Abstract
Objective
To compare the effectiveness of cyanoacrylate to other treatments or placebo in the management of dentin hypersensitivity (DH).
Materials and Methods
The present review was organized based on the preferred reporting items for systematic reviews and meta-analysis (PRISMA) guidelines. The search aimed to answer the following question: is cyanoacrylate effective in the treatment of DH when compared to other treatments or placebo? The following databases were used: PubMed/MEDLINE, Scopus, BVS, Web of Science, Cochrane, Clinicaltrials.gov, Portal Periódicos Capes, Google Scholar, and manual search. The evaluation process started with the information collected from the selected articles according to the Consolidated Standards of Reporting Trials (CONSORT).
Results
Two randomized and five nonrandomized clinical trials were analyzed in the qualitative synthesis. The studies presented different cyanoacrylate formulations, different scales for evaluating pain, and different methods for provoking a painful stimulus. Cyanoacrylate-based products reduce DH in shorter follow-up periods and this reduction persisted throughout the study. The results varied according to the methods used to stimulate the pain. Only two articles showed a low risk of bias and a high level of scientific evidence.
Conclusion
Although there is a limited number of studies in the scientific literature with appropriate methodological quality, the available evidence proves the effectiveness of cyanoacrylate in the treatment of DH. Clinical Relevance. Cyanoacrylate is easy to access, effective, easily applicable, and a low-cost product with satisfactory results.
1. Introduction
Dentin hypersensitivity (DH) is defined as a short and acute pain that appears from exposure to open dentin tubules [1]. It has been agreed that it is generated by chemical, thermal, tactile, or osmotic stimuli once it is not related to any other dental condition [2].
DH is one of the most common dental problems faced by dentists [3]. It could be caused by dental or periodontal damage as a result of enamel attrition and erosion, abrasion and abfraction, corrosion, periodontal tissue loss, or gingival recession [4–7]. Dental caries [8] and a fragile quantitatively defective enamel or hypomineralization [9] could also cause DH. In addition, other conditions could lead to dentin exposure and consequently unpleasant sensory experiences such as aggressive brushing, soft tissue dehiscence, and aging [7].
Several studies and theories have been proposed to explain how the stimuli could affect the dental pulp [10, 11]. Nowadays, it is widely accepted that the hydrodynamic theory could confirm the process involved in DH [12]. However, as different stimuli can affect the nerve fibers in different ways, researchers have contested how the hydrodynamic theory could explain all forms of DH. Evidence indicates that odontoblasts could play an important role in the mechanosensory mechanism associated with DH [13].
Although DH is a frequent dental issue, the prevalence presents a vast variation due to the different criteria to classify the same [14]. It is known that it could range from a minor inconvenience to the patient to a disturbance in the quality of life [15].
The wide number of treatment proposals is an obstacle to clinical professionals [14]. A large number of dental materials such as chemical components have been presented by pharmaceutical industries and recent research [16]. In this context, a few studies have tested the effectiveness of cyanoacrylate in reducing the symptoms presented in patients with DH [17, 18].
Cyanoacrylate adhesive is a commonly used material in medical sciences. Studies have shown its use in different areas of dentistry due to its properties [19]. From this evidence, this material has proved to be tolerated by human tissues, which could lead to the management of a large number of wounds in the oral cavity [20]. The role of cyanoacrylate in DH is related to its effective action in occluding the tubules preventing the displacement of fluids [18]. Thus, this agent could be a useful material to deal with DH as it is effective, easy to manipulate, and a low-cost product [15].
To verify how cyanoacrylate could be a viable therapy in the treatment of DH, this systematic review aimed to compare the effectiveness of cyanoacrylate to other treatments or placebo in the management of DH.
2. Materials and Methods
2.1. Protocol and Registration
The present review was organized based on the preferred reporting items for systematic reviews and meta-analysis (PRISMA) guidelines [21]. Furthermore, it was registered at PROSPERO with the protocol registration number: CRD42022370465.
