Abstract
Background
Adipokines are hormones secreted from adipose tissue and are associated with cardiometabolic diseases (CMD). Functional differences between adipokines (leptin, adiponectin, and resistin) are known, but inconsistently reported associations with CMD and lack of studies in Hispanic populations are research gaps. We investigated the relationship between subclinical atherosclerosis and multiple adipokine measures.
Methods
Cross-sectional data from the Cameron County Hispanic Cohort (N = 624; mean age = 50; Female = 70.8%) were utilized to assess associations between adipokines [continuous measures of adiponectin, leptin, resistin, leptin-to-adiponectin ratio (LAR), and adiponectin-resistin index (ARI)] and early atherosclerosis [carotid-intima media thickness (cIMT)]. We adjusted for sex, age, body mass index (BMI), smoking status, cytokines, fasting blood glucose levels, blood pressure, lipid levels, and medication usage in the fully adjusted linear regression model. We conducted sexes-combined and sex-stratified analyses to account for sex-specificity and additionally tested whether stratification of participants by their metabolic status (metabolically elevated risk for CMD as defined by having two or more of the following conditions: hypertension, dyslipidemia, insulin resistance, and inflammation vs. not) influenced the relationship between adipokines and cIMT.
Results
In the fully adjusted analyses, adiponectin, leptin, and LAR displayed significant interaction by sex (p < 0.1). Male-specific associations were between cIMT and LAR [β(SE) = 0.060 (0.016), p = 2.52 × 10–4], and female-specific associations were between cIMT and adiponectin [β(SE) = 0.010 (0.005), p = 0.043] and ARI [β(SE) = − 0.011 (0.005), p = 0.036]. When stratified by metabolic health status, the male-specific positive association between LAR and cIMT was more evident among the metabolically healthy group [β(SE) = 0.127 (0.015), p = 4.70 × 10–10] (p for interaction by metabolic health < 0.1). However, the female-specific associations between adiponectin and cIMT and ARI and cIMT were observed only among the metabolically elevated risk group [β(SE) = 0.014 (0.005), p = 0.012 for adiponectin; β(SE) = − 0.015 (0.006), p = 0.013 for ARI; p for interaction by metabolic health < 0.1].
Conclusion
Associations between adipokines and cIMT were sex-specific, and metabolic health status influenced the relationships between adipokines and cIMT. These heterogeneities by sex and metabolic health affirm the complex relationships between adipokines and atherosclerosis.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12933-023-01968-4.
Keywords: Adipokines, Carotid intima-media thickness, Cardiometabolic health, Sex-differences, Population-based cohort, Mexican–American, Health disparities
Background
Adipokines are hormones secreted from adipose tissue that have regulatory functions related to inflammatory and metabolic processes [1]. The molecular interactions of adipokines are susceptible to metabolic perturbations from chronic diseases such as obesity and cardiometabolic diseases (CMD), which suggests that adipokines may influence and be influenced by pathophysiological actions [2]. Among the diverse spectrum of adipokines, the roles of adiponectin and leptin are well-studied in the context of CMD development, but less so for resistin [3]. Generally, adiponectin protects against CMD risk as it is associated with anti-inflammatory pathways [4]. Leptin has been linked to both protective and proatherogenic states [5, 6], which is contingent on the integrity of leptin signaling. On the other hand, resistin has been more consistently implicated in cardiovascular disease (CVD) and pro-inflammatory states [7].
Among the plethora of CVD complications that have been associated with adipokine profile shifts, atherosclerosis, assessed using carotid intima-media thickness (cIMT), has been associated with decreased levels of adiponectin [8–10]. On the other hand, elevated leptin [11–13] and resistin [14–16] have been implicated in increased cIMT [14–16]. Emerging markers of adipose tissue function, leptin/adiponectin ratio (LAR) [or adiponectin/leptin ratio (ALR)] [17, 18] and adiponectin-resistin index (ARI) [19], have also been associated with cIMT [14, 20]. Thus, the role of adipokines in abnormal cIMT are still considerably inconsistent in the literature [8, 20–22].
Other notable research gaps include a lack of studies in Hispanic/Latino populations, inconsistent associations of adipokines and CMD by sex [23, 24], and inadequate consideration of pertinent CVD covariates [25], such as CMD related traits [26]. As there is heterogeneity in the clinical manifestation of CMD traits across racial groups and by sex, more population directed research is warranted.
In this study, we investigated the relationship between an early measure of subclinical atherosclerosis, cIMT, and adipokine levels, specifically adiponectin, leptin, and resistin, in a Hispanic/Latino cohort. We tested associations with two additional composite indices of adipose tissue function, LAR and ARI. We hypothesized that lower adiponectin levels would be associated with elevated cIMT, whereas higher leptin (and LAR), resistin (and ARI) would be associated with elevated cIMT in Hispanic/Latinos.
Methods
Study population
The Cameron County Hispanic Cohort (CCHC), initiated in 2004, is an ongoing community-based cohort study of Mexican Americans in Brownsville, TX. Households from the U.S. census tract/block were randomly ascertained through a two-stage sampling method. To date, more than 5000 individuals have been recruited, and demographic, lifestyle, and clinical factors were extensively examined by questionnaires, clinical examinations, and biospecimen collection. From the full cohort (N = 5020), we excluded participants from the pediatric study (age < 18 years; N = 392) and participants without exposure or outcome measures (N = 3815). We additionally excluded those who reported to have major cardiovascular events (i.e., heart attack and stroke) or a carotid endarterectomy (N = 26), were without genetic data (N = 24), whose adipokine levels or cytokine levels (as a covariate) were considered biologically implausible (as described in the following section) (N = 8), or missing covariates in primary analyses (N = 127). Ultimately, a total of 624 participants were included in the analysis. Adipokine typing began many years after the cohort began in 2004 thereby explaining the smaller sample size of this study (624 from a total cohort of 5020), yet distribution of age, sex, and BMI across participants in the sub-study were comparable to all CCHC participants. (Additional file 1: Table S3).
Measures and definitions
Exposure
Circulating adipokines levels (explanatory variables)—adiponectin (ug/mL), leptin (ng/mL), and resistin (ng/mL)—and cytokines (covariates), including Interleukin-6 (IL-6; pg/mL), Interleukin-1 Beta (IL-1β; pg/mL), Interleukin-8 (IL-8; pg/mL), and Tumor Necrosis Factor-alpha (TNF-α; pg/mL), were assessed using the multiplex enzyme-linked immunosorbent assays (ELISA) (Milliplex Map, Millipore, CA) with two separate panels for different adipokines and cytokines [27]. Plasam samples were coated with analyte-specific antibody beads and analyzed using the Luminex 200 platform (Luminex Corp, Austin, TX) [27, 28]. We excluded abnormally high adiponectin measures (> 200 ug/mL) (N = 7) from our analysis as these values were biologically implausible and/or reflective of measurement errors in the assays. In addition, to avoid the biased estimation due to a few outliers, we winsorized the outliers of each adipokine (< 5% or > 95% of each adipokine measure). To carefully evaluate the potential influence of the outliers on the association between adipokines and cIMT, we performed multiple sensitivity analyses taking different approaches to treat the outliers (Additional file 1: Table S2). In addition to the three single adipokine measures (adiponectin, leptin, and resistin levels), two composite adipokine indices—LAR and ARI—were derived. LAR was calculated by dividing leptin levels (ng/mL) by adiponectin levels (ug/mL). ARI was calculated by applying a formulated index, [1 + log10(resistin levels (ng/mL)) − log10(adiponectin levels (ug/mL))], per previous derivations in the literature [19].
Outcome
Carotid ultrasound was conducted to assess subclinical atherosclerosis using the Siemens Acuson X300 ultrasound system (Malvern, PA) with a VF 13–5 linear array transducer, as previously described [29]. The implemented protocol aligned with the consensus statement on the application of carotid ultrasound for capturing subclinical vascular disease by the American Society of Echocardiography [30]. A total of 6 images of common arteries—i.e., anterior, lateral, and posterior images of left and right common carotid arteries—were taken. The cIMT measurements were ascertained with Carotid Analyzer software (Medical Imaging Applications, Coralville, IA), a semi-automated border detection program. Measurements were obtained at the R-wave of the electrocardiogram and on a minimum of 2 clips from each side. Continuous average cIMT measures in millimeters were recorded [30] and used in the current analysis.
