Key Points
Question
What is the association of vitiligo with patient-reported quality of life and psychosocial health globally?
Findings
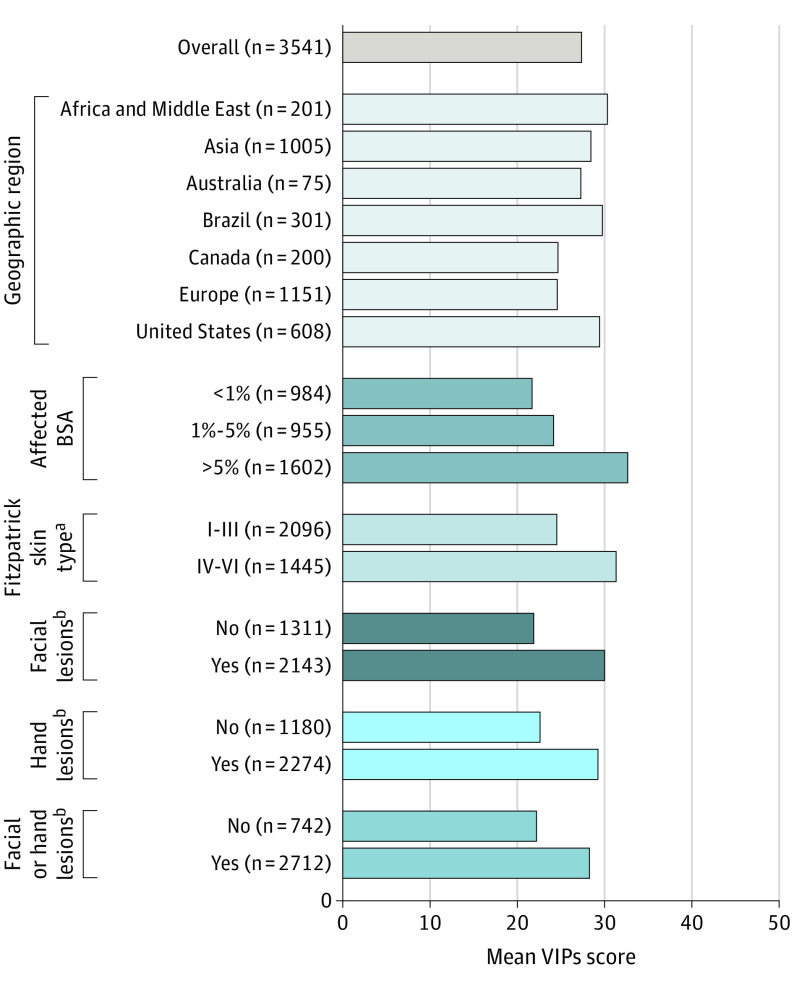
In this population-based qualitative study, 3541 patients with vitiligo across 17 countries reported substantial burden on quality of life, emotional well-being, daily life, and psychosocial health, with greater burden noted among patients with more than 5% affected body surface area, Fitzpatrick skin types IV to VI (ie, darker skin), facial involvement, or hand involvement vs their counterparts.
Meaning
Findings suggest that improvement in the psychosocial health of patients should be prioritized in the management and treatment of vitiligo.
Abstract
Importance
Patients with vitiligo often have impaired quality of life (QOL) and experience substantial psychosocial burden.
Objective
To explore the global association of vitiligo with QOL and mental health from the patient perspective.
Design, Setting, and Participants
This qualitative study of the cross-sectional population-based Vitiligo and Life Impact Among International Communities (VALIANT) study was conducted from May 6, 2021, to June 21, 2021. Potential participants for this qualitative study were recruited from an online panel in 17 countries. Of 5859 surveyed adults (aged ≥18 years) who reported a vitiligo diagnosis, 3919 (66.9%) completed the survey, and 3541 (60.4%) were included in the analysis.
Exposures
Patients were asked questions regarding their emotional well-being, including QOL and mental health.
