Abstract
Introduction
This study aimed to compare the knowledge and skills of medical students in chronic pain assessment after being trained using the PQRST (P, provoke and palliate; Q, quality; R, region and radiation; S, severity; T, time) and ACT-UP (A, activity; C, coping; T, think; U, upset; P, people) mnemonics with those using only the PQRST mnemonic.
Methods
A double-blind, randomized controlled trial was conducted at the Faculty of Medicine, Universitas Indonesia, including forty students who participated in a simulation-based chronic pain assessment workshop. Pre- and post-test scores were used to assess participants’ knowledge. Two independent raters assessed the students’ skills.
Results
No significant differences in knowledge or skills were observed between the groups; however, a significant improvement in the post-test scores (85.71 [71.43–95.24]) compared to the pre-test scores (61.90 [25.87–90.48]) was observed. The students reported high satisfaction with the workshop.
Conclusions
Training with the PQRST and ACT-UP mnemonics is not better than training with the PQRST mnemonic alone in improving students’ knowledge and skills in chronic pain assessment. Nevertheless, this pain education workshop was beneficial for student learning. Learning of patient-oriented chronic pain assessment should be provided in a repetitive and integrative fashion using different approaches, such as lectures, demonstrations, simulations, and interactions with patients experiencing chronic pain. To conclude, mnemonics are helpful but not a primary learning tool.
Keywords: chronic pain assessment, PQRST, ACT-UP, pain education, randomized controlled trial
1. Introduction
Chronic pain affects psychological conditions, reduces productivity and daily activity, and significantly affects a patient's social and economic status (1, 2). The prevalence of chronic pain varies worldwide, with an estimate of 10.1%–55.2% of the adult populations, indicating that pain management initiatives frequently face barriers (1, 3).
One of these barriers is the lack of knowledge and skills among health professionals to comprehensively understand the subjective pain experienced by patients (4). Studies have shown that the competence of health professionals in pain-related assessment is inadequate (5, 6), and pain education is not a priority in their training curricula (7). Therefore, the paradigm of pain learning should change radically, focusing not only on biological aspects but also on psychosocial aspects (8, 9). An essential part of pain learning is pain assessment (10). Pain assessment is a process that involves dialogue between patients and health professionals regarding the description of pain and its intensity, patient's response to pain, and the impact of pain on patients’ lives (11). Although pain assessment has been discussed in the literature, research on this topic is still limited (12).
The PQRST mnemonic (P, provoke and palliate; Q, quality; R, region and radiation; S, severity; T, time) has been used for pain assessment in clinical practice and education (11, 13). Mnemonics offer several benefits. First, mnemonics are helpful for systematically memorizing and operationalizing concepts (14). Second, mnemonics are simple and fit well into the context of communication between patients and health professionals with time constraint (15). Nevertheless, the PQRST mnemonic focuses on the biomedical aspects of pain and is less supportive in exploring the psychosocial aspects of patients (11, 13).
Some experts have recommended the use of ACT-UP (A, activity; C, coping; T, think; U, upset; P, people) in patients with chronic pain. The ACT-UP mnemonic has an additional value in helping students conduct functional and psychosocial chronic pain assessments more comprehensively (16, 17). A combination of PQRST and ACT-UP is helpful and straightforward in guiding students to perform a comprehensive pain assessment. This can help students memorize and structure their history-taking process (18). However, the use of this combination for pain education has not yet been studied.
This study aimed to investigate whether pain assessment training using the PQRST and ACT-UP mnemonics is more effective than that with the PQRST mnemonic alone in improving the knowledge and skills of medical students. We hypothesized that pain assessment training using the PQRST and ACT-UP mnemonics is more effective in improving the knowledge and skills of medical students than the PQRST mnemonic alone. The results of this study could guide the development of pain education programs for students.
