Abstract
Introduction
Choledocholithiasis is common, with patients usually treated with endoscopic retrograde cholangiopancreatography (ERCP) and subsequent cholecystectomy to remove the presumed source of common bile duct (CBD) stones. However, previous investigations into the management of patients following ERCP have focused on recurrent CBD stones, negating the risks of cholecystectomy. This article appraises the role of cholecystectomy following successful endoscopic clearance of bile duct stones.
Methods
Patients undergoing ERCP and CBD clearance for choledocholithiasis at St James’s University Hospital January 2015–December 2018 were included. Patients were divided into those who received cholecystectomy and those managed non-operatively. Readmissions, operative morbidity, mortality and treatment costs were investigated.
Results
Eight hundred and forty-four patients received ERCP and CBD clearance with 3.9 years follow-up. Two hundred and nine patients underwent cholecystectomy with 15% requiring complex surgery. Three hundred and seventy-three patients were non-operatively managed. Unplanned readmissions occurred in 15% following ERCP, mostly within two years. There was no difference in readmissions between the two groups. Accounting for the entire patient pathway, non-operative management was less expensive.
Conclusions
The majority of patients do not require readmission following ERCP for CBD stones, and cholecystectomy did not reduce the risk of readmission. Few patients have recurrent CBD stones, but complex biliary surgery is frequently required. Routine cholecystectomy following ERCP needs to be re-evaluated and a more stratified approach to future risk developed.
Keywords: Cholecystectomy, ERCP, Common bile duct, Stones, Readmissions
Introduction
Choledocholithiasis is a common presentation, causing pain, jaundice, cholangitis and pancreatitis. These patients usually undergo treatment in the form of endoscopic retrograde cholangiopancreatography (ERCP) and sphincterotomy, to clear the bile duct of stones and allow drainage of bile into the duodenum.1–3 This enlarges the biliary orifice, which in many cases allows for the passage of future stones without impaction. Furthermore, endoscopic sphincterotomy separates the biliary and pancreatic orifices eliminating the common channel and significantly reducing the risk of gallstone pancreatitis.4 Complete stone removal after endoscopic sphincterotomy can be achieved in up to 97% of cases with low morbidity and negligible mortality.5
To mitigate against the perceived risk of recurrent problems with CBD stones, some patients are offered laparoscopic cholecystectomy (LC) to remove the presumed source of CBD stones. Four RCTs have examined LC versus non-operative management.5–8 These studies show LC is associated with a reduced risk of recurrent CBD stones (4% versus 10%).9
However, LC following ERCP is associated with a high chance of conversion to an open operation (8.4%)10 and increased rates of serious complications including CBD injury, which result in longer hospital stays and more readmissions.11–15 Finally, marked biliary pain occurs in 4–9% of people after cholecystectomy, and 13–37% of people continue to experience persistent abdominal or nonspecific pain.13,14,16–19 Taken together, the literature shows that: (i) following bile duct clearance at ERCP, the majority of patients do not have further CBD stones; and (ii) LC may reduce the risk of CBD stones at the cost of operative risk and other adverse events.
In order to examine this balance of risks between future biliary events and operative complications, we sought to quantify the effect of LC on unplanned readmissions in a large single-centre cohort of consecutive patients following ERCP, sphincterotomy and duct clearance. These patients either proceeded to LC or were managed non-operatively. In addition, patient costs for both LC and non-operative management (NOM) were analysed.
Methods
Participants
All patients undergoing ERCP in St James’ Endoscopy Unit, Leeds Teaching Hospitals NHS Trust (LTHT) between 1 January 2015 and 31 December 2018 in whom bile duct stones were confirmed at cholangiography were included.
