Abstract
Background
Nutraceutical plants play a potential role as supportive treatment with antiretroviral drugs in the management of opportunistic infections associated with HIV/AIDS. There is limited documentation of nutraceutical plants in Northern Uganda and limited literature addressing processes to be adopted for quality assurance of herbal formulations in Uganda. This study aimed to document plant species with nutritional and medicinal properties used for managing opportunistic infections associated with HIV/AIDS by traditional medicine practitioners (TMPs), who included professional herbalists, herbal farmers and herbal sellers in Acholi sub region, Northern Uganda.
Methods
An ethnobotanical study was carried out in Amuru, Gulu and Pader districts, Northern Uganda. Cross-sectional data were collected using purposive and snowball sampling techniques. A total of four hundred (378 women and 22 men) informants were selected. Data were collected using semistructured interviews, focus group discussions and direct observation. Data were analysed using descriptive statistics, familiarity index (FI), fidelity level (FL) and informant consensus factor (ICF).
Results
This study recorded a total of 84 nutraceutical plant species, which are used to manage opportunistic infections associated with HIV/AIDS. Most abundant families were Leguminoceae, Asteraceae and Solanaceae. Six nutraceutical plants that had higher fidelity level and familiarity index values included Momordica foetida Schumach, Erigeron floribundus (Kunth) Sch. Bip, Mangifera indica L, Cajanus cajan L. Millsp, Eucalyptus globulus Labill and Cucurbita pepo L. Respondents’ knowledge on nutraceutical plants had a positive significant correlation with age (R2 = 0.0524, p ≤ 0.01). The popular mode of preparation are decoctions/boiling in water (70%), while the most used route of administration is oral (76%). TMPs tried to ensure that during collection and processing, plant materials were free from contamination. TMPs reported limited knowledge on preservation techniques.
Conclusions
This study demonstrates the availability and diversity of nutraceutical plants in Uganda and reports methods of processing and administration used by TMPs. Both men and women used nutraceutical plants to manage opportunistic infections associated with HIV/AIDS and showed great extent of their traditional knowledge. Most of the nutraceutical plants in study area are wild and abundant; however, high percentage use of plant roots and bark threatens the sustainable use from the wild.
Keywords: Ethnobotany, HIV/AIDS, Nutraceutical plants, Opportunistic infections, Safety
Introduction
Globally, 38.4 million people were living with human immunodeficiency virus/acquired immune deficiency syndrome (HIV/AIDS) in 2021 [1]. Of these, 25.6 million people were in Eastern and Southern Africa alone [1]. Currently, the number of people with HIV in Uganda is estimated to be about 1.4 million [2] and the national prevalence rate of HIV/AIDS is 6.4%, Gulu district is at 13%, Amuru district at 4.5% and Pader district at 8.5% [2–4].
A weak immune system in patients with HIV/AIDS infection results in patients being susceptible to opportunistic infections, such as oral candidiasis and genital infections that are caused by opportunistic pathogens, such as Candida albicans [2–4]. Other opportunistic pathogens include Staphylococcus aureus, Mycobacterium tuberculosis, Streptococcus pneumoniae, Klebsiella pneumoniae, Cryptococcus neoformans and Pseudomonas aeruginosa [5, 6]. There are no vaccines for HIV, but people living with HIV/AIDS, who have a timely diagnosis and access to medication, proper care and treatment with effective antiretroviral drugs can lead normal, healthy and productive lives and are expected to live nearly as long as the general population [7–9]. However, in resource poor countries, such as Uganda, the use of antiretroviral (ARV) drugs in managing opportunistic infections by HIV positive patients is limited by toxic side effects, poor adherence to treatment and limited access to the drugs [10, 11]. Antimicrobial resistance (AMR) due to continued use of antibiotics to which pathogens such as bacteria and fungi have developed resistance, has been reported [10, 12, 13]. The increasing prevalence of HIV-1 drug resistance in low and middle income countries hinders successful ART [14]. Even when several pharmaceutical drugs are available at subsidized cost, most Ugandans cannot afford to buy modern medicine due to their low income status [15]. Other factors, such as high exposure to infectious agents, poverty and malnutrition, have all led to significant crisis in the management of HIV/AIDS [10, 11]. Opportunistic infections due to HIV results in morbidity and mortality and this loss of labour force results in loss of productivity, profitability and hence poverty [16, 17]. There is a high need to explore and develop reliable, safe drugs and supportive treatment from natural resources to manage HIV infection [18].
One of the potential ways of managing opportunistic infections associated with HIV/AIDS could be nutraceutical plants, as sources of new antimicrobial molecules [12]. The research and development of alternative safe drugs should follow standards, parameters and protocols to ensure quality control is guaranteed [19, 20]. Nutraceutical plants are the most popular form of traditional medicine, and are used worldwide as an alternative and/or complementary medicine [21–23]. Nutraceutical plants are plants with nutritional or medicinal properties or both [24]. Medicinal plants are plants that exert beneficial pharmacological effect on the human or animal body or possess therapeutic properties [24]. Living organisms can grow, maintain themselves and reproduce by assimilation of nutritious plants that contain vitamins A, C, K, Fibre, Riboflavin and minerals, which are essential requirements for the health of HIV positive patients [25]. Nutraceutical plants have a potential in the management of opportunistic infections associated with of HIV/AIDS especially among rural poor [18].
There have been reports of nutraceutical plant use worldwide, such as in Pakistan, Cassia fistula and Punica granatum have been used against fungal opportunistic infections associated with HIV [26]. Approximately, 137 medicinal plants were used to treat pneumonia and tuberculosis opportunistic infections in Pakistan [27]. In Thailand, 12 medicinal plants used among HIV patients, were evaluated for antibacterial activities [28].
Ethnobotanical studies conducted in different African countries [29–36] reported that nutraceutical plants were being used to manage a wide range of diseases. For example, ninety four (94) plant species were reported to be used in managing HIV/AIDS opportunistic infections in Livingstone, Zambia [33]. Seventeen (17) plants located in Western and Eastern Cape, South Africa were reported as being used in the management of HIV and related opportunistic infections [37]. Thirty three (33) plant species were identified in the management of opportunistic fungal infections (O.F.I) by HIV/AIDS patients in the Amathole district of the Eastern Cape Province, South Africa [34]. Nagata et al. [38] identified 40 medicinal plant species used among people living with HIV/AIDS in Suba district, Kenya.
Poor health facilities and limited access to antiretroviral drugs in Uganda have perpetuated and increased the use of nutraceutical plants, especially in rural areas for opportunistic ailments of HIV/AIDS [39]. Nutraceutical plant, Albizia coriaria Oliv. is widely used in traditional medicine for treating opportunistic infections, such as skin infections, cough, syphilis, and sore throat among PLHIV in Uganda [12, 40, 41]. The root of Serudaca pedunculata Fresen. is commonly used in Uganda for treating STDs, TB, Coughs [12]. Ethnobotanical survey by Shehu et al. [32] in Buikwe district, Uganda indicated that 52 plants were used in the management of HIV/AIDS opportunistic infections.
There is limited documentation of nutraceutical plants in Northern Uganda and limited literature addressing processes to be adopted for quality assurance of herbal formulations in Uganda. This ethnobotanical study aimed to document plant species with nutritional and medicinal potentials used for managing opportunistic infections associated with HIV/AIDS by traditional medicine practitioners (TMPs) in Acholi sub region, Northern Uganda. This study reported the quality control methods employed by TMPs and the prioritized problems encountered during harvest, processing, production and administration of the documented nutraceutical plants. This study also provided information on the local solutions to prioritized problems and recommendations to the government on opportunities to help with quality control measures.
Methods
Description of the study area
Uganda is a landlocked country that lies astride the equator and covers an area of 236,000 square kilometres comprising dryland, open water and permanent swamp [42]. Uganda population census of 2013 [43], reported approximately 7.3 million households with a population of 34.1 million were in Uganda [43]. There are 56 tribes and 9 indigenous communities [43]. There are approximately 5000 species of higher plants in Uganda, of which 70 are endemic [42]. There are more than 200 species of non-cultivated edible plants and 75 species of edible fruit trees in Uganda, while forestland covers approximately 3.3 million hectares [42]. Ethnobotanical research in Uganda has identified more than 300 trees, shrubs and herbs growing wild associated with medicinal value [42]. Traditional knowledge of plants with medicinal value is passed on from one generation to another [42].
The agricultural sector is composed of crop and animal production, forestry, fisheries and major crops produced include cotton, maize, tea, sugarcane, bananas [42]. According to livestock census, Uganda had fourteen point two (14.2) million cattle, 16 million goats, 6 million sheep, 47.6 million poultry and 4.1 million pigs [42]. This study was carried out in Amuru, Gulu and Pader districts. In general, altitude ranges between 1000 and 1200 Metres above sea level [42]. The districts experience tropical climate with average annual rainfall of 1507 mm and average temperatures is 23 °C, vegetation is intermediate savannah grassland [42]. The districts have established health centres. Despite the presence of established health centres, people are still reported to seek medical attention from traditional medicine practitioners [44, 45]
Gulu district is located at 2° 46′ 54.0″ N and 32° 17′ 57.0″ E in Northern Uganda [42]. Main economic activity of ninety percent (90%) of the population is subsistence agriculture [43]. The climate is tropical wet and dry, according to Koppen–Geiger climate classification system [46]. Total population in Gulu district is 275,613, while total households are 55,441 [43]
Pader district, homeland of Acholi ethnic group is located in Northern Uganda at 2° 49′ 59.99″ N and 33° 04′ 60.00″ E [42]. Total area is 3.362 square kilometres. Food crops grown are beans, peas, cassava, cotton, groundnuts, and sunflower. Ninety percent (90%) of the economic activity is subsistence agriculture. The total population in Pader district is 178,000, while total households are 34,183 [43]
Amuru district located at 2° 46′ 54″ N and 32° 17′ 57″ E in Northern Uganda. Ninety-eight percent (98%) of the economic activity is subsistence agriculture [42]. Total area is 3625.9 square kilometres. Crops grown include cotton, millet, sorghum, sweet potatoes, simsim. The Total population in Amuru district is 186,696, total households are 36,650 [43].
Data collection and selection of the informants
A cross-sectional study was conducted between September 2020 and April 2021. Three districts were purposively selected based on rich biodiversity of nutraceutical plant species and presence of TMPs.
Study population were all people from Amuru, Gulu and Pader districts who have used nutraceutical plants for 1 year or more to acquire adequate knowledge on herbal medicine [12].
Sampling strategies
In this research, four hundred TMPs were purposively selected and interviewed from Gulu, Amuru and Pader districts, Northern Uganda. The sample size was determined using the Yamane formula [47] (1) with 95% confidence level presented as follows:
| 1 |
where n is the sample size required = 400. N is the total number of people in the study area (739,700) [43]. e is the maximum variability or margin of error 5% (0.05). 1 is the probability of the event occurring.
Sample size included one hundred and thirty three (133) people from Amuru district, 133 from Gulu district and 134 from Pader district. With Prior Informed Consent (PIC), Purposive sampling [48–50] was used to select 400 authentic and well-known traditional medicine practitioners (TMPs) who included key informants, such as professional herbalists, herbal farmers and herbal sellers. Professional herbalists owned herbal ‘clinics’, where they diagnosed and treated people for money, herbal farmers owned gardens, where they grew nutraceutical plants, while herbal sellers bought nutraceuticals in bulk and sold retail in the market. Subsequent respondents were identified using snowball sampling method [48, 51]. Respondents were identified with the help of local government officers, particularly local councillors LC I, LC II, and LC III heading village, parish and sub-county levels, respectively.
Data were collected using semi-structured interviews, focus group discussions and direct observation. The prior-informed consent (PIC) form was translated into the local Acholi language. The scope, possible benefits and risks of the study were explained to willing TMP interviewees and Focus Group participants who signed consent forms after agreement. Identification of interviewees and Focus Group participants were protected via anonymisation.
The TMPs were asked whether they were familiar with signs and symptoms of HIV/AIDS and associated opportunistic infections. TMPs were asked how they assumed a person probably has HIV and if they relied on biomedical lab diagnoses for confirming the patient’s HIV sero status or depended on confession by the patient. The TMPs were asked if they treated patients already receiving ARVs. Informants were not required to reveal HIV/AIDS status to researcher.
During the conversation, data on respondent characteristics and information related to Nutraceutical uses of plants for the management of HIV/AIDS-related diseases were captured. Interviews were conducted at the herbalist ‘clinic’, at market place, where some nutritious plants sold, at the home of respondents and also during field excursions to point out the plants. This information included a complete list of local names of plants, plant parts used to treat HIV/AIDS Opportunistic infections, methods of preparation, route of administration and dosages were recorded. According to US Centres for disease control [52], the major opportunistic infections associated with HIV/AIDS are candidiasis, pneumonia and tuberculosis, which were considered in this study. Other symptomatic but undefined conditions considered included diarrhoea, cough, stomach ache, skin fungal infection and venereal diseases [53]. Nutrition-related conditions were considered, such as anaemia, low appetite for food and low immunity. Focus Group Discussions (FGD) used the Participatory Action Research (PAR) Model [54, 55]. TMPs such as professional herbalists, herbal farmers and herbal sellers participated in the FGD. Approximately eight to ten (8–10) participants in each FGD were involved [54, 55]. FGD is where the researcher assembled a group of individuals to discuss a specific topic, aiming to draw from complex personal experiences, beliefs, perceptions and attitudes of participants through a moderated interaction [56]. Four FGD per district were conducted. FGD were conducted at a central convenient meeting point, such as under a tree or a shelter.