Main Outcomes and Measures
Reported analyses are descriptive and hypothesis generating. Vitiligo Impact Patient scale (VIPs) scores ranged from 0 to 60, with higher scores indicating more psychosocial burden.
Results
The median age of the 3541 patients was 38 years (range, 18-95 years), and 1933 (54.6%) were male; 1602 patients (45.2%) had more than 5% affected body surface area (BSA; Self-Assessment Vitiligo Extent Score assessed), and 1445 patients (40.8%) had Fitzpatrick skin types IV to VI (ie, darker skin). The mean (SD) global short-form VIPs score was 27.3 (15.6) overall; patients from India (mean [SD], 40.2 [14.1]) reported the highest scores (ie, most burden). The QOL burden according to the scale was profound for patients with more than 5% affected BSA (mean [SD] score, 32.6 [14.2]), darker skin (mean [SD] score, 31.2 [15.6]), and lesions on the face (mean [SD] score, 30.0 [14.9]) or hands (mean [SD], 29.2 [15.2]). At least 40% of patients globally reported that vitiligo frequently affected aspects of their daily lives, including choosing clothes to wear (1956 of 3541 [55.2%]). Most patients (2103 of 3541 [59.4%]) reported concealing their vitiligo frequently. More than half of patients (2078 of 3541 [58.7%]) reported diagnosed mental health conditions, including anxiety (1019 of 3541 [28.8%]) and depression (866 of 3541 [24.5%]). The Patient Health Questionnaire–9 depression screener showed that 55.0% of patients (1948 of 3541) had moderate to severe depressive symptoms; the highest rates were in India (271 of 303 [89.4%]) and among patients with more than 5% affected BSA (1154 of 1602 [72.0%]) and darker skin (987 of 1445 [68.3%]).
Conclusions and Relevance
This qualitative study found that, globally, patients with vitiligo reported being substantially affected in their emotional well-being, daily lives, and psychosocial health; the burden was typically greatest among patients with more than 5% affected BSA, darker skin types, and lesions on the face or hands. Survey findings suggest that patients reported having altered their behavior, expressed clear discontent, and have symptoms consistent with depression, which may be underdiagnosed.
This qualitative study investigates the mental health and psychosocial quality-of-life burden worldwide among patients with vitiligo.
Introduction
Vitiligo is a chronic autoimmune disease characterized by destruction of melanocytes, resulting in pale or white patches of skin.1 Patients with vitiligo encounter significant quality-of-life (QOL) impairment in routine activities, employment, and psychosocial health.2,3 Previous reports suggest that patients with greater body surface area (BSA) involvement and visible lesions experience greater psychosocial burden.4,5 Patients with vitiligo are also more likely to have depression and anxiety than individuals without vitiligo serving as controls.6,7 Psychosocial stressors are associated with vitiligo onset or flares.8,9
There is a need to further understand the global burden of vitiligo from the patient perspective. Here we explore sociodemographic characteristics and QOL and describe differences in psychosocial burden across geographic regions and subgroups of disease characteristics among patients surveyed in the Vitiligo and Life Impact Among International Communities (VALIANT) study.
Methods
Study Participants
This cross-sectional observational qualitative study provided a survey that was administered to adults (aged ≥18 years) who received a diagnosis of vitiligo from a health care professional and were recruited via an online panel from 17 countries between May 6 and June 21, 2021, using a general population sampling approach (eAppendix in Supplement 1). The study protocol received an exemption from informed consent from the Western Institutional Review Board based on survey procedures and use of deidentified data. Participants completed a brief online screener before continuing to the 25-minute survey. The survey was designed to assess self-reported emotional well-being, QOL, and depressive symptoms in a target sample of approximately 3500 patients. Additional assessment instruments (eg, the Vitiligo Impact Patient scale [VIPs] and the Patient Health Questionnaire–9 depression screener) are described in the eAppendix and eTable 1 in Supplement 1. Data were summarized with descriptive statistics. This qualitative study followed the Standards for Reporting Qualitative Research (SRQR) reporting guidelines.
