Key Points
-
•
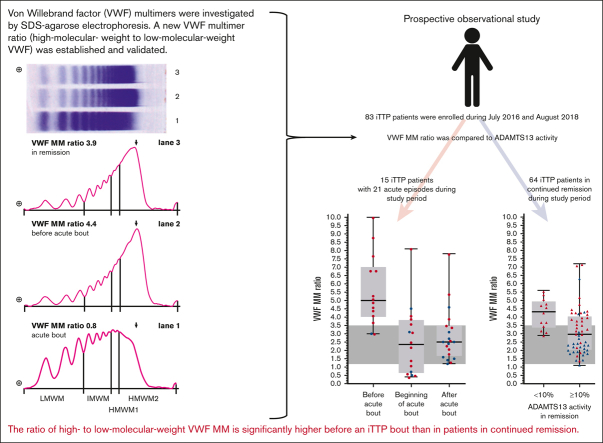
Eighty-three patients with iTTP were prospectively evaluated for ADAMTS13 activity, conformation, and for a novel VWF MM ratio.
-
•
This ratio of high- to low-molecular weight VWF MM is significantly higher before an iTTP bout than in patients in continued remission.
Visual Abstract
Abstract
Immune-mediated thrombotic thrombocytopenic purpura (iTTP), an autoantibody-mediated severe ADAMTS13 deficiency, is caused by insufficient proteolytic processing of von Willebrand factor (VWF) multimers (MMs) and microvascular thrombi. Recurrence of acute iTTP is associated with persistence or reappearance of ADAMTS13 deficiency. Some patients remain in remission despite recurring or persisting severe ADAMTS13 deficiency. In a prospective 2-year observational study, we investigated VWF MM patterns and ADAMTS13 in patients with iTTP in remission and at acute episodes. Of the 83 patients with iTTP, 16 suffered 22 acute episodes whereas 67 remained in clinical remission during follow-up, including 13 with ADAMTS13 <10% and 54 with ADAMTS13 ≥10%. High -molecular weight to low-molecular weight VWF MM ratio based on sodium dodecyl sulfate-agarose gel electrophoresis was compared with ADAMTS13 activity. VWF MM ratio was significantly higher in patients in remission with <10% compared with ≥10% ADAMTS13 activity. Fourteen samples obtained from 13 to 50 days (interquartile range; median, 39) before acute iTTP onset (ADAMTS13 <10% in 9 patients and 10%-26% in 5) showed VWF MM ratios significantly higher than those from 13 patients remaining in remission with ADAMTS13 <10%. At acute iTTP onset, VWF MM ratio decreased significantly and was low in all patients despite <10% ADAMTS13. The VWF MM ratio does not depend exclusively on ADAMTS13 activity. The disappearance of high molecular weight VWF MMs resulting in low VWF MM ratio at iTTP onset may be explained by consumption of larger VWF MMs in the microcirculation. The very high VWF MM ratio preceding acute iTTP recurrence suggests that VWF processing is hampered more than in patients remaining in remission.
Introduction
Immune-mediated thrombotic thrombocytopenic purpura (iTTP) is caused by a severe deficiency of ADAMTS13 (a disintegrin and metalloprotease with thrombospondin type 1 motifs 13) because of autoantibodies that inhibit or clear the protease.1, 2, 3 In patients with severe ADAMTS13 deficiency, the proteolytic processing of high molecular weight prothrombotic von Willebrand factor (VWF) multimers (MMs) into smaller, less adhesive molecules fails. Under high shear stress in arterioles and capillaries, VWF- and platelet-rich microthrombi occur4, 5, 6 resulting in thrombocytopenia and microangiopathic hemolytic anemia with schistocytes. The microthrombi lead to organ ischemia, dysfunction, and clinical symptoms.6, 7, 8 The acute iTTP episode is associated with high mortality and therefore requires rapid, appropriate therapy. Apart from therapeutic plasma exchange (TPE), plasma replacement and corticosteroids,9,10 the anti-CD20 monoclonal antibody (mAb) rituximab11, 12, 13, 14 and since 2018, caplacizumab, a therapeutic nanobody binding to the A1 domain of VWF and preventing platelet binding and activation, became available.15, 16, 17
After an initial acute episode, up to 40% of survivors relapse over the ensuing years.18,19 However, ADAMTS13 deficiency alone is not sufficient to trigger recurrence because some patients do not relapse despite consistently low ADAMTS13 levels. The complement system, inflammation, and cytokines seem to play an important, but currently not completely clarified, role in iTTP pathophysiology.20, 21, 22 In addition, Roose et al demonstrated that ADAMTS13 is present in an open conformation during acute iTTP23 and that open conformation in remission may herald recurrence.24 In a mouse model using ADAMTS13 and VWF double-knockout mice (ADAMTS13−/−/VWF−/−), Chauhan et al25 demonstrated that VWF deficiency abrogates the prothrombotic state of ADAMTS13 deficiency, suggesting that VWF is the indispensable mediator for platelet clumping.
VWF is secreted as an ultra-large MM, mainly from endothelial cells, and mediates platelet adhesion and aggregation at sites of vascular damage.26,27 Cleavage by ADAMTS13 results in a typical MM pattern of higher and lower molecular weight MMs in plasma.26,27 High molecular weight multimers (HMWM) (∼5500-10 000 kDa) are more adhesive than lower molecular weight multimers (LMWM), and excessive cleavage reduces the ability of VWF to recruit platelets.4,6,28 Unusually large VWF MMs (>10 000 kDa) are particularly adhesive and observed in the plasma of patients with TTP as a result of low ADAMTS13 activity. They are detectable only in remission and disappear during the acute episode, most likely because of the consumption in microthrombi.29,30 For ∼3 decades the analysis of ultra-large VWF MMs has been a part of the extended diagnostics in TTP,29 but the method is laborious, requires a lot of expertise, and is therefore rarely offered for diagnostic purpose. The complicated procedure is not standardized and shows high gel-to-gel variability, even in the hands of the same investigator.31 The Hydragel method is a well-standardized precast agarose gel system for VWF MM analysis.32, 33, 34, 35, 36 Although the resolution of the gel is not sufficient for assessing the triplet structure of LMWM bands, the detection of absent HMWM is reliable and thus von Willebrand disease types 2A and 2B can be distinguished from type 1.32,36,37 Ultra-large VWF MMs cannot be clearly separated from physiologic HMWM, but densitometric quantification of 3 predefined MM ranges (HMWM, intermediate molecular weight multimers [IMWM], and LMWM) are so reliable that reference ranges have been established.27,32,35,37 Therefore, we investigated whether quantification of a newly defined fraction of HMWM compared with LMWM is an appropriate marker for ultra-large VWF MMs and may, in conjunction with other risk markers (ADAMTS13 activity and ADAMTS13 conformation index [CI]), be used as prognostic follow-up marker in iTTP.
