Abstract
Background
Young people’s ability to use their preferred contraceptive method is an indicator of reproductive autonomy and healthcare access. State policies can hinder or facilitate access to a preferred contraceptive method.
Objective
This study compared use of preferred contraceptive method in Texas and California, states with contrasting health policy contexts that impact health insurance coverage and access to subsidized family planning services.
Methods
We used baseline survey data from an ongoing cluster randomized controlled trial of sexually active students, assigned female at birth, ages 18–25, at 29 community colleges in Texas and California (N = 1,974). We described contraceptive preferences and use, as well as reasons for nonuse of a preferred method. We conducted multivariable-adjusted mixed-effects logistic regression analyses for clustered data, and then calculated the predicted probability of using a preferred contraceptive method in Texas and California by insurance status.
Results
More Texas participants were uninsured than Californians (30% vs. 8%, p<0.001). Thirty-six percent of Texas participants were using their preferred contraceptive method compared to 51% of Californians. After multivariable adjustments, Texas participants had lower odds of using their preferred method (adjusted odds ratio = 0.62, 95% confidence interval = 0.48–0.81) compared to those in California. Texas participants in all insurance categories had a lower predicted probability of preferred method use compared to California participants. In Texas, we found a 12.1 percentage-point difference in the predicted probability of preferred method use between the uninsured (27.5%) and insured (39.6%) (p<0.001). Texans reported financial barriers to using their preferred method more often than Californians (36.7% vs. 19.2%, p<0.001) as did the uninsured compared to the insured (50.9% vs. 18.7%, p<0.001).
Conclusion
These findings present new evidence that state of residence plays an important role in young people’s ability to realize their contraceptive preference. Young people in Texas, with lower insurance coverage and more limited access to safety net programs for contraceptive care than in California, have lower use of preferred contraception. It has become urgent in states with abortion bans to support young people’s access to their preferred methods.
Introduction
The ability for young people to use their preferred contraceptive method is an indicator of health care access and reproductive autonomy [1]. However, a growing literature demonstrates that current contraceptive method use often does not reflect method preferences. Several recent studies have found a mismatch between the methods that people use and the methods they want to use, with many desiring to use a more effective method [2–6]. Cost barriers are frequently cited as reasons for unfulfilled preferences [2–4, 7]. Analyses of the 2015–2017 National Survey of Family Growth found that 22% of women at risk of an unplanned pregnancy would have preferred a different contraceptive method if cost were not a factor [8] and 39% of nonusers of contraception would start using a method if not for the cost [9]. However, results are mixed on the association between insurance coverage and preference-use mismatch. Some studies found that uninsured people were less likely to be using their preferred method [4, 5], while others found no association [3, 6].
State-level policies, including whether a state has expanded Medicaid, may facilitate access to contraception by increasing insurance coverage and reducing cost and other barriers [10]. Thirty-eight states, including California, have expanded full-benefit Medicaid coverage [11]. California’s Medicaid program, Medi-Cal, covers all U.S. citizens, permanent residents, and legal residents who live in households with incomes up to 138% of the federal poverty level (FPL) [12]. California’s program also covers young adults under age 26 [13], regardless of immigration status. In contrast, twelve states, including Texas, have not expanded full Medicaid. Texas extends full Medicaid coverage only to U.S. citizens and legal immigrants who are parents/guardians of dependent children and have incomes up to 16% FPL [14].
While both states have implemented policies to provide contraception to people who do not qualify for full-benefit Medicaid but who meet other eligibility criteria [15] such as lower incomes or for those who cannot use their insurance because of confidentiality concerns [16], California’s program covers far more people. California’s Family Planning, Access, Care and Treatment (Family PACT) program provides comprehensive family planning services at no cost to all California residents of childbearing age who have incomes of up to 200% FPL and no other source of insurance coverage for family planning services or who have confidentiality concerns [17].
In contrast, Texas’s program, Healthy Texas Women, covers U.S. citizens and qualified legal immigrants who can get pregnant with incomes of up to 204% FPL [18]. Rather than implement policies to maintain or expand coverage, Texas has implemented a series of restrictive state policies that have excluded certain providers from participating in family planning programs [19, 20], which led to a large number of family planning clinic closures [21–23].
Given differing state policy environments affecting insurance coverage, it is not surprising that Texas and California have large differences in the percentage of young adults who are uninsured. In Texas, 30% of 19–25 year old young adults were uninsured in 2019 compared to 12% in California [24]. However, even in states with more expansive health coverage policies for both the insured and uninsured, young adults, including students, may still have cost concerns. A study of community college students aged 18–25 in California and Oregon found that nearly half of students were concerned about the cost of contraception, and that the uninsured had the highest cost concerns [25].
