Abstract
Background
Higher dietary quality, including increased vegetable consumption, was associated with a reduced risk of metabolic syndrome (MetS). However, specific vegetable consumption in the development of MetS remains obscure. Our study aimed to investigate the correlation between starchy and non-starchy vegetables and MetS.
Methods
Secondary data analysis from the National Health and Nutrition Examination Survey (NHANES 1999–2018). MetS was defined by National Cholesterol Education Program-Adult treatment Panel III (NCEP ATPIII) and dietary consumption was assessed by trained staff using two 24-h diet recall methods. Weighted logistic regression analysis was carried out to estimate odds ratios (ORs) and 95% confidence intervals (CIs). Subgroup analyses and restricted cubic spline (RCS) regression were performed to further investigate specific vegetable subtypes and MetS.
Results
This research enrolled 24,646 individuals (11,725 females and 12,921 males), with an average age of 45.84 ± 0.23 years. Approximately 15,828(64.22%) participants were defined to be with non-MetS and 8818(35.78%) were with MetS. Both total starchy vegetables and potatoes were associated with increased MetS risk, with the corresponding OR per standard deviation (SD) (95%CI, p-trend) being 1.06(1.02–1.11, p-trend = 0.028) and 1.08(1.04–1.13, p-trend = 0.011), respectively. However, an inverse correlation was found between dark-green vegetables and MetS, and the OR per SD (95%CI, p-trend) was 0.93(0.90–0.97, p-trend = 0.010). Subgroup analyses showed that the positive associations of starchy vegetables and potatoes on MetS risk were stronger in non-Hispanic White participants (p for interaction < 0.050).
Conclusion
Total starchy vegetables and white potatoes were both associated with an increased risk of MetS, while consumption of dark-green vegetables was negatively associated with MetS risk. These findings might provide a promising and healthy dietary strategy for preventing MetS.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12986-023-00760-1.
Keywords: Metabolic syndrome, Vegetables, Potatoes, Nutrition, Risk
Introduction
Metabolic Syndrome (MetS) is a cluster of interrelated metabolic disorders, including hypertension, dyslipidemia, glucose intolerance, and abdominal obesity, that has been linked to an increased risk of stroke, type 2 diabetes, cardiovascular disease, and other serious adverse health outcomes [1–3]. The prevalence of MetS has been increasing worldwide during the previous 20 years, with more than one billion people estimated to be affected [4, 5]. Between 1999 and 2014, the prevalence of MetS among American adults approached nearly 34%, with higher rates in non-Hispanic whites and individuals aged over 65 [5, 6]. Accordingly, MetS has emerged as a major public health concern and represents a substantial burden on human society, underscoring the need for more effective strategies to prevent and manage MetS [7].
To date, much of the research has been conducted to explore the relationships between vegetable consumption or different dietary patterns and MetS [8, 9]. However, limited data are available on the correlation between different categories of vegetables and the risk of MetS, and the existing studies have produced conflicting results [10–18]. For instance, previous studies suggested the intake of non-starchy vegetables was related to weight loss, while the intake of starchy vegetables, particularly potatoes, was linked to greater body weight [10, 11], as well as higher incidence of diabetes [12], hypertension [13], and mortality [19]. This may be due, in part, to their antioxidant loss and high glycemic index (GI) during processing [16, 20]. However, a prospective cohort study among the American adult population found that a higher intake of starchy vegetables was beneficial to health when excluding potatoes [17]. Additionally, Li et al. reported null relationships between starchy vegetable and potato intake and MetS risk [18]. Concurrently, previous studies have shown that the intake of non-starchy vegetables, especially dark-green vegetables, was inversely associated with certain cancers, depression, hepatic steatosis, and mortality [21–25]. However, the relationship with MetS has not been specifically investigated. Although current dietary guidelines generally treat all types of vegetables equally, it’s necessary to investigate potentially distinct health effects of different subgroups of vegetables [26].
Due to the existing uncertainty regarding the impact of specific vegetable consumption on MetS, we examined the correlations between starchy and non-starchy vegetable consumption as well as their subtypes and MetS risk in a nationally representative population from the US National Health and Nutrition Examination Survey (NHANES).
Materials and methods
Study design and population
The NHANES is a biennial and nationally replicated cross-sectional program conducted by National Center for Health Statistics (NCHS) to explore the risk factors and prevalence of common diseases among the US population. Detailed NHANES datasets were collected by highly trained staff and consisted of face-to-face interviews, biochemical tests, and physical examinations. Briefly, a complex and stratified multi-stage strategy was adopted to screen participants in NHANES [27]. All NHANES examinees were eligible to have two interviews. The first interview was completed in their home and the second was conducted in the mobile examination center (MEC) through a series of health examinations. Written informed consent was provided by all participants when they were enrolled. More detailed information about NHANES survey design, codebooks, and methods can be found at NHANES’s online website: https://www.cdc.gov/nchs/nhanes/index.htm.
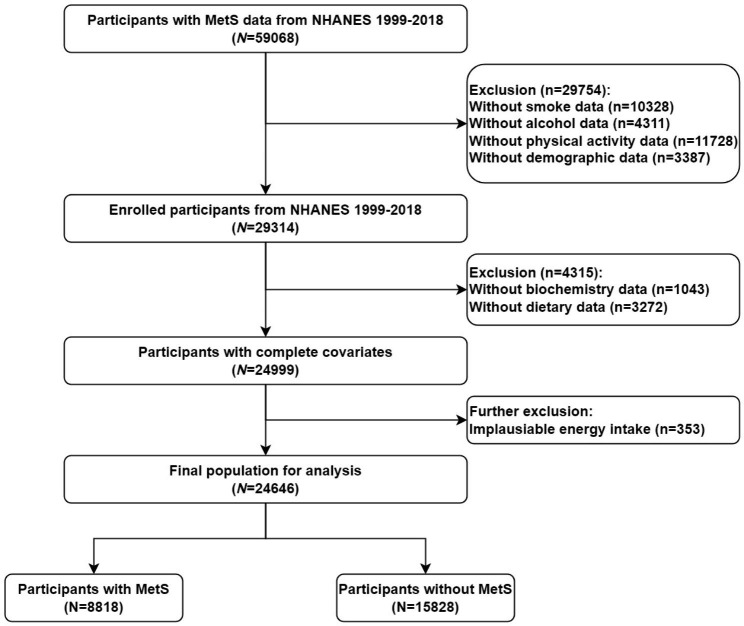
In current analyses, we downloaded 10 consecutive datasets (1999–2000,2001–2002,2003–2004,2005–2006,2007–2008,2009–2010,2011–2012,2013–2014,2015–2016,2017–2018) from the NHANES website to accurately assess the relationship between different kinds of vegetables and MetS. Specifically, a total of 59,068 participants with complete MetS data were evaluated. Among them, we firstly excluded participants with the missing value of the following conditions: smoking (n = 10,328), alcohol consumption (n = 4311), physical activity (n = 11,728), and demographic data (n = 3387). Secondly, we excluded participants without biochemistry data (n = 1043) and dietary data (n = 3272). Then, we further excluded participants with unreasonable daily energy intake (≤ 500 or ≥ 5000 kcal per day, n = 353) [28]. Eventually, 24,646 eligible participants were divided into 8818 with MetS and 15,828 without MetS in the current study (Fig. 1).
Fig. 1.
