Abstract
Interventional therapies including chemotherapies and radiotherapies are the most preferred treatment for liver cancer. However, these therapies have adverse effects. Therefore, careful care is required to relieve these adverse effects. The objectives of this study were to evaluate the quality of life, pain, anxiety, depression, adverse effects, and satisfaction of patients with liver cancer who received pre- and post-operative comprehensive nursing care against those of patients who received conventional nursing care. Patients with liver cancer who underwent surgeries and interventional therapies for liver cancer received pre- and post-operative comprehensive nursing care (CMN cohort, n = 105) or conventional nursing care (CNN cohort, n = 135), or did not receive any kind of nursing care (NNC cohort, n = 175). Before the non-treatment intervention(s) (BL), none of the patients had absent post-operative pain, all patients had mild or moderate anxiety and depression, and patients had ≤70 overall quality of life score. In the NNC cohort, a few of the patients reported being completely dissatisfied with overall personal satisfaction, and anxiety, depression, and overall the quality of life of patients were clinically worse during the follow-up period generally after completion of all doses of chemo radiotherapies (EL) as compared to BL. Hospital stays due to surgery, visual analog scale (VAS) score, Zung Self-rating Anxiety Scale score, the Self-rating Depression Scale score, and rehospitalization due to any reason(s) in follow-up were fewer and overall quality of life score and overall personal satisfaction score were higher for patients of the CMN cohort than those of patients at BL and those of patients of the CNN and the NNC cohorts at EL (P < .05 for all). Fever, bleeding, urinary retention, gastrointestinal disturbance, and hepatic and renal impairments reported in patients of the NNC cohort. Fever, bleeding, and urinary retention reported in patients of the CNN cohort (P < .05 for all). Nursing non-treatment intervention(s) is necessary for liver cancer patients after surgery, in the follow-up, and between 2 doses of chemoradiotherapies. Pre- and post-operative comprehensive nursing care relieves postoperative pain, psychological burden and improves quality of life in the follow-up period in patients who underwent surgeries and interventional therapies for liver cancer (Level of Evidence: IV; Technical Efficacy: Stage 5).
Keywords: anxiety, depression, interventional therapies, liver cancer, nursing care, personal satisfaction, quality of life
1. Introduction
A malignant tumor that occurs in the liver is referred to as liver cancer.[1] Liver cancer is the most common type of cancer in China.[2] Primary and secondary types of liver cancers are more prevalent in China and both cause serious issues including death in Chinese men and women.[3,4] Various parameters are associated with the development of liver cancer in the Chinese population, for example, hepatitis B and hepatitis C virus infections, aflatoxins, alcohol consumption, cirrhosis, and nitrosamine traces.[5]
Surgeries and interventional therapies including chemotherapies and radiotherapies are the preferred treatment option(s) for liver cancer.[6] However, these therapies have adverse effects.[2] Therefore, careful care is required to relieve these adverse effects.[7] Traditional Chinese medicine is sometimes given with chemotherapies to reduce toxicities and improve the efficacies of interventional therapies in China among liver cancer patients.[2] Traditional Chinese medicine nursing is applied to emergency treatment and has a good role in recovery after treatment(s). Conventional nursing care is not sufficient in patients with increasing modes of tumors because patients who had higher tumors may have a worse quality of life and less survival.[8] In addition, unlike conventional nursing care, comprehensive nursing care is a combination of nursing philosophy, nursing quality, and nursing plan.[9] Conventional nursing care is not sufficient to relieve anxiety and depression in patients with liver cancer after surgeries and while on interventional therapies.[2] However, patients with liver cancer have high levels of anxiety and depression.[10]
The objectives of this retrospective study were to evaluate the quality of life, pain, anxiety, depression, adverse effects (after an operation during follow-up and between 2 doses of chemotherapies), and satisfaction of patients with liver cancer who received pre- and post-operative comprehensive nursing care against those of patients who received conventional nursing care.
2. Materials and methods
2.1. Ethics approval and consent to participate
The protocols of the study were designed and established by the authors and approved by the first affiliated Hospital of Suchow University review board (Approval No. GMU15147 dated February 3, 2019) and the nursing society of China. The study protocols follow the law of China and the 2008 Declaration of Helsinki. Being a retrospective study, registration in the Chinese clinical trial registry and the informed consent of patients to participate in the study were waived by the first affiliated Hospital of Suchow University review board.
2.2. Inclusion criteria
Patients who underwent surgeries for liver cancer following chemoradiotherapies were included in the study.
2.3. Exclusion criteria
Patients whose records were incomplete (≥3 important data) in the hospital data were not included in the study.
2.4. Treatment of liver cancer
Partial resection surgery of the liver following chemoradiotherapies was the preferred treatment(s) for patients with liver cancer.