Covariates
Measured weight (kg) and height (m) included in calculations of the body mass index (BMI; kg/m2) for participants. Information on smoking history (> 100 cigarettes in a lifetime) was collected. Fasting blood cytokine levels (IL-6, IL-1β, IL-8, and TNF-α) were measured through multiplex ELISA (Milliplex Map, Millipore, CA) along with adipokine levels. Glucose tolerance status was assessed with HbA1c and fasting blood glucose levels (FBG) (HbA1c < 5.7% and FBG < 100 mg/dL for normal), and normal or high blood pressure (BP) status was assessed via systolic blood pressure (SBP) and diastolic blood pressure (DBP) (SBP < 120 mmHg and DBP < 80 mmHg for normal BP). Lipid levels were stratified via high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), and triglyceride (TG) levels. (HDL-C 40 mg/dL in males or 50 mg/dL in females, LDL-C < 160 mg/dL, and TG < 200 mg/dL, were considered normal). Type 2 Diabetes (T2D), hypertension, and lipid-lowering medication status were collected. In our post hoc investigation, participants were further classified into two groups based on their metabolic health status—metabolically elevated risk or metabolically healthy. As implemented in a previous study [29], the metabolically elevated risk group was defined as having at least two of the following components—(1) SBP ≥ 130 mmHg or DBP ≥ 85 mmHg or taking antihypertensive medication; (2) TG ≥ 150 mg/dL; (3) HDL < 40 mg/dL in males or < 50 mg/dL in females; (4) FBG ≥ 100 mg/dL or taking hypoglycemic medication; (5) Homeostatic Model Assessment for Insulin Resistance (HOMA-IR) > 5.13; or (6) C-reactive protein (CRP) > 3 mg/L. Multiple imputations by chained equations were conducted to impute missing CRP measures (N = 308) and HOMA-IR measures (N = 9) based on all the measured variables included in the fully adjusted model using Predictive Mean Matching approach in mice R package (10 imputations were performed).
Kinship matrix
We accounted for the genetic relatedness structure in CCHC participants by adjusting for a familial relationship (calculated as a kinship matrix) when estimating the association between adipokine levels and cIMT. We leveraged participants’ genome-wide genotype information to generate a kinship matrix using the GENESIS R package. Participants were genotyped on the MEGA-EX Array panel at the Vanderbilt University Medical Center Genotyping core facility, VANTAGE and undergone standard quality control processes (i.e., filtering the variants or samples with variant call rate < 90%, minor allele frequency < 0.01, sample or variant missing rate > 5%, deviation from Hardy–Weinberg Equilibrium (p < 1 × 10−10) as well as checks for heterozygosity and sex). A total of 182,799 single nucleotide polymorphisms were used in generating the kinship matrix.
Statistical analysis
Descriptive summary statistics of variables were calculated as a mean and a standard deviation for continuous variables and the count and percentage for categorical variables using SAS 9.4 (SAS Institute Inc., Cary, NC). We performed a linear mixed effects model to test the association between continuous cIMT measures and adipokines, while accounting for the relatedness among CCHC participants with the kinship matrix included as a random effect. Explanatory variables were three single adipokine levels (adiponectin, leptin, and resistin) and two composite adipokine indices (LAR and ARI), and each explanatory variable was included in each regression model separately. Other covariates, described below, were included as fixed effects in the linear mixed-effect model. The linear mixed-effect model was implemented using the lme4qtl package in R.
We ran linear mixed-effect regression models and assessed covariate effects by adding up the group of covariates as followed: (1) demographic variables (age and sex), (2) lifestyle variables (BMI and smoking status), (3) cytokines (IL-1β, IL-6, TNF-α, and IL-8), (4) metabolic profile (normal vs. elevated risk in glycemic, blood pressure, lipid profile), and (5) medication status (T2D, hypertension, and lipid-lowering medication). Thus, the covariates in each model are age, sex in Model 1; age, sex, BMI, and ever smoking in Model 2; age, sex, BMI, ever smoking, and cytokines (IL-6, IL-8, TNF-a, IL-1b) in Model 3; age, sex, BMI, ever smoking, cytokines, and metabolic health (glucose tolerance, BP, and lipid profile) in Model 4; age, sex, BMI, ever-smoking, cytokines, metabolic health, and medication usage for T2D, hypertension, or lipid-lowering in Model 5 (the fully adjusted model). We thereby demonstrate how the estimated associations between adipokine levels and cIMT measures were influenced by different categories of covariates and present the effect estimates from all five models.
Adipokine levels were standardized to a mean of 0 and a standard deviation (SD) of 1. Thus, beta coefficients for regression analyses for the continuous cIMT measures were interpreted as the estimated increase in cIMT levels per 1-SD increase of adipokine or adipokine index levels.
In our primary analyses, we conducted both sexes-combined and sex-stratified analyses. We tested the interaction by sex at the significance level of p < 0.1. In our post hoc investigation, we further stratified the participants by their metabolic health status (metabolically elevated risk or not) and conducted regression analyses within strata to evaluate the potential influences of metabolic health status on the interplay between adipokines and cIMT. Interaction by metabolic health status was also tested.
Results
Characteristics of study participants
A total of 624 participants (442 females; 182 males) were included in this cross-sectional study. Descriptive statistics of study participants are summarized in Table 1. Of note, the mean BMI of participants was notably higher [30.7 kg/m2 (SD: 6.03)] than the average BMI of adults in the US [31], and about 20% of the overall participants reported taking a medication for either T2D, hypertension, or lipid-lowering purposes. Also, in this subset of CCHC subjects, more than 80% of the participants were classified as having metabolically elevated risk for CMD. Females had significantly (p < 0.05) higher levels of adiponectin, leptin, LAR, and IL-1β, lower levels of ARI, higher proportion of normal blood pressure profile, lower proportion of life-time smokers and normal lipid profile, and were more often taking T2D medications, as compared to males. When comparing cIMT levels, males had higher average cIMT measurements (0.71 ± 0.19 mm), as compared to females (0.66 ± 0.14 mm) (p < 0.05).
Table 1.
Distributions of variables among the Cameron County Hispanic Cohort (CCHC) study participants
| Combined (N = 624) | Male (N = 182) | Female (N = 442) | p-valuese | |
|---|---|---|---|---|
| Mean or N | Mean or N | Mean or N | ||
| Adipokines | ||||
| Adiponectin (ug/mL) | 26.3 (21.5) | 19.5 (18.3) | 29.1 (22.1) | < 0.001 |
| Leptin (ng/mL) | 21.9 (15.3) | 11.0 (10.3) | 26.4 (14.8) | < 0.001 |
| Resistin (ng/mL) | 34.5 (16.5) | 35.0 (17.5) | 34.3 (16.1) | 0.661 |
| Leptin-adiponectin ratio (LAR) | 1.24 (1.15) | 0.82 (0.87) | 1.41 (1.21) | < 0.001 |
