Abstract
Nocardia asteroides is a rare cause of keratitis usually associated with trauma. We report a case of corneal ulceration caused by N. asteroides in a patient with leprosy. This is the first case report of nocardial keratitis from Southeast Asia. The diminished corneal sensation in a patient with leprosy could be a predisposing factor for development or exacerbation of corneal ulceration.
Nocardia asteroides is a rare cause of keratitis usually associated with trauma (3). All of the cases of nocardial keratitis reported so far had been in Western countries (3, 7, 8, 10). Cases of bilateral conjunctivitis and of endophthalmitis due to N. asteroides have been reported from India (6) and Japan (9), respectively. This case is the 12th report of N. asteroides as a causative agent of corneal ulceration and the first report from Southeast Asia. Of all the cases reported so far, only one case involved a questionable diagnosis, of scarlet fever, as a condition predisposing the patient to the development of corneal ulceration. In the present case, there was no history of injury. A predisposing condition which may have led to the development of ulceration was leprosy.
Case report.
A 45-year-old housewife presented with diminished vision in the left eye of 5 days’ duration. She also experienced pain, redness, and watering in the left eye. On examination, the patient had lagophthalmos. There was perception and propagation of light in all four quadrants. The conjunctiva was congested. Corneal sensation was totally absent in the left eye and was decreased in the right eye. Sensation was determined by the sterile cotton wisp test. The corneal ulcer in the left eye was central and 4 mm in diameter, with a surrounding infiltrate and a few satellite lesions that were inferotemporal and inferomedial. The anterior chamber, which showed intense iritis, exhibited hypopyon in one-fifth of the area. Tension was digitally high. The lacrimal sac was patent. An examination of the right eye showed a peripheral corneal opacity in the inferior quadrant with evidence of pannus, suggestive of an old trachoma and the presence of an immature cataract.
The patient gave no history of trauma or foreign-body implantation preceding the development of corneal ulceration in the left eye. A gynecological, medical, otolaryngological, and dental examination was done to rule out a septic focus. On dermatological examination, the patient was diagnosed with borderline tuberculoid leprosy, with an anesthetic patch on the left forearm with a thickened left ulnar nerve. Split-skin smears did not show any acid-fast bacilli. Human immunodeficiency virus and Venereal Disease Research Laboratory tests were negative, and the results of other hematological and biochemical investigations were within normal limits.
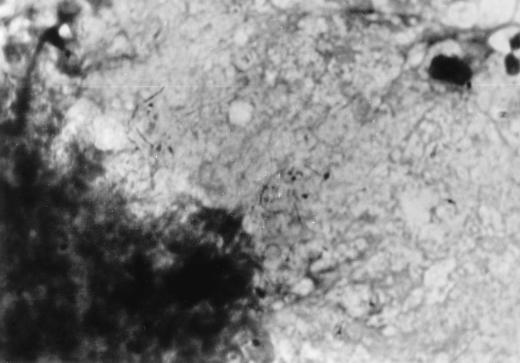
Corneal scrapings collected from the left eye were stained by Gram stain and also observed in a 10% KOH mount to rule out fungi. The gram-stained smear revealed numerous epithelial cells, few pus cells, and gram-positive thin branching hyphae, some of which were broken into bacillary and coccoid forms (Fig. 1). The smear was suggestive of an actinomycete. Modified acid-fast staining using 1% sulfuric acid as the decolorizer revealed acid-fast branching hyphae.
FIG. 1.
Gram-stained smear of corneal scrapings showing polymorphonuclear cells, gram-positive branching hyphae, and bacillary and coccoid forms of N. asteroides. Magnification, ×1,000.
Culture was performed on Sabouraud dextrose agar, Lowenstein-Jensen medium, and modified Thayer-Martin medium. After an incubation of 7 days, light-orange-colored, rough, wrinkled, dull colonies appeared on all three of the media. Detailed biochemical and physiological testing (11) revealed the growth to be N. asteroides.