2.5. Cohorts
A total of 105 patients with liver cancer received pre- and post-operative comprehensive nursing care (CMN cohort). A total of 135 patients with liver cancer received conventional nursing care (CNN cohort). A total of 175 patients with liver cancer did not receive any kind of nursing care, receive literature and visual aid only from institute from hospital staff during hospital visits (NNC cohort). The decision to have no/conventional/comprehensive nursing care were made by patients themselves. In Chinese law, patients have rights for selection of treatment(s) for their disease(s).
2.6. Comprehensive nursing care
2.6.1. Preoperative care.
During the admission of patients at the hospital for surgery, patients were informed of the environment of the surgery room and the work schedules of the surgery to bridge gap between nursing staff and patients. On the other site, lectures with pictorial presentations were also provided to patients to overcome their negative psychology for surgery, for example, fear, anxiety, and nervousness. The core benefits and principles of priorities of surgery and interventional procedures were described to patients before surgeries. Illustrations of successful surgeries and treatment(s) can improve the confidence of patients in careful care through nursing care so those patients can actively, seriously, and consciously cooperate with the nursing and the other staff of the institutes with an optimistic attitude. A vibrant and more positive environment in the hospital for patients would help them to recover. The preparation area was quiet and peaceful. Patients were instructed for fasting before surgery accordingly. Hemodynamic parameters were monitored by a nurse in the preparation room.[9]
2.6.2. Postoperative care.
The nursing staff starts communicating when patients were conscious in the post-surgery intensive care unit, asking about their pain and the other adverse effects, for example, drowsiness, nausea, vomiting, chest tightness, etc. Also, patients were continuously guided, and their confidence levels increased during chemo radiotherapies. The nursing staff provided explanations of the adverse effects of chemo radiotherapies and overcoming measures of these effects.[9]
2.7. Conventional nursing care
It included monitoring of hemodynamic parameters in the preparation room before surgery, communicating with patients after surgeries, and motivating patients during chemo radiotherapies.[9]
2.8. Outcome measures
2.8.1. Demographical and clinical parameters.
Demographical parameters and clinical conditions of patients before operation, operative conditions, postoperative conditions, chemotherapies, and radiotherapies-related parameters of patients were evaluated from hospital records of patients and analyzed.
2.8.2. Post-operative pain.
A visual analog scale (VAS) in the range of 0 to 10 was used for the revaluation of post-operative pain where 0: absent pain, 1 to 3: mild pain, 4 to 6: moderate pain, and 7 to 10: severe pain.[2]
2.8.3. Adverse effects.
Adverse effects after an operation during follow-up and between 2 doses of chemotherapies were evaluated and analyzed.
2.8.4. Zung self-rating anxiety scale and the self-rating depression scale.
Both Zung Self-rating Anxiety Scale and the Self-rating Depression Scale are 20-item questionaries. Each question had 4 options for answers (1, 2, 3, and 4). The total score was 100. Score <50: no anxiety/no depression, 51 to 70: mild anxiety/mild depression, 71 to 90: moderate anxiety/moderate depression, and more than 90: severe anxiety/severe depression.[11]
2.8.5. SF-36 instruments.
The Chinese version of SF-36 instruments with 8 dimensions (physical functions, body pain, physical role, general health, emotional functions, social functions, vitality, and mental health) was used for the evaluation of the quality of life of the enrolled patients with liver cancer. Each dimension has a score range from 0 to 100. The higher the score, the better the quality of that dimension of patients. The overall quality of life of patients ranges from 0 to 100. The higher the score, the higher the overall quality of life of patients.[12]
2.8.6. Patients’ overall satisfaction.
Our institutes have their own developed patients’ overall satisfaction questionnaires. The tool is a survey questionnaire. The questionnaires are about available facilities in the institutes, the ability of staff to explain the disease(s) and related parameters, and the attitude of the staff of institutes towards them. The tool contains 3 questions. The score is range from 0 to 3, where 0: completely dissatisfied, 1: less satisfied, 2: satisfied, and 3: fully satisfied.
Zung Self-rating Anxiety Scale, the Self-rating Depression Scale, and overall quality of life were evaluated before operation and during the follow-up period generally after completion of all doses of chemo radiotherapies. The self-rated patients’ overall satisfaction score was evaluated during the follow-up period generally after completion of all doses of chemo radiotherapies.
2.9. Statistical analysis
InStat 3.01, GraphPad Software, San Diego, CA, was used for statistical analysis. Categorial parameters are presented as frequencies with percentages in parentheses. Continuous or ordinal non-linear parameters are depicted as median with Q3-Q1 in parenthesis. Continuous or ordinal linear parameters are depicted as median ± standard deviation. Kolmogorov and Smirnov method was used to check the linearity of parameters. The chi-square test (χ2 test; in the 4-grid table, when the total number of cases was n ≥ 40 and the theoretical frequency of all grids was greater than or equal to 5) or Fisher exact test was used for statistical analysis of categorial variables. One-way analysis of variance (ANOVA) was used for the analysis of continuous or ordinal linear parameter. Kruskal-Wallis’ test (non-parametric ANOVA) was used for the analysis of not linear continuous or ordinal variables. Tukey-Kramer multiple comparisons tests (for parametric variables) and Dunn multiple comparisons tests (for non-parametric variables) were used for post hoc analysis. All results were considered significant at a 95% confidence interval if the P value was <.05.