FGD answered clear and simple questions set to elicit information on Quality Assurance and Quality Control of nutraceutical plant preparation. The questions intended mainly to understand the Acholi cultural context of Quality control methods employed in the management of Opportunistic infections using Nutraceutical plants. Information on harvesting equipment, utensils used, source of water and fuel or location of plants was got by direct observation.
Fresh plant materials were collected from forests, bushes or people’s herbal medicine gardens by this researcher (trained botanist/taxonomist) and a research assistant using standard procedures [57, 58] and the practitioners were used as guides in field excursions. Plant specimens were collected based on ethnomedical information provided by TMPs and were identified in the field basing on the African Plant Database and Flora of Tropical East Africa catalogue [59]. Plant names were checked and updated with online website (www.theplantlist.org). The voucher plant specimens were pressed, dried, mounted, coded [57, 58] and deposited at the Herbarium in the Department of Plant science, microbiology and Biotechnology, Makerere University Kampala, Uganda. Further confirmation and identification of botanical specimens was done via comparison with herbarium material stored in the Makerere University Herbarium and consultation with curators [57, 58]. Accession numbers of plant species were recorded.
Data analysis
Collected Ethnobotanical data were entered into Microsoft Excel spreadsheet 2013. Descriptive statistics (graphs and tables) was used to summarize ethnobotanical and socio-demographic data. All recorded plant species are presented in tabular format, alongside corresponding ethnomedicinal usage information. The number of nutraceutical plants cited per TMP was used as a proxy for the extent of their traditional knowledge.
Differences in traditional nutraceutical knowledge due to gender, age, level of education, religion and location were analysed using analysis of variance (one-way ANOVA) test and independent T test. Number of nutraceutical plants reported set as the dependent variable, while gender, age, level of education, religion, location set as the independent variable. A Linear Regression model was used to understand whether age and time in schooling system predict nutraceutical plant knowledge. Qualitative data analysis used Thematic Content Analysis technique [37, 60–62] and narrative analysis [63, 64] to understand traditional methods used during collection, processing and storage of nutraceuticals as an indicator of quality control.
Quantitative data were analysed using the familiarity index, Fidelity level and informant consensus factor [65].
The familiarity index (FI), a relative indicator of the familiarity of a plant species is defined as the frequency a given plant is mentioned as an ethnomedicine divided by the total number of knowledge holders or TMPs interviewed in the study [65].
Fidelity level
Fidelity level (FL) values indicate most preferred plant species for particular ailments [65].
FL = IP/N × 100, where IP is the number of informants who indicated use of a species for the same major ailment, N is the total number of informants who mentioned the plant for any other use. Increasing values of FL for a species indicate its uniqueness to treat a particular illness.
Informant consensus factor
The Informant consensus factor (ICF) is the number of citations in each ailment category minus the number of species used, divided by the number of use citations in each category minus one. The ICF value indicates the Level of Agreement among Herbalists in the use of plants for various ailments [65]. Fic = (Nur − Nt)/(Nur − 1), where Nur is the number of use reports of informants for particular ailment/disease category, Nt is the number of plant species used for a particular ailment category by all informants.
Informant consensus factor is performed to test the consistency of the informants’ knowledge in treating a particular opportunistic infection caused by bacteria and fungi. ICF values range between 0 and 1, where 1 indicates the highest level of informant agreement. Ethnomedicinal use were classified by body systems according to disease categories proposed by the International Classification of Diseases [53].
Results
Profile of traditional medicine practitioners
Results indicate that Traditional healing is widely acknowledged as an occupation in Northern Uganda. Of the four hundred (400) respondents, 55.75% were Professional Herbalists, 20% regarded themselves as herbal farmers and 23% were herbal sellers (Fig. 1). Some informants were involved in other activities, such as hairdressing, teaching, and tailoring.
Fig. 1.
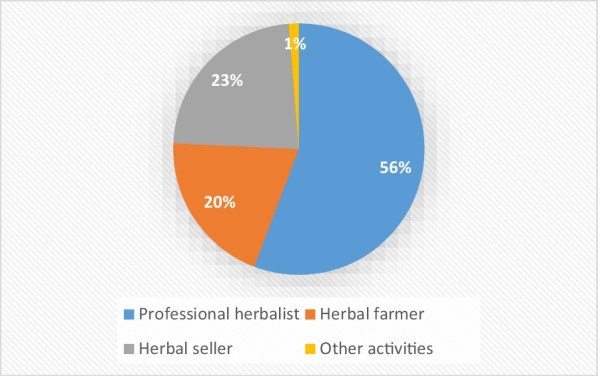
Profession of informants
The profile of informants regarding age, gender, education, religion, location is shown in Table 1. Nutraceutical plant knowledge was significantly influenced by gender, age, and location (p ≤ 0.05) (Table 1). Both men and women used nutraceutical plants to manage opportunistic infections associated with HIV/AIDS (Table 1). Ninety-four point five percent (94.5%) of the TMPs were women and 5.5% men (Table 1). The mean number of Nutraceutical plants used to manage opportunistic infections associated with HIV/AIDS, cited by women (3.608 plants) showed great extent of their traditional knowledge than the men (2.454 plants) (p ≤ 0.05) (Table 1).
Table 1.
Nutraceutical plant knowledge among different social groups of the study area
| Parameter | Informant group | N (sample size) | Mean no. of plants cited | T statisics | p value | Sum of squares SS (total) | Degree of freedom df (total) | F value | p value | F critical |
|---|---|---|---|---|---|---|---|---|---|---|
| Gender | Male | 22 | 2.454 | 2.748 | 0.011 | 1955.19 | 399 | 5.7160 | 0.017275 | 3.8649 |
| Female | 378 | 3.608 | ||||||||
| Age (years) | Below 21 | 23 | 2.352 | 0.011 | 818.1 | 170 | 4.848 | 0.001008 | 2.4260 | |
| 21–35 | 170 | |||||||||
| 36–50 | 103 | 3.365 (adult) | ||||||||
| 51–65 | 67 | 4.058 (elder) | ||||||||
| above 65 | 37 | |||||||||
| Religion | Catholic | 344 | 542.57 | 83 | 2.1018 | 0.1065 | 2.7188 | |||
| Muslim | 1 | |||||||||
| Protestant | 27 | |||||||||
| Born-again | 28 | |||||||||
| Education level | no formal education (illiterate) | 58 | 3.948 (iliterate | 1.463 | 0.147 | 69.69 | 12 | 0.4311 | 0.7829 | 3.8379 |
| Primary school | 324 | 3.476 (literate) | ||||||||
| Completed O’Level | 14 | |||||||||
| Completed A’Level | 3 | |||||||||
| Diploma | 1 | |||||||||
| Degree | 0 | |||||||||
| Location | Gulu | 133 | 1955.19 | 399 | 6.0810 | 0.002504 | 3.0185 | |||
| Amuru | 133 | |||||||||
| Pader | 134 |
Evaluation of the influence of age indicated that few TMPs were in the age group of the youth, where 5.75% were below age 21 years (Table 1). Forty-two point five percent (42.5%) were between ages 21–35% and 25.75% between ages 36–50 years (Table 1). Most of the people who had substantive knowledge on Nutraceutical plants (4.058 plants) were mostly older than 50 years of age (Table 1). The mean number of Nutraceutical plants used to manage opportunistic infections associated with HIV/AIDS, cited by Elders (above 50 years) (4.058 plants) was higher than that cited by adults (3.365 plants) and this showed the great extent of elders’ traditional knowledge. TMPs’ knowledge on nutraceutical plants grows during their lifetime as seen from the Linear Regression Analysis which showed that Nutraceutical plant knowledge and age had a Positive significant Correlation (R2 = 0.0524, p ≤ 0.01) (Table 2). Linear regression was used for time series forecasting. Age and level of education change with time unlike gender and religion which do not change with time.
Table 2.
Age and level of education predicting knowledge of nutraceutical plants used to manage opportunistic infections associated with HIV/AIDS
| Parameter | R-square value | F value | p value |
|---|---|---|---|
| Age | 0.0524 | 22.028 | 0.0000037 |
| Level of education | 0.0038 | 1.527 | 0.217200 |
As regards the Education level of the TMPs, fourteen point five percent (14.5%) were illiterate and most of the TMPs had incomplete fundamental education, where 81% reported attending Primary school (Table 1). Although the illiterate TMPs had higher knowledge on nutraceuticals than TMPs who attended primary school, the difference in plant knowledge was not significant. (p > 0.05) (Table 1). Results from Linear Regression analysis indicate that the level of education attained had a significant negative correlation with Nutraceutical plant knowledge (R2 = 0.0038, p ≤ 0.01) (Table 2). Nutraceutical plant knowledge was not significantly influenced by education as most respondents had incomplete fundamental education (p ≥ 0.05) (Table 1). Respondents belonged to different religions (Table 1).
Diversity of neutraceutical plants, their use, and growth forms
This ethnobotanical study recorded a total of eighty four (84) nutraceutical plant species distributed in 38 plant families and 76 genera, used to manage opportunistic infections associated with HIV/AIDS (30 of the 84 plants are shown in Tables 3, 4, and 5) (See “Appendix” for the 54 plants). Most abundant families were Leguminoceae (13 species), Asteraceae (6 species), Solanaceae (4 species), Verbenaceae (4 species) and Moraceae (4 species).
Table 3.
Nutraceutical plants used to manage bacterial opportunistic infections associated with HIV/AIDS and mode of preparation for quality control
| Scientific name, family, Local name in native “Acholi dialect” | Accession number | Habit | Habitat | Conservation status | Bacterial opportunistic infection treated (uses) | Part used | Mode of preparation and administratn | Familiarity index | Fidelity level |
|---|---|---|---|---|---|---|---|---|---|
|
Acacia hockii De Wild (Leguminoceae) Okuto-oriang |
MHU 32118 |
Shrub | Bu | W/A | Cough. Diarrhea, stomachache | FL | Mix leaves in hot water, drink infusion | 0.058 | 0.115 |
|
Aloe vera L. Aloaceae Ataka-rach |
MHU 50969 |
Herb | Ho | Cu/A | Cough. Stomachache, diarrhea | S | Mix sap from leaves in cold water, drink | 0.102 | 0.205 |
|
Bidens pilosa L Asteraceae Labika |
MHU 51149 |
Herb | Rs | W/A | Cough, wounds, eye infection, ear infection | FL | Mix leaves in hot water, drink infusion | 0.075 | 0.006 |
|
Bridelia scleroneura Mull.-Arg Phyllanthaceae Larwece |
MHU 35756 |
Shrub | Bu | W/A | Diarrhea, cough.eye infection | FSB, FR | Boil bark or roots, drink decoction | 0.065 | 0.26 |
|
Cajanus cajan L.Millsp. Leguminoceae Lapena |
MHU 51151 |
Shrub | Ga | Cu/A | Cough. Diarrhea | FL | Chew Leaves | 0.20 | 0.80 |
|
Cassia nigricans Vahl Leguminoseae Abanceng |
MHU 32957 |
Shrub | Bu | W/A | Abdominal pain, cough, sore throat | FL | Mix leaves with hot water, drink infusion | 0.045 | 0.09 |
|
Combretum collinum Fresen Combretaceae Oduku |
MHU 34092 |
Tree | Fo | W/A | Diarrhea, stomachache, wounds | FR, FL | Boil roots or leaves, drink decoction | 0.073 | 0.097 |
|
Eucalyptus globulus Labill Myrtaceae Kalatuc |
MHU 51152 |
Tree | P | Cu/A | Cough | FL | Mix Leaves in hot water, drink infusion | 0.203 | 0.405 |
|
Euphorbia tirucalli L Euphorbiaceae Kilajok |
MHU 50984 |
Shrub | Bu | W/A | Eye infection, cough, eye infection, diarrhoea | S | Squeeze sap into eye | 0.063 | 0.250 |
|
Ficus sycomorus L Moraceae Olam |
MHU 37779 |
Tree | Bu | W/A | Syphilis, diarrhea, stomachache | FL,FSB | Boil leaves or bark in water, drink decoction | 0.048 | 0.011 |
|
Mangifera indica L Anacardiaceae Muyeeme |
MHU 41712 |
Tree | Ho | Cu/A | Cough, diarrhea, stomachache | FSB | Boil bark, drink decoction | 0.188 | 0.750 |
|
Momordica foetida Schumach Cucurbitaceae Bomo |
MHU 51150 |
Climber | Bu | W/A | Syphilis, diarrhea, stomachache | FR | Boil roots, drink decoction | 0.075 | 0.008 |
|
Piliostigma thonningii (Schumach.) Milne.Redh Leguminaceae Ogali |
MHU 35791 |
Tree | Bu | W/A | Cough, wounds, bloody diarrhea, stomachache | FL | Mix leaves in hot water, drink infusion | 0.093 | 0.09 |
|
Solanum incanum L Solanaceae Ocok |
MHU 32003 |
Shrub | Rs | W/A | Stomachache, ear infection, sore throat | FR,FL | Boil roots or leaves, drink decoction | 0.078 | 0.310 |
|
Vernonia lasiopus O.Hoffm Asteraceace Labuka |
MHU 35754 |
Shrub | Bu | W/R | Eye and ear infection, stomachache | S | Squeeze sap into ear, eye | 0.048 | 0.095 |
Parts used: FL: fresh leaf, FR: fresh root, FSB: fresh stem bark FSe: fresh seed, FFr: fresh fruit, Bu: bulb, S: sap
Habitat: Bu—bushland, Gr—grassland, Ho—homestead, Rs—roadside, P—plantation Sw—swamp, Ga—garden, Fo—forest, Wo—woodland
Conservation status: W/A: wild and abundant, W/R: wild and rare, Cu/A: cultivated and abundant, Cu/R: cultivated and rare
Decoction: water extraction by boiling of dissolved plant material and drank
Infusion: plant material is added to hot water and left to stand for few minutes and drank
Table 4.