Flow diagram of the study design
Definition of MetS
According to the previous guideline, we selected the National Cholesterol Education Program-Adult treatment Panel III (NCEP ATPIII) as the diagnostic criteria of MetS [29]. Specifically, participants were considered to be MetS if they met three or more of the following conditions: (1). Hypertriglyceridemia: serum triglyceride ≥ 150 mg/dL(1.7mmol/L), or drug treatment for elevated triglycerides; (2). Central obesity: waist circumference ≥ 102 cm in men or ≥ 88 cm in women; (3). Reduced high density cholesterols (HDL): serum HDL < 40 mg/dL(1.03mmol/L) in men and < 50 mg/dL(1.29mmol/L) in women;(4). Hypertension: systolic blood pressure (SBP) ≥ 130 mmHg or diastolic blood pressure (DBP) ≥ 85 mmHg or drug treatment for hypertension;(5). Hyperglycemia: fasting glucose ≥ 100 mg/dL(5.6mmol/L) or drug treatment for elevated blood glucose. For blood pressure measurement, all participants were allowed to rest quietly for five minutes in MEC and determine the maximum inflation level. In the current study, we obtained three consecutive measurement of blood pressure, and then calculated the arithmetic mean of blood pressure to obtain the final recording.
Dietary assessment
In the current study, data on dietary intake were obtained using two 24-hour dietary recall surveys. All NHANES examinees were eligible to take part in these interviews. The first 24-hour recall survey was conducted face-to-face by trained food recall data collectors in the interview room of MEC, then the second was carried out over the phone 3–10 days later. In our statistical analysis, dietary intake data were completed for all participants. Therefore, the average vegetable intake over 2 days was used in this statistical analysis to reduce bias.
Based on the 2017–2018 American Food Pattern Equivalent Database (FPED), we defined different types of vegetables (Additional file 1: Table S1). White potatoes (such as fried, boiled, baked potatoes and potatoes and potato chips) and other starchy vegetables (such as unripe peas, lima beans, corn, breadfruit, burdock, and cassava) are all starchy vegetables. Dark-green vegetables (such as arugula, basil, beet greens, bitter melon leaves, and broccoli), red and orange vegetables (such as carrots, red peppers, red or orange bell peppers, and squash), and other non-starchy vegetables (such as artichokes, asparagus, avocado, bamboo shoots, and beets) are all non-starchy vegetables.
Covariates
Age, gender, race, marital status, poverty income ratio (PIR), education, smoking, alcohol status, physical activity, serum creatinine, uric acid, alanine aminotransferase (ALT), aspartate aminotransferase (AST), and intake of energy, carbohydrate, whole grains, meat, and nuts were considered as covariates that associated with MetS. Age was treated as continuous variable. Race was stratified into Non-Hispanic Black, Non-Hispanic White, Mexican American, and other races. PIR was stratified into three levels: <1.30, 1.30–3.49, and ≥ 3.50. Marital status was grouped into married and unmarried. Education was stratified into 5 levels: less than 9th grade, 9th-11th grade, high school, some college, and college or above. Based on prior literature’s definition of alcohol consumption, we divided participants into four groups:1) Never drinking: no history of alcohol consumption or former drinkers, 2) Current heavy drinking (≥ 3 drinks/day for women, ≥ 4 drinks/day for men),3) current moderate drinking (≥ 2 drinks/day for women, ≥ 3 drinks/day for men,4) current light drinking: does not meet above [30]. In addition, physical activity was calculated as metabolic equivalent (MET)-minutes/week and classified into 3 categories:<600, 600–1200, and ≥ 1200 MET- minute/week [31].
Statistical analysis
According to NHANES analysis tutorial, a complex survey design was fully considered and dietary 2-day sample weight was applied in the current analyses. Continuous variables were presented as mean and standard error (SE), and categorical variables were expressed as the frequency with percentage. Chi-square test and Student’s t-test were carried out to assess individuals’ baseline characteristics according to MetS status. Based on previously published literature [14], the standard intake of all types of vegetables was 80 g, thus vegetable intake in the current study was stratified into three groups:0 serving/day, < 2 servings/day, and ≥ 2 servings/day. We established three multivariable logistic regression models to analyze the risk of MetS and different kinds of vegetables. Model 1 was a crude model for none variables adjustment. Model 2 was adjusted for age, gender, and race. Model 3 was further adjusted for model 2, plus marital status, PIR, education, smoking, alcohol status, physical activity, serum creatinine, uric acid, ALT, AST, and intake of energy, carbohydrate, whole grains, meat, and nuts. Additionally, we also calculate the odds ratios (ORs) for per standard deviation (SD) increment of different vegetables in these models. We further tested the linear trend by using each vegetable group as an ordinal variable. The potential nonlinear relationship between vegetables and MetS risk was investigated by restricted cubic spline (RCS) analysis. In the RCS model, we adjusted for all the confounding factors mentioned above. Subgroup analyses were used to investigate the stratified correlation between vegetables and MetS risk in different populations. Finally, the likelihood ratio test was used to check the interaction among these subgroups.
Furthermore, we examined the association of specific vegetables with MetS components in a fully-adjusted model to further identify the influence of vegetables on lipid metabolism, glucose metabolism, and blood pressure. All participants with missing values were excluded from the current analysis. The significance level was defined as α = 0.05 and all statistical tests were bilateral. R software (version 4.1.3) was conducted for all statistical analyses.
Results
Characteristics of participants
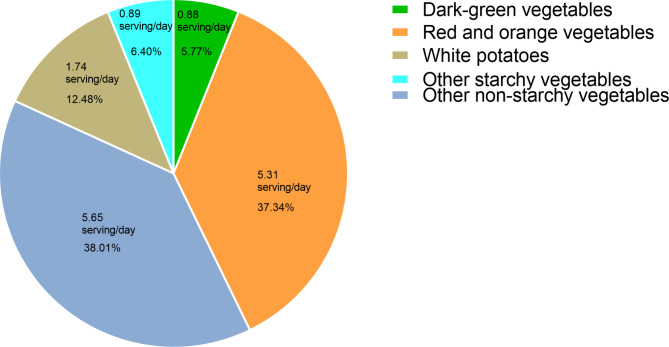
A total of 24,646 eligible participants were enrolled in our study, representing approximately 137.57 million US population. Detailed baseline characteristics are shown in Table 1. Specifically, variables of age, gender, race, education, PIR, marital status, serum creatinine, smoke, and physical activity were all associated with intake of total starchy vegetables and non-starchy vegetables (all p < 0.050). Of the 24,646 study participants, 11,725(47.57%) were females and 12,921(52.43%) were males, with a mean age of 45.84 ± 0.23 years old. Approximately 15,828(64.22%) participants were defined to be with non-MetS and 8818(35.78%) were with MetS. Compared with the non-MetS group, participants with MetS were more likely to be older, male, Non-Hispanic White, non-college-educated, married, have a lower level of PIR, and have a higher level of serum creatinine, uric acid, ALT, and AST. In addition, participants with MetS tend to be inactive in physical activity, be non-smokers and non-drinkers, have higher meat and carbohydrate intake, and have lower intake of fruits, energy, whole grains, and nuts (all p < 0.050). There was no significant difference between the two groups in consumption of fat, refined grains, and coffee (all p > 0.050, Additional file 1: Table S2). Intake of red and orange vegetables and other non-starchy vegetables accounted for a significant portion of total vegetable intake, with 5.31 servings/day (37.34%) of the intake coming from red and orange vegetables, 5.65 servings/day (38.01%) from other non-starchy vegetables, 1.74 servings/day (12.48%) from white potatoes, 0.89serving/day (6.40%) from other starchy vegetables and 0.88 serving/day (5.77%) from dark green vegetables (Fig. 2).
Table 1.