2.2. Eligibility Criteria
This systematic review aimed to answer the following question: Is cyanoacrylate effective in the treatment of DH when compared to other treatments or placebo? The search was based on the following items of the PICOS question: population (any patient with DH not associated with pulpal and periodontal pathology), intervention (use of cyanoacrylate), comparator (any DH treatment or placebo), outcome (effectiveness of cyanoacrylate), and study design (randomized and nonrandomized clinical trials (RCTs)). Studies were excluded if they were observational studies, in vitro, animal studies, and review articles.
2.3. Search Strategy
All studies included in this review were obtained by an electronic search that took place in October 2022. The following databases were used: PubMed/MEDLINE, Scopus, BVS, Web of Science, Cochrane, Clinicaltrials.gov, Portal Periódicos Capes, Google Scholar, and manual search. No language limitation was considered to decrease the risk of language bias. All keywords were checked with the MeSH (Medical Subject Headings) database and then were used: (cyanoacrylate OR cyanoacrylates OR bucrylate OR enbucrilate) AND (dentin sensitivity OR dentin sensitivities OR dentine hypersensitivity OR dentin hypersensitivities OR dentin sensitivity OR dentin sensitivities OR tooth sensitivity OR tooth sensitivities OR DH OR dentin hypersensitivities). The search strategy has been presented in Table S1.
2.4. Study Selection
The articles underwent an independent and rigorous assessment by two reviewers (AST and OBLM) in two different stages. First, the reviewers independently selected all articles retrieved from the databases and manual search based on eligibility criteria after reading the titles and abstracts. Second, the full text of the selected papers was collected and appraised by the reviewers. Any disagreement about eligibility and any controversies between the two reviewers were resolved through a discussion to reach a consensus.
2.5. Data Extraction
The two authors extracted data from the selected studies and then double checked all the information. All the data obtained by the articles were tabulated with the following information: author and year of publication, country/region, study design, sample size, intervention, comparator, follow-ups, parameters of evaluation of hypersensitivity stimuli, and findings. The authors of the selected papers would be contacted at any time to provide insufficient data if necessary.
2.6. Risk of Bias
Two reviewers (MGT and KHS) independently evaluated the risk of bias. The evaluation process started with the information collected from the selected articles according to the Consolidated Standards of Reporting Trials (CONSORT). The data were tabulated following He et al. [22] and Belém et al. [23] with established criteria to qualify the methodology in different evidence levels. Studies were analyzed in five domains: sample size, randomization, allocation concealment, masking, and losses. The criterion was considered appropriate (A) when reported by the authors and explained. If it was only mentioned and not explained as B (partially reported). However, if it was not mentioned it was marked as C. Once all the criteria, or at least four, in the evaluated clinical trial were marked as A, it was rated as the level of evidence I. If it partially met the criteria (at most two evaluations C) it was rated as the level of evidence II and if it followed two criteria or less, it was rated as the level of evidence III (Table 1).
Table 1.
Risk of bias assessment.
| Author/Year/Country | Sample size | Randomization | Allocation concealment | Masking | Losses | EL |
|---|---|---|---|---|---|---|
| Flecha et al. [18, 24], Brazil | YES = A | YES = A | YES = A | YES = A | YES = A | I |
| Flecha et al. [18, 24], Brazil | NM = C | YES = A | YES = A | YES = A | YES = A | I |
| Naregal and Raju [27], India | NM = C | NM = C | NM = C | NM = C | YES = A | III |
| de la Caridad Perez-Alvarez et al. [17] Cuba | YES = A | NM = C | NM = C | NM = C | YES = A | III |
| Santos et al. [25] Brazil | NM = C | NM = C | NM = C | NM = C | YES = A | III |
| Guimarães [26] Brazil | NM = C | NM = C | NM = C | NM = C | YES = A | III |
| Javid et al. [28] Iran | NM = C | NM = C | NM = C | NM = C | YES = A | III |
Note. Table template reference: Belém et al. [23]. Abbreviations: EL, evidence level; NM, not mentioned.
3. Results
Initially, 76 papers were found in the databases. After removing duplicates, 33 papers were screened based on titles and abstracts. A total of 13 studies remained and were assessed for full-text evaluation. Hence, six papers and one specialization final paper were analyzed for qualitative synthesis (Figure 1). The characteristics of the included studies are presented in Table 2.
Figure 1.
