Abstract
Background:
Posterolateral corner (PLC) knee injuries associated with different injury mechanisms are not well known.
Purpose/Hypothesis:
This study sought to assess the patterns of associated injuries in the setting of PLC injury. The hypothesis was that there are recognizable injury patterns in PLC injuries that may correlate with injury mechanism.
Study Design:
Cross-sectional study; Level of evidence, 3.
Methods:
Patients who sustained a multiligament knee injury were retrospectively reviewed. Patients who sustained an acute grade 3 PLC injury and underwent surgery were enrolled in this study. A description of the PLC injury (location of the injury of the fibular collateral ligament [FCL], popliteus tendon, and/or popliteofibular ligament) and reported concomitant injuries (biceps femoris tendon or meniscal tears, cartilage pathology and/or peroneal nerve palsy, or bone bruises) were collected and classified based on intraoperative and magnetic resonance imaging (MRI) findings.
Results:
Of 135 patients reviewed, 83 did not have PLC involvement and 13 were excluded due to insufficient MRI scans available. Thus, 39 patients were included in this study. For both the anterior cruciate ligament (ACL)–PLC and ACL–posterior cruciate ligament–PLC injury patterns, the most frequent injury pattern entailed a bone bruise of the anteromedial (AM) femur and tibia, an FCL tear from the fibular head, the popliteus tendon avulsed off the femur, a biceps femoris tendon torn off the fibular head, and a common peroneal nerve palsy. Conversely, when no bone bruise occurred on the AM femur and tibia, the FCL was injured on the femoral side and the popliteus tendon, biceps femoris, and peroneal nerve were not injured.
Conclusion:
AM bone bruise was associated with a peroneal nerve injury in almost half of the patients, and peroneal nerve injury was not seen if there was no AM bone bruise.
Keywords: knee, ligaments, lateral/posterolateral knee ligaments, peroneal nerve injury
The main static stabilizers of the posterolateral corner (PLC) of the knee are the fibular collateral ligament (FCL), popliteus tendon, and popliteofibular ligament. They are important for providing varus and external rotation stability. 8,10,16 The other surgically and clinically important structures of the PLC include the biceps femoris tendon and the common peroneal nerve (CPN). 2,14,21 PLC injuries rarely occur in isolation, more often occurring as part of a multiligament knee injury (MLKI) with or without a knee dislocation. 12 Furthermore, PLC injuries in the setting of MLKIs are associated with high risk of CPN and vascular injuries. 21 However, the structures injured with specific mechanisms involving the PLC are not well understood, and until recently the PLC was considered the “dark side” of the knee. 5 Often, the patients themselves are unable to explain the injury mechanism of a PLC injury because it is frequently part of a more complex injury with concomitant pathology. 21 It is essential to identify concurrent injuries with a PLC injury due to the high rate of concurrent cruciate ligament graft failures with untreated PLC injuries. 17,18 If the associated injuries in the setting of a PLC injury are further described, the risk of overlooking them could be reduced.
The purpose of this study was to investigate and report on the injury patterns in the setting of a PLC injury. The hypothesis was that there are recognizable injury patterns in PLC injuries that may correlate with injury mechanism.
Methods
Participants
This study was conducted in the setting of a level I trauma center; the study protocol received ethics committee approval. Patients provided informed consent. Patients who underwent MLKI surgery were entered into a prospective medical database. This database was retrospectively reviewed, and 135 patients with MLKI were identified between January 2016 and February 2021. We included patients who underwent concurrent ligament repair or reconstruction for a grade 3 PLC injury and a reconstruction to one or both cruciate ligaments. Patients were excluded if they did not have T2-weighted, fat-suppressed, magnetic resonance imaging (MRI) sequences available in both the coronal and sagittal planes or if MRI was conducted >30 days after the primary injury. 7,11,13,22,26
Data Collection and Definitions
The patients’ medical records and imaging were reviewed, and deidentified data were entered into a data sheet (Microsoft Office Excel, Version 2019) and stored on a secure server. Patient characteristics, including age, sex, height, weight, body mass index, and mechanism of injury (high energy, low energy, and ultra–low energy), were recorded from the medical charts and clinical reports for all patients. A high-energy injury was defined as a motor vehicle accident, a pedestrian struck by a vehicle, a motorcycle crash, an industrial accident, a direct crush, or a fall from a height >5 feet (1.52 meters). A low-energy mechanism was defined as an injury from low-velocity sporting activities or a fall from a height <5 feet. An ultra–low energy injury was defined as occurring during activities of daily living, such as stepping off a curb, stepping off a stair, or falling while walking.
