Abstract
Context:
When caring for an adolescent client, providers of contraceptive services must consider whether and how to encourage parent/guardian–child communication about the adolescent’s reproductive health. The objective of this systematic review was to summarize the evidence on the effectiveness of programs designed to increase parent–child communication about reproductive health. The review was used to inform national recommendations on quality family planning services. Data analysis occurred from mid-2011 through 2012.
Evidence acquisition:
Several electronic bibliographic databases were used to identify relevant articles, including PubMed, CINAHL, PsycINFO, and Popline, published from January 1985 through February 2011.
Evidence synthesis:
Sixteen articles met the inclusion criteria: all studies examined the impact on at least one medium- or short-term outcome, and two studies assessed the impact on teen pregnancy. One study examined the impact of a program conducted in a clinic setting; the remainder examined the impact of programs in community settings. All studies showed a positive impact on at least one short-term outcome, and 12 of 16 studies showed an increase in parent–child communication about reproductive health. Four of seven studies found an impact on sexual risk behavior.
Conclusions:
Most programs increased parent–child communication, and several resulted in reduced sexual risk behavior of adolescents. This suggests that delivering a clinic-based program that effectively helps parents/guardians talk to their adolescent child(ren) about reproductive health, or referring parents/guardians to an evidence-based program in the community, may be beneficial. However, further rigorous research on delivery of these programs in clinical settings is needed.
Context
Each year in the U.S., approximately 700,000 pregnancies occur among women aged less than 20 years, and more than 300,000 give birth.1 As a result, many teen mothers attain less education and have lower incomes, and their children may experience higher rates of negative outcomes such as poorer health, lowered academic achievement, and higher rates of teen pregnancy for female children and incarceration for male children.2 Taxpayers also pay a steep price for the nation’s high rate of teen and unintended pregnancy. The cost of teen pregnancy was estimated to be more than $9 billion in 2010.3
Ensuring that sexually active adolescents have access to contraceptive services is a critically important aspect of teen pregnancy prevention. Yet, when caring for an adolescent client, providers of contraceptive services are often faced with the challenge of whether and how to encourage parent–child communication about the adolescent’s reproductive health. Research has shown that parent–child communication about reproductive health is associated with reduced sexual risk behavior.4–6 However, there are many barriers to providers’ ability to encourage parent–child communication. For example, existing research has shown that many teens report that they will not seek reproductive health services if their parents/guardians will be informed.7 Many pediatricians do not talk to parents/guardians about sexual risk reduction owing to lack of training, lack of request from parents/guardians, and feelings of awkwardness.8 Interventions that build parent–child communication, which could be used in clinical settings, may remove some of these barriers.
The objective of this systematic review was to summarize the evidence on the effectiveness of programs designed to increase parent–child communication about reproductive health. This evidence was used by CDC and the Office of Population Affairs (OPA) to develop guidelines for providing family planning services, which are published in “Recommendations for Providing Quality Family Planning Services.”9
Evidence Acquisition
The methods for conducting the systematic review have been described elsewhere.10 In summary, the review of the evidence was a multistep process that began with developing six key questions (Table 1) and applying an analytic framework to show the relationships among the population of interest (adolescents and their parents/guardians); the intervention of interest (efforts to encourage parent–child communication); and the short-, medium-, and long-term outcomes of interest (Figure 1). Short-term outcomes examined in this review included improved parental communication with adolescents about reproductive health. Medium-term outcomes of interest included adolescent sexual behaviors, such as use of contraception (the inverse of these outcomes are sexual risk behaviors such as initiation of sexual intercourse and non-use or inconsistent use of contraception). Long-term outcomes included decreased rates of pregnancy, abortion, and births among female adolescents. Search strategies were developed that included the identification of key terms (Appendix A), which were applied to several electronic databases (Appendix B) to identify potential articles to include in this systematic review.
Table 1.
Key Questions
| Key question no. | Question |
|---|---|
|
| |
| 1 | Is there a relationship between programs designed to strengthen parent–child communication and improved long-term outcomes (e.g., decreased teen and unintended pregnancies, increased birth spacing, decreased abortion rates, decreased repeat teen pregnancy rates, increase in achieving desired family size)? |
| 2 | Is there a relationship between programs designed to strengthen parent–child communication and improved medium-term outcomes (e.g., increased contraceptive use, increased use of more effective contraception, increased correct use of contraception, increased consistent use of contraception, increased continuation of contraception use, increased use of service, increased repeat/follow-up service use, increased dual-method use)? |
| 3 | Is there a relationship between programs designed to strengthen parent–child communication and improved short-term outcomes (e.g., quality/satisfaction with service, strengthened social norms, intention to use contraception, knowledge/awareness, other psychosocial determinants, intentions to use service, acceptance by the community, increased parental involvement and/or communication, increased intentions to delay sexual initiation)? |
| 4 | What are the barriers and facilitators to clinics to adopting and implementing programs designed to strengthen parent–child communication? |
| 5 | Are there unintended negative consequences associated with providing programs designed to strengthen parent–child communication? |
| 6 | What are the barriers and facilitators to adolescent clients to participating in programs designed to strengthen parent–child communication? |
Figure 1. Analytic framework for systematic review on impact of contraceptive counseling in clinical settings.