In this study, we examined the impact of no insurance coverage on use of a preferred method of contraception in Texas and California. Specifically, we compare mismatch between contraceptive preference and use between young people in these states with contrasting contraceptive policy and service environments. We focus on young people attending community college because more students from lower income families attend two year institutions than attend four year institutions [26], and this overwhelming difference contributes to structural inequities that limit access to health insurance [27].
Methods and materials
We used baseline survey data from an ongoing cluster randomized controlled trial of first-year community college students, assigned female at birth, ages 18–25, who had vaginal sex with a male partner in the last year, and were not currently pregnant or wanting to become pregnant in the next year [28]. We enrolled students attending 29 community college sites in Texas and California from April 2018 through May 2023. Of these 29 colleges, two were located in rural (nonmetropolitan) counties and the remainder in metropolitan counties– 15 large central metro, two large fringe metro, nine medium metro, and one small metro [29].
Pre-pandemic, we recruited and enrolled students in person, which we completed at 17 colleges. After March 2020, we shifted to remote recruitment and enrollment. We conducted exclusively remote recruitment and enrollment at four colleges. At the remaining eight colleges, we resumed in-person recruitment at a later date, ranging from August 2021 through April 2023, and continued with remote enrollment. Throughout the study, in both California and Texas, college staff sent emails to students and posted study information on college course content management systems inviting students to participate. In addition, in Texas, where students’ names and email addresses were available upon request, the study team emailed first-year female students. Students were given a written consent form and provided electronic consent to participate. Participants then completed baseline surveys covering sociodemographic characteristics, health insurance status, and reproductive health history, including current and preferred contraceptive methods. Study participants received remuneration of a $50 electronic gift card following study enrollment.
This study was approved by the Institutional Review Boards (IRBs) at the University of California, San Francisco (#17–23183) and The University of Texas at Austin (#2019010078); participating college sites either approved the study with their IRB (7 sites) or used the corresponding state university’s IRB approval (22 sites).
Measures
To measure current contraceptive method, participants selected their method or methods from a list. For those who selected more than one method, we used the method that participants identified as their “main method” of contraception. We categorized methods into the following: oral contraceptive pill, transdermal patch or vaginal ring, intrauterine device (IUD) or sub-dermal implant, injectable, condom, fertility awareness, emergency contraception or other, withdrawal, and no method.
To measure preferred contraceptive method, participants were asked, “If you could use any birth control method you wanted, what method would you use?” Response options included “I am using the method that I want,” and the same list of contraceptive methods as for current contraceptive methods, with the addition of male and female sterilization and “don’t know.” For participants who selected multiple preferred contraceptive methods, we selected as preferred method the one that matched their current main method (n = 141). For the remaining participants (n = 194), we did not want to prioritize any particular method characteristic when assigning preferred method because evidence indicates that people choose contraceptive methods for a range of reasons [30]. Therefore, we randomly assigned a preferred method from the list of methods these participants selected.
The primary study outcome is whether participants reported that they were using their preferred method of contraception. Students whose current contraceptive method was the same as their preferred method were coded as using their preferred method.
We also explored challenges in using a preferred contraceptive method. Participants who were not using their preferred method were asked why not and could choose multiple responses from a list of reasons as well as write in other reasons. We grouped 1,452 responses from the 1,002 participants who gave a reason or reasons for not using their preferred method into several categories. Information/availability barriers included “I don’t know where to get it,” “It’s too much hassle to get it,” “My doctor/clinic doesn’t offer it,” and “My doctor advised against it.” Parents/partner barriers included “My parents don’t know that I’m sexually active” and “My partner doesn’t want me to use it.” Financial barriers were “I can’t afford it” and “My insurance doesn’t cover it.” Other reasons were fear of side effects; not needing a method, which included “I’m not sexually active” and mentions of not wanting or needing a method; those who stated that they had an appointment to get the method soon; and other reasons (e.g., it feels better without a condom).
Our independent variables include state, Texas or California, and health insurance status, uninsured, insured (private, Medicaid), and did not know insurance status.
We included sociodemographic covariates that have been associated with contraceptive preferences in previous research [3, 4, 6]. Covariates were age, categorized into adolescents (18–19 year-olds) and young adults (20–25 year-olds), has a child or children (yes, no), self-reported race and ethnicity (Hispanic, White non-Hispanic, Asian/Pacific Islander non-Hispanic, Black non-Hispanic, American Indian/Other/Multi-racial non-Hispanic; for brevity, Latinx, White, Asian/Pacific Islander, Black, American Indian/Multi-racial/other), and language spoken at home (English, language other than English).
