Abstract
During hospitalisation with COVID-19, individuals may experience prolonged periods of immobilisation. Combined with the inflammatory effects of the virus, this may lead to a significant reduction in both muscle mass and strength. Data from several long-term studies suggest that these symptoms may not fully resolve within one year. Owing to its effectiveness at inducing muscle fibre hypertrophy and improving neuromuscular efficiency, resistance training is of great interest in the rehabilitation of this population. This narrative review aims to identify the rationale and potential efficacy of resistance training for restoring physical function following infection with SARS-CoV-2, as well as evidence of its use in clinical practice. The studies included in this narrative review consisted mostly of multi-component rehabilitation trials. Of these, widespread improvements in muscle strength were reported using intensities of up to 80% of participants’ 1-repetition-maximum. Evidence thus far indicates that resistance training may be safe and effective in patients following COVID-19, although its individual contribution is difficult to discern. Future exercise intervention studies investigating the efficacy of resistance training as a sole modality are needed.
Keywords: COVID-19, Exercise, Muscle, Resistance training, Rehabilitation
Introduction
A prospective cohort study of 1077 individuals hospitalised with COVID-19 found that 92.8% still experienced a minimum of one persistent symptom six months after discharge[1]. Physically slowing down (49.9%) and limb weakness (46.3%) were among the most commonly reported symptoms. Functional impairment, indicated by a score of 10 or less in the Short Performance Physical Battery, was present in 46.2% of this population. Hospitalisation and intensive care admission leads to a reduction in both muscle mass and strength, even with short hospital stays of 5 days[2,3]. This is particularly concerning for elderly individuals who are more likely to initially present with low muscle mass and functional impairment[4,5]. Due to the nature of the COVID-19 virus and its impact on energy production, it has been hypothesised that it could be more detrimental to the musculoskeletal system compared to other conditions causing similar lengths of immobilisation, such as limb fracture or severe pneumonia[6].
Resistance training has proved an effective strategy for preventing the deterioration of muscle and strength loss induced by ageing and chronic disease[7-9]. Compared to aerobic exercise, resistance training elicits superior hypertrophic and strength adaptations in skeletal muscle tissue[10,11]. In acutely hospitalised elderly individuals, a recent meta-analysis reported an average improvement in hand grip strength and maximum leg press of 2.5 kg and 19.28 kg, respectively, following the implementation of a high-frequency (5–7 days per week) resistance training programme[12]. The same review noted a mean score improvement of 1.79 in the Short Performance Physical Battery, indicating improved lower limb functional capacity. Several papers have demonstrated the effectiveness of modified pulmonary rehabilitation in those discharged from hospital with COVID-19, which includes elements of resistance training[13-15], but the isolated effect of resistance training on functional capacity and quality of life in this population is not well understood. This narrative review will explore the rationale behind resistance training prescription in COVID-19 survivors and identify the potential effects on physical function and quality of life.
Skeletal muscle consequences of COVID-19
Individuals hospitalised with COVID-19 experience prolonged periods of inactivity in addition to common viral symptoms such as reduced appetite, nausea, vomiting and diarrhoea[16]. This combination of nutrient loss and muscle disuse provides an environment conducive to skeletal muscle catabolism[17]. As a result, it has been identified that individuals discharged from hospital following COVID-19 are at an increased risk of muscle loss and resultant functional impairment[18]. Previous evidence from 55 individuals with an acute exacerbation of chronic respiratory disease showed an average 8.3% loss of quadriceps muscle thickness over a median of 5 days of hospitalisation[3]. The same study observed a sustained loss of muscle thickness at 6-week follow-up and only partial recovery at 3 months. In individuals with COVID-19, these effects may be more profound. An average 30% loss of quadriceps muscle thickness has been observed after ten days of immobilisation in a COVID-19 intensive care unit[19]. It is currently unclear how long is required for muscle function to return to previous levels in these individuals, or what rehabilitative strategies may be optimal.
Severe acute weight loss during hospitalisation can have a detrimental impact on muscle mass and may contribute to the development of acute sarcopenia[20,21]. Muscle strength is also impacted, with 86% of individuals displaying quadriceps weakness at discharge (categorised as maximal voluntary isometric contraction less than 80% of predicted normal value[22]. Although total body mass may return to pre-illness levels several months following hospitalisation, this may not necessarily coincide with muscle function. Despite receiving dietary support, physical activity guidance, and physiotherapy assistance during the recovery period, 14.3% of individuals reported a persistent loss of muscle strength six months after discharge from hospital with COVID-19[23]. Data from the PHOSP-COVID trial suggests that this figure may be significantly larger when taking into account fatigue, physical slowness and limb weakness, with around half of all patients affected at six months[1].
