Abstract
BACKGROUND AND OBJECTIVES
Children and Youth with Special Health Care Needs (CYSHCN) have differing risk factors and injury characteristics compared with peers without special health care needs (SHCN). We examined the association between SHCN status and complications, mortality, and length of stay (LOS) after trauma hospitalization.
METHODS
We conducted a cross-sectional study using 2018 data from the National Trauma Data Bank for patients aged 1 to 18 years (n = 108 062). We examined the following hospital outcomes: any complication reported, unplanned admission to the ICU, in-hospital mortality, and hospital and ICU LOS. Multivariate regression models estimated the effect of SHCN status on hospital outcomes after controlling for patient demographics, injury severity score, and Glasgow Coma Score. Subanalyses examined outcomes by age, SHCN, and injury severity score.
RESULTS
CYSHCN encounters had a greater adjusted relative risk (ARR) of any hospital complications (ARR = 2.980) and unplanned admission to the ICU (ARR = 1.996) than encounters that did not report a SHCN (P < .001). CYSHCN had longer hospital (incidence rate ratio = 1.119) and ICU LOS (incidence rate ratio = 1.319, both P < .001). There were no statistically significant in-hospital mortality differences between CYSHCN and those without. Lower severity trauma was associated with a greater ARR of hospital complications for CYSHCN encounters versus non-CYSHCN encounters.
CONCLUSIONS
CYSHCN, particularly those with lower-acuity injuries, are at greater risk for developing complications and requiring more care after trauma hospitalization. Future studies may examine mechanisms of hospital complications for traumatic injuries among CYSHCN to develop prevention and risk-minimization strategies.
Children and youth with special health care needs (CYSHCN) require more medical care and other services than their nonspecial health care needs peers because of ongoing chronic condition management.1 Almost 14 million US children have special health care needs (SHCN).2 SHCN can include physical, developmental, behavioral, or emotional conditions such as attention-deficit disorder or attention-deficit/hyperactivity disorder (ADHD), anxiety/depression, arthritis, asthma, autism cerebral palsy, cystic fibrosis, diabetes, Down syndrome, and hemophilia. In the United States, CYSHCN, such as those with disabilities,3 complex chronic conditions,4 and specific SHCN like neurologic impairments,5 use more inpatient care than children without SHCN.
Some CYSHCN who are hospitalized are admitted through the pediatric trauma system, where just <17% of encounters in the 2018 National Trauma Data Bank were associated with at least 1 chronic condition.6 In adult trauma patients, patient-level factors such as preexisting conditions contribute to mortality and length of stay (LOS) differences.7,8 Previous literature suggests that CYSHCN generally have longer hospital and ICU LOS after injury,9,10 as well as longer hospital LOS for specific SHCN.11–14 However, studies differ as to whether CYSHCN have a lower risk of mortality after physical trauma,9,15 and most do not examine trauma system outcomes other than mortality and LOS; they also do not consider variation by subpopulation such as comparisons among children of similar injury severity.
The objective of this study is to examine the association between CYSHCN status and pertinent hospital outcomes in the trauma system. We hypothesize that CYSHCN will be more likely to: have any reported hospital complications after physical trauma, have an unplanned admission to the ICU, die in the hospital, and have a longer ICU LOS and total LOS. We also subdivide the data to examine associations at different ages, SHCN categories, and injury severity scores (ISS) to potentially identify priority SHCN populations on which to focus future research to improve hospital care quality.
Methods
Data
This cross-sectional study employed data from the 2018 Trauma Quality Programs Participant Use File, which is managed by the American College of Surgeons (ACS). The Participant Use File includes the National Trauma Data Bank (NTDB) and is composed of US trauma registry data from state-designated trauma centers. In 2015, the most recent year for which data are available, 744 centers voluntarily submitted their data, which are entered by trained trauma registrars.16 Data are submitted on the basis of the trauma system encounter; therefore, we refer to observations as encounters rather than patients. We extracted data on the basis of encounter age limited to those ages 1 to 18 years on the date of traumatic injury as captured by the NTDB. Before beginning this study, we obtained approval from the ACS to use their data and from our institution’s institutional review board, which determined that this study was exempt from review (STUDY00004642).
Variables and Measures
We employed or generated the following independent variables using the NTDB: SHCN status, demographic variables, ISS, and Glasgow Coma Score (GCS). To operationalize SHCN status, we generated a dichotomous variable that uses the presence or absence of 1 or more of 25 chronic conditions required to be tracked by the 2018 NTDB (Supplemental Table 4).6 We also employed variables that capture encounter demographics such as sex and ethnicity. We coded encounter race as white with no other race indicated, Black race indicated or in combination with another race, and other; this latter category includes encounters specified as “other race” by the NTDB, as well as those races that did not meet a 5% threshold in the population of NTDB encounters. We include race and ethnicity variables because of the established literature indicating racial and ethnic disparities in trauma outcomes.17–19 We condensed insurance status as recorded by the NTDB into 3 categories: private, public (Medicaid, Medicare, and other government), and other (self-pay, not billed, and other) insurance. We constructed the following age categories using ∼5-year increments: 1 to 5, 6 to 11, and 12 to 18.6 In addition to these encounter-specific demographic factors, hospital outcomes after trauma also depend on the extent of injury. Therefore, we control for abbreviated injury scale-derived ISS, which is a composite score based on the 3 body regions with the most severe injuries, and total GCS as recorded in the NTDB. For a description of how ISS translates to the presentation of admitted patients, please see Supplemental Table 5.
