.
Intervention Delivery by Site and Cohort
| Rural Site 1 | Rural Site 2 | |
|---|---|---|
| Cohort 1 |
|
|
|
|
|
| Cohort 2 |
|
|
|
|
|
| Cohort 3 |
|
|
|
|
Note. 3-Month = 3-month follow-up assessment; Baseline = baseline assessment; EUC = Enhanced Usual Care.
Assessments were conducted at baseline, end of treatment (6 weeks after baseline), and 3 months after the first intervention session for both ADAPT+ and EUC (see Table I for dates). Apart from the overseeing Project Coordinator, all study staff conducting assessments were masked to condition. To address literacy concerns, all measures were delivered verbally in Spanish to parents and in English to youth. Responses were recorded by bilingual study staff. Families received a $20 gift card for baseline and end-of-treatment assessments and $25 for the 3-month follow-up assessment. Parents and children were given a fitness tracker at the baseline assessment that they were allowed to keep. Boxed meals were provided for all ADAPT+ and EUC sessions, as sessions were mainly conducted in the early evening after the workday.
Interventions
HSC Promotoras were trained to deliver both the ADAPT+ intervention and EUC (Soca Lozano et al., 2021). All parent sessions were conducted in Spanish; all youth sessions were conducted in English.
ADAPT+
The ADAPT+ intervention was refined based on findings from our proof-of-concept single-arm pilot trial (Soca Lozano et al., 2021). The original eight-session intervention was shortened to six longer sessions based on parental preferences. HSC Promotoras delivered ADAPT+ to parents in Spanish, with research staff available to help with logistical issues and childcare and to take treatment fidelity and process notes. Trained bilingual research staff led parallel child sessions in English. Parents and children participated in six 2-hr group meetings, each followed by a joint parent–child goal-setting session. Each of our six ADAPT+ sessions integrated a mindfulness stress reduction component within the behaviorally focused content (e.g., meal prep, mindful eating, PA) for both parents and children. A more comprehensive overview of ADAPT+ session content is reported elsewhere (Stern et al., 2021a).
Enhanced Usual Care (EUC)
EUC was a 2-hr session led by HSC Promotoras discussing the role of diet and exercise in pediatric obesity. EUC content was adapted from the We Can! Manual, a National Institutes of Health program to promote healthy weight in children aged 8–13 years through healthy diet and PA (National Institutes of Health). EUC families also received publicly available brochures and web-based information about various health behaviors (e.g., healthy diet, the benefits of PA) over six weeks to correspond with the number of ADAPT+ intervention sessions. These materials were distributed via email, text message, or WhatsApp, based on participants’ preferences. The EUC content had some overlap with information provided in ADAPT+, primarily related to psychoeducation about health and nutrition, and basic behavioral strategies to improve nutrition and health (e.g., reading labels, portion sizes).
Measures
Feasibility
Sample selection and recruitment: HSC Promotoras were responsible for identifying and recruiting families to the study, with a goal of ≥75% of families approached enrolling in the study. The recruitment target was the enrollment of a total of 48 parent–child dyads (total N = 96 participants).
Randomization by rural community: Randomization by the rural community was evaluated by the feasibility of site randomization and the extent to which participants could be recruited and enrolled for each intervention at each site.
Data collection procedures: Physical and self-report measurements were obtained from parents (in Spanish) and youth (in English). Research staff took anthropometric measures (height, weight, body circumference of waist and hips) and orally administered a battery of self-report measures. A trained study nurse measured resting blood pressure in triplicate (Stern et al., 2021a). See Table II for a full list of self-report measures administered as part of feasibility testing.
Table II.
Battery of Measures Assessed for Feasibility and Acceptability
| Construct | Measure |
|
|---|---|---|
| Parent | Child | |
| Acculturation |
|
|
| Physical activity |
|
|
| Dietary behaviors |
|
|
| Stress |
|
|
| Mindfulness |
|
|
| Anthropometrics & Other Health Metrics |
|
|
Feasibility of physical and self-reported data collection was operationalized based on the percentage of data provided (≥90% of all data collected at each assessment session), data quality, and the percentage of participants returning to complete end-of-treatment and 3-month follow-up assessments. Data quality was evaluated through staff reports, including participant understanding of questions and variability of responses. Measures that required extensive explanation or had limited response variability were deemed unfeasible for use in a larger clinical trial.
Fidelity of intervention implementation: Promotoras were trained to deliver the intervention with fidelity defined as promotoras delivering at least 80% of the content in line with the ADAPT+ and EUC manuals (Soca Lozano et al., 2021). Bilingual study staff attended all sessions and notes on (1) the extent to which the content delivered was consistent with the manual (fidelity) and (2) participants’ reports of their experiences in the program (process).
Acceptability
Participant retention: Retention was evaluated in two ways: (1) at least 80% of participants complete the end-of-intervention assessment and 70% of participants complete the 3-month follow-up assessment and (2) 60% of participants attend all ADAPT+ sessions and 75% attend at least 50% of all session.
Program satisfaction ratings: Both parents and youth completed a program satisfaction measure. Items assessed how satisfied parents were with the intervention (e.g., “How enjoyable did you find the program?”), how helpful they found the intervention, what they liked/disliked about the intervention, what additional information they might have wanted, and the extent to which they felt the program increased their understanding of healthy lifestyle behaviors and stress reduction strategies (e.g., “How helpful were the eating/nutrition topics?” and “How helpful were the mindfulness strategies?”). Items were rated on a scale from 0 (Not at all) to 4 (Very) enjoyable, comfortable, receptive, relevant, or helpful, depending on the item's content. A mean score was calculated using all items to reflect overall satisfaction, with higher scores indicating greater satisfaction. The helpfulness of the group sessions, eating/nutrition, PA, and mindfulness topics were also examined individually. A threshold for demonstrating program satisfaction was set a priori as 80% of participants reporting satisfaction ratings of very satisfied or satisfied (i.e., ≥3.00/4.00).