Procedures were performed using Olympus TJF 260V duodenoscopes by one of four experienced endoscopists. Patients were primarily under conscious sedation, though selected patients received general anaesthesia (GA). The unit performs more than 650 procedures per year. In any patient with confirmed CBD stones, sphincterotomy and balloon stone extraction is performed. If during the initial ERCP CBD clearance is incomplete, uncertain or not possible, a further procedure is scheduled, often under GA, to clear the duct. Additional duct clearance techniques include mechanical lithotripsy, balloon sphincteroplasty and intraductal cholangioscopy with electrohydraulic lithotripsy. CBD clearance after the index or subsequent ERCP(s) was confirmed by a balloon occlusion cholangiogram and the free passage of an inflated extraction balloon through the sphincterotomy.
All patients were entered prospectively onto a database prior to procedure as part of the departmental audit programme. This database records patient demographics and procedural details. Each patient’s electronic record is reviewed more than 30 days after the procedure and 30-day outcomes entered, including procedural success (biliary drainage), complications and mortality. Digital patient records were interrogated to identify the complete patient pathway including biliary surgery and complications, and biliary-related readmissions. Data collected included patient demographics, surgery type, date of surgery, elective or emergency surgery, American Society of Anesthesiologists (ASA) grade and follow-up. Importantly, at the initial surgical outpatient appointment, the reason for NOM was identified and recorded. Patients were divided into groups based on management plan. Patients in the LC group were either operated on during their index admission or booked for elective surgery either at discharge or at their follow-up outpatient appointment. The NOM group includes patients assessed to be unfit for surgery at their follow-up appointment and those who elected for non-operative management.
Outcomes
Planned analysis comprised readmission rates for recurrent biliary events including biliary colic, cholecystitis, cholangitis, pancreatitis or obstructive jaundice. In the patient group that underwent cholecystectomy following ERCP, the type of cholecystectomy, the length of stay following cholecystectomy and readmissions as a result of post-cholecystectomy complications were recorded. A complex cholecystectomy was defined as any operation other than LC or LC and intraoperative cholangiogram. This included, but was not limited to, conversion to open cholecystectomy, subtotal cholecystectomy, hepaticojejunostomy and abandoned procedure. Thirty-day and 90-day mortality following ERCP and cholecystectomy were recorded. The causes of death for those patients who died during the study were obtained from death certificates. Deaths due to obstructive jaundice, cholangitis, pancreatitis or cholecystitis were considered to be caused by gallstones.
Costings
The Department of Finance at LTHT analysed the complete patient pathway following ERCP for both groups of patients. They calculated overall costings and then determined cost per patient and cost difference between the groups.
Statistical analysis
Continuous data were described using mean and SD (or median and range if skewed), and categorical data were summarised as number and percentage. To measure differences between the groups, the Wilcoxon rank-sum test was used for non-parametric continuous variables. The independent-sample t-test was used for parametric continuous variables and the χ2 test for categorical variables. To determine the effect of cholecystectomy on unplanned hospital admission following ERCP, cholecystectomy was analysed as a time-varying covariate and unplanned admissions compared using time-to-event analyses with death analysed as a competing risk factor. Statistical analysis was performed using STATA (StataCorp, Texas, USA) version 11.2.
Ethical approval
The study protocol did not require research registration as anonymised, observational data were collected. This was confirmed by the online National Research Ethics Service decision tool (http://www.hra-decisiontools.org.uk/research/). The study was registered as a clinical audit at St James’ University Hospital, Leeds, UK. The STROBE statement checklist of items for cohort studies was followed (http://www.strobe-statement.org/).