Pediatric Trauma Hospital Outcomes
We considered the following pediatric trauma hospital outcomes. We generated a dichotomous hospital complications variable on the basis of whether the encounter had any known complications of 22 possible complications captured by the 2018 NTDB.20 We used a dichotomous variable coded by the NTDB on the basis of whether an unplanned admission to the ICU occurred during the encounter’s hospital stay. We used the NTDB’s hospital discharge disposition variable to code a dichotomous in-hospital mortality variable. We also considered 2 continuous pediatric trauma hospital outcomes: hospital LOS and ICU LOS.
Statistical Analyses
We assessed demographic, ISS, and GCS differences by comparing encounters identified as CYSHCN with non-SHCN encounters. For these comparisons, we used χ2 or t tests and reported either frequencies and percentages for categorical variables or mean and SDs for continuous variables. We also describe the presence of hospital complications by reporting frequencies and percentages overall, as well as segmented by SHCN status. Similarly, we describe hospital and ICU LOS overall and by SHCN status, reporting the mean and SD for these outcomes.
We then estimated multivariate models to examine the association between the outcome variables and SHCN status, controlling for demographic and clinical characteristics. For the dichotomous variables, any hospital complication, unplanned admission to the ICU, and in-hospital mortality, we estimated logistic regression models. When presenting these results, we include both the unadjusted and adjusted relative risks (ARR),21 95% confidence intervals, and P values. The skewed distribution of the LOS variables indicates that count models should be estimated. Negative binomial models with mean dispersion were selected on the basis of Akaike information criterion and Bayesian information criterion specification tests. When presenting results from negative binomial models, we include both the unadjusted and adjusted incident rate ratios (IRR), 95% confidence intervals, and P values.
After the main results, we conducted subanalyses by age, SHCN type, and ISS to examine within-group differences. For age, we used the following groups: 1 to 5, 6 to 11, and 12 to 18 years. We then conducted subanalyses by SHCN, grouping on the basis of mental health (ie, mental/personality disorders and attention-deficit disorder/ADHD), alcohol/substance use disorder (SUD), and medical (ie, all remaining disorders except for other) SHCN.6 We conducted subanalyses by ISS (minor/1–8, moderate/9–15, severe/16–24, and most severe/25 and higher)22 and separately evaluated interaction effects of ISS and age with SHCN. Subanalyses models controlled for sex, race, ethnicity, insurance type, and GCS; ISS-focused models controlled for age and age-focused models controlled for ISS.
For statistical significance, we used both nominal P values and false discovery rate (FDR)-adjusted P values (q values) for multiple comparisons using the Benjamini–Hochberg method. A q value <0.05 controls an FDR at 5%. Stata/SE version 17.0 was used to perform the analyses, except for the following: R version 4.1.0 was used for the FDR-adjusted P values and to generate figures. This study follows the Strengthening the Reporting of Observational Studies in Epidemiology guidelines (Supplemental Table 6).
Missing Data
We examined each independent variable for missing data, where rates of missingness were low. Only 2 variables had >2.5% missing: ethnicity (4.6%) and GCS (6.1%). We addressed missing data in 2 ways. In the main analyses, encounters in which 1 or more values were missing for the independent variables (ie, demographic and clinical characteristics) were excluded from the analyses. χ2 and t tests indicated that encounters with missing data differed from those without missing data across all demographic and clinical characteristics (P < .050), with the exception of SHCN status (P = .060) (Supplemental Table 7). We then conducted sensitivity analyses by also using the missing indicator method to address missing values and reestimated the models described above.23
Results
Descriptive Statistics and Categorical Comparisons
The 2018 NTDB contains 108 062 pediatric encounters with full demographic data and clinical variables of interest, where 16 426 were excluded because of missing data (Fig 1). Of included encounters, 16.5% reported 1 or more SHCN. Pediatric encounters reporting SHCN differed across all demographic and clinical characteristics examined (Table 1). Encounters reporting SHCN had an older mean age, and a higher proportion were male and indicated a higher mean ISS (P < .001). A lower proportion of encounters reporting SHCN indicated Hispanic/Latino ethnicity (P < .001); differences by race, insurance type, and GCS were also observed.
FIGURE 1.