3. Results
3.1. Study population
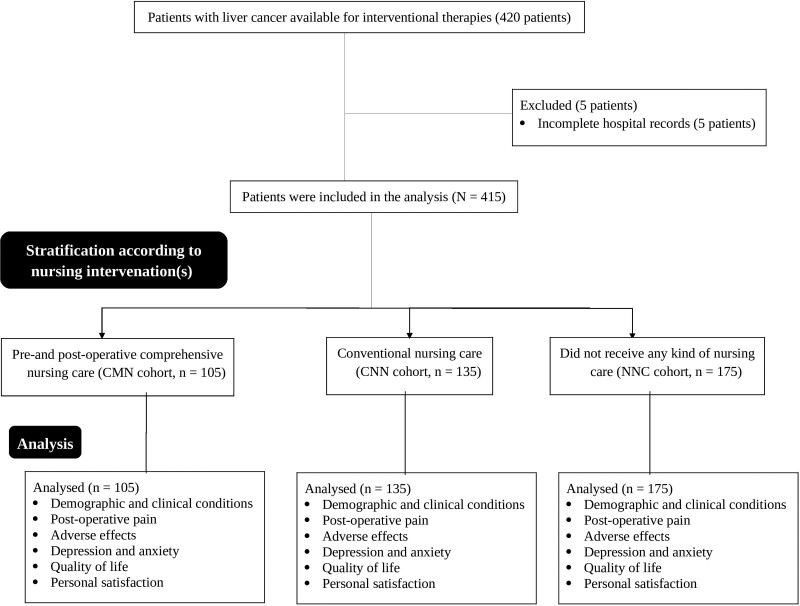
From January 15, 2017 to February 3, 2020, 420 patients with liver cancer were available at the Department of Hepatopancreatobiliary & Thyroid Breast, the first affiliated Hospital of Suchow University, Suzhou, Jiangsu, China, and the referring hospitals for surgery and interventional therapies for liver cancer. Among them, the records of 5 patients were incomplete in the hospital data. Therefore, data of them were excluded from the analysis. Demographic and clinical parameters before surgeries, operative conditions, postoperative conditions, chemotherapies-related parameters, post-operative pain, adverse effects, anxiety scale, depression scale, quality of life, and patient satisfaction scores of a total of 415 patients with liver cancer were collected from hospital records and analyzed. The summary chart of the study is presented in Figure 1.
Figure 1.
Summary chart of the study.
3.2. Demographical and clinical parameters
Males were higher among patients with liver cancer than females. Almost 2 third of patients had primary liver cancer and one third of patients had secondary liver cancer. Gender, age before the operation, type of cancer, ethnicity, Zung Self-rating Anxiety Scale score before the operation, the Self-rating Depression Scale score before the operation, and the overall quality of life score before the operation were comparable among cohorts (Table 1, P > .05 for all). All patients underwent partial liver resection surgeries. After surgeries, all patients underwent chemotherapies of cisplatin, doxorubicin, mitomycin, and 5-fluorouracil following radiotherapies. Each dose of chemotherapy and radiotherapy was scheduled at 21 days of the gap. Before the operation, all patients had mild or moderate anxiety (Zung Self-rating Anxiety Scale and the Self-rating Depression Scale: minimum: 55–maximum: 85) and depression (Zung Self-rating Anxiety Scale and the Self-rating Depression Scale: minimum: 54–maximum: 85), and all patients had a diminished (≤70) overall quality of life score.
Table 1.
Demographical and clinical parameters of patients before operation.
| Parameters | Total | Cohorts | Comparisons between cohorts | ||||
|---|---|---|---|---|---|---|---|
| CMN | CNN | NNC | |||||
| Nursing care | Yes/no | Pre- and post-operative comprehensive | Conventional | None | |||
| Patients | 415 | 105 | 135 | 175 | P value | Df | |
| Gender | Male | 265 (64) | 70 (67) | 80 (59) | 115 (66) | .3591 (χ2-test for independence) | 2 |
| Female | 150 (36) | 35 (33) | 55 (41) | 60 (34) | |||
| Type of cancer | Primary liver cancer | 287 (69) | 80 (76) | 90 (67) | 117 (67) | .1958 (χ2-test for independence) | 2 |
| Secondary liver cancer | 128 (31) | 25 (24) | 45 (33) | 58 (33) | |||
| Age (yr) | 50.55 ± 5.45 | 50.75 ± 5.67 | 49.67 ± 5.08 | 51.11 ± 5.54 | 0.0615 (ANOVA) | N/A | |
| Ethnicity | Han Chinese | 387 (93) | 97 (92) | 127 (94) | 163 (93) | .4007 (χ2-test for independence) | 4 |
| Mongolian | 25 (6) | 7 (7) | 7 (5) | 11 (6) | |||
| Tibetan | 3 (1) | 1 (1) | 1 (1) | 1 (1) | |||
| Zung Self-rating Anxiety Scale score | 69 (74–65) | 70 (74–67) | 70 (75–62) | 68 (73–64) | .0578 (Kruskal-Wallis’ test) | N/A | |
| Self-rating Depression Scale score | 68 (70–65) | 68 (70–66) | 67 (69–65) | 68 (75–61.5) | .1598 (Kruskal-Wallis’ test) | N/A | |
| Overall quality of life score | 57 (60–55) | 56 (60–54) | 58 (60–55) | 56 (61–54) | .051 (Kruskal-Wallis’ test) | N/A | |
Categorial variables are depicted as the frequency with percentages in parentheses.
