Abstract
Objective
Human papillomavirus (HPV) vaccination rates remain low among adolescent girls across ethnic minority groups that experience high incidences of HPV-related cervical cancer with poor outcomes. This systematic review aimed to synthesize the available evidence on the factors affecting HPV vaccination among ethnic minority adolescent girls.
Methods
Six databases (PubMed, OVID MEDLINE, EMBASE, CINAHL, PsycINFO, and Scopus) were searched from inception to October 17, 2022. Guided by the conceptual model of vaccine hesitancy, the factors affecting HPV vaccine uptake were descriptively synthesized and analyzed using meta-analyses.
Results
This review included 14 studies. The pooled uptake rate of at least one dose of HPV vaccine among ethnic minority adolescent girls was only 38% (95% confidence interval = 0.22, 0.39). At individual level, age of adolescent girls, knowledge of HPV, perceived importance of HPV vaccination, and perceived risk of HPV infection promoted the vaccine uptake. Beliefs in conspiracy theories and lack of trust in the government and HPV vaccine discouraged the utilization. At social and policy levels, health professionals' recommendations, subjective norms, sexuality-related communication, and vaccine policies such as insurance coverage facilitated HPV vaccination. The religious and moral convictions regarding abstinence from sex until marriage negatively influenced the vaccine acceptance.
Conclusions
HPV vaccination among ethnic minority adolescent girls was influenced by multi-level factors that highlighted a combined effort, including culturally sensitive health education programmes, sexuality-related communication skills training, collaboration with religious organizations, debunking conspiracy theories in HPV vaccine, and promoting school-based vaccination programs, to increase the coverage.
Systematic review registration
PROSPERO, CRD42022366805.
Keywords: Adolescent girls, Ethnic minority, Human papillomavirus, Vaccine, Systematic review, Nursing
Introduction
Of the 604,127 cases of cervical cancer diagnosed globally in 2020, approximately 90% were caused by infection with sexually transmitted human papillomavirus (HPV).1 HPV-related cervical cancer disproportionately affects ethnic minorities. In the United States, Laotian, Kampuchean, Vietnamese, and Native Hawaiian and other Pacific Islanders had much higher age-standardized incidence rates of HPV-related cervical cancer (20.7, 15.5, 13.7, and 9.5 per 100,000, respectively) than non-Hispanic White women (7.4 per 100,000).2 In addition, ethnic minorities had higher metastatic cervical cancer rates (13.3% and 8.3%, respectively) and lower 5-year survival rates (68% and 77%, respectively) than the dominant social groups in the US.3 These data suggest that ethnic minorities are in higher need for more effective prevention of cervical cancer.
To prevent infection with cancer-causing HPV, licensed bivalent, quadrivalent, and nonavalent HPV vaccines have been introduced in 125 countries.4 Adolescent girls prior to sexual debut, especially those aged 9–14 years, are the primary target population for HPV vaccination in most of these countries.4 HPV vaccines have high immunogenicity among adolescent girls, which reduces their risks of persistent infection with carcinogenic HPV types and development of cervical intraepithelial neoplasia.5 As an initiative to eliminate cervical cancer, the World Health Organization (WHO) has emphasized that 90% of all adolescent girls by the age of 15 should have received HPV vaccination by 2030.6 To increase HPV vaccine coverage, a one- or two-dose regimen of HPV vaccine in adolescent girls is being recommended by the WHO to replace the three-dose schedule that requires complex follow-ups to complete the vaccination series.4 Other approaches used to increase HPV vaccine uptake among adolescent girls are the inclusion of HPV vaccines in national immunization programs, adoption of school-based immunization programs, and introduction of policies to support adolescent self-consent procedures.7,8
Despite these public health efforts, HPV vaccination rates among adolescent girls across ethnic groups in 2019 remained markedly lower than the goal of 90% vaccination rate set by the WHO (53.2% in Black, 54.8% in American Indian/Alaska Native, and 62.8% in Hispanic adolescent girls).6,9 Only 29% and 45.3% of Black and Hispanic adolescent girls, respectively, in the US had received at least two doses of HPV vaccine before 13 years of age in 2019.9 Ethnic differences in the HPV vaccine uptake rate have also been reported among other ethnic groups, including Latinos in the US, Somalis in the Netherlands, and ethnically diverse samples in the United Kingdom (UK).8,10 For example, although the overall high HPV coverage rates in the UK ranged from 67.8% to 95.3%, adolescent females from Asian and other ethnic backgrounds had a lower uptake rate of 41% and were approximately twice as likely as their White counterparts to have their parents refuse to allow them to receive the vaccine.8,11 Although interventions such as negotiated interviewing have been developed to increase HPV vaccination rates among ethnic minority adolescents, the post-test HPV vaccine initiation and completion rates only ranged from 5.6% to 56% for most of the interventions.12,13 Given the low HPV vaccination rate among ethnic minority adolescents despite the intervention efforts, it is imperative to understand the factors affecting the HPV vaccine uptake to direct future research and practice in alleviating disparities in HPV vaccine utilization among ethnic minority adolescent girls.
Several reviews of ethnic disparities in HPV vaccination have been conducted.10,14,15 They have primarily focused on individual level influencing factors and identified that inadequate knowledge of HPV, unawareness of HPV vaccine,14 lack of recommendations from physicians,10 and cost of the vaccine preclude ethnic minority parents from vaccinating their adolescent daughters.15 The syntheses failed to account for multi-level effects and cultural, social, and political barriers unique to the ethnic minorities.16 In addition, these reviews have mainly included adults and males, focused on specific ethnic groups (eg, Hispanic in the US), and only identified barriers to HPV vaccination among ethnic minorities.10,16 A comprehensive view of both barriers and facilitators to the HPV vaccination among ethnic minority girls across global regions remain unclear. In addition to socio-cultural and policy aspects, spiritual perspectives that are specific to ethnic minorities could also inform the development of multi-level interventions to enhance vaccine uptake. Hence, the current review was conducted to further synthesize evidence for factors associated with HPV vaccination uptake specifically among ethnic minority adolescent girls in a multi-level perspective to inform interventional programs.
The conceptual model of vaccine hesitancy was previously developed to facilitate understanding of the factors contributing to vaccine acceptance and hesitancy among children and adolescents.17,18 This model explains such factors at the individual (knowledge and information, perceived importance of vaccination, risk perception, and trust), social (subjective norms, health professionals' recommendation, and communication and media), policy (public health and vaccination policies), and cultural and religious levels (eg, religious and moral convictions).17 Guided by this conceptual model, our review aims to synthesize the available evidence on the barriers and facilitators to HPV vaccination among ethnic minority adolescent girls. Findings of this review will inform public policy makers on the potential interventions and public health efforts specifically to increase HPV vaccination coverage among ethnic minority adolescents and decrease the burden of HPV-related cervical cancers.
Methods
This systematic review was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement19 and it was registered in the International Prospective Register of Systematic Reviews (CRD42022366805).
Literature search
From inception to October 2022, six databases (PubMed, Ovid MEDLINE, EMBASE, CINAHL, PsycINFO, and Scopus) were searched to systematically identify relevant articles. As shown in Table 1, the key terms related to ‘ethnic minorities’, ‘HPV vaccination’, ‘barriers’, ‘facilitators’, ‘factors’, and ‘uptake’ were used in the search (Table 1). These key terms were used in the search fields for the title and abstract. No restriction was imposed on the publication year.