Statistical Analysis
Analyses included comparison of the 17 countries, 7 geographic regions, and demographic and clinical characteristic subgroups, with t tests for comparisons of mean values and χ2 tests for categorical counts. Statistical significance was conferred at P < .05 (2-sided). The software used for analysis was WinCross, version 20 (The Analytical Group).
Results
Patient Demographic Characteristics
Of 5859 participants who reported a vitiligo diagnosis and were directed to the survey, 3919 (66.9%) completed the survey, 378 (6.5%) were excluded for data quality issues (eTable 2 in Supplement 1), and 3541 (60.4%) were included in the analysis. The median age was 38 years (range, 18-95 years); 1933 (54.6%) were male, 1603 (45.3%) were female, and 5 were nonbinary (0.1%). Race and ethnicity were not solicited in France (n = 250) or Germany (n = 250). A total of 929 of the 3041 patients with available data were Asian (30.5%), 283 were Black (9.3%), 144 were Central or South American (4.7%), 135 were Middle Eastern or North African (4.4%), and 1555 were White (51.1%). A total of 75 patients (2.5%) reported race and ethnicity as “other,” as categorized within the survey, with no further breakdown available. Thirteen patients (0.4%) preferred not to report race and ethnicity. A total of 1445 patients (40.8%) had Fitzpatrick skin types IV to VI (ie, darker skin), and 1602 (45.2%) reported more than 5% affected BSA (Table).
Table. Patient Demographics and Disease Characteristics.
| Characteristic | All patients (N = 3541) |
|---|---|
| Age, median (range), y | 38 (18-95) |
| Age group, No. (%), y | |
| 18-34 | 1280 (36.1) |
| 35-54 | 1543 (43.6) |
| ≥55 | 718 (20.3) |
| Sex, No. (%) | |
| Female | 1603 (45.3) |
| Male | 1933 (54.6) |
| Nonbinary | 5 (0.1) |
| Race and ethnicity, No. (%)a,b | |
| Asian | 929 (30.5) |
| Black | 283 (9.3) |
| Central or South American | 144 (4.7) |
| Middle Eastern or North African | 135 (4.4) |
| White | 1555 (51.1) |
| Otherc | 75 (2.5) |
| Prefer not to answer | 13 (0.4) |
| Fitzpatrick skin type, No. (%)d | |
| I-III | 2096 (59.2) |
| IV-VI | 1445 (40.8) |
| Geographic region, No. (%) | |
| Africa or Middle East | 201 (5.7) |
| Asia | 1005 (28.4) |
| Australia | 75 (2.1) |
| Brazil | 301 (8.5) |
| Canada | 200 (5.6) |
| Europe | 1151 (32.5) |
| US | 608 (17.2) |
| Age at diagnosis, median (range), y | 30 (0-95) |
| Time before diagnosis, mean (SD), y | 2.4 (4.1) |
| Disease duration, mean (SD), y | 12.7 (12.6) |
| Affected BSA, median (range), % | 4.0 (0-73.9) |
| More than 5% affected BSA, No. (%) | 1602 (45.2) |
Abbreviation: BSA, body surface area.
Multiple answers were accepted.
Race and ethnicity were not solicited in France (n = 250) or Germany (n = 250).
Category taken from the survey with no further breakdown available.
Fitzpatrick skin types are defined as follows: type I, pale white skin; type II, white skin; type III, light brown skin; type IV, moderate brown skin; type V, dark brown skin; and type VI, deeply pigmented dark brown to black skin.