| Adiponectin-Resitin Index (ARI) | 1.18 (0.31) | 1.31 (0.30) | 1.12 (0.29) | < 0.001 |
| cIMT | ||||
| Average cIMT (mm) | 0.67 (0.15) | 0.71 (0.19) | 0.66 (0.14) | 0.003 |
| Potential confounders | ||||
| Age (years) | 50.2 (14.4) | 48.6 (15.7) | 50.8 (13.7) | 0.097 |
| BMI (kg/m2) | 30.7 (6.03) | 30.2 (5.94) | 30.9 (6.05) | 0.174 |
| Life time smoking > 100 cigarettes (N, %) | 182 (29.2%) | 99 (54.4%) | 83 (18.8%) | < 0.001 |
| Cytokines | ||||
| InterLeukin-6 (pg/mL) | 4.91 (6.77) | 4.55 (5.25) | 5.06 (7.31) | 0.331 |
| InterLeukin-1 Beta (pg/mL) | 1.83 (6.55) | 1.20 (1.26) | 2.08 (7.73) | 0.02 |
| InterLeukin-8 (pg/mL) | 9.14 (8.70) | 9.69 (7.91) | 8.91 (9.00) | 0.284 |
| Tumor Necrosis Factor alpha (pg/mL) | 5.27 (3.58) | 5.49 (3.65) | 5.17 (3.55) | 0.311 |
| Metabolic profile | ||||
| Normal glucose tolerance (yes) (N, %)a | 215 (34.5%) | 56 (30.8%) | 159 (36.0%) | 0.25 |
| Normal blood pressure (N, %)b | 342 (54.8%) | 86 (47.3%) | 256 (57.9%) | 0.019 |
| Normal lipid level (N, %)c | 239 (38.3%) | 87 (47.8%) | 152 (34.4%) | 0.002 |
| Medications | ||||
| T2D Medication (yes) (N, %) | 123 (19.7%) | 26 (14.3%) | 97 (21.9%) | 0.038 |
| Hypertension medication (yes) (N, %) | 195 (31.3%) | 55 (30.2%) | 140 (31.7%) | 0.794 |
| Lipid lowering medication (yes) (N, %) | 172 (27.6%) | 47 (25.8%) | 125 (28.3%) | 0.599 |
| Metabolic health | ||||
| Metabolically elevated riskd (yes) (N, %) | 507 (81.3%) | 146 (80.2%) | 361 (81.7%) | 0.756 |
aNormal glucose tolerance: HbA1c < 5.7 and fasting blood glucose < 100
bNormal blood pressure: SBP < 120 and DBP < 80
cNormal lipid levels: HDL-C ≥ 40 for males and ≥ 50 for females, LDL-C < 160, and TG < 200
dMetabolically elevated risk defined as having at least 2 of the following components: (1) SBP ≥ 130 mmHg or DBP ≥ 85 mmHg or taking antihypertensive medication; (2) TG ≥ 150 mg/dL; (3) HDL < 40 mg/dL in males or < 50 mg/dL in females; (4) FBG ≥ 100 mg/dL or taking hypoglycemic medication; (5) HOMA-IR > 5.13; (6) CRP > 3 mg/L
ep-values from t-test (for continuous variables) and chi-square test (for binary variables) for the sex-differences
Key associations between adipokines and cIMT
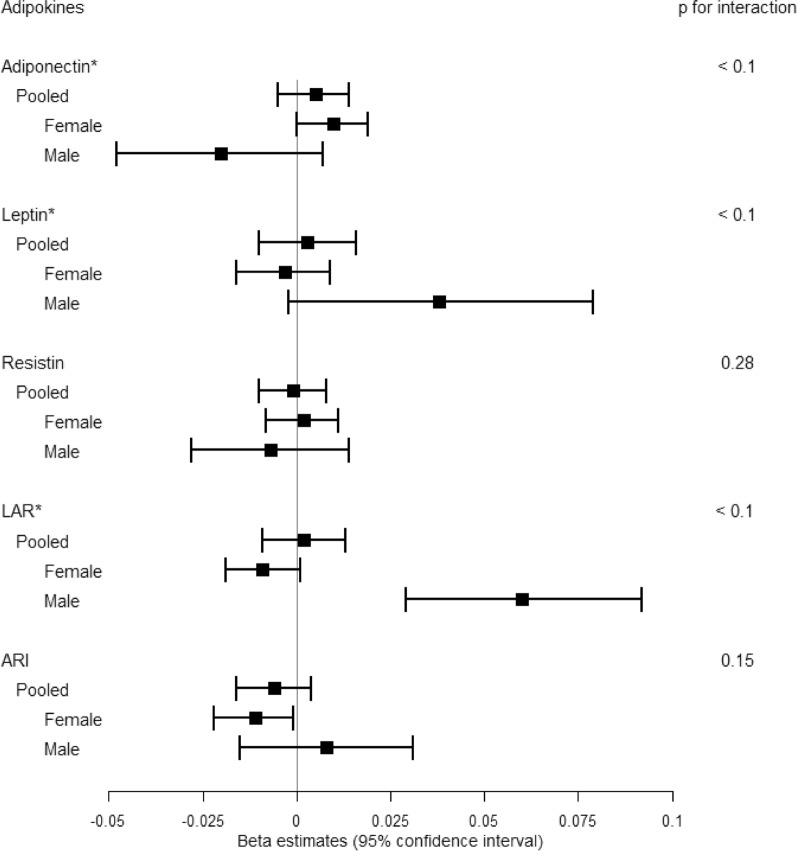
Associations of adipokine measures with continuous cIMT measures across each adjustment to the linear regression models are reported in Table 2. In the sexes-combined fully adjusted model, no significant associations between any adipokine and cIMT measurements were observed. However, associations between adipokine and cIMT demonstrated significant interactions by sex (p < 0.1) for adiponectin, leptin and LAR (Fig. 1 and Table 2).
Table 2.
Estimated association between adipokines and cIMT (continuous) in CCHC study participants
| Model 1* | Model 2 * | Model 3* | Model 4* | Model 5* | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Beta | SE | p | Beta | SE | p | Beta | SE | p | Beta | SE | p | Beta | SE | p | |
| Both sexes-combined | |||||||||||||||
| Adiponectina | 0.004 | 0.005 | 0.472 | 0.005 | 0.005 | 0.358 | 0.002 | 0.005 | 0.716 | 0.003 | 0.005 | 0.520 | 0.005 | 0.005 | 0.350 |
| Leptina | 0.004 | 0.005 | 0.427 | 0.003 | 0.007 | 0.680 | − 0.001 | 0.007 | 0.860 | 0.001 | 0.007 | 0.930 | 0.003 | 0.007 | 0.655 |
| Resistin | 0.003 | 0.005 | 0.568 | 0.002 | 0.005 | 0.634 | 0.000 | 0.005 | 0.954 | − 0.001 | 0.005 | 0.839 | − 0.001 | 0.005 | 0.810 |
| LARa | 0.004 | 0.005 | 0.423 | 0.003 | 0.006 | 0.642 | 0.002 | 0.006 | 0.713 | 0.002 | 0.006 | 0.723 | 0.002 | 0.006 | 0.730 |
| ARI | − 0.001 | 0.005 | 0.867 | − 0.002 | 0.005 | 0.658 | − 0.002 | 0.005 | 0.700 | − 0.004 | 0.005 | 0.415 | − 0.006 | 0.005 | 0.243 |
| Female | |||||||||||||||
| Adiponectin | 0.008 | 0.005 | 0.074 | 0.009 | 0.005 | 0.060 | 0.007 | 0.005 | 0.170 | 0.008 | 0.005 | 0.076 | 0.010 | 0.005 | 0.043 |
| Leptin | − 0.002 | 0.005 | 0.741 | − 0.003 | 0.006 | 0.634 | − 0.007 | 0.006 | 0.291 | − 0.005 | 0.006 | 0.436 | − 0.003 | 0.006 | 0.588 |
| Resistin | 0.006 | 0.005 | 0.263 | 0.005 | 0.005 | 0.330 | 0.002 | 0.005 | 0.631 | 0.002 | 0.005 | 0.713 | 0.002 | 0.005 | 0.754 |
| LAR | − 0.006 | 0.005 | 0.184 | − 0.008 | 0.005 | 0.130 | − 0.009 | 0.005 | 0.089 | − 0.009 | 0.005 | 0.075 | − 0.009 | 0.005 | 0.069 |
| ARI | − 0.005 | 0.005 | 0.351 | − 0.006 | 0.005 | 0.270 | − 0.006 | 0.005 | 0.244 | − 0.009 | 0.005 | 0.083 | − 0.011 | 0.005 | 0.036 |
| Male | |||||||||||||||
| Adiponectin | − 0.016 | 0.013 | 0.240 | − 0.015 | 0.013 | 0.244 | − 0.020 | 0.014 | 0.146 | − 0.020 | 0.014 | 0.154 | − 0.020 | 0.014 | 0.148 |
| Leptin | 0.043 | 0.016 | 0.011 | 0.041 | 0.020 | 0.048 | 0.036 | 0.021 | 0.087 | 0.038 | 0.021 | 0.070 | 0.038 | 0.021 | 0.064 |
| Resistin | − 0.001 | 0.011 | 0.898 | − 0.002 | 0.011 | 0.859 | − 0.006 | 0.011 | 0.575 | − 0.007 | 0.011 | 0.546 | − 0.007 | 0.011 | 0.521 |
| LAR | 0.060 | 0.014 | 4.41E−05 | 0.062 | 0.016 | 1.39E−04 | 0.061 | 0.016 | 2.12E−04 | 0.062 | 0.016 | 1.90E−04 | 0.060 | 0.016 | 2.52E−04 |
| ARI | 0.010 | 0.011 | 0.397 | 0.009 | 0.011 | 0.441 | 0.010 | 0.011 | 0.396 | 0.009 | 0.012 | 0.451 | 0.008 | 0.012 | 0.477 |
*Linear mixed effect model was applied. A kinship matrix estimated based on genotype information among samples was included as a random effect. Fixed effect covariates were age, sex in model 1; age, sex, BMI, and ever smoking in model 2; age, sex, BMI, ever smoking, and cytokines (IL-6, IL-8, TNF-a, IL-1b) in model 3; age, sex, BMI, ever smoking, cytokines, and metabolic health (glucose tolerance, BP, and lipid profile) in model 4; age, sex, BMI, ever-smoking, cytokines, metabolic health, and medication usage for T2D, hypertension, or lipid-lowering in model 5. (Sex was included only in the sexes-combined models)
Beta coefficients indicate the increase in cIMT levels by every 1-SD unit increase of adipokines
aSignificant interaction by sex (p for interaction < 0.1) from Model 5
Fig. 1.
Associations between adipokines and cIMT in both sexes-combined, females, and males. Associations between adipokines and cIMT (continuous) from the fully adjusted linear mixed effects model (Model 5) are demonstrated on the forest plot. Beta coefficients and 95% confidence interval indicate the increase of cIMT levels by every 1-SD increase of adipokines [1-SD: 21.5 ug/mL for adiponectin, 15.3 ng/mL for leptin, 16.5 ng/mL for resistin, 1.15 for LAR, 0.31 for ARI]. Results for sexes-combined and sex-stratified analyses are shown. Significant interaction by sex (p for interaction < 0.1) is indicated (*)
When stratified by sex, higher adiponectin levels and lower ARI were associated with increased cIMT among females [β(SE) = 0.010 (0.005), p = 0.043 for adiponectin; β(SE) = − 0.011 (0.005), p = 0.036 for ARI] in the fully adjusted Model 5. The same variables (in same model) displayed opposite directions of effect in males but were statistically nonsignificant. Among males, one significant association was observed—higher LAR was associated with increased cIMT across all adjustment models [e.g., β(SE) = 0.060 (0.016), p = 2.52 × 10–4 in Model 5]. The effect estimate for LAR (in the same model) moved in the opposing direction among females without statistical significance (Fig. 1 and Table 2).