A description of the PLC injury (injury of the FCL, popliteus tendon, and/or popliteofibular ligament) and reported concomitant injuries (cruciate ligament injuries, biceps femoris tendon or meniscal tears, cartilage pathology and/or peroneal nerve palsy, or bone bruises) were recorded, and the location of the injury was collected and classified based on descriptions in the surgical notes and radiologic findings.
Based on findings from the initial physical examination, peroneal nerve injuries were classified into 2 groups: complete and partial peroneal nerve palsy. A complete peroneal palsy was defined as having both complete motor and complete sensory loss with 0/5 tibialis anterior (TA) strength, 0/5 extensor hallucis longus strength, and complete sensory anesthesia in the CPN distribution (dorsal and lateral foot). A partial peroneal nerve palsy was defined as a deficit in ≥1 of the following physical examination measures: TA strength, extensor hallucis longus strength, and peroneal nerve sensation. Partial sensory loss was defined as decreased sensation, paresthesia, dysesthesias, and/or numbness in the CPN distribution.
Radiographic Analysis
All MRI scans were preoperatively interpreted by a board-certified musculoskeletal radiologist, regardless of whether the imaging was conducted at a referring hospital or performed in-house. At the time of data collection, the MRI scans were again assessed by a board-certified, orthopaedic sports medicine fellowship–trained surgeon (S.T.), and the results were compared with the original MRI report. All injuries were listed and classified according to the location of the structural injury. The location of the ligament injury was evaluated based on the MRI findings. The ligament injury was categorized as proximal, midsubstance, or distal depending on where the main pathology was observed.
Fat-suppressed, T2-weighted coronal and sagittal images were reviewed to determine the location of bone bruises, which were defined as areas with high signal intensity adjacent to joint surfaces within the tibiofemoral compartment in the injured knee. The articulating surfaces of the femur and tibia were divided into 4 quadrants, and coronal, sagittal, and axial images were used to categorize the lesion location primarily in the anterior or posterior and medial or lateral compartments according to the method used by Geeslin and LaPrade. 11 For example, a bone bruise anterior to the mid–medial femoral condyle was considered anteromedial (AM) and posterior to it was considered posteromedial (PM). Similarly, when we evaluated the lateral tibial condyle in the sagittal plane of an MRI scan, an anterior bone bruise was considered anterolateral (AL) and posterior was considered posterolateral (PL).
Operative Record Findings
Intraoperative arthroscopic findings were used to determine the presence of meniscal and/or cartilage injuries. Cartilage injury was evaluated by the International Cartilage Regeneration & Joint Preservation Society grading system, with grade ≥2 injury defined as entailing cartilage damage. 4
The status of the popliteus tendon was observed from the lateral joint compartment using an arthroscope and under direct view at the femoral attachment during open surgery. After the biceps bursa over the distal FCL was opened, the midsubstance of the FCL was identified and tension was applied to determine under direct view whether the injury was at the distal or proximal attachment. 15
If there was a discrepancy between the MRI assessments and intraoperative findings or if there was uncertainty as to the structural diagnosis, then clinical and/or intraoperative findings and the orthopaedic surgeon’s final postoperative diagnosis were used as the definitive diagnosis of the patient’s PLC injury and concomitant injuries.
Data Analysis
The data collected in this study were analyzed with descriptive statistics. Continuous variables were reported as means and standard deviations, and categorical variables were reported as frequencies with proportions.