Results
Participants
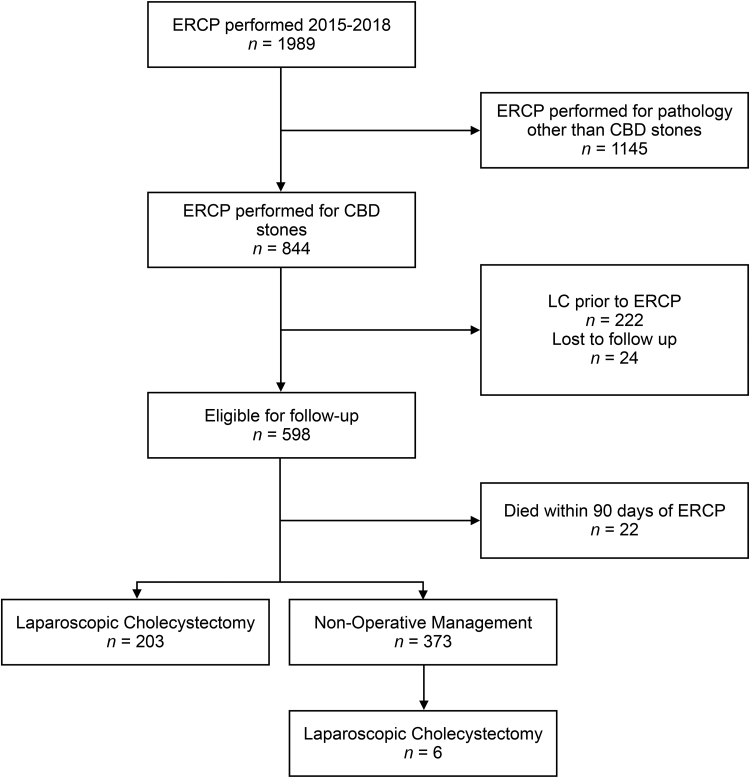
Between 1 January 2015 and 31 December 2018, 1989 ERCPs were performed. Eight hundred and forty-four patients underwent successful ERCP and duct clearance for CBD stones. Of these, 222 patients had previously undergone a cholecystectomy and 24 patients were lost to follow-up so were excluded from the study. Twenty-two patients died within 90 days of ERCP. Two hundred and three patients underwent planned cholecystectomy after ERCP. Three-hundred and seventy-three were initially managed non-operatively, of which six went on to have a LC; four patients had biliary colic and two cholecystitis. Sixty-five of 373 (17.4%) patients did not undergo surgery due to personal choice (Figure 1).
Figure 1 .
Flow diagram of study cohort selection. ERCP = endoscopic retrograde cholangiopancreatography; CBD = common bile duct; LC = laparoscopic cholecystectomy
Patient characteristics
The median age of the entire cohort was 70 years (range 17–97); patients were more frequently female (57%) than male. The median age of patients undergoing NOM was greater than patients undergoing LC (79 versus 61 years, p = 0.0001) and patients in the NOM group were more likely to have a higher ASA grade at the time of ERCP than patients undergoing planned LC (p = 0.0001) (Table 1). Median follow-up for the entire cohort of patients was 3.8 years (range 0.01–5.9 years). Median follow-up was 3.5 years in the NOM group compared to 4.4 years in the LC group.
Table 1 .
Baseline characteristics
| Variable | NOM | LC | p-value | |
|---|---|---|---|---|
| Overall | 395 | 203 | — | |
| Age (years), median (range) | 79 (19–97) | 61 (17–89) | 0.0001 | |
| ASA grade | 1 | 18 | 59 | 0.0000 |
| 2 | 140 | 107 | ||
| 3 | 217 | 31 | ||
| 4 | 17 | 5 | ||
| 5 | 2 | — | ||
| Female, n (%) | 221 (55) | 118 (58) | 0.61 | |
NOM = non-operative management; LC = laparoscopic cholecystectomy; ASA = American Society of Anesthesiologists
Survival
Following ERCP, 30- and 90-day mortality was 13/844 (1.5%) and 22/844 (2.7%), respectively. Mean age at death was 81 years. At 30 days, seven deaths were due to multi-organ failure secondary to cholangitis and two patients died as a result of acute severe pancreatitis secondary to ERCP. The other four deaths at 30 days and the additional nine deaths at 90 days were as a direct result of unrelated medical conditions. Overall survival was significantly greater for patients undergoing LC than NOM (HR 24.4, 95% CI 9.05–66.01, p = 0.000).
Operative intervention
The median time between ERCP and surgery was 118 days (IQR, 42 to 217). Two hundred and nine (203 planned cholecystectomy and 6 failed NOM) patients underwent operative intervention. Thirty-three patients (16%) had complex surgery; 23 had open cholecystectomy, either converted or planned, 4 patients had laparoscopic subtotal cholecystectomy, 1 had an open subtotal cholecystectomy, 4 had hepatico-jejuonostomies and 1 procedure was abandoned (Table 2). In 76 patients (36%), the length of stay was greater than 48h and in 54 patients (26%) the length of stay was greater than 72h.