2. Materials and methods
We conducted a double-blind, randomized controlled trial. The study population comprised pre-clinical medical students in the Faculty of Medicine, Universitas Indonesia. Participants were chosen randomly from a list of third-year pre-clinical students. Eligibility criteria included students who completed modules on pain physiology, had basic knowledge of diseases causing pain in primary care, physical examinations, and communication skills. Students with experience in extracurricular chronic pain assessment training and those with chronic pain were excluded. Non-attendance or students who did not finish the workshops were considered as dropouts. Sample size was calculated based on a difference of five points, power of 90%, alpha of 5%, one-way, and dropout of 25%. The sample size was 40 for two groups of participants.
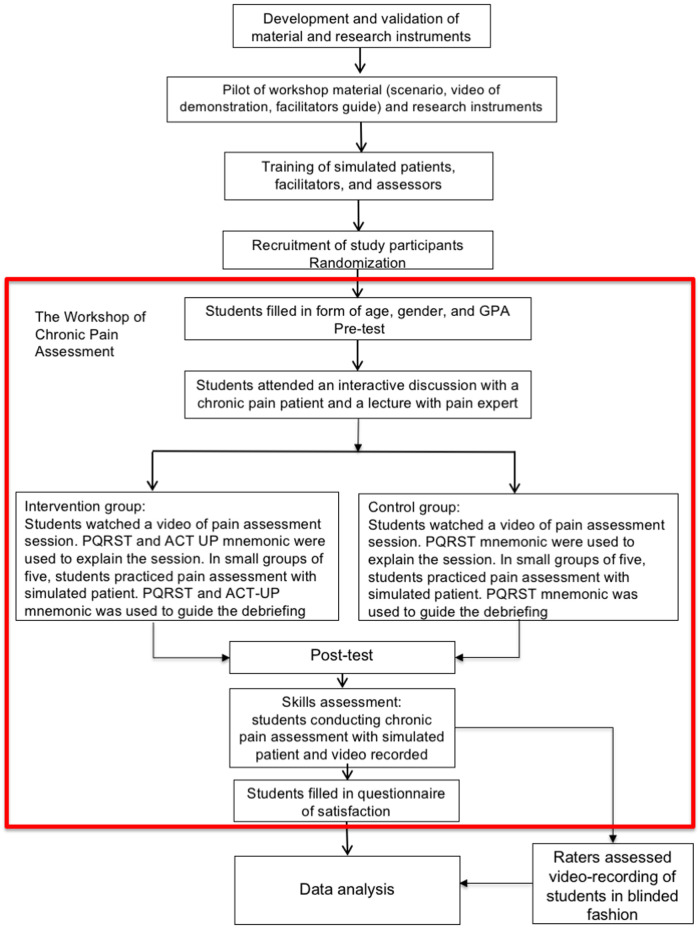
In this study, the competence of pain assessment was in concordance with the pain curriculum of International Association for the Study of Pain (IASP) (10) and the Indonesian Standard of Competence of Medical Doctors (19). The study process is described below and summarized in Figure 1.
Figure 1.
Study process.
2.1. Preparation
Learning materials and research instruments were developed based on the literature and discussion among the research team. The research instruments included (i) pre- and post-test scores to assess knowledge; (ii) a checklist to assess skills; and (iii) a questionnaire to assess student's satisfaction with the training (see Supplementary Files). The skill assessment scenario involved a case of low back pain. The instruments were validated by eight experts from Indonesia, the Netherlands, and USA. They were anesthesiologist and pain management physicians, family medicine physicians, and experts in medical education and communication skills training. One of them was the inventor of the ACT-UP mnemonics. The final drafts were translated into Indonesian language and back-translated into English language by an independent translator. Cultural and language comprehension was ensured by an independent bilingual third party with a background in anesthesiology.
Three national experts conducted a content validation. Aiken's V Coefficients (range, 0–1) were calculated for each item, with a score of >0.5 considered adequate (20, 21). The Aiken's V coefficient for the knowledge test was 0.78–1; for the checklist was 0.78–1, and for the questionnaire was 0.89–1. Finally, the instruments were piloted and their reliability was measured.