It should be considered that the long-term effects of COVID-19 on the musculoskeletal system may not be as pronounced in young healthy populations, where baseline muscle mass and strength is greater than that of older individuals. In the elderly population, exposure to the inflammatory burden of an acute illness such as COVID-19, combined with high levels of inactivity during hospital admission, is likely to have a detrimental effect on long-term health outcomes[24]. It is therefore of paramount importance to deliver safe and effective rehabilitation strategies to assist recovery in these individuals.
Resistance training as a therapeutic intervention in COVID-19
Rationale
In contrast to aerobic exercise, resistance training involves greater levels of mechanical tension, comparatively fewer repetitions, and greater control of movement. Performing regular resistance training at an adequate intensity and volume results in positive muscular and neurological adaptations (Figure 1), such as increased muscle cross-sectional area and greater and more efficient motor unit recruitment[25]. These effects have proven beneficial in improving functional capacity in elderly individuals and those with respiratory, circulatory, infectious, renal, urological, neurological, gastrointestinal, and musculoskeletal conditions[12].
Figure 1.
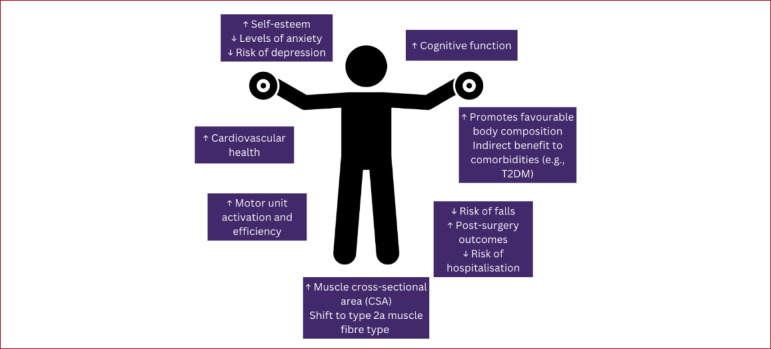
Diagram detailing the physiological and psychological response to resistance training. Whole-body responses are outlined and include both short-term and long-term adaptations and effects. (Abbreviations: T2DM = type 2 diabetes mellitus).
In an initial attempt to reduce the severity of functional deterioration during a period of intensive care, activities such as sitting out of bed, standing up, walking, arm exercises and self-care activities are often performed as soon as the patient is physically able. Strategies such as these may have a positive short-term effect on muscle strength and mobility[26,27]. In patients at risk of hospital-acquired disability (indicated by the loss of ability to perform one or more basic activities of daily living), performing bodyweight resistance exercises twice per day during hospital admission reduced the risk of functional decline by 70% compared to those who received standard care[28]. This effect remained significant three months following discharge, despite adjusting for clinical characteristics and functional performance at admission. Externally loaded exercises may also be utilised to elicit positive adaptations where feasible. Individuals hospitalised with an acute exacerbation of chronic respiratory disease increased quadriceps maximal voluntary force by 9.7% following a 7-day knee extension programme, performing 3 sets of 8 repetitions at 70% of their 1-repetition-maximum (1RM)[29].
In an outpatient setting, resistance training has demonstrated high levels of effectiveness and tolerability in those with respiratory conditions. In a 2015 meta-analysis of chronic obstructive pulmonary disease (COPD) exercise intervention studies, resistance training increased muscle strength both with and without the inclusion of aerobic exercise[30]. Importantly, no related adverse events were reported across the 18 trials with a total of 750 participants. Even when exercises are performed with heavier loads (80% of 1-repetition maximum), the effectiveness and safety of the intervention remains unchanged[31].
Safety
Mechanistically, resistance training induces both peripheral and central demands on the body. Intrathoracic pressure increases rapidly during the eccentric-to-concentric portion of the movement, precipitating the Valsalva manoeuvre at higher intensities and causing a notable haemodynamic response[32]. Although those with respiratory conditions may have a reduced work capacity, the elicited physiological response during resistance training does not seem to result in dangerous cardio-pulmonary manifestations, with VO2 and minute ventilation changes during resistance training similar to that of healthy individuals[33]. Although there are several distinct differences in the sequelae and manifestations of chronic respiratory conditions and COVID-19, studies such as these suggest a low ventilatory demand and dyspnoea associated with resistance training[34,35].