Table 1.
The search strategy.
| ‘ethnic minorit∗’ or ‘minority group∗’ or ‘ethnic group∗’ or ‘racial group∗’ or ‘racial minorit∗’ |
| AND |
| ‘facilitator∗’ or ‘barrier∗’ or ‘predictor∗’ or ‘factor∗’ or ‘determinant∗’ or ‘motivator∗’ or ‘challenge∗’ ‘associate∗’ or ‘correlate∗’ |
| AND |
| ‘papillomavirus vaccine’ or ‘papilloma virus vaccine’ or ‘HPV vaccination’ or ‘HPV vaccine’ or ‘HPV immunization’ or ‘HPV immunization’ or ‘papillomavirus vaccination’ or ‘Papilloma virus vaccination’ or ‘papillomavirus immunization’ or ‘papilloma virus immunization’ or ‘papillomavirus immunization’ or ‘papilloma virus immunization’ or ‘Gardasil’ |
| AND |
| ‘uptake’ or ‘receipt’ or ‘initiation’ or ‘completion’ or ‘complete’ or ‘initiate’ or ‘receive’ or ‘undergo’ or ‘undertake’ |
Eligibility criteria
Quantitative, qualitative, and mixed-methods studies were eligible for inclusion if they reported the factors (barriers to and/or facilitators of) affecting HPV vaccine uptake, and/or initiation or completion of HPV vaccination series among ethnic minority adolescent girls. Consistent with the WHO's definition of adolescents and recommendations of age eligibility criteria for HPV vaccination,4 adolescent girls in this review were defined as girls aged 9–19 years. An ethnic minority is defined as a population that constitutes less than 20% of the total population in a country.20 Given that HPV vaccination is recommended for adolescent girls,4 their parents are likely to be the primary decision makers regarding vaccine utilization. Hence, the factors influencing the decision making of ethnic minority parents regarding whether to have their adolescent daughters vaccinated against HPV were also considered as outcomes of this review, and papers reporting this outcome were included in this review. Studies were included if all their recruited participants were ethnic minorities. Studies involving samples comprising both ethnic minorities and the general population were only included if a subgroup analysis of ethnic minorities was conducted. In this review, only original articles published in English were included, where conference abstracts, dissertations, reviews, and study protocols were excluded.
Study selection
Two authors independently screened the titles and abstracts of the identified studies against the eligibility criteria after removing the duplicates using the Covidence software (Veritas Health Innovation, Melbourne, Australia) to identify articles that are potentially eligible for inclusion. The full texts of these articles were retrieved and assessed, and any discrepancies in the selection of studies for inclusion were discussed and resolved between the two authors.
Critical appraisal of methodological quality
The Mixed Methods Appraisal Tool Version 2018 was used to appraise the methodological quality of the included studies.21 This tool contains two general items for screening empirical studies and five specific methodological appraisal items for each of the following three study designs–quantitative descriptive, qualitative, and mixed-methods studies. For quantitative descriptive studies, five domains of study elements are evaluated, including the relevance of sampling strategy, representativeness of study sample, appropriateness of measurements, risk of nonresponse bias, and appropriateness of statistical analysis.21 For qualitative studies, five domains are also assessed, including the appropriateness of qualitative approach and coherence between data collection, analysis, and interpretation.21 For mixed-methods studies, the adherence with the quality criteria of qualitative and quantitative methods and adequacy of integration of both components, including their inconsistencies, are evaluated.21 One mark was given for each item, and the total score was transformed into a percentage score. One author first rated the studies based on each item, which were further verified by a second author. Disagreements in the ratings were discussed and resolved between the two authors.
Data extraction
The extracted data included study design, study setting, ethnicity, sample size, HPV vaccination rates, findings pertaining to factors associated with HPV vaccination among ethnic minority adolescent girls, and/or those influencing parental decisions to have their ethnic minority adolescent girls vaccinated against HPV. The significance of the associations between these factors and HPV vaccination uptake was indicated based on their odds ratios (ORs), 95% confidence intervals (CIs), and P values if available. Examined factors not exhibited such association were also extracted for comparison across studies. One author extracted and presented the data narratively in a table. The completeness and accuracy of the data were verified by a second author, and any discrepancies were resolved through discussions between the two authors.
Data synthesis
The identified factors associated with HPV vaccine uptake among ethnic minority adolescent girls from the included studies were narratively summarized and integrated according to the conceptual model of vaccine hesitancy.17 Using the Review Manager 5.4 software (The Cochrane Collaboration, Copenhagen, Denmark), meta-analyses were conducted to obtain the pooled rates of HPV vaccination among ethnic minority adolescent girls and the pooled effect sizes of factors associated with HPV vaccine utilization. The effect sizes of the included studies were converted to ORs for data pooling, if needed. In view of the heterogeneity of study populations and designs across the included studies, the pooled rates and ORs were calculated using the random-effects model. Heterogeneity of estimates of rates and ORs among the studies was assessed using the I2 statistic, an I2 > 50% was considered to indicate considerable heterogeneity.22 Meta-analyses were not conducted when the ORs and 95% CIs were not reported in the included studies or if there are less than two studies reporting the same associated factor with comparable classifications of the factors.
Results
Search results
The literature search identified 919 articles, of which 373 remained after removing the duplicates. Following screening of the titles and abstracts and the removal of those not relevant to the review aims (n = 300), we examined the full texts of the remaining 73 articles. Further, 59 articles were excluded because they either did not involve samples comprising entirely adolescent girls or their parents (n = 42) or did not report the factors associated with HPV vaccination uptake (n = 17). In the end, 14 articles were deemed eligible for inclusion in this review. Fig. 1 shows the Preferred Reporting Items for Systematic Reviews and Meta-Analyses diagram.
Fig. 1.
The PRISMA diagram.
Study characteristics
Table 2 presents the characteristics of the included studies. Published between 2009 and 2021, the 14 included studies were conducted in either the US (n = 10), the UK (n = 3) or the Netherlands (n = 1). The included studies adopted quantitative descriptive (n = 9), qualitative (n = 4), and mixed-methods (n = 1) designs. Seven studies (50%) involved samples of ethnic minorities recruited in community settings (eg, health fairs, residences, and workplaces).23, 24, 25, 26, 27, 28, 29 In total, 5935 ethnic minority adolescent girls and their parents (including guardians) participated, with Hispanic (n = 2879), Latina (n = 1070), and Asian (Chinese, Korean, Japanese, Filipino, Indian, Pakistani, Cambodian, Bangladeshi, and Sri Lankan; n = 675) ethnic groups constituting the largest proportions of the sample. Other participants were members of African, Hawaiian and Caribbean ethnic minority groups living in the US, the UK, and the Netherlands.
Table 2.
