Abstract
Background
For patients with self-harm behaviors, the urge to hurt themselves persists after hospital discharge, leading to costly readmissions and even death. Hence, postdischarge intervention programs that reduce self-harm behavior among patients should be part of a cogent community mental health care policy.
Objective
We aimed to determine whether a combination of a self-help mobile app and volunteer support could complement treatment as usual (TAU) to reduce the risk of suicide among these patients.
Methods
We conducted a pragmatic randomized controlled trial on discharged patients aged between 18 and 45 years with self-harm episodes/suicide attempts, all of whom were recruited from 4 hospital emergency departments in Hong Kong. Participants were randomly assigned to one of three groups: (1) mobile app + TAU (“apps”), (2) mobile app + volunteer support + TAU (“volunteers”), or (3) TAU only as the control group (“TAU”). They were asked to submit a mobile app–based questionnaire during 4 measurement time points at monthly intervals.
Results
A total of 40 participants were recruited. Blending volunteer care with a preprogrammed mobile app was found to be effective in improving service compliance. Drawing upon the interpersonal-psychological theory of suicide, our findings suggested that a reduction in perceived burdensomeness and thwarted belongingness through community-based caring contact are linked to improvement in hopelessness, albeit a transient one, and suicide risk.
Conclusions
A combination of volunteer care with a self-help mobile app as a strategy for strengthening the continuity of care can be cautiously implemented for discharged patients at risk of self-harm during the transition from the hospital to a community setting.
Trial Registration
ClinicalTrials.gov NCT03081078; https://clinicaltrials.gov/study/NCT03081078
Keywords: self-harm, suicidal ideation, volunteers, mobile app, thwarted belongingness, suicide, youth, community, support, treatment, effectiveness, risk, patient, intervention, model, care, hospital
Introduction
Background
Among the 127,801 self-harm records identified from January 1, 2002, to December 31, 2016, in the inpatient units of Hong Kong emergency departments, an alarming 22.45% were readmissions [1]. The greatest risk was observed within the same year of the index self-harm episode, regardless of gender or age [1]. These findings suggest that postdischarge patients with self-harm behaviors may require additional community-based interventions to complement usual care. Clinical trials have shown follow-up contact with such patients significantly reduces self-harm repetition. Some studies have also examined the mechanism by which caring contact as a form of engagement potentially leads to a reduction in suicidal behavior [2-4], but the evidence remains inconclusive [5-7].
The interpersonal-psychological theory of suicide (IPTS) provides a theoretical explanation, positing that social connectedness and assurance buffer against perceived loneliness and burdensomeness, which are closely related to hopelessness and suicidal behaviors [8-11]. It suggests that low thwarted belongingness (TB, “I am alone”) and perceived burdensomeness (PB, “I am a burden”) induce suicide [10].
There is an intrinsic value in ascertaining a community-based intervention that is based on the 3 IPTS-related concepts in reducing suicide risks among discharged individuals, especially when it has never been done before. In particular, we hypothesized that community-based interventions that increase TB and PB will reduce suicide risk among patients who receive only treatment as usual (TAU). TAU was prescribed by the hospitals as per individual patients’ medical conditions, which may include psychiatric outpatient follow-up, medication, and psychosocial interventions related to the index self-harm episode.
In this study, 2 community-based interventions were tested. One intervention relied on mobile apps to deliver programmed care for mental health care purposes. Previous studies have examined the efficacy of mobile apps on mental illness management and the prevention of behavioral problems, as well as their use as interventions aimed at reducing depression, anxiety, and substance use in randomized controlled trials (RCTs) [12]. Although the results are mixed, they can still be used to facilitate evidence-based self-monitoring [13]. The second intervention combines programmed care on a mobile app and personalized care delivered by trained volunteers. Volunteers are vital in the suicide prevention pipeline, fielding crisis calls and providing emotional support to callers from around the world since the 1950s [14-17], and they continued to feature prominently during the COVID-19 pandemic [18]. Unlike boilerplate responses from mobile apps, the human element in personalized care is better received by people in emotional distress, which could be key to reducing levels of hopelessness among individuals who practice or are at risk of self-harm. However, owing to several methodological issues, particularly a lack of rigorous hypothesis testing research, the effects of volunteer care or peer support in suicide prevention have yet to be conclusively defined [16,19].
Aims
This study aimed to determine the efficacy of complementary community-based caring contact via a mobile app regardless of volunteer support to TAU (psychiatric and psychosocial treatments) in reducing the suicide risk among postdischarge young adults practicing self-harm. This study also aimed to suggest tools supported by empirical evidence to engage and support this high-risk group who often default on prescribed treatments. The anticipated effects were hypothesized as a reduction in interpersonal relationship-state TB and PB, hopelessness, and suicide risk in patients aged between 18 and 45 years with self-harm episodes or suicide attempts discharged from the emergency departments of 4 local hospitals. They were also expected to exhibit an improvement in self-reported compliance with treatment.
Methods
Overview
This study took the form of a pragmatic RCT examining the effects of community-based caring contact via a mobile app regardless of volunteer support relative to TAU on young adults with self-harm behaviors. After providing informed written consent for participation, participants were randomly assigned to 1 of 3 groups for a 3-month observation period: (1) mobile app + TAU (“apps”), (2) mobile app + volunteer support + TAU (“volunteers”), or (3) TAU only as the control group (“TAU”). The intervention period spanned between T0 and T2. Group assignments were based on a pregenerated sequence returned by the pseudorandom generator. Each participant was asked to complete a questionnaire at each of the 4 measurement time points (T0 = baseline; T1 = 1 month; T2 = 2 months; T3 = 3 months after T0 (post intervention). All participants completed the baseline questionnaire during a face-to-face interview with a research team member around hospital discharge, with the rest self-administered via a mobile app. Incentives were offered for every completed questionnaire.
Participants
An International Classification of Disease 10th revision (ICD-10)–based definition was used to encompass individuals with an index episode of self-poisoning or self-injury regardless of suicide intent (ie, X60 to X84 and R45.8) [20,21]. Other inclusion criteria were (1) 18 to 45 years of age, (2) admission to the emergency departments of any of the 4 public general hospitals, and (3) approval from a psychiatrist or psychiatric nurse. Young adults were targeted for their digital proficiency and altruism, which makes them less likely to turn down volunteer-initiated contact [22]. The exclusion criteria were (1) any DSM IV-TR (Diagnostic and Statistical Manual of Mental Disorders, 4th Edition, Text Revision) Axis II personality disorder and (2) severe psychotic mental illness or bipolar disorder because patients with these diagnoses may be too demanding for lay volunteers to deal with. Among the 156 referrals given, 1 was a duplicate referral, and 46 potential candidates explicitly turned down the invitation. Another 43 failed to meet the inclusion criteria, and 26 people failed to show up to the study after giving (verbal) consent. The remaining 40 referrals signed a consent to participate in this study. Figure 1 contains a more detailed breakdown of the recruitment process.
Figure 1.