Based on these findings, a diagnosis of N. asteroides keratitis was made. The patient was treated systemically with gentamicin (60 mg) by injection three times a day, oral ampicillin (250 mg) four times a day, oral trimethoprim-sulfamethoxazole (160 mg-800 mg) twice daily, and oral acetazolamide (250 mg) twice daily. For treatment of leprosy, the use of oral rifampin (600 mg) for 1 month and oral diaminodiphenyl sulfone (100 mg) for 6 months was advised. Topical treatment of the left eye consisted of ciprofloxacin eye drops (0.03%) once hourly, penicillin eye drops (1:10,000) once hourly, tobramycin-fortified eye drops (15 mg%) once hourly, and atropine (1%) ointment twice daily. With this treatment, marked improvement was seen in the affected eye after 10 to 12 days. After 2 weeks of hospitalization, the patient was better and the eye was quiet. The infiltrate was reduced in size, with a hypopyon streak.
The patient was discharged but was asked to visit the outpatient department for follow-up. Thereafter, however, she was lost to follow-up.
Discussion.
Nocardia species are associated with environmental materials, including soil. They commonly cause mycetomas and pulmonary infections but rarely are pathogens of the eye (3). In all of the previously reported cases (Table 1), a diagnosis was based on smear and/or culture positivity. Although clinical photographs and photographs of cultures were provided, primary-smear photographs were lacking in these reports. A primary smear made directly from a clinical lesion offers a rapid diagnosis, which is critical for institution of appropriate therapy for serious infections like corneal ulcers. The classical appearance of the organisms in the smears (Fig. 1), fortified by culture results, helped us to obtain an unequivocal diagnosis in this case.
TABLE 1.
Review of literature on ocular nocardiasis
| Case report authors (yr) | Patient’s age (yr) | Patient’s sexa | Predisposing event | Clinical presentation | Diagnostic criteria | Reference |
|---|---|---|---|---|---|---|
| Bruce and Locatcher-Khorazo (1942) | 50 | M | NKb | Punctate keratoconjunctivitis | NK | 2 |
| Benedict and Iverson (1944) | 23 | F | Scarlet fever? | Chronic keratoconjunctivitis | Positive smear and culture | 1 |
| Schardt, Unsworth, and Hayes (1956) | 33 | M | Stone trauma on farm | Corneal ulcer | Positive culture | 14 |
| Sigtenhorst and Gingrich (1957) | NK | NK | Cotton branch injury | Corneal ulcer | NK | 15 |
| Gingrich (1962) | 53 | M | Cotton plant scratch | Corneal ulcer | Positive culture | 5 |
| Newmark, Polack, and Ellison (1971) | 6 | M | Dirt injury | Corneal ulcer | Positive culture | 12 |
| Ralph, Lemp, and Liss (1976) | 11 | F | Fishline sinker abrasion | Corneal ulcer | Positive culture | 13 |
| Hirst, Harrison, Merz, and Start (1979) | 17 | M | Dirt injury | Corneal ulcer | Positive smear and culture | 7 |
| Hirst, Merz, and Richard Green (1982) | 30 | M | Gravel injury | Corneal ulcer with hypopyon | Positive smear and culture | 8 |
| Meurs and van Bijsterveld (1984) | 65 | M | No history of trauma or foreign-body implant | Corneal ulcer | Positive smear and culture | 10 |
| Donnenfeld, Cohen, Barza, and Baum (1985) | 31 | M | Agricultural injury | Corneal laceration and abscess | Positive smear and culture | 3 |
| Tendolkar, Varaiya, Ahuja, Motwane, and Gogate (1997) | 45 | F | No history of injury or foreign-body implant | Corneal ulcer | Positive smear and culture | This report |
M, male; F, female.
NK, not known.
Corneal ulcers are predominantly seen in males (Table 1), which may be a result of occupational exposure. This is evident in the seven cases of Nocardia keratitis reviewed by Hirst et al. in 1979 (7). A questionable diagnosis of scarlet fever as a predisposing cause has been reported by Benedict and Iverson (1). Overall, in eight cases, patients had a definite history of injury to the eye.
In both the lepromatous and tuberculoid types of leprosy, some degree of corneal anesthesia or hypesthesia may occur. In the lepromatous type, ocular complications are common, taking the form of lepromatous nodules and keratitis. In the tuberculoid type, on the other hand, exposure keratoconjunctivitis associated with paralytic lagophthalmos may occur (4).
In our case, there was no obvious history of injury. The ulcer apparently developed spontaneously in an eye affected by lagophthalmos resulting from a borderline tuberculoid type of leprosy. Absence of corneal sensation could be the reason that the patient did not feel any pain even if there was a trauma.