Nutraceutical plants used to manage fungal opportunistic infections and mode of preparation for quality control
| Scientific name, Family, Local name in native “Acholi dialect” | Accession number | Habit | Habitat | Conservation status | Fungal opportunistic infection (uses) | Part used | Mode of preparation | Familiarity index | Fidelity level |
|---|---|---|---|---|---|---|---|---|---|
|
Afromomum angustifolium (Sonn.) K. Schum Zingiberaceae Oceyu |
MHU 32633 |
H | Bu | W/R | Oral candidiasis | FL | Boil leaves, drink decoction | 0.020 | 0.026 |
|
Erigeron floribundus (Kunth) Sch.Bip Asteraceae Dingtong |
MHU 51148 |
H | Rs | W/A | Skin fungal infection | FL | Rub leaves on skin with shea butter | 0.075 | 0.021 |
|
Ficus sycomorus L Moraceae Olam |
MHU 37779 |
T | Bu | W/A | Skin fungal infection | S | Rup sap on skin | 0.045 | 0.011 |
|
Gynandropsis gynandria (L.)Briq Cleomeaceae Akeyo |
MHU 35837 |
H | Ga | Ga | Oral candidiasis, skin fungal infection | FL | Boil leaves, drink decoction | 0.025 | 0.006 |
|
Khaya senegalensis (Desr.). A. Juss Meliaceae Tido |
MHU 42488 |
T | Bu | W/A | Oral candidiasis, candida | FL | Boil bark, drink decoction | 0.053 | 0.019 |
|
Momordica foetida Schumach..Cucurbitaceae Bomo |
MHU 51150 |
C | Bu | W/A | Oral candidiasis, candida | FR | Boil roots drink, decoction | 0.090 | 0.017 |
|
Occimum gratissimum Linn.Lamiaceae Mida |
MHU 35677 |
H | Bu | W/A | Skin fungal infection | FL | Rub leaves on skin | 0.050 | 0.040 |
|
Pseudocedrela kotschyi (Schweinf.) Harms Meliaceae Ofuti |
MHU 50947 |
T | Bu | W/R | Oral candidiasis | FR | Boil roots, drink decoction | 0.028 | 0.037 |
|
Sanseviera neutoniana T.G Forrest Asparagaceae Tworo-gwok |
MHU 42552 |
H | Bu | W/R | Oral candidiasis | FL | Boil leaves, drink decoction | 0.025 | 0.025 |
|
Sarcocephalus latifolius (Smith)Rubiaceae munyu) |
MHU 50529 |
S | Bu | W/A | Oral candidiasis | FL | Boil roots, drink decoction | 0.020 | 0.027 |
Parts used: FL: fresh leaf, FR: fresh root, FSB: fresh stem bark, FSe: fresh seed, FFr: fresh fruit, Bu: bulb, S: sap
Habitat: Bu—bushland, Gr—Grassland, Ho—homestead, Rs—roadside, P—plantation, Sw—swamp, Ga—garden, Fo—forest, Wo—woodland
Habit: S—shrub, T—tree, H—herb, C—climber, G—grass
Conservation status: W/A: wild and abundant, W/R: wild and rare, Cu/A: cultivated and abundant, Cu/R: cultivated and rare
Decoction: water extraction by boiling of dissolved plant material and drank
Infusion: plant material is added to hot water and left to stand for few minutes and drank
Table 5.
Nutraceutical plants used to boost immunity against opportunistic infections and mode of preparation for quality control
| Scientific name Family, Local name (Ethnic language) in native “Acholi dialect” |
Accession number | Habit | Habitat | Conservation status | Use | Part used | Mode of preparation | Familiarity index |
|---|---|---|---|---|---|---|---|---|
|
Amaranthus dubius Mart.ex Thell Amaranthaceae Obuga |
MHU 42023 |
Herb | Ga | Cu/a | Immune booster | FL | Decoction leaves | 0.005 |
|
Bidens pilosa. L Asteraceae Labika |
MHU 51149 |
Herb | Rs | w/a | Increases CD4/wound healing properties/blood clotting | FL | Decoction leaves | 0.005 |
|
Carica papaya Linn Caricaceae Papai |
MHU 42266 |
Shrub | Ho | Cu/a | Immune booster | FL/FFr | Decoction leaves | 0.003 |
|
Cucurbita pepo L Cucurbitaceae Okono |
MHU 42492 |
Climber | Ga | Cu/a | Increases appetite immune booster | FL/FFr | Decoction leaves | 0.013 |
|
Vigna unguiculata L. (Walp) Leguminoseae Boo |
MHU 35800 |
Herb | Ga | Cu/a | Immune booster | FL | Decoction leaves | 0.005 |
Parts used: FL: fresh leaf, FFr: fresh fruit
Habitat: Bu—bushland, Gr—grassland, Ho—homestead, Rs—roadside, P—plantation, Sw—swamp, Ga—garden, Fo—forest, Wo—woodland
Habit: S—shrub, T—tree, H—herb, C—climber, G—grass
Conservation status: W/A: wild and abundant, W/R: wild and rare, Cu/A: cultivated and abundant, Cu/R: cultivated and rare
Decoction: water extraction by boiling of dissolved plant material and drank
Infusion: plant material is added to hot water and left to stand for few minutes and drank
High Familiarity Index values (FI) and high-fidelity level (FL) values show outstanding preference for treating opportunistic infections (Tables 3, 4 and 5). Six nutraceutical plants that had higher fidelity level and familiarity index values included Momordica foetida Schumach, Erigeron floribundus (Kunth) Sch. Bip, Mangifera indica L, Cajanus cajan L. Millsp, Eucalyptus globulus Labill and Cucurbita pepo L. Plant growth forms (habits) analysis indicated that 38% were shrubs and 33% were trees. Herbs comprised 21% of total number (Fig. 2).
Fig. 2.
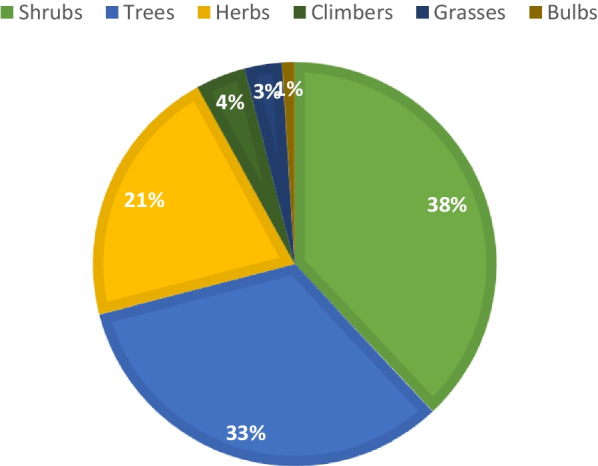
Growth form of nutraceutical plants
Majority of plants were collected from the bushes (47%) and 13.8% cultivated in gardens, and 13% were got from around homestead and forests (9.8%). Others were obtained from roadsides (7.3%), plantations (3.3%) or woodland (2.4%) (Fig. 3).
Fig. 3.
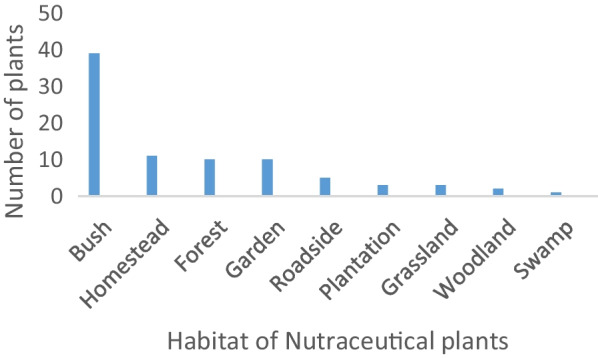
Source of nutraceutical plants
Methods of preparation, administration and ailments treated
Decoctions/boiling in water (70%) were commonly used as mode of preparation followed by infusion/mixing with hot water (25%), maceration/soaking in cold water (3%), and others (2%) (Tables 3, 4, 5). Routes of administration included oral (76%), dermal (17%), auricular (3%), ocular (2%) and others (2%) (Tables 3, 4, 5).
The most preferred plant species for bacterial opportunistic infections include Cajanus cajan leaves (for cough, tuberculosis, chest infections) (FI = 0.20, FLI = 0.80), Mangifera indica Bark (for diarrhoea and stomach-ache) (FI = 0.19, FLI = 0.75) and Eucalyptus globulus leaves (FI = 0.20, FLI = O.41) (for cough, tuberculosis, chest infections) (Table 3).
The most preferred plant species for Treating Fungal opportunistic infections include Momordica foetida roots (For oral candidiasis) (FI = 0.090, FLI = 0.017) and Erigeron floribundus leaves (for skin fungal infection) (FI = 0.075, FLI = 0.021) (Table 4).
Most preferred Nutraceutical plants that are used to boost immunity were also noted (Table 5). The percentage of total number of plants that provided nutritional support in boosting immunity was 12% (Table 5).
The Informant Consensus Factor (ICF) indices indicated that the highest level of herbalists’ agreement on the nutraceutical plants used to manage bacterial and fungal infections was for Digestive system, Respiratory system and Dermatological systems with ICF Values of 0.88, 0.87 and 0.85, respectively, as shown in Table 6.
Table 6.
Informant consensus factor for six categories of ailments
| Body system according to disease category | Number of use reports (Nur) | Number of plant species used (Nt) | Informant consensus factor Fic = (Nur − Nt)/(Nur − 1) |
|---|---|---|---|
| Digestive system (mouth, oesophagus, stomach, small and large intestine, rectum, anus) | 610 | 74 | 0.88 |
| Respiratory system (nose, trachea, bronchi, lungs, diaphragm) | 326 | 38 | 0.87 |
| Dermatological system (skin) | 106 | 17 | 0.85 |
| Nervous system (brain, eye, ear. Spinal cord) | 103 | 25 | 0.76 |
| Reproductive system | 11 | 9 | 0.20 |
Thematic content analysis and narrative analysis of responses by TMPs about the prioritized problems encountered during harvest, processing, production and administration of the documented nutraceutical plants, the local solutions to prioritized problems and recommendations to the government on opportunities to help with quality control measures are shown in Table 7.
Table 7.
Challenges encountered during harvesting, processing and administration of nutraceuticals and recommendations to authorities
| Theme | Sample narrative | Recommendation |
|---|---|---|
| Problems encountered during collection of nutraceutical plants |
Distance to source of nutraceuticals ‘Long distance walking to forest, bush to find nutraceuticals’ Safety of TMPs during collection ‘We meet wild animals, get pricked by thorns, sharp objects in bush ‘ Availability of protective gear ‘we lack gumboots’ |
‘We ask Government of Uganda to facilitate with gumboots and protective gear’ |
| Problems encountered during processing of nutraceutical plants |
Availability of equipment ‘we lack processing equipment such as grinding machines’ ‘Crushing or grinding is done using two rough stones or mortar and pestle. Utensils used are clay pots or Aluminium/steel saucepans’ It was observed that during processing, nutraceutical plant materials had visible signs of contamination, while some equipment used were not clean. TMPs engaged in herbal processing did not maintain hygiene or wear protective clothing |
‘We ask Government of Uganda to facilitate with crushing equipment’ |
| Problems encountered during preservation of nutraceuticals |
Methods of preservation ‘we don’t preserve nutraceuticals, plants are abundant’ ‘we have limited knowledge on preservation of herbal formulations’ |
‘We need training’ |
| Problems encountered during packaging nutraceuticals |
Packaging of nutraceuticals ‘we lack packaging materials ‘ |
|
| Problems encountered during treatment of clients |
Methods of treatment ‘we estimate doses for nutraceuticals ‘We treat opportunistic infections till no symptoms seen’ Cooperation with medical doctors ‘there is Lack of cooperation with medical doctors’ |
‘we ask for collaboration and communication between biomedical clinicians and Traditional medicine practitioners should be encouraged |
| Problems encountered during payment for nutraceuticals |
Payment for herbal medicine ‘payment is low or is made inkind in exchange for chicken or harvested crops’ |
Ministry of Education, Uganda is called upon to convene and train TMPs about basic knowledge on diagnosis of disease, record maintenance, Legal systems, business management, processing and packaging nutraceutical plants for commercial use, how to maximize profits and protect their knowledge |
| Problems encountered in keeping information |
Methods of storing information ‘Most TMPs cannot read or write especially the elderly, therefore, unable to record information’ ‘Information passed orally from generation to generation’ |
Most TMPs reported that they had limited knowledge on preservation of herbal formulations and most times used freshly collected nutraceutical plant parts, because most plants are still abundant (Table 7).