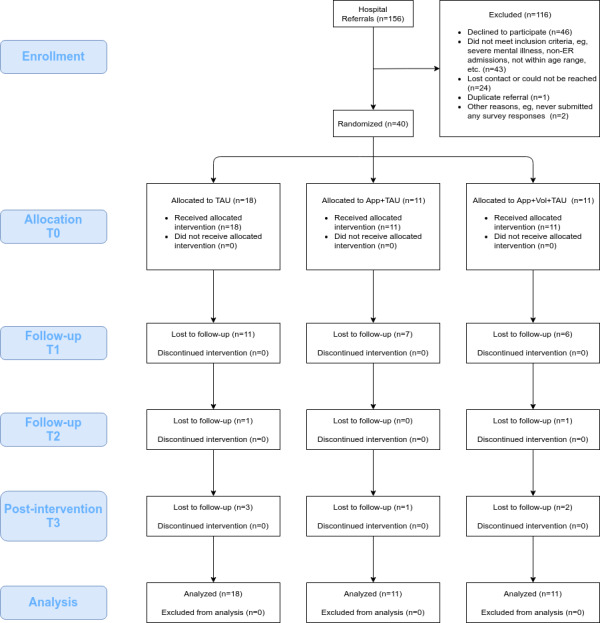
CONSORT (Consolidated Standards of Reporting Trials) flow diagram of research participant recruitment. ER: emergency room; TAU: treatment as usual.
Procedures
Admitted patients were subjected to the standard of care in emergency departments before they went through the vetting process that identified them as potential participants. Patients who met the inclusion and exclusion criteria were notified and briefed on the study by a research team member. Then, they were asked to sign a written informed consent to participate in this study. Immediately upon giving consent, the participants downloaded the app onto their mobile devices and completed a baseline questionnaire. Group assignments and corresponding interventions were given via the app. Grocery gift coupons were offered as incentives for every questionnaire completed thereafter.
Mobile App Features
The main pages of the mobile app were positive quotes/messages displayed on the home page, a mental health information library, emergency information including the number of a 24-hour suicide prevention hotline, a medical follow-up appointment reminder, a survey, a user feedback form, and, if applicable, volunteer support services (Table 1).
Table 1.
Components of mobile app and volunteer interventions focusing on reducing TBa and PBb.
| IPTSc components | TB | PB | ||||
| Aims of intervention |
|
|
||||
| Programmed | ||||||
|
|
Mobile app |
|
|
|||
| Personalized | ||||||
|
|
Volunteer support (at least 2 contacts per month made by volunteers for each assigned participant) |
|
|
|||
| Personalized additional components as a safety measure | ||||||
|
|
Suicide risk screening through simple questions (ie, ask and refer) report crisis to the research team |
|
|
|||
aPB: perceived burdensomeness.
bTB: thwarted belongingness.
cIPTS: interpersonal-psychological theory of suicide.
dN/A: not applicable.
Volunteer Support
Volunteers aged 25 years or above with at least a bachelor’s degree were recruited and asked to attend six 3-hour training sessions on basic knowledge of suicide prevention, suicide risk screening skills, empathetic communication skills, and other topics. A similar intervention was examined in a pilot study and found to be effective in reducing depressive symptoms and hopelessness [16]. Volunteers who completed the training and met the assessment criteria were invited to take part in this study. They were paired up with other participants of the “volunteers” group and made first contact within 24 hours. Volunteers’ duties included initiating at least 2 contacts per week with the assigned patients, having at least 1 monthly meetup, conducting suicide risk screening, and sending supportive messages and reminders of follow-up treatment. They were also required to report back on the patients’ progress and attend in-service training and supervision sessions (Table 1). Among the 85 volunteers who applied, 29 (34%) were selected to join the training sessions. Of those, 17 (59%) completed the training and committed to a service contract with a list of duties and promised to comply with ethical practices. A total of 11 (28%) participants were successfully paired with trained volunteers.
Measurements
The expected outcomes were a reduction in suicidal ideation, hopelessness, TB, and PB total scores and an increase in compliance with professional help. Suicidal ideation was measured by the self-report Chinese version of the 4-item short-form Adult Suicidal Ideation Questionnaire (ASIQ4) adapted from the full-form Adult Suicidal Ideation Questionnaire (ASIQ), which has been demonstrated to exhibit a modest level of sensitivity (64%) and superior specificity (76%), as well as a positive predictive value of 8.4% on nonfatal suicidality and suicide deaths at a cut-off of 1 [23]. Hopelessness was measured by the self-report 4-item short-form Beck Hopelessness Scale (BHS4) [24], which was tested in a local panel survey [25] based on the Chinese version developed by Shek [26]. The BHS4 is highly correlated (0.88) with the long-form Beck Hopelessness Scale (BHS), and its area under the curve (95% CI 0.65-0.75) is as strong as that of the BHS in identifying people with suicidal ideation. The cut-off score of 11 for suicidal ideation provides 65.8% sensitivity and 67.3% specificity [25]. TB and PB were assessed by the Interpersonal Needs Questionnaire (INQ), a 15-item measure of beliefs about whether one’s need to belong is met or unmet and self-perceptions of being a burden to others. Each item is rated on a 7-point Likert scale, with higher scores indicating higher levels of TB and PB [11]. Self-reported compliance with prescribed treatment (frequency) in relation to the index self-harm episode, including psychiatric follow-up care (eg, medication, outpatient follow-up treatment, and community psychiatric nursing service) and psychosocial services (eg, “formal help” provided by clinical psychology service, medical social work service), as well as obtaining “informal help” from families and friends, was measured by a self-developed service utilization checklist. Depressive state was treated as a covariate and measured by the Center for Epidemiological Studies Depression Scale (CESD) [27]. CESD scores measured by 2 factors, an affective and somatic symptom factor and an interpersonal problem factor that patients encountered in the past week, were controlled in growth models. The a priori estimated sample size for each group was 36, with projected retention rates of 80%, 70%, and 60% at T1, T2, and T3, respectively, a 2-sided significance level (α) of 0.05, and a statistical power (1-β) of 0.8 [28]. Participants were assigned to groups by simple random sampling.
Data Analysis
Chi-square (categorical variables) and Kruskal-Wallis (continuous variables) tests at a significance level of P<.05 were performed to detect differences in the distribution of the key variables, (ie, age, sex, hospital, and depressive state) among the 3 groups. Correlations among the measurements were also tested at T0 to verify their association with each other at baseline. Compliance was a binary variable coded in terms of true (1) if the participant reported seeking informal or formal help and false (0) otherwise. An intention-to-treat (ITT) analysis was conducted to compare the participants in all groups, including those who did not comply with the assigned interventions and dropouts, to ensure that all groups remained the same apart from random variation, with the specific purpose of not overestimating the effects of interventions in a pragmatic trial [29]. Following the ITT approach outlined in [30], all cases with only the baseline record (n=21, 52%) available were selectively imputed as if they were in the “TAU” (control) group. Due to the large rates of attrition, group results were analyzed graphically in a manner similar to single-subject research design plots, and the effects were visually inspected. Python (Python Software Foundation) libraries pandas (version 1.4.3), missingpy (version 0.2.0), and scikit-learn (version 0.24.2) were used for all data analyses, and seaborn (version 0.11.1) was used to visualize the data.
Ethics Approval
This study was approved by the Institutional Review Boards of the Hospital Authority Research Ethics Committee across 4 public hospitals: North District Hospital (ref 2016.155-T), Pamela Youde Nethersole Eastern Hospital (ref HKECREC-2017-002), Queen Mary Hospital (ref UW 16-181) and United Christian Hospital (ref KC/KE-16-0027/FR). The study was registered with the US National Institutes of Health Clinical Trials Registry (NCT03081078). Regarding ethical approval, we are also bound to observe and comply with all applicable requirements under the Hospital Authority’s standard operating procedure, the Declaration of Helsinki, and, if applicable, the International Conference on Harmonization of Technical Requirements for Pharmaceuticals for Human Use Guideline for Good Clinical Practice (ICH-GCP).