Testing the influence of metabolic health status on the associations between adipokines and cIMT
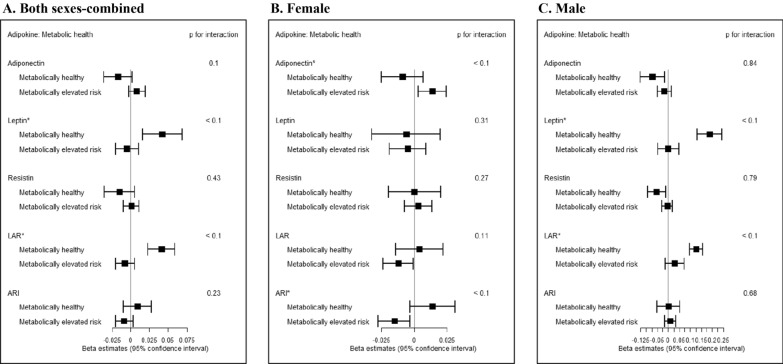
Figure 2 and Additional file 1: Table S1 summarize the effect estimates from the fully adjusted regression model (Model 5 from Table 2) of adipokines and cIMT when participants are stratified by metabolic health status. In contrast to the metabolically elevated risk group, the metabolically healthy group showed positive associations of leptin and LAR with cIMT [β(SE) = 0.042 (0.014), p = 0.002 for leptin; β(SE) = 0.041 (0.009), p = 4.86 × 10–5 for LAR] in the sexes-combined analyses, which was not observed in the pooled (metabolically healthy and elevated risk groups combined) analyses (p for interaction by metabolic health status < 0.1 for leptin and LAR).
Fig. 2.
Associations between adipokines and cIMT stratified by metabolic health status. Associations between adipokines and cIMT levels stratified by metabolic health status from the fully adjusted linear mixed effects model are demonstrated on the forest plot (A. Both sexes-combined, B. Female, and C. Male) Beta coefficients (95% confidence intervals) indicate the increase in cIMT levels by every 1-SD increase of adipokines [1-SD: 21.5 ug/mL for adiponectin, 15.3 ng/mL for leptin, 16.5 ng/mL for resistin, 1.15 for LAR, 0.31 for ARI]. Significant interaction by metabolic health status (p for interaction < 0.1) is indicated by * on the name of adipokines
In the sex-specific analyses, a positive association between adiponectin and cIMT and an inverse association between ARI and cIMT were observed only among females in the metabolically elevated risk group [β(SE) = 0.014 (0.005), p = 0.012 for adiponectin; β(SE) = − 0.015 (0.006), p = 0.013 for ARI]. In addition, an inverse association between LAR and cIMT was observed among metabolically elevated risk group (β(SE) = − 0.012 (0.006), p = 0.040) among females. Among metabolically healthy females, the estimated associations for adiponectin, ARI, and LAR were in opposing directions, though not significant [β(SE) = − 0.009 (0.008), p = 0.267 for adiponectin; β(SE) = 0.014 (0.009), p = 0.113 for ARI; β(SE) = 0.004 (0.009), p = 0.690 for LAR], and the interactions by metabolic health status were significant (p < 0.1) for adiponectin and ARI among females.
Among males, four adipokine measures (adiponectin, leptin, resistin, and LAR) demonstrated significant associations with cIMT only in the metabolically healthy group. Lower adiponectin levels and resistin levels and higher leptin levels and LAR were associated with increased cIMT measures (β(SE) = − 0.072 (0.028), p = 0.015 for adiponectin; β(SE) = 0.188 (0.029), p = 1.04 × 10–7 for leptin; β(SE) = − 0.053 (0.021), p = 0.017 for resistin; and β(SE) = 0.127 (0.015), p = 4.70 × 10–10 for LAR) among males in the metabolically healthy group. The interactions by metabolic health were significant for leptin and LAR (p < 0.1).
Discussion
In this cross-sectional study of Mexican Americans in the CCHC cohort, we investigated the association of adiponectin, leptin, resistin, and composite measures of ARI and LAR with an early marker of atherosclerosis, cIMT, both across and within sexes. Based on previous literature, we expected inverse associations of adiponectin [3] and positive associations of resistin (and ARI) [19, 32] as well as leptin (and LAR) [18, 33] with cIMT. We also hypothesized sex-specificity in these associations to a certain degree, as adipokine levels show variation by sex [34]. We observed sexual dimorphisms, measured as significant interaction by sex, in associations between adipokines and cIMT for adiponectin, leptin, and LAR. Specifically, we observed the hypothesized positive associations between LAR and cIMT among males and unexpected positive associations for adiponectin and inverse associations for ARI among females. We also observed the heterogeneities of these sex-specific associations by metabolic health status. The male-specific association for LAR was specific to the metabolically healthy group, whereas the female-specific associations for adiponectin or ARI were specific to the metabolically elevated risk group.
First, we observed the expected positive direction of effect in the association of a composite index of leptin and adiponectin, LAR, with cIMT among males across all adjustment models. The associations between LAR and cIMT, as well as leptin and cIMT, were further strengthened by restricting analyses to males in the metabolically healthy group and remained significant even among both sexes-combined in the metabolically healthy group (Additional file 1: Table S1). This finding aligns with previous studies of the LAR (or ALR) with CVD-related traits [35–43], including insulin resistance [39], metabolic perturbations [44], and T2D [45]. Although the directions of associations for single measure of adiponectin or leptin were consistent with previous literature among males and among the both sexes-combined metabolically healthy group, the associations were weaker compared to analyses with LAR (Additional file 1: Table S1). Studies applying LAR have indicated an improvement of CVD risk prediction by applying the composite index compared to assessing adiponectin and/or leptin measures alone [46]. Thus, our findings support the notion that composite indices of adipokines expand our understanding of adipose tissue dysfunction [17, 47–51] and suggest that LAR may serve as a better surrogate biomarker for early atherosclerosis among males or among metabolically healthy group than single adipokine measures. However, while LAR may be a promising metric, our data also support the importance of sex-specific differences in the sensitivity and specificity of LAR for assessing metabolic health [52]. Furthermore, given that single leptin measures were more strongly associated with cIMT compared to single adiponectin measures, the significant relationship between LAR and cIMT was largely driven by leptin instead of adiponectin (Additional file 1: Table S1 and Table 2).
By measuring effect modification by sex in the associations between adipokines and cIMT, we further elucidated sex-specific relationships. We identified significant effect modification by sex (p for interaction by sex < 0.1) (Table 2 and Fig. 1), with opposing directions of association in females and males for adiponectin, leptin, and LAR measures. Among females, higher adiponectin levels (with statistical significance), lower leptin levels (without statistical significance), and lower LAR levels (without statistical significance) were associated with higher levels of cIMT; whereas among males, lower adiponectin levels (without statistical significance), higher leptin levels (without statistical significance), and higher LAR levels (with statistical significance) were associated with higher cIMT measures, in line with the previous literature. By restricting participants to the metabolically healthy group, sex-specific analyses indicated heterogeneous associations between adipokines and cIMT across sexes – i.e., metabolically healthy males showed more evident associations consistent with previous literature, except for resistin, but no remarkable associations were observed among metabolically healthy females. Instead, females-only of the metabolically elevated risk group displayed multiple significant, but counterintuitive, associations of adiponectin, LAR, and ARI with cIMT.
Sexual dimorphism in adipokine biology is well-known [53] and is closely related to sex-differences in body composition [54]. Hormonal differences emerge in puberty when sex steroid hormones cause distinct effects on body-fat distribution in males and females—i.e., females typically have greater fat mass than males, whereas males typically have greater lean mass and mineral mass than females [54]. Since adipokines are primarily secreted from adipose tissue, differences in body composition, especially in fat mass, can lead to differences in the average amount of adipokine secretion. Indeed, on average, females have higher levels of leptin and adiponectin than males [53]. Furthermore, previous studies demonstrate that sex hormones such as androgens and estrogens can directly influence the gene expression of adipokines [55–57].
The influence of sex-based differences in adipokine levels may help explain the heterogeneity by sex observed in CVD cases. For example, a sex specific influence of adipokines on the severity of coronary artery calcification (CAC) [58], coronary heart disease events [59], cIMT [60], and blood pressure progression [61] has been noted. Sex-specific positive associations between adiponectin and cardiovascular mortality (non-protective) have been observed among male patients with T2D [62] as well as associations of adipokines on CAC among female patients [63]. Thus, further studies are needed to determine the patterns of sexual dimorphisms in the effect of various adipokines on CVD and their underlying biological mechanisms.
