Abstract
Introduction and importance
Colorectal intussusception can be quite challenging to identify, especially its malignant nature. This is a fairly rare presentation and hence, there is not much associated research or cases reported in the literature.
Case presentation
We present a 69 year old male with lower abdominal pain and a significant rectal prolapse. He has a background history of heavy smoking and significant alcohol intake. The prolapse was irreducible and had papillomatous changes present on the prolapsed mucosa. A computerized tomography (CT) scan demonstrated a large rectal prolapse followed by a Magnetic Resonance Imaging (MRI) Pelvis which showed an intussusception at the S2–3 level, consistent with a carcinoma, The patient then proceeded to have a flexible sigmoidoscopy with a planned proceed to an anterior resection. Histopathology revealed sigmoid and descending colon adenocarcinoma with mucinous differentiation pT3N0. He had an unremarkable hospital stay and remained well on follow up. His case was discussed at the multidisciplinary meeting and was not for any adjuvant chemotherapy.
Clinical discussion
Imaging can help aid early diagnosis of a colorectal intussusception. Colonoscopies can be useful too; however these can be tricky to diagnose pre-operatively. If there is a high suspicion of malignancy, routine resection is the preferred method of treatment in cases of colorectal intussusception.
Conclusion
Although not a very common presentation, diagnosis of colorectal cancer presenting as an intussusception can be dealt with imminently by considering operative measures.
Keywords: Rectal intussusception, Rectal prolapse, Anterior resection, Malignancy, Case report
Highlights
-
•
Intussusception is more common in children than in adults.
-
•
Rectal prolapse is a rare presentation of rectal intussusception.
-
•
Timely intervention is required if the rectal prolapse is suspicious for malignancy.
-
•
If suspicious for cancer, a colonic resection is considered vital.
-
•
Laparoscopic resection has been shown to have benefits compared to open surgery.
1. Introduction
Intussusception in adults is rare compared to children, moreover colorectal intussusception is very rare compared to those occurring more proximal [1]. Intussusception is 20 times more frequent in children compared to adults [2]. Adult intussusception is rare and accounts for only 1–5 % of bowel obstructions [3].
It is normally caused by a lead point which could be due to any of the following causes: neoplasm, post-surgical adhesion, ulceration or diverticulum [2]. These lead points can get caught in an adjacent bowel segment and subsequently be pulled forward by peristalsis. The affected bowel then becomes oedematous as the intussusception increases, and can lead to ischaemia and necrosis if it is left untreated due to compromised blood flow [2].
Patients with intussusception can present with very chronic and nonspecific symptoms such as abdominal pain, nausea, vomiting, constipation and gastrointestinal bleeding [4]. Rectal prolapse is an even more rare presentation of intussusception [4] and our case report will present one such case. This becomes important when a rectal prolapse is actually mimicking a malignancy and hence timely diagnosis and intervention becomes challenging.
There are not many cases reported in the literature regarding many colorectal malignancies presenting as an intussusception. Adult intussusception in the colon is less common than that in the small bowel, accounting only for about 20–25 % of all intussusceptions [3].
This case report has been produced in keeping with the SCARE criteria [5].
2. Case
We present the case of GS, a 69 year old male presenting to a regional hospital in New South Wales; with lower abdominal pain and significant rectal prolapse. The prolapse had progressed over 3–4 months, and until presentation had self-reduced. The patient has a background of heavy smoking and alcohol intake. He had never previously had a colonoscopy.
On presentation the prolapse protruded about 10 cm and was irreducible. There were papillomatous changes present on the prolapsed mucosa; with no evidence of ischaemia. Multiple biopsies were taken, histopathology of which revealed a low grade ulcerated adenocarcinoma.