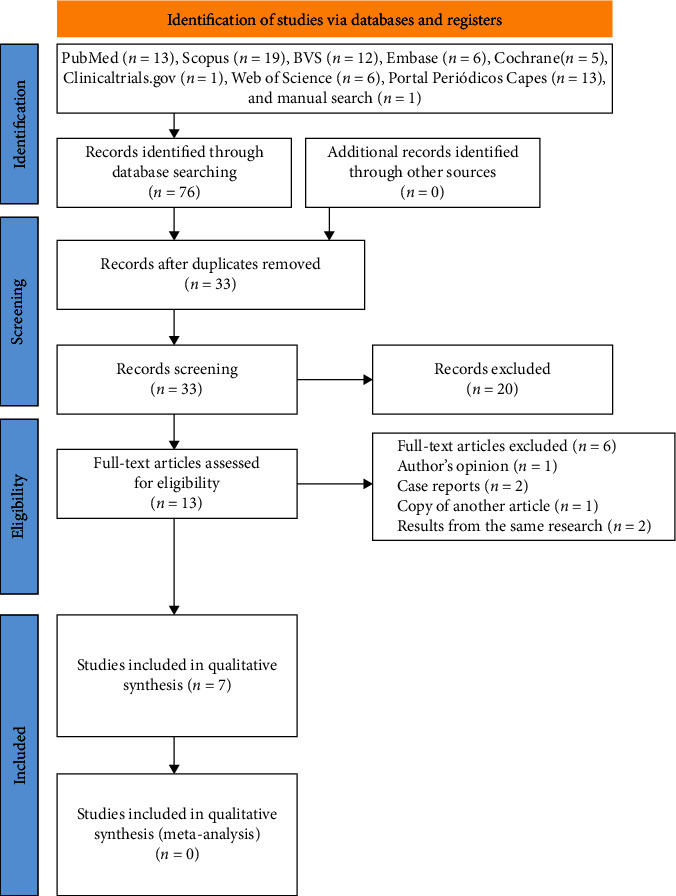
PRISMA flowchart showing the screening of the articles.
Table 2.
Characteristics of selected studies.
| Author/Year/Country/Study design | Sample size | Interventions/protocols | Evaluations/follow-up | Findings |
|---|---|---|---|---|
| Flecha et al., [18, 24]/Brazil/RCT, Double-blind, split-mouth | 434 Teeth | TG - Super Bonder® CG - LLLT Protocol: 3x 48/48 hs |
NRS: - Air spray = 4s - Tetrafluormethan spray (Endo Ice®) = 4s Baseline, 24 hr, 30, 90, and 180 days |
Reduction in DH ≠ a significant. Within 24 hr better results were recorded for cyanoacrylate |
|
| ||||
| Flecha et al., [18, 24]/Brazil/RCT, Double-blind, split-mouth -Pilot study | 34 Hemiarch | TG - Super Bonder® CG - LLLT Protocol: 3x 48/48 hs |
NRS: - Air spray = 5s - Tetrafluormethan spray (Endo Ice®) = 5s Baseline, 24 hr, 30, and 120 days |
TG = Endo-Ice: 24 hr ≠ significant TG = Air blast: 120 days ≠ significant CG = Endo-Ice: 120 days ≠ significant |
|
| ||||
| Naregal and Raju [27]/Índia/NRCT | 45 Teeth 15 Patients |
G1 (CG) = Distilled water G2 = Potassium oxalate 30% G3—N-butyl 2-cyanoacrylate Protocol: 1 min |
VAS: - Tactile stimuli - Electrical stimulation Baseline, immediate and once a week for 12 weeks |
Tactile stimulus: G2 and G3 = ≠ significant 7 weeks G2 = w/o DH until end Electrical stimulation: G2 and G3 = ≠ significant 6 weeks G3 = > DH reduction |
|
| ||||
| de la Caridad Perez-Alvarez et al. [17]/Cuba/NRCT | 152 Patients | - Chlorhexidine 0,2% = 1 min - Tisuacryl® = 60s |
Pain evaluation: Level 1 = absence Level 2 = pain remains 2, 4, 5 e 6 days after intervention |
Treatment with Tisuacryl: was successful in 96.7% of patients: Severe DH = 81.5% Light/moderate = 100% |
|
| ||||
| Santos et al. [25]/Brazil/NRCT | 655 Teeth 73 Patients |
G1: Super Bonder® = 1 G2: Prime & Bond 2.1 = 1 G3: Super Bonder® = 4 G4: Prime & Bond 2.1 = 4 |
- Mechanical stimuli = exploratory probe n 5 - Thermal stimuli = air spray/Endo Ice® Baseline, weekly, and 60 days |
Groups 3 and 4: statistically significant results in DH reduction |
|
| ||||
| Guimarães [26]/Brazil/NRCT | 60 Teeth 23 Patients |
G1: Fluorniz® = 4 G2: Super Bonder® = 1 |
- Mechanical stimuli = exploratory probe - Thermal stimuli = water spray/air spray 7/7 days - 3 weeks |
Super Bonder® Group: 93.3% - DH reduction Fluorniz® Group: 90% - DH reduction |
|
| ||||
| Javid et al. [28]/Iran/NRCT | 60 Patients | G1: NaF 33% = 6 G2: cyanoacrylate = 1 |
- Air spray for 1s 24 hr and weekly (6x) |
Cyanoacrylate group: 25 = immediate and continuous relief. Fluoride Group: 21 = had lower scores than initial |
Note. Table template font: Belém et al. [23]. Abbreviations: CG, control group; DH, dentin hypersensitivity; LLLT, low-level laser therapy; NaF, sodium fluoride; NRCT, nonrandomized clinical trial; NRS, Numerical Rating Scale; RCT, randomized clinical trial; TG, test group; VAS, Visual Analoge Scale.
Two studies were RCTs and five were nonrandomized. Regarding the number of participants, it ranged from 11 [24] to 152 patients [17]. Only one study described how sample size calculation was performed [18].
