Abstract
Purpose:
People who stutter often experience significant adverse impact related to stuttering. However, it is unclear how adverse impact develops in children who stutter (CWS) and whether there are protective factors that may mitigate its development. This study examined the relationship between resilience, a potentially protective factor, and stuttering's adverse impact in CWS. Resilience comprises external factors, such as family support and access to resources as well as personal attributes, making it a comprehensive protective factor to explore.
Method:
One hundred forty-eight CWS aged 5–18 years completed the age-appropriate version of the Child and Youth Resilience Measure (CYRM) and the Overall Assessment of the Speaker's Experience of Stuttering. Parents completed a caregiver version of the CYRM and a behavioral checklist for their child. The adverse impact of stuttering was modeled as a function of resilience (external, personal, and total), controlling for child age and behavioral checklist score. We also estimated correlations between child-report and parent-report CYRM measures to assess rater agreement.
Results:
Children reporting greater external, personal, or total resilience were more likely to experience lower degrees of adverse impact related to their stuttering. We documented stronger correlations between younger child and parent ratings of resilience and weaker correlations between older child and parent ratings.
Conclusions:
These results yield valuable insight into the variability of adverse impact experienced by CWS and offer empirical support for strength-based speech therapy approaches. We discuss the factors that contribute to a child's resilience and provide practical suggestions for how clinicians can incorporate resilience-building strategies into intervention for children experiencing significant adverse impact from their stuttering.
Supplemental Material:
Research on the adverse impact of stuttering has sought to capture the real-life consequences of stuttering, aiming to identify those characteristics unobservable to the listener that contribute to how an individual experiences stuttering. It is unclear, however, how adverse impact develops in people who stutter. We define the adverse impact of stuttering as the summative effect of the negative thoughts, feelings, and behaviors that a person develops in reaction to the underlying impairment, combined with the real-world limitations that result from living with the condition (Tichenor & Yaruss, 2019; Yaruss & Quesal, 2004). Yaruss and colleagues adapted the World Health Organization's (WHO) International Classification of Functioning, Disability and Health (WHO, 2001) classification scheme for stuttering to provide a more comprehensive profile of the condition and meaningful framework to capture how individuals experience stuttering (Tichenor & Yaruss, 2019; Yaruss, 1998; Yaruss & Quesal, 2004). Their adaptation includes barriers associated with the impairment (observable characteristics including speech disfluencies) along with the adverse impact (e.g., negative thoughts, societal stigma, and limitations/barriers to participation) to a person's life. They emphasized that internal or personal and external or environmental/societal factors play a role in how stuttering affects a person's life, leading to widely different experiences.
Many adults experience significant adverse impact related to their stuttering. Individuals may feel shame, anxiety, a diminished sense of self-confidence, or experience social isolation (Blumgart et al., 2010; Iverach et al., 2009; Menzies et al., 2008; Stein et al., 1996). They may engage in repetitive negative thought patterns (Tichenor & Yaruss, 2020), encounter societal stigma or harbor self-stigma (Boyle, 2013, 2018), and, concerningly, have increased suicidal thoughts (Briley et al., 2021; Tichenor et al., in press). For some individuals, stuttering may impact employment or economic opportunities (Gerlach et al., 2018; J. F. Klein & Hood, 2004) or cause difficulties with romantic relationships (Van Borsel et al., 2011).
We do not yet know how or when adverse impact related to stuttering develops; yet, a growing literature reveals that children who stutter (CWS), like adults, also face significant adverse impact (Beilby et al., 2012; Samson et al., 2021). Awareness of stuttering emerges in the preschool years (Ambrose & Yairi, 1994; Boey et al., 2009). Yairi and Ambrose (2005) argued that stuttering awareness should logically precede the development of negative emotions and reactions, yet it is possible that the two develop in parallel considering that many early signs of stuttering awareness are inherently negative. A large parent-report study of over 800 preschoolers established awareness in preschool CWS that increased over time from approximately 57% of 2-year-olds to 80% of 5-year-old CWS when overt and more nuanced indicators of awareness were considered (Boey et al., 2009). Indicators of awareness reported by parents included sadness/crying, impatience, anger, or leaving/stop speaking, for example, supporting the notion that, for some children, awareness and negative emotions emerge concurrently (Boey et al., 2009; Langevin et al., 2010). Although it remains unclear exactly how or when adverse impact emerges between early stuttering awareness and adulthood, research involving CWS has revealed important factors to consider in its development. CWS are more likely to harbor negative attitudes toward their communication abilities than children who do not stutter (CWNS), and these sentiments become more pronounced over time (Clark et al., 2012; De Nil & Brutten, 1991; Guttormsen et al., 2015; Vanryckeghem et al., 2005). Several studies focusing on temperament have reported increased anger or frustration and greater difficulty regulating emotions or adapting to change among young CWS compared with CWNS per parent report (Anderson et al., 2003; Eggers et al., 2010; Karrass et al., 2006). Although other research, including our own, did not corroborate group differences in temperament between young CWS and CWNS using similar parent-report measures (C. A. Johnson et al., 2021; Kefalianos et al., 2014, 2017; Reilly et al., 2013; Walsh et al., 2019), individual profiles characterized by challenging behaviors should be considered as a potential factor in the development of adverse impact in CWS (Eggers et al., 2021). Higher levels of social anxiety have also been documented in some school-aged CWS (Iverach et al., 2016), becoming more prevalent in adolescents who stutter (Iverach & Rapee, 2014; Mulcahy et al., 2008; Smith et al., 2014). Finally, studies reveal that CWS are at greater risk for bullying by their peers (Blood & Blood, 2004; Langevin & Bortnick, 1998). Blood and Blood (2004) hypothesized that CWS are particularly vulnerable to victimization and bullying due, in part, to their poorer self-ratings of self-esteem and reduced confidence in their communication abilities.
Prior research in CWS thus confirms that many CWS, like adults, experience adverse impact and suggests several factors that may place children at greater risk for its development. We lack a firm grasp, however, of protective factors that may mitigate the development of adverse impact. Craig et al. (2011) lamented, “It is regrettable that little or no emphasis has been placed on research that has investigated factors that protect people from negative outcomes due to their chronic stuttering…” (p. 1486). In the child development literature, protective factors, such as resilience, have been shown to support positive adjustment or coping so that potentially negative outcomes may be avoided (Zolkoski & Bullock, 2012). For children with speech and language disorders, Lyons and Roulstone (2018) suggest that resilience plays a key role in strengths-based treatment approaches that mitigate a communication disorder's adverse impact. The purpose of this study is to explore the relationship between children's resilience, a potentially protective factor, and the adverse impact of stuttering.
Resilience
Resilience encompasses one's ability to persevere in the face of challenging situations, making it a promising protective factor to target in therapy with the goal of helping CWS manage difficult communication situations (Caughter & Dunsmuir, 2017; Druker et al., 2019). Resilience theory focuses on the strengths and supportive elements of a child's environment that promote positive outcomes (A. S. Masten, 2001; Thomlison, 1997). Resilience research has grown exponentially in recent years, expanding from an early focus on at-risk youth facing poverty, abusive situations, family discord, or parental mental illness (e.g., Rutter et al., 1976; Werner, 1971) to applications with different populations such as those suffering from chronic illness (Cal et al., 2015), military/combat-related trauma (McGeary, 2011), or occupational burnout (Hart et al., 2014). Diverse theoretical perspectives of resilience have also evolved over the past five decades. Early research focused on inherent traits possessed by seemingly invulnerable children, which allowed them to persevere despite being in significantly disadvantaged situations (Garmezy et al., 1984; Rutter, 1985; Werner, 1971). Masten then advanced an “ordinary magic” perspective that “resilience is made of ordinary rather than extraordinary processes” (p. 227), meaning that each child has the innate capacity for resilience (A. S. Masten, 2001). More recently, Ungar and colleagues (Ungar, 2004a, 2004b, 2011) shifted away from a child-centered focus toward an ecological view that recognizes children are a part of their family and community and these relationships, along with access to resources, also impact a child's capacity for positive functioning.
Given the diverse perspectives on resilience, it is unsurprising that it has been defined and operationalized in different ways. However, there is consensus in the broader literature that definitions of resilience comprise two essential parts: (a) a stressor be present and (b) a recovery, adaptation, or rebound has occurred (see Table 1 in Schafer, 2022, for an aggregation of resilience definitions by prominent researchers in the field). There is also general agreement that resilience is not simply a trait that you have or do not have (Luthar & Cicchetti, 2000; A. S. Masten et al., 1999); rather, it is a dynamic, malleable construct, changing within an individual over time and shaped or cultivated through intervention and experiences (Alvord & Grados, 2005; Fergus & Zimmerman, 2005). Boyce et al. (2021) present a compelling framework for the development of adversity and resilience implicating interrelations among genes, environment, and developmental stage as key players in a child's capacity for resilience. According to the authors, early environmental exposures to significant trauma or adversity may alter the developing brain and “render a child more susceptible to second or third hits by…psychological stressors later in life” (p. 5). The timing of environmental exposures is a crucial piece to the puzzle, as there are hypothesized critical periods where positive and negative experiences may have the greatest impact on a child's capacity for resilience.
Child attributes associated with greater resilience include social competence, problem-solving skills, critical consciousness or the ability to consider different perspectives, autonomy or self-control, and a sense of purpose or having goals or aspirations (Bernard, 1993, as cited in Zolkoski & Bullock, 2012). However, a family's access to resources such as adequate health/mental health care, stable housing, and economic opportunities, for example, can be more influential on a child's resilience development than individual attributes (Benzies & Mychasiuk, 2009; A. S. Masten & Coatsworth, 1998; Thomlison, 1997; Ungar et al., 2013). In addition, supportive relationships with parents/caregivers are crucial to the development of a child's resilience. A. S. Masten and Coatsworth (1998) suggest that having at least one committed and nurturing adult who sets firm boundaries and expectations was instrumental in helping a child cope with life stressors. Outside of the immediate family, community support can help to nurture a child's resilience. Participation in spiritual organizations or recreational activities, for example, has been associated with greater resilience (Benzies & Mychasiuk, 2009). Finally, healthy, supportive friendships are associated with positive coping (Hartup & Stevens, 1997). Graber et al. (2016) found a positive association between a child's perception of the quality of their friendships and greater resilience. In summary, the development of resilience in a child is nurtured through interactions between personal and environmental factors with supportive caregiving and adequate access to resources (Schafer, 2022).
Resilience and Stuttering
Recognizing that individuals living who stutter are particularly vulnerable to adverse outcomes such as poorer mental health and reduced quality of life, Craig et al. (2011) explored whether higher resilience was associated with healthier psychosocial outcomes in a group of 200 adults who stutter (AWS). They measured resilience indirectly using outcomes from a self-report measure of psychopathology, the Global Severity Index (GSI; Derogatis, 1994), assuming that higher psychopathological scores would be associated with fewer protective factors. AWS identified as being more resilient (having lower scores on the GSI) reported, on average, greater social support, a higher sense of self-efficacy, and better social functioning compared with AWS reporting higher GSI scores.
Similarly, Plexico et al. (2019) examined the role that protective factors play in individuals' self-esteem and overall life satisfaction to gain insight into general adverse impact reported by AWS. In their study, they explored how coping skills, as measured by the Brief COPE (Coping Orientation to Problems Experienced) Inventory, and resilience, as measured by the Connor-Davidson Resilience Scale (CD-RISC; Connor & Davidson, 2003), impacted reports of life satisfaction and self-acceptance in AWS and adults who do not stutter (AWNS). Plexico et al. (2019) found that AWS reported lower overall life satisfaction than AWNS, yet, encouragingly, greater resilience moderated the effect of stuttering status such that AWS with higher resilience scores were more likely to report greater life satisfaction and self-acceptance than AWS with lower resilience. On the other hand, maladaptive coping mechanisms such as substance abuse or disengagement were associated with lower self-acceptance. Findings from these studies in AWS suggest that greater resilience may protect AWS from general adverse impact and is associated with higher quality of life.