Incentives were given as a token of appreciation. The maximum value of compensation allotted to each participant was HK $500 (roughly US $64), including an HK $200 (US $25) supermarket coupon for the baseline questionnaire submission and then an HK $100 (US$ 12.50) supermarket coupon for each returned follow-up questionnaire. Data that could be used to identify the participants were anonymized before data analysis.
Results
Descriptive Data of All Cases
A total of 40 participants aged between 18 and 45 years with an index episode of self-poisoning or self-injury, regardless of suicide intent, were recruited between 2018 and 2020 from 4 public hospitals. Participants were randomly assigned to 1 of 3 groups: TAU (n=18, 45%), “apps” (n=11, 28%), and “volunteers” (n=11, 28%). Recruitment at the emergency departments was periodically suspended in 2019 owing to social unrest and in 2020 in the wake of the COVID-19 pandemic, which led to a small sample size with a higher number of participants in the TAU group and a high attrition rate between 55% and 63% at T1. The overall attrition rate measured at the end of the intervention at T2 was between 33.3% and 36.4%. At T0, there were no significant differences among the groups in terms of age, sex, depressive symptoms measured by CESD, or attrition rates. Table 2 shows the age, sex, depressive symptoms, and group of all participants at the 4 time points, and Table 3 shows a descriptive summary of outcomes at 4 time points (as per the protocol). The psychometric responses received at all time points had good internal consistency, with Cronbach alpha values above 0.76, similar to the range reported in the prior literature. The correlations between the measurement scales were statistically significant (Table 4), except for that between hopelessness and PB, again confirming earlier findings in the literature. However, hopelessness was correlated with TB and the overall INQ, suggesting that hopelessness exhibited stronger interdependence with TB than PB.
Table 2.
Age, sex, depressive symptoms, and intervention group of all participants at the 4 time points.
| Characteristics | Time points | |||||||||
| T0 (n=40) | T1 (n=16) | T2 (n=14) | T3 (n=8) | |||||||
| Age (years), n (%) | ||||||||||
|
|
17-25 | 18 (45) | 9 (56) | 8 (57) | 5 (63) | |||||
|
|
26-45 | 22 (55) | 7 (46) | 6 (43) | 3 (38) | |||||
| Sex, n (%) | ||||||||||
|
|
Female | 29 (73) | 7 (44) | 9 (64) | 4 (50) | |||||
|
|
Male | 11 (28) | 9 (56) | 5 (36) | 4 (50) | |||||
| Intervention group |
|
|
|
|
||||||
|
|
Volunteer | 11 (28) | 5 (31) | 4 (29) | 2 (25) | |||||
|
|
App | 11 (28) | 4 (25) | 4 (28.6) | 3 (38) | |||||
|
|
TAUa | 18 (45) | 7(44) | 6 (43) | 3 (38) | |||||
| CESDb depressive symptoms, mean (SD) | 34 (8.3) | 29.8 (10.5) | 29.3 (11.9) | 33.4 (10.3) | ||||||
| Breakdown of total score by group, mean (SD) | ||||||||||
|
|
CESD | |||||||||
|
|
|
Volunteer | 37.6 (6.2) | 34.6 (6.7) | 34.8 (5.4) | 37.3 (9.6) | ||||
|
|
|
App | 35.2 (9.7) | 34.4 (9.5) | 37.3 (10.3) | 30.5 (2.1) | ||||
|
|
|
TAU | 31.2 (7.9) | 23 (9.6) | 20.3 (10.7) | 31.3 (15.5) | ||||
|
|
Age (years), mean (SD) | |||||||||
|
|
|
Volunteer | 25.9 (8.1) | 26.2 (10.2) | 25.7 (9.6) | 27.9 (8.6) | ||||
|
|
|
App | 29.7 (8.7) | 29 (9.3) | 29.9 (8.8) | 30.4 (8.8) | ||||
|
|
|
TAU | 29.4 (9) | 29.9 (10.3) | 30.3 (9.9) | 28.5 (8.7) | ||||
aTAU: treatment as usual.
bCESD: Center for Epidemiological Studies Depression Scale.
Table 3.
Descriptive summary of outcomes at the 4 time points.
| Components | Time points | ||||||||
| T0 | T1 | T2 | T3 | ||||||
| Total scores, mean (SD) | |||||||||
|
|
ASIQ4a | 12.5 (7.9) | 12 (8.1) | 10.1 (9.4) | 16.1 (9) | ||||
|
|
BHS4b | 14.2 (4.8) | 14.8 (5.5) | 14.4 (4.7) | 14.6 (5.5) | ||||
|
|
INQc | 60.5 (17.8) | 55.8 (19.1) | 53.9 (20.2) | 57.5 (23.4) | ||||
|
|
INQ-PBd | 21.3 (8.7) | 20.3 (11.2) | 18.1 (10) | 19.6 (10.2) | ||||
|
|
INQ-TBe | 39.2 (11.4) | 35.5 (13.5) | 35.9 (12.5) | 37.9 (16) | ||||
| Breakdown of total scores by group, mean (SD) | |||||||||
|
|
ASIQ4 | ||||||||
|
|
|
Volunteer | 10.7 (7) | 14.6 (8.2) | 6.8 (3.9) | 15 (11.5) | |||
|
|
|
App | 14.5 (8.1) | 13.5 (10.2) | 17 (11.5) | 21.5 (2.1) | |||
|
|
|
TAUf | 12.3 (8.5) | 9.3 (7) | 7.7 (9.4) | 13.7 (10.4) | |||
|
|
BHS4 | ||||||||
|
|
|
Volunteer | 14.4 (4.5) | 16.2 (5.4) | 16.3 (3.4) | 18 (7.2) | |||
|
|
|
App | 16 (5.1) | 16.8 (5.2) | 14.3 (4.6) | 11.5 (0.7) | |||
|
|
|
TAU | 12.9 (4.6) | 12.7 (5.4) | 13.2 (5.7) | 13.3 (5) | |||
|
|
INQ | ||||||||
|
|
|
Volunteer | 59.5 (17.1 | 57.8 (20.2) | 48.8 (17.5) | 65.3 (34.5) | |||
|
|
|
App | 63.6 (23.4) | 60.2 (23.7) | 60.5 (25.2) | 67 (11.3) | |||
|
|
|
TAU | 59.2 (14.9) | 52.1 (15.6) | 53 (20.9) | 43.3 (13.3) | |||
|
|
INQ-PB | ||||||||
|
|
|
Volunteer | 20.5 (8.8) | 24.8 (15.1) | 18.3 (8.5) | 21 (15) | |||
|
|
|
App | 21.9 (12.2) | 19.6 (11.2) | 21.8 (12) | 19.5 (0.7) | |||
|
|
|
TAU | 21.5 (6.3) | 17 (7.2) | 15.5 (10.5) | 18.3 (11.6) | |||
|
|
INQ-TB | ||||||||
|
|
|
Volunteer | 39.1 (9.8) | 33 (7.2) | 30.5 (11.2) | 44.3 (19.6) | |||
|
|
|
App | 41.7 (13.8) | 40.6 (17.8) | 38.8 (16.7) | 47.5 (12) | |||
|
|
|
TAU | 37.7 (11) | 35.1 (14.1) | 37.5 (11.5) | 25 (6.1) | |||
| Participants reporting service compliance by group, n (%) | |||||||||
|
|
Yes | ||||||||
|
|
|
Volunteer | 10 (91) | 4 (80) | 4 (100) | 2 (67) | |||
|
|
|
App | 9 (82) | 3 (75) | 3 (75) | 2 (100) | |||
|
|
|
TAU | 15 (83) | 2 (29) | 2 (33) | 1 (33) | |||
| Participants seeking professional consultation by group, n (%) | |||||||||
|
|
Yes | ||||||||
|
|
|
Volunteer | 9 (82) | 4 (80) | 4 (100) | 2 (67) | |||
|
|
|
App | 8 (73) | 3 (75) | 3 (75) | 2 (100) | |||
|
|
|
TAU | 13 (72) | 2 (29) | 2 (33) | 1 (33) | |||
| Participants seeking informal help by group, n (%) | |||||||||
|
|
Yes | ||||||||
|
|
|
Volunteer | 9 (82) | 3 (60) | 3 (75) | 1 (33) | |||
|
|
|
App | 7 (64) | 2 (50) | 3 (75) | 2 (100) | |||
|
|
|
TAU | 11 (61) | 2 (29) | 0 (0) | 1 (33) | |||
aASIQ4: 4-item short-form Adult Suicidal Ideation Questionnaire.