Some studies used ethyl cyanoacrylate [18, 24–26], others N-butyl-2-cyanoacrylate, in the treatment of dental hypersensitivity [17, 27] and only one study did not refer to the brand or chemical composition of the cyanoacrylate used in the experimental group [28].
de la Caridad Perez-Alvarez et al. [17] did not compare the use of cyanoacrylate with another material. The other studies compared the efficacy of cyanoacrylate with low-level laser [18, 24], potassium oxalate 30% [27], Prime & Bonder [25], 33% sodium fluoride [28], and 5% fluoride varnish [26] for the treatment of DH.
The studies used different scales for pain assessment, such as Numerical Rating Scale (NRS) [18, 24], Visual Analog Scale [27], pain Level 1 and Level 2 [17], and discomfort levels from 0 to 3 [26, 28]. In addition, there were differences regarding the methods used to provoke the painful stimuli and different results for the different stimuli, such as cold air jet, Endo Ice, tactile stimulus, electrical stimulus, and mechanical stimulus.
It was found that cyanoacrylate-based products reduce DH in shorter follow-up times and this reduction persisted throughout the study and the results varied according to the methods used to the stimulate pain.
Only two articles in this review had a low risk of bias and a high level of scientific evidence [18, 24] (Table 1).
4. Discussion
Cyanoacrylate is a biocompatible compound that can block dentin tubules, which could be used in the treatment of DH [18, 28]. However, there is scarce evidence in the literature. This review found a few studies comparing the use of cyanoacrylate to other treatments, such as laser therapy, the use of adhesive systems, and compounds containing fluorine or potassium oxalate.
All evaluated studies have shown positive results regarding the use of cyanoacrylate in the treatment of DH. On the other hand, the papers that presented evidence level III must be interpreted with caution as the studies could present methodological bias [29].
RCT is considered the second level of evidence for clinical decisions and the gold-standard study design to evaluate the health interventions [29]. The low-methodological quality found in most of the studies could be explained by the fact that five papers [17, 25–28] are non-RCTs, which were evaluated with evidence level III. In RCTs, the randomization process could achieve results without bias among groups exposed to different forms of treatments. Also, to ensure that the results could not be affected by the participants' characteristics, the random assignment is performed in all groups [30].
In addition to randomization, other criteria are important to classify the levels of evidence in the present review. The sample size is important to determine the precise amount to obtain valid results [31]; the allocation concealment protects the assignment sequence until interventions, which prevents selection bias [32]; masking avoids subjectivities [33], determination bias and it controls the observer bias and protects the sequence after allocation [32]; finally, losses of participants could interfere in the initial equivalence in both experimental and control groups due to the absences [30].