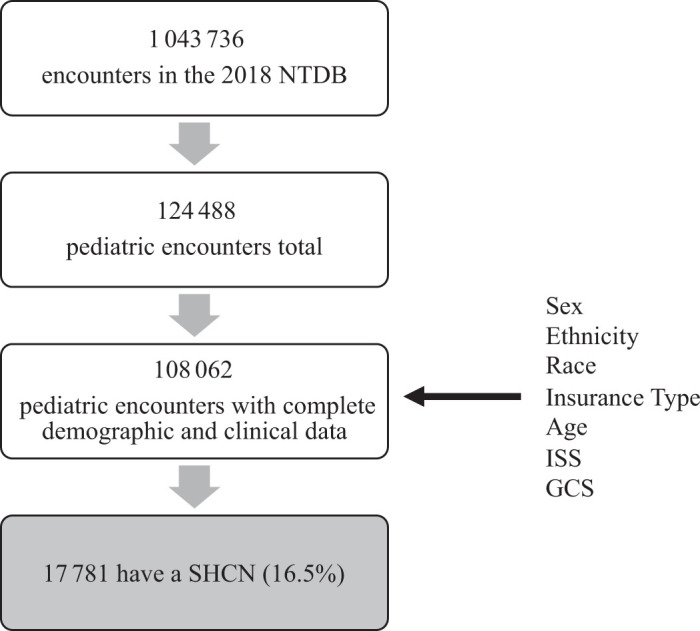
Participant Flow Diagram.
TABLE 1.
Demographic and Clinical Variables by SHCN Status, 2018 NTDB Pediatric Encounters
| Characteristic | Overall | Without SHCN | SHCN | P | ||||
|---|---|---|---|---|---|---|---|---|
| N (%) | 108 062 | 100.0% | 90 281 | 83.6% | 17 781 | 16.5% | ||
| Male sex, n % | 70 390 | 65.1% | 58 102 | 64.4% | 12 288 | 69.1% | <.001c | |
| Hispanic/Latino, n % | 19 730 | 18.3% | 16 928 | 18.8% | 2802 | 15.8% | <.001c | |
| Race, n % | <.001c | |||||||
| White | 71 994 | 66.6% | 59 980 | 66.4% | 12 014 | 67.6% | ||
| Black | 20 575 | 19.0% | 17 129 | 19.0% | 3446 | 19.4% | ||
| Othera | 15 493 | 14.3% | 13 172 | 14.6% | 2321 | 13.1% | ||
| Insurance type, n % | <.001c | |||||||
| Private | 49 357 | 45.7% | 41 463 | 45.9% | 7894 | 44.4% | ||
| Public | 47 217 | 43.7% | 38 921 | 43.1% | 8296 | 46.7% | ||
| Otherb | 11 488 | 10.6% | 9897 | 11.0% | 1591 | 8.9% | ||
| Age, mean (SD) | 10.4 | 5.6 | 10.0 | 5.6 | 12.3 | 5.1 | <.001c | |
| Age category, n % | <.001c | |||||||
| 1–5 y | 27 930 | 25.8% | 25 356 | 28.1% | 2574 | 14.5% | ||
| 6–11 y | 28 190 | 26.1% | 24 075 | 26.7% | 4115 | 23.1% | ||
| 12–18 y | 51 942 | 48.1% | 40 850 | 45.2% | 11 092 | 62.4% | ||
| ISS, mean (SD) | 7.2 | 7.7 | 7.1 | 7.7 | 7.7 | 8.0 | <.001c | |
| ISS category, n % | <.001c | |||||||
| 1–8 | 72 316 | 67% | 61 155 | 68% | 11 161 | 63% | ||
| 9–15 | 23 844 | 22% | 19 526 | 22% | 4318 | 24% | ||
| 16–24 | 6871 | 6% | 5523 | 6% | 1348 | 8% | ||
| 25 and above | 5031 | 5% | 4077 | 5% | 954 | 5% | ||
| GCS, mean (SD) | 14.3 | 2.4 | 14.4 | 2.4 | 14.3 | 2.5 | <.001c | |
Other race is composed of other (10.8%), Asian American (2.0%), Pacific Islander (0.3%), and American Indian (1.3%). Encounters can be coded as 1 or more race.
Other insurance is composed of other (2.6%), self-pay (7.9%), and not billed (0.15%).
Results statistically significant after FDR adjustment.
Overall, 4% of pediatric encounters (n = 4335) reported a hospital complication; a higher percentage of CYSHCN encounters reported any hospital complications in comparison with non-SHCN encounters (9.2% vs 3.0%, P < .001) (Table 2). Pediatric encounters reported a maximum of 8 complications, where the modal value was 1 (n = 3859) (Supplemental Fig 3). Of the 22 types of hospital complications reported, the most common overall were other (2.60%), cardiac arrest with cardiopulmonary resuscitation (0.31%), unplanned admission to the ICU (0.29%), and unplanned return to the operating room (0.27%) (Table 2). Additionally, a higher proportion of CYSHCN encounters reported the following complications: pressure ulcers, acute respiratory distress syndrome, unplanned intubation, and acute kidney injury.
TABLE 2.