Patients and methods
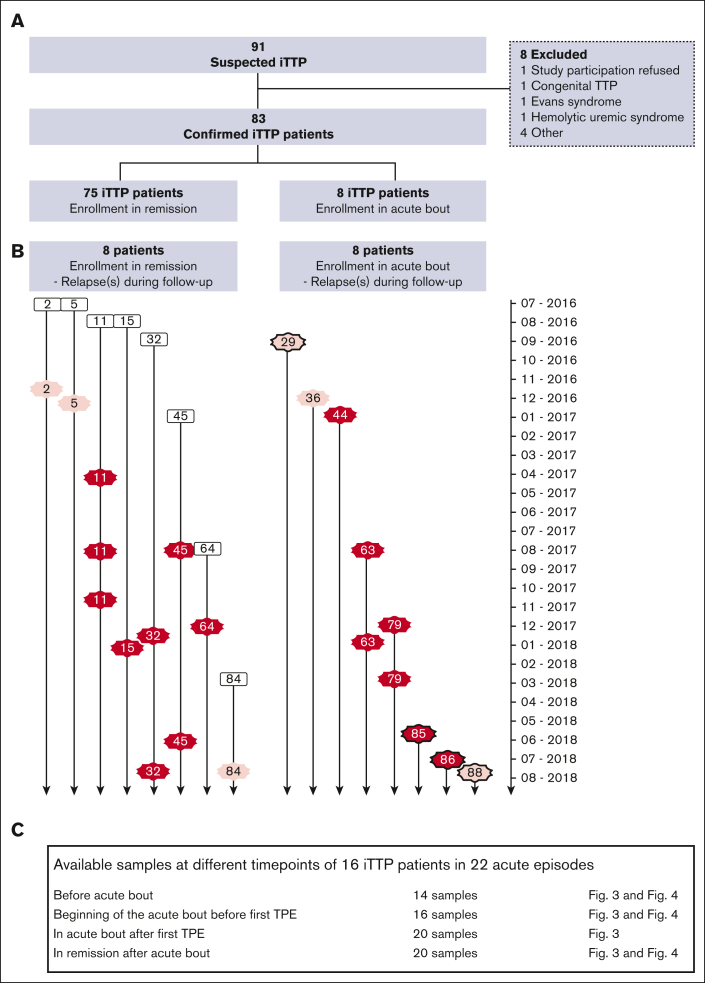
In the study period from July 2016 to August 2018, 91 patients with suspected or known iTTP were screened. One patient refused to participate. Of 90 initially included patients, 83 were confirmed to have iTTP (Figure 1). In 7 patients with suspected iTTP, a different diagnosis was made shortly after inclusion (Figure 1A). Of the 83 patients with iTTP, 8 were enrolled in the study during an acute episode including 4 with a first iTTP bout (Figure 1B). Seventy-five patients were enrolled during clinical remission. After inclusion in the study, 14 acute relapses occurred in 10 different patients during follow-up. Therefore, a total of 22 acute episodes were recorded in 16 patients over the study period (Figure 1B).
Figure 1.
Recruitment of patients with iTTP cohort highlighting all acute iTTP episodes occurring during the prospective study. (A) Overview of patients enrolled in remission and during an acute iTTP episode. (B) All patients suffering 1 or several acute bouts are represented over the whole study period (time axis from July 2016 to August 2018 indicated on the right side). The left side of the panel shows the 8 patients enrolled in remission who suffered from relapse(s) during follow-up (black outlined boxes with patient numbers #2, 5, 11, 15, 32, 45, 64, 84). The red and pink stars show the acute relapse(s). The right side of the panel shows the 8 patients enrolled in acute episodes, indicated by red and pink stars (patient numbers #29, 36, 44, 63, 79, 85, 86, 88). The black outline of the stars indicates initial diagnoses (patients #29, 85, 86, 88). Pink stars indicate the acute episodes of patients who received treatment prior to biobanking. No blood samples were available from them at begin of the acute bout before first TPE (refer to panel C below). Red stars mark acute bouts with complete data and biobanking. (C) Summary of all available samples of 16 patients with 22 acute iTTP episodes at various time points (days-weeks before, acute iTTP onset before first TPE, during acute iTTP after first TPE, in remission after acute iTTP).
According to the outcome criteria proposed by an International Working Group on TTP,38 acute TTP relapses are defined as platelet decrease (<150 000 cells/μL), LDH increase (>400 U/L), with or without clinical symptoms occurring in remission. This latter is defined as normalized platelets (>150 000cells/μL) and LDH <1.5× upper normal limit after discontinuing TPE and is sustained for >30 days.38 Our cohort study ended before the introduction of caplacizumab into clinical practice obviating the need to apply the revised outcome criteria.39
Optimally, patients in remission were followed up as outpatients from every 3 to 4 months (52%), sometimes more often if a pending relapse was suspected, and others (34%) were seen only once a year. Patients in remission received a clinical examination, and blood was drawn for laboratory analysis and biobanking (supplemental Methods). Patients with acute iTTP were hospitalized and received a comprehensive laboratory analysis and biobanking before the first TPE. Laboratory routine testing and biobanking were performed daily before the TPE session for 10 days and twice a week thereafter until hospital discharge.
The prospective study was approved by German law (Landeskrankenhausgesetz §36 and §37) in accordance with the Declaration of Helsinki and by the ethics committee of the “Landesärztekammer Rheinland-Pfalz” (837.506.15 [10274]).
Controls
Forty pseudonymized patient controls and 25 controls were analyzed for deriving a reference VWF MM ratio (supplemental methods).
Assays (see also supplemental Methods)
VWF antigen and VWF activity
VWF antigen (VWF:Ag) as well as activity (VWF:Ab)40 were measured at the University Medical Center Mainz using an ACL Top 750 coagulation analyzer (Instrumentation Laboratory/Werfen Diagnostics). In these immunoassays, VWF:Ag agglutinates with the polyclonal antibody–coated latex particles. Agglutination is proportional to the amount of VWF:Ag and is determined photometrically. VWF:Ab was also determined by an immunoturbidimetric assay, but the latex particles were coated with a mAb against the glycoprotein Ib binding site of VWF (HaemosIL VWF activity).40
ADAMTS13 activity and antigen
ADAMTS13 activity (ADAMTS13:act) was examined in Mainz using the fluorescence resonance energy transfer (FRET) method41 (Peptide Institute, INC FRETS-VWF73 substrate) modified as described.42,43 ADAMTS13 activity was expressed as a percentage of pooled normal plasma. The normal range in healthy donors is >50% with a detection limit of 1%.
ADAMTS13 antigen (ADAMTS13:Ag), experiment conducted in KU Leuven Campus Kortrijk, Belgium, was measured by an in-house developed ADAMTS13 antigen enzyme-linked immunosorbent assay (ELISA) as previously described.23,44 In brief, plasma samples and a dilution series of normal human plasma (NHP) were added to a 96-well plate coated with mouse mAb 3H9.45 Captured ADAMTS13 was colorimetrically detected using a mixture of biotinylated murine mAbs, 17G2 and 19H446 and horseradish peroxidase (HRP)–labeled streptavidin (Roche Diagnostics). The ADAMTS13 antigen levels were interpolated from the NHP reference.
ADAMTS13 conformation ELISA
ADAMTS13 conformation in plasma samples, conducted in Kortrijk, was determined using an in-house developed conformation ELISA as previously described.23,24 In brief, 96-well plates were coated with the murine mAb 1C4 (5 μg/mL) which recognized a cryptic epitope in the spacer domain. After blocking, plasma samples were added in a 1 over 4 starting dilution and further diluted in a 1 over 2 dilution series. A dilution series of NHP, preincubated with the opening murine mAb 17G2,46,47 was used for calibration. Detection of bound ADAMTS13 using biotinylated 3H945 followed by HRP-labeled streptavidin and colorimetric reaction allowed assaying open ADAMTS13 and calculating CI. A minimum of ≥0.02 μg/mL ADAMTS13:Ag is needed for CI assay. A CI of >0.5 indicates an open ADAMTS13 conformation whereas a CI of ≤0.5 indicates a closed ADAMTS13 conformation.