Results
Patient Demographic Characteristics
Of the 135 patients with MLKI, patients without PLC lesions were excluded. Of the remaining 52 patients, 13 were excluded due to insufficient available MRI scans. Thus, 39 patients (75%; 39 knees) were included in this study (Figure 1).
Figure 1.
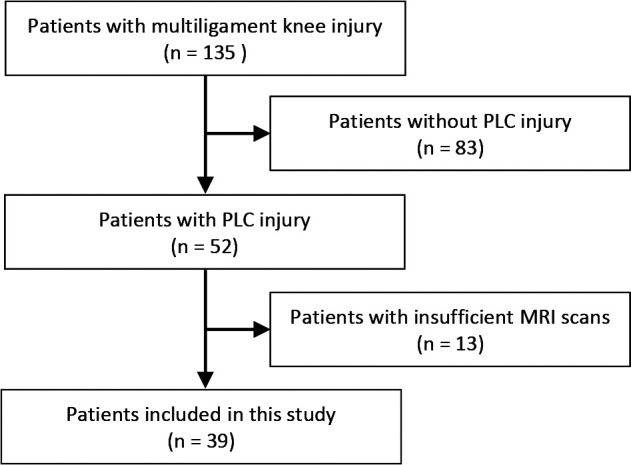
Flowchart of patient inclusion. MRI, magnetic resonance imaging; PLC, posterolateral corner.
The patient characteristics are reported in Table 1. The mean patient age was 33.0 ± 13.6 years (range, 15-58 years) with the majority (69.2%) of patients being male. The mean time from injury to surgery was 12.3 ± 5.0 days (range, 6-30 days). The injury mechanism was high-energy trauma in 10 patients (25.6%), low-energy trauma in 16 patients (41.0%), and ultra–low energy trauma in 13 patients (33.3%).
Table 1.
Characteristics of Patients With Posterolateral Knee Injuries (N = 39 patients, 39 knees) a
| Variable | Value |
|---|---|
| Age, y | 33.0 ± 13.6 |
| Sex, male/female | 27/12 |
| Height, cm | 178.1 ± 9.0 |
| Weight, kg | 83.0 ± 13.6 |
| Body mass index, kg/m2 | 26.3 ± 4.1 |
| Injury mechanism | |
| High-energy trauma | 10 |
| Low-energy trauma | 16 |
| Ultra–low energy trauma | 13 |
a Data are presented as mean ± SD or No. of patients.
Injury Patterns and Concomitant Injuries
The 2 most common ligament injury patterns found in this cohort were anterior cruciate ligament (ACL)–PLC and ACL–posterior cruciate ligament (PCL)–PLC injuries, accounting for 56.4% and 35.9% of the cohort, respectively (Table 2).
Table 2.
Concomitant Knee Ligament Injury Patterns Associated With Posterolateral Knee Injuries a
| Injury Pattern | No. (%) of Knees |
|---|---|
| ACL-PCL-PLC | 14 (35.9) |
| ACL-PLC | 22 (56.4) |
| PCL-PLC | 1 (2.6) |
| ACL-PCL-PLC-MCL | 1 (2.6) |
| ACL-MCL-PLC | 1 (2.6) |
a ACL, anterior cruciate ligament; MCL, medial collateral ligament; PCL, posterior cruciate ligament; PLC, posterolateral corner.
The FCL was torn distally in the majority of patients (84.6%) (Table 3). The biceps femoris tendon attachment to the fibular head was injured in two-thirds (66.7%) of patients and was always accompanied by a distal FCL tear. Six patients (15.4%) had a distal FCL tear without injury to the biceps femoris tendon. The popliteus tendon was torn at its femoral attachment in 56.4% of the patients. Medial and lateral meniscal injuries were present in 5.1% and 17.9% of patients, respectively. No patient sustained an injury to both menisci. There was a low prevalence of reported cartilage injuries (medial femoral condyle injuries, 7.7%; patellofemoral joint injuries, 2.6%). The injury was complicated by a peroneal nerve neurapraxia in 17 patients (43.6%), of whom 10 patients had complete paralysis and sensory loss. Of the 26 patients who sustained a torn biceps femoris tendon attachment off the fibular head, 14 patients (53.8%) had partial or complete peroneal nerve palsy.