We conducted preparation courses for facilitators, raters, and simulated patients through lectures, demonstrations, and practice sessions. The raters piloted the checklist and measured its reliability.
2.2. Intervention
We conducted a one-day integrative workshop on chronic pain assessment in the Simulation-Based Medical Education and Research Center, Indonesia Medical Education and Research Institute. An independent party conducted the randomization. The students were blinded to the group allocation, but they knew that there were two learning approaches.
To ensure that both groups received equal intervention, all students participated in the first integrative sessions together. A patient with chronic pain shared her experiences of living with pain and its influence on functional and psychosocial conditions. An expert in pain management provided interactive lectures. The ACT-UP mnemonic was not used to ensure blinding.
Thereafter, the intervention and control groups were separated into two locations to maintain blinding. Each group underwent a demonstration of chronic pain assessment using a doctor-patient simulation video. There was a significant difference between the videos of the two groups. In addition to the explanation of the PQRST mnemonics and principles of comprehensive chronic pain assessment, the intervention group received an explanation of the PQRST and ACT-UP mnemonics in the video.
Subsequently, the students practiced pain assessment in small groups of five with one facilitator. Each student practiced a one-time simulation and provided feedback to the other group members. There were four scenarios, based on diseases (chronic low back pain or headache) and functional and psychosocial problems. We provided a flipchart with information on the mnemonics; the intervention group obtained information about the PQRST and ACT-UP mnemonics, whereas the control group obtained information about the PQRST mnemonic only. Differences in the use of mnemonics were also noted in the feedback session.
2.3. Data collection
The students completed the pre- and post-tests at the beginning of the training and at the end of the workshop. They conducted a chronic pain assessment on a simulated patient with back pain, which was video-recorded. Four raters, blinded to the group allocation, assessed the video recordings of the simulations. Each student was independently assessed by a pair of raters. At the end of the training, students completed questionnaires on satisfaction.
2.4. Data analysis
We used Statistical Package for the Social Sciences (SPSS) version 20.0 for data analysis. An independent t-test was used to compare means between the groups, or the Mann–Whitney U-test was applied when the data were not normally distributed. We compared pre- and post-test data using the Wilcoxon signed-rank test.
2.5. Ethical consideration
Ethical approval was granted by the Ethical Committee of the Faculty of Medicine, Universitas Indonesia and Cipto Mangunkusumo General Hospital (0467/UN2. F1/ETIK/2018). All the participants had the right to obtain information about the study and refuse to participate. Refusal did not influence the students’ academic assessments. Students who agreed to participate signed an informed consent form.
To ensure blinding, the students were informed about the different intervention approaches in the two groups; however, they were no given detailed information about the differences. Furthermore, the information sheet and consent form did not mention the PQRST or ACT-UP mnemonics. This concealment did not pose an additional risk to the students and was approved by the Ethical Committee.
3. Results
The participants’ flow chart is presented in Figure 2. Table 1 shows the comparable characteristics of the participants in each group. The pre- and post-tests consisted of 21 items with a split-half reliability of 0.70, showing moderate reliability (22). Table 2 shows a comparison of students’ knowledge and skills between the two groups. Knowledge was assessed by calculating the percentage of correct responses. Difference was obtained by subtracting the pre-test score from the post-test score. This difference was p = 0.066 or >0.025 (one-tail hypothesis). The skill assessment was used to obtain the skill score by calculating the total score × weight × 100 divided by the maximum score. The reliability test between raters showed an adequate agreement of Intraclass Correlation (ICC) 0.76 (23). This finding indicates that the knowledge and skill levels of students trained with the PQRST and ACT-UP mnemonics were not higher than those trained with the PQRST mnemonics only.
Figure 2.