ADAMTS13:act, ADAMTS13:Ag, and CI of some iTTP samples had been analyzed for a previous study and were already published in this context.24
VWF MM ratio
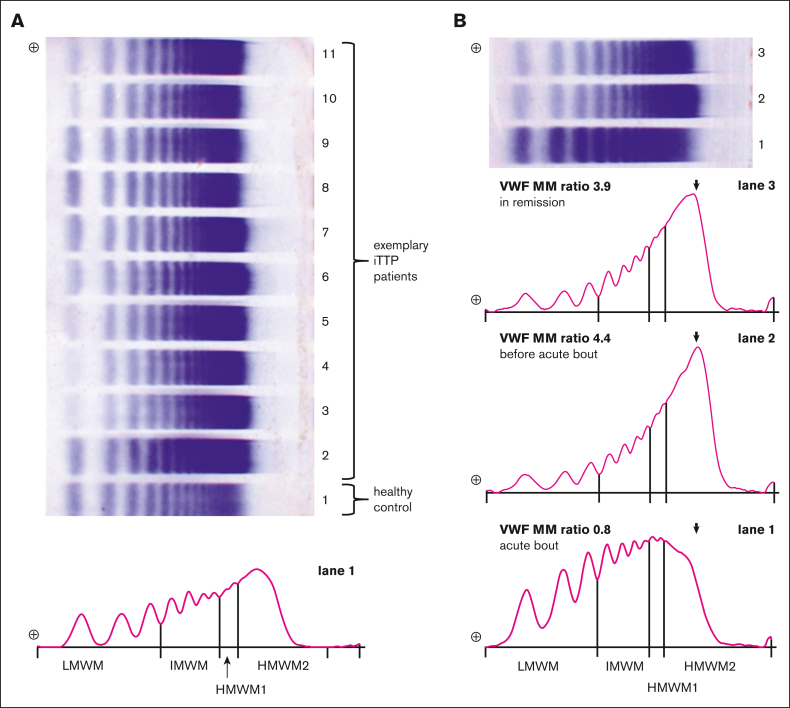
VWF MM analysis was performed in Mainz using the Hydragel 11 von Willebrand Multimers kit (Sebia GmbH, Fulda, Germany) on the Sebia Hydrasis 2 system (Figure 2A). Plasma samples were thawed at room temperature, diluted with sample diluent (Sebia), incubated at 45°C for 20 minutes, adjusted to room temperature for a maximum of 10 minutes and loaded onto a precast agarose gel (sample volume 5 μL). To avoid saturated, not quantifiable MM bands, the samples were not only roughly diluted according to VWF:Ag concentration ranges (as suggested by the manufacturer) but were also adjusted exactly to 20% VWF:Ag. On each gel, 1 healthy control and 10 patient samples were separated. Electrophoresis, in-gel immunofixation and VWF staining, scanning of the gel, densitometry (Software Phoresis version 6.3, Sebia), and quantification by integrating the areas under the curves were part of a semiautomated workflow optimized by the manufacturer. Preliminarily, the electrophoretic pattern of VWF MMs was divided into following 3 zones according to the molecular weight: LMWM, 3 bands; IMWM, 4 bands; and HMWM. Because the manufacturer’s classification was not optimized for the use in TTP, we complemented the MM classification by splitting HMWMs in 2 separate categories, the anodal 2 bands (HMWM1) and the residual-HMWM bands (HMWM2) (Figure 2A).
Figure 2.
VWF MM ratio evaluation. (A) Exemplary VWF MM gel with plasma samples from patients with iTTP (lanes 2-11) and from a healthy control (lane 1). The densitometry trace below the stained gel represents lane 1 with its electrophoretic pattern divided in 4 zones according to the molecular weight: LMWM; IMWM; HMWM1; and HMWM2. The VWF MM ratio is defined as HMWM2/ LMWM. (B) Electrophoretic patterns and densitometry traces of 1 patient with iTTP in the course of the disease. Lane 3: in remission; lane 2: before acute bout; lane 1: in the acute bout before first TPE.
Statistical analysis
Clinical symptoms and medical history of each patient were recorded in Open Clinica. Laboratory parameters and biobanking were recorded in Nexus/Swisslab (version 2.22.5.00). Statistical analysis was performed using GraphPad Prism 9. The descriptive statistics included frequency, mean, standard deviation, median, interquartile range, and minimum and maximum. The differences between 2 groups were tested using Student t test for normally distributed data and the nonparametric Mann-Whitney U test for nonnormally distributed data. Any P values <.05 were considered to be statistically significant.
Results
Characteristics of the enrolled patients with iTTP
Eighty-three patients with confirmed iTTP were included (Table 1). The majority of 61 (73%) were female. Patients were followed for a median of 468 days and were aged 49 years (median) at study inclusion. The patients were first diagnosed with iTTP at a median age of 38 years (range 12-85 years). The median number of previous acute episodes before inclusion in the study was 2. Four patients were enrolled during their initial iTTP episode, 2 of them directly admitted to the University Medical Center Mainz and 2 transferred from external hospitals. Five (7%) patients had already had ≥10 acute prior episodes.
Table 1.
Characteristics of the cohort of patient with iTTP
| Characteristics | n | % |
|---|---|---|
| Total number of patients with iTTP | 83∗ | |
| Sex | ||
| Female | 61 | 73 |
| Male | 22 | 27 |
| Ethnicity | ||
| Caucasian | 83 | 100 |
| Observation time, d | ||
| Median (minimum, 25th percentile, 75th percentile, maximum) | 468 (1, 56, 680, 782) | |
| Age at time of enrollment, y | ||
| Median (minimum, 25th percentile, 75th percentile, maximum) | 49 (20, 39, 57, 86) | |
| Age at time of diagnosis of first acute iTTP episode, years† | ||
| Median (minimum, 25th percentile, 75th percentile, maximum) | 38 (12, 27, 49, 85) | |
| Number of acute TTP episodes during study | 22 in 16 patients | |
| Patients enrolled during acute iTTP | 8 | |
| Initial diagnosis during study | 4 | |
| Relapse of iTTP | 4 | |
| Relapses during follow-up after enrollment | 14 | |
| Number of patients with iTTP in continued remission during study | 67 | |
| Number of all acute episodes per patient before enrollment into the study‡ | ||
| Median (minimum, 25th percentile, 75th percentile, maximum) | 2 (0, 1, 3, 23) | |
| Risk factors for iTTP | ||
| Smoking | 17 | 20 |
| Overweight (BMI, 27-29.9)§ | 12 | 16 |
| Obesity (BMI >30)§ | 26 | 34 |
| Arterial hypertension | 28 | 31 |
| Type 1 diabetes mellitus | 1 | 1 |
| Type 2 diabetes mellitus | 11 | 13 |
BMI, body mass index.
Ninety-one patients were screened (refer to supplemental Figure 1).
Known for 80 patients with iTTP.
Known for 75 patients with iTTP.
Known for 76 patients with iTTP.
Data on the acute iTTP episodes
Of the 22 acute episodes recorded in 16 patients during the study period, complete clinical and laboratory data and biobanking of plasma samples before TPE were available for 16 episodes in 10 patients (Figure 1B-C). All 16 well-documented acute episodes were characterized by severely decreased ADAMTS13 activity, thrombocytopenia, increased LDH, and signs of microangiopathic hemolysis (Table 2). The severity of the acute bouts assessed by our clinical score48 was mild in 5, moderate in 8, and severe in 2 instances, and 1 patient with 3 previous acute episodes showed only laboratory signs of acute TTP (Table 2; supplemental Table 1). For all 16 acute iTTP episodes, from 4 to 29 TPEs were performed over 8 to 36 days, most patients received prednisolone and 5 rituximab (supplemental Table 1). All patients survived. Comorbidities besides iTTP are listed in supplemental Table 2.
Table 2.
