Abstract
Introduction:
Varicocelectomy is the prevailing management of scrotal pain secondary to varicocele. However, the literature is controversial on this topic. Some data showed that pain may persist after the surgery even if the varicocele is not detected postoperatively.
Objectives:
The objectives of the study were to identify the effect of varicocelectomy in patients with chronic scrotal pain, to report the association between the clinical grade and postoperative pain resolution, and to identify the need for a secondary procedure after varicocelectomy to control the pain.
Materials and Methods:
This was a retrospective study of 47 patients who underwent varicocelectomy between March 2016 and December 2018.
Results:
Postoperatively, the pain totally resolved after surgery in 64.3% of patients with scrotal pain; it improved in 21.4%, 11.9% have persistent pain, and the pain got worse in only 2.4%. Our study showed 100% complete resolution or improvement with Grade I, 85.7% in Grade II, and 81.3% in Grade III. In addition, all patients who underwent bilateral varicocelectomy had pain that either completely resolved or improved postoperatively. On the other hand, all patients who had persistent pain or pain worsening postoperatively had unilateral varicocelectomy. An additional intervention for postoperative pain control was needed in only 14% of patients, 7% of them underwent embolization, 4.7% had a cord block, and 2.3% were sent to a pain clinic.
Conclusion:
Varicocelectomy offers good outcomes in most patients with varicocele-related scrotal pain. The most significant predictor for success was low grade and bilaterality. However, there is a subset of patients whose symptoms will not improve postoperatively. Careful preoperative counseling and expectation management are crucial when discussing surgical options for those patients.
Keywords: Scrotal pain, varicocele, varicocelectomy
INTRODUCTION
Varicocele is a well-recognized cause of decreased testicular function and affects approximately 15%–20% of all males and up to 40% of infertile males.[1] It is the most common cause of reversible infertility, yet the majority are asymptomatic and fertile.[2] Varicocele-related scrotal pain accounts for 2%–10% of all varicocele cases.[1] Varicocele-related pain is usually described as dull aching pain and scrotal heaviness that may be aggravated by standing or exercising.[3]
Varicocelectomy is recommended to patients who present with testicular pain. The American Urological Association and the American Society of Reproductive Medicine recommend varicocele repair for patients with clinically palpable varicocele, documented infertility, one or more abnormal semen parameters, or with normal or potentially correctable female infertility.[4,5]
Varicocelectomy is the prevailing management of scrotal pain secondary to varicocele.[6] However, the literature on this matter is controversial.[6] The data show that pain may persist after surgery even if the varicocele is not detected postoperatively.[7] Therefore, our study explores the beneficial effects of surgical repair of varicocele-related scrotal pain and defines the factors that may improve the outcome.
MATERIALS AND METHODS
This was a retrospective cohort study of 131 patients; 48 out of 131 underwent varicocelectomy due to pain performed between March 2016 and December 2018 at King Abdul Aziz Medical City National Guard Hospital, Riyadh, Saudi Arabia.
The study included all patients who underwent varicocelectomy at the mentioned period with no exclusion criteria. We reviewed each patient for demographic data, varicocele diagnosis based on radiological or clinical diagnosis, or both. We evaluated the clinical grade and radiological grade if obtained, site of operation, the indication, and associated symptoms. If the pain is one of the associated symptoms, then it was further detailed including the site, the use of pain medications, assessment of postoperative pain, and if the patient underwent any additional intervention for pain control.
Our primary end point is the postoperative pain resolution. The secondary end point is the association between clinical grade and postoperative pain and the need for an additional procedure after varicocelectomy to control the scrotal pain.
The data were entered and analyzed using SPSS Version 20.0 Armonk, NY: IBM Corp. The categorical variables are presented as frequencies and percentages. Fisher’s exact test was used to compare the categorical variables. A P < 0.05 was considered statistically significant.
RESULTS
There were 131 patients included in this study; 48 had a varicocelectomy due to pain. The mean age was 31.87 years [Table 1], and 47 out of 48 reported scrotal pain. The data on the remaining patient’s pain site were not available. Therefore, we analyzed the 47 patients who had documented scrotal pain with 5 out of 47 lost follow-up. Of these, 35 patients had left, two patients had right, and 10 had bilateral varicocelectomy [Chart 1].
Table 1.
Patient demographics
| n | % | |
|---|---|---|
| Total | 47 | 100% |
| Age | Mean=31.87 | |
| Median=30.00 | ||
| Site (Scrotal) | 47 | 100% |
| Varicocele Side | ||
| Left | 35 | 74.5% |
| Right | 2 | 4.3% |
| Bilateral | 10 | 21.2% |
| Use of pre-operative pain medications | 4 | 8.5% |
Chart 1.