QOL and Emotional Well-Being
Globally, the mean (SD) total 12-item VIPs score was 27.3 (15.6) (Figure 1). Scale scores ranged from 0 to 60, with higher scores indicating more psychosocial burden. Patients in India (mean [SD] score, 40.2 [14.1]), Brazil (mean [SD] score, 29.7 [17.1]), and the US (mean [SD] score, 29.4 [12.8]) reported the highest scores (ie, the greatest burden) among countries surveyed (eFigure 1 in Supplement 1). Worse QOL was observed among patients with more than 5% affected BSA (Vitiligo Impact Patient scale mean [SD] score, 32.6 [14.2] vs 24.1 [13.9] for 1%-5% BSA and 21.6 [16.4] for <1% BSA; both P < .001), darker skin (mean [SD] score, 31.2 [15.6] vs 24.5 [15.0] for fairer skin; P < .001), and facial lesions (mean [SD] score, 30.0 [14.9] vs 21.8 [14.9] for no facial lesions; P < .001) or hand lesions (mean [SD] score, 29.2 [15.2] vs 22.5 [14.8] for no hand lesions; P < .001).
Figure 1. Global Vitiligo Impact Patient Scale (VIPs) Scores.
aFitzpatrick skin types I to III were characterized as fairer skin types, and types IV to VI as darker skin types.
bPatients with 0% affected body surface area (BSA) (n = 87) were excluded from analysis. The mean (SD) VIPs score for Africa and the Middle East was 30.2 (16.0) (P < .001 vs Europe and Canada); for Asia, 28.3 (16.1) (P < .01 vs Europe and Canada); for Brazil, 29.7 (17.1) (P < .001 vs Europe and Canada); and for the US, 29.4 (12.8) (P < .001 vs Europe and Canada). The mean (SD) VIPs score for affected BSA was 24.1 (13.9) for 1% to 5% (P < .001 vs <1% BSA) and 32.6 (14.2) for more than 5% (P < .001 vs 1%-5% BSA and <1% BSA). The mean (SD) VIPs score for Fitzpatrick skin type IV to VI was 31.2 (15.6) (P < .001 vs Fitzpatrick skin types I to III). The mean (SD) VIPs score for facial lesions (yes) was 30.0 (14.9) (P < .001 vs no facial lesions); for hand lesions (yes), 29.2 (15.2) (P < .001 vs no hand lesions); and for facial or hand lesions (yes), 28.2 (15.3) (P < .001 vs no facial or hand lesions).
More than 30% of patients (range across questions, 32.8% [1160 of 3541] to 53.5% [1893 of 3541]) reported agreeing or strongly agreeing that vitiligo affected multiple aspects of their emotional well-being, including self-esteem or stigma, relationships, and careers (eFigure 2 in Supplement 1). Among all domains evaluated, patients with more than 5% affected BSA consistently reported being more greatly affected compared with those with less extensive disease. A total of 49.0% of patients (1735 of 3541) agreed that having vitiligo made them feel less confident or more self-conscious. Furthermore, 46.6% of patients (1649 of 3541) believed that “no one understands what it’s like to live with vitiligo.” Patients also felt frustrated with their career prospects, with 41.9% (1483 of 3541) reporting that they believed that they would have been further along in their career if they did not have vitiligo. In contrast, 35.5% (1258 of 3541) reported that having vitiligo made them feel empowered, suggesting that the question may have been misinterpreted.