Characteristics and major findings of included studies (N = 14).
| Author, year, and country | Study design and setting | Ethnic population | HPV vaccination rate | Results |
|---|---|---|---|---|
| Alberts et al, 2017,23 The Netherlands | A longitudinal study at a community district | a. Surinamese, Netherlands Antillean, and Aruban (SNA, n = 126) b. Middle Eastern and North African (MENA, n = 237) c. other non-Dutch (n = 223) |
One dose: 6.66% (39/586) Two doses: 52.73% (309/586) |
Factors influencing the uptake of at least one dose of HPV vaccine among adolescent girls
|
| Bastani et al, 2011,30 USA | An analytical cross-sectional study conducted by telephone interviews | a. Latina (n = 255) b. Chinese (n = 98) c. Korean (n = 66) d. African American (n = 38) e. Non-Hispanic White, multi-racial, or other Asian subgroups (n = 35) |
Three doses: 11.57% (56/484) |
Factors influencing the uptake of at least one dose of HPV vaccine among adolescent girls
|
| Dela Cruz et al,34 2020, USA | An analytical cross-sectional survey conducted by telephone | a. Native Hawaiian (n = 189) b. Filipino (n = 199) c. Japanese (n = 200) |
One dose: 45.53% (224/492) Two doses: 9.15% (50/492) Three doses: 35.16% (173/492) |
Facilitators of HPV vaccine uptake among adolescent girls
|
| Forster et al, 2017,24 UK | A comparative qualitative study. Parents were recruited from community groups or online advertising. | a. Non-British White (n = 8) b. Bangladeshi (n = 6) c. African (n = 2) d. Caribbean (n = 2) e. Sri Lankan Tamil (n = 1) f. Somali (n = 1) g. Indian (n = 1) h. Pakistani (n = 1) i. White & Asian (n = 1) j. White & Black African (n = 1) |
N.S. |
Barriers to HPV vaccine uptake among adolescent girls
|
| Fowler et al, 2016,25 USA | A pre-intervention survey conducted at community health fairs | Latinas (n = 206). Only 67 of them were caregivers for a daughter | At least one dose: 35.82% (24/67) |
Factors influencing the uptake of at least one dose of HPV vaccine among adolescent girls
|
| Lechuga et al,26 2020, USA | A mixed method study conducted at mothers' residences | Latinas of Mexican descent, including 65 mother-daughter dyads | At least one dose: 47.69% (31/65) |
Factors influencing the uptake of at least one dose of HPV vaccine among adolescent girls
|
| Marlow et atl.,27 2009, UK | A qualitative study conducted at participants' home or workplace | a. Caribbean and African (n = 10) b. Asian Indian, Asian Pakistani, Asian Bangladeshi, and Asian other (n = 10) |
N.A. |
Facilitators of the decision to accept HPV vaccination for adolescent girls
|
| Mupandawana et al,28 2016, UK | A qualitative study conducted at a university library | African parents (5 mothers and 5 fathers) | N.A. |
Facilitators of the decision to accept HPV vaccination for adolescent girls
|
| Reiter et al, 2014,35 USA | Secondary data analysis of data from National Immunization Survey 2010–2011 | Hispanic adolescent girls aged 13–17 (n = 2786) | At least one dose: 58.83% (1639/2786) Three doses: 36.79% (1025/2786) |
Factors influencing the uptake of at least one dose of HPV vaccine among adolescent girls
|
| Savas et al, 2012,33 USA | A cross-sectional study embedded in a larger cancer prevention study | Hispanic and Black parents (n = 80) | At least one dose: 28.75% (23/80) |
Factors influencing the uptake of at least one dose of HPV vaccine among adolescent girls
|
| Taylor et al, 2014,29 USA | A cross-sectional survey conducted at the Seattle metropolitan area | Cambodian American mothers (n = 86) | At least one dose: 29.07% (25/86) Three doses: 13.95% (12/86) |
Factors influencing the uptake of at least one dose of HPV vaccine among adolescent girls
|
| Tsui et al, 2013,31 USA | A secondary data analysis of a cross-sectional survey (the 2005–2009 American Community Survey) | a. Latina (n = 243) b. Chinese (n = 87) c. Korean (n = 60) d. African (n = 38) e. Other race (n = 30) |
At least one dose: 28.16% (129/458) |
Factors influencing the uptake of at least one dose of HPV vaccine among adolescent girls
|
| Tsui et al, 2013,32 USA | A secondary data analysis of a cross-sectional survey of low-income caregivers of adolescent girls | a. Latina (n = 236) b. Chinese (n = 88) c. Korean (n = 65) d. African (n = 37) e. Other race (n = 31) |
At least one dose: 25.82% (118/457) |
Factors influencing the uptake of at least one dose of HPV vaccine among adolescent girls
|
| Vamos et al, 2021,16 USA | A qualitative study embedded in a large interview study | Hispanic farmworkers (n = 13) | N.A. |
Facilitators of HPV vaccine among adolescent girls
|
CI, confidence interval; HPV, human papillomavirus; MENA, Middle Eastern and North African; N.A., not applicable (the HPV vaccination rates were not calculated in qualitative studies); N.S., not specified (the vaccination rates for ethnic minority adolescent girls were not given); OR; odds ratio; UK, The United Kingdom; USA, the United States; SNA, Surinamese, Netherlands Antillean, and Aruban.
Results of critical appraisal
The results of the critical appraisal of the included studies are shown in Table 3, Table 4. Of the nine quantitative studies that attained quality assessment scores ranging from 42.9% to 85.7%, five had potential risks of recruiting non-representative samples, as non-probability sampling was used during subject recruitment,25,29, 30, 31, 32, 33 four did not provide sufficient details of how outcomes were measured,25,29,30,34 and three had concerns over non-responsive bias due to the low participant response rates to surveys used in the studies, ranging from 22.4% to 34%.23,34,35 Of the five qualitative or mixed-methods studies (Table 4), two had excellent methodological quality with assessment scores of 100%,26,27 and three had quality assessment scores ranging from 57.1% to 85.7% as data synthesis approaches were not explained in sufficient detail or the themes generated from the qualitative data were not sufficiently supported by participants' quotes.16,24,28
Table 3.
Appraisal of the methodological quality of included quantitative descriptive studies (N = 9).
| Study | Clear research questions | Data allow to address research questions | Appropriate sampling strategy | Representative sample | Appropriate measurements | Low risk of non-response bias | Appropriate statistical analyses | Score (Range 1 to 7) | % Score |
|---|---|---|---|---|---|---|---|---|---|
| Alberts et al, 201723 | Yes | Yes | Yes | Yes | Yes | No | Yes | 6 | 85.7% |
| Bastani et al, 201130 | Yes | Yes | No | Yes | Can't tell | Yes | Yes | 5 | 71.4% |
| Dela Cruz et al, 202034 | Yes | Yes | Yes | Yes | Can't tell | No | Yes | 5 | 71.4% |
| Fowler et al, 201625 | Yes | Yes | Can't tell | Yes | Can't tell | Can't tell | No | 3 | 42.9% |
| Reiter et al, 201435 | Yes | Yes | Yes | Yes | Yes | No | Yes | 6 | 85.7% |
| Savas et al, 201233 | Yes | Yes | No | No | Yes | Can't tell | Yes | 4 | 57.1% |
| Taylor et al, 201429 | Yes | Yes | Can't tell | Yes | Can't tell | Yes | Yes | 5 | 71.4% |
| Tsui et al, 201331 | Yes | Yes | Yes | No | Yes | Yes | Yes | 6 | 85.7% |
| Tsui et al, 201332 | Yes | Yes | Yes | No | Yes | Yes | Yes | 6 | 85.7% |
Table 4.