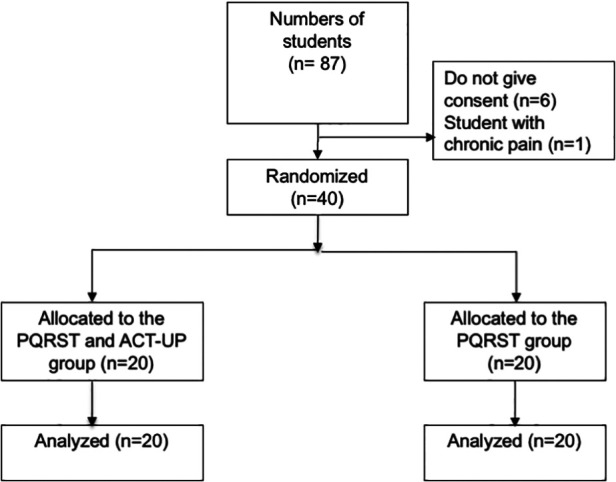
Participants’ flow chart.
Table 1.
Characteristics of students in both the groups.
| Characteristics | PQRST and ACT UP | PQRST |
|---|---|---|
| (n = 20) | (n = 20) | |
| Age (year)a | 20 (SD, 1) | 21 (SD, 0.5) |
| Genderb | ||
| Male | 12 (60) | 12 (60) |
| Female | 8 (40) | 8 (40) |
| Grade point averagea | 3.39 (SD, 0.14) | 3.39 (SD, 0.21) |
Data are presented as mean (SD).
Data is presented in n (%).
Table 2.
Comparison of students’ knowledge and skills between the two groups.
| PQRST and ACT-UP | PQRST | 95% CI from the mean difference | p-Value | |
|---|---|---|---|---|
| Knowledge | ||||
| Pre-test | 63.81 (SD, 14.69) | 66.67 (SD, 8.18) | 0.183a | |
| Post-test | 85.95 (SD, 6.08) | 82.14 (SD, 8.30) | 3.17 (−1.54–7.89) | 0.106b |
| Difference | 22.14 (SD, 12.29) | 15.47 (SD, 9.88) | 5.00 (−4.71–13.80) | 0.066b |
| Skills | 71.92 (SD, 7.26) | 74.00 (SD, 9.63) | −2.08 | 0.445b |
| −7.54 (SD, 3.38) | ||||
For the readers’ accessibility, all data are presented in mean (SD).
Mann–Whitney test.
Independent t-test.
However, there was a significant difference between the pooled group of 40 participants in their knowledge before and after the workshop (Table 3).
Table 3.
Comparison of students’ pre- and post-test scores.
| Knowledge | p-Value | |
|---|---|---|
| Pre-test | 61.90 (25.87–90.48) | 0.000a |
| Post-test | 85.71 (71.43–95.24) |
Wilcoxon signed-rank test.
In the satisfaction questionnaires, the participants responded on a scale of 1–4 to the question, “How do the following items support your learning process?” (1 = not very supportive, 2 = not supportive, 3 = supportive, 4 = very supportive). The questionnaire for the intervention group consisted of 15 items, while that of the controlled group consisted of only 14 items; the item “the use of ACT-UP mnemonic” was not asked. Therefore, the alpha coefficient of reliability was calculated using the questionnaire with 14 items. The alpha coefficient was 0.76 and was considered acceptable (24). The level of satisfaction in both the groups was high, with a median score of 3.8 (3.33–4) for the PQRST and ACT-UP group and 3.75 (3.07–4) for the PQRST group. The results of the questionnaire are presented in the Supplementary Material.
4. Discussion
This study aimed to investigate whether the incorporation of the ACT-UP mnemonic in pain assessment training could improve the knowledge and skills of medical students. The intervention and control groups were comparable. There were no significant differences in knowledge at the beginning of the intervention. After the training, there was no difference in skills or knowledge between the intervention and control groups. This showed that training with the PQRST and ACT-UP mnemonic was not better than training with only the PQRST mnemonic.