Statistical analysis
From the total sample of 2,084, we excluded observations for those who did not state a preference (i.e., answered “don’t know”; n = 94), were missing whether they were using their preferred method (n = 5), had missing data on the sociodemographic covariates (n = 8), or were missing on all these variables (n = 3), for a final analytical sample of 1,974. Given that study participants are clustered within colleges, in the descriptive statistical analysis, we used univariate logistic regression models with cluster robust standard errors to test for differences between the state samples and between those who were and were not using their preferred method. Finally, we conducted multivariable-adjusted mixed-effects logistic regression analyses for clustered data to assess participant likelihood of using their preferred contraceptive method. We estimated a main effects model with our two independent variables of state and insurance status. Next, given the much higher rates of uninsured in Texas than in California, we modeled the interaction between state and insurance status. Finally, in the full model, we added sociodemographic controls: age, race/ethnicity, has a child, and language spoken at home. Using the full model, we calculated margins to illustrate the predicted probability of using a preferred contraceptive method in Texas and California and by insurance status in each state. All analyses were conducted in Stata 17 (College Station, TX).
Results
Over 29% of Texas participants were uninsured compared to 7.7% of California participants (p<0.001) (Table 1). The majority of participants in both states were 18–19 years old with no children. The Texas sample was slightly older, with 27.2% who were 20–25 years old at enrollment compared to 15.2% in California (p<0.01); more Texas participants also had a child (8.8% vs. 3.2%, p<0.001). The state samples were racially and ethnically diverse, with the Texas sample having a larger percentage of Latinx participants (71.5% in Texas vs. 51.6% in California; p<0.05) and Black participants (10.2% vs. 4.2%, p<0.05). The study samples were largely reflective of the racial and ethnic composition of community college student populations in each state [31, 32]. More Texas participants reported speaking a language other than English at home (58.1 vs. 46.4%), though the difference was not statistically significant.
Table 1. Participant characteristics by state (N = 1,974).
| State | ||||
|---|---|---|---|---|
| Texas (n = 558) | California N = 1,416) | |||
| Insurance status | ||||
| Uninsured | 164 | 29.4*** | 109 | 7.7 |
| Insured (ref) | 332 | 59.5 | 1,153 | 81.4 |
| Don’t know status | 62 | 11.1 | 154 | 10.9 |
| Age | ||||
| 18–19 (ref) | 406 | 72.8 | 1,201 | 84.8 |
| 20–25 | 152 | 27.2** | 215 | 15.2 |
| Has child(ren) | ||||
| No | 509 | 91.2 | 1,371 | 96.8 |
| Yes (ref) | 49 | 8.8*** | 45 | 3.2 |
| Race/ethnicity | ||||
| Hispanic/Latinx | 399 | 71.5* | 730 | 51.6 |
| White (ref) | 70 | 12.5 | 342 | 24.2 |
| Black | 57 | 10.2* | 60 | 4.2 |
| Asian/Pacific Islander | 20 | 3.6 | 176 | 12.4 |
| Amer. Indian/ Multi–racial/other | 12 | 2.2 | 108 | 7.6 |
| Language spoken at home | ||||
| English | 234 | 41.9 | 759 | 53.6 |
| Language other than English (ref) | 324 | 58.1 | 657 | 46.4 |
Note: * p <05
** p < .01
*** p <0.001
Univariate logistic regression models with cluster robust standard errors compared California to Texas.
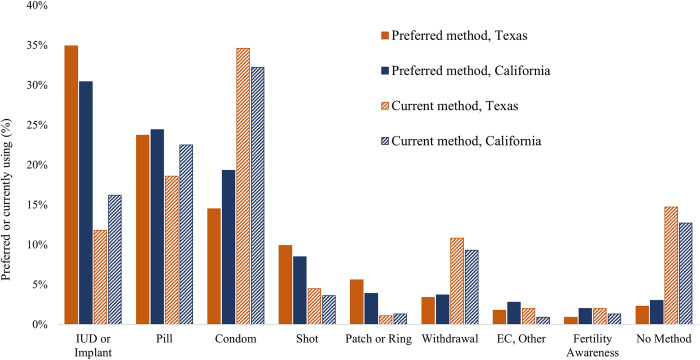
Fig 1 shows contraceptive preferences and use for Texas and California. In both states, preference was highest for the IUD or implant (34.9% in Texas, 30.4% in California), while these methods were used by 11.8% in Texas and 16.2% in California. Oral contraceptive pills were the second-most preferred method in both states (23.7% in Texas and 24.4% in California) and were used by 18.6% in Texas, 22.5% in California. Although not as many participants reported a preference for condoms (14.5% in Texas, 19.3% in California), condoms were used by the most participants in both states (34.6% in Texas, 32.2% in California). Just 2.3% of participants in Texas and 3.0% in California stated a preference for using no method, while 14.7% of Texans and 12.7% of Californians reported using no method.