Appraisal of the methodological quality of included qualitative and mixed-method studies (N = 5).
| Study | Clear research questions | Data allow to address research questions | Qualitative method is appropriate/Mixed method is justified | Qualitative method is adequate/Qualitative and quantitative data are integrated | Findings derived from data/mixed data are interpreted | Interpretations are substantiated by data/Addressed inconsistencies in mixed data | Coherence between data collection, analysis and interpretation/Adhered to the quality criteria | Score (Range 1 to 7) | % Score |
|---|---|---|---|---|---|---|---|---|---|
| Forster et al, 201724 | Yes | Yes | Yes | Yes | No | No | Yes | 5 | 71.4% |
| Lechuga et al, 202026 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | 7 | 100% |
| Marlow et al, 201927 | Yes | Yes | Yes | Yes | Yes | Yes | Yes | 7 | 100% |
| Mupandawana et al, 201628 | Yes | Yes | Yes | Yes | No | Yes | Yes | 6 | 85.7% |
| Vamos et al, 202116 | Yes | Yes | No | Yes | No | No | Yes | 4 | 57.1% |
HPV vaccination uptake rates
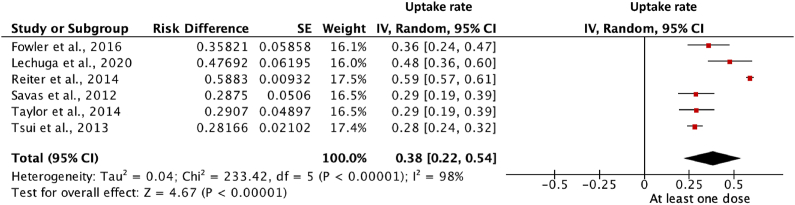
Six studies reported the uptake rate of at least one dose HPV vaccine among ethnic minority adolescent girls (including African, Asian, Black, Cambodian, Hispanic, and Latina) in the US.25,26,29,31,33,35 Meta-analysis of the six studies showed a 38% pooled uptake rate of at least one dose HPV vaccine (95% CI = 0.22, 0.39; P < 0.001; I2 = 98%) among ethnic minority adolescent girls in the US (Fig. 2). Only four studies reported the completion rates of HPV vaccination (having taken three doses of HPV vaccine), ranging from 11.6% to 36.8%.29,30,34,35
Fig. 2.
Forest plot of the pooled uptake rate of at least one dose of HPV vaccination among ethnic minority adolescent female. HPV, human papillomavirus.
Factors affecting HPV vaccine uptake among ethnic minority adolescent girls
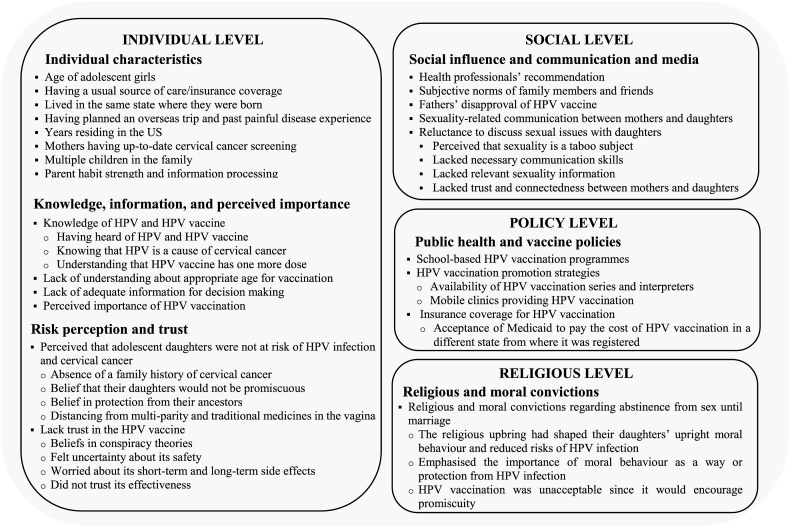
Analysis of the studies revealed multiple factors that are associated with HPV vaccine uptake (initiation or completion of vaccination series). As shown in Fig. 3, these factors can be grouped into four levels, including individual (individual characteristics, knowledge, information and perceived importance of vaccination, risk perception, and trust), social (social influence, communication, and media), policy (public health and vaccination policies), and religious (religious and moral convictions) levels.
Fig. 3.
Multi-level factors influencing HPV vaccination among ethnic minority adolescent girls. HPV, human papillomavirus; US, the United States.
Individual characteristics
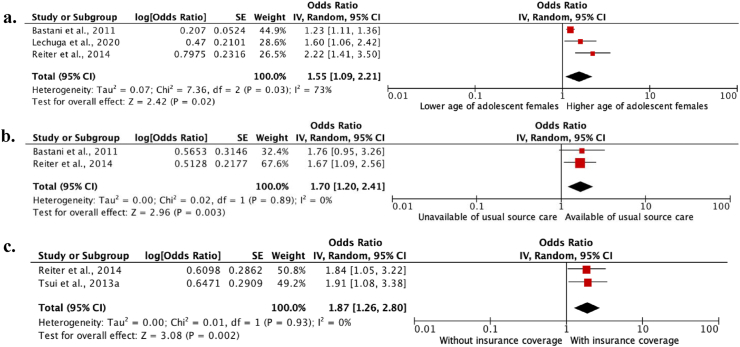
Meta-analyses of four studies26,30,31,35 showed that an increased age of adolescent girls (OR = 1.55; 95% CI = 1.09, 2.21; P = 0.02; I2 = 73%) (Fig. 4a), having a usual source of care (OR = 1.70; 95% CI = 1.20, 2.41; P = 0.003; I2 = 0%) (Fig. 4b) and insurance coverage (OR = 1.87; 95% CI = 1.26, 2.80; P = 0.002; I2 = 0%) (Fig. 4c) were significantly associated with increased odds of initiating and completing HPV vaccination among ethnic minority adolescent girls. Furthermore, ethnic minority parents who were up to date with cervical cancer screening were more likely than others to vaccinate their adolescent daughters.25,29
Fig. 4.
Forest plot of studies examining the association between the likelihood of adolescent females’ initiation and completion of HPV vaccination and their age (a), availability of usual source care (b), and insurance coverage (c). HPV, human papillomavirus.
Conflicting results were obtained regarding whether ethnicity,30,32,33 parents' health insurance status,25,34 and annual household income25,26 were associated with HPV vaccination uptake among ethnic minority adolescent girls.