Continuous linear variables are depicted as mean ± standard deviation with standard deviation (SD) in parentheses.
Score < 50: no anxiety/no depression, 51 to 70: mild anxiety/mild depression, 71 to 90: moderate anxiety/moderate depression, and >90: severe anxiety/severe depression.
Continuous not linear variables are depicted as mean with Q3–Q1 in parenthesis.
All results were considered significant if the P value was <.05.
ANOVA = analysis of variance, Df = degree of freedom, χ2-test = Chi-square test.
3.3. Outcome measures
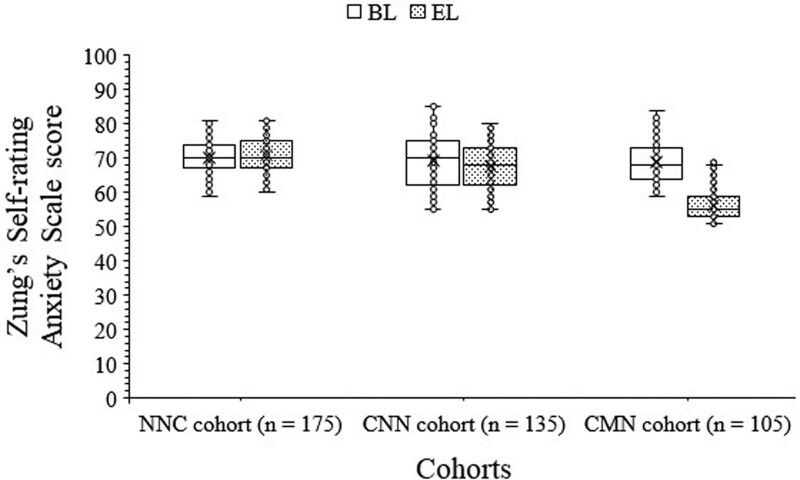
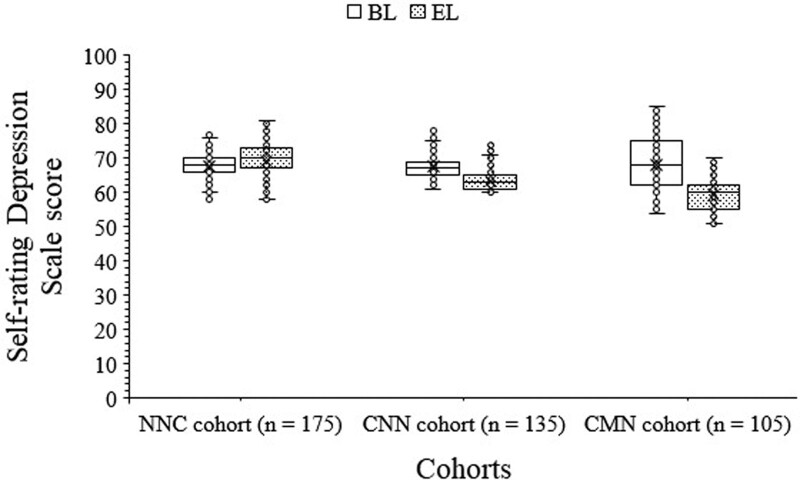
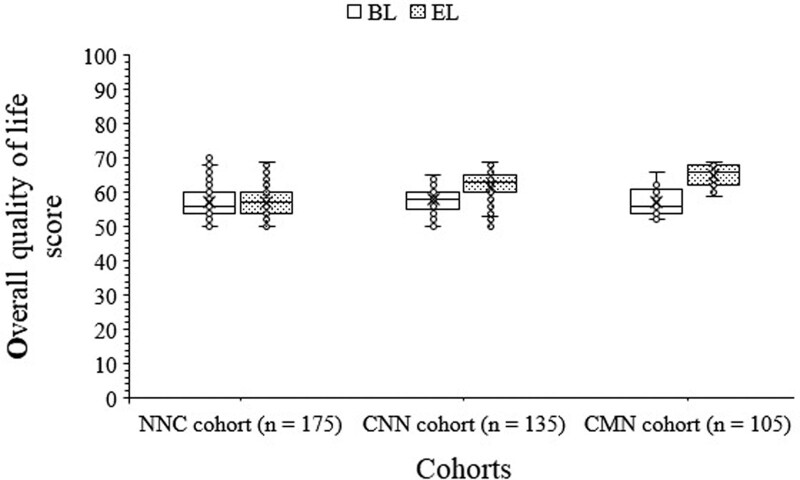
Hospital stays due to surgery were fewer for patients of the CMN cohort than those of patients of the CNN and the NNC cohort. Hospital stays due to surgery were fewer for patients of the CNN cohort than those for patients of the NNC cohort. None of the patients had absent pain (VAS score = 0). VAS scores of patients of the NNC cohort and the CNN cohort were statistically the same after surgery. The VAS score of patients after surgery of the CMN cohort was smaller than those of the NNC and CNN cohorts. During the follow-up period generally after completion of all doses of chemo radiotherapies, all patients had mild or moderate anxiety (Zung Self-rating Anxiety Scale and the Self-rating Depression Scale score: minimum: 51–maximum: 81) and depression (Zung Self-rating Anxiety Scale and the Self-rating Depression Scale score: minimum: 51–maximum: 81). Patients of the CNN and the CMN had smaller scores for the Zung Self-rating Anxiety Scale and the Self-rating Depression Scale than those of patients of the NNC cohort during the follow-up period generally after completion of all doses of chemo radiotherapies. During the follow-up period generally after completion of all doses of chemo radiotherapies, patients of the CMN cohort had smaller scores for the Zung Self-rating Anxiety Scale and the Self-rating Depression Scale than those of patients of the CNN cohort. The overall quality of life score and overall personal satisfaction scores were higher for patients of the CNN and the CMN cohorts than those of patients of the NNC cohort during the follow-up period generally after completion of all doses of chemo radiotherapies. The overall quality of life score and overall personal satisfaction score were higher for patients of the CMN cohort than those of patients of the CNN cohort during the follow-up period generally after completion of all doses of chemo