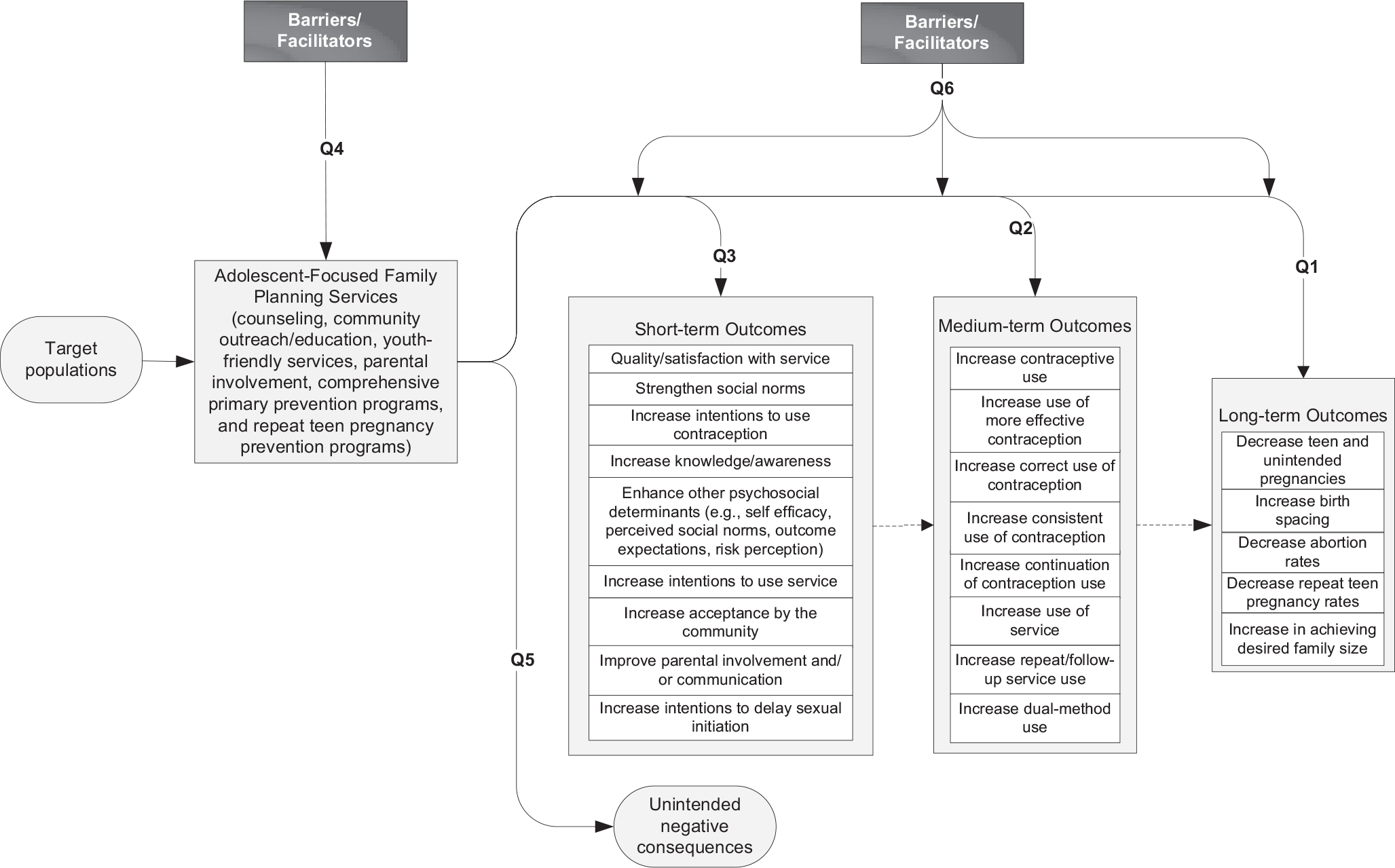
Note: The numbered lines map onto the key questions. Dashed lines show logical relationships between outcomes, but these relationships are not assessed in this systematic review.
Selection of Studies
Retrieval and inclusion criteria were developed a priori and applied to the search results. Retrieval criteria for this review were as follows: published between January 1, 1985, and February 28, 2011; published in the English language; article described a study that addressed at least one of the six key questions addressed by the evidence report; all articles were full-length (abstracts and letters to the editor did not meet the inclusion criteria); and, if the same study was reported in multiple publications, the most complete publication was the primary reference. Data analysis occurred from mid-2011 through 2012.