Table 2 .
Operative intervention
| Procedure | n |
|---|---|
| Laparoscopic cholecystectomy | 125 |
| Laparoscopic cholecystectomy+IOC | 51 |
| Laparoscopic converted to open cholecystectomy | 18 |
| Open cholecystectomy (planned) | 5 |
| Laparoscopic subtotal cholecystectomy | 4 |
| Cholecystectomy+hepaticojejunostomy | 4 |
| Open subtotal cholecystectomy | 1 |
| Abandoned procedure | 1 |
| Total | 209 |
IOC = intraoperative cholangiogram
Readmissions
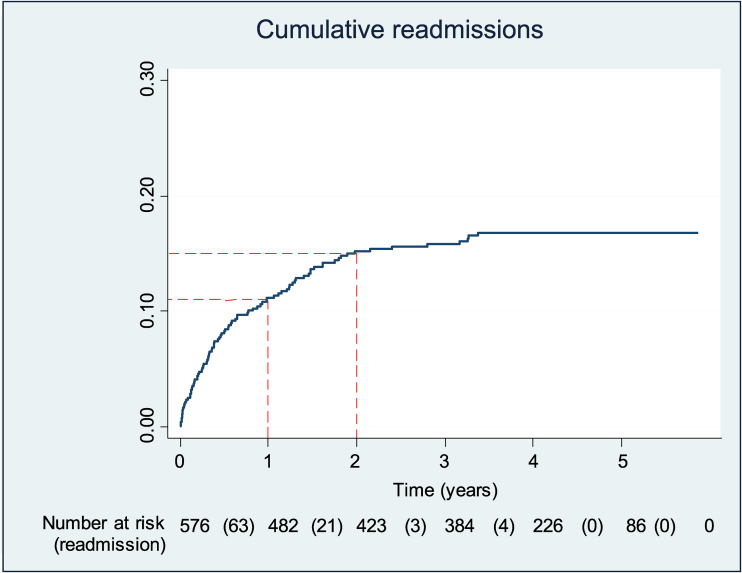
At least one unplanned readmission to hospital occurred in 91 patients (15%) following ERCP. Most readmissions occurred within two years of ERCP, 63 (69%) occurred within the first year and 21 (23%) within the second year post-ERCP (Figure 2). Thirty-six of 395 patients in the NOM group were readmitted (9%) compared with 55 of 203 patients in the LC group (27%). In the LC group, 33 patients (16.3%) were readmitted prior to surgery and 24 (11.8%) following surgery (2 patients were readmitted both pre- and post-surgery).
Figure 2 .
Cumulative readmissions following endoscopic retrograde cholangiopancreatography
Fourteen of the 24 readmissions following LC were directly attributable to complications of the surgery. Ten of 24 readmissions were due to further gallstone-related problems (9 patients had cholangitis requiring further ERCP and 1 biliary colic following subtotal cholecystectomy). In the group that had further readmissions after surgery, the median time from ERCP to surgery was 97 days, whereas in those with no further admissions, the median time was 164 days.
Recurrent choledocholithiasis occurred in 28 patients in the entire cohort (4.9%); 9 patients in the NOM group (2.3%), 10 patients while awaiting an LC (4.9%) and 9 patients following planned LC (4.4%).