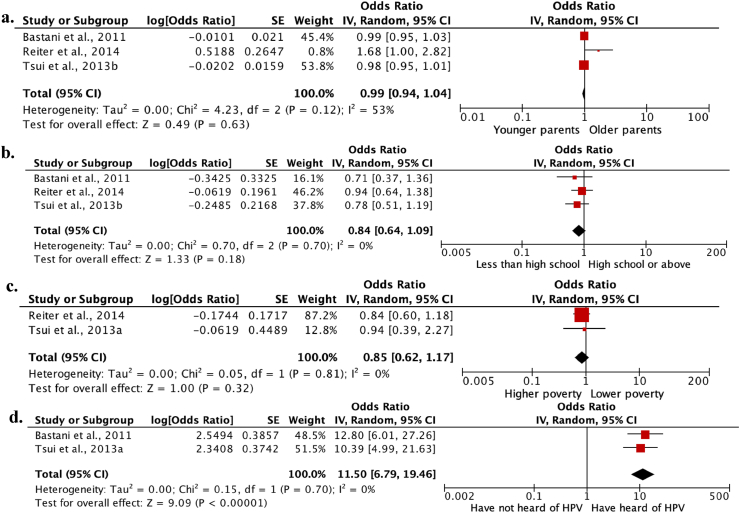
Ethnic minority parents' acculturation factors (including their age when they migrated, country of birth, and English proficiency) did not significantly associated with HPV vaccine uptake among adolescent girls.29,31,32,35 Meta-analyses of four studies30, 31, 32,35 also showed that parents' age (OR = 0.99; 95% CI = 0.94, 1.04; P = 0.63; I2 = 53%) (Fig. 5a), educational attainment (OR = 0.84; 95% CI = 0.64; 1.09; P = 0.18; I2 = 0%) (Fig. 5b), and poverty level (OR = 0.85; 95% CI = 0.62, 1.17; P = 0.32; I2 = 0%) (Fig. 5c) did not significantly associate with HPV vaccine uptake among ethnic minority adolescent girls.
Fig. 5.
Forest plot of studies examining the association between the likelihood of adolescent females’ initiation and completion of HPV vaccination and parents' age (a), educational attainment (b), poverty level (c), and whether have heard of HPV or not (d). HPV, human papillomavirus.
Knowledge, information, and perceived importance
Knowledge and information
Ten studies reported that knowledge of HPV and the HPV vaccine were facilitators of HPV vaccine uptake among ethnic minority adolescent girls, whereas lack of understanding about the appropriate age for vaccination and lack of adequate information for decision making were barriers.16,24,25,27, 28, 29, 30, 31,33,34 A meta-analysis of the two studies reporting their findings with OR values30,31 found that ethnic minority (Latina, Asian, and African) parents in the US who had heard of HPV were 11.5 times more likely to vaccinate their adolescent daughters against HPV with at least one dose (95% CI = 6.79, 19.46; P < 0.001; I2 = 0%) (Fig. 5d).
In contrast, lack of understanding of the rationale for having HPV vaccination at 12–13 years of age precluded ethnic minority parents from vaccinating their adolescent daughters.27,34 Ethnic minority parents might possess misconceptions that cervical cancer is hereditary27 and that only young and sexually active females, and older women who have multiparity should be vaccinated against HPV.28
Importantly, more than 66% of Asian, African, Filipino, Latina, and Native Hawaiian parents in the US expressed a need for more information before making HPV vaccination decisions for their adolescent daughters.30,34 Ethnic minority parents suggested that the information should include cervical cancer (eg, symptoms and mortality rates), HPV, and the HPV vaccine, including the vaccine's relationship with cervical cancer prevention. They also expressed a desire for information on the contents, dose, and side effects of HPV vaccines; the vaccination schedule; effectiveness as supported by statistics.16,24
Perceived importance of vaccination
Seven studies reported that lower perceived importance of HPV vaccination among ethnic minority parents negatively influenced their decision making on and acceptance of HPV vaccination for their adolescent daughters.16,27, 28, 29, 30,33,34 For example, ethnic minority parents in the UK neglected the importance of HPV vaccination for their daughters and believed that they can prevent HPV infection and cervical cancer through their natural immunity, adoption of healthy lifestyles, and God's will.24
In contrast, higher perceived importance of HPV vaccination in the prevention of HPV infection and cervical cancer among ethnic minority (Asian, African, Cambodian, Caribbean, Filipino, native Hawaiian, and Hispanic) parents in the US was consistently reported as a facilitator of decision making on and acceptance of HPV vaccination for their adolescent daughters.16,27, 28, 29,34
Risk perception and trust
Risk perception
The perception that adolescent girls would not be at risk of HPV infection or cervical cancer discouraged ethnic minority parents from vaccinating their adolescent daughters.24,28,34 The absence of a family history of cervical cancer and the belief that their daughters would not be promiscuous or have high-risk sex were major reasons for the lower perceived risks.24 Moreover, African parents also believed that the protection from their ancestors, preventing their daughters from having multiparity, and the use of traditional medicines for tightening the vagina or preparing the birth canal would also lower the risks of HPV infection.28
Trust
Lack of trust in the HPV vaccine, including its purpose, safety, side effects, and effectiveness, was a barrier for ethnic minority parents to vaccinate their adolescent daughters.24,27, 28, 29, 30,33,34 Ethnic minority parents in the UK were reported to mistrust the government, medical system, and vaccine manufacturers. They were also reported to believe in conspiracy theories.28 For example, they perceived that the HPV vaccine was manufactured and distributed for profit,24 or developed with the aim to make their daughters sterile.28 Additionally, ethnic minority parents also expressed concerns over its short-term (eg, pain and allergic reactions) and unknown long-term side effects24,27,30 and believed that it did not protect against all types of HPV for a long duration.24
Social influence and communication and media
Social influence
Four studies found that health professionals' recommendation positively influenced HPV vaccination uptake among ethnic minority adolescent girls.29,33, 34, 35 In addition, subjective norms reflect the attitudes about whether important persons of an individual approval or disapproval of vaccinating the individual's daughter against HPV and the motivation to comply with the opinion.23 The subjective norm of non-Dutch ethnic minority parents in the Netherlands enhanced the odds of HPV vaccination uptake among their adolescent girls by 3.52 times,23 and having family members and friends who have their daughters vaccinated positively influenced parental decision making regarding and acceptance of HPV vaccination for their adolescent daughters.27,34 By contrast, ethnic minority fathers' disapproval of HPV vaccination negatively affected HPV vaccination uptake among adolescent girls.28,29
Communication and media
Sexuality-related communication (eg, discussions on the appropriate time for sexual debut and birth control measures) between mothers and daughters positively influenced HPV vaccination uptake among ethnic minority adolescent girls.26 In contrast, mothers who were reluctant to discuss sexual issues with daughters perceived that sexuality is a taboo subject, lacked the necessary communication skills, relevant sexuality information, trust, and connectedness with their daughters were less likely to initiate such communication, and subsequently, have their adolescent daughters vaccinated.26
Unexpectedly, the influence of social media, including those involved in disseminating health information on HPV vaccination such as television or commercial programs, did not significantly influence HPV vaccination uptake among ethnic minority adolescent girls.29
Public health and vaccine policies
Four studies found that public health and vaccination policies, including the implementation of school-based HPV vaccination programmes, HPV vaccination promotion strategies (including providing reminder phone calls from clinics, making HPV vaccination services and interpreters available at clinics, and offering mobile clinics), were facilitators of HPV vaccination uptake among ethnic minority adolescent girls.16,28, 29, 30 In addition, insurance coverage for HPV vaccination would also facilitate parental decision making to vaccinate their adolescent daughters, as evidenced by the findings that the uncertainty about insurance coverage of HPV vaccination33 and inability of parents to use Medicaid to pay for the cost of HPV vaccination in a different state from where the Medicaid was registered13 would serve as barriers to HPV vaccination among ethnic minority adolescent girls.