Regarding the heterogeneity of the different interventions, all studies compared the effectiveness of cyanoacrylate for the treatment of DH [17, 18, 24–28]. All studies have shown satisfactory results regarding the use of cyanoacrylate in DH, although the response varied according to the method used to stimulate pain. The comparison of potassium oxalate 30% and cyanoacrylate showed better results for the oxalate after the 7th week of evaluating tactile stimuli and the absence of hypersensitivity until the end of the study [27]. When the results of electrical stimuli were evaluated, the difference was statistically significant until 6 weeks for both groups (experimental and control). The cyanoacrylate group showed a greater reduction in DH than potassium oxalate 30% [27].
The study comparing cyanoacrylate to laser therapy found a significant reduction in DH. The cyanoacrylate group showed a reduction in 24 hr (Endo Ice) and 120 days (air spray), while the laser therapy group showed its best efficacy in 120 days (Endo Ice) [24]. In the results presented by Flecha et al. [18], there was a statistically significant difference in the intergroup comparison only in 24 hr for the air spray and Endo Ice. In addition, it has been shown that during the other follow-ups, the air spray and Endo-Ice stimuli did not present any differences between the cyanoacrylate and laser therapy groups. It proves the noninferiority of cyanoacrylate in relation to the laser therapy [18].
The included studies used different follow-ups ranging from a total of 6 [17] to 180 days [18]. Also, it was found a significant reduction in pain immediately after the application of both potassium oxalate and cyanoacrylate [27] and 24 hr after the application of cyanoacrylate compared to 6 weeks of application of a paste of sodium fluoride 33% [28].
The studies performed reapplication of the interventional methods if the symptoms of DH remained [17, 27]. In the study of Flecha et al. [18, 24], authors applied three sessions at intervals of 48 hr for both laser and cyanoacrylate. Santos et al. [25] performed applications in a single session and four sessions. In the study conducted by Guimarães [26] three applications took place in three weeks. In these last two studies, significant reductions in DH after the reapplication of cyanoacrylate were observed. In the study by Javid [28], cyanoacrylate was reapplied after 6 weeks due to sensitivity caused by the erosion and abrasion.
The present review had notable strengths. First, this study conducted an electronic and manual search in the main available databases. Second, it followed a methodologic rigor to evaluate the level of evidence of the selected studies. All these points were important to ensure that the review has high-internal validity.
Some factors contributed to the limitations in this study such as the high heterogeneity in the interventions, low level of evidence of the selected studies, low number of available reports, different evaluation methods and follow-ups, and cyanoacrylate in different formulations. Therefore, it is difficult to compare the studies with different methodologies.
Cyanoacrylate is a useful compound that could be used in an emergency, it is easy to access, effective, easily applicable, and a low-cost product with satisfactory results [34]. Regarding these advantages, it is still necessary for more studies using this product in the treatment of DH, with a high-methodologic rigor to ensure a high level of evidence once there is not yet a gold standard treatment for DH [35, 36].
Recent systematic reviews concluded that the best therapy for DH seems to be an association of protocols with physical (laser) and chemical agents (neural agents and blockers), in addition to a detailed anamnesis and physical examination that allow an individualized treatment plan [36, 37]. Currently, therapies are capable of reducing DH in the short and medium term [37]. Several studies have been carried out using biomimetic hydroxyapatite. RCT studied the use of biomimetic hydroxyapatite in dentifrices and found favorable results in the reduction of hypersensitivity/pain values, superior to conventional dentifrices with fluoride [38]. Furthermore, an updated systematic review and meta-analysis concluded that the use of biomimetic hydroxyapatite in oral care products is a safer and more effective agent than fluoride in controlling dentin hypersensitivity and may be superior to other desensitizers [39]. Therefore, it is suggested that new RCTs compare cyanoacrylates with other desensitizing agents with methodological rigor and short, medium, and long-term follow-up times.
5. Conclusion
Although there are a few studies in the scientific literature of good methodological quality on the effectiveness of cyanoacrylate in the treatment of DH, all studies found that this material proves to be effective for this purpose.