Laboratory parameters of 16 well-documented acute iTTP episodes in 10 patients
| Laboratory parameters at onset of the acute iTTP episode | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pat.ID | Sex | Severity of the acute episode (clinical score)∗ | Platelets [cells/nL] 150-360 |
Hemoglobin [g/dL] m 13.5-17.5 f 12.0-16.0 |
Schistocytes [%] <5% |
Haptoglobin [g/L] m 0.14-2.68 f 0.11-2.73 |
LDH [U/L] <245 |
VWF antigen [%] 42-176 |
VWF activity [%] 40-170 |
VWF MM ratio 1.1-3.5 |
ADAMTS13 activity [%] >50 |
ADAMTS13 antigen [μg/mL] >0.5 |
ADAMST13 CI <0.5 |
ADAMTS13 inhibitor [BU/mL] <0.5 |
IL-6 [pg/mL] <7 |
TNI [pg/mL] <24 |
| 11 | F | Moderate (2) | 97 | 11.1 | 10 | 0.09 | 307 | 242 | 336 | 3.1 | 1.4 | 0.24 | 7.57 | 0.3 | <2 | 2.6 |
| 11 | F | Moderate (2) | 54 | 7.2 | 17 | <0.08 | 609 | 216 | 373 | 3.1 | 2.6 | 0.25 | 0.48 | 0.8 | 3 | 252.6 |
| 11 | F | Moderate (2) | 65 | 9 | 5 | 0.82 | 444 | 228 | >390 | 2.6 | 5.7 | 0.22 | 0.49 | 0 | 3 | 85.9 |
| 15 | F | Laboratory abnormalities only (0) | 17 | 11.7 | 3 | <0.08 | 506 | 214 | 199 | 2.6 | <1.0 | 0.07 | 8.49 | 1.0 | 3.53 | <1.95 |
| 32 | M | Moderate (2) | 20 | 10.8 | 15 | <0.08 | 527 | 226 | 215 | 2.2 | <1.0 | 0.60 | 1.06 | 0.6 | 2 | 1.8 |
| 32 | M | Moderate (2) | 60 | 12.2 | 4 | <0.08 | 505 | 227 | 283 | 3.2 | <1.0 | 0.09 | 13.45 | 1.3 | <2 | 9.4 |
| 44 | M | Moderate (2) | 88 | 9.9 | 14 | <0.08 | 612 | 216 | 159 | 3.1 | <1.0 | 0.20 | 3.9 | 2.6 | 3 | 133.6 |
| 45 | F | Mild (1) | 30 | 9.6 | 17 | <0.08 | 413 | 106 | 70 | 0.7 | 1.6 | 0.08 | 0.33 | 0.9 | <2 | 15.7 |
| 45 | F | Moderate (2) | 11 | 10.3 | 20 | <0.08 | 697 | 162 | 130 | 0.9 | <1.0 | 0.08 | 0.39 | 2.6 | 3 | 4.4 |
| 63 | F | Mild (1) | 29 | 10.4 | 17 | <0.08 | 488 | 68 | 43 | 0.4 | <1.0 | 0.06 | 9.56 | 0.7 | 3 | 1.8 |
| 63 | F | Mild (1) | 39 | 11.0 | 4 | <0.08 | 297 | 78 | 69 | 2.8 | 4.8 | 0.17 | 5.13 | 1.4 | <2 | 1.6 |
| 64 | F | Mild (1) | 49 | 10.2 | 11 | <0.08 | 560 | 243 | 235 | 1.8 | 2.2 | 0.11 | 4.32 | 0.6 | 44 | 53.9 |
| 79 | F | Moderate (2) | 17 | 7.4 | 38 | not done | 749 | 177 | 149 | 0.5 | <1.0 | 0.37 | 1.51 | 1.8 | 9 | 180.6 |
| 79 | F | Mild (1) | 11 | 7.8 | 31 | <0.08 | 634 | 99 | 74 | 1.4 | 1.3 | 0.08 | 1.36 | 1.7 | 3 | 13.9 |
| 85 | F | Severe (3) | 6 | 6.9 | 23 | <0.08 | 1678 | 261 | not done | 1.1 | <1.0 | 0.05 | 4.03 | 1.2 | 14 | 2236.3 |
| 86 | M | Severe (3) | 8 | 10.1 | 15 | <0.08 | 1165 | 230 | 122 | 0.6 | <1.0 | 0.03 | 3.95 | 2.6 | 24 | 13.2 |
BU, Bethesda Units; F, female; LDH, lactate dehydrogenase; M, male; Pat.ID, patient identification; TNI, troponin I.
Clinical severity score for acute iTTP episodes.48
Follow-up of all patients with iTTP and development of the VWF MM ratio
We monitored all 83 patients with iTTP (Figure 1A) for clinical signs and symptoms, blood values, ADAMTS13 parameters, LDH and VWF MM pattern over the study period up to 2 years. An example for 1 closely followed patient is shown in supplemental Figure 1. VWF MM pattern turned out as potentially interesting parameter (see below).
Set up and evaluation of a new VWF MM ratio
To define an informative VWF MM fraction including predominantly ultra-large MMs, the HMWM fraction was split in 2 zones, the anodal 2 bands (HMWM1), which could be clearly differentiated in all lanes, and the remaining HMWM2 (Figure 2A). After analyzing the 65 control samples and the first 77 samples of patients with TTP and quantifying the predefined fractions, the preliminary evaluation revealed that, among all fractions, HMWM2 and LMWM differed most pronouncedly between patients with iTTP and controls, expressed by increased HMWM2 and decreased LMWM in TTP. IMWM were slightly decreased in patients with iTTP and no difference was observed for HMWM1. Therefore, the ratio of HMWM2 to LMWM (VWF MM ratio) was considered as the most discriminative parameter (Figure 2B).
Set up and coefficient of variation (CV) of VWF MM ratio
On 38 gels, each with 11 slots, 1 aliquot of a total of 4 individual healthy control samples was analyzed in parallel with sample of 10 patients, respectively. For healthy control #1, a VWF MM ratio of 1.7 was found with a CV of 15% (n = 26 gels). This was confirmed with healthy controls #2 to 4 with VWF MM ratio 1.9, CV 19% (n = 6), VWF MM ratio 1.3, CV 15% (n = 3), and VWF MM ratio 1.3, CV 14% (n = 3), respectively. Furthermore, 20 samples of patients with iTTP were analyzed and repeated at another day: The relative deviation of the recorded duplicates (calculated as |d| × 100/m; d: absolute value of the duplicates’ difference, m: mean of the duplicates) was found to be 9.12% ± 7.03% (mean ± standard deviation).
Set up and sample stability to freeze-thaw cycles
One gel was loaded with 5 technical replicate samples of each, 1 healthy control, and 1 patient with TTP. Replicates had been subjected to 1 to 5 freeze-thaw cycles. A tendency neither toward higher nor toward lower VWF MM ratios was observed (healthy control: VWF MM ratio with increasing freeze-thaw cycles: 1.8, 2.4, 1.9, 1.8, 1.7, CV 14%; patient with TTP: VWF MM ratio with increasing freeze-thaw cycles: 4.9, 4.7, 5.0, 4.9, 4.1, CV 8%).
Set up and patient controls and healthy controls
Forty pseudonymized patient controls and 25 anonymized healthy controls were analyzed. To ensure optimal predilution of the samples for the VWF MM gels, VWF:Ag was determined in all controls (patient controls: mean ± standard deviation 156% ± 55%; minimum 77%, maximum 275%; healthy controls: mean ± standard deviation 108% ± 32%; minimum 59%, maximum 170%). The VWF MM ratio values were normally distributed for both collectives. In patient controls a mean ratio of 2.3 ± 0.6 (SD) was detected, in healthy controls 2.3 ± 0.7. Because results were very similar in both control groups, the reference range for the VWF MM ratio was calculated from a total of 65 controls: 1.1 to 3.5 (2.5th-97.5th percentile).
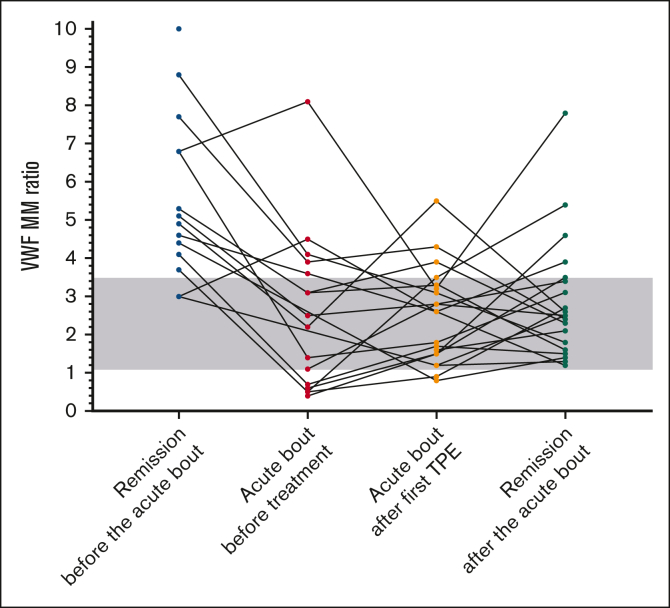
Course of VWF MM ratio in patients with iTTP with and without acute episodes
The VWF MM ratio typically increased before the acute iTTP bouts and dropped at onset of the acute episode (Figure 3). The values of VWF MM ratio before acute episodes were significantly higher than in controls (P < .0001), but also compared to patient with iTTP who did not experience an acute bout (Figure 4). At the onset of an acute episode, the VWF MM ratio dropped significantly (P = .0003) to values often below the lower limit (<1.1). In contrast, both patient with iTTP in continuing remission and healthy controls showed a constant VWF MM ratio (supplemental Figure 2). Toward remission (median 58 days after last TPE), the VWF MM ratio values normalized and exhibited no difference to the control group (Figures 3 and 4).