Religious and moral convictions
Ethnic minority parents expressed religious and moral convictions regarding abstinence from sex until marriage, which influenced their HPV risk perception and acceptance of HPV vaccine for their adolescent daughters.27,28 They believed that their religious upbringing in Christian churches or Muslim background had shaped their daughters' upright moral behavior and reduced their risks of HPV infection.27,28 To some extent, ethnic minority parents were reluctant to participate in interventions such as HPV vaccination that seemed to encourage sexual behavior and potentially trigger promiscuous behavior among their daughters,28 thus putting them at risk of sexually transmitted diseases.24,27,34
Discussion
This systematic review was guided by the conceptual model of vaccine hesitancy to synthesize evidence on factors affecting HPV vaccination among ethnic minority adolescent girls, and we identified multi-level factors associated with HPV vaccination uptake among this population. Findings could potentially inform interventions and vaccination policies to decrease ethnic disparities in HPV vaccine uptake among adolescent girls.
Meta-analysis of this review found that the pooled uptake rate of at least one dose HPV vaccine was only 38% among ethnic minority adolescent girls. Such vaccination uptake rate is substantially below the WHO's target of immunizing 90% of adolescent girls against HPV6 and lower than the HPV vaccination initiation rate (56.6%) observed among the general population that comprises Caucasians in the US in 2019.9 These findings reinforce the need to further understand the factors influencing HPV vaccination uptake among ethnic minority adolescent girls to inform targeted interventions.
At the individual level, the most prominent factor affecting HPV vaccination uptake among ethnic minority adolescent girls was increased age, which concurs with other reviews.14,36 This finding might be explained by the parental tendency to relate HPV vaccination with sexual activity and their hesitance to vaccinate their daughters at younger ages.34 However, ethnic minority adolescents in the US were approximately two-fold more likely to have early sexual initiation, ie, before 15 years of age, than their White counterparts,37 putting them at greater risk of HPV infection at a young age. Hence, the importance of vaccinating girls at 9–14 years of age, before their sexual debut, should be highlighted to ethnic minority parents.
Lower perceived importance of HPV vaccination and lower perceived risks of HPV infection were reported to be barriers for ethnic minority parents to have their adolescent girls vaccinated. This might be explained by their traditional medical practices and idiosyncratic beliefs, such as being protected by God and their ancestors, avoidance of using traditional medicines for preparing the birth canal, and abstinence from sex are more effective for preventing HPV infection and cervical cancer than HPV vaccination.27,28 Hence, culturally sensitive educational materials with consideration of the relevant cultural values of ethnic minorities should be developed and used for dissemination among ethnic minorities to emphasize the risks of HPV infection and cervical cancer and the importance of vaccination to eliminate ethnic disparities in HPV vaccination.
Mistrust of the HPV vaccine was another prominent individual-level barrier. This finding is consistent with previous systematic reviews that have suggested mistrust as a main obstacle to HPV vaccination among ethnic minorities.38,39 Hence, interventions to debunk conspiracy theories, establish trust with ethnic communities, and inform about the benefits and risks of vaccination might facilitate parents' decision to vaccinate their ethnic minority adolescent daughters, thereby increasing HPV vaccination coverage in this population.38
At the social level, the initiation and completion of HPV vaccination among ethnic minority adolescent girls were influenced by health professionals' recommendations, subjective norms, and sexuality- and birth control-related communication between mothers and adolescent daughters. Similarly, in previous reviews, receiving a health professional's recommendation was consistently cited by ethnic minority parents as a strong facilitator of HPV vaccination for their adolescent daughters.10,15 However, ethnic minorities were less likely to receive an HPV vaccination recommendation from health care professionals, which significantly decreased their initiation and completion of the vaccination.10 Continued efforts are needed to explore and address barriers, including vaccine hesitancy, that hinder health professionals from recommending the HPV vaccine and thus reduce missed opportunities for ethnic minority adolescent girls to receive their full vaccine series.40
At the policy level, public health and vaccination policies were important to inform ethnic minority parents about the HPV vaccine, improve their awareness, and remind them to undertake HPV vaccination for their adolescent daughters.28,29 A meta-analysis of this review found that insurance coverage increased the odds of HPV vaccine uptake among ethnic minority adolescent girls by 1.87 times. Nevertheless, immigration rules, language barriers, and low income might prevent members of ethnic minority groups from enrolling in public or private insurance, and hence, ethnic minority adolescent girls might face important barriers to acquiring health care, including HPV vaccination.35,41 Policies should be created to improve the availability of HPV vaccination for uninsured ethnic minority adolescent girls.35
At the religious level, this review found that religion might negatively influence HPV vaccination among ethnic minority adolescent girls. This is consistent with a previous study that reported that religious beliefs and practices, including attending religious services, reduced the odds of receiving any dose of the HPV vaccine among young women, including ethnic minorities.42 Religion might play a vital role in influencing ethnic minority parents' HPV risk perception, joint decision making, and acceptance of the HPV vaccine for their adolescent daughters.27,28 The parents exhibited HPV risk denial, as they believed that their religious beliefs emphasized abstinence of sex outside marriage and that a religious upbringing shaped their daughters' moral behavior, which would reduce the risk of HPV infection.28 There was also evidence that those who perceived high religious importance and attended church regularly were less likely to have early sexual initiation and unprotected sex.42 Hence, ethnic minority parents might perceive that their daughters were not at risk of HPV infection and be less inclined to accept HPV vaccination.27,43 Additionally, given the link between HPV vaccination and sex, discussion of HPV vaccination was considered shameful and a taboo by ethnic minority parents, which hindered joint decision making with their daughters.28 HPV vaccination was thus less approachable, resulting in low HPV vaccine uptake among ethnic minority adolescent girls.28
Limitations
First, this review only covered original articles published in English. Non-English articles, conference abstracts, dissertations, reviews, and study protocols that reported results relevant to this review were excluded. Thus, publication bias might exist.44 Second, the search strategy might have excluded studies examining ethnic disparities in the use of HPV vaccination without mentioning that the participants were minorities. Third, owing to lack of quantitative explorations and data missing for OR values and the fact that the authors of these studies were not contacted to obtain further information, meta-analyses were not conducted for potentially influencing factors such as subjective norms, religious, and moral convictions. Last, the included studies primarily employed cross-sectional study designs, causal relationships between the identified factors and HPV vaccine uptake among ethnic minority adolescent girls could not be guaranteed.