The inclusion criteria depended on the key question being addressed. For questions 1–3, which sought to examine the relationships between interventions to improve parent–child communication and improved long-, medium-, and short-term outcomes, case reports and program descriptions were excluded and studies had to directly determine the impact on at least one long-, medium-, or short-term outcome. We focused on studies of interventions that attempted to increase parent–child communication about reproductive health. The interventions could be conducted in either a clinical setting or a community setting to which clinic clients were referred. Articles were excluded if they focused solely on HIV/sexually transmitted infection (STI) prevention (i.e., no focus on pregnancy prevention), and if they focused solely on sex education because the effect of these programs on adolescent sexual risk behavior has already been well documented in several other systematic reviews.11–13 Further, either the studies had to include a comparison group or pre-exposure measures pertaining to the outcomes of interest or change scores (before and after) had to be available. Finally, the studies must have enrolled individuals aged between 10 and 24 years inclusive and results must be presented separately for this population. Defining adolescents as being part of the 10–24-year age group is consistent with the UN’s focus on adolescents aged 10–19 years and youth aged 15–24 years14; this definition also acknowledges recent research that has showed the brain does not finish developing until the early 20s, which can lead to increased risk behavior.15,16 For Questions 4 and 6, which sought to examine barriers and facilitators to the delivery of parent–child communication programs, articles had to also examine the impact of such a program. All summary measures reporting relevant outcomes were considered for review.
Assessment of Study Quality and Synthesis of Data
The assessment of study quality and synthesis of data has been described elsewhere.10 The articles that met all inclusion and retrieval criteria comprised the body of evidence for the systematic review. The quality of each study was assessed in accordance with the methodology developed by the U.S. Preventive Services Task Force (USPSTF).17 It included assessing the quality of each individual study to determine confounding due to systematic bias. Once the quality of each study was assessed, data were abstracted in a series of summary tables and a qualitative synthesis of the evidence was prepared. Summary measures of association were not computed across studies because of the diversity of the interventions, study designs, and populations.
Evidence Synthesis
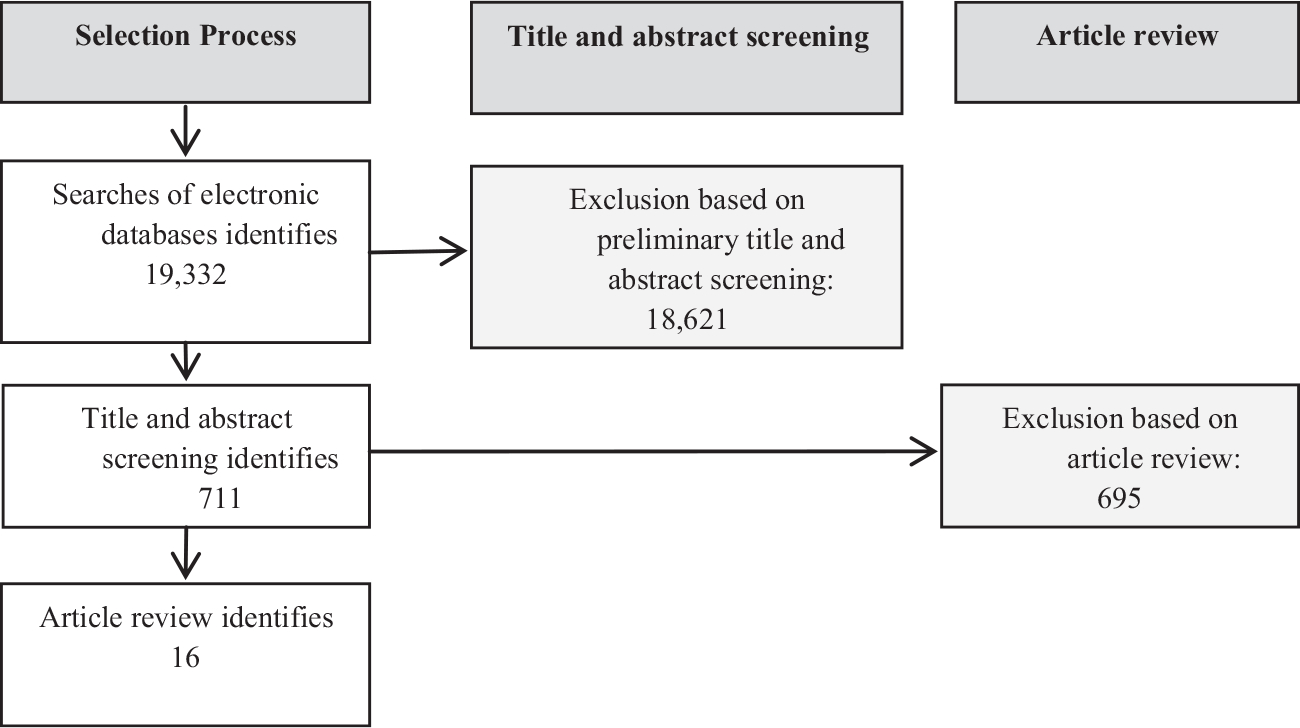
The search strategy identified 19,332 articles; after applying the retrieval criteria, 711 articles were retrieved for closer review. Sixteen articles met the inclusion criteria for parental involvement programs, and comprised the evidence base for this topic (Figure 2). All 16 studies attempted to determine if programs that increase parental involvement had an impact on at least one medium- or short-term outcome. Two of the 16 studies also assessed the impact of these programs on long-term outcomes, particularly rates of pregnancy, and one study examined barriers and facilitators related to adolescents’ use of family planning services. None of the included studies examined barriers and facilitators to clinics adopting adolescent-focused family planning services or unintended negative consequences of providing such services.