When consulted by a patient, the TMPs interview patient orally about their problem and history. Some patients bring along their medical diagnosis from hospitals. Symptoms of various HIV/AIDS opportunistic infections are described to the healers so as to enable them give the appropriate plant species they usually use to manage infections. Doses were measured using 0.5 L plastic cups or stainless-steel tablespoons but there was ambiguity on how this was applied (Tables 3, 4, 5, 6, 7). Duration of treatment depended on time of disappearance of symptoms and was not specific but varied from herbalists to herbalist. Time of treatment depends on when one recovers. Estimates of doses is not uniform and depend on age, and type of infection. Most of the TMPs did not keep record on infections treated or nutraceutical plants used (Table 7). All TMPs had insufficient knowledge about packaging and presentation techniques. Transmission of knowledge to trainers of nutraceutical plant use was mainly informal (Table 7).
Discussion
Profile of traditional medicine practitioners
Although both men and women use nutraceutical plants to manage opportunistic infections associated with HIV/AIDS, women showed great extent of their traditional knowledge than men (Table 1). These results are in agreement with several other reports which found the same tendency in their studies about nutraceutical plant knowledge [66–68], in that women knew more about nutraceutical plants than men. The predominance of women, could be because women had double role as the nutritional food providers and family primary health caregivers during an illness, this may explain their expertise in nutraceutical plant use. Cheikhyoussef et al. [69], observed that traditional healing is a gender-based practice. Results in this study are similar to reports from Jeddah, Saudi Arabia, where preference for medicinal plant use is dependent on gendered socio roles and experience [70]. Gender role analysis by Singhal [71] in relation to medicinal plants revealed that collection, processing, storage, utilisation of medicinal plants is mainly assigned to women.
Although both adults and elders (above 50 years) use nutraceutical plants to manage opportunistic infections associated with HIV/AIDS, elders (above 50 years) showed great extent of their traditional knowledge than adults (Table 1). These results are consistent with those obtained by [72–74], where diversity on nutraceutical plant species and uses cited among the young people were on average lower than number cited by the elderly. Ouhaddou et al. [75] also reported that elderly herbalists, above 50 years of age, have more knowledge on medicinal plants with regard to other age groups. Reasons for greater knowledge could be that with progressive age, people have more time to accumulate knowledge and, therefore, show greater nutraceutical plant knowledge and the lesser knowledge in the younger population is because of the ongoing socio-economic and cultural changes [72].
Although there was no significant difference in nutraceutical plant knowledge between the illiterate and literate respondents (p>0.05), the mean number of plants cited by illiterate TMPs was higher than those of their literate counterparts (Table 1). These results are consistent with those obtained by [66, 73, 76], who observed that nutraceutical plant species and uses cited among the educated are on average lower than the number cited by the illiterate. Weckmuller et al., [66] observed that among Waorani society, Equador, formal education programs marginalise indigenous knowledge on nutraceutical plants by encouraging an urban lifestyle that leads to lack of interest in nutraceutical plants. Bruyere et al., [76] proposes that communities undergoing change should develop options to transmit traditional knowledge on nutraceutical plants to its younger population who are undertaking formal education and lack interest in nutraceutical plant knowledge. Respondents belonged to different religions (Table 1). Religion teaches people moral behaviour, provides support during depression, anxiety and offers guidance with coping skills during an illness [77].
Diversity of nutraceutical plants, their use, and growth forms
This Ethnobotanical study recorded eighty four (84) nutraceutical plant species distributed in 38 plant families and 76 genera, used to manage opportunistic infections associated with HIV/AIDS in Gulu, Amuru and Pader districts. Most abundant families were Leguminoceae, Asteraceae, Solanaceae. Family Leguminosae contain alkaloids, amino acids, cynogenetic glucosides, anthocyanins, tannins, flavonoids [79]. Asteraceae contain terpenes/terpenoids, carboxylic and fatty acids [80], while Solanaceae contain solanine, tomatidine, capsaicin [81]. Shrubs were mostly used, because they are easily found and can withstand semi-arid climate while taking shorter time to mature than trees [78]. Most of the nutraceutical plants were found in bushes, where they were wild and abundant [45]. Al-Obaidi et al. [78] agrees that medicinal shrubs are easily available than herbs, because they can grow in arid and semi-arid areas. The bioactivity of nutraceutical plant shrubs could be attributed to the presence of secondary metabolites [79–81].
Methods of preparation, administration and preservation
Leaves were most frequently used for preparation of medicine, followed by bark and roots (Tables 3, 4, 5). The bioactivity of these leaves, bark and roots of nutraceutical plant could be attributed to the presence of secondary metabolites. The frequent use of leaves, bark and roots was also reported by [45], who observed unsustainable harvesting techniques of nutraceutical plants in Northern Uganda.
Decoctions/boiling in water (70%) were commonly used as mode of preparation and oral route (76%) was most used route of adminstration. Majority of preparation was made using water as a medium, as also reported in studies by [87, 88]. According to Tugume et al. [67] boiling in water is effective in extracting plant materials and preserving remedies for a longer period compared to maceration in water. Saikia et al. and Mesfin et al. [87, 88] also reported that most common route of administration of herbal preparation was oral route. According to Kim and De Jesus [88] the oral route of administration is a convenient, cost-effective and most commonly used drug administration route. The primary site of drug absorption is usually the small intestine and the bioavailability of the drug is influenced by the amount of drug absorbed across the intestinal epithelium [88].
The number of nutraceutical plants recorded in the study area is lower than medicinal plants recorded by Anywar et al. [13] (n = 236), but comparable to the the number of medicinal plants recorded by Mugisha et al. [82], (n = 81), Tahir et al. [31] (n = 103) Lamorde et al. [39] (n = 103) and Shehu et al. [32] (n = 52). These ethnobotanical studies, indicate that the majority of nutraceutical and aromatic plants come from wild sources and is the source of livelihood for millions of people. Ethnobotanical studies facilitate participation of an ethnic people in the collection and assessment of botanical knowledge through field studies, which give valid information about the utility of plant species [83–85].
Ailments treated
The antibacterial properties of Eucalytptus globulus Labill, Cajanus cajan L. Millsp and Mangifera indica L.
The leaves of Eucalytptus globulus Labill (known as Kalatuc in Acholi) are used for treating cough, tuberculosis, and chest infections. Bachir and Benali [89] reported that essential oil in leaves of Eucalyptus globulus has antimicrobial activity against bacteria. Alvarenga et al. [90], also reported thirty two (32) airbone anti-Tuberculosis components were identified in Eucalyptus citriodora. Phytochemical analysis of leaf extract of Eucalyptus globulus proved the presence of tannins, saponins, terpenoids, glycosides, alkaloids, phenolic compounds, cardiac glycosides, terpenes, reducing sugars, acrbohydrates, flavonoids [91].
The leaves of Cajanus cajan L. Millsp (also known as pigeon pea—English, Lapena—Acholi), are used to treat cough, tuberculosis, chest infections. Cajanus cajan is an important grain–legume food crop with high levels of proteins [92]. Saxena et al. [93] reported that Pigeon pea Cajanus cajan is capable to prevent and cure bronchitis, cough, pneumonia and respiratory infection. Oke [94] reported Cajanus cajan leaves to contain alkaloids, flavonoids, tannins, saponins, terpenes, phlobatannins, anthraquinones and sterols.
The tree bark of Mangifera indica L. (known as Mango—English, Muyeeme—Acholi) are used for treating Diarrhoea, dysentry and stomach-ache. Study by Osei-Djarberg et al. [95] showed that bark and leaf extracts of Mangifera indica has antimicrobial activity. Sanusi et al. [96] reported that the antimicrobial activity obtained in their study support the claim by the local communities for the use of Mangifera indica stem bark decoction for treatment of infections, such as diarrhoea. Phytochemical screening of crude stem bark extracts of Mangifera indica revealed the presence of tannins, saponins, alkaloids, flavonoids, cardiacglycosides and phytosterols [96].
The antifungal properties of Momordica foetida Schumach and Erigeron floribundus (Kunth) Sch. Bip
The roots of Momordica foetida Schumach (known as Bitter cucumber—English and Bomo—Acholi) are used to treat genital and oral candidiasis. Our results are supported by findings of [44] who reported that commonest plant used to manage candidiasis in Northern Uganda was Momordica foetida. Muronga et al. [97] found Momordica foetida to contain proteins, fibres, terpenoids, glycocides, alkaloids, flavonoids, tannins, phenolic compounds, gallic acid, phenolic glycosides, steroids, cardiac glycosides, phenolics, saponin, carotene.
Erigeron floribundus (Kunth) Sch. Bip (Dingtong—Acholi), leaves used for treating skin fungal infection. Berto et al., [98] reported that Erigeon floribundus is used for treatment of fungal skin infections and Candida. Bi et al. [99], observed antifungal activity of Erigeron floribundus against a wide range of dermatophytes. Moungang et al. and Dall’Acqua et al. [100, 101] found Erigeron floribundus to contain alkaloids, saponins, polyphenols, tannins, cardiac glycosides, flavonoids, quinones.
The immune boosting properties of Cucurbita pepo L.
Cucurbita pepo L. (Pumpkin—English, okono—Acholi) leaves was widely used for immune boosting. These results are consistent with a study by Almohaimeed et al. [102], were Cucurbita pepo L. enhanced wound healing process in rats through the antioxidant, anti-inflammatory and anti depressant activities.
Other nutraceutical plants recorded in this study were reported elsewhere. Albizia coriaria Oliv. is widely used in traditional medicine for treating opportunistic infections, such as skin infections, cough, syphilis, and sore throat among PLHIV in Uganda [12, 40]. Erythrina abyssinica Lam. has been reported to be used to treat tuberculosis in Uganda [103]. The root of Serudaca pedunculata Fresen. is commonly used in Uganda for treating STDs, T.B, and Coughs [12]. Maud et al. [104] noted that Hibiscus sabdariffa L, Plumeria obtuse L and Abutilon guineense were most frequently used by immune-compromised people with HIV/AIDS in Western Uganda. Acacia hockii used to manage opportunistic infections as reported by [36, 105]. A study conducted in Mieso district, eastern Ethiopia by [106] reported that of the 41 wild edible plant species, 13 species had medicinal value.
Analysis of informant consensus factor (ICF) indicated that the highest level of herbalists’ agreement on the nutraceutical plants used to manage bacterial and fungal infections was for Digestive system, Respiratory system and Dermatological systems with ICF Values of 0.88, 0.87 and 0.85, respectively, as shown in Table 6. These plants become target in efficacy tests [107, 108]. This determination of Informant consensus factor among local communities helps to evaluate drugs of herbal origin [109].
Conservation status of nutraceutical plants
Plant parts such as roots, bark, leaves, fruits or sap were harvested from bush, forest or garden (Tables 3, 4, 5). Most of the nutraceutical plants in study area are wild and abundant (Tables 3, 4, 5). These results are consistent with Uganda National Environment Management Authority report [42], where approximately 5000 species of higher plants in Uganda were recorded, of which 70 are endemic [42]. However, high percentage use of plant roots and bark threatens the sustainable use from the wild. The TMPs confirmed decrease in the richness and abundance of some plant species. The high nutraceutical plant species richness and species diversity in Northern Uganda needs to be protected [45]. Akwongo et al. [44] observed that unsustainable harvesting techniques in Northern Uganda, like uprooting plants may lead to loss of plant species diversity and indegenous knowledge. Oryema et al. [45], noted that plants used to manage tuberculosis in Northern Uganda faced conservation threats due to exploitation of roots.
Problems faced during quality control of nutraceuticals
Methods observed for quality control may not guarantee safety of use of these nutraceuticals (Tables 7). According to WHO [19] environmental pollution, misidentification and contamination all affect safety and quality of nutraceutical plants products. During collection, nutraceutical plant materials should be free from visible signs of contamination by insects, moulds, animal excreta. Any soil, sand, stones and other foreign inorganic matter should be removed before nutraceutical plants are cut or ground for testing [19]. No poisonous or dangerous foreign matter or residue allowed and no abnormal odour or discolouration allowed [19]. All equipment, tools and utensils used should be clean. Personnel engaged in herbal processing should maintain hygiene and wear protective clothing, gloves, head/hair covering and footwear [19].
TMPs reported lack of knowledge on preservation techniques and low earnings from selling nutraceutical plants. During storage, nutraceutical plants should be kept in a clean hygienic place to avoid contamination and formation of aflatoxins [19]. Nutraceutical plants should be protected from microbial insect, rodent and other pest contamination. Packaging should provide the best protection against moisture, light, heat and physical damage to the processed nutraceutical materials [19]. Stores should be clean, well-lit and have acceptable temperature [19]. Most of the TMPs did not keep records on infections treated or nutraceutical plants used. This was also reported by Addo-Fordjour [110], where no records of treatment were written down by TMPs, as they mostly depend on memory. According to WHO [19] record keeping is important in drug administration. Mahomoodally [111] reported that proper validation of traditional knowledge and quality control standards are lacking in Africa and these are some of the limitations to the growth of a modern African nutraceutical industry, compared to Europe and Asia, where Traditional methods and formulations have been recorded and evaluated both at national and local levels [111].