Theoretically, mnemonics work as a tool to help memorize and structure lines of thinking (14, 18, 24). Our result differs from those of the other studies that have compared the two mnemonics during training in an emergency context, showing that mnemonics are superior in supporting memory and organizing the causes of emergencies (14). The ACT-UP mnemonic, consisting of functional and psychosocial items, potentially helps students perform a comprehensive chronic pain assessment. However, our study showed that even without the ACT-UP mnemonic, students in the control group could perform a comprehensive pain assessment. Our results also showed a significant difference between the pre- and post-test scores and high post-test and skills test scores of the pooled group of 40 students.
These findings indicate that in our study, an additional mnemonic may not be necessary to improve students’ learning, or that our measurements may not have the sensitivity to illuminate the psychosocial and functional strengths of the ACT-UP mnemonic. We believe that the integrative approaches, structured from simple to complex, consisting of various methods, including talk shows with real patients, expert lectures, demonstrations, and simulations, are beneficial and adequate as learning tools. The students’ improvement was also attributed to the reinforcement of chronic pain assessment principles across various learning activities (25). A systematic review has shown that simulations can improve students’ skills (26), while interactions with patients with chronic pain provide exposure to real-world scenarios (27, 28). This result was consistent with the high satisfaction of students in both the groups. Students reported that the different integrative approaches used in this workshop supported learning.
This is the first empirical study on the ACT-UP mnemonic. Previous studies on the ACT-UP mnemonic have not included empirical data (16, 17). Additionally, previous studies on pain learning did not use control groups (29) or blinding (12, 28). Thus, the internal validity of this study was adequate. An independent party conducted the group allocation, and blinding was maintained for both the groups (23). Expert validation showed that the items measuring knowledge, skills, and satisfaction had good content validation. The reliability of these instruments is moderate and reasonable (24).
This study has some limitations. First, we limited the training to one day in order to maintain blinding and prevent students from communicating the differences between the interventions. Additionally, repeating the simulation was also difficult, owing to time constraints. Each student was able to conduct the simulation once and participate in the other four simulations in a group. Therefore, we could not assess the skills retention (30). Long-term training evaluation can be conducted when students are exposed to real patients during their clinical rotations. Second, this study was conducted at a single institution, and the adoption of this study should take into consideration the curriculum and student characteristics. Future studies should be conducted in other institutions, involving other health professionals or in a continuing education context.
In conclusion, to improve the knowledge and skills of medical students, training with the PQRST and ACT-UP mnemonics is not superior to that with the PQSRT mnemonic alone. Mnemonics are helpful, but they are not a primary learning tool. Patient-oriented chronic pain assessment learning should be integrated and provided repetitively using different approaches, such as lectures, demonstrations, simulations, and interaction with patients experiencing chronic pain.
Acknowledgments
We thank all students who participated this study. We also thank Simulated-Based Education and Research Center—Indonesian Medical Research and Education Institute (SIMUBEAR—IMERI), the Simulated Patients Community of Faculty of Medicine Universitas Indonesia, and the residents in the Department of Anesthesiology and Intensive Care FMUI for their support in the workshop. We also thank Aida Tantri, Pryambodho, Diantha Soemantri, Dennis Turk, Jan van Dalen, Marijke Kruithof, and Carine Vossen for their support in the instrument validation. We have presented some data from this study as a poster at the International Association for the Study of Pain (IASP) Virtual World Congress on Pain 2021.