Reported Pediatric Trauma Outcomes by SHCN Status, 2018 NTDB Encounters
| Trauma Outcome (n % Unless Otherwise Specified) | Overall | SHCN Status | P | ||||
|---|---|---|---|---|---|---|---|
| No SHCN | SHCN | ||||||
| Any reported hospital complication | 4332 | 4.01% | 2703 | 2.99% | 1629 | 9.16% | <.001a |
| Other | 2808 | 2.60% | 1510 | 1.67% | 1298 | 7.30% | <.001a |
| Unplanned admission to the ICU | 310 | 0.29% | 214 | 0.24% | 96 | 0.54% | <.001a |
| Unplanned return to the OR | 289 | 0.27% | 231 | 0.26% | 58 | 0.33% | .097 |
| Cardiac arrest with CPR | 339 | 0.31% | 291 | 0.32% | 48 | 0.27% | .254 |
| Pressure ulcer | 174 | 0.16% | 133 | 0.15% | 41 | 0.23% | .011a |
| Acute respiratory distress syndrome | 119 | 0.11% | 80 | 0.09% | 39 | 0.22% | <.001a |
| Ventilator-associated pneumonia | 166 | 0.15% | 130 | 0.14% | 36 | 0.20% | .069 |
| Unplanned intubation | 132 | 0.12% | 98 | 0.11% | 34 | 0.19% | .004a |
| Deep vein thrombosis | 152 | 0.14% | 120 | 0.13% | 32 | 0.18% | .126 |
| Acute kidney injury | 95 | 0.09% | 69 | 0.08% | 26 | 0.15% | .004a |
| Catheter-associated urinary tract infection | 69 | 0.06% | 54 | 0.06% | 15 | 0.08% | .236 |
| Extremity compartment syndrome | 84 | 0.08% | 71 | 0.08% | 13 | 0.07% | .809 |
| Stroke/CVA | 54 | 0.05% | 41 | 0.05% | 13 | 0.07% | .131 |
| Severe sepsis | 54 | 0.05% | 42 | 0.05% | 12 | 0.07% | .253 |
| In-hospital mortality | 1046 | 0.97% | 882 | 0.98% | 164 | 0.92% | .497 |
| Hospital LOS, mean (SD) (n = 106 534) | 3.3 | 6.4 | 3.2 | 6.3 | 3.9 | 6.9 | <.001a |
| ICU LOS, mean (SD) | 0.7 | 3.3 | 0.7 | 3.3 | 0.9 | 3.5 | <.001a |
N = 108 062 unless otherwise specified. The following were reported by <50 encounters: Deep surgical site infection, superficial incisional surgical site infection, organ/space surgical site infection, pulmonary embolism, central line-associated bloodstream infection, alcohol withdrawal syndrome, osteomyelitis, and myocardial infarction. Shaded rows indicate that this variable is an outcome explicitly examined through multivariate analyses. CPR, cardiopulmonary resuscitation; CVA, cerebrovascular accident; OR, operating room.
Results statistically significant after FDR adjustment.
The mean hospital LOS was 3.3 days (range: 1–376) and the mean ICU LOS was 0.7 days (range: 0–376). Compared with encounters not reporting a SHCN, CYSHCN encounters had a longer hospital LOS (3.9 vs 3.2, P < .001) and ICU LOS (0.9 vs 0.7 P < .001). In-hospital mortality was relatively rare, reported in <1% of encounters, and did not differ by SHCN status (Table 2).
Multivariate Analyses
CYSHCN encounters had a higher likelihood of reporting any hospital complications (ARR = 2.980) and a higher likelihood of unplanned admission to the ICU (ARR = 1.996) (P < .001) (Table 3). There were no statistically significant differences in risk for in-hospital mortality when comparing encounters by SHCN status (P = .267). CYSHCN encounters also reported longer hospital (IRR = 1.119) and ICU LOS (IRR = 1.319) (P < .001).
TABLE 3.
Maximum Likelihood Estimates for Pediatric Trauma Outcomes and Association With Special Health Care Needs Status, 2018 NTDB Encounters
| Outcome (Logistic Regression) | Unadjusted RR (95% CI) | P | ARR (95% CI) | P |
|---|---|---|---|---|
| Any hospital complications | 3.060 (2.884–3.247) | <.001 | 2.980 (2.812–3.158) | <.001a |
| Unplanned admission to the ICU | 2.278 (1.791–2.896) | <.001 | 1.996 (1.567–2.540) | <.001a |
| In-hospital mortality | 0.944 (0.800–1.115) | .497 | 0.926 (0.804–1.065) | .279 |
| Outcome (negative binomial) | Unadjusted IRR (95% CI) | P | Adjusted IRR (95% CI) | P |
| Hospital LOS (n = 106 534) | 1.234 (1.216–1.253) | <.001 | 1.119 (1.104–1.134) | <.001a |
| ICU LOS | 1.394 (1.310–1.484) | <.001 | 1.319 (1.258–1.383) | <.001a |
Separate models that control for sex, race, ethnicity, insurance type, age category, ISS, and GCS were estimated for each pediatric trauma outcome to produce the ARR. Boldface risk ratios indicate significance at P < .05. Unless otherwise specified, n = 108 062 for each model. CI, confidence interval; RR, risk ratio.
Results statistically significant after FDR adjustment (unadjusted results were not included in this calculation).