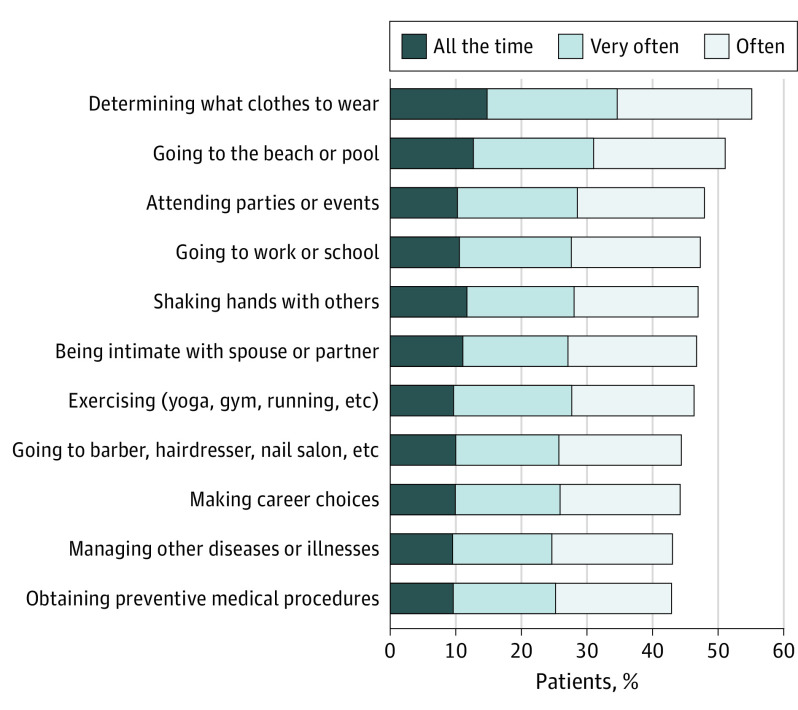
Daily Activities
More than 40% of patients (range across questions, 42.9% [1520 of 3541] to 55.2% [1956 of 3541]) reported that aspects of their daily lives were frequently affected by vitiligo. Among the most stressful daily activities were making clothing choices, attending social activities, shaking hands, and being intimate with their partner (Figure 2). Furthermore, 59.4% of patients (2103 of 3541) reported that they frequently concealed their vitiligo with makeup or concealer or clothing, the rates of which were higher among patients with more than 5% affected BSA (1164 of 1602 [72.7%]), darker skin (955 of 1445 [66.1%]), and facial or hand lesions (1690 of 2712 [62.3%]).
Figure 2. Repercussions of Vitiligo on Patients’ Daily Lives.
Patients were asked how frequently vitiligo affected their decision to participate in daily activities before the COVID-19 pandemic.
Mental Health
More than half of patients (2078 of 3541 [58.7%]) reported diagnosed mental health conditions, most commonly anxiety disorder (1019 of 3541 [28.8%]) and depression (866 of 3541 [24.5%]) (eFigure 3 in Supplement 1). Rates of diagnosed mental health conditions were highest for patients with more than 5% affected BSA (73.8% [1183 of 1602] vs 52.0% [497 of 955] for 1%-5% BSA and 40.4% [398 of 984] for <1% BSA; both P < .001), darker skin (73.4% [1061 of 1445] vs 48.5% [1017 of 2096] for fairer skin; P < .001), and facial lesions (67.2% [1441 of 2143] vs 45.8% [600 of 1311] for no facial lesions; P < .001) or hand lesions (67.2% [1527 of 2274] vs 43.6% [514 of 1180] for no hand lesions; P < .001) and for those from India (90.1% [273 of 303]; P < .05 vs other countries).
Globally, 55.0% of patients (1948 of 3541) reported moderate to severe symptoms of depression according to the Patient Health Questionnaire–9, with the highest rates among patients from India (271 of 303 [89.4%]) (eFigure 4 in Supplement 1). Rates of moderate to severe depressive symptoms were greater among patients with more than 5% affected BSA (1154 of 1602 [72.0%]), darker skin (987 of 1445 [68.3%]), and facial or hand involvement (1607 of 2712 [59.3%]) than among their counterparts (eFigure 5 in Supplement 1).