Freud and Amir (2020) noted that these two earlier studies focused broadly on resilience and overall mental health or, alternatively, life satisfaction but did not examine the relationship between resilience and stuttering's adverse impact specifically. They hypothesized that AWS with less resilience measured with the CD-RISC would report more frequent/severe stuttering along with greater adverse impact as measured by the Overall Assessment of the Speaker's Experience of Stuttering (OASES; Yaruss & Quesal, 2016). Although a relationship between stuttering frequency and resilience was not confirmed in their sample of 30 AWS, they found a strong negative correlation between resilience, as measured by the CD-RISC and OASES overall scores. Participants reporting higher resilience reported less adverse impact related to their stuttering. Since aspects of resilience can be cultivated/shaped through purposeful therapy (Alvord & Grados, 2005), Freud and Amir proposed that factors promoting healthy resilience be targeted in speech therapy to help mitigate the negative effects that people who stutter may experience.
The relationship between resilience and the adverse impact of stuttering has not been explicitly explored in CWS. However, two recent studies recognized the potential value of resilience in stuttering treatment toward the goal of helping children cope with the negative effects of stuttering. In an exploratory case study with seven school-aged CWS, Caughter and Dunsmuir (2017) examined the role of resilience in an evidence-based 2-week intensive stuttering treatment program that aims to enhance fluency and reduce the adverse impact of stuttering on children and parents (Millard, 2011). Children completed the Resiliency Scales for Children and Adolescents (Prince-Embury, 2006) at seven time points across treatment: a pretherapy baseline, immediately before and after the 2-week intervention, and at four intervals across the remainder of a 1-year interval. Findings showed that over half of the participants experienced increases in resourcefulness and all but one child reported decreases in their vulnerability scores—two integral components of resilience measured by this scale. Encouragingly, children in the study also showed clinically meaningful improvement in OASES scores, suggesting that the negative impact of stuttering had lessened over the course of the treatment. A thematic analysis of children's interviews confirmed these positive changes. Children in the study reported being better able to cope with negative communication experiences, relying more on support networks (i.e., peers, parents, and teachers), and were more willing to speak in challenging communicative situations than before treatment. It is important to note that this stuttering treatment program did not specifically target resilience; nevertheless, the positive preliminary outcomes from this study suggest that resilience in CWS can be cultivated in different ways and provide some support for its inclusion in holistic stuttering treatment approaches.
Another recent study examined the potential benefits of integrating a resilience component into a stuttering therapy program for preschoolers (Druker et al., 2019). CWS–parent dyads were randomly divided into an experimental group that received stuttering therapy combined with a parent-led resilience component and a control group that received stuttering therapy alone. Parents of children in the experimental group received a 30-min training session scheduled within the first 3 weeks of the 12-week program on how to foster resilience in their child and were asked to journal how they implemented these principles in the weeks that followed. The percentage of syllables stuttered decreased by a similar degree in both groups; however, the experimental group saw a positive shift in parenting practice scores, as measured by the Parenting and Family Adjustment Scales (Sanders et al., 2014). Druker et al. (2019) also found a significant decrease in behavioral and emotional problems and an increase in resilience characteristics using an exploratory measure designed for the preschool population, the Curtin Early Childhood Stuttering Resilience Scale. Although adverse impact related to stuttering was not measured, these results suggest that intentional parent training may facilitate positive adjustment and better coping skills in their CWS—outcomes of greater resilience.
This Study
Resilience comprises personal attributes (e.g., self-efficacy and problem-solving skills) and external/environmental factors (e.g., one's experiences and level of community support). Fostering greater resilience in CWS to help them manage difficult communication situations is a promising therapeutic goal, yet there are scant data on the relationship between resilience and the adverse impact of stuttering to offer empirical support for such an approach. The aim of this study is to investigate the relationship between resilience and stuttering's adverse impact in children across the developmental spectrum. We hypothesize that children with greater resilience will report experiencing less adverse impact of stuttering. An additional aim of this study is to assess the alignment of child- and parent-report measures of resilience. Multi-informant approaches incorporate valuable perspectives from children and parents that uniquely contribute to overall patterns of findings (De Los Reyes et al., 2015; Ungar, 2010). To address our aims, we use established clinical measures of stuttering's adverse impact with the age-appropriate version of the OASES and resilience with the Child and Youth Resilience Measure–Revised (CYRM-R; Resilience Research Centre, 2018). We also consider aspects of a child's behavioral development using a parent-report checklist (Yaruss & Reardon-Reeves, 2017), because individual behavioral profiles could be an important factor to consider in the development of adverse impact in a child who stutters. Research into the factors influencing the development of adverse impact in CWS will provide a deeper understanding of how children experience stuttering and advance treatment approaches to mitigate its adverse effects.
Method
The data presented in this study were collected as part of a larger ongoing project in the Developmental Speech Lab at Michigan State University exploring the development of stuttering and its adverse impact on children. OASES data presented in this study have been reported for many of these participants in a separate study (Tichenor et al., 2022). This research is approved by the institutional review board at Michigan State University (STUDY# 00001704).
Participants and Procedure
Survey data for the study were collected from 148 CWS aged 5–18 years (M = 10.14 years; SD = 3.41 years) and their primary caregiver (henceforth, parent). Families were recruited to the project using a combination of convenience, purposive, and snowball sampling. We directly contacted speech-language pathologists (SLPs) employed in schools, outpatient clinics, university clinics, and specialty stuttering clinics nationwide to disseminate information about the project to parents of CWS. We intentionally targeted schools and clinics in urban and suburban areas in an effort to enhance the diversity of our participant pool. We recruited via word of mouth and through forums and social media outlets for SLPs working in the schools and/or with clients who stutter. We also disseminated information about the study to faculty specializing in stuttering/fluency disorders as well as national and international stuttering support and interest groups. Parties contacted through these various methods were encouraged to share study information with other prospective families. Due to these sampling methods, the total number of parents of children and adults who were contacted cannot be determined.
The surveys were presented online using Qualtrics. Families interested in participating completed an initial screening survey to affirm that their child stuttered and to provide their child's age. Families of eligible children—those who stuttered and were between the ages of 5 and 18 years—were then e-mailed unique links to a series of parent and age-appropriate child surveys. Informed consent was obtained from parents of CWS or CWS who were 18 years of age. Assent was obtained for CWS over the age of 8 years. Measures related to this study were collected in one child survey and two parents surveys; remuneration was provided for each completed survey.
Survey Measures
Background Information
Parents of CWS provided demographic data and information about their child's developmental history. All parents confirmed that their child stuttered, and 142 parents (~96%) reported that their child had been diagnosed by an SLP or other professional. Parents of 139 CWS (93.4%) indicated their child had received speech therapy for stuttering, and 64 (43.2%) indicated that their child had a concomitant speech and/or language deficit. Other demographic and developmental history information reported by parents for their child is provided in Table 1.
Table 1.
Child demographic data.
| Demographic variable (N = 148) | Value |
|---|---|
| Age | |
| M (SD) | 10.1 years (3.4 years) |
| Range; min–max | 13; 5–18 years |
| Sex | |
| Female | 35 (23.6%) |
| Male | 113 (76.4%) |
| Race | |
| Asian | 3 (2.0%) |
| Black or African American | 10 (6.8%) |
| American Indian/Alaskan Native | 2 (1.4%) |
| White | 119 (80.4%) |
| Mixed/other | 14 (9.5%) |
| Ethnicity | |
| Hispanic/Latino/a | 9 (6.1%) |
| Not Hispanic/Latino/a | 133 (89.9%) |
| Prefer not to say/missing data | 6 (4.1%) |
| Family income | |
| Under $25,000 | 3 (2.0%) |
| $25,000–$49,000 | 11 (7.4%) |
| $50,000–$74,000 | 18 (12.2%) |
| $75,000–$99,000 | 23 (15.5%) |
| $100,000–$124,000 | 23 (15.5%) |
| $125,000–$149,000 | 14 (9.5%) |
| $150,000–$174,000 | 4 (2.7%) |
| $175,000–$199,000 | 7 (4.7%) |
| $200,000 or greater | 30 (20.3%) |
| Prefer not to say/missing data | 15 (10.1%) |
| Country/continent of residency | |
| United States | 147 (99.3%) |
| North America (not United States) | 1 (0.7%) |
| Neurodevelopmental disorder | |
| No diagnosis | 112 (75.7%) |
| Attention-deficit/hyperactivity disorder (ADHD) | 21 (14.2%) |
| Autism | 3 (2.0%) |
| Multiple (e.g., ADHD and OCD) | 7 (4.7%) |
| Other (e.g., learning, sensory, and unspecified) | 2 (1.4%) |
| Prefer not to say/missing data | 3 (2.0) |
| Psychiatric disorder | |
| No diagnosis | 130 (87.8%) |
| Anxiety and/or depression | 15 (10.1%) |
| Unspecified psychiatric disorder | 3 (2.0%) |
Note. OCD = obsessive-compulsive disorder.
Behavioral Checklist
Recognizing that behavioral profiles could impact the development of stuttering's adverse impact, parents also completed a developmental behavioral checklist to document the frequency that their child displayed these 14 behaviors: inattentiveness, hyperactivity, nervousness, sensitivity, excitability, frustration, strong fears, excessive neatness, excessive shyness, difficulty regulating emotions, lack of confidence, competitiveness, perfectionism, and difficulty with change/transition (Yaruss & Reardon-Reeves, 2017). This checklist is a parent-report measure that is part of an assessment battery that SLPs can use to individualize stuttering treatment for families seeking services (Yaruss & Reardon-Reeves, 2017). Parents respond to the 14 behaviors using a 3-point. scale (1 = often, 2 = sometimes, 3 = never); therefore, a higher cumulative score indicates a less often occurrence of these behaviors or healthier behavioral development.
OASES
The adverse impact of stuttering was measured using the age-appropriate version of the OASES. The OASES is designed to capture the experience of stuttering including its potential adverse impact. Children aged 7–12 years completed the OASES–School-Age (OASES-S; Yaruss & Quesal, 2016). The OASES-S is most often completed by the CWS with guidance from their SLP as needed. In this case, parents were asked to read items to their child (particularly for younger participants) and/or help their child interpret directions or questions on the assessments. Parents were instructed not to answer for their child or influence their responses. Children aged 13–18 years took the OASES–Teen (OASES-T, OASES-S; Yaruss & Quesal, 2016). Twenty-one parents of children aged 5–6 years took the OASES–Early Childhood–Parent (OASES-EC-P; Yaruss & Yaruss, 2021). The OASES-EC-P is a newer version designed to assess the adverse impact of stuttering in young children aged 3–6 years and is completed by the parent of the child who stutters. All versions of the OASES include four sections: (a) general perspectives/knowledge about stuttering; (b) affective, behavioral, and cognitive reactions to stuttering; (c) functional communication in daily situations; and (d) impact of stuttering on the individual's quality of life. Each OASES section includes questions requiring a 5-point Likert scale response. Impact scores are computed for each of the four sections by dividing the total number of points in each section by the total number of items completed in each section; if there are missing data points, the average is taken over the questions respondents answered. A total score is computed similarly by summing points over the entire measure and dividing them by the number of total items completed. OASES scores are interpreted on a 5-point scale: mild impact (1.00–1.49), mild/moderate impact (1.50–2.24), moderate impact (2.25–2.99), moderate/severe impact (3.00–3.74), and severe impact (3.75–5.00). In this study, the OASES total score was measured as a latent variable (LV; otherwise known as confirmatory factor analysis; Jöreskog, 1969) using the mean scores from each of the four OASES sections as items of a single factor. The OASES total LV is comparable with the OASES total (overall mean of all items/sections) score in terms of what their validity and what they are measuring; however, random measurement error that can affect the mean scores of raw data is removed from the LV, rendering the OASES total LV perfectly reliable. Thus, the OASES total LV allows for more precise and comprehensive measurement than the OASES total mean score, resulting in less biased estimates of R 2 and regression coefficients.