bBHS4: 4-item short-form Beck Hopelessness Scale.
cINQ: Interpersonal Needs Questionnaire.
dINQ-PB: Interpersonal Needs Questionnaire-Perceived Burdensomeness items.
eINQ-TB: Interpersonal Needs Questionnaire-Thwarted Belongingness items.
fTAU: treatment as usual.
Table 4.
Baseline Holm-Bonferroni—corrected Spearman correlations between measurement scales and subscales.
| Variable | ASIQ4a | BHS4b | CESDc | PBd | TBe | INQ-PB + TBf | |
| ASIQ4 | |||||||
| r | 1 | 0.475g | 0.546g | 0.646g | 0.48g | 0.686g | |
| P value | —h | .016 | .004 | .000 | .015 | .004 | |
| BHS4 | |||||||
| r | 0.475g | 1 | 0.605g | 0.375 | 0.567g | 0.555g | |
| P value | .016 | — | .001 | .086 | .003 | .004 | |
| CESD | |||||||
| r | 0.546g | 0.605g | 1 | 0.537g | 0.549g | 0.655g | |
| P value | .004 | .001 | — | .005 | .004 | <.001 | |
| PB | |||||||
| r | 0.646g | 0.375 | 0.537g | 1 | 0.496g | 0.865g | |
| P value | <.001 | .086 | .005 | — | .011 | <.001 | |
| TB | |||||||
| r | 0.48g | 0.567g | 0.549g | 0.496g | 1 | 0.848g | |
| P value | .015 | .003 | .004 | .011 | — | <.001 | |
| INQ-PB + TB | |||||||
| r | 0.686g | 0.555g | 0.655g | 0.865g | 0.848g | 1 | |
| P value | 0.004 | 0.004 | <.001 | <.001 | <.001 | — | |
aASIQ4: 4-item short-form Adult Suicidal Ideation Questionnaire.
bBHS4: 4-item short-form Beck Hopelessness Scale.
cCESD: Center for Epidemiological Studies Depression Scale.
dPB: perceived burdensomeness.
eTB: thwarted belongingness.
fINQ: Interpersonal Needs Questionnaire-Perceived Burdensomeness and Thwarted Belongingness items.
gThe correlation is significant at a significance level of P=.05.
h—: not applicable.
When the results are considered per protocol, for “volunteer” and “TAU” cases, none of the participants reported readmission to the hospital because of self-harm.
Primary Outcomes
The proportions of reported compliance with service treatment and the seeking of professional and informal help in the “app” and “volunteer” groups were much higher in general than that in the “TAU” group. After applying ITT (Figures 2-5), “app” only led to better improvement in hopelessness than either “TAU” or “volunteer” at time points T1 and T2, but it brought no noticeable improvement to ASIQ4 and INQ. However, between the same time interval, “volunteer” was effective in bringing down ASIQ4, BHS4, and INQ at rates equal to or better than “TAU.” Much of the change in “volunteer” INQ was due to a noticeable fall in PB scores and a gradual decline in TB scores relative to “app” and “TAU.” A larger sample size is needed to determine the effective size and ascertain the mediation effects in the interventions (ie, to verify the existence of causal pathway TB>BHS4>ASIQ4).
Figure 2.
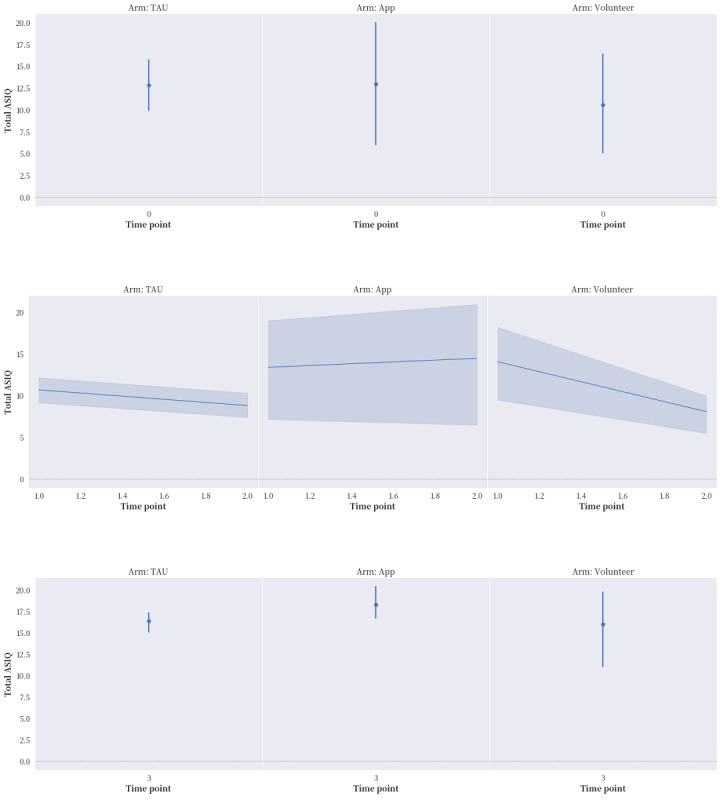
The effects of the intervention on the 4-item short-form Adult Suicidal Ideation Questionnaire (ASIQ4) at the 4 time points, with intention-to-treat (ITT) analysis applied. ASIQ: Adult Suicidal Ideation Questionnaire; TAU: treatment as usual.
Figure 5.