Preliminary Effect Sizes
Effect sizes of differences in key outcomes between ADAPT+ and EUC—specifically parent-reported stress and mindful eating—were examined at baseline, end of treatment, and 3-month follow-up. Changes within the condition from baseline to end of treatment and from end of treatment to 3-month follow-up also were explored. Our trial was powered to detect an average estimated effect size of Cohen’s d = 0.50 (medium) for the primary outcome of parent stress with the minimum sample size of 96 participants (i.e., 48 children, 48 parents).
Parent stress: Parent stress was measured by the Spanish version of the 10-item Perceived Stress Scale (PSS-10; Sanz-Carrillo et al., 2002). Items are rated on a scale from 0 (Never) to 4 (Very Often) and are averaged, with higher scores indicating greater perceived stress (e.g., “In the last month, how often have you felt difficulties were piling up so high that you could not overcome them?”). The PSS-10 demonstrated acceptable internal consistency at baseline (α = .78), end of treatment (α = .69), and 3-month follow-up (α = .74).
Parent mindful eating: The 9-item Recognition subscale of the Mindful Eating Questionnaire (MEQ; Clementi et al., 2017) measured the extent to which individuals recognize their satiety cues (e.g., “When I eat at all you can eat buffets, I tend to overeat.”). Items are rated on a scale from 1 (never/rarely) to 4 (usually/always) and are averaged for a total score. Higher scores indicate more mindful eating based on the recognition of satiety cues. A back-translation method was used (Colina et al., 2017) to translate this measure from English to Spanish. The translated MEQ demonstrated modest internal consistency at baseline (α = .62), poor internal consistency at the end of treatment (α = .38), and acceptable internal consistency at 3-month follow-up (α = .77).
Data Analysis
Descriptive and attrition analyses were conducted in SPSS v28. Missing baseline data were minimal; two ADAPT+ and two EUC parents missing high school graduate data, two ADAPT+ parents missing household income data, seven ADAPT+ parents missing step counting data, one ADAPT+ and six EUC parents missing food insecurity status, one ADAPT+ parent missing a number of years in the U.S. data. Generalized estimating equations do not require that dependent variables have a specific distribution and were conducted in SAS v9.4 to test the hypothesis that parents randomized to ADAPT+ would demonstrate greater reductions in stress and greater improvements in mindful eating compared to parents randomized to EUC. Two separate models were estimated for each outcome examining parents’ scores from baseline to post-treatment and from post-treatment and 3-month follow-up. The treatment group was a binary indicator.
Results
Feasibility
Sample Selection and Recruitment
Despite challenges posed by the pandemic (e.g., lack of events at which to recruit participants, difficulty securing a community location for each cycle of the study) and some mothers’ misconceptions about their children’s eligibility based on BMI criteria, the recruitment process conducted by HSC Promotoras was successful. Over 80% of the individuals approached agreed to participate in the study. A total of 95 (from a target of n = 96) participants were recruited (one parent failed to bring her child to the baseline assessment), meeting nearly 100% of our target recruitment rate. Of these 48 families, HSC Promotoras recruited 10 families who were ineligible based on youths’ BMI (n = 7; 14.9%; MBMI% = 58.78, SD = 16.09; ADAPT+ = 1, EUC = 6) or age (n = 3; 6.25%; Mage = 6.76, SD = 0.57; all ADAPT+). One family had an eligible 12-year-old child at recruitment; the child turned 13 years old right as the family started the study.
Youth participants were aged 6 to 13 years (M = 9.87, SD = 1.56) and approximately evenly split by sex (52.1% female: n = 25). Forty of the 47 youth (85.1%) had BMI percentiles at or above the 85th percentile (M = 97.28, SD = 2.77). Participating parents were aged 24–50 years (M = 38.98, SD = 7.01) and primarily female (91.7%; n = 44). Parents’ BMI ranged from 20.0 to 44.0, with the average BMI in the obese category (M = 31.43, SD = 5.25). All families were of Hispanic descent, with the majority of parents being immigrants (97.9%, n = 47) and primarily from Mexico (85.1%), followed by Guatemala (10.7%), the Dominican Republic (2.1%), and one undisclosed origin (2.1%). Demographic characteristics by treatment group are summarized in Table III.
Table III.
Baseline Demographic Characteristics of Rural Latino Children and Parents Participating in a Health Promotion Program Including Mindfulness Strategies for Stress Reduction by the Treatment Group
| ADAPT+ | EUC | p | Effect Size | |
|---|---|---|---|---|
| (n = 24) | (n = 24) | |||
| M/% (SD) | M/% (SD) | |||
| Youth | ||||
| Age | 9.73 (1.62) | 10.36 (1.45) | .165 | .41 |
| Female | 50.0% | 54.2% | 1.00 | .04 |
| Immigrant status | 12.5% | 8.3% | 1.00 | .07 |
| Average years in United Statesa,b | 4.10 (1.17) | 4.86 (3.16) | .793 | .63 |
| Weekly exercise | 41.7% | 54.2% | .564 | .13 |
| Parents | ||||
| Age | 39.60 (7.19) | 38.56 (6.92) | .545 | .18 |
| Female | 95.8% | 87.5% | .609 | .15 |
| Married or civil union | 70.8% | 79.2% | .740 | .10 |
| High school graduate or more | 54.5% | 58.3% | 1.00 | .04 |
| Parent works outside the home | 37.5% | 62.5% | .148 | .25 |
| Household income <$15,000 | 40.9% | 54.5% | .547 | .14 |
| Food insecure | 34.8% | 33.3% | 1.00 | .02 |
| Immigrant status | 95.8% | 100.0% | 1.00 | .15 |
| Average years in USA | 16.85 (7.70) | 17.04 (6.63) | .927 | −.03 |
| Weight-related family illness | 66.7% | 45.8% | .244 | .21 |
| Weekly exercise | 29.2% | 16.7% | .494 | .15 |
| Step counting | 11.8% | 0.0% | .166 | .27 |
| Average number of children | 3.46 (1.41) | 3.21 (1.25) | .520 | .19 |
| Concern with child’s weight | 91.7% | 66.7% | .072 | .31 |
Only reported for youth indicating immigrant status.