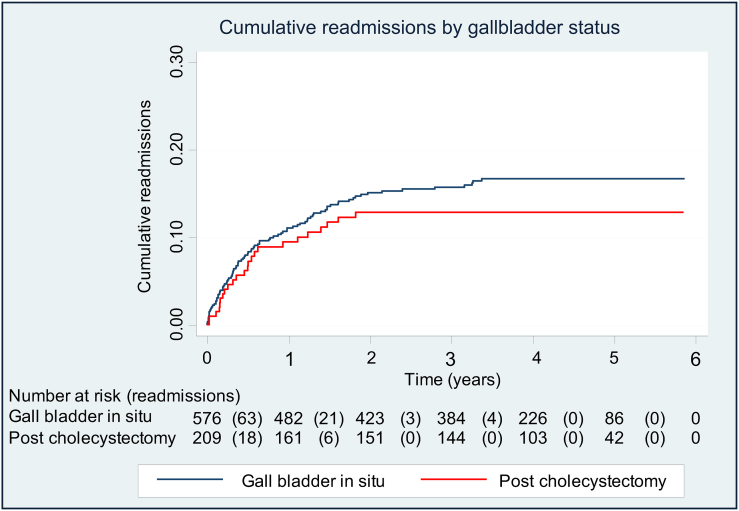
Adjusted readmissions
To assess the effect of operative intervention on unplanned readmissions, cholecystectomy was analysed as a time-varying covariate. For patients in the LC group, patient episodes were split into time with gall bladder in situ and time post-cholecystectomy. Patients pre-cholecystectomy were analysed in the same group as patients in the NOM group (gall bladder in situ) and compared with patients’ post-cholecystectomy. Readmissions of 576 patients with gall bladder in situ were compared with 209 patients after cholecystectomy with adjustment for death as a competing risk factor. The cumulative incidence of readmissions by group is seen in Figure 3. There was no statistically significant difference in readmissions between the two groups (subdistribution hazard ratio (SHR) 0.93, 95% CI 0.75–1.03).
Figure 3 .
Cumulative readmissions following endoscopic retrograde cholangiopancreatography by gallbladder status
Cost analysis
Cost analysis of the complete patient pathway showed that the average cost per patient in the NOM group was £7,487 compared with £10,584 in the LC group. This occurred despite NOM patients having a longer overall length of stay (15 versus 14 days). The additional cost incurred in the LC group was driven by the cost of an additional procedure and a greater average number of outpatient attendances (four versus three).
Discussion
In this large single-centre study we found that cholecystectomy was not associated with a reduction in readmissions following ERCP, sphincterotomy and duct clearance for CBD stones. In addition, low rates of recurrent bile duct stones were found overall (4.9%) and within subgroups, and the majority of readmissions occurred within two years. Finally, cholecystectomy was frequently complex following ERCP. Taken together, these findings support a reappraisal of the benefits of routine LC following ERCP.
Four previous RCTs have compared LC to expectant management following ERCP.5–8 These have shown expectant management is associated with an increased risk of future CBD stone events. These occurred in 10% of expectant management patients compared with 4% in the LC group (RR 2.31, 95% CI: 1.21–4.43]).9 The present study found a lower overall rate of recurrent CBD stones (4.9%), with rates of 4.7% in the LC group and 2.3% in the NOM group, despite longer follow-up. This may reflect improvements in endoscopic techniques or differences in assessment and follow-up. The RCTs5–8 found similar rates of complex LC following ERCP to this study (16%); 18% in patients randomised to LC and 10% in those randomised to NOM who then crossed over during the study period.
The remaining literature,11,20–36 primarily composed of small retrospective cohort studies, shows recurrent biliary events are more common in NOM patients, but this is driven by episodes of biliary colic or cholecystitis not ductal pathology (pancreatitis or cholangitis). A large retrospective administrative database cohort study37 compared outcomes in patients older than 64 years. It showed a clinically important difference in recurrent rates of CBD stones for patients undergoing NOM compared with LC (28% versus 13%) as well as low rates of surgical complications. However, the recurrent CBD stone rate is much higher than this study and published RCT evidence which makes it difficult to generalise and interpret these results.