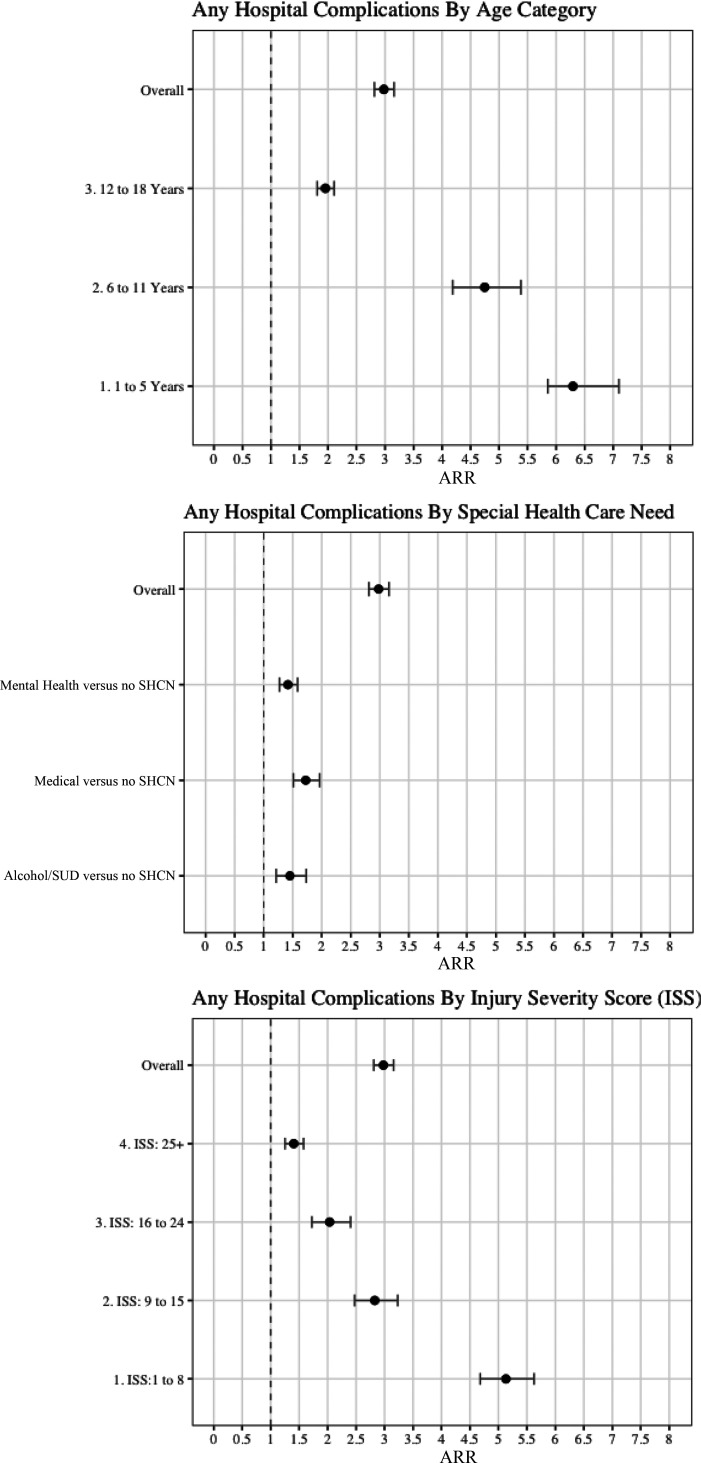
In subanalyses based on age, SHCN, and ISS categories, the risk of hospital complications in CYSHCN encounters relative to non-SHCN encounters was elevated in the younger age categories (P < .001) (Fig 2; Supplemental Table 8). CYSHCN encounters between the ages of 12 and 18 had a lower relative risk of in-hospital mortality (ARR = 0.850, P = .044). The risk of a longer hospital LOS increased by age category (P < .01) (Supplemental Table 8). Across the different SHCN categories, all indicated a greater risk of any hospital complications than encounters not reporting an SHCN: medical (ARR = 1.724, P < .001), mental health (ARR = 1.418, P < .001), and alcohol/SUD SHCN (ARR = 1.452, P = .001) (Fig 2) encounters. Compared with encounters without SHCN, encounters with alcohol/SUD had the greatest difference in ICU LOS (∼70% longer), followed by medical (∼40% longer) and mental health (∼30% longer) (all P < .001) (Supplemental Table 9). The risk of hospital complications in CYSHCN encounters relative to non-SHCN encounters increased as ISS decreased (P < .001) (Fig 2; Supplemental Table 10). This inverse relationship was also generally present for ICU LOS (P < .001) when comparing encounters with and without SHCN by ISS category (Supplemental Table 10). When using gross ISS categories (<25 as compared with 25), the ARR of any hospital complications was greater among the lower ISS group (3.763 vs 1.405, P < .001) (results not shown).
FIGURE 2.