Furthermore, the discontinuous nature of a typical resistance training session enables a greater accumulation of training volume whilst minimising the risk of symptom exacerbation[36]. Likely due to a combination of these factors, a recent review concluded that resistance training was better tolerated than aerobic exercise (86–95% vs 73%) in individuals hospitalised with an exacerbation of chronic obstructive pulmonary disease or with community-acquired pneumonia[35]. However, tolerability was measured by session attendance rather than physical parameters, with a significant number of non-attendances due to logistical reasons such as interruptions by medical staff or unavailability of the patient/therapist, and therefore this misrepresents tolerability.
The exclusion of individuals with certain clinical features in some studies may result in limited applicability to the COVID-19 patient, who is likely to suffer from multiple comorbidities[37,38]. For example, the study by Kongsgaard and colleagues[31] excluded those with cardiac conditions when screening, however, cardiac comorbidities have been reported in 42.2% of individuals following hospitalisation with COVID-19[1]. In addition, the aforementioned systematic review by Rice and colleagues[35] excluded intensive-care patients from their criteria, a group that would likely benefit most from a resistance training intervention due to the high probability of muscle mass and strength loss[39]. Considerations will need to be assessed on an individual basis when planning any form of exercise for these individuals.
Current evidence
Guidelines for pulmonary rehabilitation in adults published by The British Thoracic Society recommend progressive resistance training that targets major muscle groups, consisting of two to four sets of 10-15 repetitions per exercise[40]. Although there are currently no specific guidelines for the use of resistance training in COVID-19 rehabilitation, many studies have reported positive results from programmes that follow a similar structure[41]. Gobbi and colleagues[42] assessed the effects of a 28-day strength programme combined with aerobic exercise in 34 individuals with and without low muscle mass following discharge from hospital with COVID-19. Participants performed 1-3 sets of 8-12 repetitions for each exercise, with 2 minutes of rest in between sets. When assessed at the end of the programme, appendicular skeletal muscle mass increased in both low muscle and normal muscle groups by 8.51% and 10.67%, respectively. However, this study implemented a concurrent nutritional programme which may prevent practitioners from replicating these results where nutritional support may not be feasible.
Evidence of widespread improvements in muscle cross-sectional area following a post-COVID-19 exercise intervention has been reported by Nambi and colleagues[43]. Individuals with clinically diagnosed low muscle mass were prescribed 8 weeks of resistance training combined with either low or high-intensity aerobic exercise. Three sets of 10 repetitions were performed 4 times per week targeting both the upper and lower body. Muscle cross-sectional area of the arm (5.3%, 4.8%), calf (10.1%, 10.3%) and thigh (7.8%, 7.8%) all increased in both groups over the intervention period as well as hand-grip strength (10.9% and 4.5%). Perhaps most valuably, quality of life (measured by the Sarcopenia and Quality of Life (SarQol) questionnaire) improved by 20.4% in the low-intensity group and 4.8% in the high-intensity group. The session frequency in this study exceeded the amount outlined in current pulmonary rehabilitation guidelines (minimum twice per week)[40]. Future research may need to explore the optimal, tolerable frequency and volume of resistance training in those at an increased risk of low muscle mass following COVID-19 hospitalisation.
In multi-component COVID-19 exercise trials, descriptions of resistance training load prescription, intensity and selection of exercises vary significantly. This is likely due to a greater focus on outcomes such as aerobic capacity and symptoms such as breathlessness and fatigue. However, several trials have provided detailed descriptions of their methods relating to resistance training prescription, with the majority reporting improvements in muscle strength and functional capacity[41]. In a larger trial, individuals with reduced exercise capacity following COVID-19 (defined by the authors as the value below 85% of predicted peak oxygen uptake (V̇O2peak)) performed aerobic and resistance training for 8-weeks[44]. Resistance exercises included: leg extension/flexion, abduction/adduction, leg press, push-up/pull-down and abdomen and back exercises. Load was prescribed using 40% of the subjects’ 1-repetition-maximum and was performed for 2-3 sets of 12 repetitions for each muscle group. Interestingly, the authors reported a 0% dropout rate throughout the intervention period, which is supportive of a previous systematic review demonstrating higher tolerability among patients on pulmonary rehabilitation programmes when resistance training was included[35]. The intervention was effective at improving 1-repetition-maximum in all major muscle groups, with overall strength improvements ranging from 16% to 33%. The absence of any functional or quality-of-life outcomes or control group limits the interpretability of these results, although previous evidence has indicated that improvements in muscle strength may translate to improved functional capacity in vulnerable, hospitalised individuals[12].