In this study, the effect of LC on unplanned admissions following ERCP and sphincterotomy has been assessed. The results show that patients are as likely to require emergency admission (for biliary problems or treatment of complications of surgery) in the first three years following an ERCP and CBD clearance whether they undergo LC or not. Second, the current rationale for LC, based on 4 RCTs, is a reduction in recurrent CBD stones and associated complications. Compared with these studies, the rate of recurrent CBD stones was reduced in this study. This raises the possibility that with contemporary endoscopy techniques, there is a reduced benefit to routine LC following ERCP. In the NOM group, only 9 of 395 patients (2.3%) developed further CBD stones with just 6 patients (1.5%) undergoing a cholecystectomy. We found that most unplanned readmissions occurred within the first two years. This is clinically important because it suggests patients opting for NOM do not need a long length of follow-up. Finally, there were potential reduced overall costs of NOM when compared with LC.
A study strength is the large population of patients who underwent ERCP for CBD stones by experienced endoscopists with a long follow-up period. Duct clearance was confirmed in each patient and the decision for LC or NOM clearly identified. Clinically significant events, readmissions, have been used as the primary outcome. A weakness of this study is that the two groups of interest, those managed with LC and non-operatively, are not equivalent. The NOM group includes a significant proportion of patients who would not be fit to undergo LC. This is evidenced by the significantly higher mortality rate demonstrated in patients who received NOM, reflecting the age and comorbidity of this group as opposed to a treatment effect of LC. For this reason, we did not compare the groups directly but used cholecystectomy as a time-varying covariate and death as a competing risk factor to mitigate against the inherent biases. As a single-centre study we cannot generalise our outcomes; our rate of recurrent CBD stones following ERCP is lower than historical RCT literature and contemporary cohort studies. If replicated in other centres, the value of routine LC should be questioned.
Conclusions
In summary, the majority of patients did not require readmission following ERCP, sphincterotomy and duct clearance for CBD stones and cholecystectomy did not reduce the risk of readmission. Furthermore, only a small number of patients had recurrent CBD stones, but complex biliary surgery was three times more likely. In light of these findings, routine LC following ERCP should be re-evaluated and a more stratified approach to future risk developed. Randomised controlled trials powered to investigate an outcome that encompasses the risks and benefits of routine LC are required for this common biliary condition.
References
- 1.Poulose BK, Arbogast PG, Holzman MD. National analysis of in-hospital resource utilization in choledocholithiasis management using propensity scores. Surg Endosc Other Interv Tech 2006; 20: 186–190. [DOI] [PubMed] [Google Scholar]
- 2.Baucom RB, Feurer ID, Shelton JSet al. ERCP, and laparoscopic common bile duct exploration: do we need a standard approach for common bile duct stones? Surg Endosc 2016; 30: 414–423. [DOI] [PubMed] [Google Scholar]
- 3.Wandling MW, Hungness ES, Pavey ESet al. Nationwide assessment of trends in choledocholithiasis management in the United States from 1998 to 2013. JAMA Surg 2016; 151: 1125. [DOI] [PubMed] [Google Scholar]
- 4.da Costa DW, Schepers NJ, Römkens TEet al. Endoscopic sphincterotomy and cholecystectomy in acute biliary pancreatitis. Surgeon 2016; 14: 99–108. [DOI] [PubMed] [Google Scholar]