Discussion
In this first international survey to date exploring the burden of vitiligo, patients, especially those with more than 5% affected BSA, darker skin, and facial or hand involvement, reported that this burden profoundly affected their emotional well-being, daily activities, and mental health. Smaller studies have reported a higher burden for patients with at least 25% affected BSA or darker skin,2,10 supporting our findings that QOL impairment was greater among patients with more than 5% affected BSA and darker skin vs their counterparts. Lesion location was also associated with disease burden, with greater QOL impairment and higher prevalence of depressive symptoms among patients with vs without facial or hand involvement, expanding on previous results.3,11 Corroborating previous findings, the VALIANT study demonstrated frequent avoidance behavior and concealment strategies.11,12 One-quarter of patients in the VALIANT study reported diagnosed depression, and approximately three-tenths reported anxiety, which may substantially affect health care resources.13 Furthermore, depression may be underdiagnosed, possibly owing to lack of access to mental health care, with more than half of patients in the VALIANT study reporting symptoms consistent with moderate to severe depression. Regional differences were observed in the burden of vitiligo and were particularly notable in India. There is reportedly a highly negative perception of vitiligo in India, with patients reporting how having vitiligo has affected their marriage prospects, education, and employment.14 These perceptions may be a reason why patients in India reported the greatest burden among all countries surveyed.
Limitations
This study has some limitations. For example, the VALIANT survey is limited by factors observed with other online surveys, including selection and recall biases and reliance on self-report of physician diagnosis. Also, patients with lower disease burden may have been less likely to complete the survey. Some questions may also have been misread or misunderstood by patients. For example, 35.5% of patients (1258 of 3541) reported feeling empowered by their vitiligo in contrast to clinical experience, in which most patients express considerable disempowerment.15 This result could be because terminology was interpreted differently across ethnic and national groups; therefore, translated survey validation across groups is warranted. Nonetheless, stratifications by BSA and skin type demonstrated similar trends in emotional well-being despite the fact that the questions were a mix of positive and negative characteristics. Finally, multivariate analysis was not undertaken; thus, confounding cannot be excluded.
Conclusions
In this qualitative study, the results of the VALIANT survey indicate that vitiligo affects patients’ daily lives, emotional well-being, and careers. Patients altered their behavior, expressed clear discontent, and had symptoms consistent with depression, which may be underdiagnosed. Patients with more than 5% affected BSA, darker skin, and facial or hand lesions reported being more affected than their counterparts. Findings highlight the need to prioritize reduction in the psychosocial burden of vitiligo and increase efforts to educate patients and health care professionals on vitiligo, particularly in countries where patients experience the highest burden.
eAppendix. Supplementary Methods
eTable 1. Vitiligo Impact Patient Scale
eReferences.
eTable 2. Characterization of Participant Survey Respondents
eFigure 1. Global VIPs Scores by Country
eFigure 2. Impact of Vitiligo on Self-Esteem, Relationships, and Careers Overall and by Affected BSA
eFigure 3. Formal Mental Health Diagnoses Among Patients With Vitiligo
eFigure 4. Moderate-to-Severe Depressive Symptoms as Assessed by the PHQ-9 in Patients With Vitiligo by Country
eFigure 5. Moderate-to-Severe Depressive Symptoms as Assessed by the PHQ-9 in Patients With Vitiligo by Geographic Region, Affected BSA, Fitzpatrick Skin Types, and Location of Lesions
Data Sharing Statement
References