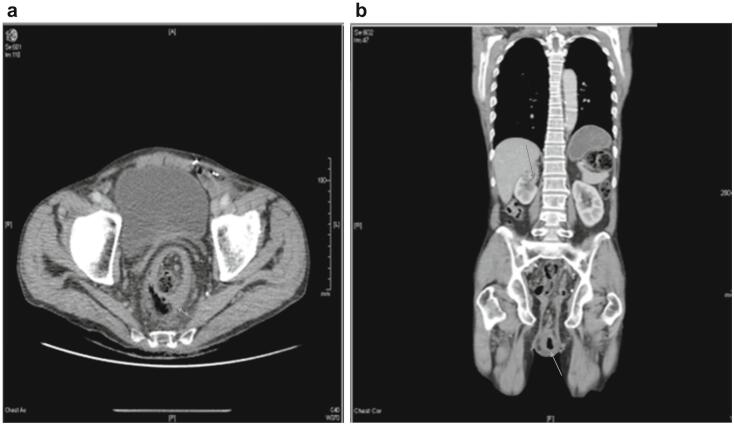
A Computer Tomography (CT) Abdomen Pelvis was performed which revealed a large rectal prolapse (Fig. 1A & B) as well as an incidental finding of a 4.9 × 2.4 × 3.1 cm mass arising from the superior pole of the right kidney (Fig. 1B).
Fig. 1.
1A and 1B demonstrating rectal prolapse on CT (white arrows). Fig. 1B also demonstrates the incidental right renal mass (grey arrow).
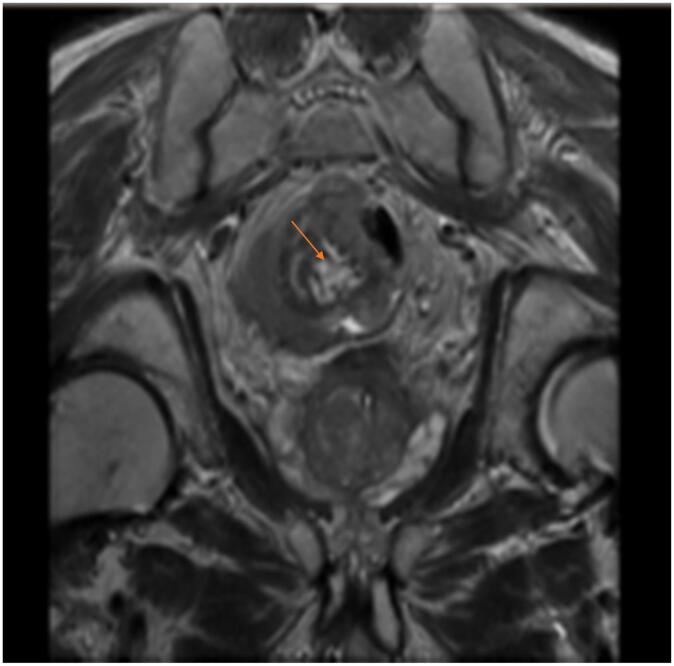
A Magnetic Resonance Imaging (MRI) pelvis was performed shortly after following the reduction of the prolapse. It showed an intussusception situated at approximately S2–3 level (Fig. 2). Findings were consistent with carcinoma, situated at least 12 cm from anal verge, with involvement of the muscuralis, without any obvious extramural spread and no suspicious lymphadenopathy (Stage T3N0).
Fig. 2.
Demonstrates intussusception at S2–S3 level (orange arrow) → Irregular intermediate signal cauliflower like lesion with diffusion restriction situated at least 12 cm from anal verge consistent with carcinoma, with involvement of the muscuralis, without any obvious extramural spread and no suspicious lymphadenopathy on MRI.