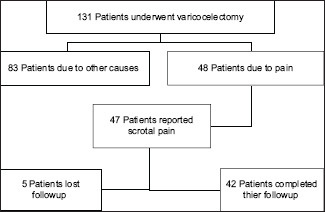
Patient flow chart
Thirty-three patients underwent varicocelectomy solely because of pain, and the remaining 14 patients had pain and infertility. Pain requiring pain medications was seen in only 8.5% of the patients, and most (91.5%) of them did not use any analgesics.
The associated symptoms were studied as well – we found that two patients had lower urinary tract symptoms. The pain improved postoperatively in only one of them. The diagnosis was made in 68.1% by both clinical diagnosis and radiological features; 17% had a clinical examination only, and the remaining 14.9% only had a testicular ultrasound. Twenty patients were Grade III, 15 were Grade II, 6 were Grade I, and 4 had no clinical varicocele. The remaining two patients had no documented grade in their charts.
Postoperative pain totally resolved after the surgery in 64.3% of patients and improved in 21.4%. The postoperative outcome for each grade is detailed in Table 2. In addition, bilateral cases observed to be associated with better pain resolution in comparison to unilateral cases [Table 3]. Postoperatively, 37 patients required no additional intervention for pain. Three of them underwent varicocele embolization, two had a cord block, and one was sent for pain clinic service; the remaining patients were lost follow-up.
Table 2.
Post-operative pain and clinical grades
| Post-op pain Resolved/Improved | Post-op pain No change/Worse | Total | ||
|---|---|---|---|---|
| Clinical Grade | 0* | 100% | 0.0% | 100% |
| G1 | 100% | 0.0% | 100% | |
| G2 | 85.7% | 14.3% | 100% | |
| G3 | 81.3% | 18.8% | 100% | |
| Total | 87.5% | 12.5% | 100% | |
| Chi-Square test | P= 0.56 | |||
Abbreviations: Post-op: Post-operative, 0*: Clinical varicocele documented in patient chart without grading.
Table 3.
Post-operative pain and side of varicocelectomy
| Post-operative Pain | Total | ||
|---|---|---|---|
|
| |||
| Resolved / Improved | No Change / Worse | ||
| Unilateral | 26 (81.3%) | 6 (18.8%) | 32 (100%) |
| Bilateral | 10 (100%) | 0 | 10 (100%) |
| total | 36 (85.7%) | 6 (14.3%) | 42 (100%) |
| P= 0.31 | |||
DISCUSSION
Painful varicocele accounts for 2%–10% of all varicocele cases.[1] Painful varicocele used to be debatable for surgical repair as varicocelectomy was preserved for male factor infertility, semen analysis abnormality, and testicular atrophy.
In 2014, the American Society for Reproductive Medicine together with the Society for Male Reproduction and Urology issued new guidelines suggesting surgery for the management of painful varicoceles when other pathologies of orchialgia have been ruled out and pain is persistent despite conservative treatment.[2,3] However, there is a lack of sufficient evidence of varicocelectomy indications for painful varicocele. Thus, the decision to treat surgically is difficult because there is no clear guidance on preoperative indicators.[6,8,9]
The patient should be carefully evaluated preoperatively for pain and other causes of chronic orchialgia such as epididymitis, epididymal cyst, and hydrocele. Conservative treatment including scrotal support, nonsteroidal inflammatory drugs, and limited vigorous physical activities must be initiated before the surgical option is decided.[7,10-12]
In 2015, a prospective study was completed consisting of Grade 3 varicocele patients who underwent microsurgical varicocelectomy for chronic pain and 88% showed complete resolution of the pain.[1] Persistent postoperative pain was reported to be around 10%. In our study, complete resolution of pain after surgery was seen in 64.3% of patients, and pain improvements were reported in 21.4% of patients.
Many groups have tried to explore the predictors of varicocelectomy success. Some studies questioned if the surgical approach is a factor and reported that microsurgery has more satisfactory results than laparoscopy. Subinguinal varicocelectomy is found to be superior to inguinal or high-inguinal varicocelectomy.[6,9] All of our patients underwent microscopic subinguinal varicocelectomy by ligation of the veins only per the approach at our intuition.