- 5.Boerma D, Rauws EAJ, Keulemans YCAet al. Wait-and-see policy or laparoscopic cholecystectomy after endoscopic sphincterotomy for bile-duct stones: a randomised trial. Lancet 2002; 360: 761–765. [DOI] [PubMed] [Google Scholar]
- 6.Heo J, Jung MK, Cho CM. Should prophylactic cholecystectomy be performed in patients with concomitant gallstones after endoscopic sphincterotomy for bile duct stones? Surg Endosc 2014; 29: 1574–1579. [DOI] [PubMed] [Google Scholar]
- 7.Zargar SA, Mushtaq M, Beg MAet al. Wait-and-see policy versus cholecystectomy after endoscopic sphincterotomy for bile-duct stones in high-risk patients with co-existing gallbladder stones: A prospective randomised trial. Arab J Gastroenterol 2014; 15: 24–26. [DOI] [PubMed] [Google Scholar]
- 8.Lau JYW, Leow CK, Fung TMKet al. Cholecystectomy or gallbladder In situ after endoscopic sphincterotomy and bile duct stone removal in Chinese patients. Gastroenterology 2006; 130: 96–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Khan MA, Khan Z, Tombazzi CRet al. Role of cholecystectomy after endoscopic sphincterotomy in the management of choledocholithiasis in high-risk patients. J Clin Gastroenterol 2018; 52: 579–589. [DOI] [PubMed] [Google Scholar]
- 10.Sutcliffe RP, Hollyman M, Hodson Jet al. Preoperative risk factors for conversion from laparoscopic to open cholecystectomy: a validated risk score derived from a prospective U.K. database of 8820 patients. HPB 2016; 18; 922–928. [DOI] [PMC free article] [PubMed]
- 11.Rochefort H, Matsuoka LEA, Chouliaras Ket al. Multiple preoperative endoscopic retrograde cholangiopancreatography and large common bile duct diameter predict the need for complex surgery. Am Surg 2016; 82: 122–127. [PubMed] [Google Scholar]
- 12.Middelfart HV, Kristensen JU, Laursen CNet al. Pain and dyspepsia after elective and acute cholecystectomy. Scand J Gastroenterol 1998; 33: 10–14. [DOI] [PubMed] [Google Scholar]
- 13.Bates T, Harrison M, Ebbs SR, A'Hern RP. Influence of cholecystectomy on symptoms. Br J Surg 1991; 78: 964–967. [DOI] [PubMed] [Google Scholar]
- 14.Borly L, Anderson IB, Bardram Let al. Preoperative prediction model of outcome after cholecystectomy for symptomatic gallstones. Scand J Gastroenterol 1999; 34: 1144–1152. [DOI] [PubMed] [Google Scholar]
- 15.Gui GP, Cheruvu CV, West Net al. Is cholecystectomy effective treatment for symptomatic gallstones? clinical outcome after long-term follow-up. Ann R Coll Surg Engl 1998; 80: 25–32. [PMC free article] [PubMed] [Google Scholar]
- 16.Gui G, Cheruvu CVN, West Net al. Fiennes AG: Is cholecystectomy effective treatment for symptomatic gallstones? clinical outcome after long-term follow-up. Ann R Coll Surg Engl 1998; 80: 25–32. [PMC free article] [PubMed] [Google Scholar]
- 17.Lorusso D, Porcelli P, Pezzolla Fet al. Persistent dyspepsia after laparoscopic cholecystectomy. The influence of psychological factors. Scand J Gastroenterol 2003; 38: 653–658. [DOI] [PubMed] [Google Scholar]
- 18.Ure BM, Troidl H, Spangenberger Wet al. Long-term results after laparoscopic cholecystectomy. Br J Surg 1995; 82: 267–270. [DOI] [PubMed] [Google Scholar]
- 19.Vetrhus M, Berhane T, Søreide O, Søndenaa K. Pain persists in many patients five years after removal of the gallbladder: observations from two randomized controlled trials of symptomatic, noncomplicated gallstone disease and acute cholecystitis. J Gastrointest Surg 2005; 9: 826–831. [DOI] [PubMed] [Google Scholar]
- 20.Aziret M, Karaman K, Ercan Met al. Early laparoscopic cholecystectomy is associated with less risk of complications after the removal of common bile duct stones by endoscopic retrograde cholangiopancreatography. Turk J Gastroenterol 2019; 30: 336–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Trejo-Ávila M, Solórzano-Vicuña D, García-Corral Ret al. Laparoscopic cholecystectomy after endoscopic treatment of choledocholithiasis: a retrospective comparative study. Updates Surg 2019; 71: 669–675. [DOI] [PubMed] [Google Scholar]