When considering outcomes following rehabilitation, it is important that any gains in strength and lean body mass translate to enhanced functional capacity, especially following intensive care admission where functional deterioration is likely[45]. Udina and colleagues[46] recruited post-acute care COVID-19 individuals for a multi-component exercise intervention study. Resistance exercises were performed with 1–2 sets of 8–10 repetitions per exercise at an intensity of 30–80% of individuals’ 1-repetition-maximum. Whilst muscle strength and lean body mass were not assessed in this trial, lower limb functional capacity measured by the Short Physical Performance Battery chair stand test improved from 35.4 to 14.1 seconds. Improvements in similar functional measures such as the sit-to-stand test have also been observed in another cohort of COVID-19 patients where bodyweight exercises such as sit-to-stand, calf raises, and squats were regularly performed[47]. However, contrary to these findings, Piquet and colleagues[47] also reported that independence for personal tasks of daily living had not returned to pre-infection levels. Therefore, further research is needed to understand the impact of COVID-19 rehabilitation on health-related quality of life and long-term functional outcomes.
One problem that is encountered when interpreting the effects of resistance training in COVID-19 rehabilitation trials is the multi-factorial nature of the interventions. Many studies include a combination of exercise modes including aerobic, resistance, power, and flexibility training[41], making it difficult to interpret the contribution of each element to the resultant physiological adaptations. It is important to recognise that aerobic capacity will play an important role in mediating the recovery in those with impaired physical function, although future research may need to explore the individual effect of each mode of exercise in individuals following COVID-19. This may be done through parallel and crossover study designs where aerobic exercise interventions are compared to combined exercise interventions, replicating previous studies in individuals with COPD[48-52]. The CISCO-21[53] and EXER-COVID[54] protocols describe two COVID-19 rehabilitation studies where resistance training is the sole or primary modality. The rationale of the authors reflects the major points covered in this narrative review, highlighting the potency of resistance training as a non-pharmacological method of ameliorating the loss of lean tissue and strength. Results of such studies will develop our understanding of effective rehabilitation strategies following COVID-19.
Practical recommendations for clinicians
Current available literature exploring the direct impact and safety of resistance training in COVID-19 survivors is sparse. Therefore, any practical recommendations for exercise prescription in this population will reflect current rehabilitation practice in other respiratory conditions. Nevertheless, it seems as though resistance training remains an important component of modified pulmonary rehabilitation following COVID-19 and is generally well tolerated. Interventions mentioned in this narrative review included exercises that targeted most major muscle groups and ranged from 1-4 sets and 8-15 repetitions per exercise with loads of up to 80% of an individual’s 1-repetition-maximum. As with any resistance training programme, the intensity and volume of the work should be gradually increased over a period of several weeks to allow physiological adaptation to occur.
Clinicians should be mindful that most COVID-19 patients, even those who were physically active prior to hospitalisation, may lack familiarity with resistance training and its potential advantages[55]. Resistance training offers a feasible and well-adhered approach for home-bound elderly individuals to maintain physical activity levels[56,57], as it can be performed without access to gym facilities and with minimal associated costs[58]. For those deemed safe to engage in unsupervised exercise, clinicians should consider incorporating muscle-strengthening exercises into their general recommendations.
Although the downstream effects of resistance training on activities of daily living and quality of life in this population are unclear, short to medium-term improvements in muscle strength and functional capacity have been reported in several trials included in this narrative review. In addition, most studies thus far have included both resistance and aerobic training. Differentiating the relative benefit of resistance training in this population will be important in developing an optimal, individualised approach to rehabilitation.
Conclusion
Although numerous studies have demonstrated the efficacy of exercise interventions for various symptoms, further research is required to enable the development of targeted rehabilitation programmes. Resistance training has proven to be effective in enhancing muscle strength in several multi-component COVID-19 rehabilitation trials. Consequently, it is vital for researchers and healthcare providers to evaluate and convey the advantages of resistance training to affected individuals while incorporating it into a safe and personalised program.
Acknowledgments
We would like to thank all listed authors for their contributions. We would also like to thank the University Hospitals of Leicester NHS Trust and everyone within the Centre for Exercise and Rehabilitation Science for their continued support. Professor Sally J. Singh is a National Institute for Health Research (NIHR) Senior Investigator. This research is supported by the NIHR Leicester Biomedical Research Centre (BRC). The views expressed are those of the authors and not necessarily those of the NIHR or the Department of Health and Social Care.