Subanalyses, relative risk of hospital complications by SHCN status. Each data point represents the results from a separate logistic regression model that controls for sex, race, ethnicity, insurance type, and GCS. Age and SHCN models control for ISS; ISS and SHCN models control for age.
Sensitivity Analyses
We conducted sensitivity analyses to assess whether our method of treating missing data or other chronic conditions biased our results (results available upon request). We reestimated the models employing the missing data indicator method. The results presented did not differ in magnitude or direction on the basis of how missing data are handled. We reestimated the models to examine how changes in NTDB coding options for other chronic conditions could affect our findings by removing encounters who were coded as other or recoding other as no SHCN. Most of our results were comparable to our initial findings with a couple of exceptions, including the age pattern findings having the 1 to 5 year category with the highest ARR, followed by the 12 to 18 year category when using the recoding method.
To complement the subanalyses, we evaluated interaction effects of covariates with SHCN (results available upon request). The first model examined the conditional effects of increasing ISS on hospital complications by SHCN status. The second model examined the conditional effects of increasing age on hospital complications by SHCN status. In both models, the results were similar to the subanalyses.
Discussion
We found that CYSHCN encounters in the pediatric trauma system had a higher likelihood of experiencing any hospital complications, unplanned admission to the ICU, and longer hospital and ICU LOS compared with non-SHCN encounters. The differences were similar across type of SHCN, including medical, mental health, and alcohol/SUD, and were particularly pronounced for CYSHCN of younger age. Interestingly, CYSHCN encounters with lower ISS have a higher relative risk of hospital complications than non-SHCN encounters with injuries of similar severity. We did not find any statistically significant differences in in-hospital mortality when comparing CYSHCN and non-SHCN encounters. However, this may be because of insufficient power to detect differences for extremely rare events (<1% of encounters).
Our overall findings differ slightly from 2 comparable studies of pediatric trauma that use ACS data.12,14 Although we find that CYSHCN encounters have a greater risk of reporting a hospital complication, Traynor et al report a lower risk. In addition to the Traynor study focusing on behavioral health disorders, the complications tracked during 2018 were different from Traynor’s 2014–2016 time frame. Similar to the current study, both studies find that encounters reporting SHCN tend to have a longer hospital LOS.12,14 However, Grigorian et al find that the relationship between ADHD and ICU LOS was not statistically significant. This could be because their study does not include those with medical or alcohol/SUD SHCN, which we identified as having longer LOS.
The key question is whether poorer hospital outcomes among CYSHCN are related to their underlying condition(s), attributable to their trauma, or attributable to the hospitalization itself. First, underlying medical conditions may physiologically predispose these children to poorer posttrauma outcomes. For example, a child with a bleeding disorder may be predisposed to deep vein thrombosis (both this chronic condition and complication are tracked by the ACS). Yet, a higher hospital complications risk is present for those with mental health SHCN as well, where the physiologic link to hospital complications may not be as apparent. Second, it may be that hospital complications are attributable to the trauma sustained by CYSHCN, who may have different patterns of physical trauma than those without SHCN including intent and mechanism of injury.6 The elevated risk remained even after controlling for injury severity, so there may be aspects of the hospitalization that contribute to increased risk of complications.
These results suggest that CYSHCN of younger age with physical trauma fare particularly worse from a complications standpoint than their similarly aged peers without SHCN. In the pediatric trauma setting, each year of age decreases the odds of in-hospital complications,24 where the treatment of children has less room for error in general.25 Additionally, physiologic and anatomic features of younger children mean that more caution is needed when administering anesthesia or intubating the pediatric trauma patient.25
To our knowledge, this is the first study that identifies a disparity in hospital complications risk between children with and without SHCN with lower ISS. Identifying the underlying factors driving this finding is an important area for future study. A child with a lower ISS typically has an injury in 1 bodily region (Supplemental Table 5), whereas a child with a higher ISS typically has injuries with multisystem and likely more intensive care needs that may partly offset the complication risk posed by the SHCN. Less-severe trauma management may benefit from greater levels of awareness of the potential impact of the SHCN. For example, a systematic review of hospitalized children with autism spectrum disorder identified noncompliance, hyperactivity, sensory defensiveness, and self-injury behaviors as having the potential to interfere with care.26
Future studies will need to address clinical care pathways that address specific complications, including respiratory, renal, and postsurgical management, taking into account the heterogeneity of the CYSHCN population. Children with medical SHCN may benefit from comanagement from pediatric providers with expertise in managing chronic complex conditions, in addition to the trauma team. Children with mental health or developmental SHCN may benefit from additional psychosocial support to cope with factors such as the hospital environment and their injuries, because hospitalization alone can produce discomfort and stress.27 In examining this disparity, future studies should consider the role of care management decisions and the availability of psychosocial support by type of SHCN.