CYRM-R
The CYRM-R (Jefferies et al., 2019; Resilience Research Centre, 2018) adopts Ungar's (2008) social–ecological resilience framework that maintains resilience “is both the capacity of individuals to navigate their way to…resources, including opportunities to experience feelings of well-being, and a condition of the individual's family, community, and culture…” (p. 225). The CYRM is a measure of resilience comprising two subscales, one assessing a child's caregiver resilience (henceforth, external resilience for clarity) that probes the child's perspectives of their family dynamics and access to basic resources and one subscale assessing personal resilience that probes the child's perspectives on their personal attributes and the connections they have to their community (Jefferies et al., 2019; Resilience Research Centre, 2019).
CWS aged 5–9 years took the CYRM Child version, and children aged 10 years and older took the CYRM Youth version. Parents of 132 children completed the Person Most Knowledgeable version of the CYRM (PMK-CYRM) that assesses a child's external and personal resilience through the perspective of an informant familiar with the child and environment, for example, a parent or counselor. The CYRM Child, CYRM Youth and PMK-CYRM each include 17 items that children/parents indicated their level of agreement using a 5-point Likert scale. The CYRM Child version includes smiley faces to help children indicate their level of agreement on the 5-point Likert scale. A total score for all versions of the CYRM is obtained by summing over the 17 items, resulting in a minimum score of 17 and a maximum score of 85. A higher total score indicates greater resilience. In this study, the 17 questions comprising the CYRM were used as items in the CYRM total LV. The seven CYRM external resilience items were used as items measuring the external CYRM LV, and the remaining 10 CYRM personal items were used as items measuring the personal CYRM LV. If a respondent skipped an item, the subscale belonging to that item and a total score would not be computed for that participant.
The CYRM-R was developed with samples from populations around the world. However, the authors caution against comparing results to other populations stating, “resilience is likely to vary between contexts, and so any thresholds would similarly vary. For this reason, our recommendation is to instead contrast high and low scorers within your sample” (p. 14).
Statistical Analysis
Data were analyzed using descriptive and inferential statistics. To assess the relationship between resilience and stuttering's adverse impact (Aim 1), a regression model with LVs was estimated in a structural equation modeling framework (Bollen, 2014; Kline, 2016). In Model 1, adverse impact related to stuttering (OASES total LV) was modeled as a function of the focal resilience predictors: the child-report version (Child or Youth) of the CYRM total LV and controlled for child age and behavioral development (behavioral checklist score). Two additional linear models were also estimated to model adverse impact (OASES total LV) as a function of external (Model 2) and personal (Model 3) resilience using the CYRM external LV and personal LV subscale measures. The three models were estimated again with the addition of a squared term for the CYRM LVs (A. Klein & Moosbrugger, 2000). Thus, the three models tested for a (nonlinear) relationship between the CYRM variables and OASES outcome. Figure 1 is a depiction of the linear version of the structural equation model using the CYRM total LV. Mplus Version 8.7 was used to estimate the models. Note that we combined the three versions of the OASES (EC-P, S, and T) and two versions of the CYRM (Child and Youth) in the models to reduce the number of statistical tests and increase statistical power. This is justifiable as the versions of these measures are directly comparable. The behavioral checklist was included in all three models, because it was associated with both the outcome (OASES total LV) and the focal predictors (CYRM LVs). Bivariate regression estimates indicated that the following behavioral characteristics included in the checklist were significantly associated with the OASES total LV: nervousness, sensitivity, frustration, strong fears, excessive neatness, excessive shyness, difficulty regulating emotions, lack of confidence, and perfectionism (see Table 2). We included age and behavioral checklist score as covariates in each model to control for their potential effect on the relationship between resilience and adverse impact. Finally, we assessed the alignment of child-report (CYRM Child or Youth) and parent-report (PMK-CYRM) measures of resilience (Aim 2) by estimating three Pearson product–moment correlations of child/parent report external resilience, child/parent report personal resilience, and child/parent total resilience ratings.
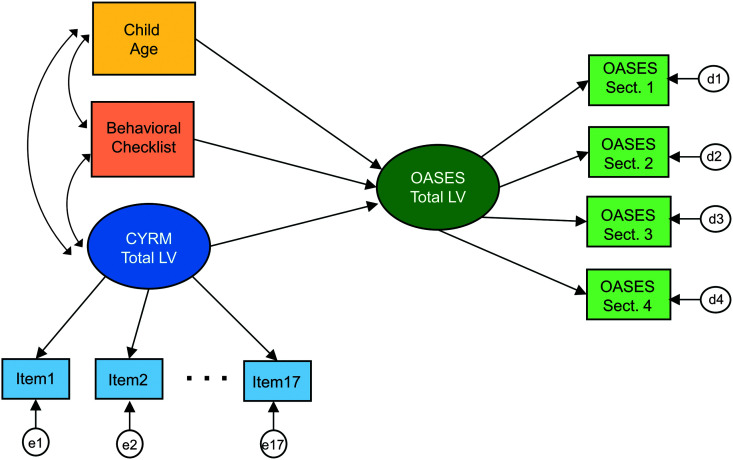
Figure 1.
Schematic diagram of the structural equation modeling framework used in the statistical analysis. The ovals represent latent (unobserved) variables, and the rectangles represent manifest (observed) variables. The e1–e17 terms represent measurement errors for the 17 CYRM-R items. The d1–d4 terms represent measurement errors for the four OASES sections. Curved, two-headed arrows represent covariances. Independent variables are allowed to covary as is standard in multiple variable regression. Straight, single-headed arrows represent direct paths (regression coefficients). OASES = Overall Assessment of the Speaker's Experience of Stuttering; CYRM = Child Youth and Resilience Measure; LV = latent variable.
Table 2.
Bivariate associations of behavioral checklist items with the Overall Assessment of the Speaker's Experience of Stuttering latent variable.
| Behaviors | Estimate | Standardized estimate | p value |
|---|---|---|---|
| Inattentiveness | −0.14 | −0.13 | .119 |
| Hyperactivity | 0.05 | 0.05 | .530 |
| Nervousness | −0.33 | −0.32 | < .001** |
| Sensitivity | −0.22 | −0.20 | .020* |
| Excitability | 0.04 | 0.04 | .649 |
| Frustration | −0.48 | −0.38 | < .001** |
| Strong fears | −0.30 | −0.29 | < .001** |
| Excessive neatness | −0.24 | −0.17 | .044* |
| Excessive shyness | −0.31 | −0.27 | .001** |
| Difficulty regulating emotions | −0.17 | −0.18 | .037* |
| Lack of confidence | −0.51 | −0.45 | < .001** |
| Competitiveness | −0.12 | −0.14 | .118 |
| Perfectionism | −0.19 | −0.20 | .021* |
| Difficulty with change/transition | −0.13 | −0.14 | .114 |
p < .05.
p < .001.
The CYRM-R and the OASES are established assessments of resilience and the adverse impact of stuttering, respectively. Given that these assessments were administered to parents and CWS in an online/survey format, we computed Cronbach's alpha for each section of the CYRM-R and the OASES to document internal consistency (see Supplemental Material S1). All sections exceeded .70 except for OASES Section 1 (General Information) of the OASES-EC-P (.39) and the external subscale of the PMK-CYRM (.57), suggesting that these sections examined more than one underlying construct. Mean scores based on raw data can be affected by measurement error and multidimensionality. This concern, however, is mitigated in this study, as we used LVs in the linear regression analysis rather than mean scores of the raw data to account for potential measurement error and multidimensionality.
Results
Descriptive Statistics
The observed range for this sample on the behavioral checklist was 19–42 with a mean of 30.5 and an SD of 4.62. Table 3 provides the mean, standard deviation, and range of OASES total scores and scores for each of the four sections for the OASES-EC-P, OASES-S, and OASES-T. The average total score on the OASES-EC-P version was 2.02, indicating a mild/moderate impact rating. The average total score for children completing the OASES-S was 2.17, also indicating a mild/moderate impact impact rating. The average total score for older children completing the OASES-T was 2.42, indicating a moderate impact rating.
Table 3.
Descriptive statistics for the three versions of the Overall Assessment of the Speaker's Experience of Stuttering (OASES).
| Measure | OASES–Early Childhood–Parent (n = 21) |
OASES–School-Age (n = 89) |
OASES–Teen (n = 38) |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| I | II | III | IV | Total | I | II | III | IV | Total | I | II | III | IV | Total | |
| M | 2.52 | 1.90 | 2.18 | 1.80 | 2.02 | 2.63 | 2.20 | 2.02 | 1.59 | 2.17 | 2.63 | 2.54 | 2.55 | 1.99 | 2.42 |
| SD | 0.36 | 0.62 | 0.79 | 0.82 | 0.57 | 0.49 | 0.80 | 0.72 | 0.59 | 0.58 | 0.46 | 0.69 | 0.61 | 0.71 | 0.53 |
| Range | 1.33 | 2.25 | 2.57 | 3.00 | 2.03 | 2.43 | 3.50 | 3.47 | 3.30 | 3.10 | 2.20 | 2.64 | 2.65 | 2.45 | 1.84 |
Note. I = General Information section; II = Reactions to Stuttering section; III = Communication in Daily Situations section; IV = Quality of Life section.
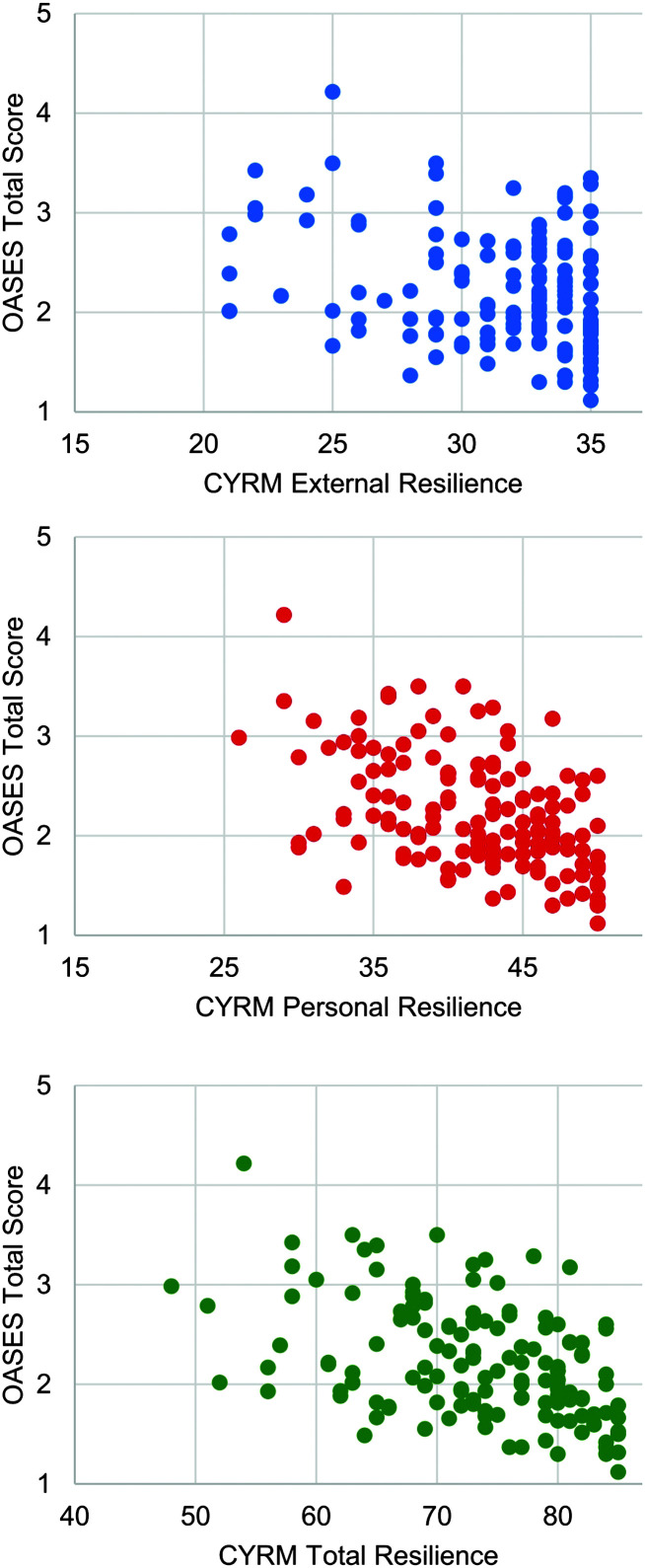
Table 4 provides means, standard deviations, and ranges for total CYRM scores as well as scores for the external and personal subscales of the Child, Youth, and PMK versions. On average, parents (M = 76.25, SD = 6.43) tended to report higher resilience ratings than children (M = 73.43, SD = 8.29). This difference, 2.81, 95% CI [1.48, 4.14], was statistically significant, t(131) = 4.18, p < .001. A participant's external, personal, and total resilience was plotted against their OASES total score in Figure 2 to visualize the individual data points.