Table 3.
Posterolateral Corner Injury Morphology and Concomitant Injuries
| Injury | No. (%) of Knees |
|---|---|
| Fibular collateral ligament tear | |
| Proximal | 5 (12.8) |
| Midsubstance | 1 (2.6) |
| Distal | 33 (84.6) |
| Biceps femoris tendon tear | |
| Intact | 13 (33.3) |
| Distal | 26 (66.7) |
| Popliteus tendon tear | |
| Intact | 17 (43.6) |
| Proximal injury | 22 (56.4) |
| Meniscal tear | |
| Medial meniscus | 2 (5.1) |
| Lateral meniscus | 7 (17.9) |
| Cartilage injury | |
| Medial femoral condyle | 3 (7.7) |
| Patellofemoral joint | 1 (2.6) |
| Peroneal nerve palsy | |
| Intact | 22 (56.4) |
| Partial | 7 (17.9) |
| Complete | 10 (25.6) |
Bone Bruise Patterns on MRI
MRI evaluation of the included patients showed a high proportion of AM bone bruises (femoral side, 87.2%; tibial side, 74.4%) (Table 4). Five of the AM tibial-side bone bruises had ipsilateral fractures at this site. Figure 1 presents the most common, typical bone bruises seen in the present cohort. A few cases of combined AL femoral and PL tibial bone bruises were noted, which are common in ACL injuries. Two patients (5.1%) had only AL femoral and PL tibial bone bruises; 1 patient (2.6%) had AM, AL femoral, and PL tibial bone bruises; and 1 patient (2.6%) had AM femoral, AM, and PL tibial bone bruises. An AM bone bruise was associated with a peroneal nerve injury in 42% of ACL-PLC injuries and 46% of ACL-PCL-PLC injuries. Furthermore, no peroneal nerve injury occurred in any patient without an AM bone bruise.
Table 4.
Bone Bruise Pattern of Posterolateral Corner Injuries on Magnetic Resonance Imaging
| Bone Bruise Location | No. (%) of Knees |
|---|---|
| Femoral side | |
| Anteromedial | 34 (87.2) |
| Anterolateral | 2 (5.1) |
| Tibial side | |
| Anteromedial | 29 (74.4) |
| Posterolateral | 4 (10.3) |
Figure 2.
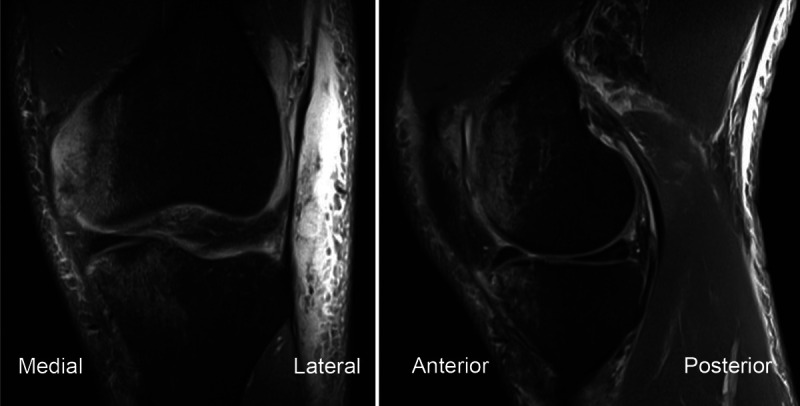
Example of the most common typical bone bruise pattern seen in this study, simultaneous bone bruises of the anteromedial femur and tibia, in a left knee.
The relationship between femoral and tibial bone bruise incidence and location for injury pattern subgroups is reported in Table 5. For both the femur and the tibia, a high rate of AM bone bruises was seen for both ACL-PLC and ACL-PCL-PLC injury patterns.
Table 5.