- 1.Rodrigues M, Ezzedine K, Hamzavi I, Pandya AG, Harris JE; Vitiligo Working Group . New discoveries in the pathogenesis and classification of vitiligo. J Am Acad Dermatol. 2017;77(1):1-13. doi: 10.1016/j.jaad.2016.10.048 [DOI] [PubMed] [Google Scholar]
- 2.Silverberg JI, Silverberg NB. Association between vitiligo extent and distribution and quality-of-life impairment. JAMA Dermatol. 2013;149(2):159-164. doi: 10.1001/jamadermatol.2013.927 [DOI] [PubMed] [Google Scholar]
- 3.Picardo M, Huggins RH, Jones H, Marino R, Ogunsola M, Seneschal J. The humanistic burden of vitiligo: a systematic literature review of quality-of-life outcomes. J Eur Acad Dermatol Venereol. 2022;36(9):1507-1523. doi: 10.1111/jdv.18129 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ezzedine K, Eleftheriadou V, Jones H, et al. Psychosocial effects of vitiligo: a systematic literature review. Am J Clin Dermatol. 2021;22(6):757-774. doi: 10.1007/s40257-021-00631-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Amer AA, Gao XH. Quality of life in patients with vitiligo: an analysis of the Dermatology Life Quality Index outcome over the past two decades. Int J Dermatol. 2016;55(6):608-614. doi: 10.1111/ijd.13198 [DOI] [PubMed] [Google Scholar]
- 6.Wang G, Qiu D, Yang H, Liu W. The prevalence and odds of depression in patients with vitiligo: a meta-analysis. J Eur Acad Dermatol Venereol. 2018;32(8):1343-1351. doi: 10.1111/jdv.14739 [DOI] [PubMed] [Google Scholar]
- 7.Liu J, Tang R, Xiao Y, et al. Meta-analytic review of high anxiety comorbidity among patients with vitiligo. Biomed Res Int. 2021;2021:6663646. doi: 10.1155/2021/6663646 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Silverberg JI, Silverberg NB. Vitiligo disease triggers: psychological stressors preceding the onset of disease. Cutis. 2015;95(5):255-262. [PubMed] [Google Scholar]
- 9.Condamina M, Shourick J, Seneschal J, et al. Factors associated with perceived stress in patients with vitiligo in the ComPaRe e-cohort. J Am Acad Dermatol. 2022;86(3):696-698. doi: 10.1016/j.jaad.2021.02.083 [DOI] [PubMed] [Google Scholar]
- 10.Ezzedine K, Grimes PE, Meurant JM, et al. Living with vitiligo: results from a national survey indicate differences between skin phototypes. Br J Dermatol. 2015;173(2):607-609. doi: 10.1111/bjd.13839 [DOI] [PubMed] [Google Scholar]
- 11.Krüger C, Schallreuter KU. Stigmatisation, avoidance behaviour and difficulties in coping are common among adult patients with vitiligo. Acta Derm Venereol. 2015;95(5):553-558. doi: 10.2340/00015555-1981 [DOI] [PubMed] [Google Scholar]
- 12.Chen D, Tuan H, Zhou EY, Liu D, Zhao Y. Quality of life of adult vitiligo patients using camouflage: a survey in a Chinese vitiligo community. PLoS One. 2019;14(1):e0210581. doi: 10.1371/journal.pone.0210581 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Patel KR, Singam V, Rastogi S, Lee HH, Silverberg NB, Silverberg JI. Association of vitiligo with hospitalization for mental health disorders in US adults. J Eur Acad Dermatol Venereol. 2019;33(1):191-197. doi: 10.1111/jdv.15255 [DOI] [PubMed] [Google Scholar]
- 14.Pahwa P, Mehta M, Khaitan BK, Sharma VK, Ramam M. The psychosocial impact of vitiligo in Indian patients. Indian J Dermatol Venereol Leprol. 2013;79(5):679-685. doi: 10.4103/0378-6323.116737 [DOI] [PubMed] [Google Scholar]
- 15.Talsania N, Lamb B, Bewley A. Vitiligo is more than skin deep: a survey of members of the Vitiligo Society. Clin Exp Dermatol. 2010;35(7):736-739. doi: 10.1111/j.1365-2230.2009.03765.x [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix. Supplementary Methods
eTable 1. Vitiligo Impact Patient Scale
eReferences.
eTable 2. Characterization of Participant Survey Respondents
eFigure 1. Global VIPs Scores by Country
eFigure 2. Impact of Vitiligo on Self-Esteem, Relationships, and Careers Overall and by Affected BSA
eFigure 3. Formal Mental Health Diagnoses Among Patients With Vitiligo
eFigure 4. Moderate-to-Severe Depressive Symptoms as Assessed by the PHQ-9 in Patients With Vitiligo by Country
eFigure 5. Moderate-to-Severe Depressive Symptoms as Assessed by the PHQ-9 in Patients With Vitiligo by Geographic Region, Affected BSA, Fitzpatrick Skin Types, and Location of Lesions
Data Sharing Statement