Unequal variances. Cohen’s d reported for continuous variables. Hedges’ g reported for continuous variables with unequal variances. Cramer’s V reported for categorical variables. Fisher’s exact test for categorical variables.
Randomization by Rural Community
Randomization was limited to the first intervention cycle due to COVID-19-related study implementation challenges. We successfully counterbalanced intervention delivery across our two community rural sites and recruited sufficient participants. On average, eight families (parent and youth dyads) were enrolled at each site for each cohort (Table I). There were no significant baseline differences in demographics or constructs of interest between the treatment groups; however, more ADAPT+ parents reported concern with their child’s weight and this was a medium, though non-significant, effect (V = 0.31; Table III).
Data Collection Procedures
Data collection was feasible. All attending parents and youth provided 100% data with the help of study staff at assessment sessions, including measurement of anthropometrics and blood pressure and completion of all self-report measures. Parents who were missing any data reported lower baseline stress compared to parents who provided full data (i.e., attended all three assessment sessions; d = .84).
All parents and youth randomized to ADAPT+ reported using the provided fitness trackers to set goals. Notably, families anecdotally expressed enthusiasm about using the trackers, suggesting their utility as part of a future larger trial. The fitness trackers included in the present study lacked sophisticated methods of transmitting data and were used primarily to evaluate whether fitness tracker use would be feasible and acceptable in our target population.
In terms of data quality, there were no reported concerns related to the measurement of anthropometrics or resting blood pressure. Participants generally reported understanding the questions and provided a variety of responses to all self-reported measures, except for the 5-item Acting with Awareness subscale of the Five Facets Mindfulness Questionnaire—Short Form (see Table III; Bohlmeijer et al., 2011; Cebolla et al., 2012). Parents struggled to understand the items, leading the research team to revise the response options mid-study. Participants continued to have difficulty, suggesting that this measure should not be used with this population in a larger clinical trial. See Supplementary Tables 1–4 for raw means of all data collected as part of this pilot study.
Fidelity of Intervention Implementation
All planned sessions were implemented (100%). Over 80% of each ADAPT+ session was implemented as described by the manual. HSC Promotoras improved their content delivery over time as they became more familiar with the manual and received supervision after each session (Soca Lozano et al., 2021).
Acceptability
Participant Retention
All but three participants (n = 92; 96.8%) returned to begin the intervention the week following the baseline assessment. We exceeded benchmarks for participants completing the end of treatment and 3-month follow-up assessments, with a total of 86% (n = 79) of participants completing post-assessment and 82.6% (n = 76) completing the 3-month follow-up assessment.
Average attendance rates for ADAPT+ exceeded our a priori acceptability thresholds of 60% of participants attending all sessions and 75% of participants attending at least half the sessions. Participant attendance ranged from approximately 75% to 95% of sessions. Reported reasons for absences included lack of transportation, bad weather (including hurricane warnings), being sick with COVID-19 or other illness, or work-related conflicts. There was no evidence of specific families missing multiple ADAPT+ sessions in a row.
Program Satisfaction
The 22 parents who received the ADAPT+ program and completed the end-of-treatment satisfaction survey reported a mean program satisfaction rating of 3.91/4.00 (SD = 0.18, range from 3.18 to 4.00). The vast majority of responding parents reported the group sessions were very helpful (n = 21; 95.5%), 95.5% reported the eating/nutrition topics were very helpful (n = 21), 90.9% reported the PA topics were very helpful (n = 20), and 81.8% reported the mindfulness topics were very helpful (n = 18). There was no significant difference between the satisfaction ratings of parents randomized to ADAPT+ (M = 3.91, SD = 0.18) and EUC (M = 3.85, SD = 0.32; p = .778; small effect, d = .22), suggesting comparable acceptability. This supports our EUC as an active control condition and appropriate comparison to ADAPT+.
The 22 youths who completed the satisfaction survey similarly reported satisfaction with the ADAPT+ program (M = 3.31, SD = 0.62, range from 2.00 to 4.00). The majority of youth (n = 15; 68.1%) reported at least moderate satisfaction with the program and 50% (n = 11) reported an average satisfaction score of ≥3.50. The majority of youth reported the group sessions were very helpful (n = 14; 63.6%), 72.7% reported the eating/nutrition topics were very helpful (n = 16), 63.6% reported the PA topics were very helpful (n = 14), and 68.2% reported the mindfulness topics were very helpful (n = 15).
Preliminary Effect Sizes
Parent Stress
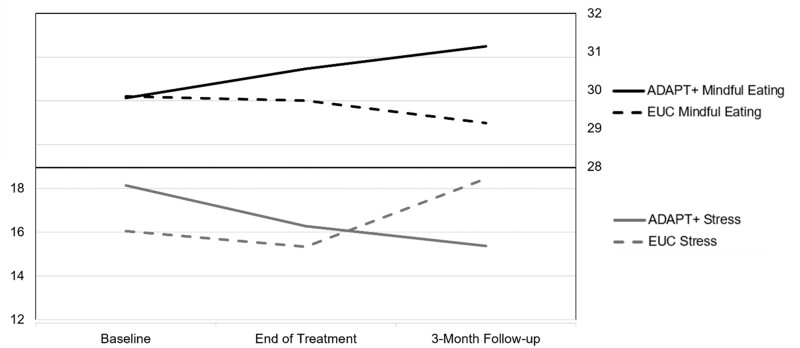
Forty participants (ADAPT+ n = 22; EUC n = 18) were included in the post-treatment analysis. Forty-one participants (ADAPT+ n = 22; EUC n = 16) were included in the 3-month follow-up analysis. ADAPT+ parents had higher stress than EUC parents at baseline (difference = 2.08, medium effect, d = .33) and end of treatment (difference = −0.94, small-to-medium effect, d = .19), but lower stress at 3-month follow-up (difference = −3.04, medium-to-large effect, d = .70). As anticipated, the decrease in parent stress from baseline to end of treatment was larger for ADAPT+ parents (change = −2.18; 95% CI −3.98 to −0.038) compared to EUC parents (change = −1.27; 95% CI −4.12 to 1.57). Stress reported by ADAPT+ parents continued to decrease modestly from end of treatment to 3-month follow-up (change = −0.91; 95% CI − 2.67 to 0.85), while it increased for EUC parents (change = 2.72; 95% CI 0.42–5.03; see Figure 1).