In contrast to the widely observed protective effects of adiponectin against cardiovascular disease in previous research, this study did not observe protective associations between adiponectin and cIMT, with the exception of the metabolically healthy male subjects. Surprisingly, some strata exhibited counterintuitive positive associations between adiponectin and cIMT and inverse associations between ARI and cIMT in the female-only analyses. We note that these counterintuitive associations were particularly strengthened when tested only among females in the metabolically elevated risk group (Fig. 2 and Additional file 1: Table S1). Although several studies on cIMT reported significant inverse or null associations with adiponectin, some studies of atrial fibrillation or CV deaths reported positive associations between adiponectin and CVD-related outcomes [64, 65]. Other studies that observed positive associations between adiponectin and CMD included patients with cardiometabolic conditions such as ischemic stroke [66], T2D [67], and non-alcoholic fatty liver disease [68], which aligns with our strong evidence of effect of the metabolic health condition on the association between adipokines and cIMT. Furthermore, females in the metabolically elevated risk group displayed an inverse association between LAR and cIMT. However, the counterintuitive results of this sub-analysis were somewhat sensitive to outliers in the phenotypic distribution and should be cautiously interpreted (Additional file 1: Table S2).
The relationship between adipokines, cIMT, and metabolic health is unsurprisingly complex. For example, although controversial, increased levels of adiponectin under metabolically perturbed conditions have been coined as the ‘adiponectin paradox’ [69, 70]. Proposed factors influencing adiponectin include insulin signaling impairments, as observed among patients with Type 1 Diabetes [71], and in animal studies that found dependence of adiponectin expression on T-cadherin and glycoprotein levels [72, 73]. Adiponectin resistance may also explain adverse CVD-related outcomes despite the higher levels of adiponectin. Indeed, a previous study observed the downregulation of the adiponectin receptor despite increased levels of adiponectin expression among patients with chronic heart failure [74]. Similarly, among patients with heart failure, higher adiponectin levels were observed in comparison to healthy controls, and reduced adiponectin levels and adiponectin expression have also observed after implantation of ventricular assist devices [75]. In the context of the aforementioned research, our observed cross-sectional association between higher levels of adiponectin and higher levels of cIMT (or inverse association between ARI and cIMT) may be driven by an adiponectin resistance-like phenomenon—i.e., poor metabolic health influencing increased levels of adiponectin without original anti-atherogenic function. Of note, adiponectin levels have also been documented to be higher among females in general [76], which may possibly explain why the effect size of this relationship was particularly greater among females. In addition, the current unexpected observations may be driven by the general poorer metabolic health (e.g., higher level of insulin resistance and obesity prevalence) in the CCHC population as compared to other populations in the U.S.
Since the unexpected relationship between adiponectin and cIMT was female-specific, it merits mentioning that menopausal status may have played a role in this association. It is known that menopause and advancement of age among females are factors associated with conditions similarly exhibited in metabolic syndrome, such as changes in sex hormone levels (i.e., estrogen) and increased visceral adipose tissue [77]. Considering the average age of the CCHC female participants [mean (SD): 50.8 (13.7) years], it is plausible that the hormonal changes of menopause could influence the interplay between adipokines, metabolic health, and subsequent early atherogenesis. However, since the current study did not formally measure the menopausal status, it is hard to reveal the exact contributions of menopause to the current female-specific results.
Though emerging evidence informs our understanding of adipokines and their influence on pro-inflammatory states and consequently manifestations of atherogenesis, conflicting findings across animal and human studies indicate the need for further investigations of specific adipokines with pre-atherosclerotic states. For example, while our finding of the negative association between resistin and cIMT among metabolically healthy males (Additional file 1: Table S2) seems counterintuitive to several studies which suggest its role in pro-inflammatory pathways [78, 79] and even cardiovascular death [7], other study has also reported null associations of resistin with mean intima-media thickness [80]. As such, contradicting evidence in the literature limits our ability to conclude whether resistin may serve as a reliable marker of early atherogenesis in this population.
The current study had notable strengths. Unlike most previous studies, we assessed not only specific adipokines (adiponectin, leptin, and resistin), but also composite indices (LAR and ARI) in association with an early marker of CVD. By considering additional metrics (LAR and ARI) that have shown strong associations between adipokines and CMD, we broadened our ability to capture relationships that may suggest associations with pathophysiological states. Also, we studied an under-represented Hispanic/Latino population with known vulnerabilities to poorer health outcomes [81]. Thus, our findings contribute to a more detailed understanding of adipokines and metabolic dysfunction across diverse populations.
There were also notable limitations in the current study. Residual confounding may remain from assessing adipokine associations with cIMT among a population with poorer metabolic health states compared to the general population. Also, due to the relatively small sample sizes (especially for males), precise effect estimates and significance were somewhat sensitive to the data points in the tails of the distribution, therefore interpretations should be made cautiously. However, we carried out multiple sensitivity analyses (Additional file 1: Table S2) which all led to consistent inferences. Moreover, methodological limitations from a cross-sectional design hinder us from drawing conclusions on the observed unexpected relationships between adipokines and cIMT, particularly for adiponectin and cIMT among females. Cross-sectional analyses also limit inferences on temporality, as seen in other studies that have pinpointed antecedent metabolic states that lead to an adiponectin paradox [82]. Other important factors such as changes in body fat distribution by age and sex are associated with changes in adipokine concentrations and require assessments of these variables over time [83]. Additionally, though cIMT is an established early marker of CVD, it is crucial to assess multiple measures over time to understand patterns of how cIMT progresses into CVD within a population [84]. Furthermore, we acknowledge that stratifying participants by a subset of cardiovascular disease risk factors to denote metabolic health may not have fully captured the total metabolically unhealthy population within our study. In all, these remaining gaps demonstrate the need for longitudinal assessment of adipokines with cIMT.
Conclusions
In conclusion, our study results add to the literature describing a complex relationship between adipokines and cIMT. We demonstrate strong sex-specific and metabolic health-dependent relationship between adipokines and cIMT among Hispanics. Our findings support the utility of the composite index of LAR as a biomarker for early atherosclerosis, especially for males and metabolically healthy individuals. We also observed an unexpected positive association between adiponectin and cIMT (and inverse association between ARI and cIMT) among females with elevated metabolic risk. Further studies exploring these relationships may lead to therapeutic targets to mitigate cardiovascular disease risk among Hispanics at metabolically elevated risk.
Supplementary Information
Additional file 1: Table S1. Estimated associations between adipokines and cIMT (continuous) in participants of CCHC stratified by metabolic health and sex. Table S2. Sensitivity analyses for different approaches to evaluate the potential influences of upper or lower outliers on the association results. Table S3. The distributions of age, sex, and BMI among the whole CCHC participants and the current sub-samples.
Acknowledgements
We thank the participants from the Cameron County Hispanic Cohort study. The authors would like to thank the CCHC cohort team, particularly Rocío Uribe who recruited and interviewed the participants. We additionally acknowledge the valuable efforts from: Marcela Morris, BS, and Hugo Soriano and their teams for laboratory and data support respectively; Norma Pérez-Olazarán, BBA, and Christina Villarreal, BA for administrative support; Valley Baptist Medical Center, Brownsville, Texas, where the Center for Clinical and Translational Science Clinical Research Unit is located; and the CCHC participants from Brownsville who graciously participated in this study.
Abbreviations
- ARI
Adiponectin-resistin index
- BMI
Body mass index
- BP
Blood pressure
- CAC
Coronary artery calcification
- CCHC
The Cameron County Hispanic Cohort
- cIMT
Carotid-intima media thickness
- CMD
Cardiometabolic diseases
- CRP
C-reactive protein
- CVD
Cardiovascular disease
- DBP
Diastolic blood pressure
- ELISA
Enzyme-linked immunosorbent assays
- FBG
Fasting blood glucose
- HDL-C
High-density lipoprotein cholesterol
- HOMA-IR
Homeostatic Model Assessment for Insulin Resistance
- IL-1β
Interleukin-1 Beta
- IL-6
Interleukin-6
- IL-8
Interleukin-8
- LAR
Leptin-to-adiponectin ratio
- LDL-C
Low-density lipoprotein cholesterol
- SBP
Systolic blood pressure
- SD
Standard deviation
- T2D
Type 2 Diabetes
- TG
Triglyceride
- TNF-α
Tumor Necrosis Factor-alpha
Author contributions
DK and AM contributed to the conception, design, analysis plan, interpretation of the work and drafted the manuscript. KEN and ADG contributed to the conception, design, analysis plan, interpretation, manuscript revision, and supervision of the work. DK carried out data analysis for the current study. H-HC, HGP, HMH, and MYA contributed to data quality control, preparation, and statistical analysis. STL, ML, JBM, SPF-H, JEB, KEN, and AGD contributed to study design, data collection and curation, and intellectual direction. All authors read, revised, and approved the final manuscript.
Funding
This work was funded in part by AHA grant 903805, NIH awards: NIH/NHLBI R01HL142302, R01HL151152, R01 DK122503, R01HD057194, R01HG010297, R01HL143885, NIH/NIDDK R01DK127084, R21DK122234. This study was also funded in part by Center for Clinical and Translational Sciences, National Institutes of Health Clinical and Translational Award grant no. UL1 TR000371 from the National Center for Advancing Translational Sciences.
Availability of data and materials
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate
The study was approved by the Committee for the Protection of Human Subjects (CPHS) at the University of Texas Health Sciences Center at Houston. Written informed consent forms were obtained from all study participants.
Consent for publication
Not applicable.