Figure 2. Flow diagram of the systematic review process for parent–child communication.
A summary overview of each of the 16 included studies is presented in Appendix C. Thirteen different interventions were assessed in the 16 included studies. Three interventions were each assessed in two different articles (i.e., Strong African American Families Program18,19; Parent-Adolescent Relationship Education20,21; and Informed Parents and Children Together22,23). Interventions varied in their level of intensity regarding parental involvement. For example, some interventions used homework that parents and adolescents would complete together as part of a larger multicomponent pregnancy prevention program, whereas other interventions were focused entirely on strengthening parental involvement, employing techniques such as multisession group programs and targeted public service announcements. Interventions also differed in their target population. Six interventions included components for both parents and adolescents, whereas seven interventions included only parental components. These components primarily consisted of a group curriculum for parents (k=12); adolescents (k=9); or both (k=7). A few implemented individual curriculums for parents alone (k=1) or with their adolescent (k=2). Five studies implemented interventions with homework or other self-administered activities. One intervention consisted of a multimedia package and another included other components, namely, physician endorsement of the intervention. All participants were adolescents or parents of adolescents aged 9–16 years. The primary settings for these studies were schools or communities. One study was conducted in clinics and one was conducted only over the Internet.
Fifteen of the studies used a RCT design (USPSTF Level I) and the remaining study used a controlled trial without randomization (USPSTF Level II-1). The included study sample sizes ranged from 50 to 2,439. The assessment of the quality of the studies found that the risk for bias in these studies varied, with three studies showing high risk for bias, two moderate to high, five moderate, and six low to moderate. The primary issues of concern included lack of blinding, recall/social desirability bias, high attrition rates, and lack of intent-to-treat analyses.
Long-Term Outcomes
The long-term outcome of reductions in teen pregnancy was examined in two studies.22,24 Stanton et al.22 found a marginally significant difference between groups on subsequent pregnancy (p ≤ 0.10). This study employed a RCT design and enrolled 817 African American adolescents aged 13–16 years living in low-income communities. Assessments were conducted at 6, 12, 18, and 24 months. Randomization occurred at the level of the 35 low-income community sites and was conducted by a random numbers table after all youths at all sites within the recruitment wave had been identified. Thirteen sites were randomized to receive the Focus On Kids intervention only, 11 to the Focus On Kids + Informed Parents and Children Together intervention, and 11 to the Focus On Kids + Informed Parents and Children Together + boosters. In another study, Anderson and colleagues24 used a clustered RCT to evaluate an intervention aimed at enhancing the active involvement of parents in their children’s family life education, but did not find a significant difference between groups in rates of pregnancy at 12-month follow-up. This study used the Reaching Adolescents and Parents intervention, which reaches out to early adolescents and their parents and was designed to increase student knowledge about puberty and human reproduction; improve communication and decision-making skills; facilitate family communication; and delay the onset of sexual activity.
A total of 405 families were recruited into the study during community meetings announced by the schools and community agencies where the program took place; schools were randomized to intervention and comparison sites in order to preserve the natural distribution of participants attending sessions in their own neighborhoods and to prevent discussion of the intervention content between participants attending sessions and participants in the comparison groups. Participants were recruited from students in Grades 5–7 who were attending summer and after-school programs and in-school classes in Los Angeles County. Almost 60% of participants were female, and multiple racial/ethnic groups were represented (21% non-Hispanic black, 46% Hispanic, and 13% non-Hispanic white). At the 12-month instrument administration, two pregnancies were reported, one in each group.
Medium-Term Outcomes
One medium-term outcome was assessed by seven studies, that is, change in sexual behavior.19,22,23,25–28 Four of these studies found an impact on sexual risk behavior.19,25–27 One of these studies was an RCT conducted in a clinic setting26; parents visiting a clinic for a school requirement with their adolescent children aged 11–14 years had a face-to-face meeting with a social work interventionist for 30 minutes, received a written manual focusing on the models of the intervention, and a booster phone call to ask if the modules has been discussed with their adolescent children using the two communication aids—a booklet and short story—they were given. Two hundred sixty-four parent–adolescent dyads were enrolled, then randomized to the treatment and control groups, and followed for 9 months. The authors reported that a statistically significant (p < 0.05) reduced rate of sexual initiation and frequency of sexual intercourse was observed among the intervention subjects compared with control subjects. Sexual activity among control subject increased from 6% to 22% while remaining at 6% among participants in the intervention group at a 9-month follow-up. The mean rating for frequency of sexual intercourse in the past 30 days was 1.08 for the intervention group and 1.53 for the control group. This difference was statistically significant (t[262]=4.06, p < 0.05).