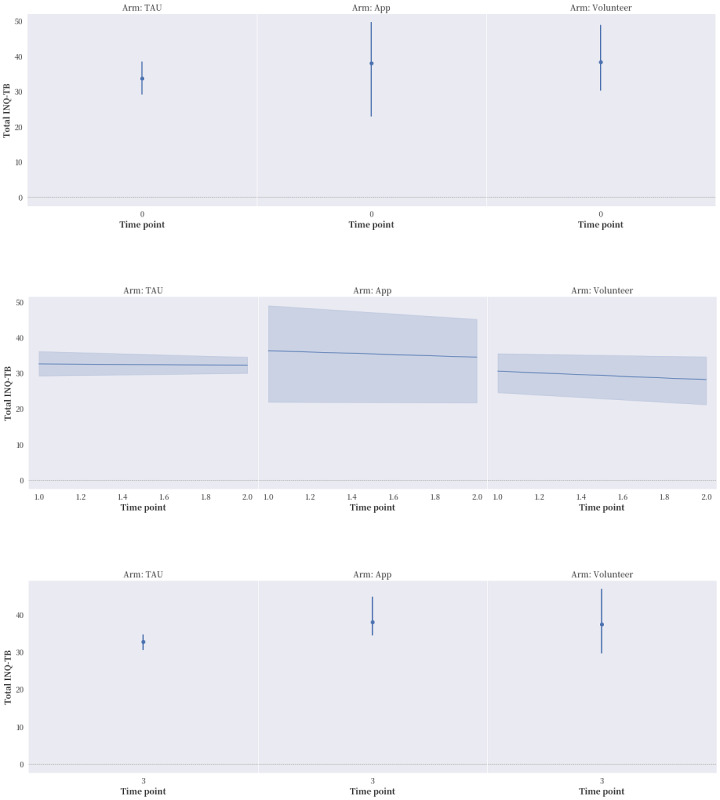
The effects of the intervention on Interpersonal Needs Questionnaire-Thwarted Belongingness items (INQ-TB) at the 4 time points with intention-to-treat (ITT) analysis applied. TAU: treatment as usual.
Figure 3.
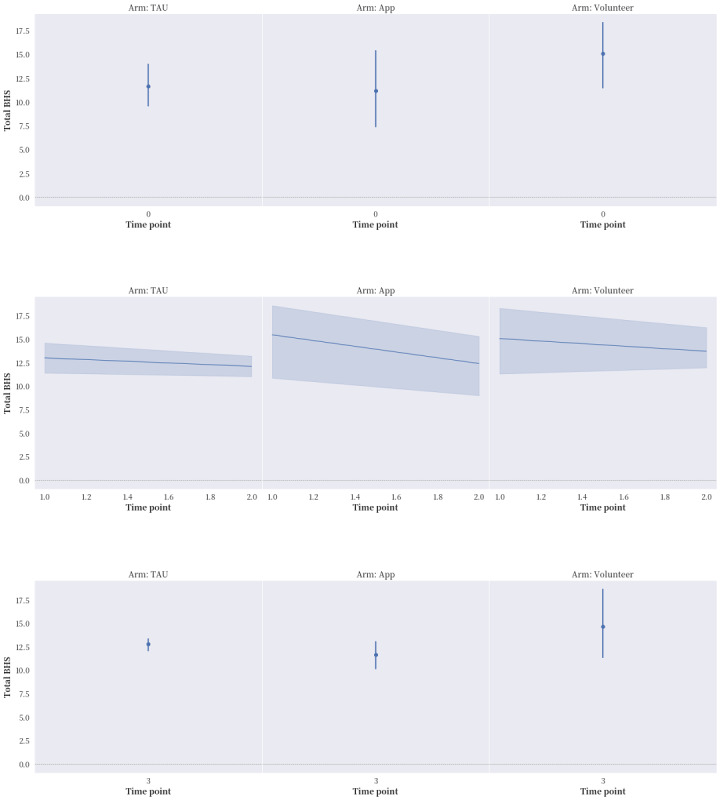
The effects of the intervention on 4-item short-form Beck Hopelessness Scale (BHS4) at the 4 time points, with intention-to-treat (ITT) analysis applied. BHS: Beck Hopelessness Scale; TAU: treatment as usual.
Figure 4.
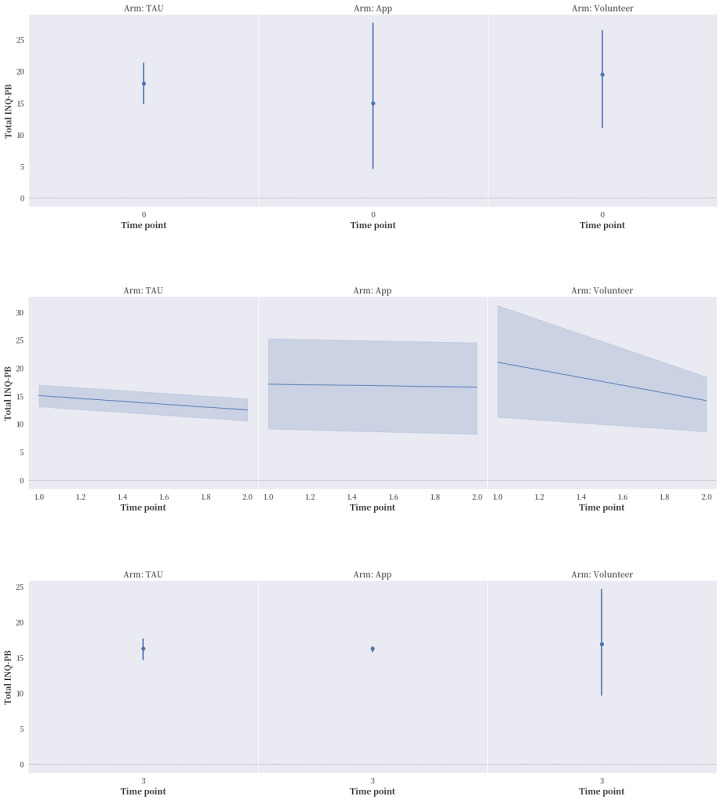
The effects of the intervention on Interpersonal Needs Questionnaire-Perceived Burdensomeness items (INQ-PB) at the 4 time points with intention-to-treat (ITT) analysis applied. TAU: treatment as usual.
Discussion
Principal Findings
The idea behind mixing volunteer care and a preprogrammed mobile app to engage discharged patients at the community level was to strengthen the continuity of care as a strategy to alleviate suicide risk through social connectedness and self-assurance, 2 categories of interpersonal needs. This contact was also expected to help them keep their standard medical follow-ups. The interventions were designed to address the aforementioned 2 categories of interpersonal needs with the aim of reducing patients’ sense of hopelessness as a predictor of suicidal ideation. The participating volunteers were stringently selected and trained to respond spontaneously based on human nature. The care scheme was piloted and tested [16] prior to the study, and the mobile app was preprogrammed to offer automated feedback to those in distress. Both interventions were well-structured, trial-run, and offered in a highly disciplined and ethical manner. No participant reported readmission to the hospital because of self-harm.
After applying ITT analysis, several important preliminary findings are particularly worthy of note. First, over time, both the “volunteer” and control groups reported an obvious improvement in suicidal ideation, whereas the “app” group did not. The ASIQ4 scores of all 3 groups bounced back to preintervention levels at T3 after the intervention period ended. Second, the control group reported worsened service compliance over time, whereas both the “volunteer” and “app” groups displayed improvement in this outcome during the intervention period. This finding is consistent with these participants’ efforts to seek professional consultation and informal help. Third, during the intervention period, all 3 groups reported improvement in interpersonal need fulfillment, but the “volunteer” group reported a more obvious and specific reduction in PB, as well as a gradual decline in TB. Fourth, the “app” group performed much better on the BHS4 across all the time points than the 2 other groups did. However, the “volunteer” group performed the best on suicidal ideation. Finally, despite the limitation of not being able to perform mediation analysis, the mixed volunteer plus app intervention seemed to produce the chain of effects theoretically hypothesized: from a reduction in INQ to hopelessness and then possibly to suicidal ideation. As can be seen in Table 4, the correlations among all the measurement scales (ASIQ4, BHS4, INQ, and CESD) were statistically significant, with the exception of those between BHS4 and PB. However, BHS4 was correlated with TB and the overall INQ, suggesting that BHS4 had a stronger interdependence with TB than PB. Ma et al [31] reviewed 58 mainly cross-sectional studies testing the IPTS. PB was found to be more commonly tested, and more support was found for its effect on suicidal ideation than TB [31]. TB might play a unique role in this study, which concurs with the longitudinal survey of youths conducted by Roeder and Cole [32], who found that TB can predict both hopelessness and PB over time, whereas a combination of the 3 factors can predict suicidal ideation. In this study, the reductions in PB and TB were only achieved with volunteer involvement. The “volunteer” group also had improved hopelessness and suicidal ideation over the other 2 groups.