Limitations
There are some limitations associated with using the NTDB to study SHCN. Although the NTDB comes close to matching the National Survey of Children’s Health in terms of prevalence of CYSHCN (∼17% vs ∼19%), future studies should examine the reliability/validity of the NTDB’s identification strategy.6 The most common chronic condition indicated for pediatric trauma encounters in the 2018 NTDB was other.6 Unfortunately, there was no clear way to disaggregate this category. Trauma registrars must abide by strict criteria, and therefore we assumed that any chronic condition coded as other does signify an actual chronic condition but did not fit 1 of the ACS’s predefined conditions. For example, certain conditions such as asthma or learning disabilities are not listed as a specific coding option despite affecting at least 7% of US children aged 3 years and older.2 In our sensitivity analyses, we found that our results were somewhat dependent on the inclusion of other as a SHCN. Future studies should employ data that more specifically identifies SHCN to determine whether CYSHCN of younger age and lower ISS are indeed at greater risk of hospital complications after physical trauma.
The NTDB also has other data limitations. The included hospital complications cannot be broken down on the basis of hospital-acquired complications and complications because of trauma. The limited number of CYSHCN encounters reporting certain hospital complications meant that we could not estimate logistic regression models for this data (eg, unplanned return to the operating room). Finally, not all pediatric trauma centers submit their data to the NTDB, meaning that this study does not fit the definition of a population-based sample.
Conclusions
We examined the association between CYSHCN status, hospital outcomes, and LOS after trauma. CYSHCN encounters were more likely to report hospital complications and have longer hospital and ICU LOS. Additionally, less severely injured CYSHCN had a greater relative risk of reporting hospital complications than similarly injured children without SHCN. To address outcome disparities, particularly in CYSHCN with lower acuity injuries, future studies should identify aspects of pediatric trauma care management that can be improved and additional resources that may be needed.
Supplementary Material
Acknowledgments
We thank our family partners, Tondelaire Cottom, Jessica Colarusso, and Ali Perfetti, for their contributions to this research. We also thank Tiffany Fabiano, Arlene Brown, and Kathy Duke for their advisement. Finally, we thank the 2 anonymous reviewers from Children and Youth with Special Health Care Needs Research Network for their feedback on an earlier version of this article.
Footnotes
The data set used in this article is available by request to the American College of Surgeons.
Dr Lillvis conceptualized and designed this study, obtained the data and performed the statistical analysis, led the writing of the initial manuscript, and reviewed and revised the manuscript; Dr Sheehan contributed to the design of the study and data interpretation, helped draft the initial manuscript, and participated in the critical revision of the article; Dr Yu contributed to the study design and helped conduct and advise on statistical analysis, collaborated on the data interpretation, and participated in the critical revision of the article; Drs Noyes and Harmon contributed to the design of the study and data interpretation, and participated in the critical revision of the article; Dr Kuo supervised the conceptualization and design of the study, advised on statistical analysis, collaborated on the data interpretation, helped draft the initial manuscript, and participated in the critical revision of the article; and all authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
FUNDING: Research reported in this article was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health, under award KL2 TR001413-07. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The funder had no role in the design or conduct of this study. Two anonymous reviewers from Children and Youth with Special Health Care Needs Research Network provided comments on an earlier version of this article. This project is supported by the Health Resources and Services Administration (HRSA) of the U.S. Department of Health and Human Services (HHS) under UA6MC31101 Children with Special Health Care Needs Research Network. This information or content and conclusions are those of the author and should not be construed as the official position or policy of, nor should any endorsements be inferred by HRSA, HHS or the U.S. Government.
CONFLICT OF INTEREST DISCLOSURES: Dr Lillvis received funding for this research from the Health Resources and Services Administration through the Children and Youth with Special Health Care Needs Research Network, in addition to the KL2 TR001413-07 award referenced above. She and Dr Harmon also received funding support from the Oishei Children’s Hospital Foundation. Dr Noyes receives research funding from Roche Medical Devices, Pharmavite, and M&T Bank. All other authors have indicated they have no conflicts of interest relevant to this article to disclose.