Figure 1.
Means of parent stress and mindful eating at baseline, end of treatment, and 3-month follow-up.
Session fidelity and process notes supported that parents and youth were engaged in the mindfulness exercises during and outside of sessions. One mother reported “using the ‘STOP’ mindfulness strategy” she learned to deal with feelings of “stress,” and youth were able to identify times when they felt stress (e.g., “being late for school” or having to do “too much homework”). Youth expressed “feeling calmer” and that their “heart was more ‘relaxed’ after…” participating in the mindfulness exercise.
Parent Mindful Eating
ADAPT+ and EUC parents reported comparable mindful eating at baseline (difference = 0.04, small effect, d = .01). ADAPT+ parents reported more mindful eating at post-treatment (difference = 0.84, small-to-medium effect, d = .29) and 3-month follow-up (difference = 2.00, medium effect, d = .44). As anticipated, on average, ADAPT+ parents reported increases in mindful eating from baseline to end of treatment (change = 0.70; 95% CI −1.28 to 2.68), while EUC parents did not (difference = −.08; 95% CI −1.48 to 1.31). Parents randomized to ADAPT+ reported increases in mindful eating from the end of treatment to 3-month follow-up (difference = 0.59; 95% CI −1.65 to 2.83), while parents randomized to EUC reported decreases in mindful eating (difference = −0.57; 95% CI −2.95 to 1.81; see Figure 1).
Session fidelity and process notes indicated that participants reported changes in dietary behaviors. Most parents reported not reading food labels at the start of the program. During the intervention, one mother reported that according to her pediatrician, her child had lost weight and that his cholesterol was now under control. She attributed this to “learning how to read nutrition labels and about portion sizes.” Participants also more generally reported that they were practicing their “SMART” (Specific, Measurable, Achievable, Realistic/Relevant, and Timed) goals each week. The youth noted that collaboratively setting “SMART” goals with their parents made them feel involved in the healthy lifestyle process.
Discussion
This study demonstrated the feasibility and acceptability of study execution (e.g., participant recruitment and retention, full data collection) and intervention delivery of our six-session ADAPT+ intervention by community health workers—i.e., promotoras—to rural Latino families in central Florida. Preliminary evidence suggests that ADAPT+ may facilitate decreases in parents’ stress and increases in their mindful eating. Overall, findings support testing the delivery of ADAPT+ to rural Latino families in a larger clinical trial.
Study implementation was feasible. Both parents and youth attending assessment sessions completed all measures, used provided fitness trackers, and performed the mindfulness exercises. Participants reported practicing their “SMART” goals each week, and HSC Promotoras successfully delivered the ADAPT+ protocol with high fidelity during COVID-19. Although we were unable to randomize as initially proposed due to COVID-19, interventions were successfully counterbalanced across study sites. The impact of COVID-19 on the study was exacerbated by structural barriers, including a lack of adequate spaces in the community that could accommodate both parents and children after school or over the weekend. Given the myriad of barriers that the rural Latino population often endure to participate in health promotion programs (e.g., language, transportation, fear of deportation, childcare, work hours, etc.) developing an intervention that can be delivered by trained community members is important to dissemination and continuation of ADAPT+ in the community.
Despite overall evidence that study implementation was feasible, HSC Promotoras did recruit a number of families who did not meet the study inclusion criteria. It is unclear whether this was due to a need for more education and training related to study recruitment, the need for different marketing materials, or if it was related to the impact of the COVID-19 pandemic on recruitment opportunities. It will be important to address the element of family eligibility preemptively in a larger trial.
Overall, the measures included in this study were appropriate for the rural Latino population. Surprisingly, parents had no difficulty with the MEQ (Clementi et al., 2017), but struggled to understand how to answer questions related to mindfulness more generally. Recent work investigated the sensitivity of various mindfulness questionnaires to detect treatment-related change (Baer et al., 2019); however, the generalizability of these results to our primarily Spanish-speaking, low-literacy population is uncertain. Although the stress and mindful eating measures had acceptable internal consistency at baseline and 3-month follow-up, both showed lower internal consistency, especially the mindful eating measure and limited response variability at the end of treatment. Most responses clustered around the midpoint of the response scale, which may reflect social desirability effects (Hopwood et al., 2009). Measurement considerations, including social desirability and identification of reliable and valid measures of broad mindfulness constructs, need to be addressed for a larger clinical trial with this population.
Both youth and parents reported high satisfaction with the ADAPT+ program, and attendance and retention rates were high. All or nearly all parents reported that the group sessions, particularly the nutrition/eating topics, were very helpful. Importantly, both parents and youth found the mindfulness skills helpful. This is consistent with other work reporting high acceptability of mindfulness interventions among Latino family dyads (Cotter & Jones, 2020; Tobin et al., 2021). HSC Promotoras continue to use the mindfulness techniques learned during this study as icebreakers in community presentations.