Table 4.
Descriptive statistics for the three versions of the Child and Youth Resilience Measure (CYRM).
| Measure | CYRM Child |
CYRM Youth |
PMK-CYRM |
||||||
|---|---|---|---|---|---|---|---|---|---|
| External | Internal | Total | External | Internal | Total | External | Internal | Total | |
| M | 31.26 | 41.09 | 72.35 | 31.73 | 42.60 | 74.28 | 33.32 | 42.66 | 75.99 |
| SD | 3.54 | 5.98 | 8.62 | 3.89 | 5.50 | 8.10 | 6.80 | 5.71 | 1.86 |
| Range | 14 | 24 | 37 | 34 | 21 | 14 | 28 | 25 | 8 |
Note. PMK = Person Most Knowledgeable.
Figure 2.
Individual data points showing each child's resilience scores plotted against their average Overall Assessment of the Speaker's Experience of Stuttering (OASES) total score. The top graph presents external resilience scores; the middle graph, personal resilience scores; and the bottom graph, total resilience scores from the Child and Youth Resilience Measure.
Linear Regression With LVs
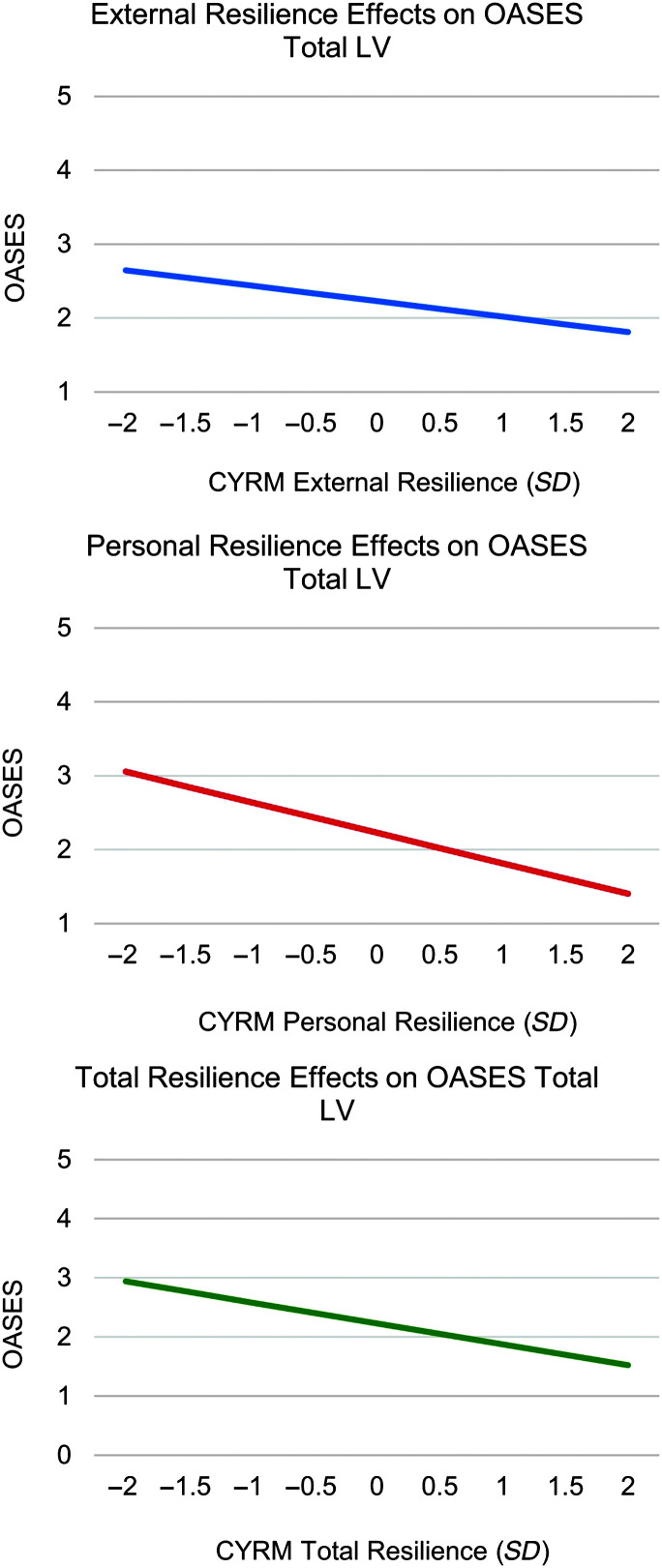
Table 5 provides the results from the three structural equation models assessing the effects of external, personal, and total resilience on the OASES total LV, respectively. The effects of external, personal, and total resilience were each significantly linearly associated with the adverse impact of stuttering as measured by the OASES total LV. We used the estimates in Table 5 for effect sizes that are comparable with Cohen's d estimates. Standard interpretation of these effect sizes—0.20 = small effect, 0.50 = moderate effect, and 0.80 = large effect—applied. Model 1 revealed that a one-unit increase in external resilience was associated with a 0.57 decline in adverse impact (p < .001), indicating a moderate effect size (see Figure 3, top graph). The fully standardized effect was −0.42, meaning that a 1 SD increase on the external resilience measure was associated with a decline of 0.42 SDs in the OASES total LV. Model 2 revealed the strongest linear association between personal resilience and adverse impact, where a one-unit increase in personal resilience was associated with a decline of 1.47 in the OASES total LV (p = .002), also representing a large effect size (see Figure 3, middle graph). The standardized effect was −0.59. Model 3 confirmed a one-unit increase in total resilience being associated with a decline of 1.14 in adverse impact (p = .001), indicating a large effect (see Figure 3, bottom graph). The standardized effect was −0.50. In all three models, the effects of age and behavioral checklist score were significant, representing small to moderate effect sizes (see Table 5). Older age and more frequent displays of the checklist behaviors predicted higher OASES LV or greater impact. There were no nonlinear relationships between resilience measures and the OASES as indicated by quadratic effects that were not statistically significant (p > .10).
Table 5.
Outcomes from the three linear regression models.
| Model | Predictors | OASES |
||
|---|---|---|---|---|
| Estimate | Standardized estimate | p value | ||
| Model 1 | Age | 0.06 | 0.32 | < .001 |
| N = 148 | Behav checklist | −0.06 | −0.39 | < .001 |
| R 2 = .51 | CYRM external | −0.57 | −0.42 | < .001 |
| Model 2 | Age | 0.07 | 0.33 | < .001 |
| N = 148 | Behav checklist | −0.03 | −0.22 | .004 |
| R 2 = .55 | CYRM personal | −1.47 | −0.59 | .002 |
| Model 3 | Age | 0.07 | 0.33 | < .001 |
| N = 148 | Behav checklist | −0.04 | −0.30 | < .001 |
| R 2 = .49 | CYRM total | −1.14 | −0.50 | .001 |
Note. OASES = Overall Assessment of the Speaker's Experience of Stuttering; Behav = behavioral; CYRM = Child and Youth Resilience Measure.
Figure 3.
These graphs depict the results from the three structural equation models assessing the effects of resilience on the adverse impact of stuttering. The top graph presents the significant linear relationship between the Child and Youth Resilience Measure (CYRM) external latent variable (LV) and the Overall Assessment of the Speaker's Experience of Stuttering (OASES) total LV, the middle graph presents the significant linear relationship between the CYRM personal LV and the OASES total LV, and the bottom graph presents the significant linear relationship between the CYRM total LV and the OASES total LV.
Correlations
Pearson product–moment correlations between the PMK-CYRM-R external, personal, and total scores and the CYRM-R Child and Youth external, personal, and total scores were estimated. Parent-report levels of child total resilience moderately correlated with younger children's resilience total score reports, r(65) = .57, p < .001, but to a lesser degree with older children and adolescents' total scores, r(67) = .34, p = .005. Similarly, parent PMK-CYRM-R personal scores were also moderately correlated with younger children's personal resilience, r(65) = .62, p < .001, but to a lesser degree with older children's reports, r(71) = .43, p < .001. The external resilience score correlation between younger children and parents was weak, r(68) = .35, p = .004, and was not statistically significant between parents and older children, r(69) = .23, p = .06.
Discussion
The broader scope of our research is to identify factors that place children at greater risk for developing adverse impact of stuttering and, in parallel, protective factors that mitigate this risk. This study examined the relationship between resilience, a protective factor, and stuttering's adverse impact in CWS. Resilience resides at the intersection between external factors, such as family support and access to resources and personal attributes, such as self-esteem and sense of autonomy, making it a comprehensive protective factor to explore. Prior studies in AWS confirmed significant relationships between resilience and adverse impact. Craig et al. (2011) reported that AWS possessing a greater number of resilience-related features (greater social support and levels of self-efficacy and social functioning) reported experiencing less overall adversity. Lower self-acceptance in AWS has been associated with lower levels of resilience (Plexico et al., 2019), whereas Freud and Amir (2020) confirmed that participants with higher resilience levels were more likely to report lower levels of adverse impact specific to stuttering. We also found a significant relationship between resilience and stuttering's adverse impact. Greater external, personal, and total resilience significantly predicted less adverse impact of stuttering in CWS. The covariates age and behavioral checklist scores were each significant in the three statistical models, suggesting that older children experience greater adverse impact from stuttering than younger children, a finding confirmed by other studies in children and adolescents (Gunn et al., 2014; Smith et al., 2014), and that more frequent displays of certain behaviors were also associated with greater adverse impact.
The discussion examines the external and personal factors that contribute to a child's resilience and provides practical suggestions for how clinicians working with CWS can nurture resilience in children experiencing significant adverse impact from their stuttering. Fostering greater resilience, particularly in individuals at risk for adversity, has long been considered an evidence-based psychotherapy approach. In their meta-analysis, Joyce et al. (2018) found that resilience-based interventions combining cognitive behavioral therapy (CBT) and mindfulness techniques had a significant positive impact on participants' baseline resilience. Several studies have discussed the value of integrating aspects of CBT or mindfulness into stuttering treatment (see, e.g., Boyle, 2011; Harley, 2018; Kelman & Wheeler, 2015; Plexico & Sandage, 2011).