Forehand et al.25 used an RCT to evaluate the efficacy of the “Parents Matter!” Program, a five-session parent-based sexual risk prevention program. Study participants were African American preadolescents aged 9–12 years and their parents/guardians living in the southern U.S. A total of 1,115 parent–adolescent dyads were enrolled, randomized to intervention and control groups, and followed for 12 months. Preadolescents whose parents/guardians attended all five sessions of the enhanced intervention had a likelihood of sexual risk at the 12-month follow-up of <1.00 relative to those whose parents attended the control (relative risk [RR]=0.65, 95% CI=0.41, 1.03) and single-session (RR=0.62, 95% CI=0.40, 0.97) interventions.
In the third study, Haggerty and colleagues27 used an RCT to assess the efficacy of two administrations of Parents Who Care (PWC) compared with a control group. PWC is a universal prevention program designed to prevent problem behaviors, and was delivered in two versions, a parent and adolescent (PA) group or a self-administered (SA) group. The study was conducted among a balanced sample of European American and African American youths in eighth grade and their parents. Three hundred thirty-one parent–adolescent dyads were enrolled, randomized to one of the three conditions, and followed for 2 years. ORs indicated that the chances of initiating sex were reduced by almost 70% (OR=0.31) for African American teens in the SA group compared with controls, and 75% (OR=0.25) for the African American teens in the PA group relative to controls.
In the fourth study, Murry and colleagues19 used a clustered RCT to identify the mechanisms by which intervention-induced increases in adaptive parenting were associated with a reduction in sexual risk behavior among rural African American adolescents. Participants were public fifth-grade middle school students and their parents/guardians. Three hundred thirty-two dyads were enrolled, randomized to treatment and control groups, and followed for 29 months. Researchers found that participation in the intervention led to an increase in the use of intervention-targeted parenting practices (β=0.34, p < 0.01), controlling for pretest levels of parenting practices. The increase in parenting practices was associated with an increase in adolescents’ self-pride (β=0.25, p < 0.01) with pretest levels of self-pride controlled for, which was inversely associated with peer orientation (β=−0.54, p < 0.01), and in turn was associated with intent to engage in sexual activity (β=−0.28, p < 0.01). Finally, intent was associated with engagement in sexual risk behavior (β=−0.31, p < 0.01).
Three studies22,23,28 that examined the impact of parent–child communication programs on sexual risk behavior found no difference between groups. Further, one study22 examined the impact of parent–child communication programs on the medium-term outcome of increased contraceptive use and did not find a significant difference between groups.
Short-Term Outcomes
A variety of short-term outcomes were assessed in this evidence base: parent–child communication (k=14); knowledge/awareness (k=6); psychosocial determinants (k=5); intentions to delay sexual initiation (k=5); social norms (k=1); and intentions to use contraception (k=1). All studies that measured short-term outcomes showed some positive impacts.
Twelve of the 14 studies that examined the outcome of parent–child communication found that the intervention effectively increased communication. For example, a study by Anderson and colleagues24 found that the intervention group changed significantly between pre- and post-test (p < 0.05), indicating improved communications with their parents as compared with the group that received the delayed intervention (effect size=0.019; observed power=0.59). Blake et al.29 found that students in the enhanced group reported more frequent communication with their parents than adolescents who did not receive the parent–child homework assignments (overall means 7.2 and 5.8, respectively). This difference reflects more frequent communication about prevention strategies (1.6 vs 1.0) and consequences of sexual intercourse (1.6 vs 1.1). In addition to having completed the homework assignments together, adolescents in the enhanced group, receiving the Managing the Pressures Before Marriage curriculum, talked more often with parents about the class lessons (2.5 vs 1.8). A study of rural African American families who participated in prevention programming by Brody and colleagues18 revealed the following significance levels: involved-vigilant parenting, p=0.001; racial socialization, p=0.07; communication about sex, p=0.02; and clear expectations about alcohol use, p=0.02. Consistent with the theory and hypotheses that guided this study, participants experienced increases in regulated, communicative parenting practices and youth protective factors. Evans et al.30 found that at the first follow-up, there was a significant treatment effect for increased initiation of conversations among fathers (OR=1.763, p=0.0004), but no such effect among mothers; at the second follow-up, there were significant treatment effects on recommending waiting to have sex among both fathers and mothers. Forehand and colleagues25 found that adolescents’ parents in the enhanced intervention group who attended all five sessions of the intervention had higher sexual communication and responsiveness to sexual communication compared with those who attended a single session (RR=0.62) and control participants (RR=0.65). Finally, a study by Schuster et al.31 showed an increase among intervention parents from baseline relative to controls that remained significant throughout (p < 0.001 at each follow-up), and adolescents’ ability to communicate with their parents about sexual topics significantly differed between the intervention and control groups at 3 months (mean, 4.3 vs 4.0, range, 0.1–0.5, p=0.02). Positive impacts were also found for other short-term outcomes, including knowledge/awareness, intentions to use contraceptives, and social norms.