Fig 1. Contraceptive preferences and use in Texas and California (N = 1,974).
Note: No students were using sterilization at baseline; preference for sterilization was 3.0% in Texas and 2.0% in California.
A lower percentage of Texas participants reported using their preferred method of contraception than California participants (36.2% vs. 51.3%; p<0.001) (Table 2). Uninsured participants (36.3%) were less likely to report using their preferred method of contraception compared to those who were insured (49.5%, p<0.001). Participants who did not know their insurance status had a lower percentage of using their preferred method (44.0%) compared to the insured, but the difference was not statistically significant.
Table 2. Percent using preferred contraceptive method, by state and insurance status (N = 1,974).
| Using preferred contraceptive method | ||||
|---|---|---|---|---|
| Yes | No | |||
| N | % | n | % | |
| State | ||||
| Texas | 202*** | 36.2 | 356 | 63.8 |
| California (ref) | 727 | 51.3 | 689 | 48.7 |
| Insurance status | ||||
| Uninsured | 99 | 36.3 | 174*** | 63.7 |
| Insured (ref) | 735 | 49.5 | 750 | 50.5 |
| Don’t know status | 95 | 44.0 | 121 | 56.0 |
Note: *** p <0.001
Univariate logistic regression models with cluster robust standard errors to compare those who realized their contraceptive preference to those who did not.
The primary reasons that participants in Texas and California reported for not using their preferred method were information/availability barriers (48.1% and 49.6%), and parent/partner barriers (36.0% and 36.6%) (Table 3). Financial barriers were more frequently reported by participants in Texas than in California (36.9% vs. 19.2%), among the uninsured (50.9%) and those who did not know their insurance status (27.2%) compared to the insured. In addition, fewer Texas participants reported not needing a method compared to those in California (8.7% vs. 12.1%). Fewer of the uninsured reported fear of side effects as a barrier to their preferred method use compared to the insured (5.2% vs. 12.3%).
Table 3. Reasons for not using preferred contraceptive method, by state and insurance status (%).
| State | Insurance Status | ||||
|---|---|---|---|---|---|
| Reason | Texas | California | Uninsured | Insured | Don’t know |
| Information/availability barriers | 48.1 | 49.6 | 46.2 | 49.5 | 50.9 |
| Parent/partner barriers | 36.0 | 36.6 | 37.0 | 36.1 | 37.7 |
| Financial barriers | 36.9*** | 19.2 | 50.9*** | 18.9 | 27.2* |
| No need | 8.7* | 12.7 | 9.3 | 11.5 | 13.2 |
| Fear of side effects | 8.7 | 12.1 | 5.2* | 12.3 | 11.4 |
| I have an appointment scheduled to get it soon | 6.3 | 6.6 | 6.9 | 6.7 | 4.4 |
| Other (e.g., it feels better without a condom) | 4.0 | 6.1 | 4.6 | 5.9 | 2.6 |
***p<0.001
*p<0.05
Note. Multiple responses allowed; percentage of 1,452 responses received from 1,002 total participants; responses missing for 43 participants. Univariate logistic regression models with cluster robust standard errors were used to test for differences by state and insurance status. The question was not asked of those who were using a method but wanted to use no method (n = 30).
In multivariable-adjusted mixed-effects logistic regression analyses, participants from Texas had lower odds of using their preferred method (adjusted odds ratio [aOR] = 0.58, 95% confidence interval [CI] = 0.41–0.82) and the uninsured had lower odds compared to the insured (aOR = 0.71, 95% CI = 0.53–0.95) (Table 4, Model 1). In Model 2, which included an interaction term between state and insurance status, we found that uninsured Texas participants had 68% lower odds of using their preferred method than insured California participants. Finally, the relationships between use of preferred methods and state and insurance persisted after inclusion of sociodemographic controls (Model 3).