Acknowledgments
The authors are grateful to the Postgraduate Research Program UFVJM where the present work was carried out. This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) and Fundo de Amparo à Pesquisa do Estado de Minas Gerais (FAPEMIG).
Data Availability
Data supporting this review article are available on request from the authors.
Conflicts of Interest
The authors declare no competing interests.
Authors' Contributions
AST, OBLM, and RPO contributed in the article selection and review writing. KHS contributed in the translation, writing and approval of the final version of the manuscript. MGT contributed in the abstract formatting and submission. PF and KHS contributed in the review writing. ODF contributed in the general orientation of the research, revision, and approval of the final version of the manuscript. AST, OBLM, RPO, KHS and ODF contributed equally to this work.
Supplementary Materials
Table S1. Databases and search strategy.
References
- 1.Holland G. R., Narhi M. N., Addy M., Gangarosa L., Orchardson R. Guidelines for the design and conduct of clinical trials on dentine hypersensitivity. Journal of Clinical Periodontology . 1997;24(11):808–813. doi: 10.1111/j.1600-051X.1997.tb01194.x. [DOI] [PubMed] [Google Scholar]
- 2.Addy M. Dentine hypersensitivity: new perspectives on an old problem. International Dental Journal . 2002;52(5):367–375. doi: 10.1002/j.1875-595X.2002.tb00936.x. [DOI] [Google Scholar]
- 3.Pashley D. H. How can sensitive dentine become hypersensitive and can it be reversed? Journal of Dentistry . 2013;41(S4):S49–S55. doi: 10.1016/S0300-5712(13)70006-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Grippo J. O., Simring M., Schreiner S. Attrition, abrasion, corrosion and abfraction revisited: a new perspective on tooth surface lesions. The Journal of the American Dental Association . 2004;135(8):1109–1118. doi: 10.14219/jada.archive.2004.0369. [DOI] [PubMed] [Google Scholar]
- 5.Lussi A., Schaffner M. Progression of and risk factors for dental erosion and wedge-shaped defects over a 6-year period. Caries Research . 2000;34(2):182–187. doi: 10.1159/000016587. [DOI] [PubMed] [Google Scholar]
- 6.Addy M., Absi E. G., Adams D. Dentine hypersensitivity. Journal of Clinical Periodontology . 1987;14(5):274–279. doi: 10.1111/j.1600-051X.1987.tb01532.x. [DOI] [PubMed] [Google Scholar]
- 7.Grippo J. O. Abfractions: a new classification of hard tissue lesions of teeth. Journal of Esthetic and Restorative Dentistry . 1991;3(1):14–19. doi: 10.1111/j.1708-8240.1991.tb00799.x. [DOI] [PubMed] [Google Scholar]
- 8.Butera A., Maiorani C., Morandini A., et al. Assessment of genetical, pre, peri and post natal risk factors of deciduous molar hypomineralization (DMH), hypomineralized second primary molar (HSPM) and molar incisor hypomineralization (MIH): a narrative review. Children . 2021;8(6) doi: 10.3390/children8060432.432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Butera A., Maiorani C., Morandini A., et al. Evaluation of children caries risk factors: a narrative review of nutritional aspects, oral hygiene habits, and bacterial alterations. Children . 2022;9(2) doi: 10.3390/children9020262.262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Absi E. G., Addy M., Adams D. Dentine hypersensitivity. Journal of Clinical Periodontology . 1987;14(5):280–284. doi: 10.1111/j.1600-051X.1987.tb01533.x. [DOI] [PubMed] [Google Scholar]
- 11.Goh V., Corbet E. F., Leung W. K. Impact of dentine hypersensitivity on oral health-related quality of life in individuals receiving supportive periodontal care. Journal of Clinical Periodontology . 2016;43(7):595–602. doi: 10.1111/jcpe.12552. [DOI] [PubMed] [Google Scholar]