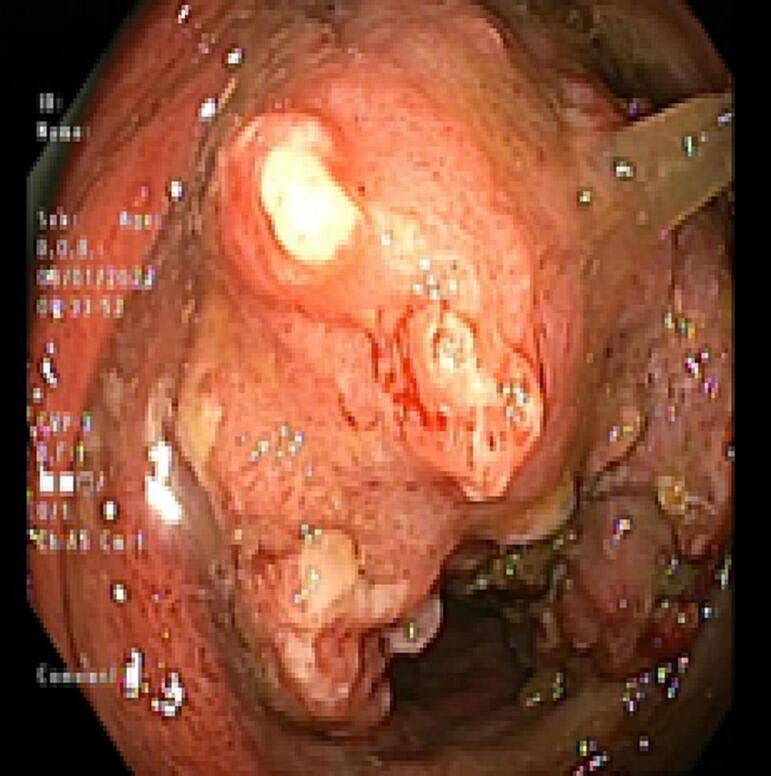
The patient proceeded to flexible sigmoidoscopy with a planned proceed to anterior resection. We found the tumour to actually be in the mid sigmoid ∼25 cm from the anal verge (Fig. 3); acting as a lead point for intussusception and prolapse. There was associated oedema and an adjacent ulcer. There was no peritoneal metastatic disease; and the patient proceeded to a laparoscopic high anterior resection, and was given a covering ileostomy. He had an uncomplicated post-operative recovery and was discharged home post-operative day 6.
Fig. 3.
Tumour in mid sigmoid ∼25 cm from the anal verge on flexible sigmoidoscopy.
Histopathology revealed sigmoid and descending colon adenocarcinoma with mucinous differentiation pT3N0. He was discussed at a multidisciplinary meeting (MDT), and decision was made not for further adjuvant treatment. He was referred to an urologist for management of his renal cancer. He was followed up with the surgeon and subsequently had a reversal of his ileostomy 12 months later. He remains well.
3. Discussion
A rectal intussusception can mimic a rectal prolapse and it can be quite difficult to differentiate between the two based on history alone [4]. On physical examination, a leading point lesion can be found on the protruding mass in the case of intussusceptions, which does not occur in cases of rectal prolapses [4]. Moreover, there is a space between the protruding mucosa and anal wall in the event of an intussusception; however it is more continuous in rectal prolapses [4]. In our case report, our patient's examination was more consistent with an intussusception over a prolapse based on the above discussion.
Early diagnosis is found to depend on accurate interpretation of radiological findings in order to prevent late diagnosis at the time of surgical intervention [6]. Ultrasound might demonstrate a “target sign” in the transverse view or “pseudo-kidney sign” on the longitudinal view [7]. A CT scan would however show a “bowel within bowel” appearance [7].
Compared to Ultrasound and CTs, defecating MRIs have been found to be more beneficial in terms of interpreting prolapsing rectosigmoid cancer due to its dynamic nature thereby allowing assessment of the presence of rectocele, enterocele and anismus, which have been found to be associated with intussusception [6]. It also permits the overall assessment of pelvic movements which helps with planning the foreseeable operation [6].
Pre-operative colonoscopies and imaging can limit the need for a colon resection with identification of benign lesions [8]. It can however be difficult to diagnose these pre-operatively [9]. The rate of diagnosis of intussusceptions pre-operatively has been shown to vary between 32 and 70% [9].
There are no set guidelines in terms of management options of colorectal intussusceptions. In patients with a high suspicion of malignancy, especially in the elderly/ with risk factors; routine resections seem to be the preferred choice of management [6]. Due to risk of intraluminal seeding and venous embolization, reduction prior to resection should be avoided when intussusception is caused by a malignant lead-point [6].