Figure 3.
VWF MM ratio before, during and after acute iTTP episodes. VWF MM ratios in patients with iTTP from 2 days to 28 weeks (median 39 days) before an acute bout (n = 14), at the onset of the acute iTTP episode (n = 16), after first TPE (n = 20), and in remission after the acute episode (n = 20). Gray background is the normal range of the VWF MM ratio assessed in controls.
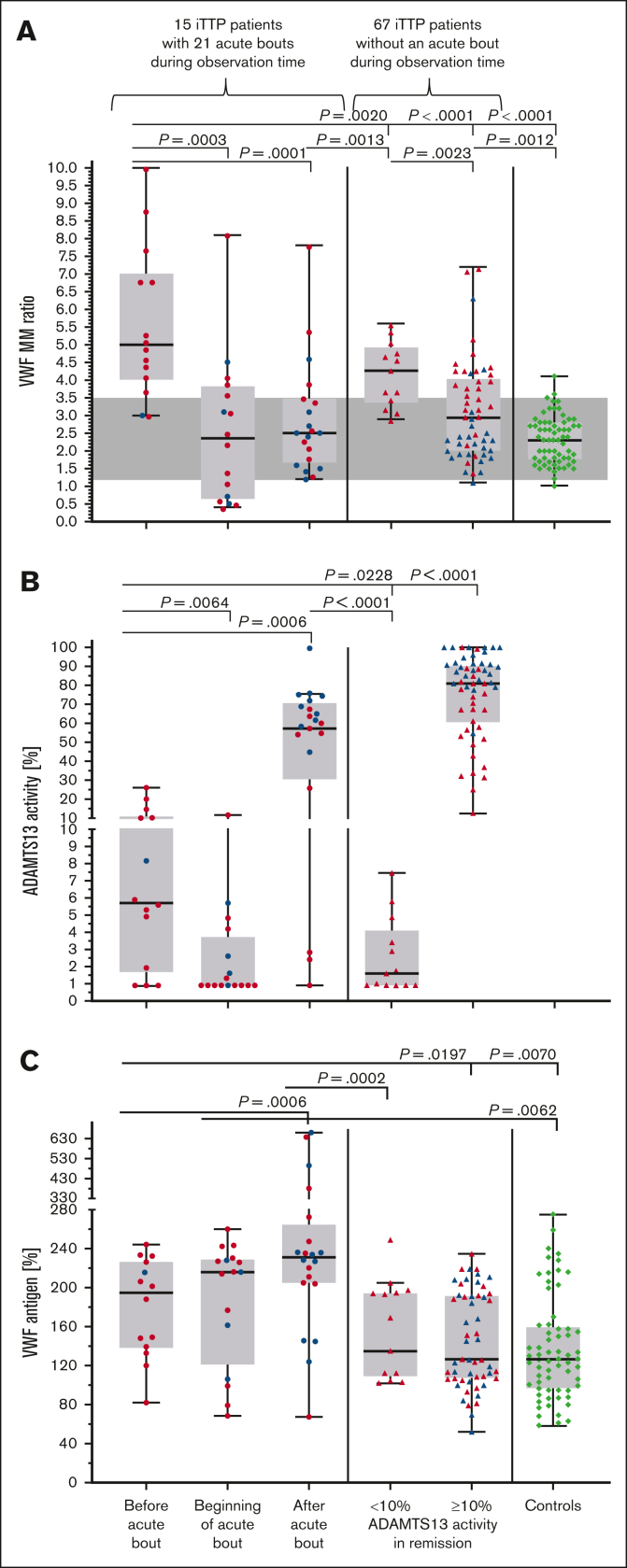
Figure 4.
VWF MM ratio, VWF antigen, ADAMTS13 activity, and ADAMTS13 CI in patients with iTTP. The VWF MM ratio (A), ADAMTS13 activity (B) and VWF antigen (C) in 82 patients with iTTP with and without acute episodes during the study period, as well as in 65 controls. On the left side of panels A, B, and C, the VWF MM ratio, ADAMTS13:act, and VWF:Ag values are shown before (n = 14), at the beginning (n = 16) as well as in remission after the acute episode (n = 20). On the middle panel, patients with iTTP who were constantly in remission are grouped according to ADAMTS13 values <10% (n = 13) and ≥10% (n = 54). An open ADAMTS13 conformation is marked with red symbols, and a closed one is marked with blue symbols in panels A-C. Controls are shown on the right side of panels A and C. Gray background is the normal range of the VWF MM ratio assessed in controls.
Comparison of VWF MM ratio, VWF antigen, ADAMTS13 activity, and ADAMTS13 CI in patient with iTTP with and without an acute episode during the study period
To detect potential differences between patients with and without acute episodes, the patients were divided into following 2 groups: those with (n = 15) and without (n = 67) acute episodes during the study period. The 67 patients remaining in remission for the complete study period were further divided into those with ADAMTS13:act ≥10% (n = 54) and <10% (n = 13). In addition, 65 healthy and patient controls were also analyzed for comparison (Figure 4).
VWF MM ratio was assessed in remission before an acute episode in 14 instances (10 different patients), at onset of acute iTTP bout in 16 instances (10 patients), and during remission after an acute iTTP in 20 instances (14 patients) (Figures 1C and 4). Patients in continuing remission with ADAMTS13:act ≥10% had a significantly lower VWF MM ratio than those with ADAMTS13:act <10% (P = .0023). Nevertheless, patients with ADAMTS13:act below (P < .0001) as well as above 10% (P = .0012) showed significantly higher VWF MM ratio than controls. Fourteen samples obtained 39 days (median; min. 2, interquartile range 13-50, max. 196 days) before acute iTTP (ADAMTS13 <10% in 9, 10%-26% in 5) showed significantly higher VWF MM ratios than those of 13 patients in continuing remission with ADAMTS13 <10% (P = .0020), as well as those of the 54 patients in remission with ≥10% (P < .0001). Sixteen samples of patients with acute iTTP displayed significantly lower VWF MM ratios than the 13 patients with iTTP in remission with an ADAMTS13 <10% (P = .0033). The VWF MM ratio in patients with iTTP in remission after an acute bout was comparable to that of controls and lower than in patients with iTTP in continuing remission.
Bernardo et al20 demonstrated that inflammatory cytokines stimulate the release of HMW VWF MM from human umbilical vein endothelial cells and that interleukin 6 (IL-6) inhibits their cleavage under flow conditions. Therefore, we examined C-reactive protein (CRP) and IL-6. CRP levels in patients before an acute bout were equal or lower than in patients in continuing remission (supplemental Figure 3). IL-6 levels were not detectable before an acute episode and were significantly higher in patients with iTTP in remission (P = .0124 and P = .0162), although still within the normal range (<7 pg/mL) (supplemental Figure 3). At the beginning of an acute bout, CRP and IL-6 were significantly higher than at all other time points and compared with that of patients with iTTP patients in remission. Thus, no correlation between these inflammatory parameters (CRP and IL-6) and high VWF MM ratio was established. The VWF antigen levels in patients were higher before, at onset, and after the acute episode than patients in remission and controls (Figure 4C). As previously reported,24 in patients in continuing remission over up to 2 years, all 13 patients with an ADAMTS13 activity <10% showed an open ADAMTS13 conformation. In those in continuing remission with ADAMTS13 activity >10%, the conformation was open in 50%. It appeared that the higher the ADAMTS13 activity the more likely it is that ADAMTS13 has a closed conformation (Figure 4B). In 13 of 14 (93%) samples obtained before an acute episode, an open ADAMTS13 conformation was evident. At the beginning of the acute bout, 12 of 16 (75%) cases showed an open ADAMTS13 conformation whereas in remission, after the acute iTTP, only 50% of cases still had an open ADAMTS13 conformation (Figure 4B). Interestingly, the lower the VWF MM ratio and the higher ADAMTS13 activity, the more likely it is that the ADAMTS13 conformation is closed (Figure 4A-B).