- 12.Liu X., Yu L., Wang Q., et al. Expression of Ecto-ATPase NTPDase2 in human dental pulp. Journal of Dental Research . 2012;91(3):261–267. doi: 10.1177/0022034511431582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Solé-Magdalena A., Martínez-Alonso M., Coronado C. A., Junquera L. M., Cobo J., Vega J. A. Molecular basis of dental sensitivity: the odontoblasts are multisensory cells and express multifunctional ion channels. Annals of Anatomy - Anatomischer Anzeiger . 2018;215:20–29. doi: 10.1016/j.aanat.2017.09.006. [DOI] [PubMed] [Google Scholar]
- 14.West N. X., Lussi A., Seong J., Hellwig E. Dentin hypersensitivity: pain mechanisms and aetiology of exposed cervical dentin. Clinical Oral Investigations . 2013;17(S1):9–19. doi: 10.1007/s00784-012-0887-x. [DOI] [PubMed] [Google Scholar]
- 15.Lima T. C., Vieira-Barbosa N. M., de Sá Azevedo C. G., et al. Oral health-related quality of life before and after treatment of dentin hypersensitivity with cyanoacrylate and laser. Journal of Periodontology . 2017;88(2):166–172. doi: 10.1902/jop.2016.160216. [DOI] [PubMed] [Google Scholar]
- 16.Schmidlin P. R., Sahrmann P. Current management of dentin hypersensitivity. Clinical Oral Investigations . 2013;17(S1):55–59. doi: 10.1007/s00784-012-0912-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.de la Caridad Perez-Alvarez M., Guerra-Bretaña R. M., Fernandez-Diaz M. I., et al. Effectiveness and safety of tisuacryl in treating dentin hypersensitivity (DH) MEDICC Review . 2010;12(1):24–28. doi: 10.37757/MR2010.V12.N1.5. [DOI] [PubMed] [Google Scholar]
- 18.Flecha O. D., Azevedo C. G. S., Matos F. R., et al. Cyanoacrylate versus laser in the treatment of dentin hypersensitivity: a controlled, randomized, double-masked and non-inferiority clinical trial. Journal of Periodontology . 2013;84(3):287–294. doi: 10.1902/jop.2012.120165. [DOI] [PubMed] [Google Scholar]
- 19.Lehman R. A. W., Hayes G. J., Leonard F. Toxicity of alkyl 2-cyanoacrylates. I peripheral nerve. Archives of Surgery . 1966;93(3):441–446. doi: 10.1001/archsurg.1966.01330030071016. [DOI] [PubMed] [Google Scholar]
- 20.Woodward S. C., Herrmann J. B., Cameron J. L., Brandes G., Pulaski C. E. J., Leonard F. Histotoxicity of cyano acrylate tissue adhesive in the rat. Annals of Surgery . 1965;162(1):113–122. doi: 10.1097/00000658-196507000-00017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Moher D., Liberati A., Tetzlaff J., Altman D. G., The PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLOS MEDICINE . 2009;6(7) doi: 10.1371/journal.pmed.1000097.e1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.He S., Wang Y., Li X., Hu D. Effectiveness of laser therapy and topical desensitising agents in treating dentine hypersensitivity: a systematic review. Journal of Oral Rehabilitation . 2011;38(5):348–358. doi: 10.1111/j.1365-2842.2010.02193.x. [DOI] [PubMed] [Google Scholar]
- 23.Belém L. M., Silva L. D. A., Douglas-de-Oliveira D. W., Gonçalves P. F., Flecha O. D. Uso da laserterapia no tratamento de pacientes com paralisia de bell: revisão crítica da literatura. Revista Portuguesa de Estomatologia Medicina Dentária e Cirurgia Maxilofacial . 2021;62(2):81–86. doi: 10.24873/j.rpemd.2021.06.832. [DOI] [Google Scholar]
- 24.Flecha O. D., Douglas de Oliveira D. W., Azevedo C. G. S., et al. Cianoacrilato como uma nova abordagem para a hipersensibilidade dentinária - um ensaio clínico-piloto. Perionews . 2013;7(5):488–494. [Google Scholar]
- 25.Santos R. L., Gusmäo E. S., Caldas Júnior A. F., Silveira R. C. J. Uso do etil-cianoacrilato e Prime & Bond 2.1 em dentes hipersensíveis pós terapia periodontal. Revista Brasileira de Odontologia . 2003;60(1):27–29. [Google Scholar]
- 26.Guimarães J. A. Estudo comparativo da eficiência do verniz com flúor a 5% (fluorniz) e do cianoacrilato (super-bonder) no tratamento da hipersensibilidade dentinária cervical. 2020. Monografia, Faculdade de Odontologia da União Educacional do Planalto Central.