Characteristics of study participants according to individual vegetable intake from NHANES 1999–2018, weighted(n = 24,646)a
| Total starchy vegetables(servings/day) | Total non-starchy vegetables(servings/day) | |||||||
|---|---|---|---|---|---|---|---|---|
| variables | 0 | < 2 | ≥ 2 | P | 0 | < 2 | ≥ 2 | P |
| Age, years | 44.91 ± 0.31 | 46.07 ± 0.34 | 46.50 ± 0.30 | < 0.001 | 44.15 ± 0.63 | 46.28 ± 0.60 | 45.88 ± 0.24 | 0.024 |
| BMI, kg/m2 | 28.26 ± 0.11 | 28.34 ± 0.14 | 28.60 ± 0.13 | 0.076 | 28.85 ± 0.30 | 28.67 ± 0.22 | 28.38 ± 0.09 | 0.146 |
| Gender, n (%) | < 0.001 | 0.016 | ||||||
| Female | 3978(49.54) | 3378(53.80) | 4369(44.37) | 455(46.62) | 951(52.87) | 10,319(48.39) | ||
| Male | 4351(50.46) | 3046(46.20) | 5524(55.63) | 609(53.38) | 905(47.13) | 11,407(51.61) | ||
| Race, n (%) | < 0.001 | < 0.001 | ||||||
| Mexican American | 1412(7.75) | 879(6.21) | 1523(7.31) | 103(4.93) | 247(4.79) | 3464(7.44) | ||
| Non-Hispanic Black | 1484(8.60) | 1336(9.96) | 1742(8.91) | 306(15.77) | 459(13.91) | 3797(8.44) | ||
| Non-Hispanic White | 4190(73.51) | 3353(74.18) | 4905(71.77) | 516(67.60) | 933(72.97) | 10,999(73.23) | ||
| Other races | 1243(10.14) | 856(9.64) | 1723(12.01) | 139(11.70) | 217(8.33) | 3466(10.89) | ||
| Education, n (%) | 0.022 | < 0.001 | ||||||
| Less than 9th grade | 763(3.93) | 405(2.89) | 747(3.62) | 104(5.26) | 194(5.39) | 1617(3.32) | ||
| 9th-11th grade | 1009(8.62) | 745(8.12) | 1213(9.16) | 202(16.38) | 267(11.98) | 2498(8.13) | ||
| High school | 1797(21.83) | 1510(23.27) | 2334(23.18) | 297(30.86) | 508(26.40) | 4836(22.12) | ||
| Some college | 2554(32.44) | 2017(32.04) | 3067(33.08) | 328(32.62) | 553(33.99) | 6757(32.48) | ||
| College or above | 2206(33.18) | 1747(33.67) | 2532(30.97) | 133(14.88) | 334(22.24) | 6018(33.95) | ||
| PIR, n (%) | < 0.001 | < 0.001 | ||||||
| < 1.30 | 2298(19.82) | 1534(16.50) | 2620(17.97) | 409(33.96) | 547(23.09) | 5496(17.18) | ||
| 1.30–3.49 | 3039(32.15) | 2360(33.39) | 3822(36.24) | 386(35.49) | 742(36.92) | 8093(33.82) | ||
| ≥ 3.50 | 2992(48.03) | 2530(50.11) | 3451(45.78) | 269(30.56) | 567(39.99) | 8137(49.00) | ||
| Marital status, n (%) | < 0.001 | < 0.001 | ||||||
| Unmarried | 3967(45.22) | 2785(40.08) | 4294(41.54) | 606(56.86) | 889(45.45) | 9551(41.56) | ||
| Married | 4362(54.78) | 3639(59.92) | 5599(58.46) | 458(43.14) | 967(54.55) | 12,175(58.44) | ||
| Serum creatinine, umol/L | 77.43 ± 0.39 | 77.05 ± 0.35 | 79.27 ± 0.31 | < 0.001 | 82.82 ± 2.02 | 76.89 ± 0.68 | 77.94 ± 0.23 | < 0.001 |
| Uric acid, µmol/L | 321.55 ± 1.34 | 318.41 ± 1.36 | 326.43 ± 1.41 | < 0.001 | 329.55 ± 3.99 | 320.94 ± 2.72 | 322.48 ± 0.98 | 0.197 |
| ALT, U/L | 25.89 ± 0.35 | 25.34 ± 0.35 | 26.32 ± 0.30 | 0.115 | 25.19 ± 0.80 | 26.76 ± 1.40 | 25.88 ± 0.17 | 0.559 |
| AST, U/L | 25.58 ± 0.26 | 25.14 ± 0.28 | 25.44 ± 0.22 | 0.513 | 25.10 ± 0.53 | 25.19 ± 0.45 | 25.44 ± 0.14 | 0.726 |
| Smoke, n (%) | 1837(21.61) | 1255(19.21) | 1922(19.38) | 0.023 | 370(36.19) | 472(25.91) | 4172(18.97) | < 0.001 |
|
Physical activity (MET- minute/week), n (%) |
0.001 | < 0.001 | ||||||
| < 600 | 2918(33.16) | 2450(37.25) | 3378(33.28) | 392(35.84) | 850(45.78) | 7504(33.36) | ||
| 600–1200 | 1236(14.33) | 945(14.73) | 1513(14.62) | 149(14.72) | 268(13.19) | 3277(14.65) | ||
| ≥ 1200 | 4175(52.51) | 3029(48.01) | 5002(52.09) | 523(49.44) | 738(41.02) | 10,945(51.99) | ||
| Alcohol status, n (%) | 0.057 | < 0.001 | ||||||
| Never | 2189(21.05) | 1735(21.83) | 2783(23.52) | 358(29.09) | 610(27.10) | 5739(21.58) | ||
| Mild | 3007(37.55) | 2334(38.75) | 3549(37.22) | 304(27.64) | 630(35.42) | 7956(38.34) | ||
| Moderate | 1369(18.74) | 1132(18.86) | 1555(17.65) | 136(13.86) | 276(17.14) | 3644(18.62) | ||
| Heavy | 1764(22.66) | 1223(20.56) | 2006(21.61) | 266(29.41) | 340(20.34) | 4387(21.46) | ||
Continuous variables were shown as mean ± SE, categorical variables were shown as frequency(percentage)
aAll estimates accounted for complex survey designs, and all percentages were weighted
Abbreviations: MetS, metabolic syndrome; PIR, poverty income ratio; ALT, alanine aminotransferase; AST, aspartate aminotransferase; MET, metabolic equivalent; SE, standard error
Fig. 2.
Proportions of specific vegetable intake that contributes to total vegetable intake
Association between vegetables and MetS
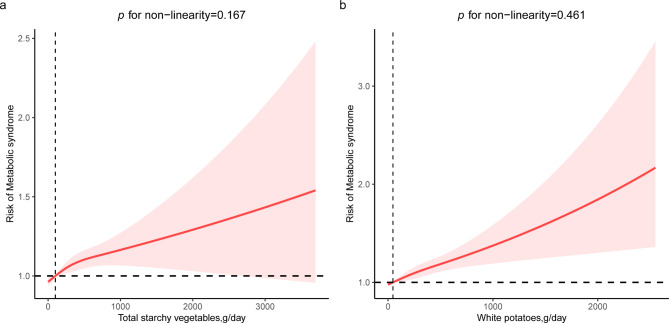
After adjusting for all confounders, consuming two or more servings of daily total starchy vegetables was related to a higher risk of MetS compared with consuming none (OR = 1.14,95%CI: 1.02–1.28, p for trend = 0.028), and the ORs(95%CI) per SD increment was 1.06(1.02–1.11) (Table 2). Furthermore, results displayed that higher white potato intake was linked to a higher risk of MetS (OR = 1.16,95%CI:1.04–1.30, p for trend = 0.011) with the corresponding ORs(95%CI) per SD increment was 1.08(1.04–1.13) (Table 2). However, no association between other starchy vegetable intake and MetS risk was found. In the multivariate-adjusted RCS model, we further observed a linear positive association between total starchy vegetables and MetS risk, and the non-linear p was 0.167 (Fig. 3). A similar positive relationship between white potatoes and the risk of MetS was observed for the same comparison. Consuming ≥ 2 servings/day of dark-green vegetables was associated with reduced risk of MetS when compared with participants consuming none (OR = 0.86, 95%CI:0.76–0.98, p for trend = 0.010), and the corresponding OR (95%CI) per SD increment was 0.93 (0.90,0.97) (Table 3). No significant associations of total non-starchy vegetables, red and orange vegetables, and other non-starchy vegetables on MetS were observed in the fully-adjusted model.