radiotherapies. All patients had <70 overall quality of life score during the follow-up period generally after completion of all doses of chemo radiotherapies. A few of the patients reported a “0” overall personal satisfaction score (completely dissatisfied) from the NNC cohort only. The detailed analyses of outcome measures are reported in Table 2. In the NNC cohort, anxiety, depression, and overall quality of life were clinically worse but statistically the same (P > .05 for all, 1-way ANOVA/Tukey test) during the follow-up period generally after completion of all doses of chemo radiotherapies as compared to those of patients before operation condition. In the CNN and the CMN cohorts, anxiety and depression of patients were relieved, and overall quality of life was improved (P < .05 for all, 1-way ANOVA/Tukey test) during the follow-up period generally after completion of all doses of chemo radiotherapies as compared to those of patients of before operation condition. The details of anxiety, depression, and overall quality of life of patients of different cohorts during the follow-up period generally after completion of all doses of chemo radiotherapies and before operation are reported in Figures 2, 3, and 4, respectively.
Table 2.
Outcome measures of the study during the follow-up period generally after completion of all doses of chemo radiotherapies.
| Parameters | Total | Cohorts | Comparisons between CNN and CMN cohorts | ||||
|---|---|---|---|---|---|---|---|
| NNC | CNN | CMN | |||||
| Nursing care | Yes/no | None | Conventional | Pre- and post-operative comprehensive | |||
| Patients | 415 | 175 | 135 | #P value | 105 | *P value | P value |
| Hospital stays due to surgery (d) | 3 (5–2) | 5 (5–4) | 3 (3–2) | <.001 | 1 (2–1) | <.001 | <.001 |
| VAS score | 4 (5–3) | 5 (6–4) | 5 (5–4) | >.05 | 3 (4–3) | <.001 | <.001 |
| Zung Self-rating Anxiety Scale score | 67 (72–60) | 70 (75–67) | 68 (73–62) | <.01 | 55 (59.5–52.5) | <.001 | <.001 |
| Self-rating Depression Scale score | 64 (70–61) | 70 (73–67) | 63 (65–61) | <.001 | 60 (62–55) | <.001 | <.001 |
| Overall quality of life score | 61 (65–57) | 57 (60–54) | 63 (65–60) | <.001 | 66 (68–62) | <.001 | <.001 |
| #Patients’ overall satisfaction | 3 (5–2) | 1 (1–1) | 2 (2–1) | <.001 | 2 (3–2) | <.001 | <.01 |
CMN cohort = patients with liver cancer received pre- and post-operative comprehensive nursing care, NNC cohort = patients with liver cancer did not receive any kind of nursing care, VAS = visual analog scale; 0: absent, 10: worse pain.