Femoral and Tibial Bone Bruise Incidence and Locations for Patterns of Acute Grade 3 PLC Injury a
| Femur | Tibia | |||||||
|---|---|---|---|---|---|---|---|---|
| Injury Pattern | AM | AL | PM | PL | AM | AL | PM | PL |
| ACL-PCL-PLC (n = 14) | 13 | 0 | 0 | 0 | 12 | 0 | 0 | 0 |
| ACL-PLC (n = 22) | 20 | 3 | 0 | 0 | 13 | 0 | 0 | 3 |
| PCL-PLC (n = 1) | 1 | 0 | 0 | 0 | 1 | 0 | 0 | 1 |
| ACL-PCL-PLC-MCL (n = 1) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| ACL-MCL-PLC (n = 1) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
a Data are reported as No. of knees. ACL, anterior cruciate ligament; AL, anterolateral; AM, anteromedial; MCL, medial collateral ligament; PCL, posterior cruciate ligament; PL, posterolateral; PLC, posterolateral corner; PM, posteromedial; PMC, posteromedial corner.
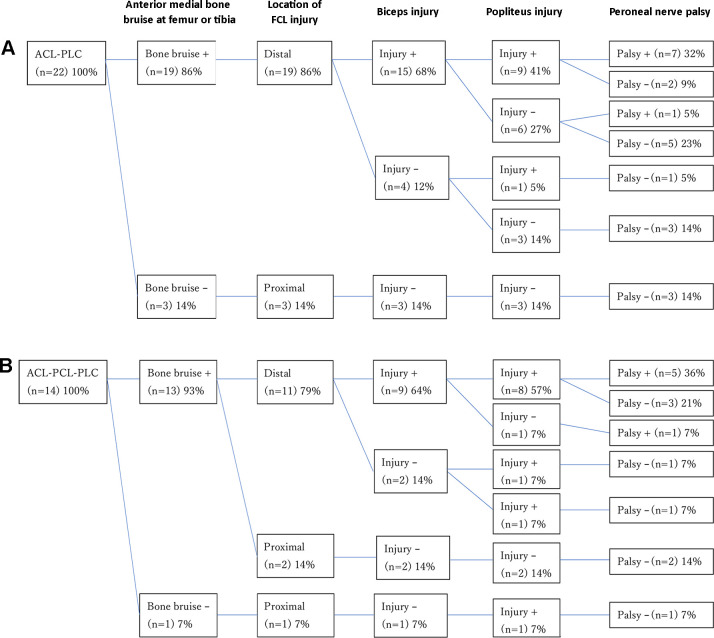
To further visualize the variation of detected injury patterns, a flowchart was created for ACL-PLC and ACL-PCL-PLC patterns (Figure 3). For both the ACL-PLC and ACL-PCL-PLC injury patterns, the most common injury pattern entailed an AM bone bruise, a distal FCL and biceps femoris tendon tear, the popliteus tendon being torn off the femur, and peroneal nerve palsy, which occurred in 14 of the 36 patients.
Figure 3.
Flowchart of injury characteristics with the (A) ACL-PLC and (B) ACL-PCL-PLC patterns. ACL, anterior cruciate ligament; FCL, fibular collateral ligament; PCL, posterior cruciate ligament; PLC, posterolateral corner.
Discussion
The most important finding of this study was that the combination of a grade 3 PLC and concurrent cruciate ligament injury entailed a high probability of bone bruises of the AM femur and tibia. In the presence of an AM bone bruise, the FCL was most frequently torn distally with a high probability of simultaneous injury wherein the distal biceps femoris tendon was torn off the fibula, the popliteus tendon was torn off the femur, and the peroneal nerve was injured. Interestingly, when no AM bone bruise was present, the FCL was torn on the femoral side and the biceps femoris, popliteus tendon, and peroneal nerve were intact. These injury patterns suggest that specific injury mechanisms may result in different injury patterns to the PL knee structures.
The occurrence of an AM bone bruise on the femoral and tibial sides suggests that the knee was injured in a varus hyperextension mechanism and the bone bruises were a result of a kissing lesion. When the knee was subjected to a varus hyperextension load, the ACL or ACL-PCL was injured (depending on several factors, including the intensity of the loading and the position of the body), the FCL was avulsed from the fibula, and the biceps femoris, popliteus tendon, and peroneal nerve were injured. This injury pattern is illustrated in Figure 4.