Competing interests
Hannah G. Polikowsky is currently employed by Verily Life Sciences, an independent subsidiary of Alphabet Inc.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Daeeun Kim and Aylin Memili contributed equally to this work.
References
- 1.Mechanick JI, Zhao S, Garvey WT. The adipokine-cardiovascular-lifestyle network: translation to clinical practice. J Am Coll Cardiol. 2016;68(16):1785–1803. doi: 10.1016/j.jacc.2016.06.072. [DOI] [PubMed] [Google Scholar]
- 2.Farkhondeh T, Llorens S, Pourbagher-Shahri AM, Ashrafizadeh M, Talebi M, Shakibaei M, et al. An overview of the role of adipokines in cardiometabolic diseases. Molecules. 2020;25(21):5218. doi: 10.3390/molecules25215218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ntaios G, Gatselis NK, Makaritsis K, Dalekos GN. Adipokines as mediators of endothelial function and atherosclerosis. Atherosclerosis. 2013;227(2):216–221. doi: 10.1016/j.atherosclerosis.2012.12.029. [DOI] [PubMed] [Google Scholar]
- 4.Ouchi N, Walsh K. Adiponectin as an anti-inflammatory factor. Clin Chim Acta. 2007;380(1–2):24–30. doi: 10.1016/j.cca.2007.01.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Martin SS, Qasim A, Reilly MP. Leptin resistance: a possible interface of inflammation and metabolism in obesity-related cardiovascular disease. J Am Coll Cardiol. 2008;52(15):1201–1210. doi: 10.1016/j.jacc.2008.05.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ahiante BO, Smith W, Lammertyn L, Schutte AE. Leptin and the vasculature in young adults: the African-PREDICT study. Eur J Clin Invest. 2019;49(1):e13039. doi: 10.1111/eci.13039. [DOI] [PubMed] [Google Scholar]
- 7.Del Cristo Rodriguez Perez M, Gonzalez DA, Rodriguez IM, Coello SD, Fernandez FJC, Diaz BB, et al. Resistin as a risk factor for all-cause (and cardiovascular) death in the general population. Sci Rep. 2022;12(1):19627. doi: 10.1038/s41598-022-24039-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dullaart RP, Kappelle PJ, Dallinga-Thie GM. Carotid intima media thickness is associated with plasma adiponectin but not with the leptin:adiponectin ratio independently of metabolic syndrome. Atherosclerosis. 2010;211(2):393–396. doi: 10.1016/j.atherosclerosis.2010.03.024. [DOI] [PubMed] [Google Scholar]
- 9.Hui E, Xu A, Chow WS, Lee PC, Fong CH, Cheung SC, et al. Hypoadiponectinemia as an independent predictor for the progression of carotid atherosclerosis: a 5-year prospective study. Metab Syndr Relat Disord. 2014;12(10):517–522. doi: 10.1089/met.2014.0024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Juonala M, Saarikoski LA, Viikari JS, Oikonen M, Lehtimaki T, Lyytikainen LP, et al. A longitudinal analysis on associations of adiponectin levels with metabolic syndrome and carotid artery intima-media thickness. The Cardiovascular Risk in Young Finns Study. Atherosclerosis. 2011;217(1):234–239. doi: 10.1016/j.atherosclerosis.2011.03.016. [DOI] [PubMed] [Google Scholar]
- 11.Singh S, Lohakare AC. Association of leptin and carotid intima-media thickness in overweight and obese individuals: a cross-sectional study. J Assoc Physicians India. 2020;68(8):19–23. [PubMed] [Google Scholar]
- 12.Asha K, Sharma SB, Singal A, Aggarwal A. Association of carotid intima-media thickness with leptin and apoliprotein b/apoliprotein a-I ratio reveals imminent predictors of subclinical atherosclerosis in psoriasis patients. Acta Medica (Hradec Kralove) 2014;57(1):21–27. doi: 10.14712/18059694.2014.4. [DOI] [PubMed] [Google Scholar]
- 13.Ciccone M, Vettor R, Pannacciulli N, Minenna A, Bellacicco M, Rizzon P, et al. Plasma leptin is independently associated with the intima-media thickness of the common carotid artery. Int J Obes Relat Metab Disord. 2001;25(6):805–810. doi: 10.1038/sj.ijo.0801623. [DOI] [PubMed] [Google Scholar]
- 14.Rubio-Guerra AF, Cabrera-Miranda LJ, Vargas-Robles H, Maceda-Serrano A, Lozano-Nuevo JJ, Escalante-Acosta BA. Correlation between levels of circulating adipokines and adiponectin/resistin index with carotid intima-media thickness in hypertensive type 2 diabetic patients. Cardiology. 2013;125(3):150–153. doi: 10.1159/000348651. [DOI] [PubMed] [Google Scholar]
- 15.Shin HJ, Park S, Yoon SJ, Choi DS, Cho DK, Kim JS, et al. Association between serum resistin and carotid intima media thickness in hypertension patients. Int J Cardiol. 2008;125(1):79–84. doi: 10.1016/j.ijcard.2007.02.028. [DOI] [PubMed] [Google Scholar]
- 16.Yazici D, Yavuz D, Ogunc AV, Sirikci O, Toprak A, Deyneli O, et al. Serum adipokine levels in type 1 diabetic patients: association with carotid intima media thickness. Metab Syndr Relat Disord. 2012;10(1):26–31. doi: 10.1089/met.2011.0052. [DOI] [PubMed] [Google Scholar]
- 17.Fruhbeck G, Catalan V, Rodriguez A, Gomez-Ambrosi J. Adiponectin-leptin ratio: a promising index to estimate adipose tissue dysfunction. Relation with obesity-associated cardiometabolic risk. Adipocyte. 2018;7(1):57–62. doi: 10.1080/21623945.2017.1402151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fruhbeck G, Catalan V, Rodriguez A, Ramirez B, Becerril S, Salvador J, et al. Adiponectin-leptin ratio is a functional biomarker of adipose tissue inflammation. Nutrients. 2019;11(2):454. doi: 10.3390/nu11020454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lau CH, Muniandy S. Novel adiponectin-resistin (AR) and insulin resistance (IRAR) indexes are useful integrated diagnostic biomarkers for insulin resistance, type 2 diabetes and metabolic syndrome: a case control study. Cardiovasc Diabetol. 2011;10:8. doi: 10.1186/1475-2840-10-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Norata GD, Raselli S, Grigore L, Garlaschelli K, Dozio E, Magni P, et al. Leptin:adiponectin ratio is an independent predictor of intima media thickness of the common carotid artery. Stroke. 2007;38(10):2844–2846. doi: 10.1161/STROKEAHA.107.485540. [DOI] [PubMed] [Google Scholar]
- 21.Everson-Rose SA, Barinas-Mitchell EJM, El Khoudary SR, Huang HH, Wang Q, Janssen I, et al. Adipokines and subclinical cardiovascular disease in post-menopausal women: study of Women's Health Across the Nation. J Am Heart Assoc. 2021;10(7):e019173. doi: 10.1161/JAHA.120.019173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wang H, Wang YT, Fan L, Guo YT, Shi Y, Tao T, et al. Resistin might not be a risk factor for carotid artery atherosclerosis in elderly Chinese males. J Geriatr Cardiol. 2014;11(3):222–228. doi: 10.11909/j.issn.1671-5411.2014.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kern PA, Di Gregorio GB, Lu T, Rassouli N, Ranganathan G. Adiponectin expression from human adipose tissue: relation to obesity, insulin resistance, and tumor necrosis factor-alpha expression. Diabetes. 2003;52(7):1779–1785. doi: 10.2337/diabetes.52.7.1779. [DOI] [PubMed] [Google Scholar]
- 24.Belin de Chantemele EJ. Sex differences in leptin control of cardiovascular function in health and metabolic diseases. Adv Exp Med Biol. 2017;1043:87–111. doi: 10.1007/978-3-319-70178-3_6. [DOI] [PubMed] [Google Scholar]
- 25.Martin SS, Blaha MJ, Muse ED, Qasim AN, Reilly MP, Blumenthal RS, et al. Leptin and incident cardiovascular disease: the multi-ethnic study of atherosclerosis (MESA) Atherosclerosis. 2015;239(1):67–72. doi: 10.1016/j.atherosclerosis.2014.12.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wattanapol P, Vichinsartvichai P, Sakoonwatanyoo P. Serum adiponectin is a potential biomarker for metabolic syndrome in peri-and postmenopausal women. Gynecol Endocrinol. 2020;36(7):620–625. doi: 10.1080/09513590.2020.1742688. [DOI] [PubMed] [Google Scholar]