There was preliminary evidence of the effects of ADAPT+ on key constructs of interest. In line with our theoretical framework, we detected decreases in stress and increases in mindful eating for parents in ADAPT+, compared to increases in stress and decreases in mindful eating among EUC parents. Although families enjoyed the nutrition and PA lessons, the stress reduction portions of our sessions were new to most families, and both parents and youth expressed interest in continuing to use these strategies. Given the role that stress plays in obesity (Tomiyama, 2019), reducing stress might be key to observable health behavior change over time. Examining whether reducing stress in marginalized families promotes health behavior change outcomes is warranted.
In terms of strengths, this study tested the feasibility of delivering a lifestyle education program to a rural and underserved community by its own community members. Despite COVID-19-related barriers, ADAPT+ was tested in two rural communities. The close working relationship with our community partner was key to successful implementation. Nonetheless, there are limitations to consider. This study was not intended to test the efficacy of ADAPT+, and the reported effects are preliminary in nature. More oversight and/or training of promotoras is needed regarding recruitment, inclusion, and exclusion criteria and the imbalance of the ineligible families due to BMI percentile and age across interventions may have biased results. Given the community-based nature of the project and the potential negative impact on community relations, all families recruited by the HSC Promotoras were included in the study and analyses, regardless of eligibility criteria. Lay persons, despite having culturally relevant perspectives, likely need more supervision/training related to study recruitment. Last, participating parents primarily were mothers, consistent with parent-based intervention research, while youth were evenly split by sex.
Conclusions
Overall, our intervention, ADAPT+, demonstrated strong feasibility and acceptability when delivered by promotoras to groups of Latino families living in rural communities. Importantly, HSC Promotoras successfully taught basic mindfulness concepts and skills to a community for whom mindfulness was a relatively novel concept, and the observed changes in parent stress and mindful eating were in the anticipated directions. In all, findings support the utility of testing ADAPT+ with a fully powered randomized control trial against our active control intervention.
Supplementary Material
Acknowledgments
Thanks to the Hispanic Services Council Promotoras Judy Ramos, Liliana Ramirez, Ruth Borude, Tania Garcia, Velia Huitron, and Veronica Ortiz, and staff members of the Hispanic Services Council Frances Luna, Rocio “Rosy” Bailey, and Maria F. Pinzon. We also want to thank our participating families from the rural communities of Plant City and Wimauma, Florida.
Contributor Information
Marilyn Stern, Department of Child and Family Studies, College of Behavioral and Community Sciences, University of South Florida, USA; Department of Health Outcomes and Behavior, Moffitt Cancer Center, USA.
Diana Rancourt, Department of Psychology, University of South Florida, USA.
Sandra Soca Lozano, College of Education, University of South Florida, USA.
Acadia W Buro, Department of Health Outcomes and Behavior, Moffitt Cancer Center, USA.
Heewon L Gray, College of Public Health, University of South Florida, USA.
Carmen Rodriguez, College of Nursing, University of South Florida, USA.
Rocio Bailey, Hispanic Services Council, USA.
Laura Redwine, Department of Family Medicine and Community Health, Miller School of Medicine, University of Miami, USA.
Supplementary Data
Supplementary data can be found at: https://academic.oup.com/jpepsy.
Funding
This work was supported by funding from the National Institutes of Health (NIH) National Center for Complementary and Integrative Health (R34AT010661-01, Stern and Redwine, MPI). AWB was supported by the National Cancer Institute Behavioral Oncology Education and Career Development Grant (T32CA090314, MPIs Vadaparampil/Brandon). NIH had no role in the study design, writing of the manuscript, or the decision to submit the paper for publication.
Conflicts of interest
None declared.
Author Contributions
Marilyn Stern (Conceptualization [lead], Funding acquisition [lead], Methodology [lead], Supervision [lead], Validation [equal], Visualization [equal], Writing—original draft [equal], Writing—review & editing [equal]), Diana Rancourt (Conceptualization [equal], Data curation [lead], Formal analysis [lead], Funding acquisition [equal], Investigation [equal], Methodology [equal], Resources [equal], Software [equal], Validation [equal], Visualization [lead], Writing—original draft [equal], Writing—review & editing [equal]), Sandra Soca Lozano (Investigation [equal], Methodology [supporting], Project administration [equal], Visualization [equal], Writing—original draft [supporting], Writing—review & editing [equal]), Acadia W. Buro (Methodology [supporting], Validation [equal], Visualization [equal], Writing—original draft [equal], Writing—review & editing [equal]), Heewon L. Gray (Conceptualization [equal], Funding acquisition [equal], Investigation [equal], Methodology [equal], Supervision [equal], Validation [equal], Visualization [equal], Writing—original draft [equal], Writing—review & editing [equal]), Carmen Rodriguez (Conceptualization [equal], Funding acquisition [equal], Investigation [equal], Validation [supporting], Writing—original draft [supporting], Writing—review & editing [supporting]), Rocio Bailey (Conceptualization [supporting], Funding acquisition [supporting], Investigation [equal], Resources [equal], Writing—review & editing [supporting]), and Laura Redwine (Conceptualization [lead], Funding acquisition [lead], Methodology [lead], Supervision [lead], Validation [equal], Visualization [equal], Writing—original draft [equal], Writing—review & editing [equal])
Ethical Approval
This study was conducted in accordance with the ethical principles outlined in the Declaration of Helsinki and was approved by the Institutional Review Board (IRB) at the University of South Florida. Informed consent was obtained from all participants prior to their participation in the study.
Data Availability
Data that support the findings of this study are available from the authors upon reasonable request.