The success rate is related to the grade and varies in the literature.[7] A meta-analysis from 2016 showed that the grade of varicocele is not significantly related to pain resolution after varicocelectomy.[1,7] Other studies found that a higher grade is associated with less success.[4,8] Nevertheless, our study showed 100% complete resolution or improvement with Grade I, 85.7% in Grade II, and 81.3% in Grade III. We also observed that bilateral cases were associated with better pain resolution. On the other hand, 18.8% of patients with persistent pain or pain worsen postoperatively had unilateral varicocelectomy although the P value was insignificant (P = 0.31). In addition, the duration of pain was a significant factor for the success of pain resolution postoperatively.[6,9] A longer duration implies better outcomes. Unfortunately, this factor was not explained in our study due to missing data about the exact duration.
The characteristics of the pain were also studied. There was a significant correlation between dull pain and pain resolution.[1] The pain characteristics were not included in our variables.
In our study, we looked for any additional intervention for postoperative pain control: 37 out of 47 patients in our study had no additional intervention, three of them underwent embolization, two had a cord block, and one was sent to the pain clinic for further management. Further interventions were considered in that five out of the six patients as they had pain that did not improve; the remaining patient had worse pain after surgery.
CONCLUSION
The great impact of varicocelectomy on infertile men was shown and proved in many studies in the literature. There are limited and insufficient data available for varicocelectomy and pain-induced varicocele. Our data showed that two-thirds of patients who underwent varicocelectomy due to varicocele-related scrotal pain had complete postoperative pain resolution or improvement. The most significant predictor for success was low grade and bilateral cases. Careful preoperative counseling and expectation management are crucial when discussing surgical options for those patients.
Limitations
The limitation of our study is the small sample size and those patients lost to follow-up. This was overcome by contacting the patients by telephone – some of them responded, and the missing data were added but others did not respond in two separate calls.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We gratefully acknowledge Dr. Aamir Omair, College of Medicine, King Saud bin Abdulaziz University for Health Sciences for his great statistical support.
REFERENCES
- 1.Han DY, Yang QY, Chen X, Ouyang B, Yao B, Liu GH, et al. Who will benefit from surgical repair for painful varicocele:A meta-analysis. Int Urol Nephrol. 2016;48:1071–8. doi: 10.1007/s11255-016-1246-7. [DOI] [PubMed] [Google Scholar]
- 2.Owen RC, McCormick BJ, Figler BD, Coward RM. A review of varicocele repair for pain. Transl Androl Urol. 2017;6:S20–9. doi: 10.21037/tau.2017.03.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Practice Committee of the American Society for Reproductive Medicine. Society for Male Reproduction and Urology. Report on varicocele and infertility:A committee opinion. Fertil Steril. 2014;102:1556–60. doi: 10.1016/j.fertnstert.2014.10.007. [DOI] [PubMed] [Google Scholar]
- 4.Chu DI, Zderic SA, Shukla AR, Srinivasan AK, Tasian GE, Weiss DA, et al. Does varicocelectomy improve semen analysis outcomes in adolescents without testicular asymmetry? J Pediatr Urol. 2017;13:76.e1. doi: 10.1016/j.jpurol.2016.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mehta A, Goldstein M. Microsurgical varicocelectomy:A review. Asian J Androl. 2013;15:56–60. doi: 10.1038/aja.2012.98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Vakalopoulos I, Kampantais S, Lymperi S, Grivas N, Ioannidis A, Mykoniatis I, et al. Should we expand the indications for varicocele treatment? Transl Androl Urol. 2017;6:931–42. doi: 10.21037/tau.2017.08.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Abrol N, Panda A, Kekre NS. Painful varicoceles:Role of varicocelectomy. Indian J Urol. 2014;30:369–73. doi: 10.4103/0970-1591.128497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Association AU. Inc. Report on Varicocele and Infertility:An AUA Best Practice Policy and ASRM Practice Committee Report, 2001. 2015 [Google Scholar]
- 9.Paick S, Choi WS. Varicocele and testicular pain:A review. World J Mens Health. 2019;37:4–11. doi: 10.5534/wjmh.170010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shridharani A, Owen RC, Elkelany OO, Kim ED. The significance of clinical practice guidelines on adult varicocele detection and management. Asian J Androl. 2016;18:269–75. doi: 10.4103/1008-682X.172641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Vakalopoulos I, Kampantais S, Lymperi S, et al. Should we expand the indications for varicocele treatment? 2017;6(2):931–42. doi: 10.21037/tau.2017.08.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dabaja AA, Goldstein M. When is a varicocele repair indicated:The dilemma of hypogonadism and erectile dysfunction? Asian J Androl. 2016;18:213–6. doi: 10.4103/1008-682X.169560. [DOI] [PMC free article] [PubMed] [Google Scholar]