Discussion
The goal of this prospective single center cohort study on patients with iTTP recruited and followed at the University Medical Center in Mainz between July 2016 and August 2018 was to identify markers associated with the disease course. Patients were enrolled during hospitalization for acute iTTP episodes or as outpatients followed in remission at ∼3-month intervals. Clinical and laboratory data were documented, and biobanking of plasma samples was performed. Caplacizumab, nowadays recommended14,49,50 and used at many specialized centers in parallel with TPE and corticosteroids during hospitalization for acute iTTP,17,51, 52, 53 was not yet available during the study period. Rituximab, now recommended both upfront in acute iTTP episodes as well as preemptively in clinical remission when ADAMTS13 activity drops below 10% to 20%,12,14,50,54,55 was not yet uniformly used in this cohort. Rituximab was given to 5 patients who were frequently relapsing during an acute iTTP episode and only to 1 patient in clinical remission with a severely deficient ADAMTS13 activity.
Persistent or recurrent deficiency of ADAMTS13 activity during follow-up of survivors of acute iTTP is an established risk factor for disease recurrence.18,56 However, 13 of the 83 included patients in our cohort remained in clinical remission for up to 2 years despite severely deficient ADAMTS13 activity of <10%. Open ADAMTS13 conformation, that is a CI of >0.5, a specific hallmark of iTTP23 was recently shown to be caused by autoantibodies binding to ADAMTS13.24 Also, long-term follow-up of 1 patients with iTTP suggested that open ADAMTS13 conformation might precede ADAMTS13 activity decrease24 and thus may be a potential early indicator of impending iTTP relapse. Interestingly, 13 of 14 patients, from 2 days to 28 weeks before an acute clinical relapse showed a CI >0.5, nevertheless all 13 patients with ADAMTS13 <10% and half of those with ADAMTS13 ≥10% remaining in clinical remission during the entire study period had an open ADAMTS13 conformation as well. However, our study did not focus on the comparative predictive value of ADAMTS13 activity, CI, and the VWF MM ratio because of limited number of patients and short follow-up. The ADAMTS13 CI is currently being tested as predictive marker for biological or clinical relapse in a multicenter cohort of patients in remission and normal ADAMTS13 activity (de Waele, Sakai et al manuscript in preparation).
Based on the fact that the hyperadhesive, ultra-large VWF directly mediates microvascular platelet adhesion and aggregation and clinical and laboratory signs of acute TTP in animal models,25,57 in this study we focused on the plasmatic VWF MMs of our patients with iTTP. Although standardization of VWF MM analysis seems to be still challenging,31 the commercially available Hydragel 11 VWF MM kit represents a reproducible assay to analyze the VWF MM distribution. Using constant amounts of VWF for electrophoresis samples, preliminary testing of a series of iTTP and control samples allowed to quantitate high-, intermediate- and low-molecular weight VWF MMs, with the high molecular weight VWF MMs split in a HMWM1 and a HMWM2 fraction. The densitometrically assessed ratio of HMWM2 to LMWM was reproducibly quantified and differed between normal and iTTP plasma samples and between different disease states in patients with iTTP.
First, the VWF MM ratio differentiated patients with iTTP in remission with <10% ADAMTS13 activity from those with ≥10%. Moreover, at the onset of acute iTTP before the first TPE, the VWF MM ratio decreased, often to subnormal values which may be explained by consumption of predominantly large and ultra-large VWF MMs during the acute microvascular thrombotic process.29,30 The most interesting finding was that plasma samples obtained a few days to several weeks before acute disease relapse showed significantly higher VWF MM ratios than to those from patients remaining in continuous remission. The reason for this unexpected finding of very high VWF MM ratios despite measurable ADAMTS13 activity (10%-26% of normal) in 5 of 14 cases, remains elusive. IL-6 has been reported to inhibit VWF cleavage by ADAMTS13 under flow conditions.20 IL-6 and CRP levels were not elevated in samples before acute iTTP relapse and could not explain this phenomenon. However, our data suggest that VWF proteolytic processing may be impaired in distinct patients with iTTP even in the presence of measurable ADAMTS13 activity and that those patients may be at high risk of experiencing a clinical iTTP relapse.
Our study is relatively small with limited numbers of patients developing a clinical relapse, and the follow-up time with maximally 26 months was rather short. However, the hypothesis is raised that VWF MM distribution, in addition to decreased ADAMTS13 activity and open ADAMTS13 conformation, may be an important marker heralding acute disease manifestation in patients with iTTP. A large, prospective, probably multicenter study with regular follow-up of patients with iTTP over several years should be undertaken to verify the prognostic role of the VWF MM ratio and to hopefully clarify its pathophysiology.
Conflict-of-interest disclosure: B.L. is chairman of the data safety monitoring committees for the Baxalta 281102 and TAK-755-3002 studies (both investigating recombinant ADAMTS13 in hereditary TTP) and for the Takeda SHP655-201 study (recombinant ADAMTS13 in immune-mediated TTP), all 3 now run by Takeda. B.L. was a member of the advisory board of Ablynx, now part of Sanofi, for the development of caplacizumab; is chairman of the data monitoring committee of the Mayari study, run by Sanofi, on iTTP patients; and received congress travel support and/or lecture fees from Baxter, Ablynx, Alexion, Siemens, Bayer, Roche, and Sanofi. The remaining authors declare no competing financial interests.
Acknowledgments
The authors thank Sebia for kindly providing the reagents for VWF multimer ratio method establishment and validation. This study (BMBF 01EO1503) was supported by the Federal Ministry of Education and Research, Germany.
Authorship
Contribution: T.F. developed study concept, analyzed and compiled data, and wrote and approved the manuscript; H.R. developed study concept and design, was responsible for assay evaluation, and wrote and approved the manuscript; L.d.W. and C.D. performed data acquisition and analysis (ADAMTS13 conformation and antigen), and revised and approved the manuscript; C.v.A. developed study concept and carried out approval and enrollment of the patients; N.M.-C. performed graphical representation and analysis and revised and approved the manuscript; F.H. performed data acquisition (ADAMTS13 activity) and revised and approved the manuscript; A.D. performed data acquisition (VWF multimer gels) and approved the study; D.M. performed blood sampling for biobanking, clinical data acquisition, and revised and approved the manuscript; X.M. performed clinical data acquisition and approved the study; M.S. performed clinical data acquisition and revised and approved the manuscript; K.J.L. provided statistical advice and revised and approved the manuscript; K.J. performed data acquisition and analysis, and revised and approved the manuscript; K.V. developed study concept, performed data analysis and acquisition, and revised and approved the manuscript; and B.L. developed study concept and design, performed data analysis, and wrote and approved the manuscript.
Footnotes
∗T.F and H.R. are joint first authors.
Data are available on request from the corresponding author, Tanja Falter (tanja.falter@unimedizin-mainz.de).
The full-text version of this article contains a data supplement.