References
- Ayala G. X., Vaz L., Earp J. A., Elder J. P., Cherrington A. (2010). Outcome effectiveness of the lay health advisor model among Latinos in the United States: An examination by role. Health Education Research, 25(5), 815–840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baer R., Gu J., Cavanagh K., Strauss C. (2019). Differential sensitivity of mindfulness questionnaires to change with treatment: A systematic review and meta-analysis. Psychological Assessment, 31(10), 1247–1263. 10.1037/pas0000744 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baskind M. J., Taveras E. M., Gerber M. W., Fiechtner L., Horan C., Sharifi M. (2019). Parent-perceived stress and its association with children's weight and obesity-related behaviors. Preventing Chronic Disease, 16, E39. 10.5888/pcd16.180368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bohlmeijer E., ten Klooster P. M., Fledderus M., Veehof M., Baer R. (2011). Psychometric properties of the five facet mindfulness questionnaire in depressed adults and development of a short form. Assessment, 18(3), 308–320. 10.1177/1073191111408231 [DOI] [PubMed] [Google Scholar]
- Bolin J. N., Bellamy G., Ferdinand A. O., Kash B. A., Helduser J. W. (Eds.). (2015). Rural healthy people 2020 (Vol. 1). Texas A&M Health Science Center School of Public Health, Southwest Rural Health Research Center. https://srhrc.tamhsc.edu/docs/rhp2020-volume-1.pdf. [Google Scholar]
- Cebolla A., Garcia-Palacios A., Soler J., Guillén V., Baños R., Botella C. (2012). Psychometric properties of the Spanish validation of the Five Facets of Mindfulness Questionnaire (FFMQ). The European Journal of Psychiatry, 26(2), 118–126. 10.4321/S0213-61632012000200005 [DOI] [Google Scholar]
- Clementi C., Casu G., Gremigni P. (2017). An abbreviated version of the mindful eating questionnaire. Journal of Nutrition Education and Behavior, 49(4), 352–356.e1. e351. 10.1016/j.jneb.2017.01.016 [DOI] [PubMed] [Google Scholar]
- Coatsworth J. D., Duncan L. G., Nix R. L., Greenberg M. T., Gayles J. G., Bamberger K. T., Berrena E., Demi M. A. (2015). Integrating mindfulness with parent training: Effects of the mindfulness-enhanced strengthening families program. Developmental Psychology, 51(1), 26–35. 10.1037/a0038212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S., , KamarckT., & , Mermelstein R. (1983). A Global Measure of Perceived Stress. Journal of Health and Social Behavior, 24(4), 385. 10.2307/2136404 [DOI] [PubMed] [Google Scholar]
- Colina S., Marrone N., Ingram M., Sanchez D. (2017). Translation quality assessment in health research: A functionalist alternative to back-translation. Evaluation & the Health Professions, 40(3), 267–293. 10.1177/0163278716648191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cotter E. W., Jones N. (2020). A review of Latino/Latinx participants in mindfulness-based intervention research. Mindfulness, 11(3), 529–553. 10.1007/s12671-019-01266-9 [DOI] [Google Scholar]
- Cruz P., Granados A. (2019). Type 2 diabetes in Latino youth: A clinical update and current challenges. Current Problems in Pediatric and Adolescent Health Care, 49(1), 16–22. 10.1016/j.cppeds.2018.11.008 [DOI] [PubMed] [Google Scholar]
- Czajkowski S. M., Powell L. H., Adler N., Naar-King S., Reynolds K. D., Hunter C. M., Laraia B., Olster D. H., Perna F. M., Peterson J. C., Epel E., Boyington J. E., Charlson M. E. (2015). From ideas to efficacy: The ORBIT model for developing behavioral treatments for chronic diseases. Health Psychology, 34(10), 971–982. 10.1037/hea0000161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Daly P., Pace T., Berg J., Menon U., Szalacha L. A. (2016). A mindful eating intervention: A theory-guided randomized anti-obesity feasibility study with adolescent Latino females. Complementary Therapies in Medicine, 28, 22–28. 10.1016/j.ctim.2016.07.006 [DOI] [PubMed] [Google Scholar]
- Falbe J., Friedman L. E., Sokal-Gutierrez K., Thompson H. R., Tantoco N. K., Madsen K. A. (2017). She gave me the confidence to open up”: Bridging communication by promotoras in a childhood obesity intervention for Latino families. Health Education & Behavior, 44(5), 728–737. 10.1177/1090198117727323 [DOI] [PubMed] [Google Scholar]
- Fernandez S., , OlendzkiB., & , Rosal M. C. (2011). A dietary behaviors measure for use with low-income, Spanish-speaking Caribbean Latinos with type 2 diabetes: the Latino Dietary Behaviors Questionnaire. Journal of the American Dietetic Association, 111(4), 589–599. 10.1016/j.jada.2011.01.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foster B. A., Weinstein K., Padilla T., Martinez C., Angeles-Ramos D. (2022). Growing healthy together: A randomized clinical trial using parent mentors for early childhood obesity in low-income, Latino families. Childhood Obesity (Print), 18(3), 168–177. 10.1089/chi.2021.0165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcini L. M., Daly R., Chen N., Mehl J., Pham T., Phan T., Hansen B., Kothare A. (2021). Undocumented immigrants and mental health: A systematic review of recent methodology and findings in the United States. Journal of Migration and Health, 4, 100058. 10.1016/j.jmh.2021.100058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hernandez, Y. (2011). Measuring the impact of youth EFNEP: Questionnaire development and validation [Doctoral dissertation, Clemson University]. All Dissertations. https://tigerprints.clemson.edu/cgi/viewcontent.cgi?article=1773&context=all_dissertations
- Halperin D. T., Laux J., LeFranc-García C., Araujo C., Palacios C. (2019). Findings from a randomized trial of weight gain prevention among overweight Puerto Rican young adults. Journal of Nutrition Education and Behavior, 51(2), 205–216. 10.1016/j.jneb.2018.07.014 [DOI] [PubMed] [Google Scholar]