Surgery can be performed laparoscopically or open. There is evidence to suggest that operative resections can be performed with minimally invasive techniques under very safe and effective conditions [6]. In our case, a laparoscopic approach was chosen. Laparoscopic surgery has been proven to hasten the healing of the gastrointestinal tract, reduce mesenteric and intestinal trauma, improve surgical cosmesis, reduce response to surgical stress, and reduce the length of hospital stay as well as the risk of incisional hernias [10].
With left sided colonic intussusceptions like our case, a primary anastomosis can be performed over a Hartmanns procedure keeping the surgeon's expertise in mind [3]. A proximal diverting loop ileostomy can be considered with a primary anastomosis if there are risk factors for an anastomostic leak like high dose steroids, chemotherapy, other immunosuppressants, malnutrition and smoking [3]. In our case, a primary anastomosis was performed with a proximal diverting loop ileostomy given our patient's significant history of heavy smoking [3].
In conclusion, this case demonstrates a fairly rare presentation. However timely diagnosis and suspicion of cancer leading to a colonic resection did help improve the prognosis of our patient's cancer. He did not require any further oncological treatment post upfront surgery and his stoma has now been reversed. Therefore, it is important to be familiar with even such rare presentations as it can be challenging to identify a malignancy in such situations.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Ethical approval
This study has been exempted from ethical approval by our institution.
Funding
There were no sponsors for this case report.
Author contribution
Dr. Sarada Ganesan and Dr. Joseph Xavier were involved in the writing of this case report.
Guarantor
Dr. Sarada Ganesan and Dr. Joseph Xavier.
Research registration number
This case report is not a “First in Man” and therefore does not require any registration.
Conflict of interest statement
There are no conflicts of interest in the creation of this case report as declared by the authors.
References
- 1.Mathis K. Expert commentary on adult intussusception. Dis. Colon Rectum. 2021;64(6):648–649. doi: 10.1097/DCR.0000000000002043. [DOI] [PubMed] [Google Scholar]
- 2.McCarthy J. Transverse colonic intussusception in an adult. J. Gen. Intern. Med. 2023;38(3):810. doi: 10.1007/s11606-022-07855-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Marsicovetere P., Joga Ivatury S., White B., Holubar S. Intestinal intussusception: etiology, diagnosis, and treatment. Clin. Colon Rectal Surg. 2017;30(01):030–039. doi: 10.1055/s-0036-1593429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Du J.Z., Teo L.T., Chiu M.T. Adult rectosigmoid junction intussusception presenting with rectal prolapse. Singap. Med. J. 2015;56(5):e78–e81. doi: 10.11622/smedj.2015078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Agha R.A., Franchi T., Sohrab C., Mathew G., Kirwan A., Thomas A., et al. The SCARE 2020 guideline: updating consensus Surgical Case Report (SCARE) guidelines. Int. J. Surg. 2020;84(1):226–230. doi: 10.1016/j.ijsu.2020.10.034. [DOI] [PubMed] [Google Scholar]
- 6.Filiberto A., Loftus T., Tan S., Read T., Igbal A. Sigmoido-rectal intussusception. SAGE Open Med. Case Rep. 2019;7 doi: 10.1177/2050313X19856242. 2050313X19856242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sseruwagi T.M., Lewis C.R. Rectal prolapse associated with intussusception and malignancy. J. Surg. Case Rep. 2023;6:rjad363. doi: 10.1093/jscr/rjad363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mahmood A., Ruan Q.Z., O’Hara R., Canna K. Adult intussusception presenting as rectal prolapse. BMJ Case Rep. 2014;2014 doi: 10.1136/bcr-2013-203281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Inada R., Nagasaka T., Toshima T., Mori Y., Kondo Y., Kishimoto H., Fujiwara T. Intussusception due to rectal adenocarcinoma in a young adult: a case report. World J. Gastroenterol. 2014;20(35):12678–12681. doi: 10.3748/wjg.v20.i35.12678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yuksel A., Coskun M. Laparoscopic surgery for adult intussusception: case series. Turk J Gastroenterol. 2021;32(8):611–615. doi: 10.5152/tjg.2020.19835. [DOI] [PMC free article] [PubMed] [Google Scholar]