Figure 4.
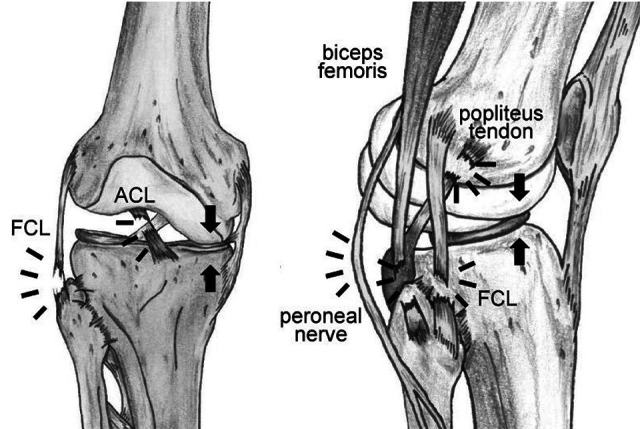
Illustration of the hyperextension injury pattern of a grade 3 posterolateral corner injury (right knee) as found in this study. ACL, anterior cruciate ligament; FCL, fibular collateral ligament.
Several reports confirm this injury pattern. Similar to the present study, Moran et al 22 examined the location of bone bruises in PLC injuries and found that many PLC injuries were accompanied by an AM bone bruise. This revealed that the injury pattern of PLC injury with these bone bruise locations was likely varus hyperextension. Moran et al also reported that a bone bruise of the AM part of the femur and tibia was a risk factor for peroneal nerve injury. The proportions of peroneal nerve palsy in grade 3 PLC injury were similar: 36.8% in the Moran et al study and 43.5% in our study. Li et al 20 and Bennett et al 2 reported that some patients with PLC injuries may have fractures of the AM tibia, which were related to hyperextension injuries. 25 In the present study, we noted 5 cases of similar AM tibial fractures in the same region as the tibial bone bruises, which were considered to be fractures resulting from a hyperextension injury. Thus, the injury pattern revealed in our study was consistent with the previous reports. Essilfie et al 9 and Bottomley et al 3 reported that the presence of a PLC injury and biceps femoris avulsion from the fibular head increased the risk for peroneal nerve injury. Kahan et al 14 reported that for PLC injuries that resulted in a peroneal nerve palsy, the majority of FCL tears occurred distally, similar to our findings.
The pattern of associated pathology in varus hyperextension PLC injuries has been reported before, and our findings were similar to those of previous reports. 1,6,10,19,23 However, in the present study, we were able to identify the entire flow of the injury pattern, including FCL, biceps femoris, and popliteus tendon injuries and peroneal nerve palsy with a varus hyperextension mechanism. In the ACL-PLC and ACL-PCL-PLC tear patterns, in patients without AM bone bruises, the FCL was torn off its femoral attachment, and the biceps femoris, popliteus tendon, and peroneal nerve were not injured. We theorize that without a varus hyperextension injury mechanism such as flexion–external rotation, pure varus load, and pure hyperextension, the FCL can be expected to be injured on the femoral side, reducing the potential for injury to the biceps femoris, popliteus tendon, and peroneal nerve. The presence of an AM bone bruise had an almost 50% incidence of peroneal nerve palsy. Therefore, the presence of an AM bone bruise should warrant careful evaluation of the peroneal nerve. In addition, the most common injury pattern was seen in only one-third of the patients, and a wide variety of injury patterns occurred. Thus, the surgeon should perform a careful physical examination and thoroughly review MRI scans before performing surgery on the PLC.
Limitations
There were some limitations to this study. The number of patients included is small. Although the center where the study was conducted is a high-volume center for complex knee injuries, PLC injuries are not common. The popliteofibular ligament, which is an important static stabilizer of the PLC, was not identified in the present study. It is difficult to identify the popliteofibular ligament on MRI scans, and it is also technically difficult to identify the injury site intraoperatively. These assessments may be possible in future prospective studies for which data collection is defined a priori. 24 The presence of injury to the popliteofibular ligament in the described injury patterns may further improve our understanding of the complex interaction of the structures of the PLC.