Table 4. Using preferred contraceptive method: Multivariable-adjusted mixed-effects logistic regression analyses (n = 1,974).
| Model 1: Main effects | Model 2: Main effects + interaction | Model 3: Main effects + interaction + sociodemographic controls§ | |||||||
|---|---|---|---|---|---|---|---|---|---|
| aOR | 95% CI | p-value | aOR | 95% CI | p-value | aOR | 95% CI | p-value | |
| State | |||||||||
| Texas | 0.58 | (0.41–0.82) | 0.002 | 0.65 | (0.47–0.90) | 0.009 | 0.62 | (0.48–0.81) | <0.001 |
| California (ref) | 1.00 | 1.00 | 1.00 | ||||||
| Insurance status | |||||||||
| Uninsured | 0.71 | (0.53–0.95) | 0.021 | 1.02 | (0.64–1.62) | 0.942 | 1.09 | (0.68–1.75) | 0.713 |
| Insured (ref) | 1.00 | 1.00 | |||||||
| Don’t know | 0.83 | (0.65–1.06) | 0.131 | 0.81 | (0.62–1.07) | 0.140 | 0.84 | (0.64–1.10) | 0.207 |
| State*Insurance interaction | |||||||||
| Texas*Uninsured | 0.48 | (0.29–0.81) | 0.006 | 0.51 | (0.30–0.87) | 0.013 | |||
| Texas*Don’t know | 1.03 | (0.56–1.88) | 0.923 | 1.11 | (0.62–2.00) | 0.725 | |||
| Constant | 1.11 | (0.91–1.34) | 0.308 | 1.08 | (0.89–1.31) | 0.454 | 1.47 | (1.17–1.84) | 0.001 |
Note. aOR = adjusted odds ratio estimated from mixed-effects logistic regression models; CI = confidence interval.
§ Sociodemographic controls are age, race/ethnicity, language spoken at home, and has child(ren).
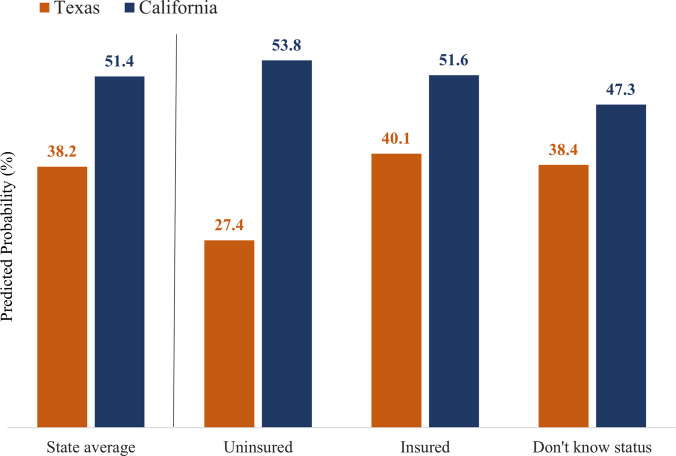
Fig 2 displays the predicted probability of participants using their preferred method overall in each state and by insurance status, based on the estimates from Model 3 in Table 4. Overall, 38.2% of the Texas participants were predicted to be using their preferred method, compared to 51.4% of California participants (Fig 2). Texas participants in all insurance categories had a lower predicted probability of preferred method use compared to California participants. In Texas, we found a 12.7 percentage-point difference in the predicted probability of preferred method use between the uninsured (27.4%) and insured (40.1%) (p<0.001). The difference between the insured and those who did not know their status (38.3%) in Texas was not significant (p = 0.779). Likewise, the probability of using a preferred method was not significant between the uninsured (53.8%) and insured (51.6%) in California (p = 0.713) or between the insured and those who did not know their status (47.3%, p = 0.206).
Fig 2. Predicted proportions of using preferred contraceptive method by state and insurance status.
Note. Predictions based on Model 3 reported in Table 4.
Discussion
We found that about one-third of student participants in Texas and one-half in California were using their preferred method of contraception. Moreover, after controlling for sociodemographic characteristics, we found that fewer uninsured Texas participants were predicted to be using their preferred method compared to insured Texans and no differences by insurance status in California.
These findings present new evidence that state of residence plays an important role in young people’s ability to realize their contraceptive preference, magnified by differences in insurance coverage, as well as through differences in state programs that provide contraceptive coverage for the uninsured. Young people residing in California, which has expanded Medicaid to provide insurance coverage for a broad swath of its low-income population, were more likely to realize their contraceptive preferences compared to young people in Texas. Moreover, we did not find a difference in the realization of contraceptive preference between the uninsured and insured in California, suggesting that California’s strong family planning safety net is accomplishing its goals of providing more widespread contraceptive coverage for the uninsured. In other words, we found higher preferred method use and no difference across insurance status for young people in California thanks to that state’s supportive policies and programs.