Table 2.
Association between starchy vegetable consumption and MetS risk
| Category of starchy vegetable intake | P trend | ||||
|---|---|---|---|---|---|
| 0 serving/day | < 2 servings/day | ≥ 2 servings/day | Per SD increase | ||
|
Total starchy vegetables (0-6249.13 g/day) |
|||||
| No. of participants | 8329 | 6424 | 9893 | ||
| Model 1 | Ref | 1.03(0.92,1.14) | 1.23(1.11,1.35) | 1.12(1.07,1.16) | < 0.001 |
| Model 2 | Ref | 1.00(0.90,1.12) | 1.16(1.05,1.28) | 1.09(1.05,1.14) | 0.004 |
| Model 3 | Ref | 0.98(0.88,1.10) | 1.14(1.02, 1.28) | 1.06(1.02,1.11) | 0.028 |
|
White potatoes (0-3828.25 g/day) |
|||||
| No. of participants | 10,745 | 6430 | 7471 | ||
| Model 1 | Ref | 1.08(0.98,1.20) | 1.28(1.17,1.41) | 1.12(1.08,1.17) | < 0.001 |
| Model 2 | Ref | 1.08(0.97,1.20) | 1.23(1.12,1.36) | 1.12(1.07,1.16) | < 0.001 |
| Model 3 | Ref | 1.04(0.93,1.16) | 1.16(1.04,1.30) | 1.08(1.04,1.13) | 0.011 |
|
Other starchy vegetables (0-3568.88 g/day) |
|||||
| No. of participants | 17,646 | 3067 | 3933 | ||
| Model 1 | Ref | 1.09(0.97,1.22) | 1.12(1.01,1.24) | 1.05(1.01,1.09) | 0.020 |
| Model 2 | Ref | 0.97(0.86,1.10) | 1.01(0.90,1.12) | 1.02(0.98,1.06) | 0.921 |
| Model 3 | Ref | 0.97(0.85,1.10) | 0.98(0.87,1.10) | 0.99(0.95,1.04) | 0.615 |
Model 1: None
Model 2: Age, gender, race
Model 3: Age, gender, race, marital status, PIR, BMI, education, smoking, alcohol status, physical activity, serum creatinine, uric acid, ALT, AST, energy, fruits, carbohydrate, whole grains, meat, nuts, and non-starchy vegetables. Of note, potatoes and other starchy vegetables were mutually adjusted
Fig. 3.
Restricted cubic spline analysis (RCS) with multivariate-adjusted associations between starchy vegetables and the risk of MetS. (a) RCS analysis between total starchy vegetable intake and MetS risk. (b) RCS analysis between white potatoes intake and MetS risk
Age, gender, race, marital status, PIR, BMI, education, smoking, alcohol status, physical activity, serum creatinine, uric acid, ALT, AST, energy, fruits, carbohydrate, whole grains, meat, nuts, and non-starchy vegetables. Of note, other starchy vegetables were further adjusted in RCS analysis for white potatoes
Table 3.
Association between non-starchy vegetable consumption and MetS risk
| Category of non-starchy vegetable intake | P trend | ||||
|---|---|---|---|---|---|
| 0 serving/day | < 2 servings/day | ≥ 2 servings/day | Per SD increase | ||
|
Total non-starchy vegetables (0-10791.56 g/day) |
|||||
| No. of participants | 1064 | 1856 | 21,726 | ||
| Model 1 | Ref | 0.95(0.76,1.20) | 0.88(0.75,1.04) | 1.01(0.97,1.05) | 0.039 |
| Model 2 | Ref | 0.88(0.70,1.12) | 0.81(0.68,0.95) | 1.03(0.98,1.07) | 0.003 |
| Model 3 | Ref | 0.92(0.72,1.18) | 0.89(0.74,1.07) | 1.03(0.98,1.08) | 0.175 |
|
Dark-green vegetables (0-3819.19 g/day) |
|||||
| No. of participants | 16,707 | 4023 | 3916 | ||
| Model 1 | Ref | 0.85(0.77,0.94) | 0.77(0.69,0.86) | 0.93(0.89,0.97) | < 0.001 |
| Model 2 | Ref | 0.77(0.69,0.86) | 0.73(0.65,0.81) | 0.92(0.88,0.97) | < 0.001 |
| Model 3 | Ref | 0.89(0.79,1.00) | 0.86(0.76,0.98) | 0.93(0.90,0.97) | 0.010 |
|
Red and orange vegetables (0-7105.43 g/day) |
|||||
| No. of participants | 3127 | 4922 | 16,597 | ||
| Model 1 | Ref | 0.89(0.78,1.02) | 0.89(0.80,1.00) | 1.03(0.98,1.08) | 0.110 |
| Model 2 | Ref | 0.90(0.78,1.04) | 0.91(0.80,1.03) | 1.05(1.00,1.10) | 0.231 |
| Model 3 | Ref | 0.98(0.83,1.16) | 1.01(0.87, 1.17) | 1.05(0.99,1.11) | 0.088 |
|
Other non-starchy vegetables (0-8470.33 g/day) |
|||||
| No. of participants | 2401 | 3942 | 18,303 | ||
| Model 1 | Ref | 1.00(0.85,1.17) | 0.97(0.85,1.10) | 1.02(0.98,1.06) | 0.485 |
| Model 2 | Ref | 0.91(0.77,1.08) | 0.87(0.76,0.99) | 1.03(0.99,1.07) | 0.028 |
| Model 3 | Ref | 0.94(0.78,1.13) | 0.93(0.80,1.08) | 1.04(0.99,1.10) | 0.409 |
Model 1: None
Model 2: Age gender, race
Model 3: Age, gender, race, marital status, PIR, BMI, education, smoking, alcohol status, physical activity, serum creatinine, uric acid, ALT, AST, energy, fruits, carbohydrate, whole grains, meat, nuts, and starchy vegetables. Of note, dark-green vegetables, red and orange vegetables, and other non-starchy vegetables were mutually adjusted
Relation between individual MetS components and specific vegetables
Table 4 summarized the results of specific vegetables on an individual component of MetS after controlling all covariates. Participants consuming ≥ 2 servings/day total starchy vegetables were 1.13-fold odds of hyperglycemia (OR = 1.13,95%CI:1.01,1.26) than participants consuming none total starchy vegetables. Similarly, intake of white potatoes ≥ 2 servings/day was related to increased risk of hyperglycemia and central obesity, with the corresponding ORs(95%CIs) being 1.15(1.03,1.28) and 1.22(1.08,1.38), respectively. However, dark-green vegetables were related to decreased risk of reduced HDL(OR = 0.83,95%CI:0.76,0.92), central obesity (OR = 0.77,95%CI:0.67,0.89), and hypertension (OR = 0.87,95%CI:0.76,1.00).
Table 4.