Implications for research, practice, and policy
The findings of this review have three major implications. First, development and implementation of health educational interventions that encourage communications within families, including fathers' support and sexuality-related communication between mothers and daughters, are warranted. Ethnic minority parents' lack of knowledge and sexuality-related communication skills, lower perceived risks of HPV infection, and sexuality-related concerns were barriers to having their adolescent daughters vaccinated. Hence, health information emphasizing the HPV infection risks, HPV vaccine benefits, and importance of HPV vaccination before sex debut should be delivered to ethnic minority parents. Based on the findings of this review, the information could be effectively delivered via health professionals and schools, such as school-based health talks for parents, and taking into account the cultural values of ethnic minorities in terms of their traditional medical practices and idiosyncratic beliefs. In addition, skills training in initiating sexuality-related communication between ethnic minority mothers and daughters would relieve discomfort in initiating discussions of sexual debut time and birth control measures and enhance communication and mutual decision making regarding HPV vaccination.26
Second, considering that religious values have affected ethnic minority parents' risk perceptions and acceptance of discussions in HPV vaccine, future HPV vaccination programs may benefit from collaborations with religious organizations.42 Church leaders may be invited to address the taboo about discussing HPV vaccination and clarify vaccination benefits among ethnic minorities.28
Third, as HPV vaccination mainly targets girls prior to sexual debut, school-based onsite HPV vaccination can improve access to the HPV vaccine. It has been implemented in the UK and some states of the US.28,45 With support from local policymakers, school board members, and parents, it might be further implemented in schools of other regions, where the vaccination program can reach other ethnically diverse adolescent girls.45 In addition, the government should establish connection and trust with ethnic minorities to overcome with the negative impact of conspiracy theories, which might improve ethnic minority parents' trust in the HPV vaccine and their decision to have their adolescent girls vaccinated against HPV.
Conclusions
With the guidance of a conceptual model of vaccine hesitancy, the factors affecting HPV vaccination uptake among ethnic minority adolescent girls were synthesized at the individual, social, policy, and religious levels. The findings highlight multi-level efforts, including implementing culturally sensitive health education programs, sexuality-related communication skills training, collaboration with religious organizations, establishing trust with ethnic minorities, and formulating vaccination policies to increase the HPV vaccination coverage among the population.
CRediT author statement
Dorothy N. S. Chan: Conceptualization; Methodology; Project administration; Supervision; Roles/Writing-original draft; Caixia Li: Formal analysis; Roles/Writing-original draft; Bernard M. H. Law: Methodology; Writing-review & editing; K.C. Choi: Methodology; Writing-review & editing; Pinky P. K. Lee: Writing-review & editing; Winnie K. W. So: Writing-review & editing. All authors had full access to all the data in the study, and the corresponding author had final responsibility for the decision to submit for publication. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Declaration of competing interest
All authors have none to declare. Dorothy N.S. Chan, K.C. Choi, and Winnie K.W. So are eidotiral board members of Asia-Pacific Journal of Oncology Nursing. The article was subject to the journal's standard procedures, with peer review handled independently of Prof. So and their research groups.
Funding
This study received no external funding.
Ethics statement
Not required.
Data availability statement
Data availability is not applicable to this article as no new data were created or analyzed in this study.
References
- 1.Singh D., Vignat J., Lorenzoni V., et al. Global estimates of incidence and mortality of cervical cancer in 2020: a baseline analysis of the WHO Global Cervical Cancer Elimination Initiative. Lancet Glob Health. 2023;11:e197–e206. doi: 10.1016/s2214-109x(22)00501-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Shing J.Z., Corbin J., Kreimer A.R., et al. Human papillomavirus-associated cancer incidence by disaggregated Asian American, Native Hawaiian, and other Pacific Islander ethnicity. JNCI Cancer Spectr. 2023;7 doi: 10.1093/jncics/pkad012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vengaloor Thomas T., Gandhi S., Bhanat E., et al. An analysis of the racial disparities among cervical cancer patients treated at an academic medical center in the Southeastern United States. Cureus. 2021;13 doi: 10.7759/cureus.13296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization . 2022. Human Papillomavirus Vaccines: WHO Position Paper.https://www.who.int/publications/i/item/who-wer9750-645-672; [Google Scholar]
- 5.Villa A., Patton L.L., Giuliano A.R., et al. Summary of the evidence on the safety, efficacy, and effectiveness of human papillomavirus vaccines: umbrella review of systematic reviews. J Am Dent Assoc. 2020;151:245–254.e24. doi: 10.1016/j.adaj.2019.10.010. [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization . 2020. Global Strategy to Accelerate the Elimination of Cervical Cancer as a Public Health Probelm.https://www.who.int/publications/i/item/9789240014107; [Google Scholar]
- 7.Rodriguez A.M., Do T.Q.N., Eyada M.F., Chen L., Schmeler K.M., Montealegre J.R. Human papillomavirus vaccination uptake in the Rio Grande Valley: results from a pilot community-based educational and school-based vaccination program and its expansion. Vaccines. 2023;11 doi: 10.3390/vaccines11020329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fisher H., Hickman M., Ferrie J., et al. Impact of new consent procedures on uptake of the schools-based human papillomavirus (HPV) vaccination programme. J Public Health. 2022;44:199–206. doi: 10.1093/pubmed/fdaa164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bandi P., Minihan A.K., Siegel R.L., et al. Updated review of major cancer risk factors and screening test use in the United States in 2018 and 2019, with a focus on smoking cessation. Cancer Epidemiol Biomark Prev. 2021;30:1287–1299. doi: 10.1158/1055-9965.Epi-20-1754. [DOI] [PubMed] [Google Scholar]
- 10.Amboree T.L., Darkoh C. Barriers to human papillomavirus vaccine uptake among racial/ethnic minorities: a systematic review. J Racial Ethn Health Dispar. 2021;8:1192–1207. doi: 10.1007/s40615-020-00877-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kerry-Barnard S., Beddows S., Reid F., et al. Human papillomavirus (HPV) vaccination and oropharyngeal HPV in ethnically diverse, sexually active adolescents: community-based cross-sectional study. Sex Transm Infect. 2021;97:458–460. doi: 10.1136/sextrans-2020-054428. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bastani R., Glenn B.A., Singhal R., et al. Increasing HPV vaccination among low-income, ethnic minority adolescents: effects of a multicomponent system intervention through a county health department hotline. Cancer Epidemiol Biomark Prev. 2022;31:175–182. doi: 10.1158/1055-9965.Epi-20-1578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lott B.E., Okusanya B.O., Anderson E.J., et al. Interventions to increase uptake of Human Papillomavirus (HPV) vaccination in minority populations: a systematic review. Prev Med Rep. 2020;19 doi: 10.1016/j.pmedr.2020.101163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jo S., Han S.Y., Walters C.A. Factors associated with the HPV vaccination among Korean Americans and Koreans: a systematic review. Int J Environ Res Public Health. 2021;19 doi: 10.3390/ijerph19010051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dike S., Freysteinson W.M. Factors associated with African American mothers' perceptions of human papillomavirus vaccination of their daughters: an integrated literature review. Oncol Nurs Forum. 2021;48:371–389. doi: 10.1188/21.Onf.371-389. [DOI] [PubMed] [Google Scholar]