Footnotes
Edited by: Yannis Dionyssiotis
References
- 1.Evans RA, McAuley H, Harrison EM, Shikotra A, Singapuri A, Sereno M, et al. Physical, cognitive, and mental health impacts of COVID-19 after hospitalisation (PHOSP-COVID):a UK multicentre, prospective cohort study. Lancet Respir Med. 2021;9(11):1275–87. doi: 10.1016/S2213-2600(21)00383-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Marusic U, Narici M, Simunic B, Pisot R, Ritzmann R. Nonuniform loss of muscle strength and atrophy during bed rest:a systematic review. J Appl Physiol (1985) 2021;131(1):194–206. doi: 10.1152/japplphysiol.00363.2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McAuley HJC, Harvey-Dunstan TC, Craner M, Richardson M, Singh SJ, Steiner MC, et al. Longitudinal changes to quadriceps thickness demonstrate acute sarcopenia following admission to hospital for an exacerbation of chronic respiratory disease. Thorax. 2021;76(7):726–8. doi: 10.1136/thoraxjnl-2020-215949. [DOI] [PubMed] [Google Scholar]
- 4.Hartley P, Romero-Ortuno R, Wellwood I, Deaton C. Changes in muscle strength and physical function in older patients during and after hospitalisation:a prospective repeated-measures cohort study. Age Ageing. 2021;50(1):153–60. doi: 10.1093/ageing/afaa103. [DOI] [PubMed] [Google Scholar]
- 5.Tanner RE, Brunker LB, Agergaard J, Barrows KM, Briggs RA, Kwon OS, et al. Age-related differences in lean mass, protein synthesis and skeletal muscle markers of proteolysis after bed rest and exercise rehabilitation. J Physiol. 2015;593(18):4259–73. doi: 10.1113/JP270699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Piotrowicz K, Gasowski J, Michel JP, Veronese N. Post-COVID-19 acute sarcopenia:physiopathology and management. Aging Clin Exp Res. 2021;33(10):2887–98. doi: 10.1007/s40520-021-01942-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Law TD, Clark LA, Clark BC. Resistance Exercise to Prevent and Manage Sarcopenia and Dynapenia. Annu Rev Gerontol Geriatr. 2016;36(1):205–28. doi: 10.1891/0198-8794.36.205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Nascimento CM, Ingles M, Salvador-Pascual A, Cominetti MR, Gomez-Cabrera MC, Vina J. Sarcopenia, frailty and their prevention by exercise. Free Radic Biol Med. 2019;132:42–9. doi: 10.1016/j.freeradbiomed.2018.08.035. [DOI] [PubMed] [Google Scholar]
- 9.Suetta C, Andersen JL, Dalgas U, Berget J, Koskinen S, Aagaard P, et al. Resistance training induces qualitative changes in muscle morphology, muscle architecture, and muscle function in elderly postoperative patients. J Appl Physiol (1985) 2008;105(1):180–6. doi: 10.1152/japplphysiol.01354.2007. [DOI] [PubMed] [Google Scholar]
- 10.Hunter GR, McCarthy JP, Bamman MM. Effects of resistance training on older adults. Sports Med. 2004;34(5):329–48. doi: 10.2165/00007256-200434050-00005. [DOI] [PubMed] [Google Scholar]
- 11.Sherwood L. Human physiology :from cells to systems. 3rd ed. Belmont, CA: Wadsworth Pub. Co; 1997. [Google Scholar]
- 12.Carneiro MAS, Franco CMC, Silva AL, Castro ESP, Kunevaliki G, Izquierdo M, et al. Resistance exercise intervention on muscular strength and power, and functional capacity in acute hospitalized older adults:a systematic review and meta-analysis of 2498 patients in 7 randomized clinical trials. Geroscience. 2021;43(6):2693–705. doi: 10.1007/s11357-021-00446-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Daynes E, Gerlis C, Chaplin E, Gardiner N, Singh SJ. Early experiences of rehabilitation for individuals post-COVID to improve fatigue, breathlessness exercise capacity and cognition - A cohort study. Chron Respir Dis. 2021;18:14799731211015691. doi: 10.1177/14799731211015691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Spielmanns M, Pekacka-Egli AM, Schoendorf S, Windisch W, Hermann M. Effects of a Comprehensive Pulmonary Rehabilitation in Severe Post-COVID-19 Patients. Int J Environ Res Public Health. 2021;18(5):2695. doi: 10.3390/ijerph18052695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zampogna E, Paneroni M, Belli S, Aliani M, Gandolfo A, Visca D, et al. Pulmonary Rehabilitation in Patients Recovering from COVID-19. Respiration. 