Association between specific vegetable consumption and individual MetS component
| 0 serving/day | < 2 servings/day | ≥ 2 servings/day | |||
|---|---|---|---|---|---|
|
Total starchy vegetablesa (0-10791.56 g/day) |
OR (95%CI) | P | OR (95%CI) | P | |
| Hyperglycemia | Ref | 1.01(0.88,1.15) | 0.917 | 1.13(1.01,1.26) | 0.033 |
| Reduced HDL | Ref | 1.05(0.94,1.17) | 0.407 | 1.10(0.99,1.23) | 0.082 |
| Hypertriglyceridemia | Ref | 0.94(0.84,1.06) | 0.328 | 1.05(0.95,1.15) | 0.363 |
| Central obesity | Ref | 0.99(0.87,1.13) | 0.916 | 1.04(0.93,1.17) | 0.502 |
| Hypertension | Ref | 1.05(0.94,1.18) | 0.392 | 1.08(0.97,1.21) | 0.151 |
|
White potatoes b (0-3828.25 g/day) |
|||||
| Hyperglycemia | Ref | 1.06(0.92,1.21) | 0.414 | 1.15(1.03,1.28) | 0.015 |
| Reduced HDL | Ref | 1.02(0.92,1.12) | 0.727 | 1.11(0.99,1.23) | 0.062 |
| Hypertriglyceridemia | Ref | 0.98(0.87,1.09) | 0.669 | 1.08(0.97,1.19) | 0.144 |
| Central obesity | Ref | 1.08(0.94,1.23) | 0.278 | 1.22(1.08,1.38) | 0.002 |
| Hypertension | Ref | 1.08(0.97,1.20) | 0.176 | 1.11(0.99,1.24) | 0.063 |
|
Dark-green vegetables c (0-3819.19 g/day) |
|||||
| Hyperglycemia | Ref | 0.96(0.84,1.09) | 0.490 | 0.98(0.88,1.10) | 0.759 |
| Reduced HDL | Ref | 0.87(0.77,0.99) | 0.032 | 0.83(0.76,0.92) | < 0.001 |
| Hypertriglyceridemia | Ref | 0.94(0.84,1.06) | 0.301 | 0.90(0.80,1.01) | 0.081 |
| Central obesity | Ref | 0.87(0.76,1.01) | 0.070 | 0.77(0.67,0.89) | < 0.001 |
| Hypertension | Ref | 0.90(0.79,1.02) | 0.108 | 0.87(0.76,1.00) | 0.044 |
aAdjusted for age, gender, race, marital status, PIR, BMI, education, smoking, alcohol status, physical activity, serum creatinine, uric acid, ALT, AST, energy, fruits, carbohydrate, whole grains, meat, nuts, and non-starchy vegetables
bAdjusted for age, gender, race, marital status, PIR, BMI, education, smoking, alcohol status, physical activity, serum creatinine, uric acid, ALT, AST, energy, fruits, carbohydrate, whole grains, meat, nuts, non-starchy vegetables, and other starchy vegetables
cAdjusted for age, gender, race, marital status, PIR, BMI, education, smoking, alcohol status, physical activity, serum creatinine, uric acid, ALT, AST, energy, fruits, carbohydrate, whole grains, meat, nuts, starchy vegetables, red and orange vegetables, and other non-starchy vegetables
Subgroup analyses
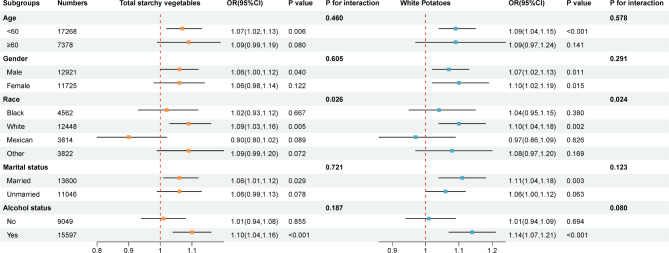
Subgroup analyses were performed to further understand the association between vegetables and MetS risk among different populations. As shown in Fig. 4, we observed both total starchy vegetables and white potatoes were positively associated with MetS risk in non-Hispanic White participants, and a significant interaction was found (both p for interaction < 0.050).
Fig. 4.
Subgroup analysis of the association between starchy vegetables (per SD increase) and MetS risk
Age, gender, race, marital status, PIR, BMI, education, smoking, alcohol status, physical activity, serum creatinine, uric acid, ALT, AST, energy, fruits, carbohydrate, whole grains, meat, nuts, and non-starchy vegetables. Of note, other starchy vegetables were further adjusted in subgroup analysis for white potatoes
Discussion
In this large observational research among American adults, we found consumption of total starchy vegetables and white potatoes displayed a positive correlation with an increased risk of MetS, whereas consumption of dark green vegetables demonstrated a negative correlation with a decreased risk of MetS. Subgroup analyses revealed that these affirmative associations were even more pronounced in the non-Hispanic white population. Although current dietary guidelines generally treat all types of vegetables equally, these findings highlight potentially distinct health effects of different subgroups of vegetables [32].
It is noteworthy that most previous studies primarily focused on dietary patterns or total vegetable consumption without considering the potential impact that particular vegetable subtypes on MetS. A study conducted in Tehran revealed that sufficient vegetable consumption could potentially lower the incidence of MetS in children and adolescents [33]. A meta-analysis of 26 observational studies reported that vegetable intake was negatively related to MetS [8], whereas another meta-analysis of 8 randomized controlled trials suggested that vegetable consumption was only associated with the decrease of diastolic blood pressure, but did not affect other MetS components. Until now, the relationship between intake of starchy vegetables and MetS remains controversial. A cross-sectional study conducted in Costa Rica found that consuming more starchy vegetables may not be related to the increasing prevalence of MetS [18], but a cohort study from China showed a positive association between total carbohydrate intake from starchy foods and MetS [34], which was in line with our findings. This discrepancy could be explained in part by differences in dietary patterns, as well as the exclusion of unhealthy starchy vegetables in the Costa Rica study, which were defined as potatoes including baked/boiled/mashed potatoes, French fries, and potato chips. Costa Rica’s dietary patterns emphasize fresh vegetables, legumes, and cereals as the main sources of starchy vegetable intake, with less red meat consumption [35, 36]. In contrast, the Western diet in the United States includes less favorable choices such as French fries, potato chips, and mashed potatoes, often accompanied by increased intake of processed meat, red meat, and refined flour [37]. Further multicenter prospective cohort studies are required to better understand the association between different types of vegetables and MetS.
Potatoes were widely consumed starchy food in many countries, as well as a good source of fiber and vitamins like folate, potassium, iron, vitamin B6, and vitamin C [38]. Remarkably, in contrast to the US Dietary Guidelines, the World Health Organization, and some previous studies did not consider potatoes to be vegetables [39, 40]. White potato intake, especially fried potatoes, has been linked to weight gain, hypertension, type 2 diabetes, and mortality in previous research [13, 41–43]. On the contrary, another study in 1881 Costa Rican adults found no conclusive links between increased potato consumption and the incidence of MetS [18]. However, in our study, white potatoes were positively associated with MetS. As part of an unhealthy Western dietary pattern, white potatoes were commonly served as French fries, potato chips, and mashed potatoes, which could help to explain the positive association between white potatoes and MetS.
According to our findings, there was a positive significant association between total starchy vegetables and hyperglycemia. A similar positive association of white potatoes with hyperglycemia and central obesity was found. Some biological mechanisms might be able to explain our findings. Numerous pieces of evidence have demonstrated that insulin resistance exerts a pivotal role in the pathogenesis of MetS [44]. Starchy vegetables are generally able to quickly elevate blood glucose levels, thereby increasing glycemic load and insulin response [23]. The glycemic index was altered by the variety of potato, as well as how it was cooked or processed [45]. The average GI value of tested potatoes in North America was 67 ± 16, which was lower than those of Australia and Europe. Phy et al. observed that low-starch diets provided benefits such as weight loss, lower blood lipid levels, and enhanced insulin sensitivity [46]. By contrast, non-starchy vegetables contain dietary fiber that can aid in lowering blood sugar, cholesterol, and weight loss [47].