Discussion
This systematic review identified 16 studies that examined the impact of programs designed to increase parent–child communication about reproductive health and met the inclusion criteria. Of these, 15 studies18–25,27–33 examined the impact of parent–child programs in community settings, and one study26 examined the impact of a program initiated in a clinic setting. All studies showed a positive impact on at least one short-term outcome, and 12 of 16 studies showed an increase in parent–child communication about reproductive health. Perhaps more importantly, four of seven studies found an impact on sexual risk behavior, including the one study initiated in a clinic setting.19,25–27 It is unclear whether parental involvement programs have an impact on long-term outcomes such as teen/unintended pregnancy rates, repeat teen/unintended pregnancy, and abortion rates. Two studies22,24 examined the effects of these programs on the long-term outcome rates of pregnancy, but only one found a significant difference between groups and this was marginal (p ≤ 0.10). This lack of observed impact may be explained by the low prevalence of pregnancy in this population and that the study was underpowered to detect a difference.
Several important papers have been published since our review was completed, which describe the results of studies evaluating the impact of interventions designed to strengthen parent–child communication about reproductive health.34–37 Three of the four studies used an RCT study design with low risk for bias, and the fourth used a post-test only design. All four studies found that exposure to the parenting intervention was associated with improved short-term outcomes (i.e., parent–child communication, youth’s condom use skills and self-efficacy, communication openness). These findings are consistent with those presented in this paper.
No studies reported on barriers or facilitators to implementation of parent–child communication programs, or that participation in a program to increase parent/guardian–child communication resulted in any unintended negative consequences.
It was not possible to assess how generalizable the findings are to all adolescents. The studies do not consistently provide information on family income or insurance providers, thus making it difficult to generalize on the basis of economic indices. The few studies that did provide socioeconomic information showed a wide range of income levels, with some samples consisting of predominately low-income individuals or households, whereas other samples included middle- to upper–middle class samples. The sex of adolescents included in the studies tended to be evenly split. There was also a wide range of races/ethnicities presented in these studies.
The evidence summarizing the impact of programs designed to improve parent/guardian–child communication about reproductive health has several strengths and limitations, which should be considered when interpreting the evidence. Of the 16 studies in this review, 1118–21,25–29,31,33 were determined to have a low to moderate risk for bias (i.e., higher quality) and five22–24,30,32 were determined to have a high risk for bias (i.e., lower quality). Studies were considered to be at risk for bias because of recall bias, self-report bias, attrition bias, and not using blinding or intent-to-treat analysis. All but one of the studies in this review used an RCT design.18,19,21–33 Seven studies19,21,22,24,25,27,28 followed participants for at least 12 months.
This systematic review highlights several important research gaps. Future research should more closely examine the impact of programs that are implemented in clinic settings and include the impact of the amount of time an adolescent spends alone with a provider, explore parents/guardians’ perspectives on ways to meet adolescents’ needs for reproductive health care, identify ways to engage parents/guardians without breaching the adolescent’s right to confidential services, explore the role of non-parental adults who can help provide guidance, consider programs that address parental monitoring and connectedness, and assess intervention opportunities when the parents/guardians and adolescents are in the clinic together versus when the adolescent or parent/guardian comes alone.
Conclusions
Although the body of evidence was limited in that it did not determine whether parent/guardian-child communication programs reduced rates of teen and unintended pregnancy, most studies included in this review found that the programs increased parent/guardian–child communication, and several resulted in reduced sexual risk behavior of adolescents, an important mediator both for unplanned pregnancy and STI prevention outcomes. Given the strong association between parent–child communication about reproductive health and sexual risk behavior,4–6 this review suggests that delivering a clinic-based program that helps parents/guardians talk to their adolescent child(ren) about reproductive health, or referring parents/guardians to an evidence-based program in the community, may be beneficial. However, further rigorous research on the delivery of these programs in clinical settings is needed.
Findings from this systematic review were presented to an expert technical panel in May 2011 at a meeting convened by the OPA and CDC. The information was used to inform recommendations for providing quality contraceptive counseling in the 2014 “Recommendations for Providing Quality Family Planning Services.”9 The evidence base on the impact of parent/guardian–child communication programs would be strengthened by examining the impact of programs that are implemented in clinic settings, as only one clinic-based study was identified.
Supplementary Material
Acknowledgments
Publication of this article was supported by the U.S. Centers for Disease Control and Prevention (CDC) and the Office of Population Affairs (OPA).
The findings and conclusions of this report are those of the authors and do not necessarily represent the official position of CDC or the Office of Population Affairs
No financial disclosures were reported by the authors of this paper.
Footnotes
Appendix
Supplementary data
Supplementary data associated with this article can be found at http://dx.doi.org/10.1016/j.amepre.2015.03.022.