Conclusion
This study demonstrates the availability and diversity of nutraceutical plants in Northern Uganda and reports traditional methods used by TMPs during processing and administration. Both men and women used nutraceutical plants to manage opportunistic infections associated with HIV/AIDS and showed great extent of their traditional knowledge. Age and gender are the main factors that seem to influence the ethnobotanical knowledge of respondents. The observed Traditional methods and formulations used by TMPs do not guarantee safety and quality assurance due to several problems reported. Most of the nutraceutical plants in the study area are wild and abundant; however, high percentage use of plant roots and bark threatens the sustainable use from the wild.
Recommendations
Recommendations to National Forestry Authority, Uganda
Harvesting of nutraceutical plants from forests in Northern Uganda should be regulated by National Forestry Authority in Uganda. This will contribute to efforts to preserve and promote Nutraceutical plants in Northern Uganda.
Recommendations to National drug Authority, Uganda
The National Drug Authority should expand their operations to other regions of Uganda and set up regulatory control measures and standards to be used during collection, processing and storage. Quality assurance during production and utilisation of nutraceutical plants needs to be taken into account, since it directly impacts the safety and efficacy of nutraceutical plant products. Ministry of Education in Uganda is called upon to convene and train TMPs from all regions in Uganda about basic knowledge on diagnosis of disease, record maintenance, Legal systems, business management, processing and packaging nutraceutical plants for commercial use, how to maximize profits and protect their knowledge.
Recommendation to the Ministry of Health Uganda
Due to this high degree of medical pluralism, collaboration and communication between biomedical clinicians and Traditional medicine practitioners should be encouraged.
Recommendation to Gulu University and Registrar of Patents office, Uganda
Since Contemporary Intellectual Property Law permits only the Patenting of an identified Active Principle from a plant, not the plant or folk information relating to Medicinal properties of a plant [112], Copyright and Intellectual Property Rights (IPR) issues of Traditional medicine practitioners can be fully exploited with the help of Gulu University and Registrar of Patents office, Uganda.
Acknowledgements
I appreciate funding support from Regional Universities Forum (RUFORUM) and am grateful to all resource users and Traditional Medicine Practitioners who volunteered to take part in this study. Many thanks go to my Supervisors for guidance and proof-reading manuscript.
Abbreviations
- A.R.T
Anti-retroviral therapy
- ARV
Antiretroviral drugs
- C.D.C
Centres for disease control and prevention
- F. I
Familiarity index
- F.L.I
Fidelity level
- HIV/AIDS
Human immunodeficiency virus/acquired immunodeficiency syndrome
- I.C.F
Informant consensus factor
- S.T.D
Sexually transmitted diseases
- T.M.P
Traditional medicine practitioner
- UNAIDS
United Nations Programme on HIV/AIDS
- W.H.O
World Health Organization
- PLHIV
People living with HIV
Appendix
Table 8.
Nutraceutical plants in Gulu, Pader and Amuru districts used to manage bacterial opportunistic infections and mode of preparation for quality control
| Scientific name, Family, Local name in native ‘Acholi dialect’ | Accession number | Habit | Habitat | Conservation status | Bacterial opportunistic infection treated (uses) | Part used | Mode of preparation and administratn | Familiarity index | Fidelity Level |
|---|---|---|---|---|---|---|---|---|---|
|
Acacia hockii De Wild (Leguminoceae) Okuto-oriang |
MHU 32118 |
shrub | Bu | W/A | Cough. Diarrhea, stomachache | FL | Mix leaves in hot water, drink infusion | 0.058 | 0.115 |
|
Acalypha villicaulis Hochst (Euphorbiaceae). Ayila |
MHU 34107 |
Shrub | Bu | W/R | Diarrhea, eye infection | FR | Boil roots, drink decoction | 0.028 | 0.110 |
|
Afromomum angustifolium Sonn (Zingiberaceae) Oceyo |
MHU 31591 |
Herb | Bu | W/R | diarrhoea | FL |
Boil leaves, drink decoction |
0.003 | 0.001 |
|
Albizia coriaria Welw.ex.Oliv (Leguminoceae Ayek–ayek |
MHU 38528 |
Tree | Wo | W/R | Tuberculosis, chest infection, sore throat | FR |
Boil roots, drink decoction |
0.023 | 0.110 |
|
Albizia grandibracteata Taub Leguminoseae Awak Owak |
MHU 34331 |
Tree | Wo | W/A | Eye infection | FL | Macerate leaves in cold water, drink extract | 0.003 | 0.010 |
|
Ammocharis tinneana (Kotschy & Peyr.) Amaryllidaceae Joda |
MHU 41025 |
Bulb | Bu | W/R | cough | FL | Soak leaves in cold water, drink maceration | 0.003 | 0.01 |
|
Ampelocissus africana (Lour.)Merr Vitaceae Olok |
MHU 41684 |
Shrub | W/R | Diarhhoea | FR | Boil roots, drink decoction | 0.008 | 0.03 | |
|
Annona muricata L Annonaceae Obvolo |
MHU 51003 |
Shrub | Bu | W/A | Diarrhea. stomachache, chest infection | FR | Boil roots, drink decoction | 0.025 | 0.05 |
|
Asparagus africana Lam Asparagaceae Lagwari |
MHU 35783 |
Herb | Fo | W/R | Eye infection | FFr | Swallow fruits | 0.005 | 0.02 |
|
Azadirachta indica A.Juss Meliaceae Neem (English) |
MHU 50969 |
Tree | P | Cu/A | Cough, diarrhea, tb, stomachache | FL | Boil leaves in water, drink decoction | 0.025 | 0.02 |
|
Carica papaya.L Caricaceae Papai |
MHU 42266 |
Herb | Ho | Cu/A | Diarrhea, sore throat, stomachache | FR | Boil roots, drink decoction | 0.03 | 0.06 |
|
Carisa edulis (Forssk) Vahl Apocynaceae Ocuga |
MHU 35814 |
Spiny shrub | Fo | W/A | Sore throat, cough | FL | Mix leaves in hot water, drink infusion | 0.005 | 0.005 |
|
Cassia singueana Delile Leguminoseae Lakodok /akwadok |
MHU 39624 |
Tree | Bu | W/R | Eye infection | S | Squeeze sap in eye | 0.003 | 0.01 |
|
Cassia nigricans Vahl Leguminoseae Abanceng |
MHU 32957 |
Shrub | Bu | W/A | Abdominal pain, cough, sore throat | FL | Mix leaves with hot water, drink infusion | 0.045 | 0.09 |
|
Citrus limon(L.)Burm Rutaceae Lemun |
MHU 42222 |
Shrub | Ho | Cu/A | Cough | FFr | Squeeze fruit in water, drink | 0.008 | 0.003 |
|
Clematis hirsuta (Perr. & Guill.) Ranunculaceae Omwombyer(Acholi) |
MHU 32013 |
Shrub | Fo | W/R | Cough, sore throat, stomachache, diarrhoea | FR |
Boil roots, drink decoction |
0.008 | 0.030 |
|
Clerodendrum myricoides (Hochst.)R.Br.ex Vatke Lamiaceae Okwero (Acholi) |
MHU 38184 |
Shrub | Fo | W/R | Cough, eye infection, stomachache | FR | Boil roots in water, drink decoction | 0.018 | 0.070 |
|
Echinops amplexicaulis Oliv Astereceae Alilokwang |
MHU 37710 |
Shrub | Bu | W/R | Ear infection | FR | Boil roots, drink decoction | 0.003 | 0.01 |
|
Erigeron floribundus (kunth) Asteraceae Aditong/ Gwelworu |
MHU 51148 |
Herb | Rs | W/A | Cough, sore throat | FL | Chew leaves, infusion leaves | 0.028 | 0.004 |
|
Erythrina abyssinica Lam.ex DC Leguminoceae Lucoro |
MHU 42157 |
Tree | Fo | W/A | Eye and ear infection, diarrhea, wounds | FSB |
Boil bark, drink decoction |
0.013 | 0.013 |
|
Euphorbia hirta L Euphorbiaceae Acak–acak |
MHU 42795 |
Herb | Rs | W/A |
Syphilis, wounds stomachache |
S | Apply sap on warts | 0.01 | 0.02 |
|
Euphorbia tirucalli L Euphorbiaceae Kilajok |
MHU 50984 |
Shrub | Bu | W/A | Eye infection, cough, eye infection, diarrhoea | S | Squeeze sap into eye | 0.063 | 0.250 |
|
Ficus sycomorus L Moraceae Olam |
MHU 37779 |
Tree | Bu | W/A | Syphilis, diarrhea, stomachache | FL,FSB | Boil leaves or bark in water, drink decoction | 0.048 | 0.011 |
|
Ficus vasta Forssk Moraceae Foyo |
MHU 36129 |
Tree | Bu | W/R | Diarrhea | FL | Mix leaves in hot water, drink infusion | 0.003 | 0.01 |
|
Gardenia ternifolia Schum.& Thorn Rubiaceae Odwong |
MHU 35775 |
Tree | Bu | W/A | Ear infection, tb, cough | S | Roast leaves, drip sap in ear | 0.013 | 0.025 |
|
Gynandropsis gynandra (L.) Cleomeaceae Akeyo |
MHU 35828 |
Herb | Ga | Cu/A | Ear and eye infection | FR | Boil roots, drink decoction | 0.043 | 0.015 |
|
Harisonia abyssinica Oliv Rutaceae Pedo |
MHU 35837 |
Shrub | Bu | W/R | Tuberculosis, cough, eye infection, diarrhoea | FL | Mix leaves in hot water, drink infusion | 0.020 | 0.03 |
|
Harungana madagascariensis Lam. Ex Poiret Hypericaceae Aremu |
MHU 32681 |
Big shrub | Fo | W/R | Diarrhea, stomachache | FR | Boil roots, drink decoction | 0.023 | 0.09 |
|
Hibiscus sabdariffa (L.) Malvaceae Malakwang |
MHU 41711 |
Shrub | Ga | Cu/A | Eye infection | FL | Cook leaves, eat as vegetable | 0.005 | 0.010 |
|
Hoslundia opposita Vahl Lamiaceae Tuutu |
MHU 41663 |
Shrub | Bu | W/R | Diarrhea, sore throat | FR |
Boil roots, drink decoction |
0.008 | 0.006 |
|
Hyparrhenia rufa (Nees) Stapf Poaceae Ajuu |
MHU 33697 |
Grass | Gr | W/A | Eye infection | FR | Boil roots, drink decoction | 0.003 | 0.01 |
|
Indigofera arrecta Hochst. A.Rich Leguminoceae Laywer |
MHU 33709 |
Shrub | Bu | W/A | Stomachache. Cough, sore throat, tb | FR | Boil roots, drink decoction | 0.030 | 0.017 |
|
Khaya senegalensis (Desr.) A.Juss Meliaceae Tido |
MHU 42488 |
Tree | Bu | W/A | Diarrhoea, cough, stomachache | FSB | Boil bark, drink decoction | 0.028 | 0.005 |
|
Kigelia africana (Lam.)Benth Bigoniaceae Yago |
MHU 31702 |
Tree | Fo | W/R | Cough | FR |
Boil roots, drink decoction |
0.005 | 0.02 |
|
Lantana camara L Verbenaceae Abelwinyu |
MHU 50924 |
Shrub | Bu | W/A | Sore throat, ear infection, cough, eye infection | FL | Mix leaves with hot water, drink infusion | 0.010 | 0.02 |
|
Lippia javanica (Burm.f.) Spreng Verbenaceae Orwo |
MHU 31966 |
Herb | Bu | W/R | Sore throat, eye infection | FL | Chew leaves | 0.003 | 0.03 |
|
Lonchocarpus laxiflorus Guill &Perr Leguminoceae Olwedo |
MHU 43280 |
Tree | Fo | W/A | T.B, Respiratory tract infection, chest pain | FL | Mix leaves in hot water, drink infusion | 0.020 | 0.011 |
|
Moringa oleifera L Moringaceae Moringa |
MHU 41303 |
Tree | Wo | Cu/A | Stomachache, cough | FL | Mix leaves in hot water, drink infusion | 0.008 | 0.010 |
|
Musa paradisiaca L Musaseae Labolo |
AAA-EA | Herb | P | Cu/A | Diarrhea, wounds | S | Mix sap in cold water, drink | 0.018 | 0.009 |
|
Occimum gratissimum L Lamiaceae Mida |
MHU 35677 |
Herb | Rs | W/A | Cough | FL | Mix leaves in hot water, drink infusion | 0.005 | 0.001 |
|
Persea americana Mill Anacardiaceae Avocado (English) |
MHU 42243 |