Furthermore, the occurrence and progression of metabolic syndrome are partly influenced by oxidative stress. Several antioxidant nutrients, flavonoids, minerals, dietary fiber, phytochemicals, and phenols found in non-starchy vegetables, particularly green leafy vegetables, can lessen deoxyribonucleic acid (DNA) damage and oxidative stress brought on by free radicals [48], as well as vivo lipid peroxidation [49]. Folic acid, magnesium, and vitamin B2 acid are all abundant in dark-green vegetables. In a prospective cohort from the CARDIA study, sufficient intake of folic acid, vitamin B6, and vitamin B12 might help prevent metabolic syndrome [50]. Magnesium has been demonstrated to have antioxidant, anti-inflammatory, and anti-diabetic capabilities [51], and it was found to be significantly inversely related to the occurrence of MetS [52, 53]. Potatoes are also rich in antioxidant ingredients, such as chlorogenic acids and ascorbic [54]. Simultaneously, the antioxidative potency during the peeling and cooking phases may experience a marked diminution [16]. According to reports, the amount of antioxidants in potatoes varies significantly depending on genotype, environment, and planting year. In comparison to pigmented potatoes such as yellow and purple potatoes, the consumption of white potatoes may not reduce DNA oxidative damage and inflammation [55].
The development of MetS is also accompanied with chronic low-grade inflammation [9, 56]. Kerrie L et al. enrolled healthy male adult participants from Washington and found that consumption of white potatoes rather than yellow or purple potatoes could increase C-reactive protein (CRP) and Interleukin 6 (IL-6) concentrations [55]. Apart from potatoes, a higher quantity of vegetables and fruits was linked to decreased CRP plasma concentrations [39]. A proinflammatory nutritional pattern, which included potatoes, was created by Janett et al. and was linked to circulating levels of CRP and IL-6 [57]. Additionally, the consumption of potato chips may elevate CRP and IL-6 levels, probably due to acrylamide, which is a vital cellular antioxidant and can decrease glutathione stores [58]. However, the Mediterranean diet, which is abundant in fruit and vegetables, has been reported to reduce plasma markers of inflammation and endothelial dysfunction [59].
The observed positive association between total starchy vegetables and white potatoes with MetS risk in non-Hispanic White participants could be due to several factors, including lifestyle, dietary patterns, and genetic predisposition. Non-Hispanic whites were reported to have dietary habits and preferences characterized by lower fruit and vegetable consumption, along with a higher intake of potatoes, bread, and vegetables paired with butter, margarine, or fats [60]. From 2011 to 2018, non-Hispanic whites showed a significant decrease in their HEI-2015 score [61], indicating diet quality trends varied across different race/ethnicity groups. Alternatively, the outcomes might be the consequence of chance. Additional research is warranted to confirm these findings and clarify the underlying mechanisms.
Our study has several noteworthy advantages. First of all, our study data is established on the NHANES database, which provides a large-scale and nationally representative database, making our study findings reliable. Second, our study is the first study to explore the potential impact of starchy vegetables and non-starchy vegetables on MetS, which has not been investigated in other studies. Third, analyses investigating the association of specific vegetables with individual MetS components are performed to provide robustness to our results.
Of note, several limitations should be pointed out in our research. In fact, the nature of the cross-sectional study precludes us from establishing causality between the vegetables and MetS, thus future longitudinal studies are needed. In addition, although our analysis provides details on vegetable intake, we regrettably omitted the consideration of various cooking methods in our analysis. Prior studies have indicated that disparate cooking or processing techniques might exert an impact on the nutrient composition and glycemic index (GI) of potatoes [62]. Moreover, the dietary intake survey was collected through 24-h recall interviews, which might have recall bias and not accurately reflect the daily intake of U.S. adults. Finally, although some conventional variables are fully controlled in the current study, other unmeasured confounders are not considered.
Conclusion
In summary, the current study findings revealed that the consumption of total starchy vegetables and white potatoes were both positively correlated with an increased risk of MetS, whereas the intake of dark-green vegetables exhibited a negative association with the risk of MetS. These findings provide a promising and healthy strategy for public to prevent MetS. Subsequent prospective cohort investigations are imperative to ascertain the causality of these findings and to delve into the potential underlying mechanisms.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Additional file 1. Table S1. The definitions of starchy and non-starchy vegetables according to FPED 2017-2018. Table S2. Characteristics of study participants by MetS status, weighted (n=24646)a
Acknowledgements
We thank the NHANES staff for their excellent work on study design and data collection.
Abbreviations
- ALT
Alanine aminotransferase
- AST
Aspartate aminotransferase
- CI
Confidence interval
- CRP
C-reactive protein
- DBP
Diastolic blood pressure
- DNA
Deoxyribonucleic acid
- FPED
Food Pattern Equivalent Database
- GI
Glycemic index
- HDL
High density cholesterols
- IL-6
Interleukin 6
- MEC
Mobile examination center
- MetS
Metabolic syndrome
- NCEP ATPIII
National Cholesterol Education Program-Adult treatment Panel III
- NCHS
National Center for Health Statistics
- NHANES
National Health and Nutrition Examination Survey
- OR
Odds ratio
- PIR
Poverty income ratio
- RCS
Restricted cubic spline
- SBP
Systolic blood pressure
- SD
Standard deviation
- SE
Standard error
- US
United States
Authors’ contributions
YL, BX, MZ, and YR had the main responsibility for data analysis and writing the manuscript. YL, BX, MZ, YR, YL, TH, YW, HY, ZL, KX, and QS contributed to the conception and design of the study, analysis, and interpretation of the data, and drafting of the manuscript. YL,TH, YW, HY, ZL, and KX contributed to the acquisition of data. QS is the guarantor. All authors contributed to the writing and final approval of the manuscript.
Funding
Not applicable.
Data Availability
The datasets generated and/or analyzed are available from the corresponding.
author on reasonable request.
Declarations
Ethics approval and consent to participate
The NHANES is a public database. The patients involved in the database received ethical approval. Users can download relevant data for free for research and publication purposes.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Yingrui Li, Bingquan Xiong, Min Zhu and Yuqian Ren contributed equally to this work.