Conclusion
AM bone bruise was associated with a peroneal nerve injury in almost half of the patients, and peroneal nerve injury was not seen if there was no AM bone bruise.
Acknowledgment
The authors thank Sverre Løken, MD, PhD, Berte Bøe, MD, PhD, Frode Mauroy, MD, Ragnhild Øydna Støen, MD, PhD, and Kristian Marstrand Warholm, MD, PhD, for providing insight and expertise. The authors also thank Hironori Takagi for creating the illustrations.
Footnotes
Final revision submitted March 8, 2023; accepted April 13, 2023.
One or more of the authors has declared the following potential conflict of interest or source of funding: R.F.L. has received consulting fees and royalties from Arthrex and Smith & Nephew, nonconsulting fees from Smith & Nephew, and speaking fees from Linvatec. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Oslo University Hospital (No. 2012/873).
References
- 1. Amis AA, Bull AM, Gupte CM, et al. Biomechanics of the PCL and related structures: posterolateral, posteromedial and meniscofemoral ligaments. Knee Surg Sports Traumatol Arthrosc. 2003;11(5):271–281. [DOI] [PubMed] [Google Scholar]
- 2. Bennett DL, George MJ, El-Khoury GY, Stanley MD, Sundaram M. Anterior rim tibial plateau fractures and posterolateral corner knee injury. Emerg Radiol. 2003;10(2):76–83. [DOI] [PubMed] [Google Scholar]
- 3. Bottomley N, Williams A, Birch R, et al. Displacement of the common peroneal nerve in posterolateral corner injuries of the knee. J Bone Joint Surg Br. 2005;87(9):1225–1226. [DOI] [PubMed] [Google Scholar]
- 4. Brittberg M, Peterson L. Introduction of an articular cartilage classification. ICRS Newsletter. 1998;1(1):5–8. [Google Scholar]
- 5. Chahla J, Murray IR, Robinson J, et al. Posterolateral corner of the knee: an expert consensus statement on diagnosis, classification, treatment, and rehabilitation. Knee Surg Sports Traumatol Arthrosc. 2019;27(8):2520–2529. [DOI] [PubMed] [Google Scholar]
- 6. Covey DC. Injuries of the posterolateral corner of the knee. J Bone Joint Surg Am. 2001;83(1):106–118. [DOI] [PubMed] [Google Scholar]
- 7. Davies NH, Niall D, King LJ, Lavelle J, Healy JC. Magnetic resonance imaging of bone bruising in the acutely injured knee—short-term outcome. Clin Radiol. 2004;59(5):439–445. [DOI] [PubMed] [Google Scholar]
- 8. Dold AP, Swensen S, Strauss E, Alaia M. The posteromedial corner of the knee: anatomy, pathology, and management strategies. J Am Acad Orthop Surg. 2017;25(11):752–761. [DOI] [PubMed] [Google Scholar]
- 9. Essilfie AA, Alaia EF, Bloom DA, et al. Distal posterolateral corner injury in the setting of multiligament knee injury increases risk of common peroneal palsy. Knee Surg Sports Traumatol Arthrosc. 2022;30(1):239–245. [DOI] [PubMed] [Google Scholar]
- 10. Figueroa F, Figueroa D, Putnis S, et al. Posterolateral corner knee injuries: a narrative review. EFORT Open Rev. 2021;6(8):676–685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Geeslin AG, LaPrade RF. Location of bone bruises and other osseous injuries associated with acute grade III isolated and combined posterolateral knee injuries. Am J Sports Med. 2010;38(12):2502–2508. [DOI] [PubMed] [Google Scholar]
- 12. Geeslin AG, LaPrade RF. Outcomes of treatment of acute grade-III isolated and combined posterolateral knee injuries: a prospective case series and surgical technique. J Bone Joint Surg Am. 2011;93(18):1672–1683. [DOI] [PubMed] [Google Scholar]