Funding Statement
This work was supported by Faculty of Medicine Universitas Indonesia.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by The Ethics Committee of the Faculty of Medicine, Universitas Indonesia. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
RFS and APS initiated the study, RFS, BS, AF, and APS designed the study. BS and APS were in charge for data collection. All authors conducted the data analysis. APS drafted the manuscript and all authors approved the final version of the manuscript. All authors contributed to the article and approved the submitted version.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpain.2023.1210370/full#supplementary-material
References
- 1.Reid K, Harker J, Bala M, Truyers C, Kellen E, Bekkering G, et al. Epidemiology of chronic non-cancer pain in Europe: narrative review of prevalence, pain treatments and pain impact. Curr Med Res Opin. (2011) 27(2):449–62. 10.1185/03007995.2010.545813 [DOI] [PubMed] [Google Scholar]
- 2.Duenas M, Ojeda B, Salazar A, Mico J, Failde I. A review of chronic pain impact on patients, their social environment and the health care system. J Pain Res. (2016) 9:457–67. 10.2147/JPR.S105892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goldberg D, McGee S. Pain as a global public health priority. BMC Public Health. (2011) 11(1):770. 10.1186/1471-2458-11-770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Thompson K, Johnson MI, Milligan J, Briggs M. Twenty-five years of pain education research what have we learned? Findings from a comprehensive scoping review of research into pre-registration pain education for health professionals. Pain. (2018) 159(11):2146–58. 10.1097/j.pain.0000000000001352 [DOI] [PubMed] [Google Scholar]
- 5.Ung A, Salamonson Y, Hu W, Gallego G. Assessing knowledge, perceptions and attitudes to pain management among medical and nursing students: a review of the literature. Br J Pain. (2015) 10(1):8–21. 10.1177/2049463715583142 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Latchman J. Improving pain management at the nursing education level: evaluating knowledge and attitudes. J Adv Pract Oncol. (2014) 5(1):10–6. Available at : https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4093457/?report=reader [PMC free article] [PubMed] [Google Scholar]
- 7.Briggs E, Battelli D, Gordon D, Kopf A, Ribeiro S, Puig M, et al. Current pain education within undergraduate medical studies across Europe: advancing the provision of pain education and learning (APPEAL) study. BMJ Open. (2015) 5(8):e006984. 10.1136/bmjopen-2014-006984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Carr DB, Bradshaw YS. Time to flip the pain curriculum? Anesthesiology. (2014) 120:12–4. 10.1097/ALN.0000000000000054 [DOI] [PubMed] [Google Scholar]
- 9.Murinson B, Gordin V, Flynn S, Driver L, Gallagher R, Grabois M. Recommendations for a new curriculum in pain medicine for medical students: toward a career distinguished by competence and compassion. Pain Med. (2013) 14(3):345–50. 10.1111/pme.12051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fishman S, Young H, Lucas Arwood E, Chou R, Herr K, Murinson B, et al. Core competencies for pain management: results of an interprofessional consensus summit. Pain Med. (2013) 14(7):971–81. 10.1111/pme.12107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Powell RA, Downing J, Ddungu H, Mwangi-Powell FN. Pain history and pain assessment. In: Kopf A, Patel NB, editors. Guide to pain management in low-resource setting. Seattle: International Association for the Study of Pain (2010). [Google Scholar]
- 12.Willis MD. Communication skills for pain assessment and management: A pilot undergraduate medical curriculum targeting the public health problem of suboptimal pain management in current medical practice. [c]. Connecticut: University of Connecticut; (2010). [Google Scholar]
- 13.Susilo A, Sukmono R. Learning pain management during clinical medical education: a case report. Indones J Med Educ. (2022) 11(2):186. 10.22146/jpki.62757 [DOI] [Google Scholar]