References
- 1.Castro-Barquero S, Ruiz-León A, Sierra-Pérez M, Estruch R, Casas R. Dietary strategies for metabolic syndrome: a Comprehensive Review. Nutrients. 2020;12(10):2983. doi: 10.3390/nu12102983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fahed G, Aoun L, Bou Zerdan M, Allam S, Bou Zerdan M, Bouferraa Y, et al. Metabolic syndrome: updates on pathophysiology and management in 2021. Int J Mol Sci. 2022;23(2):786. doi: 10.3390/ijms23020786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kassi E, Pervanidou P, Kaltsas G, Chrousos G. Metabolic syndrome: definitions and controversies. BMC Med. 2011;9:48. doi: 10.1186/1741-7015-9-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lemieux I, Després JP. Metabolic syndrome: past, Present and Future. Nutrients. 2020;12(11):3501. doi: 10.3390/nu12113501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Saklayen MG. The global epidemic of the metabolic syndrome. Curr Hypertens Rep. 2018;20(2):12. doi: 10.1007/s11906-018-0812-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Li W, Qiu X, Ma H, Geng Q. Incidence and long-term specific mortality trends of metabolic syndrome in the United States. Front Endocrinol (Lausanne) 2022;13:1029736. doi: 10.3389/fendo.2022.1029736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ambroselli D, Masciulli F, Romano E, Catanzaro G, Besharat Z, Massari M, et al. New advances in metabolic syndrome, from Prevention to Treatment: the role of Diet and Food. Nutrients. 2023;15(3):640. doi: 10.3390/nu15030640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhang Y, Zhang DZ. Associations of vegetable and fruit consumption with metabolic syndrome. A meta-analysis of observational studies. Public Health Nutr. 2018;21(9):1693–703. doi: 10.1017/S1368980018000381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gantenbein K, Kanaka-Gantenbein C. Mediterranean Diet as an antioxidant: the impact on Metabolic Health and overall wellbeing. Nutrients. 2021;13(6):1951. doi: 10.3390/nu13061951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bertoia ML, Mukamal KJ, Cahill LE, Hou T, Ludwig DS, Mozaffarian D, et al. Correction: changes in intake of fruits and vegetables and Weight Change in United States Men and Women followed for up to 24 years: analysis from three prospective cohort studies. PLoS Med. 2016;13(1):e1001956. doi: 10.1371/journal.pmed.1001956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bertoia M, Mukamal K, Cahill L, Hou T, Ludwig D, Mozaffarian D, et al. Changes in intake of fruits and vegetables and Weight Change in United States Men and Women followed for up to 24 years: analysis from three prospective cohort studies. PLoS Med. 2015;12(9):e1001878. doi: 10.1371/journal.pmed.1001878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Carter P, Gray LJ, Troughton J, Khunti K, Davies MJ. Fruit and vegetable intake and incidence of type 2 diabetes mellitus: systematic review and meta-analysis. BMJ. 2010;341:c4229. doi: 10.1136/bmj.c4229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Borgi L, Rimm EB, Willett WC, Forman JP. Potato intake and incidence of hypertension: results from three prospective US cohort studies. BMJ. 2016;353:i2351. doi: 10.1136/bmj.i2351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang D, Li Y, Bhupathiraju S, Rosner B, Sun Q, Giovannucci E, et al. Fruit and Vegetable Intake and Mortality: results from 2 prospective cohort studies of US Men and Women and a Meta-analysis of 26 Cohort Studies. Circulation. 2021;143(17):1642–54. doi: 10.1161/CIRCULATIONAHA.120.048996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Barclay AW, Petocz P, McMillan-Price J, Flood VM, Prvan T, Mitchell P, et al. Glycemic index, glycemic load, and chronic disease risk–a meta-analysis of observational studies. Am J Clin Nutr. 2008;87(3):627–37. doi: 10.1093/ajcn/87.3.627. [DOI] [PubMed] [Google Scholar]
- 16.Furrer AN, Chegeni M, Ferruzzi MG. Impact of potato processing on nutrients, phytochemicals, and human health. Crit Rev Food Sci Nutr. 2018;58(1):146–68. doi: 10.1080/10408398.2016.1139542. [DOI] [PubMed] [Google Scholar]
- 17.Zhang T, Peng Z, Li H, Liang S, Liu M, Ye S, et al. A prospective cohort study of starchy and non-starchy vegetable intake and mortality risk. Br J Nutr. 2023;130(4):719–27. doi: 10.1017/S0007114522003518. [DOI] [PubMed] [Google Scholar]
- 18.Li Z, Wang D, Ruiz-Narváez EA, Peterson KE, Campos H, Baylin A. Starchy vegetables and metabolic syndrome in Costa Rica. Nutrients. 2021;13(5):1639. doi: 10.3390/nu13051639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang DD, Li Y, Bhupathiraju SN, Rosner BA, Sun Q, Giovannucci EL, et al. Fruit and Vegetable Intake and Mortality: results from 2 prospective cohort studies of US Men and Women and a Meta-analysis of 26 Cohort Studies. Circulation. 2021;143(17):1642–54. doi: 10.1161/CIRCULATIONAHA.120.048996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jayedi A, Soltani S, Jenkins D, Sievenpiper J, Shab-Bidar S. Dietary glycemic index, glycemic load, and chronic disease: an umbrella review of meta-analyses of prospective cohort studies. Crit Rev Food Sci Nutr. 2022;62(9):2460–9. doi: 10.1080/10408398.2020.1854168. [DOI] [PubMed] [Google Scholar]
- 21.Hughes M, Antonsson A, Rodriguez-Acevedo A, Liyanage U, Green A, van der Pols JC. Dark Green Leafy Vegetable Intake, MTHFR genotype, and risk of cutaneous squamous cell carcinoma. Dermatology. 2022;238(4):657–61. doi: 10.1159/000520941. [DOI] [PubMed] [Google Scholar]
- 22.Sun J, Li Z, Li Y, Zhang D. Intakes of specific categories of vegetables and fruits are inversely Associated with depressive symptoms among adults. J Epidemiol. 2021;31(3):210–9. doi: 10.2188/jea.JE20200003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li X, Zhang T, Li H, Zhou Z, Li M, Zeng X, et al. Associations between intake of starchy and non-starchy vegetables and risk of hepatic steatosis and fibrosis. Hepatol Int. 2022;16(4):846–57. doi: 10.1007/s12072-022-10368-x. [DOI] [PubMed] [Google Scholar]
- 24.Lu YT, Gunathilake M, Kim J. The influence of dietary vegetables and fruits on endometrial cancer risk: a meta-analysis of observational studies. Eur J Clin Nutr. 2023;77(5):561–73. doi: 10.1038/s41430-022-01213-3. [DOI] [PubMed] [Google Scholar]
- 25.Li N, Wu X, Zhuang W, Xia L, Chen Y, Wang Y, et al. Green leafy vegetable and lutein intake and multiple health outcomes. Food Chem. 2021;360:130145. doi: 10.1016/j.foodchem.2021.130145. [DOI] [PubMed] [Google Scholar]
- 26.Phillips JA. Dietary guidelines for Americans, 2020–2025. Workplace Health Saf. 2021;69(8):395. doi: 10.1177/21650799211026980. [DOI] [PubMed] [Google Scholar]
- 27.National Center for Health Statistics. Centers for Disease Control and Prevention NCHS research ethics review board (ERB) approval. https://www.cdc.gov/nchs/nhanes/irba98.htm.
- 28.Wan J, Li X, Gu M, Li Q, Wang C, Yuan R, et al. The association of dietary resistance starch intake with all-cause and cause-specific mortality. Front Nutr. 2022;9:1004667. doi: 10.3389/fnut.2022.1004667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Alberti K, Eckel R, Grundy S, Zimmet P, Cleeman J, Donato K, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the study of obesity. Circulation. 2009;120(16):1640–5. doi: 10.1161/CIRCULATIONAHA.109.192644. [DOI] [PubMed] [Google Scholar]
- 30.Rattan P, Penrice D, Ahn J, Ferrer A, Patnaik M, Shah V, et al. Inverse Association of Telomere length with Liver Disease and Mortality in the US Population. Hepatol Commun. 2022;6(2):399–410. doi: 10.1002/hep4.1803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Che Z, Jia H, Chen R, Pan K, Fan Z, Su C, et al. Associations between exposure to brominated flame retardants and metabolic syndrome and its components in U.S. adults. Sci Total Environ. 2023;858:159935. doi: 10.1016/j.scitotenv.2022.159935. [DOI] [PubMed] [Google Scholar]
- 32.Arnold M, Harding M, Conley A. Dietary guidelines for Americans 2020–2025: recommendations from the U.S. Departments of Agriculture and Health and Human Services. Am Fam Physician. 2021;104(5):533–6. [PubMed] [Google Scholar]