The more restrictive healthcare policy environment in Texas, including budget cuts to publicly funded services and restrictions on who can provide those services [19–22], all likely play a role in Texas students’ limited use of their preferred contraceptive method compared to students in California. In addition, Texas’s Medicaid family planning waiver program, which does not extend services to undocumented immigrants, may also play a role in the ability of young Texans in this study to use their preferred method [33], though we are unable to confirm this with our data because, due to its sensitivity, we did not ask about immigration status.
Regardless of where they lived or whether they had insurance, about half of all participants said they were not using their preferred method because of information or availability barriers. Not finding a state difference is somewhat surprising, given that Texas has a long history of abstinence-only or no sex education in schools [34] and California has an equally long history of mandated comprehensive sex education in secondary schools, including a requirement to provide information about local sexual health service providers [35].
Similar to other studies that compared contraceptive use and preferences [2–6], we found that many young adults in community college in this study had unfulfilled preferences for contraception. Our estimates are higher than in studies with populations that included older adults [2, 3], and may be due, at least in part, to confidentiality concerns that young people face [16]. Indeed, over one-third of students in this study noted that the reason they were not using their preferred method of contraception was because they did not want their parents to know that they were sexually active. This is consistent with previous research which found that college students who have less frequent conversations with their mothers about sex are less likely to intend to use reproductive health services [36]. Also similar to other studies, we found that young people want to use more effective methods, such as the IUD, implant or injectable, that often require a clinic visit [4]. Instead, they are relying on methods that may be more convenient and accessible for them (e.g, withdrawal) or can be paid for out of pocket (e.g., condoms).
Limitations
This study focuses on a sample of community college students, and is representative of that population, but not of all 18 to 25 year-olds in Texas and California. Moreover, the California sample is larger than the Texas sample, and it is possible that if we had a larger Texas sample, we may have found greater differences in use of contraceptive preferences between the states. However, these results are indicative of significant gaps in contraceptive access for young adult community college students in Texas and California. In addition, we did not collect information about immigration status, which means that we can only hypothesize about the potential impact of policies that expand or restrict access to undocumented immigrants on preferred method use.
Conclusion
These findings present compelling evidence that state of residence, via policies and programs that affect access to services, plays a role in young people’s ability to realize their contraceptive preference. Young people in Texas, with lower insurance coverage and more limited access to safety net programs for contraceptive care than in California, have lower use of preferred contraception. It is critical to expand access to preferred contraception in all states, but it has become urgent in states with abortion bans, such as Texas, to support young people’s access to their preferred methods.
Acknowledgments
The authors thank the students for their participation; California and Texas study teams for assistance with data collection; Hannah Hecht for preparing data replication documentation; members of the study’s community advisory board; and staff at participating colleges, Health Services Association California Community Colleges (HSACCC), National Institute for Staff and Organizational Development (NISOD), Healthy Futures of Texas for their support of this work.
Data Availability
Due to confidentiality concerns, data replication files are available via restricted data access on openICPSR at http://doi.org/10.3886/E193387V1.
Funding Statement