2021;100(5):416–22. doi: 10.1159/000514387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N Engl J Med. 2020;382(18):1708–20. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ali AM, Kunugi H. Skeletal Muscle Damage in COVID-19:A Call for Action. Medicina (Kaunas) 2021;57(4):372. doi: 10.3390/medicina57040372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Welch C, Greig C, Masud T, Wilson D, Jackson TA. COVID-19 and Acute Sarcopenia. Aging Dis. 2020;11(6):1345–51. doi: 10.14336/AD.2020.1014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.De Andrade-Junior MC, de Salles ICD, de Brito CMM, Pastore-Junior L, Righetti RF, Yamaguti WP. Skeletal Muscle Wasting and Function Impairment in Intensive Care Patients With Severe COVID-19. Front Physiol. 2021;12:640973. doi: 10.3389/fphys.2021.640973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lang T, Streeper T, Cawthon P, Baldwin K, Taaffe DR, Harris TB. Sarcopenia:etiology, clinical consequences, intervention, and assessment. Osteoporos Int. 2010;21(4):543–59. doi: 10.1007/s00198-009-1059-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Reijnierse EM, Trappenburg MC, Leter MJ, Blauw GJ, de van der Schueren MA, Meskers CG, et al. The Association between Parameters of Malnutrition and Diagnostic Measures of Sarcopenia in Geriatric Outpatients. PLoS One. 2015;10(8):e0135933. doi: 10.1371/journal.pone.0135933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Paneroni M, Simonelli C, Saleri M, Bertacchini L, Venturelli M, Troosters T, et al. Muscle Strength and Physical Performance in Patients Without Previous Disabilities Recovering From COVID-19 Pneumonia. Am J Phys Med Rehabil. 2021;100(2):105–9. doi: 10.1097/PHM.0000000000001641. [DOI] [PubMed] [Google Scholar]
- 23.Gerard M, Mahmutovic M, Malgras A, Michot N, Scheyer N, Jaussaud R, et al. Long-Term Evolution of Malnutrition and Loss of Muscle Strength after COVID-19:A Major and Neglected Component of Long COVID-19. Nutrients. 2021;13(11):3964. doi: 10.3390/nu13113964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Welch C, KH-Z S, C AG, J ML, T AJ. Acute Sarcopenia Secondary to Hospitalisation - An Emerging Condition Affecting Older Adults. Aging Dis. 2018;9(1):151–64. doi: 10.14336/AD.2017.0315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bandy WD, Lovelace-Chandler V, McKitrick-Bandy B. Adaptation of skeletal muscle to resistance training. J Orthop Sports Phys Ther. 1990;12(6):248–55. doi: 10.2519/jospt.1990.12.6.248. [DOI] [PubMed] [Google Scholar]
- 26.Tipping CJ, Harrold M, Holland A, Romero L, Nisbet T, Hodgson CL. The effects of active mobilisation and rehabilitation in ICU on mortality and function:a systematic review. Intensive Care Med. 2017;43(2):171–83. doi: 10.1007/s00134-016-4612-0. [DOI] [PubMed] [Google Scholar]
- 27.Zhang L, Hu W, Cai Z, Liu J, Wu J, Deng Y, et al. Early mobilization of critically ill patients in the intensive care unit:A systematic review and meta-analysis. PLoS One. 2019;14(10):e0223185. doi: 10.1371/journal.pone.0223185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ortiz-Alonso J, Bustamante-Ara N, Valenzuela PL, Vidan-Astiz M, Rodriguez-Romo G, Mayordomo-Cava J, et al. Effect of a Simple Exercise Program on Hospitalization-Associated Disability in Older Patients:A Randomized Controlled Trial. J Am Med Dir Assoc. 2020;21(4):531–7.e1. doi: 10.1016/j.jamda.2019.11.027. [DOI] [PubMed] [Google Scholar]
- 29.Troosters T, Probst VS, Crul T, Pitta F, Gayan-Ramirez G, Decramer M, et al. Resistance training prevents deterioration in quadriceps muscle function during acute exacerbations of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2010;181((10)):1072–7. doi: 10.1164/rccm.200908-1203OC. [DOI] [PubMed] [Google Scholar]
- 30.Liao WH, Chen JW, Chen X, Lin L, Yan HY, Zhou YQ, et al. Impact of Resistance Training in Subjects With COPD:A Systematic Review and Meta-Analysis. Respir Care. 2015;60(8):1130–45. doi: 10.4187/respcare.03598. [DOI] [PubMed] [Google Scholar]