References
- 1. McPherson M, Arango P, Fox H, et al. A new definition of children with special health care needs. Pediatrics. 1998;102(1 Pt 1):137–140 [DOI] [PubMed] [Google Scholar]
- 2. Child and Adolescent Health Measurement Initiative. 2018 National Survey of Children’s Health (NSCH) data query. Data Resource Center for Child and Adolescent Health supported by the U.S., Department of Health and Human Services, Health Resources and Services Administration (HRSA), Maternal and Child Health Bureau (MCHB). Available at: www.childhealthdata.org. Accessed February 1, 2021
- 3. Newacheck PW, Inkelas M, Kim SE. Health services use and health care expenditures for children with disabilities. Pediatrics. 2004;114(1):79–85 [DOI] [PubMed] [Google Scholar]
- 4. Bucholz EM, Toomey SL, Schuster MA. Trends in pediatric hospitalizations and readmissions: 2010–2016. Pediatrics. 2019;143(2):e20181958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Berry JG, Poduri A, Bonkowsky JL, et al. Trends in resource utilization by children with neurological impairment in the United States inpatient health care system: a repeat cross-sectional study. PLoS Med. 2012;9(1):e1001158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lillvis DF, Sheehan KM, Yu J, Noyes K, Bass KD, Kuo DZ. Characterizing physical trauma in children and youth with special health care needs. J Trauma Acute Care Surg. 2022;93(3):299–306 [DOI] [PubMed] [Google Scholar]
- 7. Morris JA Jr, MacKenzie EJ, Damiano AM, Bass SM. Mortality in trauma patients: the interaction between host factors and severity. J Trauma. 1990;30(12):1476–1482 [PubMed] [Google Scholar]
- 8. MacKenzie EJ, Morris JA Jr, Edelstein SL. Effect of preexisting disease on length of hospital stay in trauma patients. J Trauma. 1989;29(6):757–764, discussion 764–765 [DOI] [PubMed] [Google Scholar]
- 9. Miller CM, Shi J, Wheeler KK, et al. Chronic conditions and outcomes of pediatric trauma patients. J Trauma Acute Care Surg. 2013;75(2):250–257 [DOI] [PubMed] [Google Scholar]
- 10. Au AK, Carcillo JA, Clark RS, Bell MJ. Brain injuries and neurological system failure are the most common proximate causes of death in children admitted to a pediatric intensive care unit. Pediatr Crit Care Med. 2011;12(5):566–571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. DiScala C, Lescohier I, Barthel M, Li G. Injuries to children with attention deficit hyperactivity disorder. Pediatrics. 1998;102(6):1415–1421 [DOI] [PubMed] [Google Scholar]
- 12. Grigorian A, Nahmias J, Dolich M, et al. Increased risk of head injury in pediatric patients with attention deficit hyperactivity disorder. J Child Adolesc Psychiatr Nurs. 2019;32(4):171–176 [DOI] [PubMed] [Google Scholar]
- 13. Nguyen QP, Saynina O, Pirrotta EA, Huffman LC, Wang NE. A retrospective observational cohort study: epidemiology and outcomes of pediatric unintentional falls in US emergency departments. Injury. 2021;52(8):2244–2250 [DOI] [PubMed] [Google Scholar]
- 14. Traynor MD Jr, Watkins RD, Zielinski MD, et al. Postinjury outcomes of children with behavioral health disorders. J Pediatr Surg. 2022;57(3):462–468 [DOI] [PubMed] [Google Scholar]
- 15. Alber DA, Dalton MK, Uribe-Leitz T, et al. A multistate study of race and ethnic disparities in access to trauma care. J Surg Res. 2021;257:486–492 [DOI] [PubMed] [Google Scholar]
- 16. Committee on Trauma. NTDB Annual/Pediatric Report 2016. Chicago, IL: American College of Surgeons, 2016 [Google Scholar]
- 17. Hakmeh W, Barker J, Szpunar SM, Fox JM, Irvin CB. Effect of race and insurance on outcome of pediatric trauma. Acad Emerg Med. 2010;17(8):809–812 [DOI] [PubMed] [Google Scholar]
- 18. Haider AH, Weygandt PL, Bentley JM, et al. Disparities in trauma care and outcomes in the United States: a systematic review and meta-analysis. J Trauma Acute Care Surg. 2013;74(5):1195–1205 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Sanchez C, Shaikh S, Dowd B, Santos R, McKenney M, Elkbuli A. Disparities in adult and pediatric trauma outcomes: a systematic review and meta-analysis. World J Surg. 2020;44(9):3010–3021 [DOI] [PubMed] [Google Scholar]
- 20. Committee on Trauma. 2018 admissions. In: American College of Surgeons, ed. National Trauma Data Standard Data Dictionary. Committee on Trauma. National Trauma Data Standard Data Dictionary 2018 Admissions. Chicago, IL: American College of Surgeons; 2018 [Google Scholar]
- 21. Norton EC, Miller MM, Kleinman LC. Computing adjusted risk ratios and risk differences in Stata. Stata J. 2013;13(3):492–509 [Google Scholar]
- 22. VanDerHaden N, Thomas B. Chapter 6: Trauma scoring. In: Current Therapy of Trauma and Surgical Critical Care. Philadephia, PA: Mosby; 2008:26–32 [Google Scholar]
- 23. Groenwold RH, White IR, Donders AR, Carpenter JR, Altman DG, Moons KG. Missing covariate data in clinical research: when and when not to use the missing-indicator method for analysis. CMAJ. 2012;184(11):1265–1269 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Khalil M, Alawwa G, Pinto F, O’Neill PA. Pediatric mortality at pediatric versus adult trauma centers. J Emerg Trauma Shock. 2021;14(3):128–135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Russell K, Biswas S. Pediatric trauma center versus adult trauma center: which is better? Curr Opin Anaesthesiol. 2023;36(2):159–162 [DOI] [PubMed] [Google Scholar]
- 26. Johnson NL, Rodriguez D. Children with autism spectrum disorder at a pediatric hospital: a systematic review of the literature. Pediatr Nurs. 2013;39(3):131–141 [PubMed] [Google Scholar]
- 27. Tavakoli P, Cheraghi MA, Jahani S, Asadizaker M. Experience of discomfort and its self-management strategies in ICU patients. J Family Med Prim Care. 2022;11(1):269–276 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.