William and Flora Hewlett Foundation, 2022-01110-GRA, Cynthia C. Harper, PI; https://hewlett.org/ The JPB Foundation, 2021-2688, Cynthia C. Harper, PI; https://www.jpbfoundation.org/ NIH/National Institute of Diabetes, Digestive, and Kidney Disorders, K12DK111028, Alison J. Huang and Stephen K. Van Den Eeden, PIs: https://www.niddk.nih.gov/ Eunice Kennedy Shriver National Institute of Child Health and Human Development, P2C HD042849, Awarded to the Population Research Center, UT Austin, Elizabeth T. Gershoff, PI; https://www.nichd.nih.gov/ The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Potter JE, Stevenson AJ, Coleman-Minahan K, Hopkins K, White K, Baum SE, et al. Challenging unintended pregnancy as an indicator of reproductive autonomy. Contraception. 2019. Mar 6;100(1):1–4. doi: 10.1016/j.contraception.2019.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.He K, Dalton VK, Zochowski MK, Hall KS. Women’s contraceptive preference-use mismatch. J Womens Health. 2017;26(6):692–701. doi: 10.1089/jwh.2016.5807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chakraborty P, Gallo MF, Nawaz S, Smith MH, Hood RB, Chettri S, et al. Use of nonpreferred contraceptive methods among women in Ohio. Contraception. 2021;103(5):328–35. doi: 10.1016/j.contraception.2021.02.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hopkins K, Hubert C, Coleman-Minahan K, Stevenson AJ, White K, Grossman D, et al. Unmet demand for short-acting hormonal and long-acting reversible contraception among community college students in Texas. J Am Coll Health. 2018. Feb 6;66(5):360–8. doi: 10.1080/07448481.2018.1431901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Potter JE, Hopkins K, Aiken ARA, Hubert C, Stevenson AJ, White K, et al. Unmet demand for highly effective postpartum contraception in Texas. Contraception. 2014. Nov 1;90(5):488–95. doi: 10.1016/j.contraception.2014.06.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Potter JE, Coleman-Minahan K, White K, Powers DA, Dillaway C, Stevenson AJ, et al. Contraception after delivery among publicly insured women in Texas: Use compared with preference. Obstet Gynecol. 2017. Aug;130(2):393–402. doi: 10.1097/AOG.0000000000002136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Frederiksen B, Ranji U, Long M, 2021. Women’s sexual and reproductive health services: Key findings from the 2020 KFF women’s health survey [Internet]. San Francisco, CA: KFF; 2021 Apr [cited 2021 Oct 13]. Available from: https://www.kff.org/womens-health-policy/issue-brief/womens-sexual-and-reproductive-health-services-key-findings-from-the-2020-kff-womens-health-survey/ [Google Scholar]
- 8.Burke KL, Potter JE, White K. Unsatisfied contraceptive preferences due to cost among women in the United States. Contracept X. 2020;2:100032. doi: 10.1016/j.conx.2020.100032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kavanaugh ML, Pliskin E, Hussain R. Associations between unfulfilled contraceptive preferences due to cost and low-income patients’ access to and experiences of contraceptive care in the United States, 2015–2019. Contracept X. 2022;4:100076. doi: 10.1016/j.conx.2022.100076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Johnston EM, McMorrow S. The Relationship Between Insurance Coverage and Use of Prescription Contraception by Race and Ethnicity: Lessons From the Affordable Care Act. Womens Health Issues. 2020. Mar;30(2):73–82. doi: 10.1016/j.whi.2019.11.005 [DOI] [PubMed] [Google Scholar]
- 11.Medicaid.gov. Adult coverage expansion as of July 2021. [Internet]. [cited 2022 Nov 10]. Available from: https://www.medicaid.gov/medicaid/program-information/downloads/medicaid-expansion-state-map-10-2021.pdf [Google Scholar]
- 12.California Department of Health Services. Do you qualify for Medi-Cal benefits? [Internet]. 2022. [cited 2022 Aug 25]. Available from: https://www.dhcs.ca.gov/services/medi-cal/Pages/DoYouQualifyForMedi-Cal.aspx [Google Scholar]
- 13.California Department of Health Services. Young adult expansion [Internet]. 2021. [cited 2022 Aug 25]. Available from: https://www.dhcs.ca.gov/services/medi-cal/eligibility/Pages/youngadultexp.aspx [Google Scholar]
- 14.Kaiser Family Foundation. Medicaid income eligibility limits for adults as a percent of the federal poverty level [Internet]. 2022. [cited 2022 Aug 16]. Available from: https://www.kff.org/health-reform/state-indicator/medicaid-income-eligibility-limits-for-adults-as-a-percent-of-the-federal-poverty-level [Google Scholar]
- 15.Guttmacher Institute. Medicaid family planning eligibility expansions [Internet]. 2022. [cited 2022 Aug 25]. Available from: https://www.guttmacher.org/state-policy/explore/medicaid-family-planning-eligibility-expansions [Google Scholar]
- 16.Sonfield A, Hasstedt K, Gold RB. Moving forward: family planning in the era of health reform. New York: Guttmacher Institute; 2014. [Google Scholar]
- 17.California Department of Health Services. Am I eligible for Family PACT? [Internet]. 2022. [cited 2022 Aug 25]. Available from: https://familypact.org/am-i-eligible/ [Google Scholar]
- 18.Texas Department of State Health Services. Healthy Texas Women [Internet]. 2022. [cited 2022 Aug 25]. Available from: https://www.healthytexaswomen.org/healthcare-programs/healthy-texas-women/htw-who-can-apply [Google Scholar]