Score < 50: no anxiety/no depression, 51 to 70: mild anxiety/mild depression, 71 to 90: moderate anxiety/moderate depression, and > 90: severe anxiety/severe depression.
Variables are depicted as mean with Q3–Q1 in parenthesis.
Kruskal-Wallis’ test was used for statistical analysis.
Dunn multiple comparisons test was used for post hoc analysis.
All results were considered significant if the P value was <.05.
#0: completely dissatisfied, 1: less satisfied, 2: satisfied, and 3: fully satisfied.
Concerning NNC cohort.
Figure 2.
Zung Self-rating Anxiety Scale score for patients of different cohorts. BL = before operation, EL = during the follow-up period generally after completion of all doses of chemo radiotherapies. Score < 50: no anxiety, 51 to 70: mild anxiety, 71 to 90: moderate anxiety, and > 90: severe anxiety.
Figure 3.
Self-rating depression scale score for patients of different cohorts. BL = before operation, EL = during the follow-up period generally after completion of all doses of chemo radiotherapies. Score < 50: no depression, 51 to 70: mild depression, 71 to 90: moderate depression, and > 90: severe depression.
Figure 4.
Overall quality of life score for patients of different cohorts. BL = before operation, EL = during the follow-up period generally after completion of all doses of chemo radiotherapies. Higher the score the higher the overall quality of life of patients.
3.4. Adverse effects
All patients faced a few episodes of nausea and vomiting after the operation and during follow-up and between 2 doses of chemotherapies. Fever, bleeding, urinary retention, gastrointestinal disturbance, and hepatic and renal impairments were reported in patients of the NNC cohort. Fever, bleeding, and urinary retention were reported in patients of the CNN cohort. Rehospitalization due to any reason(s) for patients of the CMN and the CNN cohorts was fewer than those of patients of the NNC cohort during the follow-up period. The detailed analyses of adverse effects after an operation during follow-up period and between 2 doses of chemoradiotherapies are reported in Table 3.
Table 3.
Adverse effects after an operation during follow-up period and between 2 doses of chemoradiotherapies.
| Event | Cohorts | Comparisons between CNN and CMN cohorts | ||||
|---|---|---|---|---|---|---|
| NNC | CNN | CMN | ||||
| Nursing care | None | Conventional | Pre- and post-operative comprehensive | |||
| Patients | 175 | 135 | #P value | 105 | #P value | P value |
| Fever | 35 (20) | 15 (11) | .0426 | 4 (4) | <.0001 | .0522 |
| Bleeding | 22 (13) | 10 (7) | .1871 | 0 (0) | <.0001 | .0029 |
| Urinary retention | 25 (14) | 9 (7) | .0429 | 1 (1) | <.0001 | .0459 |
| Gastrointestinal tract disturbance | 19 (11) | 8 (6) | .1563 | 1 (1) | .0012 | .0816 |
| Hepatic impairment | 15 (9) | 7 (5) | .274 | 1 (1) | .0067 | .0828 |
| Renal impairment | 16 (9) | 6 (4) | .1235 | 1 (1) | .0039 | .1401 |
| Rehospitalization due to any reason(s) | 35 (20) | 15 (11) | .0426 | 7 (7) | .0029 | .2671 |
Patients have on or more adverse effect.
Variables are depicted as the frequency with percentages in parenthesis.
χ2-test or Fisher exact test was used for statistical analysis.
All results were considered significant if the P value was <.05.
CMN cohort = patients with liver cancer received pre- and post-operative comprehensive nursing care, NNC cohort = patients with liver cancer did not receive any kind of nursing care, χ2-test = Chi-square test.
#Concerning NNC cohort.
4. Discussion
None of the patients had absent pain (VAS scale 0) before the operation, all patients had mild or moderate anxiety and depression, and all patients had diminished (≤70) overall quality of life score. In addition, A few of the patients reported a “0” overall personal satisfaction score (completely dissatisfied) from the NNC cohort only and in the NNC cohort anxiety, depression, and overall quality of life of patients were clinically worse during the follow-up period generally after completion of all doses of chemo radiotherapies as compared to before operation. The results of outcome measures of patients in the current study were consistent with those of a cross-sectional study,[12] a systematic review,[10] and a observational study.[13] Generally, preferred therapies for liver cancer are surgical resection followed by chemoradiotherapies and frequent doses of chemoradiotherapies are required for prognosis improvement of liver cancer after surgery.[14] This improves the survival of patients but the quality of life of patients becomes worse during follow-up and between 2 doses of chemotherapies.[2] Nursing non-treatment intervention(s) is necessary for liver cancer patients after surgery during follow-up and between 2 doses of chemoradiotherapies for mindful improvement of living standards.