External Resilience Factors
The CYRM-R probes external resilience by asking children about family dynamics, for example, how safe or supported they are by their parent/caregiver. It also probes access to basic resources such as food. Model 1 revealed that greater external resilience predicted less adverse impact of stuttering, yielding a moderate effect size. A robust literature suggests that having at least one stable, positive relationship with an adult is paramount to the development of a child's external resilience (Ginsburg & Jablow, 2020; A. S. Masten & Coatsworth, 1998; Ungar et al., 2013). SLPs can strive to build collaborative and trusting relationships with CWS by listening to and validating their feelings, showing warmth and concern (DiGiuseppe et al., 1996), and being knowledgeable about stuttering and its treatment (Plexico et al., 2010). Establishing a therapeutic alliance with children can foster external resilience and successful treatment outcomes (DiGiuseppe et al., 1996). SLPs can also support positive child–parent relationships by providing guidance on how parents can support their child's communication development. Ginsburg and Jablow (2020) advanced parent-driven building blocks of external resilience to support children in navigating life's challenges. They espouse the importance of parental support in the form of unconditional love and acceptance paired with high expectations and standards. Although these two building blocks seem in direct conflict, Ginsburg and Jablow clarify that expectations and standards should not be achievement or performance based but, rather, based on character to hold “…young people accountable to being their best selves” (p. 5). This is critical to keep in mind when clinicians counsel families about the best ways they can support their child who stutters. Parents can reinforce resilience in communicative situations by focusing their attention on the message their child is intending to communicate. A recent study seeking input from CWS about the best ways that their parents could support them revealed that most children simply wanted their family to be better listeners and to treat them more naturally at home (Iimura et al., 2021).
An additional building block of resilience that parents can nurture is healthy thought patterns and responses to stressful situations and challenges. The Reaching In Reaching Out (RIRO) program is an evidence-based therapy program designed to cultivate greater resilience in children from birth to 8 years of age. A key component of RIRO is educating parents and other professionals who engage with young children about techniques to reframe their own potentially negative thought processes and to model healthy responses to challenging interactions with their children (Pearson & Hall, 2006). Recognizing that CWS are vulnerable to adversity, Caughter and Crofts (2018) adopted the RIRO framework in a focus article exploring the own potential benefits of incorporating aspects of this approach into stuttering therapy toward the goal of helping children build resilience. They advocated for parents of CWS to learn how to respond effectively to daily challenges in their own lives and to identify and reframe negative thought patterns so they can model and encourage these healthy behaviors in their child. Clinical trials will help establish therapy approaches such as RIRO as an evidence-based aspect of stuttering therapy approaches.
Last, a family's access to material resources such as food, heath/mental health care, or stable housing can profoundly impact the development of a child's external resilience (Benzies & Mychasiuk, 2009; A. S. Masten & Coatsworth, 1998; Thomlison, 1997; Ungar et al., 2013). Potock (2017) provides valuable suggestions for SLPs to check in with children and families to screen for food insecurities and help them access this basic resource. Trauma or significant adverse experiences such as those captured in the Pediatrics Adverse Childhood Experiences and Related Life Events Screener (Thakur et al., 2020) may inevitably arise that exceed an SLP's scope of practice. However, SLPs can still advocate for children and families and foster greater external resilience by connecting them with school counselors, social workers, or other professionals. It is important to keep in mind that SLPs are mandated reporters of child abuse—physical, sexual, and neglect—in most U.S. states (H. Johnson, 2018). H. Johnson (2018) discusses the barriers leading to the underreporting of abuse and how SLPs can advocate for children on their caseloads and educate themselves by accessing a fact sheet delineating types of child abuse along with their signs and symptoms from https://www.childwelfare.gov/pubs/factsheets/whatiscan/.
Personal Resilience Factors
The CYRM-R personal resilience scale probes personal attributes and goals (e.g., development of life skills, perceived value of education) and connections that a child has to their community (e.g., is supported by friends, has a sense of belonging). The results of Model 2 revealed the strongest association between personal resilience and adverse impact of stuttering, indicating a large effect size. Although many personal factors are likely to play a role in the development of resilience, we focus on those factors consistently cited in the literature (Fergus & Zimmerman, 2005; Schafer, 2022; Zolkoski & Bullock, 2012) and targeted by the CYRM-R.
The first is self-efficacy or autonomy. Children who feel empowered to make key life decisions are more likely to be resilient (Sanders et al., 2015). Clinicians can support self-efficacy in home and school environments by encouraging parents to step back and allow their child to become the “expert” in their speech (Cook & Botterill, 2005) and by guiding teachers to seek children's input on how they would like to be supported in the classroom (Cozart & Wilson, 2022). Clinicians can also support greater self-efficacy and autonomy by involving the child in collaborative goal setting. Cooke and Millard (2018) conducted a study with 18 CWS who were currently receiving or waiting to receive speech therapy for stuttering to learn what they considered to be the most important outcomes from their therapy. Diverse themes emerged from their study, ranging from affective changes (e.g., feeling more comfortable and independent) to behavioral changes (e.g., having greater fluency and communicating more easily). The range in this sample of children's therapy goals tells us that what constitutes an important goal for one child may be entirely different from their same-age peer, thus emphasizing the importance of seeking a child's input. Furthermore, Alvord and Grados (2005) extol the importance of getting input from the child and involving them in therapy decisions, which not only affords them greater agency but also promotes “buy-in.” “By generating their own ideas, children receive positive feedback, remember their ideas better, and feel empowered” (p. 242).
The second factor related to greater personal resilience is problem-solving skills. Alvord and Grados (2005) maintain that resilience can be strengthened by teaching children problem-solving skills to “identify controllable and uncontrollable circumstances and adversities” (p. 241). Teaching problem-solving strategies in speech therapy to handle a communication breakdown or address stuttering issues that are troublesome to a child may ultimately help that child build personal resilience. For example, over half of school-aged and adolescent CWS report being teased or bullied about their stuttering (Blood & Blood, 2004; Erickson & Block, 2013; Langevin & Bortnick, 1998). Clinicians can explore assertive responses to teasing and bullying with a CWS and practice role-playing adverse situations they have faced or are likely to encounter (Yaruss et al., 2018). Clinicians can also help children navigate situations that exacerbate their stuttering.
Finally, having social competency skills to connect with peers and, in parallel, having healthy friendships or belonging to a community are associated with greater resilience (Fergus & Zimmerman, 2005; C. L. Masten et al., 2012; Ungar et al., 2013). As children become adolescents, they often spend more time with peers than parents. This shift in relationship dynamics is particularly relevant to resilience as positive friendships are predictive of higher levels of resilience in children and adolescents (Graber et al., 2016). Graber et al. (2016) suggested that “close friendships are a nexus between resilience processes of support, individual capacities, and interactions with the social environment” (p. 351). SLPs can support this constituent of resilience by connecting CWS and families to stuttering organizations for youth, such as The Stuttering Association for the Young (https://www.say.org) and FRIENDS: The National Association for Young People Who Stutter (https://www.friendswhostutter.org/), that provide education, advocacy, and, most critically, connection to a caring, supportive community. Overnight or day camps or group therapy with other CWS are also valuable resilience-building sources, as they promote positive communicative experiences to help CWS build confidence as communicators and cultivate opportunities for CWS to connect with peers who may be experiencing similar challenges (Byrd et al., 2016; Herring et al., 2022).
Children may possess proclivities, allowing them to be more (or less) resilient. Lower behavioral checklist scores (more frequent occurrences of behaviors such as nervousness, frustration, or strong fears) were associated with less resilience and greater adverse impact. The bivariate analysis confirmed that more frequent displays of certain characteristics, most notably nervousness, frustration, strong fears, excessive shyness, and a lack of confidence, were significantly associated with a higher OASES total LV. As we suggested in the introduction, behavioral characteristics, either alone or in combination with other characteristics, may put a child at greater risk for experiencing adverse impact related to stuttering. Nevertheless, the behavioral checklist in all three of the predictive models ultimately accounted for minimal variance in OASES scores. We suggest that administering a behavioral checklist to parents of CWS may yield valuable insight into a child's behavioral profile, allowing clinicians to personalize therapy approaches to meet the unique needs of that child.
Multi-Informant Perspectives on Resilience in CWS
We utilized child-report measures of resilience in our structural equations to evaluate the relationship between a child's perception of their resilience and their adverse impact. We were also interested in assessing resilience comprehensively using a multi-informant approach and to explore the degree that children's and their parents' perceptions of resilience aligned. Overall, we found higher correlations between the dyads for measures of personal resilience compared with external resilience. We also documented stronger correlations between young children's ratings and parents' ratings and weaker correlations between older children's and adolescents' and parents' ratings. This may be attributed, in part, to younger children receiving greater parental support to complete the CYRM, yet no correlation exceeded a “moderate” status, suggesting that dyads generally adhered to our direction to parents not to answer for their child. It is not surprising that older children's and adolescents' views on resilience did not strongly correlate with their parents'. Inconsistencies dubbed “informant discrepancies” between parents' and adolescents' ratings are commonly reported in the literature, for example, on measures probing family dynamics, communication, and parenting practices (De Los Reyes, 2011; De Los Reyes et al., 2019; Stuart & Jose, 2012). De Los Reyes (2011) argues that rather than attempting to discern which informant is necessarily “accurate,” a nearly impossible task, researchers should instead embrace these discrepancies as a valuable window into complex child–parent relationships. We will continue to explore data collected using a multi-informant approach in a forthcoming study from our lab that considers parent and child perspectives on stuttering severity across different communicative situations and on stuttering's adverse impact on the child and family to gain greater perspective on how stuttering influences family dynamics.
Limitations and Future Directions
The development of adverse impact in CWS is complex, and we expect to find many factors, both risk and protective, whose interactions influence the degree of adverse impact experienced by an individual child who stutters. This study contributed a key piece of this puzzle by establishing that greater resilience is predictive of less adverse impact of stuttering in CWS. However, we acknowledge that we are only presenting a snapshot of each child at a static point in time, a narrow view. Clearly, a child's capacity for resilience unfolds over time and is shaped by life events and the rich interactions between a child and their environment. Moreover, resilience, by necessity of its definition, requires that an individual experience some degree of stress or adversity. Many adults who struggled with stuttering and its adverse impact in their youth find themselves more resilient adults; now, they are on the “other side” of difficulties experienced in childhood. A thoughtful study captured this sentiment by exploring the potential benefits of stuttering reported by AWS (Boyle et al., 2019). Themes emerged that encompassed personal benefits, such as individuals feeling more courageous because of their stuttering, relationship benefits, such as having greater empathy for others, and gaining a unique perspective on life. On the other hand, some AWS bear a lifelong imprint from the difficulties that they experienced as youth and continue to be adversely impacted by their stuttering. Boyle and colleagues acknowledged that it was not clear whether benefits reported by AWS emerged as a function of personal growth having lived through difficult experiences as a person who stutters, or alternatively, whether inherent differences in an individual empowered them to find meaning through difficult lived experiences. Longitudinal data on adverse impact in CWS and on the risk and protective factors that influence its development are needed to gain a richer understanding of these complex underlying dynamics.
We endeavored to collect survey data from as heterogenous a sample as possible by targeting families living in urban, rural, and suburban areas across the United States. Our final sample revealed that our families represented a higher, on average, household income, a common metric of socioeconomic (SES) status (http://www.apa.org/pi/ses/resources/class/measuring-status/). Table 1 reveals that approximately 32 families out of the 133 families, or 24%, reported household income at or below 75 k. The median household income in the United States is approximately 71 k (census.gov). Families from a higher SES may have greater access to resources which may, in turn, affect a child's overall resilience (Fergus & Zimmerman, 2005; Ungar, 2008). Children in our sample may have higher, on average, resilience compared with the population at large, and we may have underestimated the relationship between resilience and stuttering's adverse impact in our statistical models.
Finally, we used the Behavioral Checklist that indexes multiple underlying behaviors that could potentially confound the relationship between resilience and stuttering's adverse impact. However, we did not control for overall adversity or trauma experienced by participants that could also affect their level of resilience (Thakur et al., 2020). We also did not administer a comprehensive assessment of child temperament. Attributes such as emotional regulation could positively impact a child's resilience. In our own work, we found that children with greater emotional regulation through self- or parent-report experienced lower levels of adverse impact related to stuttering (Tichenor et al., 2022). This study was a first step in assessing the relationship between protective factors such as resilience and stuttering's adverse impact. Follow-up studies that examine complex interrelationships among protective and risk factors will inform our understanding of the development of adverse impact in CWS.