- 27.Mirza S, Hossain M, Mathews C, Martinez P, Pino P, Gay JL, et al. Type 2-diabetes is associated with elevated levels of TNF-alpha, IL-6 and adiponectin and low levels of leptin in a population of Mexican Americans: a cross-sectional study. Cytokine. 2012;57(1):136–142. doi: 10.1016/j.cyto.2011.09.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gutierrez AD, Flores CA, Naik S, Lee M, Asgarisabet P, Resman M, et al. Resistin levels decrease as insulin resistance increases in a Mexican-American cohort. Cytokine. 2021;148:155687. doi: 10.1016/j.cyto.2021.155687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Laing ST, Smulevitz B, Vatcheva KP, Rahbar MH, Reininger B, McPherson DD, et al. Subclinical atherosclerosis and obesity phenotypes among Mexican Americans. J Am Heart Assoc. 2015;4(3):e001540. doi: 10.1161/JAHA.114.001540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stein JH, Korcarz CE, Hurst RT, Lonn E, Kendall CB, Mohler ER, et al. Use of carotid ultrasound to identify subclinical vascular disease and evaluate cardiovascular disease risk: a consensus statement from the American Society of Echocardiography Carotid Intima-Media Thickness Task Force. Endorsed by the Society for Vascular Medicine. J Am Soc Echocardiogr. 2008;21(2):93–111. doi: 10.1016/j.echo.2007.11.011. [DOI] [PubMed] [Google Scholar]
- 31.Fryar CD, Kruszon-Moran D, Gu Q, Ogden CL. Mean body weight, height, waist circumference, and body mass index among adults: United States, 1999–2000 through 2015–2016. Natl Health Stat Rep. 2018;122:1–16. [PubMed] [Google Scholar]
- 32.Schwartz DR, Lazar MA. Human resistin: found in translation from mouse to man. Trends Endocrinol Metab. 2011;22(7):259–265. doi: 10.1016/j.tem.2011.03.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Friedman JM. Leptin, leptin receptors, and the control of body weight. Nutr Rev. 1998;56(2 Pt 2):s38–46. doi: 10.1111/j.1753-4887.1998.tb01685.x. [DOI] [PubMed] [Google Scholar]
- 34.Sood A. Sex differences: implications for the obesity-asthma association. Exerc Sport Sci Rev. 2011;39(1):48–56. doi: 10.1097/JES.0b013e318201f0c4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Carmen Zaha D, Vesa C, Uivarosan D, Bratu O, Fratila O, Mirela Tit D, et al. Influence of inflammation and adipocyte biochemical markers on the components of metabolic syndrome. Exp Ther Med. 2020;20(1):121–128. doi: 10.3892/etm.2020.8663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chen VCH, Chen CH, Chiu YH, Lin TY, Li FC, Lu ML. Leptin/Adiponectin ratio as a potential biomarker for metabolic syndrome in patients with schizophrenia. Psychoneuroendocrino. 2018;92:34–40. doi: 10.1016/j.psyneuen.2018.03.021. [DOI] [PubMed] [Google Scholar]
- 37.Cicero AF, Magni P, More M, Ruscica M, Borghi C, Strollo F, et al. Metabolic syndrome, adipokines and hormonal factors in pharmacologically untreated adult elderly subjects from the Brisighella Heart Study historical cohort. Obes Facts. 2012;5(3):319–326. doi: 10.1159/000339575. [DOI] [PubMed] [Google Scholar]
- 38.Finucane FM, Luan J, Wareham NJ, Sharp SJ, O'Rahilly S, Balkau B, et al. Correlation of the leptin:adiponectin ratio with measures of insulin resistance in non-diabetic individuals. Diabetologia. 2009;52(11):2345–2349. doi: 10.1007/s00125-009-1508-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Inoue M, Maehata E, Yano M, Taniyama M, Suzuki S. Correlation between the adiponectin-leptin ratio and parameters of insulin resistance in patients with type 2 diabetes. Metabolism. 2005;54(3):281–286. doi: 10.1016/j.metabol.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 40.Masquio DCL, de Piano A, Sanches PL, Corgosinho FC, Campos RMS, Carnier J, et al. The effect of weight loss magnitude on pro-/anti-inflammatory adipokines and carotid intima-media thickness in obese adolescents engaged in interdisciplinary weight loss therapy. Clin Endocrinol. 2013;79(1):55–64. doi: 10.1111/j.1365-2265.2012.04504.x. [DOI] [PubMed] [Google Scholar]
- 41.Mednova IA, Boiko AS, Kornetova EG, Parshukova DA, Semke AV, Bokhan NA, et al. Adipocytokines and metabolic syndrome in patients with schizophrenia. Metabolites. 2020;10(10):410. doi: 10.3390/metabo10100410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Morales A, Schatz D, Brusko T, Carter C, Wasserfall C, Silverstein J, et al. Adiponectin and leptin concentrations may aid in discriminating disease forms in children and met adolescents with type 1 and type 2 diabetes. Diabetes Care. 2004;27(8):2010–2014. doi: 10.2337/diacare.27.8.2010. [DOI] [PubMed] [Google Scholar]
- 43.Zaletel J, Barlovic DP, Prezelj J. Adiponectin-leptin ratio: a useful estimate of insulin resistance in patients with Type 2 diabetes. J Endocrinol Invest. 2010;33(8):514–518. doi: 10.1007/BF03346639. [DOI] [PubMed] [Google Scholar]
- 44.Sarray S, Madan S, Saleh LR, Mahmoud N, Almawi WY. Validity of adiponectin-to-leptin and adiponectin-to-resistin ratios as predictors of polycystic ovary syndrome. Fertil Steril. 2015;104(2):460–466. doi: 10.1016/j.fertnstert.2015.05.007. [DOI] [PubMed] [Google Scholar]
- 45.Liao PJ, Ting MK, Wu IW, Chen SW, Yang NI, Hsu KH. Higher leptin-to-adiponectin ratio strengthens the association between body measurements and occurrence of type 2 diabetes mellitus. Front Public Health. 2021;9:678681. doi: 10.3389/fpubh.2021.678681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kappelle PJ, Dullaart RP, van Beek AP, Hillege HL, Wolffenbuttel BH. The plasma leptin/adiponectin ratio predicts first cardiovascular event in men: a prospective nested case-control study. Eur J Intern Med. 2012;23(8):755–759. doi: 10.1016/j.ejim.2012.06.013. [DOI] [PubMed] [Google Scholar]
- 47.Mlinar B, Marc J. New insights into adipose tissue dysfunction in insulin resistance. Clin Chem Lab Med. 2011;49(12):1925–1935. doi: 10.1515/CCLM.2011.697. [DOI] [PubMed] [Google Scholar]
- 48.Amato MC, Giordano C. Visceral adiposity index: an indicator of adipose tissue dysfunction. Int J Endocrinol. 2014;2014:730827. doi: 10.1155/2014/730827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Rodriguez-Ayala E, Gallegos-Cabrales EC, Gonzalez-Lopez L, Laviada-Molina HA, Salinas-Osornio RA, Nava-Gonzalez EJ, et al. Towards precision medicine: defining and characterizing adipose tissue dysfunction to identify early immunometabolic risk in symptom-free adults from the GEMM family study. Adipocyte. 2020;9(1):153–169. doi: 10.1080/21623945.2020.1743116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Longo M, Zatterale F, Naderi J, Parrillo L, Formisano P, Raciti GA, et al. Adipose tissue dysfunction as determinant of obesity-associated metabolic complications. Int J Mol Sci. 2019;20(9):2358. doi: 10.3390/ijms20092358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Goossens GH. The role of adipose tissue dysfunction in the pathogenesis of obesity-related insulin resistance. Physiol Behav. 2008;94(2):206–218. doi: 10.1016/j.physbeh.2007.10.010. [DOI] [PubMed] [Google Scholar]
- 52.Agostinis-Sobrinho C, Vicente S, Norkiene S, Rauckiene-Michaelsson A, Kievisiene J, Dubey VP, et al. Is the leptin/adiponectin ratio a better diagnostic biomarker for insulin resistance than leptin or adiponectin alone in adolescents? Children (Basel) 2022;9(8):1193. doi: 10.3390/children9081193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Luque-Ramirez M, Martinez-Garcia MA, Montes-Nieto R, Fernandez-Duran E, Insenser M, Alpanes M, et al. Sexual dimorphism in adipose tissue function as evidenced by circulating adipokine concentrations in the fasting state and after an oral glucose challenge. Hum Reprod. 2013;28(7):1908–1918. doi: 10.1093/humrep/det097. [DOI] [PubMed] [Google Scholar]
- 54.Wells JC. Sexual dimorphism of body composition. Best Pract Res Clin Endocrinol Metab. 2007;21(3):415–430. doi: 10.1016/j.beem.2007.04.007. [DOI] [PubMed] [Google Scholar]
- 55.Seth P, Porter D, Lahti-Domenici J, Geng Y, Richardson A, Polyak K. Cellular and molecular targets of estrogen in normal human breast tissue. Cancer Res. 2002;62(16):4540–4544. [PubMed] [Google Scholar]
- 56.Dhanasekaran SM, Dash A, Yu J, Maine IP, Laxman B, Tomlins SA, et al. Molecular profiling of human prostate tissues: insights into gene expression patterns of prostate development during puberty. Faseb J. 2005;19(2):243–245. doi: 10.1096/fj.04-2415fje. [DOI] [PubMed] [Google Scholar]
- 57.Trujillo ME, Scherer PE. Adipose tissue-derived factors: impact on health and disease. Endocr Rev. 2006;27(7):762–778. doi: 10.1210/er.2006-0033. [DOI] [PubMed] [Google Scholar]