Zung Self-rating Anxiety Scale score and the Self-rating Depression Scale score of patients of the CMN cohort were smaller than those of patients before operation and those of patients of the NNC and the CNN cohorts during the follow-up period generally after completion of all doses of chemo radiotherapies. The emotional results of patients in the current study are consistent with those of a pilot study,[2] a systematic review,[10] and a meta-analysis.[15] Based on the holistic care model, patients of the CMN cohort were guided by concept of modern nursing, and comprehensive pre- and post-operative nursing non-treatment intervention(s) were also systematically applied to patients of the CMN cohort.[2] Liver cancer patients have mental health issues, poor cognitive ability, and fear related to the disease. Proper cognitive guidance and psychotherapies in the pre- and post-operative nursing non-treatment intervention(s) boost the confidence of liver cancer patients in the CMN cohort. The use of pre- and post-operative comprehensive nursing care of patients with liver cancer has a definite effect in calming patients’ emotions and reducing the impact of bad feelings of patients due to surgery and chemoradiotherapies in follow-up period.
Adverse effects after an operation during follow-up and between 2 doses of chemoradiotherapies were fewer among patients of the CMN cohort than those of patients of the CNN and the NNC cohorts. The results of the adverse effects on patients of the current study are consistent with those of a pilot study[2] and a retrospective analysis.[9] Pre-operative comprehensive nursing improves patients’ understanding of liver cancer surgery and relieves anxiety about liver cancer treatments and related adverse effects. In addition, comprehensive nursing care pays close attention to patient care after surgery. That results in psychological improvement and accelerates the recovery in patients of the CMN cohort.[16] Comprehensive nursing care has the advantage of fewer adverse effects after surgery during follow-up and between 2 doses of chemoradiotherapies in patients with liver cancer.
The quality of life of patients of the CMN cohort was higher than those of patients before operation and those of patients of the CNN and the NNC cohorts during the follow-up period generally after completion of all doses of chemo radiotherapies. The results of the quality of life of patients in the current study are consistent with those of a pilot study,[2] prospective analysis,[17] retrospective analysis,[9] and meta-analysis.[15] Less anxiety, depression, and adverse effects lead to the involvement of patients in social functions. That would improve the quality of life of patients. The use of pre- and post-operative comprehensive nursing care of patients with liver cancer improves the quality of life of liver cancer patients in the follow-up period.
VAS scores of patients of the NNC cohort and the CNN cohort were statistically the same. The results of post-operative pain of the current study were not consistent with those of a observational study.[13] The small sample size of an observational study[13] is responsible for contradictory results. Conventional nursing failed to decrease adverse effects and rehospitalization due to any reason(s) in the follow-up period. Treatment for adverse effects and rehospitalization always have intervention(s). All these things would increase the pain of patients. In addition, conventional nursing care had no pre-operative counseling of patients. Only comprehensive nursing care would relieve the physical pain of patients of liver cancer after surgery and in between 2 doses of chemoradiotherapies. Conventional nursing care would not relieve the physical pain of liver cancer patients after surgery and in between 2 doses of chemoradiotherapies.
Overall personal satisfaction score of patients of the CMN cohort was higher than those of patients of the CNN and the NNC cohorts. The results of the overall personal satisfaction score of liver cancer patients in the current study are consistent with those of a pilot study,[2] a retrospective analysis,[9] and an observational study.[13] Pre- and post-operative comprehensive nursing care is superior to conventional nursing care in liver cancer patients who underwent surgeries following interventional therapies including chemotherapies and radiotherapies for liver cancer.
Fever, bleeding, urinary retention, gastrointestinal disturbance, and hepatic and renal impairments were reported in patients of the NNC cohort. Fever, bleeding, and urinary retention were reported in patients of the CNN cohort. Fever, bleeding, urinary retention, and hepatic and renal impairments would be determined by the illness condition of the patients, the surgery operation and the chemoradiotherapies. Comprehensive nursing has not had a significant impact on these adverse effects. Except explanations and counseling for patients, as nursing non-treatment interventions, there are not any additional medical treatments on the adverse effects of fever, bleeding, urinary retention, gastrointestinal disturbance, and hepatic and renal impairments in comprehensive nursing.
The limitations of this study, for example, are that it is retrospective and not a dynamic study.
5. Conclusions
Nursing non-treatment intervention(s) is necessary for liver cancer patients after surgery, follow-up, and between 2 doses of chemoradiotherapies. Pre- and post-operative comprehensive nursing care relieve postoperative pain, psychological burden, improves quality of life, and decrease effects due to adverse reactions in the follow-up period and in between 2 doses of chemoradiotherapies in patients who underwent surgeries following interventional therapies for liver cancer. Comprehensive nursing care is superior to conventional nursing care.
Acknowledgments
The authors are thankful to the medical and non-medical staff of the first affiliated Hospital of Suchow University, Suzhou, Jiangsu, China.
Author contributions
Conceptualization: LiQun Zhang.
Data curation: Dan Shi.
Formal analysis: Dan Shi.
Investigation: QiaoYing Xing.
Methodology: JinFeng Sun, Dan Shi.
Project administration: PeiPei Chen.