Conclusions
Research into the adverse impact of stuttering in adults and children portends that youth who stutter are likely to face adversity and encounter problems unique to stuttering, as they navigate experiences involving communication with others. Zolkoski and Bullock (2012) suggest that treatment for youth at risk for experiencing adverse impact should focus on cultivating assets and resources such as resilience—a catalyst of growth and positive change (Fergus & Zimmerman, 2005; Luthar & Cicchetti, 2000; Yates et al., 2003). We found that greater resilience—external and personal—predicted less adverse impact from stuttering in children across the developmental spectrum. These results shed light on the variability in adverse impact reported by people who stutter and, thus, into the individual experience of stuttering. Our study also provides empirical support for future clinical studies incorporating resilience building into speech therapy. Clinicians can play a key role in fostering resilience in the children they treat by educating families about stuttering and about best practices to support children's communication development at different ages and stages. SLPs can also help children build skills to increase their confidence as communicators and assist families navigating challenging contexts by connecting them to resources and social support networks. These efforts may engender greater resilience and have a lasting positive impact on a child who stutters.
Author Contributions
Bridget Walsh: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Visualization, Writing – original draft, Writing – review & editing. Hannah Grobbel: Conceptualization, Investigation, Writing – original draft. Sharon Christ: Formal Analysis, Methodology, Software, Writing – review & editing. Seth Tichenor: Conceptualization, Writing – review & editing, Project administration. Katelyn Gerwin: Conceptualization, Writing – review & editing, Project administration.
Data Availability Statement
Deidentified data are available upon request by contacting the first author, Dr. Bridget Walsh, via her email: walshb16@msu.edu.
Supplementary Material
Acknowledgments
This research was supported by the National Institute on Deafness and Other Communication Disorders (Grant R01DC018000) awarded to Bridget Walsh. Portions of this study and data were based on a master's thesis submitted by the second author in partial fulfillment of the requirements for the degree of Master of Arts from the Department of Communicative Sciences and Disorders at Michigan State University. We are grateful to all the children and their families for sharing their time and insights to help us better understand how adverse impact develops in some CWS. We would also like to thank Madelyn Holmes and Kendall Causley for their contributions to data processing and to Scott Yaruss for his invaluable feedback on the project. Finally, we are grateful to Nasreen Al-Qadi, our database programmer, for her efforts in ensuring families received survey links and reminders in an organized and efficient manner.
Funding Statement
This research was supported by the National Institute on Deafness and Other Communication Disorders (Grant R01DC018000) awarded to Bridget Walsh. Portions of this study and data were based on a master's thesis submitted by the second author in partial fulfillment of the requirements for the degree of Master of Arts from the Department of Communicative Sciences and Disorders at Michigan State University.
References
- Alvord, M. K., & Grados, J. J. (2005). Enhancing resilience in children: A proactive approach. Professional Psychology: Research and Practice, 36(3), 238–245. https://doi.org/10.1037/0735-7028.36.3.238 [Google Scholar]
- Ambrose, N. G., & Yairi, E. (1994). The development of awareness of stuttering in preschool children. Journal of Fluency Disorders, 19(4), 229–245. https://doi.org/10.1016/0094-730X(94)90002-7 [Google Scholar]
- Anderson, J. D., Pellowski, M. W., Conture, E. G., & Kelly, E. M. (2003). Temperamental characteristics of young children who stutter. Journal of Speech, Language, and Hearing Research, 46(5), 1221–1233. https://doi.org/10.1044/1092-4388(2003/095) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beilby, J. M., Byrnes, M. L., & Yaruss, J. S. (2012). The impact of a stuttering disorder on western Australian children and adolescents. SIG 4 Perspectives on Fluency and Fluency Disorders, 22(2), 51–62. https://doi.org/10.1044/ffd22.2.51 [Google Scholar]
- Benzies, K., & Mychasiuk, R. (2009). Fostering family resiliency: A review of the key protective factors. Child & Family Social Work, 14(1), 103–114. https://doi.org/10.1111/j.1365-2206.2008.00586.x [Google Scholar]
- Bernard, B. (1993). Fostering resiliency in kids. Educational Leadership, 51(3), 44–48. [Google Scholar]
- Blood, G. W., & Blood, I. M. (2004). Bullying in adolescents who stutter: Communicative competence and self-esteem. Contemporary Issues in Communication Science and Disorders, 31, 69–79. https://doi.org/10.1044/cicsd_31_S_69 [Google Scholar]
- Blumgart, E., Tran, Y., & Craig, A. (2010). Social anxiety disorder in adults who stutter. Depression and Anxiety, 27(7), 687–692. https://doi.org/10.1002/da.20657 [DOI] [PubMed] [Google Scholar]
- Boey, R. A., Van de Heyning, P. H., Wuyts, F. L., Heylen, L., Stoop, R., & De Bodt, M. S. (2009). Awareness and reactions of young stuttering children aged 2-7 years old towards their speech disfluency. Journal of Communication Disorders, 42(5), 334–346. https://doi.org/10.1016/j.jcomdis.2009.03.002 [DOI] [PubMed] [Google Scholar]
- Bollen, K. A. (2014). Structural equations with latent variables. John Wiley & Sons. [Google Scholar]
- Boyce, W. T., Levitt, P., Martinez, F. D., McEwen, B. S., & Shonkoff, J. P. (2021). Genes, environments, and time: The biology of adversity and resilience. Pediatrics, 147(2), e20201651. https://doi.org/10.1542/peds.2020-1651 [DOI] [PubMed] [Google Scholar]
- Boyle, M. P. (2011). Mindfulness training in stuttering therapy: A tutorial for speech-language pathologists. Journal of Fluency Disorders, 36(2), 122–129. https://doi.org/10.1016/j.jfludis.2011.04.005 [DOI] [PubMed] [Google Scholar]
- Boyle, M. P. (2013). Assessment of stigma associated with stuttering: Development and evaluation of the self-stigma of stuttering scale (4S). Journal of Speech, Language, and Hearing Research, 56(5), 1517–1529. https://doi.org/10.1044/1092-4388(2013/12-0280) [DOI] [PubMed] [Google Scholar]
- Boyle, M. P. (2018). Enacted stigma and felt stigma experienced by adults who stutter. Journal of Communication Disorders, 73, 50–61. https://doi.org/10.1016/j.jcomdis.2018.03.004 [DOI] [PubMed] [Google Scholar]
- Boyle, M. P., Beita-Ell, C., & Milewski, K. M. (2019). Finding the good in the challenge: Benefit finding among adults who stutter. Perspectives of the ASHA Special Interest Groups, 4(6), 1316–1326. https://doi.org/10.1044/2019_PERS-SIG4-2019-0024 [Google Scholar]
- Briley, P. M., Gerlach, H., & Jacobs, M. M. (2021). Relationships between stuttering, depression, and suicidal ideation in young adults: Accounting for gender differences. Journal of Fluency Disorders, 67, 105820. https://doi.org/10.1016/j.jfludis.2020.105820 [DOI] [PubMed] [Google Scholar]
- Byrd, C., Chmela, K., Coleman, C., Weidner, M., Kelly, E., Reichhardt, R., & Irani, F. (2016). An introduction to camps for children who stutter: What they are and how they can help. Perspectives of the ASHA Special Interest Groups, 1(4), 55–69. https://doi.org/10.1044/persp1.SIG4.55 [Google Scholar]
- Cal, S. F., Sá, L. R. D., Glustak, M. E., & Santiago, M. B. (2015). Resilience in chronic diseases: A systematic review. Cogent Psychology, 2(1), 1024928. https://doi.org/10.1080/23311908.2015.1024928 [Google Scholar]
- Caughter, S., & Crofts, V. (2018). Nurturing a resilient mindset in school-aged children who stutter. American Journal of Speech-Language Pathology, 27(3S), 1111–1123. https://doi.org/10.1044/2018_AJSLP-ODC11-17-0189 [DOI] [PubMed] [Google Scholar]
- Caughter, S., & Dunsmuir, S. (2017). An exploration of the mechanisms of change following an integrated group intervention for stuttering, as perceived by school-aged children who stutter (CWS). Journal of Fluency Disorders, 51, 8–23. https://doi.org/10.1016/j.jfludis.2016.10.003 [DOI] [PubMed] [Google Scholar]
- Clark, C. E., Conture, E. G., Frankel, C. B., & Walden, T. A. (2012). Communicative and psychological dimensions of the KiddyCAT. Journal of Communication Disorders, 45(3), 223–234. https://doi.org/10.1016/j.jcomdis.2012.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connor, K. M., & Davidson, J. R. T. (2003). Development of a new resilience scale: The Connor-Davidson resilience scale (CD-RISC). Depression and Anxiety, 18(2), 76–82. https://doi.org/10.1002/da.10113 [DOI] [PubMed] [Google Scholar]
- Cook, F., & Botterill, W. (2005). Family-based approach to therapy with primary school children: “Throwing the ball back.” In Lees R. & Star C. (Eds.), The treatment of stuttering in the young school-aged child (pp. 81–107). Wiley. [Google Scholar]
- Cooke, K., & Millard, S. K. (2018). The most important therapy outcomes for school-aged children who stutter: An exploratory study. American Journal of Speech-Language Pathology, 27(3S), 1152–1163. https://doi.org/10.1044/2018_AJSLP-ODC11-17-0195 [DOI] [PubMed] [Google Scholar]
- Cozart, G., & Wilson, L. (2022). Strategies for teachers to support children who stutter: Perspectives of speech-language pathologists. Perspectives of the ASHA Special Interest Groups, 7(1), 73–86. https://doi.org/10.1044/2021_PERSP-20-00281 [Google Scholar]
- Craig, A., Blumgart, E., & Tran, Y. (2011). Resilience and stuttering: Factors that protect people from the adversity of chronic stuttering. Journal of Speech, Language, and Hearing Research, 54(6), 1485–1496. https://doi.org/10.1044/1092-4388(2011/10-0304) [DOI] [PubMed] [Google Scholar]
- De Los Reyes, A. (2011). Introduction to the special section: More than measurement error: Discovering meaning behind informant discrepancies in clinical assessments of children and adolescents. Journal of Clinical Child & Adolescent Psychology, 40(1), 1–9. https://doi.org/10.1080/15374416.2011.533405 [DOI] [PubMed] [Google Scholar]
- De Los Reyes, A., Augenstein, T. M., Wang, M., Thomas, S. A., Drabick, D. A. G., Burgers, D. E., & Rabinowitz, J. (2015). The validity of the multi-informant approach to assessing child and adolescent mental health. Psychological Bulletin, 141(4), 858–900. https://doi.org/10.1037/a0038498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Los Reyes, A., Ohannessian, C. M., & Racz, S. J. (2019). Discrepancies between adolescent and parent reports about family relationships. Child Development Perspectives, 13(1), 53–58. https://doi.org/10.1111/cdep.12306 [Google Scholar]
- De Nil, L. F., & Brutten, G. J. (1991). Speech-associated attitudes of stuttering and nonstuttering children. Journal of Speech and Hearing Research, 34(1), 60–66. https://doi.org/10.1044/jshr.3401.60 [DOI] [PubMed] [Google Scholar]