- 13. Graf BK, Cook DA, De Smet AA, Keene JS, “Bone bruises” on magnetic resonance imaging evaluation of anterior cruciate ligament injuries. Am J Sports Med. 1993;21(2):220–223. [DOI] [PubMed] [Google Scholar]
- 14. Kahan JB, Li D, Schneble CA, et al. The pathoanatomy of posterolateral corner ligamentous disruption in multiligament knee injuries is predictive of peroneal nerve injury. Am J Sports Med. 2020;48(14):3541–3548. [DOI] [PubMed] [Google Scholar]
- 15. LaPrade RF, Hamilton CD. The fibular collateral ligament-biceps femoris bursa: an anatomic study. Am J Sports Med. 1997;25(4):439–443. [DOI] [PubMed] [Google Scholar]
- 16. LaPrade RF, Ly TV, Wentorf FA, Engebretsen L. The posterolateral attachments of the knee: a qualitative and quantitative morphologic analysis of the fibular collateral ligament, popliteus tendon, popliteofibular ligament, and lateral gastrocnemius tendon. Am J Sports Med. 2003;31(6):854–860. [DOI] [PubMed] [Google Scholar]
- 17. LaPrade RF, Muench C, Wentorf F, Lewis JL. The effect of injury to the posterolateral structures of the knee on force in a posterior cruciate ligament graft: a biomechanical study. Am J Sports Med. 2002;30(2):233–238. [DOI] [PubMed] [Google Scholar]
- 18. LaPrade RF, Resig S, Wentorf F, Lewis JL. The effects of grade III posterolateral knee complex injuries on anterior cruciate ligament graft force: a biomechanical analysis. Am J Sports Med. 1999;27(4):469–475. [DOI] [PubMed] [Google Scholar]
- 19. LaPrade RF, Terry GC. Injuries to the posterolateral aspect of the knee: association of anatomic injury patterns with clinical instability. Am J Sports Med. 1997;25(4):433–438. [DOI] [PubMed] [Google Scholar]
- 20. Li X, Song G, Li Y, et al. The “diagonal” lesion: a new type of combined injury pattern involving the impingement fracture of anteromedial tibial plateau and the injury of posterior cruciate ligament and posterolateral corner. J Knee Surg. 2020;33(6):616–622. [DOI] [PubMed] [Google Scholar]
- 21. Moatshe G, Dornan GJ, Løken S, et al. Demographics and injuries associated with knee dislocation: a prospective review of 303 patients. Orthop J Sports Med. 2017;5(5):2325967117706521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Moran J, Schneble CA, Katz LD, et al. Examining the bone bruise patterns in multiligament knee injuries with peroneal nerve injury. Am J Sports Med. 2022;50(6):1618–1626. [DOI] [PubMed] [Google Scholar]
- 23. Nannaparaju M, Mortada S, Wiik A, Khan W, Alam M. Posterolateral corner injuries: epidemiology, anatomy, biomechanics and diagnosis. Injury. 2018;49(6):1024–1031. [DOI] [PubMed] [Google Scholar]
- 24. Pękala PA, Mann MR, Pękala JR, Tomaszewski KA, LaPrade RF. Evidence-based clinical anatomy of the popliteofibular ligament and its importance in orthopaedic surgery: cadaveric versus magnetic resonance imaging meta-analysis and radiological study. Am J Sports Med. 2021;49(6):1659–1668. [DOI] [PubMed] [Google Scholar]
- 25. Tomás-Hernández J, Monyart JM, Serra JT, et al. Large fracture of the anteromedial tibial plateau with isolated posterolateral knee corner injury: case series of an often missed unusual injury pattern. Injury. 2016;47(suppl 3):S35–S40. [DOI] [PubMed] [Google Scholar]
- 26. Viskontas DG, Giuffre BM, Duggal N, et al. Bone bruises associated with ACL rupture: correlation with injury mechanism. Am J Sports Med. 2008;36(5):927–933. [DOI] [PubMed] [Google Scholar]