Tree | Ho | Cu/A | Chest infection | FL | Boil leaves, drink decoction | 0.003 | 0.001 |
|
Physalis minima Linn Solanaceae Kong-ogwal |
MHU 37418 |
Herb | Rs | W/A | Sore throat | FR | Boil roots, drink decoction | 0.003 | 0.010 |
|
Pistia stratiotes L Araceae Lagada |
MHU 40124 |
Herb | Sw | W/R | Eye infection, cough | S | Drip leaf sap in eye | 0.010 | 0.04 |
|
Pseudocedrella kotschyi (Schweinf.) Meliaceae Ofuti |
MHU 50947 |
Tree | Bu | W/A | Diarrhoea | FR | Boil roots, drink decoction | 0.008 | 0.003 |
|
Psidium guajava L Myrtaceae ‘ Mupeera |
MHU 42105 |
Tree | Ho | Cu/α | Cough | FL |
Boil leaves, drink decoction |
0.010 | 0.04 |
|
Sansevieria newtoniana T.G Asparagaceae Tworo-gwok |
MHU 42552 |
Herb | Bu | W/R | Diarrhea, ear infection | FL | Macerate leaves by soaking in cold water, drink extract | 0.010 | 0.004 |
|
Sarcocephalus latifolius Smith Rubiaceae Munyu |
MHU 50529 |
Tree | Bu | W/A | Diarrhea, syphillis | FR,FSB | Boil roots or bark in water, drink decoction | 0.008 | 0.004 |
|
Senna obtisifolia (L.) Leguminoseae Oyedo |
MHU 36690 |
Shrub | Fo | W/R | Eye infection, sore throat | S | Squeeze sap in eye | 0.005 | 0.010 |
|
Solanecio manii (Hook.f.)C Solanaceae Taa-lyec |
MHU 50551 |
Shrub | Bu | W/A | Abdominal pain, chest pain | FR | Boil roots in water, drink decoction | 0.008 | 0.003 |
|
Solanum aethiopicum L Solanaceae Tula |
MHU 32755 |
Shrub | Ga | Cu/A | Diarrhea | FFr | Cook fruits, eat as vegetable | 0.003 | 0.01 |
|
Sporobolus pyramidalis P.Beauv Poaceae Ajiki (Acholi) |
MHU 40673 |
Grass | Gr | W/A | Cough, sore throat | FL | Mix leaves in hot water, drink infusion | 0.010 | 0.04 |
|
Steganotaenia araliacea Hochst Apiaceae Olwiro |
MHU 38029 |
Shrub | Fo | W/R | Syphilis, T.B, respiratory tract infection | FR | Boil roots in water, drink decoction | 0.018 | 0.035 |
|
Tamarindus indica L Leguminoseae Cwaa |
MHU 40035 |
Tree | Ho | Cu/A | Diarrhea | FL,FSB | Boil leaves or root, drink decoction | 0.003 | 0.010 |
|
Teclea nobilis Delile Rutaceae Acha–acha |
MHU 32391 |
shrub | Bu | W/R | Stomachache | FL,FR | Mix leaves, roots in hot water, drink infusion | 0.015 | 0.06 |
|
Terminalia glaucescens Planch.ex.Benth Combretaceae Opok |
MHU 42410 |
Tree | Fo | W/R | Cough, stomachache, syphilis | FL | Chew leaves, boil roots in water, drink decoction | 0.015 | 0.06 |
|
Uapaca guineensis Mull-Arg Euphorbiaceae Acak |
MHU 32266 |
Tree | Bu | W/A | Syphilis, stomachache | FR | Boil roots, drink decoction | 0.003 | 0.020 |
|
Vernonia amygdalina Del Asteraceae Labwori |
MHU 42532 |
Shrub | Bu | W/A | Cough, diarrhea, stomachache | FL | Mix leaves in hot water, drink infusion | 0.030 | 0.003 |
|
Vernonia lasiopus O.Hoffm Asteraceace Labuka |
MHU 35754 |
Shrub | Bu | W/R | Eye and ear infection, stomachache | S | Squeeze sap into ear, eye | 0.048 | 0.095 |
|
Vigna unguiculata (L) Walp Leguminoceae Boo |
MHU 35800 |
Herb | Ga | Cu/A | Ear infection | FL | Cook leaves, eat as vegetable | 0.030 | 0.01 |
|
Vitellaria paradoxa Gaetn Sapotaceae Yaa |
MHU 33728 |
Tree | Ho | Cu/A | Diarrhea, stomachache | FSe | soak crushed seeds in cold water by maceration, drink | 0.018 | 0.01 |
|
Vitex doniana L Verbenaceae Oywelo |
MHU 35770 |
Tree | Bu | W/A | Diarrhea, chest pain, tb, ear and eye infection | FR | Boil roots in water, drink decoction | 0.015 | 0.060 |
|
Waburgia ugandensis Sprague Canellaceae Abaki |
MHU 50888 |
Tree | Bu | W/R | Tuberculosis, respiratory tract infection, chest pain, stomachache | FSB | Boil bark in water, drink decoction | 0.020 | 0.080 |
|
Zingziber officinale (L)H.Karst Zingiberaceae Tangawuzi |
MHU 51051 |
herb | Ga | Cu/A | Cough | FR |
Boil roots drink decoction |
0.008 | 0.030 |
|
Zizyphus abyssinica Hochst Rhamnaceae Lango |
MHU 33483 |
Shrub | Bu | W/A | Ear infection, diarrhea | FL | Mix leaves in cold water, drink extract | 0.005 | 0.020 |
Parts used: FL: fresh leaf, FR: fresh Root, FSB: fresh stem bark, FSe: fresh seed, FFr: fresh fruit, Bu: bulb, S: sap
Habitat: Bu—bushland, Gr—grassland, Ho—homestead, Rs—roadside, P—plantation, Sw—swamp, Ga—garden, Fo—forest, Wo—woodland
Conservation status: W/A: wild and abundant, W/R: wild and rare, Cu/A: cultivated and abundant, Cu/R: cultivated and rare
Decoction: water extraction by boiling of dissolved plant material and drank
Infusion: plant material is added to hot water and left to stand for few minutes and drank
Table 9.
Nutraceutical plants used to manage fungal opportunistic infections and mode of preparation for quality control
| Scientific name, Family, Local name in native ‘Acholi dialect’ | Accession number | Habit | Habitat | Conservation status | Fungal opportunistic infection (uses) | Part used | Mode of preparation | Familiarity Index | Fidelity level |
|---|---|---|---|---|---|---|---|---|---|
|
Anacardium occidentale L Anacardiaceae Fulmunnu |
MHU 42396 |
T | Ho | Cu/A | Oral candidiasis | FB | Boil bark, drink decoction | 0.015 | 0.020 |
|
Artocarpus heterophyllus Lam Moraceae Fene |
MHU 40229 |
T | Ho | Cu/A | Oral candidiasis | FR | Boil roots, drink decoction | 0.003 | 0.005 |
|
Cajanus cajan (L.) Millsp. Leguminoceae Lapena |
MHU 51151 |
S | Ga | Cu/A | Oral candidiasis | FL | Chew leaves | 0.003 | 0.0001 |
|
Carisa edulis (Vahl.) Apocynaceae Ocuga |
MHU 35814 |
S | W/A | Oral candidiasis | FL | Boil leaves, drink decoction | 0.005 | 0.0100 | |
|
Citrus limon (L.) Burm Rutaceae Lemun |
MHU 42222 |
S | Ho | Cu/A | Skin fungal infection | FFr | Rub fruit peel on skin | 0.003 | 0.0009 |
|
Clerodendrum swienfuthii L Lamiaceae Lacer |
MHU 40967 |
S | Bu | W/R | Oral candidiasis | FL | Boil leaves, drink decoction | 0.015 | 0.0030 |
|
Cucurbita pepo L Cucurbitaceae Okono |
MHU 42492 |
C | Ga | Cu/A | Skin fungal infection | FL | Rub leaves on skin | 0.003 | 0.0007 |
|
Cucurma longa L Zingiberaceae Binzaali |
MHU OJ55 |
H | Ga | Cu/A | Oral candidiasis | DR | Mix powdered root in water, drink | 0.003 | 0.010 |
|
Erythrina abyssinica Lam Leguminoseae Lucoro |
MHU 32166 |
T | Bu | W/A | Oral candidiasis | FR | Boil roots, drink decoction | 0.010 | 0.002 |
|
Euphorbia hirta L Euphorbaiceae Acak–acak |
MHU 50984 |
H | Bu | W/A | Skin fungal infection, oral candidiasis | FL | Rub leaves on skin | 0.005 | 0.001 |
|
Harisonia abyssinica Oliv Rutaceae Pedo |
MHU 35837 |
S | Bu | W/R | oral candidiasis | FL | Boil leaves, drink decoction | 0.005 | 0.005 |
|
Harungana madagascariensis Lam. Ex Poir Hypericaceae Aremu |
MHU 32681 |
S | Bu | W/R | Skin fungal infection | FL | Boil leaves, drink decoction | 0.003 | 0.001 |
|
Hoslundia opposita Vahl Lamiaceae Tuutu |
MHU 31950 |
S | Bu | W/R | Oral candidiasis. Candida, skin fungal infection | FR | Boil roots, drink decoction | 0.010 | 0..008 |
|
Imperata cylindrica (L.) Poaceae Obiya |
MHU 35056 |
G | Gr | W/A | Oral candidiasis | FR | Boil roots, drink decoction | 0.003 | 0.0014 |
|
Indigofera arrecta Hochst.ex A.Rich Leguminosae Laywer |
MHU 42857 |
S | Bu | W/A | Oral candidiasis | FL | Boil leaves, drink decoction | 0.003 | 0.0014 |
|
Lantana camara L Verbenaceae Abelwinyu |
MHU 50924 |
S | Bu | W/A | Oral candidiasis | FL | Soak leaves in hot water, drink infusion | 0.005 | 0.005 |
|
Lippia javanica Burm.f. spreng Verbenaceae Orwo |
MHU 31966 |
S | Bu | W/R | Skin fungal infection | FL | Boil leaves, drink decoction | 0.003 | 0.003 |
|
Lonchocarpus laxiflorus Guill. & Perr Leguminoseae Olwedo |
MHU 43280 |
T | Bu | W/R | Oral candidiasis, Skin fungal infection | FR | Boil roots, drink decoction | 0.010 | 0.0036 |
|
Luffa cylindrical (Linn.) M.J.Roem Cucurbitaceae Amoo |
MHU 41714 |
C | Ga | Cu/A | Skin fungal infection | FL | Rub leaves on skin | 0.013 | 0.005 |
|
Moringa oleifera Lam Moringaceae Moringa (scientific) |
MHU 50971 |
T | Ho | Cu/A | Oral candidiasis | FL | Boil leaves, drink decoction | 0.005 | 0.003 |
|
Musa paradisiaca L Musaceae Labolo |
AAA-EA | H | p | Cu/A | Oral candidiasis, skin fungal infection | S | Mix sap in water, drink | 0.010 | 0.0067 |
|
Piliostigma thonningii (Schumach) Milne-Redh Leguminoseae Ogali |
MHU 35791 |
S | Bu | W/A | skin fungal infect, oral candidiasis | FL | Boil leaves, drink decoction | 0.010 | 0.0014 |
|
Psidium guajava L Myrtaceae Mupera |
MHU 42105 |
T | Ho | Cu/A | Oral candidiasis | FL | Soak leaves in hot water, drink infusion | 0.003 | 0.002 |
|
Ricinus communis L Euphorbaceae Coga macon |
MHU 42123 |
S | Bu | W/A | Oral candidiasis | FL | Boil leaves, drink decoction | 0.003 | 0.005 |
|
Securidaca longipenduculata Fresen polygalaceae lalia |
MHU 35766 |
T | Bu | W/R | Skin fungal infection | FR | Boil roots, drink decoction | 0.003 | 0.0025 |
|
Senna obtisifolia L Leguminoceae oyedo |
MHU 36690 |
S | Bu | W/A | Skin fungal infection | FR | Boil leaves, drink decoction | 0.003 | 0.0033 |
|
Solanum incanum L Solanaceae Ocok |
MHU 35802 |
S | Rs | W/A | Oral candidiasis | FL | Boil roots, drink decoction | 0.003 | 0.0003 |
|
Vernonia amygdalina Del Astereceae Labwori |
MHU 42532 |
S | Bu | W/A | Skin fungal infection, oral candidiasis | FL | Boil leaves, drink decoction | 0.018 | 0.0015 |
|
Vernonia lasiopus O. Hffm Asteraceae Labuka |
MHU 35754 |
S | Bu | W/R | Candida of genitals | FL | Rub leaves on gentitals | 0.003 | 0.0005 |
|
Vitellaria paradoxa C.F.Gaetn Verbenaceae Yaa |
MHU 33728 |
T | Ho | Cu/A | Oral candidiasis | FSe | Soak crushed seeds in cold water by maceration, drink | 0.015 | 0.0088 |
Parts used: FL: fresh leaf, FR: fresh Root, FSB: fresh stem bark, FSe: fresh seed, FFr: fresh fruit, Bu: bulb, S: sap
Habitat: Bu—bushland, Gr—grassland, Ho—homestead, Rs—roadside, P—plantation, Sw—swamp, Ga—garden, Fo—forest, Wo—woodland
Habit: S—shrub, T—tree, H—herb, C—climber, G—grass
Conservation status: W/A: wild and abundant, W/R: wild and rare, Cu/A: cultivated and abundant, Cu/R: cultivated and rare
Decoction: water extraction by boiling of dissolved plant material and drank
Infusion: plant material is added to hot water and left to stand for few minutes and drank
Author contributions
NI: conceptualization, funding acquisition, methodology, investigation, data curation, validation, formal analysis, writing—original draft and editing, visualization. AL: writing—review and editing, supervision. ATM: writing—review and editing, supervision. EN: writing—review and editing, supervision. All authors read and approved the final manuscript.