- Derogatis, L. R. (1994). SCL-90-R. Symptom Checklist-90-R. Administration, scoring and procedures manual (3rd ed.). National Computer Systems. [Google Scholar]
- DiGiuseppe, R., Linscott, J., & Jilton, R. (1996). Developing the therapeutic alliance in child—adolescent psychotherapy. Applied and Preventive Psychology, 5(2), 85–100. https://doi.org/10.1016/S0962-1849(96)80002-3 [Google Scholar]
- Druker, K. C., Mazzucchelli, T. G., & Beilby, J. M. (2019). An evaluation of an integrated fluency and resilience program for early developmental stuttering disorders. Journal of Communication Disorders, 78, 69–83. https://doi.org/10.1016/j.jcomdis.2019.02.002 [DOI] [PubMed] [Google Scholar]
- Eggers, K., De Nil, L. F., & Van den Bergh, B. R. H. (2010). Temperament dimensions in stuttering and typically developing children. Journal of Fluency Disorders, 35(4), 355–372. https://doi.org/10.1016/j.jfludis.2010.10.004 [DOI] [PubMed] [Google Scholar]
- Eggers, K., Millard, S., & Kelman, E. (2021). Temperament and the impact of stuttering in children aged 8-14 years. Journal of Speech, Language, and Hearing Research, 64(2), 417–432. https://doi.org/10.1044/2020_JSLHR-20-00095 [DOI] [PubMed] [Google Scholar]
- Erickson, S., & Block, S. (2013). The social and communication impact of stuttering on adolescents and their families. Journal of Fluency Disorders, 38(4), 311–324. https://doi.org/10.1016/j.jfludis.2013.09.003 [DOI] [PubMed] [Google Scholar]
- Fergus, S., & Zimmerman, M. A. (2005). Adolescent resilience: A framework for understanding healthy development in the face of risk. Annual Review of Public Health, 26(1), 399–419. https://doi.org/10.1146/annurev.publhealth.26.021304.144357 [DOI] [PubMed] [Google Scholar]
- Freud, D., & Amir, O. (2020). Resilience in people who stutter: Association with covert and overt characteristics of stuttering. Journal of Fluency Disorders, 64, 105761. https://doi.org/10.1016/j.jfludis.2020.105761 [DOI] [PubMed] [Google Scholar]
- Garmezy, N., Masten, A. S., & Tellegen, A. (1984). The study of stress and competence in children: A building block for developmental psychopathology. Child Development, 55(1), 97–111. https://doi.org/10.2307/1129837 [PubMed] [Google Scholar]
- Gerlach, H., Totty, E., Subramanian, A., & Zebrowski, P. (2018). Stuttering and labor market outcomes in the United States. Journal of Speech, Language, and Hearing Research, 61(7), 1649–1663. https://doi.org/10.1044/2018_JSLHR-S-17-0353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ginsburg, K. R., & Jablow, M. M. (2020). Building resilience in children and teens: Giving kids roots and wings (4th ed.). American Academy of Pediatrics. https://doi.org/10.1542/9781610023863 [Google Scholar]
- Graber, R., Turner, R., & Madill, A. (2016). Best friends and better coping: Facilitating psychological resilience through boys' and girls' closest friendships. British Journal of Psychology, 107(2), 338–358. https://doi.org/10.1111/bjop.12135 [DOI] [PubMed] [Google Scholar]
- Gunn, A., Menzies, R. G., O'Brian, S., Onslow, M., Packman, A., Lowe, R., Iverach, L., Heard, R., & Block, S. (2014). Axis I anxiety and mental health disorders among stuttering adolescents. Journal of Fluency Disorders, 40, 58–68. https://doi.org/10.1016/j.jfludis.2013.09.002 [DOI] [PubMed] [Google Scholar]
- Guttormsen, L. S., Kefalianos, E., & Næss, K.-A. B. (2015). Communication attitudes in children who stutter: A meta-analytic review. Journal of Fluency Disorders, 46, 1–14. https://doi.org/10.1016/j.jfludis.2015.08.001 [DOI] [PubMed] [Google Scholar]
- Harley, J. (2018). The role of attention in therapy for children and adolescents who stutter: Cognitive behavioral therapy and mindfulness-based interventions. American Journal of Speech-Language Pathology, 27(3S), 1139–1151. https://doi.org/10.1044/2018_AJSLP-ODC11-17-0196 [DOI] [PubMed] [Google Scholar]
- Hart, P. L., Brannan, J. D., & De Chesnay, M. (2014). Resilience in nurses: An integrative review. Journal of Nursing Management, 22(6), 720–734. https://doi.org/10.1111/j.1365-2834.2012.01485.x [DOI] [PubMed] [Google Scholar]
- Hartup, W. W., & Stevens, N. (1997). Friendships and adaptation in the life course. Psychological Bulletin, 121(3), 355–370. https://doi.org/10.1037/0033-2909.121.3.355 [Google Scholar]
- Herring, C., Millager, R. A., & Yaruss, J. S. (2022). Outcomes following participation in a support-based summer camp for children who stutter. Language, Speech, and Hearing Services in Schools, 53(1), 17–29. https://doi.org/10.1044/2021_LSHSS-21-00034 [DOI] [PubMed] [Google Scholar]
- Iimura, D., Ishida, O., Takahashi, S., Yokoi, H., & Miyamoto, S. (2021). A questionnaire survey about support requests from school-age children and adolescents who stutter. Language, Speech, and Hearing Services in Schools, 52(2), 717–727. https://doi.org/10.1044/2020_LSHSS-20-00069 [DOI] [PubMed] [Google Scholar]
- Iverach, L., Jones, M., McLellan, L. F., Lyneham, H. J., Menzies, R. G., Onslow, M., & Rapee, R. M. (2016). Prevalence of anxiety disorders among children who stutter. Journal of Fluency Disorders, 49, 13–28. https://doi.org/10.1016/j.jfludis.2016.07.002 [DOI] [PubMed] [Google Scholar]
- Iverach, L., O'Brian, S., Jones, M., Block, S., Lincoln, M., Harrison, E., Hewat, S., Menzies, R. G., Packman, A., & Onslow, M. (2009). Prevalence of anxiety disorders among adults seeking speech therapy for stuttering. Journal of Anxiety Disorders, 23(7), 928–934. https://doi.org/10.1016/j.janxdis.2009.06.003 [DOI] [PubMed] [Google Scholar]
- Iverach, L., & Rapee, R. M. (2014). Social anxiety disorder and stuttering: Current status and future directions. Journal of Fluency Disorders, 40, 69–82. https://doi.org/10.1016/j.jfludis.2013.08.003 [DOI] [PubMed] [Google Scholar]
- Jefferies, P., McGarrigle, L., & Ungar, M. (2019). The CYRM-R: A Rasch-validated revision of the child and youth resilience measure. Journal of Evidence-Based Social Work, 16(1), 70–92. https://doi.org/10.1080/23761407.2018.1548403 [DOI] [PubMed] [Google Scholar]
- Johnson, C. A., Garnett, E. O., Chow, H. M., Spray, G. J., Zhu, D. C., & Chang, S.-E. (2021). Developmental factors that predict head movement during resting-state functional magnetic resonance imaging in 3-7-year-old stuttering and non-stuttering children. Frontiers in Neuroscience, 15, 753010.https://doi.org/10.3389/fnins.2021.753010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson, H. (2018). Protecting the most vulnerable from abuse. The ASHA Leader, 17(14), 16–19. https://doi.org/10.1044/leader.FTR2.17142012.16 [Google Scholar]
- Jöreskog, K. G. (1969). A general approach to confirmatory maximum likelihood factor analysis. Psychometrika, 34(2), 183–202. https://doi.org/10.1007/BF02289343 [Google Scholar]
- Joyce, S., Shand, F., Tighe, J., Laurent, S. J., Bryant, R. A., & Harvey, S. B. (2018). Road to resilience: A systematic review and meta-analysis of resilience training programmes and interventions. BMJ Open, 8(6), Article e017858. https://doi.org/10.1136/bmjopen-2017-017858 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karrass, J., Walden, T. A., Conture, E. G., Graham, C. G., Arnold, H. S., Hartfield, K. N., & Schwenk, K. A. (2006). Relation of emotional reactivity and regulation to childhood stuttering. Journal of Communication Disorders, 39(6), 402–423. https://doi.org/10.1016/j.jcomdis.2005.12.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kefalianos, E., Onslow, M., Ukoumunne, O., Block, S., & Reilly, S. (2014). Stuttering, temperament, and anxiety: Data from a community cohort ages 2-4 years. Journal of Speech, Language, and Hearing Research, 57(4), 1314–1322. https://doi.org/10.1044/2014_JSLHR-S-13-0069 [DOI] [PubMed] [Google Scholar]
- Kefalianos, E., Onslow, M., Ukoumunne, O. C., Block, S., & Reilly, S. (2017). Temperament and early stuttering development: Cross-sectional findings from a community cohort. Journal of Speech, Language, and Hearing Research, 60(4), 772–784. https://doi.org/10.1044/2016_JSLHR-S-15-0196 [DOI] [PubMed] [Google Scholar]
- Kelman, E., & Wheeler, S. (2015). Cognitive behaviour therapy with children who stutter. Procedia - Social and Behavioral Sciences, 193, 165–174. https://doi.org/10.1016/j.sbspro.2015.03.256 [Google Scholar]
- Klein, A., & Moosbrugger, H. (2000). Maximum likelihood estimation of latent interaction effects with the LMS method. Psychometrika, 65(4), 457–474. https://doi.org/10.1007/BF02296338 [Google Scholar]
- Klein, J. F., & Hood, S. B. (2004). The impact of stuttering on employment opportunities and job performance. Journal of Fluency Disorders, 29(4), 255–273. https://doi.org/10.1016/j.jfludis.2004.08.001 [DOI] [PubMed] [Google Scholar]
- Kline, R. B. (2016). Principles and practice of structural equation modeling (methodology in the social sciences) (4th ed.). The Guilford Press. [Google Scholar]
- Langevin, M., & Bortnick, K. (1998). Teasing/bullying experienced by children who stutter: Toward development of a questionnaire. Contemporary Issues in Communication Science and Disorders, 25, 8–20. https://doi.org/10.1044/cicsd_25_S_8 [Google Scholar]
- Langevin, M., Packman, A., & Onslow, M. (2010). Parent perceptions of the impact of stuttering on their preschoolers and themselves. Journal of Communication Disorders, 43(5), 407–423. https://doi.org/10.1016/j.jcomdis.2010.05.003 [DOI] [PubMed] [Google Scholar]
- Luthar, S. S., & Cicchetti, D. (2000). The construct of resilience: Implications for interventions and social policies. Development and Psychopathology, 12(4), 857–885. https://doi.org/10.1017/S0954579400004156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lyons, R., & Roulstone, S. (2018). Well-being and resilience in children with speech and language disorders. Journal of Speech, Language, and Hearing Research, 61(2), 324–344. https://doi.org/10.1044/2017_JSLHR-L-16-0391 [DOI] [PubMed] [Google Scholar]
- Masten, A. S. (2001). Ordinary magic. Resilience processes in development. The American Psychologist, 56(3), 227–238. https://doi.org/10.1037//0003-066x.56.3.227 [DOI] [PubMed] [Google Scholar]
- Masten, A. S., & Coatsworth, J. D. (1998). The development of competence in favorable and unfavorable environments. Lessons from research on successful children. The American Psychologist, 53(2), 205–220. https://doi.org/10.1037//0003-066x.53.2.205 [DOI] [PubMed] [Google Scholar]
- Masten, A. S., Hubbard, J. J., Gest, S. D., Tellegen, A., Garmezy, N., & Ramirez, M. (1999). Competence in the context of adversity: Pathways to resilience and maladaptation from childhood to late adolescence. Development and Psychopathology, 11(1), 143–169. https://doi.org/10.1017/S0954579499001996 [DOI] [PubMed] [Google Scholar]
- Masten, C. L., Telzer, E. H., Fuligni, A. J., Lieberman, M. D., & Eisenberger, N. I. (2012). Time spent with friends in adolescence relates to less neural sensitivity to later peer rejection. Social Cognitive and Affective Neuroscience, 7(1), 106–114. https://doi.org/10.1093/scan/nsq098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGeary, D. D. (2011). Making sense of resilience. Military Medicine, 176(6), 603–604. https://doi.org/10.7205/MILMED-D-10-00480 [DOI] [PubMed] [Google Scholar]