- 19.Stevenson AJ, Flores-Vazquez IM, Allgeyer RL, Schenkkan P, Potter JE. Effect of removal of Planned Parenthood from the Texas Women’s Health Program. N Engl J Med. 2016. Mar 3;374(9):853–60. doi: 10.1056/NEJMsa1511902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.White K, Hopkins K, Grossman D, Potter JE. Providing family planning services at primary care organizations after the exclusion of Planned Parenthood from publicly funded programs in Texas: Early qualitative evidence. Health Serv Res. 2018. Aug;53(4, Part II):2770–86. doi: 10.1111/1475-6773.12783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.White K, Grossman D, Hopkins K, Potter JE. Cutting family planning in Texas. N Engl J Med. 2012. Sep 27;367(13):1179–81. doi: 10.1056/NEJMp1207920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.White K, Hopkins K, Aiken ARA, Stevenson A, Hubert C, Grossman D, et al. The impact of reproductive health legislation on family planning clinic services in Texas. Am J Public Health. 2015. May;105(5):851–8. doi: 10.2105/AJPH.2014.302515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rice WS, Redd SK, Luke AA, Komro K, Jacob Arriola K, Hall KS. Dispersion of contraceptive access policies across the United States from 2006 to 2021. Prev Med Rep. 2022. Jun;27:101827. doi: 10.1016/j.pmedr.2022.101827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.State Health Compare (SHADAC). SHADAC analysis of the 2019 American Community Survey (ACS) Public Use Microdata Sample (PUMS) files [Internet]. University of Minnesota; 2022. [cited 2022 Jul 28]. Available from: http://statehealthcompare.shadac.org/ [Google Scholar]
- 25.Yarger J, Schroeder R, Blum M, Cabral MA, Brindis CD, Perelli B, et al. Concerns about the cost of contraception among young women attending community college. Womens Health Issues. 2021. Sep;31(5):420–5. doi: 10.1016/j.whi.2021.03.006 [DOI] [PubMed] [Google Scholar]
- 26.The Pell Institute for the Study of Opportunities in Higher Education and University of Pennsylvania Alliance for Higher Education and Democracy (PennAHEAD). Indicators of higher education equity in the United States: 2022 historical trend report [Internet]. 2022. [cited 2022 Apr 15]. Available from: https://www.ahead-penn.org/news/indicators-higher-education-equity-united-states-2022-historical-trends-report [Google Scholar]
- 27.United States Government Accountability Office. Most college students are covered through employer-sponsored plans, and some colleges and states are taking steps to increase coverage. Washington, D.C.; 2008. (Report to the Committee on Health, Education, Labor, and Pensions, U.S. Senate). Report No.: GAO-08-389.
- 28.Yarger J, Hopkins K, Elmes S, Rossetto I, De La Melena S, McCulloch CE, et al. Perceived access to contraception via telemedicine among young adults: inequities by food and housing insecurity. J Gen Intern Med [Internet]. 2022. Jun 3 [cited 2022 Oct 25]; Available from: https://link.springer.com/10.1007/s11606-022-07669-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.National Center for Health Statistics. NCHS urban-rural classification scheme for counties [Internet]. [cited 2023 May 11]. Available from: https://www.cdc.gov/nchs/data_access/urban_rural.htm
- 30.Jackson AV, Karasek D, Dehlendorf C, Foster DG. Racial and ethnic differences in women’s preferences for features of contraceptive methods. Contraception. 2016. May;93(5):406–11. doi: 10.1016/j.contraception.2015.12.010 [DOI] [PubMed] [Google Scholar]
- 31.California Community Colleges Chancellor’s Office Management Information Systems Data Mart. Enrollment Status Summary Report [Internet]. 2022. Available from: https://datamart.cccco.edu/Students/Enrollment_Status.aspx [Google Scholar]
- 32.Texas Higher Education Coordinating Board. Authors’ calculations from unpublished tables, Female FTIC Students by Ethnicity, Fall 2019-Fall 2022, and Female FTIC Students by Institution and Ethnicity, Fall 2019-Fall 2022. 2022. [Google Scholar]
- 33.Tapales A, Douglas-Hall A, Whitehead H. The sexual and reproductive health of foreign-born women in the United States. Contraception. 2018. Jul;98(1):47–51. doi: 10.1016/j.contraception.2018.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wiley D, Miller F, Quinn D, Valentine R, Miller K. Conspiracy of silence: Sexuality education in Texas public schools in 2015–16 [Internet]. 2017. [cited 2023 Apr 25]. Available from: https://tfn.org/sex-ed/conspiracy_of_silence.pdf [Google Scholar]
- 35.California Department of Education. Comprehensive sexual health & HIV/AIDS instruction [Internet]. 2022. [cited 2023 Apr 25]. Available from: https://www.cde.ca.gov/ls/he/se/ [Google Scholar]
- 36.Gibson LP, Denes A P. Crowley J. College women’s sexual and reproductive health screening behaviors and the role of mother–daughter communication. J Am Coll Health. 2020. May 18;68(4):357–65. doi: 10.1080/07448481.2018.1549558 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Due to confidentiality concerns, data replication files are available via restricted data access on openICPSR at http://doi.org/10.3886/E193387V1.