Funding
The Regional Universities Forum (RUFORUM) provided financial support for the conduct of the Research. The Funding source had no involvement in study design, collection, analysis and interpretation of data, writing report and decision to submit article for publication.
Availability of data and materials
The data sets during and /or analysed during the current study are available from the corresponding author on reasonable request.
Declarations
Ethics approval and consent to participate in the study
Ethical approval for the study was obtained from Gulu University Research Ethics Committee (Ref. GUREC-062-20) and Uganda National Council for Science and Technology (Ref. HS983ES). Prior to the study, permission from the Local Council chairpersons (LC I, II and III) of each Subcounty, Parish and village was obtained. Approval was sought from regional administration in the study areas who were notified of the study’s objectives. The scope, possible benefits and risks of the study were explained to willing interviewees and Focus Group participants who signed consent forms after agreement. The prior-informed consent (PIC) form was translated into the local Acholi language. Identity of interviewees and Focus Group participants were protected via anonymisation.
Consent for publication
This manuscript does not contain any individual person’s data in any form. Consent for publication is not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.H. I. V Global, “AIDS statistics—2019 fact sheet [https://www.unaids.org/en/resources/fact-sheet].” Accessed, 2021.
- 2.Bosson-Vanga H, et al. Anticandidosic activity of selected medicinal plants from Cte dIvoire. J Yeast Fungal Res. 2018;9(4):27–32. [Google Scholar]
- 3.Tang JW, Chan PK. The basics of HIV medicine. SS Lee, JCY, 2007.
- 4.Ward AB, Wilson IA. The HIV-1 envelope glycoprotein structure: nailing down a moving target. Immunol Rev. 2017;275(1):21–32. doi: 10.1111/imr.12507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Blood GAC. Human immunodeficiency virus (HIV) Transfusion Med Hemother. 2016;43(3):203. doi: 10.1159/000445852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zgoda JR, Porter JR. A convenient microdilution method for screening natural products against bacteria and fungi. Pharm Biol. 2001;39(3):221–225. [Google Scholar]
- 7.Maulsby CH, Ratnayake A, Hesson D, Mugavero MJ, Latkin CA. A scoping review of employment and HIV. AIDS Behav. 2020;24:2942–2955. doi: 10.1007/s10461-020-02845-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Phillips AN, et al. Impact of HIV drug resistance on HIV/AIDS-associated mortality, new infections, and antiretroviral therapy program costs in sub–Saharan Africa. J Infect Dis. 2017;215(9):1362–1365. doi: 10.1093/infdis/jix089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Riddler SA, et al. Impact of HIV infection and HAART on serum lipids in men. JAMA. 2003;289(22):2978–2982. doi: 10.1001/jama.289.22.2978. [DOI] [PubMed] [Google Scholar]
- 10.Rubaihayo J, Tumwesigye NM, Konde-Lule J, Wamani H, Nakku-Joloba E, Makumbi F. Frequency and distribution patterns of opportunistic infections associated with HIV/AIDS in Uganda. BMC Res Notes. 2016;9(1):1–16. doi: 10.1186/s13104-016-2317-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mustapha AA. Ethnobotanical field survey of medicinal plants used by traditional medicine practitioners to manage HIV/AIDS opportunistic infections and their prophylaxis in Keffi Metropolis, Nigeria. Asian J Plant Sci Res. 2014;4(1):7–14. [Google Scholar]
- 12.Anywar G, Kakudidi E, Byamukama R, Mukonzo J, Schubert A, Oryem-Origa H. Data on medicinal plants used by herbalists for boosting immunity in people living with HIV/AIDS in Uganda. Data Brief. 2020;29:105097. doi: 10.1016/j.dib.2019.105097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.C. UNAS. Antibiotic Resistance in Uganda: situation analysis and recommendations. Kampala, Uganda: Uganda National Academy of Sciences. Center for Disease Dynamics, Economics & Policy, 107, 2015.
- 14.Ampaire L, Muhindo A, Orikiriza P, Mwanga-Amumpaire J, Boum Y, Bebell L. A review of antimicrobial resistance in East Africa. Afr J Lab Med. 2016;5(1):1–6. doi: 10.4102/ajlm.v5i1.432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Langlois-Klassen D, Kipp W, Jhangri GS, Rubaale T. Use of traditional herbal medicine by AIDS patients in Kabarole District, western Uganda. Am J Trop Med Hyg. 2007;77(4):757. [PubMed] [Google Scholar]
- 16.Thomas JC, Agala B, Xiong K, Powell R. Improving referrals for HIV care through organizational network analysis. J Public Health Manag Pract. 2019;25(3):E36–E44. doi: 10.1097/PHH.0000000000000839. [DOI] [PubMed] [Google Scholar]
- 17.Sonnenberg P, et al. The effect of HIV infection on time off work in a large cohort of gold miners with known dates of seroconversion. Occup Environ Med. 2011;68(9):647–652. doi: 10.1136/oem.2010.058487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Organization WH, WHO global report on traditional and complementary medicine 2019. World Health Organization, 2019.
- 19.de la Salud OM, Organization WH. WHO guidelines on good agricultural and collection practices [GACP] for medicinal plants. World Health Organization, 2003.
- 20.Yadav P, Prajapati PK. Quality control parameters for medicinal plants, an overview. Asian J Biomed Pharm Sci. 2011;1(5):12–16. [Google Scholar]
- 21.Zhang X, Organization WH. Traditional medicine strategy 2002 2005. 2002.
- 22.Teke GN, Kuete V. Acute and subacute toxicities of African medicinal plants. in Toxicological survey of African medicinal plants, Elsevier, 2014, pp. 63–98.
- 23.Sofowora A, Ogunbodede E, Onayade A. The role and place of medicinal plants in the strategies for disease prevention. Afr J Tradit Complement Altern Med. 2013;10(5):210–229. doi: 10.4314/ajtcam.v10i5.2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Evans WC, Trease GE. Pharmacognosy. Saunders London, 2002.
- 25.Geethanjali D, Rani MS, Jayalakshmi V. Estimates of direct and indirect effects among yield, yield contributing and quality traits in kabuli chickpea (Cicer arietinum L.) J Food Legumes. 2018;31(3):186–190. [Google Scholar]
- 26.Ullah I et al. Quantitative study of medicinal plants and biological activities of two common species used by inhabitants of district Bannu, Pakistan. Acta Ecologica Sinica. 2021.
- 27.Adnan M, Ali S, Sheikh K, Amber R. Review on antibacterial activity of Himalayan medicinal plants traditionally used to treat pneumonia and tuberculosis. J Pharm Pharmacol. 2019;71(11):1599–1625. doi: 10.1111/jphp.13156. [DOI] [PubMed] [Google Scholar]
- 28.Voravuthikunchai SP, Phongpaichit S, Subhadhirasakul S. Evaluation of antibacterial activities of medicinal plants widely used among AIDS patients in Thailand. Pharm Biol. 2005;43(8):701–706. [Google Scholar]
- 29.Fassil A, Habtamu T, Tahir M, Terefe T. Diversity, floral phenology, and socio-economic importance of melliferous plants in Eastern Ethiopia. Nusantara Biosci. 2022;14(2).
- 30.Tahir M, Gebremichael L, Beyene T, Van Damme P. Ethnobotanical study of medicinal plants in Adwa district, central zone of Tigray regional state, northern Ethiopia. J Ethnobiol Ethnomed. 2021;17(1):1–13. doi: 10.1186/s13002-021-00498-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tahir M, Asnake H, Beyene T, Van Damme P, Mohammed A. Ethnobotanical study of medicinal plants in Asagirt District, Northeastern Ethiopia. Trop Med Health. 2023;51(1):1–13. doi: 10.1186/s41182-023-00493-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shehu MW, Bello I, Abdulkadir N, Shehu A, Jamil SE, Waziri SA. Utilization of medicinal plants used in the management of HIV/AIDS opportunistic infections in Njeru sub-county, Buikwe district, Uganda. MOJ Bioequiv Availab. 2018;5(1):85. [Google Scholar]
- 33.Chinsembu KC. “Ethnobotanical study of plants used in the management of HIV/AIDS-related diseases in Livingstone, Southern Province, Zambia. Evid-Based Complement Alternat Med. 2016;2016:1. doi: 10.1155/2016/4238625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Otang WM, Grierson DS, Ndip RN. Ethnobotanical survey of medicinal plants used in the management of opportunistic fungal infections in HIV/AIDS patients in the Amathole District of the Eastern Cape Province, South Africa. J Med Plants Res. 2012;6(11):2071–2080. [Google Scholar]
- 35.Semenya SS, Potgieter MJ, Erasmus LJC. Ethnobotanical survey of medicinal plants used by Bapedi traditional healers to manage HIV/AIDS in the Limpopo Province, South Africa. J Med Plants Res. 2013;7(8):434–441. [Google Scholar]
- 36.Kisangau DP, Lyaruu HVM, Hosea KM, Joseph CC. Use of traditional medicines in the management of HIV/AIDS opportunistic infections in Tanzania: a case in the Bukoba rural district. J Ethnobiol Ethnomed. 2007;3(1):1–8. doi: 10.1186/1746-4269-3-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Davids D, et al. Traditional health practitioners’ perceptions, herbal treatment and management of HIV and related opportunistic infections. J Ethnobiol Ethnomed. 2014;10(1):1–14. doi: 10.1186/1746-4269-10-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Nagata JM, Jew AR, Kimeu JM, Salmen CR, Bukusi EA, Cohen CR. Medical pluralism on Mfangano Island: use of medicinal plants among persons living with HIV/AIDS in Suba District, Kenya. J Ethnopharmacol. 2011;135(2):501–509. doi: 10.1016/j.jep.2011.03.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Lamorde M, et al. Medicinal plants used by traditional medicine practitioners for the treatment of HIV/AIDS and related conditions in Uganda. J Ethnopharmacol. 2010;130(1):43–53. doi: 10.1016/j.jep.2010.04.004. [DOI] [PubMed] [Google Scholar]
- 40.Schultz F, Anywar G, Wack B, Quave CL, Garbe L-A. Ethnobotanical study of selected medicinal plants traditionally used in the rural Greater Mpigi region of Uganda. J Ethnopharmacol. 2020;256:112742. doi: 10.1016/j.jep.2020.112742. [DOI] [PubMed] [Google Scholar]
- 41.Namukobe J, et al. Traditional plants used for medicinal purposes by local communities around the Northern sector of Kibale National Park, Uganda. J Ethnopharmacol. 2011;136(1):236–245. doi: 10.1016/j.jep.2011.04.044. [DOI] [PubMed] [Google Scholar]
- 42.N. Uganda . National biodiversity strategy and action plan. Uganda: National Environment Management Authority; 2002. [Google Scholar]
- 43.UBO Statistics. Statistical abstract. Kampala: Uganda Bureau of Statistics, 2013.
- 44.Akwongo B, et al. Ethnobotanical study of medicinal plants utilized in the management of candidiasis in Northern Uganda. Trop Med Health. 2022;50(1):1–22. doi: 10.1186/s41182-022-00471-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Oryema C, Rutaro K, Oyet SW, Malinga GM. Ethnobotanical plants used in the management of symptoms of tuberculosis in rural Uganda. Trop Med Health. 2021;49(1):1–10. doi: 10.1186/s41182-021-00384-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Beck HE, Zimmermann NE, McVicar TR, Vergopolan N, Berg A, Wood EF. Present and future Köppen-Geiger climate classification maps at 1-km resolution. Sci Data. 2018;5(1):1–12. doi: 10.1038/sdata.2018.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Yamane T. Statistics: an introductory analysis-3. 1973.
- 48.Dudovskiy J. The ultimate guide to writing a dissertation in business studies: a step-by-step assistance, July 2016 edition. eBook J Mixed Methods Res. 2016;4(1):6–16. [Google Scholar]
- 49.Tongco MDC. Purposive sampling as a tool for informant selection. 2007.
- 50.Lewin C, Somekh B. Theory and methods in social research. Theory and methods in social research, pp. 1–368, 2011.
- 51.Salganik MJ, Heckathorn DD. Sampling and estimation in hidden populations using respondent-driven sampling. Sociol Methodol. 2004;34(1):193–240. [Google Scholar]
- 52.C. for D. C. and Prevention. Guidelines for the prevention and treatment of opportunistic Infections in HIV-infected adults and adolescents. MMWR. 2009; 58(4): 1–206.