This study provides initial evidence supporting the safety and viability of an intervention that combines personalized care by volunteers with programmed care by a mobile app for engaging postdischarge young adults with self-harm behaviors on their pathway to care. The intervention offers promising effects in reducing feelings of hopelessness and suicide risk by addressing patients’ interpersonal need for belongingness, although these effects were not shown to be sustainable after intervention in this study. However, caring contact by nature is not meant to be therapeutic; rather, it is aimed at better engagement to help discharged patients weather the transition from clinical to community care [4].
More evidence on the use of apps to treat people with mental health issues has emerged in recent years, but it is not conclusive. For example, the use of an app as part of clinical treatment for suicide prevention was unexpectedly found to exert negative effects on suicide risk reduction in an adult clinical sample with mild-to-moderate symptoms of anxiety, depression, and adjustment disorders [33]. However, another app (LifeBuoy) with therapeutic elements was recently shown to reduce suicidal ideation to a moderate degree in a much larger community sample of young adults (N=455) [34].
In the “app” arm of this study, the preprogrammed mobile app itself (ie, without caring contact by human volunteers) provided distinct value in alleviating the sense of hopelessness among the participants, who belong to the digital generation. The app, albeit basic, offers a clear buffer to help people in distress feel a sense of connection and feel less desperate. This study thus validates the role of a mobile app with basic self-help features in alleviating a sense of loneliness and hopelessness, both of which are strong predictors of suicide risk [35].
The smartphone penetration rate in Hong Kong rose from 92.1% in 2020 to 92.9% in 2021 [22], with the rise particularly notable during the COVID-19 pandemic. Mobile apps have become part of people’s decision-making and problem-solving processes. For example, they were widely used for information-sharing, risk assessment, training, and self-management during the pandemic [36]. With such a wide reach and the ability to be offered at a very low cost, digital support seems to be a viable auxiliary for individuals at risk of suicide when standardized medical follow-up care is made available as a necessary component.
It must be noted, however, that even though the “app” group realized a clear reduction in hopelessness, it showed no improvement in suicidal ideation, whereas the “volunteer” group reported improvements across the whole spectrum (BHS4, ASIQ4, and INQ). These results suggest that care rendered by trained volunteers remains critical in leading to the desired outcome change. More importantly, the volunteers were found to cause no additional harm, which aligns with prior research on the effects of mental support offered by trained volunteers [16,37-40].
Volunteer support appeared to address interpersonal needs shortly after the intervention began, with a modest effect on TB at T1, which was 1 month after discharge from an emergency department. However, the alleviation of suicidal ideation and PB was not noticed until 2 months later at T2. Unlike a preprogrammed mobile app, human care requires sufficient time to build rapport, which is based primarily on mutual understanding and conducive feedback. It motivates people through warmth and spontaneity [19]. In this study, the blending of the 2 components worked very well, showing that they complement each other. Nevertheless, the bounce-back effect was obvious, suggesting that this type of caring contact is transient and reversible.
The control group reported steady improvements in suicidal ideation and depressive symptoms over time during the intervention period. Standard medical care at the emergency departments and medical follow-up as TAU ameliorated such symptoms and suicide risk substantially [40]. Standard care proved to benefit those patients at acute risk of suicide. Proper psychiatric assessments and medication prescriptions offered in a timely fashion and at regular intervals to patients with a suicide risk remain valuable and are necessary components of any intervention for people with self-harm with or without suicidal ideation.
Limitations
The social unrest in 2019 and the COVID-19 pandemic from 2020 onward took a heavy toll on this study, particularly given that the sole recruitment sites were hospitals. Although we adopted several measures to increase the case admission rate, including briefings with medical staff, the multiple outbreaks of COVID-19 between 2020 and 2021 resulted in the full suspension of research at hospital sites. This study’s sample size was thus suboptimal, limiting the external validity of its findings. The volunteer support intervention was also unexpectedly interrupted from time to time. Face-to-face contact was difficult to render during the aforementioned periods. Nevertheless, all the volunteers involved in the study offered their unfailing support to the participants and exercised incredible patience and care.
We are also aware of the fact that the length of the self-administered questionnaire could be a bit overwhelming to our participants, which could bias the results from one way to another. The outcomes could also have been impacted by the unblinded nature of this study. As a cross-check of the major psychometric items was in line with the results reported by the instrument authors, we could only assume the rest of their responses were also genuine.
Conclusions
The RCT reported in this paper suggested that a reduction in PB and TB through community-based caring contact, as a form of engagement, is possibly linked to improvements in hopelessness and suicide risk. In comparison with TAU, PB and TB played a role as an alleviating effect, albeit a transient one, in reducing the level of hopelessness, which is a strong predictor of suicide risk. This finding, as hypothesized by the IPTS as a theory of change, suggests that suicide risk can be improved by addressing the need for social connectedness, which is strongly correlated with hopelessness and suicidal ideation.
This study has provided preliminary evidence that illustrates the effectiveness of blending volunteer care with a preprogrammed mobile app as a strategy for strengthening the continuity of care to alleviate the risk of suicide. The alleviation of suicidal ideation cannot be achieved solely through computer-mediated support, with meaningful human interaction confirmed to exert a prospective effect on reducing such ideation over time. The combination of volunteer care with a mobile app should be explored in a larger study. When cautiously implemented, it will help discharged patients with self-harm transition from a hospital to a community setting.
Acknowledgments
This research was supported by the University Grants Committee (grant 27612816). The authors would like to thank all participants who joined this study. We would also like to express our sincere gratitude to Dr KL Law from North District Hospital and the liaison teams from Pamela Youde Nethersole Eastern Hospital and United Christian Hospital for their contribution to the case recruitment. We are also immensely grateful to Miss Chan Pik Ying and Mr Kwok Raymond for their research support. Finally, we thank Erika for the English language review.
Abbreviations
- ASIQ
Adult Suicidal Ideation Questionnaire
- ASIQ4
4-item short-form Adult Suicidal Ideation Questionnaire
- BHS
Beck Hopelessness Scale
- BHS4
4-item short-form Beck Hopelessness Scale
- CESD
Center for Epidemiological Studies Depression Scale
- DSM IV-TR
Diagnostic and Statistical Manual of Mental Disorders, 4th Edition, Text Revision
- ICD-10
International Classification of Disease, 10th revision
- ICH-GCP
International Conference on Harmonization of Technical Requirements for Pharmaceuticals for Human Use Guideline for Good Clinical Practice
- INQ
Interpersonal Needs Questionnaire
- INQ-PB
Interpersonal Needs Questionnaire-Perceived Burdensomeness items
- INQ-TB
Interpersonal Needs Questionnaire-Thwarted Belongingness items
- IPTS
interpersonal-psychological theory of suicide
- ITT
intention to treat
- PB
perceived burdensomeness
- RCT
randomized controlled trial
- TAU
treatment as usual
- TB
thwarted belongingness
CONSORT-eHEALTH checklist (V 1.6.1).