- Hopwood C. J., Flato C. G., Ambwani S., Garland B. H., Morey L. C. (2009). A comparison of Latino and Anglo socially desirable responding. Journal of Clinical Psychology, 65(7), 769–780. 10.1002/jclp.20584 [DOI] [PubMed] [Google Scholar]
- Isasi C. R., Hua S., Jung M., Carnethon M. R., Perreira K., Vidot D. C., Salazar C. R., McCurley J. L., Sotres-Alvarez D., Van Horn L., Delamater A. M., Llabre M. M., Gallo L. C. (2017). The association of parental/caregiver chronic stress with youth obesity: Findings from the study of Latino youth and the Hispanic community health study/study of Latinos sociocultural ancillary study. Childhood Obesity (Print), 13(4), 251–258. 10.1089/chi.2016.0205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Janicke D. M., Steele R. G., Gayes L. A., Lim C. S., Clifford L. M., Schneider E. M., Carmody J. K., Westen S. (2014). Systematic review and meta-analysis of comprehensive behavioral family lifestyle interventions addressing pediatric obesity. Journal of Pediatric Psychology, 39(8), 809–825. 10.1093/jpepsy/jsu023 [DOI] [PubMed] [Google Scholar]
- Jastreboff A. M., Chaplin T. M., Finnie S., Savoye M., Stults-Kolehmainen M., Silverman W. K., Sinha R. (2018). Preventing childhood obesity through a mindfulness-based parent stress intervention: A randomized pilot study. The Journal of Pediatrics, 202, 136–142.e1. 10.1016/j.jpeds.2018.07.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keck-Kester T., Huerta-Saenz L., Spotts R., Duda L., Raja-Khan N. (2021). Do mindfulness interventions improve obesity rates in children and adolescents: A review of the evidence. Diabetes, Metabolic Syndrome and Obesity, 14, 4621–4629. 10.2147/DMSO.S220671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kristeller J. L., Wolever R. Q. (2011). Mindfulness-based eating awareness training for treating binge eating disorder: The conceptual foundation. Eating Disorders, 19(1), 49–61. 10.1080/10640266.2011.533605 [DOI] [PubMed] [Google Scholar]
- Leung M., Barata-Cavalcanti O., Dada A., Brown M., Mateo K., Yeh M.-C. (2017). Treating obesity in Latino children: A systematic review of current interventions. International Journal of Child Health and Nutrition, 6(1), 1–15. [Google Scholar]
- Lutfiyya M. N., Lipsky M. S., Wisdom-Behounek J., Inpanbutr-Martinkus M. (2007). Is rural residency a risk factor for overweight and obesity for U.S. children? Obesity (Silver Spring, Md.), 15(9), 2348–2356. 10.1038/oby.2007.278 [DOI] [PubMed] [Google Scholar]
- Min J., Goodale H., Xue H., Brey R., Wang Y. (2021). Racial-ethnic disparities in obesity and biological, behavioral, and sociocultural influences in the United States: A systematic review. Advances in Nutrition (Bethesda, Md.), 12(4), 1137–1148. 10.1093/advances/nmaa162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murray E. K., , AuldG., , BakerS. S., , BaraleK., , FranckK., , KhanT., , Palmer-KeenanD., & , Walsh J. (2017). Methodology for Developing a New EFNEP Food and Physical Activity Behaviors Questionnaire. Journal of Nutrition Education and Behavior, 49(9), 777–783.e1. 10.1016/j.jneb.2017.05.341 [DOI] [PubMed] [Google Scholar]
- National Institutes of Health. ¡Podemos! Sugerencias para mejorar la actividad y nutrición de los niños. https://www.nhlbi.nih.gov/health/educational/wecan/espanol/
- Okobi O. E., Ajayi O. O., Okobi T. J., Anaya I. C., Fasehun O. O., Diala C. S., Evbayekha E. O., Ajibowo A. O., Olateju I. V., Ekabua J. J., Nkongho M. B., Amanze I. O., Taiwo A., Okorare O., Ojinnaka U. S., Ogbeifun O. E., Chukwuma N., Nebuwa E. J., Omole J. A., Udoete I. O., Okobi R. K. (2021). The burden of obesity in the rural adult population of America. Cureus, 13(6), e15770. 10.7759/cureus.15770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paixão T. M., Teixeira L. R., Andrade C. A. F., Sepulvida D., Martinez-Silveira M., Nunes C., Siqueira C. E. G. (2023). Systematic review and meta-analysis of metabolic syndrome and its components in Latino immigrants to the USA. International Journal of Environmental Research and Public Health, 20(2), 1307. 10.3390/ijerph20021307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peacock N., Issel L. M., Townsell S. J., Chapple-McGruder T., Handler A. (2011). An innovative method to involve community health workers as partners in evaluation research. American Journal of Public Health, 101(12), 2275–2280. 10.2105/ajph.2011.300263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pena M. M., Dixon B., Taveras E. M. (2012). Are you talking to ME? The importance of ethnicity and culture in childhood obesity prevention and management. Childhood Obesity (Print), 8(1), 23–27. 10.1089/chi.2011.0109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perez L. G., Arredondo E. M., Elder J. P., Barquera S., Nagle B., Holub C. K. (2013). Evidence-based obesity treatment interventions for Latino adults in the U.S.: A systematic review. American Journal of Preventive Medicine, 44(5), 550–560. 10.1016/j.amepre.2013.01.016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reis W. P., Ghamsary M., Galustian C., Galust H., Herring P., Gaio J., Dos Santos H. (2020). Childhood obesity: Is the built environment more important than the food environment? Clinical Medicine Insights. Pediatrics, 14, 1179556520932123. 10.1177/1179556520932123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rhodes S. D., Foley K. L., Zometa C. S., Bloom F. R. (2007). Lay health advisor interventions among Hispanics/Latinos: A qualitative systematic review. American Journal of Preventive Medicine, 33(5), 418–427. 10.1016/j.amepre.2007.07.023 [DOI] [PubMed] [Google Scholar]