- 31.Kongsgaard M, Backer V, Jorgensen K, Kjaer M, Beyer N. Heavy resistance training increases muscle size, strength and physical function in elderly male COPD-patients--a pilot study. Respir Med. 2004;98(10):1000–7. doi: 10.1016/j.rmed.2004.03.003. [DOI] [PubMed] [Google Scholar]
- 32.Perry BG, Lucas SJE. The Acute Cardiorespiratory and Cerebrovascular Response to Resistance Exercise. Sports Med Open. 2021;7(1):1–19. doi: 10.1186/s40798-021-00314-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Houchen-Wolloff L, Sandland CJ, Harrison SL, Menon MK, Morgan MD, Steiner MC, et al. Ventilatory requirements of quadriceps resistance training in people with COPD and healthy controls. Int J Chron Obstruct Pulmon Dis. 2014;9:589–95. doi: 10.2147/COPD.S59164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Probst VS, Troosters T, Pitta F, Decramer M, Gosselink R. Cardiopulmonary stress during exercise training in patients with COPD. Eur Respir J. 2006;27(6):1110–8. doi: 10.1183/09031936.06.00110605. [DOI] [PubMed] [Google Scholar]
- 35.Rice H, Harrold M, Fowler R, Watson C, Waterer G, Hill K. Exercise training for adults hospitalized with an acute respiratory condition:a systematic scoping review. Clin Rehabil. 2020;34(1):45–55. doi: 10.1177/0269215519877930. [DOI] [PubMed] [Google Scholar]
- 36.Beauchamp MK, Nonoyama M, Goldstein RS, Hill K, Dolmage TE, Mathur S, et al. Interval versus continuous training in individuals with chronic obstructive pulmonary disease--a systematic review. Thorax. 2010;65(2):157–64. doi: 10.1136/thx.2009.123000. [DOI] [PubMed] [Google Scholar]
- 37.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, et al. Clinical Characteristics of 138 Hospitalized Patients With 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA. 2020;323(11):1061–9. doi: 10.1001/jama.2020.1585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Zhou F, Yu T, Du R, Fan G, Liu Y, Liu Z, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China:a retrospective cohort study. Lancet. 2020;395(10229):1054–62. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fan E, Cheek F, Chlan L, Gosselink R, Hart N, Herridge MS, et al. An official American Thoracic Society Clinical Practice guideline:the diagnosis of intensive care unit-acquired weakness in adults. Am J Respir Crit Care Med. 2014;190(12):1437–46. doi: 10.1164/rccm.201411-2011ST. [DOI] [PubMed] [Google Scholar]
- 40.Bolton CE, Bevan-Smith EF, Blakey JD, Crowe P, Elkin SL, Garrod R, et al. British Thoracic Society guideline on pulmonary rehabilitation in adults. Thorax. 2013;68(Suppl 2):ii1–30. doi: 10.1136/thoraxjnl-2013-203808. [DOI] [PubMed] [Google Scholar]
- 41.Ahmadi, Hekmatikar AH, Ferreira Junior JB, Shahrbanian S, Suzuki K. Functional and Psychological Changes after Exercise Training in Post-COVID-19 Patients Discharged from the Hospital:A PRISMA-Compliant Systematic Review. Int J Environ Res Public Health. 2022;19(4):2290. doi: 10.3390/ijerph19042290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gobbi M, Bezzoli E, Ismelli F, Trotti G, Cortellezzi S, Meneguzzo F, et al. Skeletal Muscle Mass, Sarcopenia and Rehabilitation Outcomes in Post-Acute COVID-19 Patients. J Clin Med. 2021;10(23):5623. doi: 10.3390/jcm10235623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Nambi G, Abdelbasset WK, Alrawaili SM, Elsayed SH, Verma A, Vellaiyan A, et al. Comparative effectiveness study of low versus high-intensity aerobic training with resistance training in community-dwelling older men with post-COVID 19 sarcopenia:A randomized controlled trial. Clin Rehabil. 2022;36(1):59–68. doi: 10.1177/02692155211036956. [DOI] [PubMed] [Google Scholar]