Resources: PeiPei Chen, LiQun Zhang.
Software: PeiPei Chen, LiQun Zhang, Dan Shi.
Supervision: PeiPei Chen, LiQun Zhang, QiaoYing Xing.
Validation: QiaoYing Xing.
Visualization: JinFeng Sun, QiaoYing Xing.
Writing – original draft: JinFeng Sun.
Writing – review & editing: JinFeng Sun.
Abbreviations:
- ANOVA
- analysis of variance
- CMN cohort
- patients with liver cancer received pre- and post-operative comprehensive nursing care
- CNN cohort
- patients with liver cancer received conventional nursing care
- NNC cohort
- patients with liver cancer did not receive any kind of nursing care
- VAS
- visual analog scale
PC and LZ contributed equally to this work.
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
The authors have no funding and conflicts of interest to disclose.
How to cite this article: Chen P, Zhang L, Sun J, Xing Q, Shi D. Pre- and post-operative comprehensive nursing care versus conventional nursing care: An evaluation of quality of life, postoperative pain, adverse effects, and treatment satisfaction of patients who underwent surgeries and interventional therapies for liver cancer. Medicine 2023;102:34(e34643).
Contributor Information
PeiPei Chen, Email: c095844@163.com.
LiQun Zhang, Email: g557253@163.com.
QiaoYing Xing, Email: c095846@163.com.
Dan Shi, Email: u421171@163.com.
References
- [1].Anwanwan D, Singh SK, Singh S, et al. Challenges in liver cancer and possible treatment approaches. Biochim Biophys Acta Rev Cancer. 2020;1873:188314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [2].Yuan Y, Li Y, Yang G, et al. Effect of comprehensive nursing approach in perioperative stage of patients with hepatocellular carcinoma interventional therapy. Evid Based Complement Alternat Med. 2022;2022:6862463. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- [3].Li L, Wang H. Heterogeneity of liver cancer and personalized therapy. Cancer Lett. 2016;379:191–7. [DOI] [PubMed] [Google Scholar]
- [4].Bruix J, Han KH, Gores G, et al. Liver cancer: approaching a personalized care. J Hepatol. 2015;62(1 Suppl):S144–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].An L, Zeng HM, Zheng RS, et al. Liver cancer epidemiology in China, 2015. Chin J Oncol. 2019;41:721–7. [DOI] [PubMed] [Google Scholar]
- [6].Llovet JM, Kelley RK, Villanueva A, et al. Hepatocellular carcinoma. Nat Rev Dis Primers. 2021;7:6. [DOI] [PubMed] [Google Scholar]
- [7].El Jabbour T, Lagana SM, Lee H. Update on hepatocellular carcinoma: pathologists’ review. World J Gastroenterol. 2019;25:1653–65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Keating NL, Landrum MB, Lamont EB, et al. Tumor boards and the quality of cancer care. J Natl Cancer Inst. 2013;105:113–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Gou Y, Yi J, Jiang M, et al. Analysis on effects of comprehensive nursing care applied in interventional therapy for patients with liver cirrhosis and liver cancer. Iran J Public Health. 2019;48:494–500. [PMC free article] [PubMed] [Google Scholar]
- [10].Graf J, Stengel A. Psychological burden and psycho-oncological interventions for patients with hepatobiliary cancers-a systematic review. Front Psychol. 2021;12:662777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Dunstan DA, Scott N. Norms for Zung’s self-rating anxiety scale. BMC Psychiatry. 2020;20:90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Chen P, Zhang F, Shen Y, et al. Health-related quality of life and its influencing factors in patients with hepatitis B: a cross-sectional assessment in southeastern China. Can J Gastroenterol Hepatol. 2021;2021:9937591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Wang XB, Sun LF, Niu ME, et al. The effect of nursing management of patients undergoing interventional therapy for liver cancer compared with standard care on patient-reported outcomes. Clin Nurs Res. 2022;31:1100–6. [DOI] [PubMed] [Google Scholar]
- [14].Lurje I, Czigany Z, Bednarsch J, et al. Treatment strategies for hepatocellular carcinoma-a multidisciplinary approach. Int J Mol Sci . 2019;20:1465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Zhang Q, Wan R, Liu C. The impact of intense nursing care in improving anxiety, depression, and quality of life in patients with liver cancer: a systematic review and meta-analysis. Medicine (Baltimore). 2020;99:e21677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Pearson EJM, Morris ME, di Stefano M, et al. Interventions for cancer-related fatigue: a scoping review. Eur J Cancer Care. 2018;27:1–14. [DOI] [PubMed] [Google Scholar]
- [17].Yang Y, Niu G, Mi Q, et al. Analysis of rehabilitation effect of neurology nursing on stroke patients with diabetes mellitus and its influence on quality of life and negative emotion score. Dis Markers. 2022;2022:1579928. [DOI] [PMC free article] [PubMed] [Google Scholar]