- 53.C. for D. C. and Prevention. Guidelines for prevention and treatment of opportunistic infections in HIV-infected adults and adolescents: recommendations from CDC, the National Institutes of Health, and the HIV Medicine Association of the Infectious Diseases Society of America. MMWR Recomm Rep. 2009; 58(RR-4): 1. [PubMed]
- 54.Sokhanvar Z, Salehi K. Participatory action research to promote educational quality: a literature review. Res Rev J Educ Stud. 2018;4(2):23–34. [Google Scholar]
- 55.Minkler M. Using participatory action research to build healthy communities. Public Health Rep. 2000;115(2–3):191. doi: 10.1093/phr/115.2.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Hayward C, Simpson L, Wood L. Still left out in the cold: problematising participatory research and development. Sociol Ruralis. 2004;44(1):95–108. [Google Scholar]
- 57.Hildreth J, Hrabeta-Robinson E, Applequist W, Betz J, Miller J. Standard operating procedure for the collection and preparation of voucher plant specimens for use in the nutraceutical industry. Anal Bioanal Chem. 2007;389:13–17. doi: 10.1007/s00216-007-1405-x. [DOI] [PubMed] [Google Scholar]
- 58.Maden K. Plant collection and herbarium techniques. Our Nature. 2004;2(1):53–57. [Google Scholar]
- 59.Polhill RM, Nordal I, Kativu S, Poulsen AD. Flora of tropical east Africa. CRC Press; 2020. [Google Scholar]
- 60.Anderson R. Intuitive inquiry: inviting transformation and breakthrough insights in qualitative research. Qual Psychol. 2019;6(3):312. [Google Scholar]
- 61.Neuendorf KA. Content analysis and thematic analysis. in Advanced research methods for applied psychology, Routledge, 2018, pp. 211–223.
- 62.Krippendorff K. Content analysis: an introduction to its methodology 2nd Thousand Oaks. CA: Sage Publications; 2004. [Google Scholar]
- 63.Schwandt TA. The Sage dictionary of qualitative inquiry. Sage publications; 2014. [Google Scholar]
- 64.Ollerenshaw JA, Creswell JW. Narrative research: a comparison of two restorying data analysis approaches. Qual Inq. 2002;8(3):329–347. [Google Scholar]
- 65.Friedman J, Yaniv Z, Dafni A, Palewitch D. A preliminary classification of the healing potential of medicinal plants, based on a rational analysis of an ethnopharmacological field survey among Bedouins in the Negev Desert, Israel. J Ethnopharmacol. 1986;16(2–3):275–287. doi: 10.1016/0378-8741(86)90094-2. [DOI] [PubMed] [Google Scholar]
- 66.Weckmüller H, Barriocanal C, Maneja R, Boada M. Factors affecting traditional medicinal plant knowledge of the Waorani, Ecuador. Sustainability. 2019;11(16):4460. [Google Scholar]
- 67.Tugume P, et al. Ethnobotanical survey of medicinal plant species used by communities around Mabira Central Forest Reserve, Uganda. J Ethnobiol Ethnomed. 2016;12:1–28. doi: 10.1186/s13002-015-0077-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Panghal M, Arya V, Yadav S, Kumar S, Yadav JP. Indigenous knowledge of medicinal plants used by Saperas community of Khetawas, Jhajjar District, Haryana, India. J Ethnobiol Ethnomed. 2010;6:1–11. doi: 10.1186/1746-4269-6-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Cheikhyoussef A, Shapi M, Matengu K, Mu Ashekele H. Ethnobotanical study of indigenous knowledge on medicinal plant use by traditional healers in Oshikoto region, Namibia. J Ethnobiol Ethnomed. 2011;7:1–11. doi: 10.1186/1746-4269-7-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Alqethami A, Aldhebiani AY, Teixidor-Toneu I. Medicinal plants used in Jeddah, Saudi Arabia: a gender perspective. J Ethnopharmacol. 2020;257:112899. doi: 10.1016/j.jep.2020.112899. [DOI] [PubMed] [Google Scholar]
- 71.Singhal R. Medicinal plants and primary health care: the role of gender. J Health Manag. 2005;7(2):277–293. [Google Scholar]
- 72.dos Silva F, Ramos MA, Hanazaki N, de Albuquerque UP. Dynamics of traditional knowledge of medicinal plants in a rural community in the Brazilian semi-arid region. Rev Bras. 2011;21:382–391. [Google Scholar]
- 73.Pascual-Mendoza S, Saynes-Vásquez A, Pérez-Herrera A. Traditional knowledge of edible plants in an indigenous community in the Sierra Norte of Oaxaca, Mexico. Plant Biosyst-Int J Dealing All Aspects Plant Biol. 2022;156(2):515–527. [Google Scholar]
- 74.Merétika AHC, Peroni N, Hanazaki N. Local knowledge of medicinal plants in three artisanal fishing communities (Itapoá, Southern Brazil), according to gender, age, and urbanization. Acta Bot Brasilica. 2010;24:386–394. [Google Scholar]
- 75.Ouhaddou H, Boubaker H, Msanda F, El Mousadik A. An ethnobotanical study of medicinal plants of the Agadir Ida Ou Tanane province (southwest Morocco) J Appl Biosci. 2014;84:7707–7722. [Google Scholar]
- 76.Bruyere BL, Trimarco J, Lemungesi S. A comparison of traditional plant knowledge between students and herders in northern Kenya. J Ethnobiol Ethnomed. 2016;12(1):1–10. doi: 10.1186/s13002-016-0121-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Bukhori B, Hidayanti E, Situmorang DDB. Religious coping strategies for people with HIV/AIDS (PLWHA) Muslims in Indonesia: a qualitative study with a telling-the-stories. Heliyon. 2022;8(12):e12208. doi: 10.1016/j.heliyon.2022.e12208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Al-Obaidi JR, et al. Uncovering prospective role and applications of existing and new nutraceuticals from bacterial, fungal, algal and cyanobacterial, and plant sources. Sustainability. 2021;13(7):3671. [Google Scholar]
- 79.Wink M. Evolution of secondary metabolites in legumes (Fabaceae) S Afr J Bot. 2013;89:164–175. [Google Scholar]
- 80.Soković M, Skaltsa H, Ferreira ICFR. Bioactive phytochemicals in asteraceae: structure, function, and biological activity. Front Plant Sci. 2019;10:1464. doi: 10.3389/fpls.2019.01464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Yadav SA, Koshi FS. Phytochemicals from solanaceae family and their anticancer properties. in Medicinal Plants, IntechOpen, 2022.
- 82.Mugisha MK, Asiimwe S, Namutebi A, Borg-Karlson A-K, Kakudidi EK. Ethnobotanical study of indigenous knowledge on medicinal and nutritious plants used to manage opportunistic infections associated with HIV/AIDS in western Uganda. J Ethnopharmacol. 2014;155(1):194–202. doi: 10.1016/j.jep.2014.05.012. [DOI] [PubMed] [Google Scholar]
- 83.Bhattarai N, Karki M. Medicinal and aromatic plants: ethnobotany and conservation status. 2004.
- 84.Iwu MM. Ethnobotanical approach to pharmaceutical drug discovery: strengths and limitations. in Advances in Phytomedicine, Elsevier, 2002, pp. 309–320.
- 85.Okogun JI. Drug discovery through ethnobotany in Nigeria: some results. in Advances in Phytomedicine, Elsevier, 2002, pp. 145–154.
- 86.Saikia AP, Ryakala VK, Sharma P, Goswami P, Bora U. Ethnobotany of medicinal plants used by Assamese people for various skin ailments and cosmetics. J Ethnopharmacol. 2006;106(2):149–157. doi: 10.1016/j.jep.2005.11.033. [DOI] [PubMed] [Google Scholar]
- 87.Mesfin K, Tekle G, Tesfay T. Ethnobotanical study of traditional medicinal plants used by indigenous people of Gemad District, Northern Ethiopia. J Med Plants Stud. 2013;1(4).
- 88.Kim J, De Jesus O. Medication routes of administration. 2021. [PubMed]
- 89.Bachir RG, Benali M. Antibacterial activity of the essential oils from the leaves of Eucalyptus globulus against Escherichia coli and Staphylococcus aureus. Asian Pac J Trop Biomed. 2012;2(9):739–742. doi: 10.1016/S2221-1691(12)60220-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Ramos Alvarenga RF, Wan B, Inui T, Franzblau SG, Pauli GF, Jaki BU. Airborne antituberculosis activity of Eucalyptus citriodora essential oil. J Nat Prod. 2014;77(3):603–610. doi: 10.1021/np400872m. [DOI] [PubMed] [Google Scholar]
- 91.Shala AY, Gururani MA. Phytochemical properties and diverse beneficial roles of Eucalyptus globulus Labill.: a review. Horticulturae 2021, 7, 450.” s Note: MDPI stays neutral with regard to jurisdictional claims in published …, 2021.
- 92.Pal D, Mishra P, Sachan N, Ghosh AK. Biological activities and medicinal properties of Cajanus cajan (L) Millsp. J Adv Pharm Technol Res. 2011;2(4):207. doi: 10.4103/2231-4040.90874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Saxena K, et al. The alternative breeding approaches for improving yield gains and stress response in pigeonpea (Cajanus cajan) Plant Breeding. 2021;140(1):74–86. [Google Scholar]
- 94.Oke DG. Proximate and phytochemical analysis of Cajanus cajan (Pigeon pea) leaves. Chem Sci Trans. 2014;3(3):1172–1178. [Google Scholar]
- 95.Osei-Djarbeng SN, Kwarteng RO, Osei-Asante S, Owusu-Dapaah G. Comparative antimicrobial activities of ethanolic extracts of leaves, seed and stem bark of Mangifera indica (Mango) J Pharmacogn Phytochem. 2020;9(1):1240–1243. [Google Scholar]
- 96.Sanusi BM, Garba A, Muhammad A, Mohammed A, David O. Phytochemical screening and antimicrobial efficacy of aqueous and methanolic extract of Mangifera indica (mango stem bark). 2011.
- 97.Muronga M, et al. Three selected edible crops of the genus Momordica as potential sources of phytochemicals: biochemical, nutritional, and medicinal values. Front Pharmacol. 2021;12:625546. doi: 10.3389/fphar.2021.625546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Berto C, Maggi F, Nya PCB, Pettena A, Boschiero I, Dall’Acqua S. Phenolic constituents of Erigeron floribundus (Asteraceae), a Cameroonian medicinal plant. Nat Prod Commun. 2014;9(12):1934578X1400901207. [PubMed] [Google Scholar]
- 99.Bi FHT, Koné MW, Kouamé NF. Antifungal activity of Erigeron floribundus (Asteraceae) from Côte d’Ivoire, West Africa. Trop J Pharm Res. 2008;7(2):975–979. [Google Scholar]
- 100.Moungang LM et al. Antimicrobial potential of Erigeron floribundus extracts against some aquatic bacteria of sanitary importance: influence of pH. 2022.
- 101.Dall’Acqua S, et al. Chemical and biological characterization of Erigeron floribundus (Kunth) Sch. Bip extracts obtained by four isolation procedures. Anal Lett. 2020;53(17):2799–2811. [Google Scholar]
- 102.Almohaimeed HM, et al. Accelerating effect of Cucurbita pepo L. fruit extract on excisional wound healing in depressed rats is mediated through its anti-inflammatory and antioxidant effects. Nutrients. 2022;14(16):3336. doi: 10.3390/nu14163336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Ssegawa P, Kasenene JM. Medicinal plant diversity and uses in the Sango bay area, Southern Uganda. J Ethnopharmacol. 2007;113(3):521–540. doi: 10.1016/j.jep.2007.07.014. [DOI] [PubMed] [Google Scholar]
- 104.Maud KM, Savina A, Agnes N, Anna-Karin B-K, Peace M. Ethnobotanical study of nutri-medicinal plants used for the management of HIV/AIDS opportunistic ailments among the local communities of western Uganda. 2013. [DOI] [PubMed]
- 105.Chinsembu KC, Hedimbi M. An ethnobotanical survey of plants used to manage HIV/AIDS opportunistic infections in Katima Mulilo, Caprivi region, Namibia. J Ethnobiol Ethnomed. 2010;6(1):1–9. doi: 10.1186/1746-4269-6-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Tahir M, et al. The traditional use of wild edible plants in pastoral and agro-pastoral communities of Mieso District, eastern Ethiopia. Trop Med Health. 2023;51(1):1–15. doi: 10.1186/s41182-023-00505-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Njoroge G. Traditional medicinal plants in two urban areas in Kenya (Thika and Nairobi): diversity of traded species and conservation concerns. Ethnobot Res Appl. 2012;10:329–338. [Google Scholar]
- 108.Bussmann RW, Paniagua-Zambrana NY, Njoroge GN. Thunbergia alata Sims Acanthaceae. in Ethnobotany of the Mountain Regions of Africa, Springer, 2021, pp. 1033–1035.
- 109.Tumoro G, Maryo M. Determination of informant consensus factor and fidelity level of ethnomedicinal plants used in Misha Woreda, Hadiya Zone, Southern Ethiopia. Int J Biodivers Conserv. 2016;8(12):351–364. [Google Scholar]
- 110.Addo-Fordjour P, Anning AK, Belford EJD, Akonnor D. Diversity and conservation of medicinal plants in the Bomaa community of the Brong Ahafo region, Ghana. J Med Plants Res. 2008;2(9):226–233. [Google Scholar]
- 111.Mahomoodally MF. Traditional medicines in Africa: an appraisal of ten potent African medicinal plants. Evid-based Complement Alternat Med. 2013;2013:1. doi: 10.1155/2013/617459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Bakibinga DJ. Intellectual property rights in Uganda: reform and institutional management policy formulation. 2006.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data sets during and /or analysed during the current study are available from the corresponding author on reasonable request.