- 44.Barbara C, Clavario P, De Marzo V, Lotti R, Guglielmi G, Porcile A, et al. Effects of exercise rehabilitation in patients with long coronavirus disease 2019. Eur J Prev Cardiol. 2022;29(7):e258–e60. doi: 10.1093/eurjpc/zwac019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Medrinal C, Prieur G, Bonnevie T, Gravier FE, Mayard D, Desmalles E, et al. Muscle weakness, functional capacities and recovery for COVID-19 ICU survivors. BMC Anesthesiol. 2021;21(1):64. doi: 10.1186/s12871-021-01274-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Udina C, Ars J, Morandi A, Vilaro J, Caceres C, Inzitari M. Rehabilitation in adult post-COVID-19 patients in post-acute care with Therapeutic Exercise. J Frailty Aging. 2021;10(3):297–300. doi: 10.14283/jfa.2021.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Piquet V, Luczak C, Seiler F, Monaury J, Martini A, Ward AB, et al. Do Patients With COVID-19 Benefit from Rehabilitation?Functional Outcomes of the First 100 Patients in a COVID-19 Rehabilitation Unit. Arch Phys Med Rehabil. 2021;102(6):1067–74. doi: 10.1016/j.apmr.2021.01.069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Ortega F, Toral J, Cejudo P, Villagomez R, Sanchez H, Castillo J, et al. Comparison of effects of strength and endurance training in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2002;166(5):669–74. doi: 10.1164/rccm.2107081. [DOI] [PubMed] [Google Scholar]
- 49.Silva C, Gomes Neto M, Saquetto MB, Conceicao CSD, Souza-Machado A. Effects of upper limb resistance exercise on aerobic capacity, muscle strength, and quality of life in COPD patients:a randomized controlled trial. Clin Rehabil. 2018;32(12):1636–44. doi: 10.1177/0269215518787338. [DOI] [PubMed] [Google Scholar]
- 50.Spruit MA, Gosselink R, Troosters T, De Paepe K, Decramer M. Resistance versus endurance training in patients with COPD and peripheral muscle weakness. Eur Respir J. 2002;19(6):1072–8. doi: 10.1183/09031936.02.00287102. [DOI] [PubMed] [Google Scholar]
- 51.Vonbank K, Strasser B, Mondrzyk J, Marzluf BA, Richter B, Losch S, et al. Strength training increases maximum working capacity in patients with COPD-randomized clinical trial comparing three training modalities. Respir Med. 2012;106(4):557–63. doi: 10.1016/j.rmed.2011.11.005. [DOI] [PubMed] [Google Scholar]
- 52.Zambom-Ferraresi F, Cebollero P, Gorostiaga EM, Hernandez M, Hueto J, Cascante J, et al. Effects of Combined Resistance and Endurance Training Versus Resistance Training Alone on Strength, Exercise Capacity, and Quality of Life in Patients With COPD. J Cardiopulm Rehabil Prev. 2015;35(6):446–53. doi: 10.1097/HCR.0000000000000132. [DOI] [PubMed] [Google Scholar]
- 53.Morrow A, Gray SR, Bayes HK, Sykes R, McGarry E, Anderson D, et al. Prevention and early treatment of the long-term physical effects of COVID-19 in adults:design of a randomised controlled trial of resistance exercise-CISCO-21. Trials. 2022;23(1):660. doi: 10.1186/s13063-022-06632-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ramirez-Velez R, Oteiza J, de Tejerina J, Garcia-Alonso N, Legarra-Gorgonon G, Oscoz-Ochandorena S, et al. Resistance training and clinical status in patients with postdischarge symptoms after COVID-19:protocol for a randomized controlled crossover trial “The EXER-COVID Crossover Study”. Trials. 2022;23(1):643. doi: 10.1186/s13063-022-06608-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kontopoulou S, Daniil Z, Gourgoulianis KI, Kotsiou OS. Exercise Preferences and Benefits in Patients Hospitalized with COVID-19. J Pers Med. 2022;12(4):645. doi: 10.3390/jpm12040645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hill KD, Hunter SW, Batchelor FA, Cavalheri V, Burton E. Individualized home-based exercise programs for older people to reduce falls and improve physical performance:A systematic review and meta-analysis. Maturitas. 2015;82(1):72–84. doi: 10.1016/j.maturitas.2015.04.005. [DOI] [PubMed] [Google Scholar]
- 57.Kis O, Buch A, Stern N, Moran DS. Minimally supervised home-based resistance training and muscle function in older adults:A meta-analysis. Arch Gerontol Geriatr. 2019;84:103909. doi: 10.1016/j.archger.2019.103909. [DOI] [PubMed] [Google Scholar]
- 58.Vitale JA, Bonato M, Borghi S, Messina C, Albano D, Corbetta S, et al. Home-Based Resistance Training for Older Subjects during the COVID-19 Outbreak in Italy:Preliminary Results of a Six-Months RCT. Int J Environ Res Public Health. 2020;17(24):9533. doi: 10.3390/ijerph17249533. [DOI] [PMC free article] [PubMed] [Google Scholar]