Supplementary Material
References
- 1.Furlan M, Robles R, Galbusera M, et al. von Willebrand factor-cleaving protease in thrombotic thrombocytopenic purpura and the hemolytic-uremic syndrome. N Engl J Med. 1998;339(22):1578–1584. doi: 10.1056/NEJM199811263392202. [DOI] [PubMed] [Google Scholar]
- 2.Tsai HM, Lian EC. Antibodies to von Willebrand factor-cleaving protease in acute thrombotic thrombocytopenic purpura. N Engl J Med. 1998;339(22):1585–1594. doi: 10.1056/NEJM199811263392203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Veyradier A, Obert B, Houllier A, Meyer D, Girma JP. Specific von Willebrand factor-cleaving protease in thrombotic microangiopathies: a study of 111 cases. Blood. 2001;98(6):1765–1772. doi: 10.1182/blood.v98.6.1765. [DOI] [PubMed] [Google Scholar]
- 4.Moake JL, Turner NA, Stathopoulos NA, Nolasco LH, Hellums JD. Involvement of large plasma von Willebrand factor (vWF) multimers and unusually large vWF forms derived from endothelial cells in shear stress-induced platelet aggregation. J Clin Invest. 1986;78(6):1456–1461. doi: 10.1172/JCI112736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Dong JF, Moake JL, Nolasco L, et al. ADAMTS-13 rapidly cleaves newly secreted ultralarge von Willebrand factor multimers on the endothelial surface under flowing conditions. Blood. 2002;100(12):4033–4039. doi: 10.1182/blood-2002-05-1401. [DOI] [PubMed] [Google Scholar]
- 6.Kremer Hovinga JA, Coppo P, Lammle B, Moake JL, Miyata T, Vanhoorelbeke K. Thrombotic thrombocytopenic purpura. Nat Rev Dis Primers. 2017;3:17020. doi: 10.1038/nrdp.2017.20. [DOI] [PubMed] [Google Scholar]
- 7.Hellmann M, Hallek M, Scharrer I. [Thrombotic-thrombocytopenic purpura] Internist (Berl) 2010;51(9):1136. doi: 10.1007/s00108-010-2599-0. 1138-1144. [DOI] [PubMed] [Google Scholar]
- 8.Shaw RJ, Dutt T. Mind and matter: the neurological complications of thrombotic thrombocytopenic purpura. Br J Haematol. 2022;197(5):529–538. doi: 10.1111/bjh.18127. [DOI] [PubMed] [Google Scholar]
- 9.Rock GA, Shumak KH, Buskard NA, et al. Comparison of plasma exchange with plasma infusion in the treatment of thrombotic thrombocytopenic purpura. Canadian Apheresis Study Group. N Engl J Med. 1991;325(6):393–397. doi: 10.1056/NEJM199108083250604. [DOI] [PubMed] [Google Scholar]
- 10.Bell WR, Braine HG, Ness PM, Kickler TS. Improved survival in thrombotic thrombocytopenic purpura-hemolytic uremic syndrome. Clinical experience in 108 patients. N Engl J Med. 1991;325(6):398–403. doi: 10.1056/NEJM199108083250605. [DOI] [PubMed] [Google Scholar]
- 11.Scully M, McDonald V, Cavenagh J, et al. A phase 2 study of the safety and efficacy of rituximab with plasma exchange in acute acquired thrombotic thrombocytopenic purpura. Blood. 2011;118(7):1746–1753. doi: 10.1182/blood-2011-03-341131. [DOI] [PubMed] [Google Scholar]
- 12.Owattanapanich W, Wongprasert C, Rotchanapanya W, Owattanapanich N, Ruchutrakool T. Comparison of the long-term remission of rituximab and conventional treatment for acquired thrombotic thrombocytopenic purpura: a systematic review and meta-analysis. Clin Appl Thromb Hemost. 2019;25 doi: 10.1177/1076029618825309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Froissart A, Buffet M, Veyradier A, et al. Efficacy and safety of first-line rituximab in severe, acquired thrombotic thrombocytopenic purpura with a suboptimal response to plasma exchange. Experience of the French Thrombotic Microangiopathies Reference Center. Crit Care Med. 2012;40(1):104–111. doi: 10.1097/CCM.0b013e31822e9d66. [DOI] [PubMed] [Google Scholar]
- 14.Zheng XL, Vesely SK, Cataland SR, et al. ISTH guidelines for treatment of thrombotic thrombocytopenic purpura. J Thromb Haemost. 2020;18(10):2496–2502. doi: 10.1111/jth.15010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Scully M, Cataland SR, Peyvandi F, et al. Caplacizumab treatment for acquired thrombotic thrombocytopenic purpura. N Engl J Med. 2019;380(4):335–346. doi: 10.1056/NEJMoa1806311. [DOI] [PubMed] [Google Scholar]
- 16.Knoebl P, Cataland S, Peyvandi F, et al. Efficacy and safety of open-label caplacizumab in patients with exacerbations of acquired thrombotic thrombocytopenic purpura in the HERCULES study. J Thromb Haemost. 2020;18(2):479–484. doi: 10.1111/jth.14679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dutt T, Shaw RJ, Stubbs M, et al. Real-world experience with caplacizumab in the management of acute TTP. Blood. 2021;137(13):1731–1740. doi: 10.1182/blood.2020007599. [DOI] [PubMed] [Google Scholar]
- 18.Peyvandi F, Lavoretano S, Palla R, et al. ADAMTS13 and anti-ADAMTS13 antibodies as markers for recurrence of acquired thrombotic thrombocytopenic purpura during remission. Haematologica. 2008;93(2):232–239. doi: 10.3324/haematol.11739. [DOI] [PubMed] [Google Scholar]
- 19.Kremer Hovinga JA, Vesely SK, Terrell DR, Lammle B, George JN. Survival and relapse in patients with thrombotic thrombocytopenic purpura. Blood. 2010;115(8):1500–1511. doi: 10.1182/blood-2009-09-243790. quiz 1662. [DOI] [PubMed] [Google Scholar]
- 20.Bernardo A, Ball C, Nolasco L, Moake JF, Dong JF. Effects of inflammatory cytokines on the release and cleavage of the endothelial cell-derived ultralarge von Willebrand factor multimers under flow. Blood. 2004;104(1):100–106. doi: 10.1182/blood-2004-01-0107. [DOI] [PubMed] [Google Scholar]
- 21.Fuchs TA, Kremer Hovinga JA, Schatzberg D, Wagner DD, Lammle B. Circulating DNA and myeloperoxidase indicate disease activity in patients with thrombotic microangiopathies. Blood. 2012;120(6):1157–1164. doi: 10.1182/blood-2012-02-412197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cao W, Pham HP, Williams LA, et al. Human neutrophil peptides and complement factor Bb in pathogenesis of acquired thrombotic thrombocytopenic purpura. Haematologica. 2016;101(11):1319–1326. doi: 10.3324/haematol.2016.149021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Roose E, Schelpe AS, Joly BS, et al. An open conformation of ADAMTS-13 is a hallmark of acute acquired thrombotic thrombocytopenic purpura. J Thromb Haemost. 2018;16(2):378–388. doi: 10.1111/jth.13922. [DOI] [PubMed] [Google Scholar]
- 24.Roose E, Schelpe AS, Tellier E, et al. Open ADAMTS13, induced by antibodies, is a biomarker for subclinical immune-mediated thrombotic thrombocytopenic purpura. Blood. 2020;136(3):353–361. doi: 10.1182/blood.2019004221. [DOI] [PubMed] [Google Scholar]
- 25.Chauhan AK, Walsh MT, Zhu G, Ginsburg D, Wagner DD, Motto DG. The combined roles of ADAMTS13 and VWF in murine models of TTP, endotoxemia, and thrombosis. Blood. 2008;111(7):3452–3457. doi: 10.1182/blood-2007-08-108571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sadler JE, Moake JL, Miyata T, George JN. Recent advances in thrombotic thrombocytopenic purpura. Hematology Am Soc Hematol Educ Program. 2004;2004(1):407–423. doi: 10.1182/asheducation-2004.1.407. [DOI] [PubMed] [Google Scholar]
- 27.Turecek PL, Peck RC, Rangarajan S, et al. Recombinant ADAMTS13 reduces abnormally up-regulated von Willebrand factor in plasma from patients with severe COVID-19. Thromb Res. 2021;201:100–112. doi: 10.1016/j.thromres.2021.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Favaloro EJ, Lippi G. Post-analytical issues in hemostasis and thrombosis testing. Methods Mol Biol. 2017;1646:545–559. doi: 10.1007/978-1-4939-7196-1_40. [DOI] [PubMed] [Google Scholar]