- Rodriguez R., Weffer S. E., Romo J., Aleman A., Ortiz R. M. (2011). Reduced physical activity levels associated with obesity in rural Hispanic adolescent females. Childhood Obesity, 7(3), 194–205. 10.1089/chi.2011.0007 [DOI] [Google Scholar]
- Rogers J. M., Ferrari M., Mosely K., Lang C. P., Brennan L. (2017). Mindfulness‐based interventions for adults who are overweight or obese: A meta‐analysis of physical and psychological health outcomes. Obesity Reviews, 18(1), 51–67. https://doi.org/10.1111 [DOI] [PubMed] [Google Scholar]
- Rosado J. I., Johnson S. B., Wang Y., Fundingsland S., Salazar J. (2022). Addressing Childhood Obesity among Latino Agricultural Families: Data from a Feasibility Study at a Community Health Center. Journal of Health Care for the Poor and Underserved, 33(1), 286–300. 10.1353/hpu.2022.0021 [DOI] [PubMed] [Google Scholar]
- Sanz-Carrillo C., Garcıa-Campayo J., Rubio A., Santed M., Montoro M. (2002). Validation of the Spanish version of the Perceived Stress Questionnaire. Journal of Psychosomatic Research, 52(3), 167–172. 10.1016/S0022-3999(01)00275-6 [DOI] [PubMed] [Google Scholar]
- Seguin R., Connor L., Nelson M., LaCroix A., Eldridge G. (2014). Understanding barriers and facilitators to healthy eating and active living in rural communities. Journal of Nutrition and Metabolism, 2014, 146502. 10.1155/2014/146502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soca Lozano S., Gonzalez K., Stern M. (2021). Training “Promotoras” in the Delivery of ADAPT+: A Healthy Lifestyle Intervention for Latinos with Obesity in Rural Communities. Paper presented to the meetings of the Society of Pediatric Psychology, virtual. [Google Scholar]
- Stephenson M. (2000). Development and validation of the Stephenson Multigroup Acculturation Scale (SMAS). Psychological Assessment, 12(1), 77–88. 10.1037/1040-3590.12.1.77 [DOI] [PubMed] [Google Scholar]
- Stern M., Redwine L., Soca Lozano S., Rancourt D., Rodriguez C., Gray H. L., Lock S., Bailey R. (2021a). Design and rationale for ADAPT+: Optimizing an intervention to promote healthy behaviors in rural, Latino youth with obesity and their parents, using mindfulness strategies. Contemporary Clinical Trials, 101, 106243. 10.1016/j.cct.2020.106243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stern M., Soca Lozano S., Lescano C., Rodriguez C., Redwine L. (2021b). Developing Adaptando Dieta Y Acción Para Todos (ADAPT): An intervention to improve healthy lifestyle behaviors among Latino parents and children living in rural communities. Journal of Immigrant and Minority Health, 23(1), 88–94. 10.1007/s10903-020-01037-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stierman B., Joseph A., Carroll M. D., Chen T.-C., Davy O., Fink S., Fryar C. D., Gu Q., Hales C. M., Hughes J. P., Ostchega Y., Storandt R. J., Akinbami L. J. (2021). National Health and Nutrition Examination Survey 2017–March 2020 prepandemic data files development of files and prevalence estimates for selected health outcomes. National Health Statistics Reports. https://stacks.cdc.gov/view/cdc/106273
- Stone G. A., Fernandez M., DeSantiago A. (2022). Rural Latino health and the built environment: A systematic review. Ethnicity & Health, 27(1), 1–26. 10.1080/13557858.2019.1606899 [DOI] [PubMed] [Google Scholar]
- Tobin J., Hardy J., Calanche M. L., Gonzalez K. D., Baezconde-Garbanati L., Contreras R., Bluthenthal R. N. (2021). A community-based mindfulness intervention among Latino adolescents and their parents: A qualitative feasibility and acceptability study. Journal of Immigrant and Minority Health, 23(2), 344–352. 10.1007/s10903-020-00985-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tomiyama A. J. (2019). Stress and Obesity. Annual Review of Psychology, 70, 703–718. 10.1146/annurev-psych-010418-102936 [DOI] [PubMed] [Google Scholar]
- Townsend M. S., , JohnsM., , ShiltsM. K., & , Farfan-Ramirez L. (2006). Evaluation of a USDA nutrition education program for low-income youth. Journal of Nutrition Education and Behavior, 38(1), 30––41.. 10.1016/j.jneb.2005.11.014 [DOI] [PubMed] [Google Scholar]
- Tucker K., Ingram M., Doubleday K., Piper R., Sander A., Flores R., Martinez D., Carvajal S. (2022). Results from La Vida Buena (the good life): A quasi-experimental intervention of a community health worker-led family-based childhood obesity program for Latino children 5-8 years of age on the U.S.-Mexico border. Health Promotion Practice, 15248399221112691. 10.1177/15248399221112691 [DOI] [PubMed] [Google Scholar]
- Van Jaarsveld C. H., Fidler J. A., Steptoe A., Boniface D., Wardle J. (2009). Perceived stress and weight gain in adolescence: A longitudinal analysis. Obesity (Silver Spring, Md.), 17(12), 2155–2161. 10.1038/oby.2009.183 [DOI] [PubMed] [Google Scholar]
- Viramontes O., Swendeman D., Moreno G. (2017). Efficacy of behavioral interventions on biological outcomes for cardiovascular disease risk reduction among Latinos: A review of the literature. Journal of Racial and Ethnic Health Disparities, 4(3), 418–424. 10.1007/s40615-016-0242-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y., Beydoun M. A., Min J., Xue H., Kaminsky L. A., Cheskin L. J. (2020). Has the prevalence of overweight, obesity and central obesity levelled off in the United States? Trends, patterns, disparities, and future projections for the obesity epidemic. International Journal of Epidemiology, 49(3), 810–823. 10.1093/ije/dyz273 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson S. M., Sato A. F. (2014). Stress and paediatric obesity: What we know and where to go. Stress and Health, 30(2), 91–102. 10.1002/smi.2501 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data that support the findings of this study are available from the authors upon reasonable request.