- 27.Naregal G., Raju C. Comparative assessment of efficacy of a single application of potassium oxalate and N-butyl 2-cyanoacrylate in treatment of hypersensitive teeth—a clinical study. Indian Journal of Public Health Research and Development . 2012;3(2):20–24. [Google Scholar]
- 28.Javid B., Barkhordar R. A., Bhinda S. V. Cyanoacrylate—a new treatment for hypersensitive dentin and cementum. The Journal of the American Dental Association . 1987;114(4):486–488. doi: 10.14219/jada.archive.1987.0092. [DOI] [PubMed] [Google Scholar]
- 29.Flecha O. D., de Oliveira D. W. D., Marques L. S., Gonçalves P. F. A commentary on randomized clinical trials: how to produce them with a good level of evidence. Perspectives in Clinical Research . 2016;7(2):75–80. doi: 10.4103/2229-3485.179432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Polit D. F., Gillespie B. M. Intention-to-treat in randomized controlled trials: recommendations for a total trial strategy. Research in Nursing & Health . 2010;33(4):355–368. doi: 10.1002/nur.20386. [DOI] [PubMed] [Google Scholar]
- 31.Editorial. Importância do cálculo amostral em pesquisa científica [Editorial] Revista de cirurgia e Traumatologia Buco Maxilo Facial . 2005;5(3)7 [Google Scholar]
- 32.Schulz K. F. Randomised trials, human nature, and reporting guidelines. The Lancet . 1996;348(9027):596–598. doi: 10.1016/S0140-6736(96)01201-9. [DOI] [PubMed] [Google Scholar]
- 33.de Lourdes Veronese Rodrigues M. Estudos “cegos” ou “mascarados”? Medicina (Ribeirão Preto) . 2000;33(1):1–2. doi: 10.11606/issn.2176-7262.v33i1p1-2. [DOI] [Google Scholar]
- 34.Kaplan M., Bozkurt S., Kut M. S., Kullu S., Demirtas M. M. Histopathological effects of ethyl 2-cyanoacrylate tissue adhesive following surgical application: an experimental study. European Journal of Cardio-Thoracic Surgery . 2004;25(2):167–172. doi: 10.1016/j.ejcts.2003.11.016. [DOI] [PubMed] [Google Scholar]
- 35.Douglas-de-Oliveira D. W., Paiva S. M. D., Cota L. O. M. Etiologia, epidemiologia e tratamento da hipersensibilidade dentinária: uma revisão de literatura. Periodontia . 2017;27(4):76–85. [Google Scholar]
- 36.Mendes S. T. C., Pereira C. S., de-Oliveira J. L., Santos V. C. S., Gonçalves B. B., Mendes D. C. Tratamento da hipersensibilidade dentinária com laser. Brazilian Journal of Pain . 2021;4(2):152–160. doi: 10.5935/2595-0118.20210025. [DOI] [Google Scholar]
- 37.Marto C. M., Paula A. B., Nunes T., et al. Evaluation of the efficacy of dentin hypersensitivity treatments—a systematic review and follow-up analysis. Journal of Oral Rehabilitation . 2019;46(10):952–990. doi: 10.1111/joor.12842. [DOI] [PubMed] [Google Scholar]
- 38.Butera A., Gallo S., Pascadopoli M., et al. Home oral care with biomimetic hydroxyapatite vs. conventional fluoridated toothpaste for the remineralization and desensitizing of white spot lesions: randomized clinical trial. International Journal of Environmental Research and Public Health . 2022;19(14) doi: 10.3390/ijerph19148676.8676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Limeback H., Enax J., Meyer F. Clinical evidence of biomimetic hydroxyapatite in oral care products for reducing dentin hypersensitivity: an updated systematic review and meta-analysis. Biomimetics . 2023;8(1) doi: 10.3390/biomimetics8010023.23 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1. Databases and search strategy.
Data Availability Statement
Data supporting this review article are available on request from the authors.