- Menzies, R. G., O'Brian, S., Onslow, M., Packman, A., St Clare, T., & Block, S. (2008). An experimental clinical trial of a cognitive-behavior therapy package for chronic stuttering. Journal of Speech, Language, and Hearing Research, 51(6), 1451–1464. https://doi.org/10.1044/1092-4388(2008/07-0070) [DOI] [PubMed] [Google Scholar]
- Millard, S. K. (2011). Intensive group therapy for children who stutter: Early evidence. SIG 4 Perspectives on Fluency and Fluency Disorders, 21(1), 22–32. https://doi.org/10.1044/ffd21.1.22 [Google Scholar]
- Mulcahy, K., Hennessey, N., Beilby, J., & Byrnes, M. (2008). Social anxiety and the severity and typography of stuttering in adolescents. Journal of Fluency Disorders, 33(4), 306–319. https://doi.org/10.1016/j.jfludis.2008.12.002 [DOI] [PubMed] [Google Scholar]
- Pearson, J., & Hall, D. K. (2006). Reaching in…reaching out: Resiliency guidebook. https://www.wellington.ca/en/social-services/riro.aspx
- Plexico, L. W., Erath, S., Shores, H., & Burrus, E. (2019). Self-acceptance, resilience, coping and satisfaction of life in people who stutter. Journal of Fluency Disorders, 59, 52–63. https://doi.org/10.1016/j.jfludis.2018.10.004 [DOI] [PubMed] [Google Scholar]
- Plexico, L. W., Manning, W. H., & DiLollo, A. (2010). Client perceptions of effective and ineffective therapeutic alliances during treatment for stuttering. Journal of Fluency Disorders, 35(4), 333–354. https://doi.org/10.1016/j.jfludis.2010.07.001 [DOI] [PubMed] [Google Scholar]
- Plexico, L. W., & Sandage, M. J. (2011). A mindful approach to stuttering intervention. SIG 4 Perspectives on Fluency and Fluency Disorders, 21(2), 43–49. https://doi.org/10.1044/ffd21.2.43 [Google Scholar]
- Potock, M. (2017). Feeding disorders and food insecurity: A 6-step action plan. The ASHA Leader Live. https://leader.pubs.asha.org/do/10.1044/feeding-disorders-and-food-insecurity-a-6-step-action-plan/full/ [Google Scholar]
- Prince-Embury, S. (2006). The resiliency scales for children and adolescents: A profile of personal strengths. Harcourt Assessment Inc. [Google Scholar]
- Reilly, S., Onslow, M., Packman, A., Cini, E., Conway, L., Ukoumunne, O. C., Bavin, E. L., Prior, M., Eadie, P., Block, S., & Wake, M. (2013). Natural history of stuttering to 4 years of age: A prospective community-based study. Pediatrics, 132(3), 460–467. https://doi.org/10.1542/peds.2012-3067 [DOI] [PubMed] [Google Scholar]
- Resilience Research Centre. (2018). CYRM and ARM user manual. Dalhousie University. [Google Scholar]
- Rutter, M. (1985). Resilience in the face of adversity. The British Journal of Psychiatry: The Journal of Mental Science, 147(6), 598–611. https://doi.org/10.1192/bjp.147.6.598 [DOI] [PubMed] [Google Scholar]
- Rutter, M., Tizard, J., Yule, W., Graham, P., & Whitmore, K. (1976). Research report: Isle of Wight studies, 1964-1974. Psychological Medicine, 6(2), 313–332. https://doi.org/10.1017/s003329170001388x [DOI] [PubMed] [Google Scholar]
- Samson, I., Lindström, E., Sand, A., Herlitz, A., & Schalling, E. (2021). Larger reported impact of stuttering in teenage females, compared to males—A comparison of teenagers' result on Overall Assessment of the Speaker's Experience of Stuttering (OASES). Journal of Fluency Disorders, 67, 105822.https://doi.org/10.1016/j.jfludis.2020.105822 [DOI] [PubMed] [Google Scholar]
- Sanders, M. R., Morawska, A., Haslam, D. M., Filus, A. & Fletcher, R. (2014). Parenting and Family Adjustment Scales (PAFAS): Validation of a brief parent-report measure for use in assessment of parenting skills and family relationships. Child Psychiatry and Human Development, 45(3), 255–272. https://doi.org/10.1007/s10578-013-0397-3 [DOI] [PubMed] [Google Scholar]
- Sanders, J., Munford, R., Thimasarn-Anwar, T., Liebenberg, L., & Ungar, M. (2015). The role of positive youth development practices in building resilience and enhancing wellbeing for at-risk youth. Child Abuse & Neglect, 42, 40–53. https://doi.org/10.1016/j.chiabu.2015.02.006 [DOI] [PubMed] [Google Scholar]
- Schafer, E. S. (2022). Recognizing resilience in children: A review. Trauma Care, 2(3), 469–480. https://doi.org/10.3390/traumacare2030039 [Google Scholar]
- Smith, K. A., Iverach, L., O'Brian, S., Kefalianos, E., & Reilly, S. (2014). Anxiety of children and adolescents who stutter: A review. Journal of Fluency Disorders, 40, 22–34. https://doi.org/10.1016/j.jfludis.2014.01.003 [DOI] [PubMed] [Google Scholar]
- Stein, M. B., Baird, A., & Walker, J. R. (1996). Social phobia in adults with stuttering. The American Journal of Psychiatry, 153(2), 278–280. https://doi.org/10.1176/ajp.153.2.278 [DOI] [PubMed] [Google Scholar]
- Stuart, J., & Jose, P. E. (2012). The influence of discrepancies between adolescent and parent ratings of family dynamics on the well-being of adolescents. Journal of Family Psychology, 26(6), 858–868. https://doi.org/10.1037/a0030056 [DOI] [PubMed] [Google Scholar]
- Thakur, N., Hessler, D., Koita, K., Ye, M., Benson, M., Gilgoff, R., Bucci, M., Long, D., & Harris, N. B. (2020). PEdiatrics Adverse Childhood Experiences and Related Life Events Screener (PEARLS) and health in a safety-net practice. Child Abuse & Neglect, 108, 104685. https://doi.org/10.1016/j.chiabu.2020.104685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomlison, B. (1997). Risk and protective factors in child maltreatment. In Fraser M. W. (Ed.), Risk and resilience in childhood: An ecological perspective (pp. 50–72). NASW Press. [Google Scholar]
- Tichenor, S. E., Palasik, S., & Yaruss, J. (in press). Understanding the broader impact of stuttering: Suicidal ideation. American Journal of Speech-Language Pathology. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tichenor, S., & Yaruss, J. S. (2020). Repetitive negative thinking, temperament, and adverse impact in adults who stutter. American Journal of Speech-Language Pathology, 29(1), 201–215. https://doi.org/10.1044/2019_AJSLP-19-00077 [DOI] [PubMed] [Google Scholar]
- Tichenor, S. E., Walsh, B. M., Gerwin, K. L., & Yaruss, J. S. (2022). Emotional regulation and its influence on the experience of stuttering across the life span. Journal of Speech, Language, and Hearing Research, 65(7), 2412–2430. https://doi.org/10.1044/2022_JSLHR-21-00467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tichenor, S. E., & Yaruss, J. S. (2019). Stuttering as defined by adults who stutter. Journal of Speech, Language, and Hearing Research, 62(12), 4356–4369. https://doi.org/10.1044/2019_JSLHR-19-00137 [DOI] [PubMed] [Google Scholar]
- Ungar, M. (2004a). The importance of parents and other caregivers to the resilience of high-risk adolescents. Family Process, 43(1), 23–41. https://doi.org/10.1111/j.1545-5300.2004.04301004.x [DOI] [PubMed] [Google Scholar]
- Ungar, M. (2004b). A constructionist discourse on resilience. Youth & Society, 35(3), 341–365. https://doi.org/10.1177/0044118X03257030 [Google Scholar]
- Ungar, M. (2008). Resilience across cultures. The British Journal of Social Work, 38(2), 218–235. https://doi.org/10.1093/bjsw/bcl343 [Google Scholar]
- Ungar, M. (2010). Families as navigators and negotiators: Facilitating culturally and contextually specific expressions of resilience. Family Process, 49(3), 421–435. https://doi.org/10.1111/j.1545-5300.2010.01331.x [DOI] [PubMed] [Google Scholar]
- Ungar, M. (2011). The social ecology of resilience: Addressing contextual and cultural ambiguity of a nascent construct. The American Journal of Orthopsychiatry, 81(1), 1–17. https://doi.org/10.1111/j.1939-0025.2010.01067.x [DOI] [PubMed] [Google Scholar]
- Ungar, M., Ghazinour, M., & Richter, J. (2013). Annual research review: What is resilience within the social ecology of human development? The Journal of Child Psychology and Psychiatry and Allied Disciplines, 54(4), 348–366. https://doi.org/10.1111/jcpp.12025 [DOI] [PubMed] [Google Scholar]
- Van Borsel, J., Brepoels, M., & De Coene, J. (2011). Stuttering, attractiveness, and romantic relationships: The perception of adolescents and young adults. Journal of Fluency Disorders, 36(1), 41–50. https://doi.org/10.1016/j.jfludis.2011.01.002 [DOI] [PubMed] [Google Scholar]
- Vanryckeghem, M., Brutten, G. J., & Hernandez, L. M. (2005). A comparative investigation of the speech-associated attitude of preschool and kindergarten children who do and do not stutter. Journal of Fluency Disorders, 30(4), 307–318. https://doi.org/10.1016/j.jfludis.2005.09.003 [DOI] [PubMed] [Google Scholar]
- Walsh, B., Smith, A., Christ, S. L., & Weber, C. (2019). Sympathetic nervous system activity in preschoolers who stutter. Frontiers in Human Neuroscience, 13, 356. https://doi.org/10.3389/fnhum.2019.00356 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Werner, E. E. (1971). The children of Kauai: A longitudinal study from the prenatal period at age ten. University of Hawaii Press. [Google Scholar]
- World Health Organization. (2001). International classification of functioning, disability, and health. World Health Organization. [Google Scholar]
- Yairi, E., & Ambrose, N. G. (2005). Early childhood stuttering for clinicians by clinicians. Pro-Ed. [Google Scholar]
- Yaruss, J. S. (1998). Describing the consequences of disorders: Stuttering and the International Classification of Impairments, Disabilities, and Handicaps. Journal of Speech, Language, and Hearing Research, 41(2), 249–257. https://doi.org/10.1044/jslhr.4102.249 [DOI] [PubMed] [Google Scholar]
- Yaruss, J. S., & Quesal, R. W. (2004). Stuttering and the international classification of functioning, disability, and health: An update. Journal of Communication Disorders, 37(1), 35–52. https://doi.org/10.1016/S0021-9924(03)00052-2 [DOI] [PubMed] [Google Scholar]
- Yaruss, J. S., & Quesal, R. W. (2016). Overall Assessment of the Speaker's Experience of Stuttering. Stuttering Therapy Resources. [Google Scholar]
- Yaruss, J. S., & Reardon-Reeves, N. (2017). Early childhood stuttering therapy: A practical guide. Stuttering Therapy Resources. [Google Scholar]
- Yaruss, J. S., Reeves, N., & Herring, C. (2018). How speech–language pathologists can minimize bullying of children who stutter. Seminars in Speech and Language, 39(4), 342–355. https://doi.org/10.1055/s-0038-1667163 [DOI] [PubMed] [Google Scholar]
- Yaruss, J. S., & Yaruss, V. R. (2021). Overall Assessment of the Speaker's Experience of Stuttering—Early Childhood and Family Response Forms. Stuttering Therapy Resources, Inc. [Google Scholar]
- Yates, T. M., Egeland, B., & Sroufe, L. A. (2003). Rethinking resilience: A developmental process perspective. In Resilience and vulnerability: Adaptation in the context of childhood adversities (pp. 243–266). Cambridge University Press. https://doi.org/10.1017/CBO9780511615788.012 [Google Scholar]
- Zolkoski, S. M., & Bullock, L. M. (2012). Resilience in children and youth: A review. Children and Youth Services Review, 34(12), 2295–2303. https://doi.org/10.1016/j.childyouth.2012.08.009 [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Deidentified data are available upon request by contacting the first author, Dr. Bridget Walsh, via her email: walshb16@msu.edu.