- 58.Larsen BA, Laughlin GA, Cummins K, Barrett-Connor E, Wassel CL. Adipokines and severity and progression of coronary artery calcium: findings from the Rancho Bernardo Study. Atherosclerosis. 2017;265:1–6. doi: 10.1016/j.atherosclerosis.2017.07.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Laughlin GA, Barrett-Connor E, May S, Langenberg C. Association of adiponectin with coronary heart disease and mortality: the Rancho Bernardo study. Am J Epidemiol. 2007;165(2):164–174. doi: 10.1093/aje/kwk001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Nishida M, Moriyama T, Ishii K, Takashima S, Yoshizaki K, Sugita Y, et al. Effects of IL-6, adiponectin, CRP and metabolic syndrome on subclinical atherosclerosis. Clin Chim Acta. 2007;384(1–2):99–104. doi: 10.1016/j.cca.2007.06.009. [DOI] [PubMed] [Google Scholar]
- 61.Kaze AD, Musani SK, Bidulescu A, Correa A, Golden SH, Bertoni AG, et al. Plasma adiponectin and blood pressure progression in African Americans: the Jackson heart study. Am J Hypertens. 2021;34(11):1163–1170. doi: 10.1093/ajh/hpab101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Menzaghi C, Xu M, Salvemini L, De Bonis C, Palladino G, Huang T, et al. Circulating adiponectin and cardiovascular mortality in patients with type 2 diabetes mellitus: evidence of sexual dimorphism. Cardiovasc Diabetol. 2014;13:130. doi: 10.1186/s12933-014-0130-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Mehta A, Patel J, Al Rifai M, Ayers CR, Neeland IJ, Kanaya AM, et al. Inflammation and coronary artery calcification in South Asians: the mediators of atherosclerosis in South Asians living in America (MASALA) study. Atherosclerosis. 2018;270:49–56. doi: 10.1016/j.atherosclerosis.2018.01.033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Knuiman M, Briffa T, Divitini M, Chew D, Eikelboom J, McQuillan B, et al. A cohort study examination of established and emerging risk factors for atrial fibrillation: the Busselton Health Study. Eur J Epidemiol. 2014;29(3):181–190. doi: 10.1007/s10654-013-9875-y. [DOI] [PubMed] [Google Scholar]
- 65.Macheret F, Bartz TM, Djousse L, Ix JH, Mukamal KJ, Zieman SJ, et al. Higher circulating adiponectin levels are associated with increased risk of atrial fibrillation in older adults. Heart. 2015;101(17):1368–1374. doi: 10.1136/heartjnl-2014-307015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Tu WJ, Qiu HC, Liu YK, Liu Q, Zeng X, Zhao J. Elevated levels of adiponectin associated with major adverse cardiovascular and cerebrovascular events and mortality risk in ischemic stroke. Cardiovasc Diabetol. 2020;19(1):125. doi: 10.1186/s12933-020-01096-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Sun Q, Yan B, Yang D, Guo J, Wang C, Zhang Q, et al. Serum adiponectin levels are positively associated with diabetic peripheral neuropathy in chinese patients with type 2 diabetes. Front Endocrinol (Lausanne) 2020;11:567959. doi: 10.3389/fendo.2020.567959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ebrahimi R, Shanaki M, Mohassel Azadi S, Bahiraee A, Radmard AR, Poustchi H, et al. Low level of adiponectin predicts the development of Nonalcoholic fatty liver disease: is it irrespective to visceral adiposity index, visceral adipose tissue thickness and other obesity indices? Arch Physiol Biochem. 2022;128(1):24–31. doi: 10.1080/13813455.2019.1661496. [DOI] [PubMed] [Google Scholar]
- 69.Menzaghi C, Trischitta V. The Adiponectin paradox for all-cause and cardiovascular mortality. Diabetes. 2018;67(1):12–22. doi: 10.2337/dbi17-0016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Kalkman HO. An explanation for the adiponectin paradox. Pharmaceuticals (Basel) 2021;14(12):1266. doi: 10.3390/ph14121266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Pereira RI, Snell-Bergeon JK, Erickson C, Schauer IE, Bergman BC, Rewers M, et al. Adiponectin dysregulation and insulin resistance in type 1 diabetes. J Clin Endocrinol Metab. 2012;97(4):E642–E647. doi: 10.1210/jc.2011-2542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Matsuda K, Fujishima Y, Maeda N, Mori T, Hirata A, Sekimoto R, et al. Positive feedback regulation between adiponectin and T-cadherin impacts adiponectin levels in tissue and plasma of male mice. Endocrinology. 2015;156(3):934–946. doi: 10.1210/en.2014-1618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Obata Y, Kita S, Koyama Y, Fukuda S, Takeda H, Takahashi M, et al. Adiponectin/T-cadherin system enhances exosome biogenesis and decreases cellular ceramides by exosomal release. JCI Insight. 2018;3(8):e99680. doi: 10.1172/jci.insight.99680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Van Berendoncks AM, Garnier A, Beckers P, Hoymans VY, Possemiers N, Fortin D, et al. Functional adiponectin resistance at the level of the skeletal muscle in mild to moderate chronic heart failure. Circ Heart Fail. 2010;3(2):185–194. doi: 10.1161/CIRCHEARTFAILURE.109.885525. [DOI] [PubMed] [Google Scholar]
- 75.Khan RS, Kato TS, Chokshi A, Chew M, Yu S, Wu C, et al. Adipose tissue inflammation and adiponectin resistance in patients with advanced heart failure: correction after ventricular assist device implantation. Circ Heart Fail. 2012;5(3):340–348. doi: 10.1161/CIRCHEARTFAILURE.111.964031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Boyne MS, Bennett NR, Cooper RS, Royal-Thomas TY, Bennett FI, Luke A, et al. Sex-differences in adiponectin levels and body fat distribution: longitudinal observations in Afro-Jamaicans. Diabetes Res Clin Pract. 2010;90(2):e33–e36. doi: 10.1016/j.diabres.2010.08.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Mankowska A, Nowak L, Sypniewska G. Adiponectin and metabolic syndrome in women at menopause. EJIFCC. 2009;19(4):173–184. [PMC free article] [PubMed] [Google Scholar]
- 78.Reilly MP, Lehrke M, Wolfe ML, Rohatgi A, Lazar MA, Rader DJ. Resistin is an inflammatory marker of atherosclerosis in humans. Circulation. 2005;111(7):932–939. doi: 10.1161/01.CIR.0000155620.10387.43. [DOI] [PubMed] [Google Scholar]
- 79.Langheim S, Dreas L, Veschini L, Maisano F, Foglieni C, Ferrarello S, et al. Increased expression and secretion of resistin in epicardial adipose tissue of patients with acute coronary syndrome. Am J Physiol Heart Circ Physiol. 2010;298(3):H746–H753. doi: 10.1152/ajpheart.00617.2009. [DOI] [PubMed] [Google Scholar]
- 80.Kunnari A, Ukkola O, Paivansalo M, Kesaniemi YA. High plasma resistin level is associated with enhanced highly sensitive C-reactive protein and leukocytes. J Clin Endocrinol Metab. 2006;91(7):2755–2760. doi: 10.1210/jc.2005-2115. [DOI] [PubMed] [Google Scholar]
- 81.Fisher-Hoch SP, Rentfro AR, Salinas JJ, Perez A, Brown HS, Reininger BM, et al. Socioeconomic status and prevalence of obesity and diabetes in a Mexican American community, Cameron County, Texas, 2004–2007. Prev Chronic Dis. 2010;7(3):A53. [PMC free article] [PubMed] [Google Scholar]
- 82.Loo LH, Lin HJ, Singh DK, Lyons KM, Altschuler SJ, Wu LF. Heterogeneity in the physiological states and pharmacological responses of differentiating 3T3-L1 preadipocytes. J Cell Biol. 2009;187(3):375–384. doi: 10.1083/jcb.200904140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Cnop M, Havel PJ, Utzschneider KM, Carr DB, Sinha MK, Boyko EJ, et al. Relationship of adiponectin to body fat distribution, insulin sensitivity and plasma lipoproteins: evidence for independent roles of age and sex. Diabetologia. 2003;46(4):459–469. doi: 10.1007/s00125-003-1074-z. [DOI] [PubMed] [Google Scholar]
- 84.Olmastroni E, Baragetti A, Casula M, Grigore L, Pellegatta F, Pirillo A, et al. Multilevel models to estimate carotid intima-media thickness curves for individual cardiovascular risk evaluation. Stroke. 2019;50(7):1758–1765. doi: 10.1161/STROKEAHA.118.024692. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Table S1. Estimated associations between adipokines and cIMT (continuous) in participants of CCHC stratified by metabolic health and sex. Table S2. Sensitivity analyses for different approaches to evaluate the potential influences of upper or lower outliers on the association results. Table S3. The distributions of age, sex, and BMI among the whole CCHC participants and the current sub-samples.
Data Availability Statement
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.