References
- 1.Ventura S, Curtin S, Abma J, Henshaw S. Estimated pregnancy rates and rates of pregnancy outcomes for the United States, 1990–2008. Natl Vital Stat Rep. 2012;60(7). [PubMed] [Google Scholar]
- 2.Hoffman S, Maynard R. Kids Having Kids: Economic Costs and Social Consequences of Teen Pregnancy, 2nd ed., Washington, DC: Urban Institute Press; 2008. [Google Scholar]
- 3.Hoffman S Counting It Up: The Public Costs of Teen Childbearing. Washington, DC: The National Campaign to Prevent Teen and Unplanned Pregnancy; 2010. [Google Scholar]
- 4.Markham CM, Lormand D, Gloppen KM, et al. Connectedness as a predictor of sexual and reproductive health outcomes for youth. J Adolesc Health. 2010;46(3 suppl):S23–S41. 10.1016/j.jadohealth.2009.11.214. [DOI] [PubMed] [Google Scholar]
- 5.Miller BC. Family influences on adolescent sexual and contraceptive behavior. J Sex Res. 2002;39(1):22–26. 10.1080/00224490209552115. [DOI] [PubMed] [Google Scholar]
- 6.Rupp R, Rosenthal SL. Parental influences on adolescent sexual behaviors. Adoles Med State Art Rev. 2007;18(3):460–470, vi. [PubMed] [Google Scholar]
- 7.Reddy D, Fleming R, Swain C. Effect of mandatory parental notification on adolescent girls’ use of sexual health care services. JAMA. 2002;288(6):710–714. 10.1001/jama.288.6.710. [DOI] [PubMed] [Google Scholar]
- 8.Miller K, Wyckoff S, Lin C, Whitaker D, Sukalack T, Fowler M. Pediatricians’ role and practices regarding provision of guidance about sexual risk reduction to parents. J Prim Prev. 2008;29:279–291. 10.1007/s10935-008-0137-9. [DOI] [PubMed] [Google Scholar]
- 9.CDC, Office of Population Affairs. Providing quality family planning services: recommendations of CDC and the U.S. Office of Population Affairs. MMWR Recomm Rep. 2014;63(RR04):1–29. [PubMed] [Google Scholar]
- 10.Tregear SJ, Gavin LE, Williams JR. Systematic review evidence methodology: providing quality family planning services. Am J Prev Med. 2015;49(2S1):S23–S30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kirby D Comprehensive sex education: strong public support and persuasive evidence of impact, but little funding. Arch Pediatr Adolesc Med. 2006; 160(11):1182–1184. 10.1001/archpedi.160.11.1182. [DOI] [PubMed] [Google Scholar]
- 12.Kirby DB, Laris BA, Rolleri LA. Sex and HIV education programs: their impact on sexual behaviors of young people throughout the world. J Adolesc Health. 2007;40(3):206–217. 10.1016/j.jadohealth.2006.11.143. [DOI] [PubMed] [Google Scholar]
- 13.Oringanje C, Meremikwu MM, Eko H, Esu E, Meremikwu A, Ehiri JE. Interventions for preventing unintended pregnancies among adolescents. Cochrane Database Syst Rev. 2009;(4):CD005215. 10.1002/14651858.CD005215.pub2. [DOI] [PubMed] [Google Scholar]
- 14.UN General Assembly. International Youth Year: Participation, Development, Peace: Report of the Secretary-General. New York: United Nations; 1981. [Google Scholar]
- 15.Casey BJ, Getz S, Galvan A. The adolescent brain. Dev Rev. 2008;28 (1):62–77. 10.1016/j.dr.2007.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Spear LP. The adolescent brain and age-related behavioral manifestations. Neurosci BioBehav Rev. 2000;24(4):417–463. 10.1016/S0149-7634(00)00014-2. [DOI] [PubMed] [Google Scholar]
- 17.Harris RP, Helfand M, Woolf SH, et al. Current methods of the U.S. Preventive Services Task Force: a review of the process. Am J Prev Med. 2001;20(3 suppl):21–35. 10.1016/S0749-3797(01)00261-6. [DOI] [PubMed] [Google Scholar]
- 18.Brody GH, Murry VM, Gerrard M, et al. The Strong African American Families Program: translating research into prevention programming. Child Dev. 2004;75(3):900–917. 10.1111/j.1467-8624.2004.00713.x. [DOI] [PubMed] [Google Scholar]
- 19.Murry VM, Berkel C, Brody GH, Gerrard M, Gibbons FX. The Strong African American Families program: longitudinal pathways to sexual risk reduction. J Adolesc Health. 2007;41(4):333–342. 10.1016/j.jadohealth.2007.04.003. [DOI] [PubMed] [Google Scholar]
- 20.Lederman RP, Chan W, Roberts-Gray C. Sexual risk attitudes and intentions of youth aged 12–14 years: survey comparisons of parent-teen prevention and control groups. Behav Med. 2004;29(4):155–163. 10.3200/BMED.29.4.155-166. [DOI] [PubMed] [Google Scholar]