- 22.Nakai Y, Isayama H, Tsujino Tet al. Cholecystectomy after endoscopic papillary balloon dilation for bile duct stones reduced late biliary complications: a propensity score-based cohort analysis. Surg Endosc 2016; 30: 3014–3020. [DOI] [PubMed] [Google Scholar]
- 23.Nakeeb AE, Ezzet H, Askar Wet al. Early versus late cholecystectomy after clearance of common bile duct stones by endoscopic retrograde cholangiopancreatography. Surg Laparosc Endosc Percutan Tech 2016; 26: 202–207. [DOI] [PubMed] [Google Scholar]
- 24.Kim MH, Yeo SJ, Jung MK, Cho CM. The impact of gallbladder status on biliary complications after the endoscopic removal of choledocholithiasis. Dig Dis Sci 2016; 61: 1165–1171. [DOI] [PubMed] [Google Scholar]
- 25.Reinders JSK, Gouma DJ, Heisterkamp Jet al. Laparoscopic cholecystectomy is more difficult after a previous endoscopic retrograde cholangiography. HPB (Oxford) 2013; 15: 230–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yasui T, Takahata S, Kono Het al. Is cholecystectomy necessary after endoscopic treatment of bile duct stones in patients older than 80 years of age? J Gastroenterol 2012; 47: 65–70. [DOI] [PubMed] [Google Scholar]
- 27.Lai J-H, Wang H-Y, Chang W-Het al. Recurrent cholangitis after endoscopic lithotripsy of common bile duct stones with gallstones In situ: predictive factors With and without subsequent cholecystectomy. J Laparoendosc Adv Surg Tech 2012; 22: 324–329. [DOI] [PubMed] [Google Scholar]
- 28.Tsai T-J, Lai K-H, Lin C-Ket al. The relationship between gallbladder status and recurrent biliary complications in patients with choledocholithiasis following endoscopic treatment. J Chin Med Assoc 2012; 75: 560–566. [DOI] [PubMed] [Google Scholar]
- 29.Reinders JSK, Goud A, Timmer Ret al. Early laparoscopic cholecystectomy improves outcomes after endoscopic sphincterotomy for choledochocystolithiasis. Gastroenterology 2010; 138: 2315–2320. [DOI] [PubMed] [Google Scholar]
- 30.Li VKM, Yum JLK, Yeung YP. Optimal timing of elective laparoscopic cholecystectomy after acute cholangitis and subsequent clearance of choledocholithiasis. Am J Surg 2010; 200: 483–488. [DOI] [PubMed] [Google Scholar]
- 31.Kageoka M, Watanabe F, Maruyama Yet al. Long-term prognosis of patients after endoscopic sphincterotomy for choledocholithiasis. Dig Endosc 2009; 21: 170–175. [DOI] [PubMed] [Google Scholar]
- 32.Pierce RA, Jonnalagadda S, Spitler JAet al. Incidence of residual choledocholithiasis detected by intraoperative cholangiography at the time of laparoscopic cholecystectomy in patients having undergone preoperative ERCP. Surg Endosc 2008; 22: 2365–2372. [DOI] [PubMed] [Google Scholar]
- 33.Schiphorst AHW, Besselink MGH, Boerma Det al. Timing of cholecystectomy after endoscopic sphincterotomy for common bile duct stones. Surg Endosc 2008; 22: 2046–2050. [DOI] [PubMed] [Google Scholar]
- 34.Costi R, DiMauro D, Mazzeo Aet al. Routine laparoscopic cholecystectomy after endoscopic sphincterotomy for choledocholithiasis in octogenarians: is it worth the risk? Surg Endosc 2007; 21: 41–47. [DOI] [PubMed] [Google Scholar]
- 35.Drake BB, Arguedas MR, Kilgore MLet al. Economical and clinical outcomes of alternative treatment strategies in the management of common bile duct stones in the elderly: wait and See or surgery? Am J Gastroenterol 2006; 101: 746–752. [DOI] [PubMed] [Google Scholar]
- 36.Schreurs WH, Vles WJ, Stuifbergen WHNM, Oostvogel HJM. Endoscopic management of common bile duct stones leaving the gallbladder in situ. Dig Surg 2004; 21: 60–65. [DOI] [PubMed] [Google Scholar]
- 37.Elmunzer JB, Noureldin M, Morgan KAet al. The impact of cholecystectomy after endoscopic sphincterotomy for complicated gallstone disease. Am J Gastroenterol 2017; 112: 1596–1602. [DOI] [PubMed] [Google Scholar]