Data Availability
The data sets generated and/or analyzed during this study are not publicly available due to the limitations set by the University of Hong Kong Human Research Ethics Committee, but they are available from the corresponding author on reasonable request. The submission of a Data Access Request Form is required.
Footnotes
Conflicts of Interest: None declared.
References
- 1.Chai Y, Luo H, Yip PS. Prevalence and risk factors for repetition of non-fatal self-harm in Hong Kong, 2002-2016: A population-based cohort study. Lancet Reg Health West Pac. 2020 Sep;2:100027. doi: 10.1016/j.lanwpc.2020.100027. https://linkinghub.elsevier.com/retrieve/pii/S2666-6065(20)30027-4 .S2666-6065(20)30027-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dimeff LA, Jobes DA, Chalker SA, Piehl BM, Duvivier LL, Lok BC, Zalake MS, Chung J, Koerner K. A novel engagement of suicidality in the emergency department: Virtual collaborative assessment and management of suicidality. Gen Hosp Psychiatry. 2020 Mar;63:119–126. doi: 10.1016/j.genhosppsych.2018.05.005.S0163-8343(18)30088-4 [DOI] [PubMed] [Google Scholar]
- 3.Luxton DD, June JD, Comtois KA. Can postdischarge follow-up contacts prevent suicide and suicidal behavior? A review of the evidence. Crisis. 2013 Jan 01;34(1):32–41. doi: 10.1027/0227-5910/a000158.7665358R64R15551 [DOI] [PubMed] [Google Scholar]
- 4.Milner AJ, Carter G, Pirkis J, Robinson J, Spittal MJ. Letters, green cards, telephone calls and postcards: Systematic and meta-analytic review of brief contact interventions for reducing self-harm, suicide attempts and suicide. Br J Psychiatry. 2018 Jan 02;206(3):184–190. doi: 10.1192/bjp.bp.114.147819. [DOI] [PubMed] [Google Scholar]
- 5.Simon GE, Shortreed SM, Rossom RC, Beck A, Clarke GN, Whiteside U, Richards JE, Penfold RB, Boggs JM, Smith J. Effect of offering care management or online dialectical behavior therapy skills training vs usual care on self-harm among adult outpatients with suicidal ideation: a randomized clinical trial. J Am Med Assoc. 2022 Feb 15;327(7):630–638. doi: 10.1001/jama.2022.0423. https://europepmc.org/abstract/MED/35166800 .2789028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vaiva G, Berrouiguet S, Walter M, Courtet P, Ducrocq F, Jardon V, Larsen M, Cailhol L, Godesense C, Couturier C, Mathur A, Lagree V, Pichene C, Travers D, Lemogne C, Henry J, Jover F, Chastang F, Prudhomme O, Lestavel P, Gignac C, Duhem S, Demarty A, Mesmeur C, Bellivier F, Labreuche J, Duhamel A, Goldstein P. Combining postcards, crisis cards, and telephone contact into a decision-making algorithm to reduce suicide reattempt: a randomized clinical trial of a personalized brief contact intervention. J Clin Psychiatry. 2018 Sep 25;79(6) doi: 10.4088/JCP.17m11631.17m11631 [DOI] [PubMed] [Google Scholar]
- 7.Van Orden KA, Cukrowicz KC, Witte TK, Joiner TE. Thwarted belongingness and perceived burdensomeness: construct validity and psychometric properties of the Interpersonal Needs Questionnaire. Psychol Assess. 2012 Mar;24(1):197–215. doi: 10.1037/a0025358. https://europepmc.org/abstract/MED/21928908 .2011-21186-001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Joiner T.E. Why People Die by Suicide. Cambridge, MA and London, UK: Harvard University Press; 2005. [Google Scholar]
- 9.Joiner TE, Pettit JW, Walker RL, Voelz ZR, Cruz J, Rudd MD, Lester D. Perceived burdensomeness and suicidality: two studies on the suicide notes of those attempting and those completing suicide. J Soc Clin Psychol. 2002 Nov;21(5):531–545. doi: 10.1521/jscp.21.5.531.22624. [DOI] [Google Scholar]
- 10.Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, Joiner TE. The interpersonal theory of suicide. Psychol Rev. 2010 Apr;117(2):575–600. doi: 10.1037/a0018697. https://europepmc.org/abstract/MED/20438238 .2010-06891-010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Van Orden KA, Bower E, Lutz J, Silva C, Gallegos AM, Podgorski CA, Santos EJ, Conwell Y. Strategies to promote social connections among older adults during "social distancing" restrictions. Am J Geriatr Psychiatry. 2021 Aug;29(8):816–827. doi: 10.1016/j.jagp.2020.05.004. https://europepmc.org/abstract/MED/32425473 .S1064-7481(20)30333-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lecomte T, Potvin S, Corbière M, Guay S, Samson C, Cloutier B, Francoeur A, Pennou A, Khazaal Y. Mobile apps for mental health issues: meta-review of meta-analyses. JMIR Mhealth Uhealth. 2020 May 29;8(5):e17458. doi: 10.2196/17458. https://mhealth.jmir.org/2020/5/e17458/ v8i5e17458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Witt K, Spittal MJ, Carter G, Pirkis J, Hetrick S, Currier D, Robinson J, Milner A. Effectiveness of online and mobile telephone applications ('apps') for the self-management of suicidal ideation and self-harm: a systematic review and meta-analysis. BMC Psychiatry. 2017 Aug 15;17(1):297. doi: 10.1186/s12888-017-1458-0. https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-017-1458-0 .10.1186/s12888-017-1458-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gould MS, Kalafat J, HarrisMunfakh JL, Kleinman M. An evaluation of crisis hotline outcomes part 2: suicidal callers. Suicide Life-Threat Behav. 2010 Dec 31;37(3):338–352. doi: 10.1521/suli.2007.37.3.338. [DOI] [PubMed] [Google Scholar]
- 15.Kalafat J, Gould MS, Munfakh JLH, Kleinman M. An evaluation of crisis hotline outcomes. Part 1: Nonsuicidal crisis callers. Suicide Life-Threat Behav. 2007 Jun 31;37(3):322–37. doi: 10.1521/suli.2007.37.3.322. [DOI] [PubMed] [Google Scholar]
- 16.Law Y, Yip PSF, Lai CCS, Kwok CL, Wong PWC, Liu K, Ng PWL, Liao CWM, Wong T. A pilot study on the efficacy of volunteer mentorship for young adults with self-harm behaviors using a quasi-experimental design. Crisis. 2016 Nov;37(6):415–426. doi: 10.1027/0227-5910/a000393. [DOI] [PubMed] [Google Scholar]
- 17.Shaw FF, Chiang W. An evaluation of suicide prevention hotline results in Taiwan: Caller profiles and the effect on emotional distress and suicide risk. J Affect Disord. 2019 Feb 01;244:16–20. doi: 10.1016/j.jad.2018.09.050.S0165-0327(18)31024-3 [DOI] [PubMed] [Google Scholar]
- 18.Vattøe IE, DeMarinis V, Haug SHK, Lien L, Danbolt LJ. Emotional stressors among volunteers operating a diaconal suicide-prevention crisis line in Norway: a qualitative study. Br J Guid Couns. 2019 Jul 25;48(4):563–575. doi: 10.1080/03069885.2019.1646409. [DOI] [Google Scholar]
- 19.Bowersox NW, Jagusch J, Garlick J, Chen JI, Pfeiffer PN. Peer-based interventions targeting suicide prevention: A scoping review. Am J Community Psychol. 2021 Sep 15;68(1-2):232–248. doi: 10.1002/ajcp.12510. https://europepmc.org/abstract/MED/33720444 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ougrin D, Tranah T, Stahl D, Moran P, Asarnow JR. Therapeutic interventions for suicide attempts and self-harm in adolescents: systematic review and meta-analysis. J Am Acad Child Adolesc Psychiatry. 2015 Feb;54(2):97–107.e2. doi: 10.1016/j.jaac.2014.10.009.S0890-8567(14)00731-X [DOI] [PubMed] [Google Scholar]
- 21.International statistical classification of diseases and related health problems, 10th revision. World Health Organization. 2016. [2017-03-15]. https://apps.who.int/iris/handle/10665/246208 .