- 21.Lederman RP, Chan W, Roberts-Gray C. Parent-adolescent relationship education (PARE): program delivery to reduce risks for adolescent pregnancy and STDs. Behav Med. 2008;33(4):137–143. 10.3200/BMED.33.4.137-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Stanton B, Cole M, Galbraith J, et al. Randomized trial of a parent intervention: parents can make a difference in long-term adolescent risk behaviors, perceptions, and knowledge. Arch Pediatr Adolesc Med. 2004;158(10):947–955. 10.1001/archpedi.158.10.947. [DOI] [PubMed] [Google Scholar]
- 23.Stanton BF, Li X, Galbraith J, et al. Parental underestimates of adolescent risk behavior: a randomized, controlled trial of a parental monitoring intervention. J Adolesc Health. 2000;26(1):18–26. 10.1016/S1054-139X(99)00022-1. [DOI] [PubMed] [Google Scholar]
- 24.Anderson NLR, Koniak-Griffin D, Keenan CK, Uman G, Duggal BR, Casey C. Evaluating the outcomes of parent-child family life education… including commentary by Hayman LL. Sch Inq Nurs Pract. 1999;13(3):211–238. [PubMed] [Google Scholar]
- 25.Forehand R, Armistead L, Long N, et al. Efficacy of a parent-based sexual-risk prevention program for African American preadolescents: a randomized controlled trial. Arch Pediatr Adolesc Med. 2007;161 (12):1123–1129. 10.1001/archpedi.161.12.1123. [DOI] [PubMed] [Google Scholar]
- 26.Guilamo-Ramos V, Bouris A, Jaccard J, Gonzalez B, McCoy W, Aranda D. A parent-based intervention to reduce sexual risk behavior in early adolescence: building alliances between physicians, social workers, and parents. J Adolesc Health. 2011;48(2):159–163. 10.1016/j.jadohealth.2010.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Haggerty KP, Skinner ML, MacKenzie EP, Catalano RF. A randomized trial of Parents Who Care: effects on key outcomes at 24-month follow-up. Prev Sci. 2007;8(4):249–260. 10.1007/s11121-007-0077-2. [DOI] [PubMed] [Google Scholar]
- 28.Miller BC, Norton MC, Jenson GO. Pregnancy prevention programs: impact evaluation of facts and feelings: a home-based video sex education curriculum. Family Relations. 1993;42(4):392–400. 10.2307/585339. [DOI] [Google Scholar]
- 29.Blake SM, Simkin L, Ledsky R, Perkins C, Calabrese JM. Effects of a parent-child communications intervention on young adolescents’ risk for early onset of sexual intercourse. Fam Plann Perspect. 2001;33 (2):52–61. 10.2307/2673750. [DOI] [PubMed] [Google Scholar]
- 30.Evans WD, Davis KC, Ashley OS, Blitstein J, Koo H, Zhang Y. Efficacy of abstinence promotion media messages: findings from an online randomized trial. J Adolesc Health. 2009;45(4):409–416. 10.1016/j.jadohealth.2009.02.014. [DOI] [PubMed] [Google Scholar]
- 31.Schuster MA, Corona R, Elliott MN, et al. Evaluation of Talking Parents, Healthy Teens, a new worksite based parenting programme to promote parent-adolescent communication about sexual health: randomised controlled trial. BMJ. 2008;337:a308. 10.1136/bmj.39609.657581.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Huston RL, Martin LJ, Foulds DM. Effect of a program to facilitate parent-child communication about sex. Clin Pediatr. 1990;29(11):626–633. 10.1177/000992289002901101. [DOI] [PubMed] [Google Scholar]
- 33.Lefkowitz ES, Sigman M, Au TK. Helping mothers discuss sexuality and AIDS with adolescents. Child Dev. 2000;71(5):1383–1394. 10.1111/1467-8624.00234. [DOI] [PubMed] [Google Scholar]
- 34.Guilamo-Ramos V, Jaccard J, Dittus P, et al. A comparative study of interventions for delaying the initiation of sexual intercourse among Latino and black youth. Perspect Sex Reprod Health. 2011;43(4): 247–254. 10.1363/4324711. [DOI] [PubMed] [Google Scholar]
- 35.Prado G, Pantin H, Huang S, et al. Effects of a family intervention in reducing HIV risk behaviors among high-risk Hispanic adolescents: a randomized controlled trial. Arch Pediatr Adolesc Med. 2012;166(2):127–133. 10.1001/archpediatrics.2011.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wang XX, Ying P, Diao F, et al. Altered protein prenylation in Sertoli cells is associated with adult infertility resulting from childhood mumps infection. J Exp Med. 2013;210(8):1559–1574. 10.1084/jem.20121806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Weekes CV, Haas BK, Gosselin KP. Expectations and self-efficacy of African American parents who discuss sexuality with their adolescent sons: an intervention study. Public Health Nurs. 2014;31(3):253–261. 10.1111/phn.12084. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