- 14.Dyson E. Educational psychology in medical learning: a randomised controlled trial of two aide memoires for the recall of causes of electromechanical dissociation. Emerg Med J. (2004) 21(4):457–60. 10.1136/emj.2003.012377 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Claramita M, Utarini A, Soebono H, Van Dalen J, Van der Vleuten C. Doctor–patient communication in a southeast Asian setting: the conflict between ideal and reality. Adv Health Sci Educ Theory Pract. (2010) 16(1):69–80. 10.1007/s10459-010-9242-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dansie E, Turk D. Assessment of patients with chronic pain. Br J Anaesth. (2013) 111(1):19–25. 10.1093/bja/aet124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stanos S, Brodsky M, Argoff C, Clauw D, D’Arcy Y, Donevan S, et al. Rethinking chronic pain in a primary care setting. Postgrad Med. (2016) 128(5):502–15. 10.1080/00325481.2016.1188319 [DOI] [PubMed] [Google Scholar]
- 18.Findyartini A, Jusuf A, Menaldi LSWS, editors. Panduan praktis bagi pengajar klinis [practical guide for clinical teachers]. Jakarta: Sagung Seto; (2017). [Google Scholar]
- 19.Konsil Kedokteran Indonesia. Standar kompetensi dokter Indonesia [Indonesian doctor standard of competence]. Jakarta: Konsil Kedokteran Indonesia; (2012). [Google Scholar]
- 20.Aiken L. Three coefficients for analyzing the reliability and validity of ratings. Educ Psychol Meas. (1985) 45(1):131–42. 10.1177/0013164485451012 [DOI] [Google Scholar]
- 21.Harijanto E, Wijaya AA, Handayani D. Uji kesahihan dan keandalan QoR-40 versi Indonesia sebagai instrumen untuk menilai kualitas pemulihan pasca anestesi umum [Validity and reliability of the Indonesian version of QoR-40 as an instrument to assess the quality of post general anesthesia recovery]. Anaesth Crit Care. (2016) 34:101–8. Available at: https://macc.perdatin.org/index.php/my-journal/article/view/126 [Google Scholar]
- 22.Fraenkel JR, Wallen NE, Hyun HH. How to design and evaluate research in education. 8th ed. New York: McGraw Hill; (2012). [Google Scholar]
- 23.Koo TK, Li MY. A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med. (2016) 15:155–63. 10.1016/j.jcm.2016.02.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Reynolds P, Kamei R, Sundquist J, Khanna N, Palmer E, Palmer T. Using the practice mnemonic to apply cultural competency to genetics in medical education and patient care. Acad Med. (2005) 80(12):1107–13. 10.1097/00001888-200512000-00008 [DOI] [PubMed] [Google Scholar]
- 25.Frerejean J, van Merriënboer JJG, Kirschner PA, Roex A, Aertgeerts B, Marcellis M. Designing instruction for complex learning: 4C/ID in higher education. Eur J Educ. (2019) 54:513–24. 10.1111/ejed.12363 [DOI] [Google Scholar]
- 26.Ryall T, Judd B, Gordon CJ. Simulation-based assessments in health professional education: a systematic review. J Multidiscip Healthc. (2016) 9:69–82. 10.2147/JMDH.S92695 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sloan P, Plymale M, LaFountain P, Johnson M, Snapp J, Sloan D. Equipping medical students to manage cancer pain: a comparison of three educational methods. J Pain Symptom Manage. (2004) 27(4):333–42. 10.1016/j.jpainsymman.2003.08.006 [DOI] [PubMed] [Google Scholar]
- 28.Argyra E, Siafaka I, Moutzouri A, Papadopoulos V, Rekatsina M, Vadalouca A, et al. How does an undergraduate pain course influence future physicians’ awareness of chronic pain concepts? A comparative study. Pain Med. (2015) 16(2):301–11. 10.1111/pme.12568 [DOI] [PubMed] [Google Scholar]
- 29.Anderson D, Zlateva I, Coman E, Khatri K, Tian T, Kerns R. Improving pain care through implementation of the stepped care model at a multisite community health center. J Pain Res. (2016) 9:1021–9. 10.2147/JPR.S117885 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wayne D, McGaghie W. Skill retention after simulation-based education. J Grad Med Educ. (2013) 5(1):165–165. 10.4300/1949-8357-5.1.165 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.