- 33.Hosseinpour-Niazi S, Bakhshi B, Betru E, Mirmiran P, Darand M, Azizi F. Prospective study of total and various types of vegetables and the risk of metabolic syndrome among children and adolescents. World J Diabetes. 2019;10(6):362–75. doi: 10.4239/wjd.v10.i6.362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Feng R, Du S, Chen Y, Zheng S, Zhang W, Na G, et al. High carbohydrate intake from starchy foods is positively associated with metabolic disorders: a Cohort Study from a chinese population. Sci Rep. 2015;5:16919. doi: 10.1038/srep16919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Luan D, Wang D, Campos H, Baylin A. Red meat consumption and metabolic syndrome in the Costa Rica Heart Study. Eur J Nutr. 2020;59(1):185–93. doi: 10.1007/s00394-019-01898-6. [DOI] [PubMed] [Google Scholar]
- 36.Pes G, Dore M, Tsofliou F, Poulain M. Diet and longevity in the Blue Zones: a set-and-forget issue? Maturitas. 2022, 164:31–7. [DOI] [PubMed]
- 37.Drake I, Sonestedt E, Ericson U, Wallström P, Orho-Melander M. A western dietary pattern is prospectively associated with cardio-metabolic traits and incidence of the metabolic syndrome. Br J Nutr. 2018;119(10):1168–76. doi: 10.1017/S000711451800079X. [DOI] [PubMed] [Google Scholar]
- 38.Robertson T, Alzaabi A, Robertson M, Fielding B. Starchy Carbohydrates in a healthy Diet: the role of the humble potato. Nutrients. 2018;10(11):1764. doi: 10.3390/nu10111764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Esmaillzadeh A, Kimiagar M, Mehrabi Y, Azadbakht L, Hu FB, Willett WC. Fruit and vegetable intakes, C-reactive protein, and the metabolic syndrome. Am J Clin Nutr. 2006;84(6):1489–97. doi: 10.1093/ajcn/84.6.1489. [DOI] [PubMed] [Google Scholar]
- 40.McGuire S, U.S. Department of Agriculture and U.S. Department of Health and Human Services., Dietary Guidelines for Americans, 2010. 7th Edition, Washington, DC: U.S. Government Printing Office, January 2011. Adv Nutr. 2011, 2(3):293–294. [DOI] [PMC free article] [PubMed]
- 41.Mozaffarian D, Hao T, Rimm E, Willett W, Hu F. Changes in diet and lifestyle and long-term weight gain in women and men. N Engl J Med. 2011;364(25):2392–404. doi: 10.1056/NEJMoa1014296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Muraki I, Rimm E, Willett W, Manson J, Hu F, Sun Q. Potato consumption and risk of type 2 diabetes: results from three prospective cohort studies. Diabetes Care. 2016;39(3):376–84. doi: 10.2337/dc15-0547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Veronese N, Stubbs B, Noale M, Solmi M, Vaona A, Demurtas J, et al. Fried potato consumption is associated with elevated mortality: an 8-y longitudinal cohort study. Am J Clin Nutr. 2017;106(1):162–7. doi: 10.3945/ajcn.117.154872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Guo S. Insulin signaling, resistance, and the metabolic syndrome: insights from mouse models into disease mechanisms. J Endocrinol. 2014;220(2):T1–T23. doi: 10.1530/JOE-13-0584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Atkinson FS, Brand-Miller JC, Foster-Powell K, Buyken AE, Goletzke J. International tables of glycemic index and glycemic load values 2021: a systematic review. Am J Clin Nutr. 2021;114(5):1625–32. doi: 10.1093/ajcn/nqab233. [DOI] [PubMed] [Google Scholar]
- 46.Phy JL, Pohlmeier AM, Cooper JA, Watkins P, Spallholz J, Harris KS, et al. Low Starch/Low dairy Diet results in successful treatment of obesity and co-morbidities linked to polycystic ovary syndrome (PCOS) J Obes Weight Loss Ther. 2015;5(2):259. doi: 10.4172/2165-7904.1000259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Fuller S, Beck E, Salman H, Tapsell L. New Horizons for the study of Dietary Fiber and Health: a review. Plant Foods Hum Nutr. 2016;71(1):1–12. doi: 10.1007/s11130-016-0529-6. [DOI] [PubMed] [Google Scholar]
- 48.Yu EY-W, Wesselius A, Mehrkanoon S, Goosens M, Brinkman M, van den Brandt P, et al. Vegetable intake and the risk of bladder cancer in the BLadder Cancer Epidemiology and Nutritional determinants (BLEND) international study. BMC Med. 2021;19(1):56. doi: 10.1186/s12916-021-01931-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.O’Sullivan A, Armstrong P, Schuster G, Pedersen T, Allayee H, Stephensen C, et al. Habitual diets rich in dark-green vegetables are associated with an increased response to ω-3 fatty acid supplementation in Americans of African ancestry. J Nutr. 2014;144(2):123–31. doi: 10.3945/jn.113.181875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Zhu J, Chen C, Lu L, Shikany J, D’Alton M, Kahe K, Folate Vitamin B6, and vitamin B12 Status in Association with metabolic syndrome incidence. JAMA Netw Open. 2023;6(1):e2250621. doi: 10.1001/jamanetworkopen.2022.50621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Shin S, Lee J, Loftfield E, Shu X, Abe S, Rahman M, et al. Coffee and tea consumption and mortality from all causes, cardiovascular disease and cancer: a pooled analysis of prospective studies from the Asia Cohort Consortium. Int J Epidemiol. 2022;51(2):626–40. doi: 10.1093/ije/dyab161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Yang N, He L, Li Y, Xu L, Ping F, Li W, et al. Reduced insulin resistance partly mediated the Association of High Dietary Magnesium Intake with less metabolic syndrome in a large Chinese Population. Diabetes Metab Syndr Obes. 2020;13:2541–50. doi: 10.2147/DMSO.S257884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Piuri G, Zocchi M, Della Porta M, Ficara V, Manoni M, Zuccotti G, et al. Magnesium in obesity, metabolic syndrome, and type 2 diabetes. Nutrients. 2021;13(2):320. doi: 10.3390/nu13020320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Akyol H, Riciputi Y, Capanoglu E, Caboni M, Verardo V. Phenolic Compounds in the Potato and its byproducts: an overview. Int J Mol Sci. 2016;17(6):835. doi: 10.3390/ijms17060835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kaspar K, Park J, Brown C, Mathison B, Navarre D, Chew B. Pigmented potato consumption alters oxidative stress and inflammatory damage in men. J Nutr. 2011;141(1):108–11. doi: 10.3945/jn.110.128074. [DOI] [PubMed] [Google Scholar]
- 56.Stadler J, Marsche G. Obesity-related changes in high-density lipoprotein metabolism and function. Int J Mol Sci. 2020;21(23):8985. doi: 10.3390/ijms21238985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Barbaresko J, Rienks J, Oluwagbemigun K, Jacobs G, Lieb W, Laudes M, et al. Dietary patterns associated with inflammatory biomarkers in a northern german population. Eur J Nutr. 2020;59(4):1433–41. doi: 10.1007/s00394-019-02000-w. [DOI] [PubMed] [Google Scholar]
- 58.Naruszewicz M, Zapolska-Downar D, Kośmider A, Nowicka G, Kozłowska-Wojciechowska M, Vikström AS, et al. Chronic intake of potato chips in humans increases the production of reactive oxygen radicals by leukocytes and increases plasma C-reactive protein: a pilot study. Am J Clin Nutr. 2009;89(3):773–7. doi: 10.3945/ajcn.2008.26647. [DOI] [PubMed] [Google Scholar]
- 59.Silva AR, Moraes BPT, Gonçalves-de-Albuquerque CF. Mediterranean Diet: lipids, inflammation, and Malaria infection. Int J Mol Sci. 2020;21(12):4489. doi: 10.3390/ijms21124489. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Neuhouser M, Thompson B, Coronado G, Solomon C. Higher fat intake and lower fruit and vegetables intakes are associated with greater acculturation among Mexicans living in Washington State. J Am Diet Assoc. 2004;104(1):51–7. doi: 10.1016/j.jada.2003.10.015. [DOI] [PubMed] [Google Scholar]
- 61.Tao M, Liu J, Nguyen U. Trends in Diet Quality by Race/Ethnicity among adults in the United States for 2011–2018.Nutrients. 2022, 14(19):4178. [DOI] [PMC free article] [PubMed]
- 62.Sagili V, Chakrabarti P, Jayanty S, Kardile H, Sathuvalli V. The Glycemic Index and Human Health with an emphasis on Potatoes. Foods. 2022;11(15):2302. doi: 10.3390/foods11152302. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Table S1. The definitions of starchy and non-starchy vegetables according to FPED 2017-2018. Table S2. Characteristics of study participants by MetS status, weighted (n=24646)a
Data Availability Statement
The datasets generated and/or analyzed are available from the corresponding.
author on reasonable request.