There is a possibility that N. asteroides was an opportunist in the dry eye resulting from lagophthalmos or that the patient was unaware of any trauma due to the absence of corneal sensation. Due to decreased corneal sensation and the resultant decreased perception of pain, the patient was treated late in the course of the disease, which is evident from the fact that a hypopyon had already developed and the eye was less irritated than is generally seen in infections with other bacteria, such as pneumococcus, Pseudomonas species, etc.
There is also a possibility that the present case is similar to a previous case report (10) and that the patient’s diagnosis of leprosy may be irrelevant. In the case reported by Meurs and van Bijsterveld (10), there was no history of trauma to the eye, nor was there any predisposing condition which could have led to an eye infection.
Even in the absence of history of injury to the eye, a patient with leprosy is likely to develop an opportunistic infection like that with N. asteroides.
Acknowledgments
We thank our dean, R. G. Shirahatti, for allowing us to publish this report of a case encountered during routine hospital care. We also acknowledge the technical assistance of Jagdish Sharma.
REFERENCES
- 1.Benedict W L, Iverson H A. Chronic keratoconjunctivitis associated with Nocardia. Arch Ophthalmol. 1944;32:89–92. [Google Scholar]
- 2.Bruce G M, Locatcher-Khorazo D. Actinomyces: recovery of the streptothrix in a case of superficial punctate keratitis. Arch Ophthalmol. 1942;27:294–298. [Google Scholar]
- 3.Donnenfeld E D, Cohen E J, Barza M, Baum J. Treatment of Nocardia keratitis with topical trimethoprim-sulfamethoxazole. Am J Ophthalmol. 1985;99:601–602. doi: 10.1016/s0002-9394(14)77973-5. [DOI] [PubMed] [Google Scholar]
- 4.Duke-Elder S, Leigh A G. System of ophthalmology, 1st ed., vol. VIII, part II. London, United Kingdom: Henry Kimpton; 1965. Disorders of the outer eye; pp. 729–859. [Google Scholar]
- 5.Gingrich W D. Keratomycosis. JAMA. 1962;179:602–608. doi: 10.1001/jama.1962.03050080014004. [DOI] [PubMed] [Google Scholar]
- 6.Gupta M L, Singh P, Goyal B K, Goyal A, Sharma R D. Bilateral conjunctivitis associated with Nocardia asteroides. Indian J Ophthalmol. 1982;30:167–168. [PubMed] [Google Scholar]
- 7.Hirst L W, Harrison K, Merz W, Start W. Nocardia asteroides keratitis. Br J Ophthalmol. 1979;63:449–454. doi: 10.1136/bjo.63.6.449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hirst L W, Merz W, Richard Green W. Nocardia asteroides corneal ulcer. Am J Ophthalmol. 1982;94:123–124. doi: 10.1016/0002-9394(82)90208-2. [DOI] [PubMed] [Google Scholar]
- 9.Ishibashi Y, Watanabe R, Hommura S, Koyama A, Ishikawa T, Mikami Y. Endogenous Nocardia asteroides endophthalmitis in a patient with systemic lupus erythematosus. Br J Ophthalmol. 1990;74:433–436. doi: 10.1136/bjo.74.7.433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Meurs P J, van Bijsterveld O P. Nocardia gypsoides corneal ulcer. Br J Ophthalmol. 1984;68:179–181. doi: 10.1136/bjo.68.3.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mishra S K, Gordon R E, Barnett D A. Indentification of nocardiae and streptomycetes of medical importance. J Clin Microbiol. 1980;11:728–736. doi: 10.1128/jcm.11.6.728-736.1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Newmark E, Polack F M, Ellison A C. Report of a case of Nocardia asteroides keratitis. Am J Ophthalmol. 1971;72:813–815. doi: 10.1016/0002-9394(71)90022-5. [DOI] [PubMed] [Google Scholar]
- 13.Ralph R A, Lemp M A, Liss G. Nocardia asteroides keratitis: a case report. Br J Ophthalmol. 1976;60:104–106. doi: 10.1136/bjo.60.2.104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schardt W M, Unsworth A C, Hayes C V. Corneal ulcer due to Nocardia asteroides. Am J Ophthalmol. 1956;42:303–305. doi: 10.1016/0002-9394(56)90937-0. [DOI] [PubMed] [Google Scholar]
- 15.Sigtenhorst M L, Gingrich W D. Bacteriologic studies of keratitis. South Med J. 1957;50:346–350. doi: 10.1097/00007611-195703000-00011. [DOI] [PubMed] [Google Scholar]