- 22.Thematic household Survey Report No. 75. Census and Statistics Department, Hong Kong Special Administrative Region. [2022-12-15]. https://www.ogcio.gov.hk/en/about_us/facts/doc/THS_Report_No_75.pdf .
- 23.Fu K, Liu KY, Yip PSF. Predictive validity of the Chinese version of the Adult Suicidal Ideation Questionnaire: psychometric properties and its short version. Psychol Assess. 2007 Dec;19(4):422–9. doi: 10.1037/1040-3590.19.4.422.2007-18415-005 [DOI] [PubMed] [Google Scholar]
- 24.Beck AT, Weissman A, Lester D, Trexler L. The measurement of pessimism: the hopelessness scale. J Consult Clin Psychol. 1974 Dec;42(6):861–5. doi: 10.1037/h0037562. [DOI] [PubMed] [Google Scholar]
- 25.Yip PS, Cheung YB. Quick assessment of hopelessness: a cross-sectional study. Health Qual Life Outcomes. 2006 Mar 01;4(1):13. doi: 10.1186/1477-7525-4-13. https://hqlo.biomedcentral.com/articles/10.1186/1477-7525-4-13 .1477-7525-4-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shek DTL. Measurement of pessimism in Chinese adolescents: The Chinese Hopelessness Scale. Soc Behav Pers. 1993 Jan 01;21(2):107–119. doi: 10.2224/sbp.1993.21.2.107. [DOI] [Google Scholar]
- 27.Cheung C, Bagley C. Validating an American scale in Hong Kong: the Center for Epidemiological Studies Depression Scale (CES-D) J Psychol. 1998 Mar 02;132(2):169–86. doi: 10.1080/00223989809599157. [DOI] [PubMed] [Google Scholar]
- 28.Lu K, Luo X, Chen P-Y. Sample size estimation for repeated measures analysis in randomized clinical trials with missing data. Int J Biostat. 2008;4(1):Article 9. doi: 10.2202/1557-4679.1098. https://www.degruyter.com/document/doi/10.2202/1557-4679.1098 . [DOI] [PubMed] [Google Scholar]
- 29.Hollis S, Campbell F. What is meant by intention to treat analysis? Survey of published randomised controlled trials. BMJ. 1999 Sep 11;319(7211):670–4. doi: 10.1136/bmj.319.7211.670. https://europepmc.org/abstract/MED/10480822 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Twisk JW, Rijnhart JJ, Hoekstra T, Schuster NA, Ter Wee MM, Heymans MW. Intention-to-treat analysis when only a baseline value is available. Contemp Clin Trials Commun. 2020 Dec;20:100684. doi: 10.1016/j.conctc.2020.100684. https://linkinghub.elsevier.com/retrieve/pii/S2451-8654(20)30168-X .S2451-8654(20)30168-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ma J, Batterham PJ, Calear AL, Han J. A systematic review of the predictions of the Interpersonal-Psychological Theory of Suicidal Behavior. Clin Psychol Rev. 2016 Jun;46:34–45. doi: 10.1016/j.cpr.2016.04.008.S0272-7358(15)30174-4 [DOI] [PubMed] [Google Scholar]
- 32.Roeder KM, Cole DA. Simultaneous longitudinal examination of hopelessness, thwarted belongingness, and perceived burdensomeness as predictors of suicide ideation. Suicide Life Threat Behav. 2019 Aug 11;49(4):1058–1071. doi: 10.1111/sltb.12508. [DOI] [PubMed] [Google Scholar]
- 33.O'Toole MS, Arendt MB, Pedersen CM. Testing an app-assisted treatment for suicide prevention in a randomized controlled trial: effects on suicide risk and depression. Behav Ther. 2019 Mar;50(2):421–429. doi: 10.1016/j.beth.2018.07.007.S0005-7894(18)30099-6 [DOI] [PubMed] [Google Scholar]
- 34.Torok M, Han J, McGillivray L, Wong Q, Werner-Seidler A, O'Dea B, Calear A, Christensen H. The effect of a therapeutic smartphone application on suicidal ideation in young adults: Findings from a randomized controlled trial in Australia. PLoS Med. 2022 May 31;19(5):e1003978. doi: 10.1371/journal.pmed.1003978. https://dx.plos.org/10.1371/journal.pmed.1003978 .PMEDICINE-D-21-03557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Büscher R, Torok M, Terhorst Y, Sander L. Internet-based cognitive behavioral therapy to reduce suicidal ideation: a systematic review and meta-analysis. JAMA Netw Open. 2020 Apr 01;3(4):e203933. doi: 10.1001/jamanetworkopen.2020.3933. https://europepmc.org/abstract/MED/32343354 .2765056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kondylakis H, Katehakis DG, Kouroubali A, Logothetidis F, Triantafyllidis A, Kalamaras I, Votis K, Tzovaras D. COVID-19 mobile apps: a systematic review of the literature. J Med Internet Res. 2020 Dec 09;22(12):e23170. doi: 10.2196/23170. https://www.jmir.org/2020/12/e23170/ v22i12e23170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Gilat I, Tobin Y, Shahar G. Offering support to suicidal individuals in an online support group. Arch Suicide Res. 2011 Jul;15(3):195–206. doi: 10.1080/13811118.2011.589675. [DOI] [PubMed] [Google Scholar]
- 38.Gilat I, Tobin Y, Shahar G. Responses to suicidal messages in an online support group: comparison between trained volunteers and lay individuals. Soc Psychiatry Psychiatr Epidemiol. 2012 Dec 11;47(12):1929–35. doi: 10.1007/s00127-012-0508-7. [DOI] [PubMed] [Google Scholar]
- 39.Mishara BL, Daigle M, Bardon C, Chagnon F, Balan B, Raymond S, Campbell J. Comparison of the effects of telephone suicide prevention help by volunteers and professional paid staff: results from studies in the USA and Quebec, Canada. Suicide Life Threat Behav. 2016 Oct 06;46(5):577–587. doi: 10.1111/sltb.12238. https://europepmc.org/abstract/MED/26946110 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Boudreaux ED, Haskins BL, Larkin C, Pelletier L, Johnson SA, Stanley B, Brown G, Mattocks K, Ma Y. Emergency department safety assessment and follow-up evaluation 2: An implementation trial to improve suicide prevention. Contemp Clin Trials. 2020 Aug;95:106075. doi: 10.1016/j.cct.2020.106075. https://europepmc.org/abstract/MED/32565041 .S1551-7144(20)30153-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
CONSORT-eHEALTH checklist (V 1.6.1).
Data Availability Statement
The data sets generated and/or analyzed during this study are not publicly available due to the limitations set by the University of Hong Kong Human Research Ethics Committee, but they are available from the corresponding author on reasonable request. The submission of a Data Access Request Form is required.