- 29.Moake JL, Rudy CK, Troll JH, et al. Unusually large plasma factor VIII: von Willebrand factor multimers in chronic relapsing thrombotic thrombocytopenic purpura. N Engl J Med. 1982;307(23):1432–1435. doi: 10.1056/NEJM198212023072306. [DOI] [PubMed] [Google Scholar]
- 30.Furlan M, Robles R, Solenthaler M, Lammle B. Acquired deficiency of von Willebrand factor-cleaving protease in a patient with thrombotic thrombocytopenic purpura. Blood. 1998;91(8):2839–2846. [PubMed] [Google Scholar]
- 31.Studt JD, Budde U, Schneppenheim R, et al. Quantification and facilitated comparison of von Willebrand factor multimer patterns by densitometry. Am J Clin Pathol. 2001;116(4):567–574. doi: 10.1309/75CQ-V7UX-4QX8-WXE7. [DOI] [PubMed] [Google Scholar]
- 32.Oliver S, Vanniasinkam T, Mohammed S, Vong R, Favaloro EJ. Semi-automated von Willebrand factor multimer assay for von Willebrand disease: further validation, benefits and limitations. Int J Lab Hematol. 2019;41(6):762–771. doi: 10.1111/ijlh.13107. [DOI] [PubMed] [Google Scholar]
- 33.Pikta M, Szanto T, Viigimaa M, et al. Evaluation of a new semi-automated Hydragel 11 von Willebrand factor multimers assay kit for routine use. J Med Biochem. 2021;40(2):167–172. doi: 10.5937/jomb0-26008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pikta M, Zemtsovskaja G, Bautista H, et al. Preclinical evaluation of a semi-automated and rapid commercial electrophoresis assay for von Willebrand factor multimers. J Clin Lab Anal. 2018;32(6):e22416. doi: 10.1002/jcla.22416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pikta M, Vasse M, Smock KJ, et al. Establishing reference intervals for von Willebrand factor multimers. J Med Biochem. 2022;41(1):115–121. doi: 10.5937/jomb0-31941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Skornova I, Simurda T, Stasko J, et al. Multimer analysis of von Willebrand factor in von Willebrand disease with a hydrasys semi-automatic analyzer-single-center experience. Diagnostics (Basel) 2021;11(11):2153. doi: 10.3390/diagnostics11112153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bowyer AE, Goodfellow KJ, Seidel H, et al. Evaluation of a semi-automated von Willebrand factor multimer assay, the Hydragel 5 von Willebrand multimer, by two European Centers. Res Pract Thromb Haemost. 2018;2(4):790–799. doi: 10.1002/rth2.12141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Scully M, Hunt BJ, Benjamin S, et al. Guidelines on the diagnosis and management of thrombotic thrombocytopenic purpura and other thrombotic microangiopathies. Br J Haematol. 2012;158(3):323–335. doi: 10.1111/j.1365-2141.2012.09167.x. [DOI] [PubMed] [Google Scholar]
- 39.Cuker A, Cataland SR, Coppo P, et al. Redefining outcomes in immune TTP: an International Working Group Consensus report. Blood. 2021;137(14):1855–1861. doi: 10.1182/blood.2020009150. [DOI] [PubMed] [Google Scholar]
- 40.Bodo I, Eikenboom J, Montgomery R, et al. Platelet-dependent von Willebrand factor activity. Nomenclature and methodology: communication from the SSC of the ISTH. J Thromb Haemost. 2015;13(7):1345–1350. doi: 10.1111/jth.12964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Kokame K, Nobe Y, Kokubo Y, Okayama A, Miyata T. FRETS-VWF73, a first fluorogenic substrate for ADAMTS13 assay. Br J Haematol. 2005;129(1):93–100. doi: 10.1111/j.1365-2141.2005.05420.x. [DOI] [PubMed] [Google Scholar]
- 42.Kremer Hovinga JA, Mottini M, Lammle B. Measurement of ADAMTS-13 activity in plasma by the FRETS-VWF73 assay: comparison with other assay methods. J Thromb Haemost. 2006;4(5):1146–1148. doi: 10.1111/j.1538-7836.2006.01904.x. [DOI] [PubMed] [Google Scholar]
- 43.Froehlich-Zahnd R, George JN, Vesely SK, et al. Evidence for a role of anti-ADAMTS13 autoantibodies despite normal ADAMTS13 activity in recurrent thrombotic thrombocytopenic purpura. Haematologica. 2012;97(2):297–303. doi: 10.3324/haematol.2011.051433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dekimpe C, Roose E, Tersteeg C, et al. Anti-ADAMTS13 autoantibodies in immune-mediated thrombotic thrombocytopenic purpura do not hamper ELISA-based quantification of ADAMTS13 antigen. J Thromb Haemost. 2020;18(4):985–990. doi: 10.1111/jth.14747. [DOI] [PubMed] [Google Scholar]
- 45.Feys HB, Roodt J, Vandeputte N, et al. Thrombotic thrombocytopenic purpura directly linked with ADAMTS13 inhibition in the baboon (Papio ursinus) Blood. 2010;116(12):2005–2010. doi: 10.1182/blood-2010-04-280479. [DOI] [PubMed] [Google Scholar]
- 46.Deforche L, Roose E, Vandenbulcke A, et al. Linker regions and flexibility around the metalloprotease domain account for conformational activation of ADAMTS-13. J Thromb Haemost. 2015;13(11):2063–2075. doi: 10.1111/jth.13149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Schelpe AS, Petri A, Roose E, et al. Antibodies that conformationally activate ADAMTS13 allosterically enhance metalloprotease domain function. Blood Adv. 2020;4(6):1072–1080. doi: 10.1182/bloodadvances.2019001375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Falter T, Herold S, Weyer-Elberich V, et al. Relapse rate in survivors of acute autoimmune thrombotic thrombocytopenic purpura treated with or without rituximab. Thromb Haemost. 2018;118(10):1743–1751. doi: 10.1055/s-0038-1668545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Mazepa MA, Masias C, Chaturvedi S. How targeted therapy disrupts the treatment paradigm for acquired TTP: the risks, benefits, and unknowns. Blood. 2019;134(5):415–420. doi: 10.1182/blood.2019000954. [DOI] [PubMed] [Google Scholar]
- 50.Coppo P, Cuker A, George JN. Thrombotic thrombocytopenic purpura: toward targeted therapy and precision medicine. Res Pract Thromb Haemost. 2019;3(1):26–37. doi: 10.1002/rth2.12160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kuhne L, Kaufeld J, Volker LA, et al. Alternate-day dosing of caplacizumab for immune-mediated thrombotic thrombocytopenic purpura. J Thromb Haemost. 2022;20(4):951–960. doi: 10.1111/jth.15637. [DOI] [PubMed] [Google Scholar]
- 52.Volker LA, Kaufeld J, Miesbach W, et al. Real-world data confirm the effectiveness of caplacizumab in acquired thrombotic thrombocytopenic purpura. Blood Adv. 2020;4(13):3085–3092. doi: 10.1182/bloodadvances.2020001973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Scully M, de la Rubia J, Pavenski K, et al. Long-term follow-up of patients treated with caplacizumab and safety and efficacy of repeat caplacizumab use: Post-HERCULES study. J Thromb Haemost. 2022;20(12):2810–2822. doi: 10.1111/jth.15892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Jestin M, Benhamou Y, Schelpe AS, et al. Preemptive rituximab prevents long-term relapses in immune-mediated thrombotic thrombocytopenic purpura. Blood. 2018;132(20):2143–2153. doi: 10.1182/blood-2018-04-840090. [DOI] [PubMed] [Google Scholar]
- 55.Hie M, Gay J, Galicier L, et al. Preemptive rituximab infusions after remission efficiently prevent relapses in acquired thrombotic thrombocytopenic purpura. Blood. 2014;124(2):204–210. doi: 10.1182/blood-2014-01-550244. [DOI] [PubMed] [Google Scholar]
- 56.Jin M, Casper TC, Cataland SR, et al. Relationship between ADAMTS13 activity in clinical remission and the risk of TTP relapse. Br J Haematol. 2008;141(5):651–658. doi: 10.1111/j.1365-2141.2008.07107.x. [DOI] [PubMed] [Google Scholar]
- 57.Zheng L, Abdelgawwad MS, Zhang D, et al. Histone-induced thrombotic thrombocytopenic purpura in adamts13 (-/-) zebrafish depends on von Willebrand factor. Haematologica. 2020;105(4):1107–1119. doi: 10.3324/haematol.2019.237396. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.