- 16.Vamos C.A., Vázquez-Otero C., Kline N., et al. Multi-level determinants to HPV vaccination among Hispanic farmworker families in Florida. Ethn Health. 2021;26:319–336. doi: 10.1080/13557858.2018.1514454. [DOI] [PubMed] [Google Scholar]
- 17.Dubé E., Laberge C., Guay M., Bramadat P., Roy R., Bettinger J. Vaccine hesitancy: an overview. Hum Vaccin Immunother. 2013;9:1763–1773. doi: 10.4161/hv.24657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dubé E., Gagnon D., Zhou Z., Deceuninck G. Parental vaccine hesitancy in Quebec (Canada) PLoS Curr. 2016;8 doi: 10.1371/currents.outbreaks.9e239605f4d320c6ad27ce2aea5aaad2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Page M.J., McKenzie J.E., Bossuyt P.M., et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chan D.N.S., So W.K.W. A systematic review of the factors influencing ethnic minority women's cervical cancer screening behavior: from intrapersonal to policy level. Cancer Nurs. 2017;40:E1–e30. doi: 10.1097/ncc.0000000000000436. [DOI] [PubMed] [Google Scholar]
- 21.Hong Q.N., Fàbregues S., Bartlett G., et al. The mixed methods appraisal tool (MMAT) version 2018 for information professionals and researchers. Educ Inf. 2018;34:285–291. [Google Scholar]
- 22.Higgins J.P., Thompson S.G., Deeks J.J., Altman D.G. Measuring inconsistency in meta-analyses. Bmj. 2003;327:557–560. doi: 10.1136/bmj.327.7414.557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Alberts C.J., van der Loeff M.F., Hazeveld Y., et al. A longitudinal study on determinants of HPV vaccination uptake in parents/guardians from different ethnic backgrounds in Amsterdam, the Netherlands. BMC Publ Health. 2017;17:220. doi: 10.1186/s12889-017-4091-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Forster A.S., Rockliffe L., Marlow L.A.V., Bedford H., McBride E., Waller J. Exploring human papillomavirus vaccination refusal among ethnic minorities in England: a comparative qualitative study. Psycho Oncol. 2017;26:1278–1284. doi: 10.1002/pon.4405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fowler B., Bodson J., Warner E.L., Dyer J., Kepka D. Poor HPV vaccine-related awareness and knowledge among Utah Latinas overdue for recommended cancer screenings. J Community Health. 2016;41:825–837. doi: 10.1007/s10900-016-0160-3. [DOI] [PubMed] [Google Scholar]
- 26.Lechuga J., Prieto C., Mata H., Belknap R.A., Varela I. Culture and sexuality-related communication as sociocultural precursors of HPV vaccination among mother-daughter dyads of Mexican descent. Prev Med Rep. 2020;19 doi: 10.1016/j.pmedr.2020.101105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Marlow L.A., Wardle J., Waller J. Attitudes to HPV vaccination among ethnic minority mothers in the UK: an exploratory qualitative study. Hum Vaccin. 2009;5:105–110. doi: 10.4161/hv.5.2.7368. [DOI] [PubMed] [Google Scholar]
- 28.Mupandawana E.T., Cross R. Attitudes towards human papillomavirus vaccination among African parents in a city in the north of England: a qualitative study. Reprod Health. 2016;13:97. doi: 10.1186/s12978-016-0209-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Taylor V.M., Burke N.J., Ko L.K., et al. Understanding HPV vaccine uptake among Cambodian American girls. J Community Health. 2014;39:857–862. doi: 10.1007/s10900-014-9844-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bastani R., Glenn B.A., Tsui J., et al. Understanding suboptimal human papillomavirus vaccine uptake among ethnic minority girls. Cancer Epidemiol Biomark Prev. 2011;20:1463–1472. doi: 10.1158/1055-9965.Epi-11-0267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tsui J., Gee G.C., Rodriguez H.P., et al. Exploring the role of neighborhood socio-demographic factors on HPV vaccine initiation among low-income, ethnic minority girls. J Immigr Minor Health. 2013;15:732–740. doi: 10.1007/s10903-012-9736-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tsui J., Singhal R., Rodriguez H.P., Gee G.C., Glenn B.A., Bastani R. Proximity to safety-net clinics and HPV vaccine uptake among low-income, ethnic minority girls. Vaccine. 2013;31:2028–2034. doi: 10.1016/j.vaccine.2013.02.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Savas L.S., Fernández M.E., Jobe D., Carmack C.C. Human papillomavirus vaccine: 2-1-1 helplines and minority parent decision-making. Am J Prev Med. 2012;43(6 suppl. 5):S490–S496. doi: 10.1016/j.amepre.2012.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dela Cruz M.R.I., Braun K.L., Tsark J.A.U., Albright C.L., Chen J.J. HPV vaccination prevalence, parental barriers and motivators to vaccinating children in Hawai'i. Ethn Health. 2020;25:982–994. doi: 10.1080/13557858.2018.1473556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Reiter P.L., Gupta K., Brewer N.T., et al. Provider-verified HPV vaccine coverage among a national sample of Hispanic adolescent females. Cancer Epidemiol Biomark Prev. 2014;23:742–754. doi: 10.1158/1055-9965.Epi-13-0979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Galbraith K.V., Lechuga J., Jenerette C.M., Moore L.A., Palmer M.H., Hamilton J.B. Parental acceptance and uptake of the HPV vaccine among African-Americans and Latinos in the United States: a literature review. Soc Sci Med. 2016;159:116–126. doi: 10.1016/j.socscimed.2016.04.028. [DOI] [PubMed] [Google Scholar]
- 37.El-Menshawi M., Castro G., Rodriguez de la Vega P., Ruiz Peláez J.G., Barengo N.C. First time cannabis use and sexual debut in U.S. high school adolescents. J Adolesc Health. 2019;64:194–200. doi: 10.1016/j.jadohealth.2018.08.018. [DOI] [PubMed] [Google Scholar]
- 38.Gopalani S.V., Sedani A.E., Janitz A.E., et al. Barriers and factors associated with HPV vaccination among American Indians and Alaska Natives: a systematic review. J Community Health. 2022;47:563–575. doi: 10.1007/s10900-022-01079-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Holman D.M., Benard V., Roland K.B., Watson M., Liddon N., Stokley S. Barriers to human papillomavirus vaccination among US adolescents: a systematic review of the literature. JAMA Pediatr. 2014;168:76–82. doi: 10.1001/jamapediatrics.2013.2752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Efua Sackey M., Markey K., Grealish A. Healthcare professional's promotional strategies in improving Human papillomavirus (HPV) vaccination uptake in adolescents: a systematic review. Vaccine. 2022;40:2656–2666. doi: 10.1016/j.vaccine.2022.03.054. [DOI] [PubMed] [Google Scholar]
- 41.Sohn H. Racial and ethnic disparities in health insurance coverage: dynamics of gaining and losing coverage over the life-course. Popul Res Policy Rev. 2017;36:181–201. doi: 10.1007/s11113-016-9416-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Best A.L., Thompson E.L., Adamu A.M., et al. Examining the influence of religious and spiritual beliefs on HPV vaccine uptake among college women. J Relig Health. 2019;58:2196–2207. doi: 10.1007/s10943-019-00890-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chan D.N.S., Lee P.P.K., So W.K.W. Exploring the barriers and facilitators influencing human papillomavirus vaccination decisions among South Asian and Chinese Mothers: a qualitative study. J Racial Ethn Health Dispar. 2023:1–13. doi: 10.1007/s40615-023-01623-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sterne J.A., Sutton A.J., Ioannidis J.P., et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. Bmj. 2011;343:d4002. doi: 10.1136/bmj.d4002. [DOI] [PubMed] [Google Scholar]
- 45.Kaul S., Do T.Q.N., Hsu E., Schmeler K.M., Montealegre J.R., Rodriguez A.M. School-based human papillomavirus vaccination program for increasing vaccine uptake in an underserved area in Texas. Papillomavirus Res. 2019;8 doi: 10.1016/j.pvr.2019.100189. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data availability is not applicable to this article as no new data were created or analyzed in this study.