Abstract
Background:
Sexually transmitted infections (STIs) are a major health issue, exacerbated by limited financial and infrastructural resources in developing countries.
Methods:
Prevalence of STIs was assessed in two urban centers of the Dominican Republic (DR) among populations at high risk for STIs: pregnant youth, men who have sex with men (MSM), trans women (TG), batey residents, female sex workers, and people living with human immunodeficiency virus (HIV). We conducted a cross-sectional survey and biological specimen collection to screen for Chlamydia trachomatis, Neisseria gonorrhea, Mycoplasma genitalium, Trichomonas vaginalis (trichomoniasis), Treponema pallidum (syphilis), HIV, hepatitis B and C, and human papillomavirus (HPV) among at-risk populations between 2015 and 2018. Ureaplasma urealyticum testing was also conducted even though it is not considered a STI. A non-probability community sample was recruited. Descriptive statistics examined the prevalence of STIs by population.
Results:
A total of 1991 subjects participated in the study. The median age was 26 years (range: 18–65). Most participants were female (65.3%), heterosexual (76.7%), and were not partnered (55.7%). Most of the participants reported unprotected vaginal sex in the last 6 months (54%); among MSM and TG almost half of the participants reported unprotected anal sex in the last 6 months and 17.6% reported drug use in the last 6 months. Almost half of the participants (49%) tested positive for one or more STIs. The most prevalent STI was Chlamydia trachomatis (12.8%), and human papillomavirus (11.9%). Among transgender women, 65.3% tested positive for an STI, 64.8% of female sex workers tested positive for an STI, and 53.8% of pregnant adolescents tested positive for an STI.
Conclusion:
There is a high prevalence of STIs among key and under resourced populations in the DR. Our findings highlight the need to conduct further research to optimize prevention and care strategies for structurally vulnerable and under resourced populations in the DR.
Keywords: key populations, prevalence of STIs, sexually transmitted infections
Introduction
The global burden of STIs among under-resourced populations remains high. 1 Chlamydia trachomatis (chlamydia), Neisseria gonorrhoeae (gonorrhea), Trichomonas vaginalis (trichomoniasis), and Treponema pallidum (syphilis) account for the majority of curable STIs globally. 2 Low- and middle-income countries bear a disproportionate part of this global burden, with the Latin American and Caribbean region accounting for the highest rate of STIs in the western hemisphere at 71 per 1000 population.2,3 To exacerbate the situation, STIs are likely underreported in low-income and rural communities in these settings, as low rates of screening, syndromic treatment guidelines, and gaps in healthcare coverage make detection challenging. 4
There is a paucity of data on the prevalence of sexually transmitted infections (STI) in the Dominican Republic (DR); however, data from human immunodeficiency virus (HIV) surveillance suggest that under-resourced populations are disproportionately impacted. 1 ‘Under-resourced populations’ is a term gradually replacing the word ‘vulnerable’ that refers to economically disadvantaged populations, stigmatized populations, racial and ethnic minorities, and sexual and/or gender minorities that experience greater barriers to social, economic, and healthcare resources and therefore, worse health outcomes than those with sufficient resources. 5
In 2019, the overall prevalence of HIV in the DR among adults age 15–49 was estimated at 0.9%, 6 lower than many other countries in the Caribbean. 6 However, key populations experience rates that are much higher, for example, immigrants of Haitian descent experience an HIV prevalence between 2.5% and 5%, men who have sex with men (MSM) (2.4–6.7%), transgender women (trans women) (17.3–28.0%), and female sex workers (FSW) (1.1–5.9%).6,7 Studies on the prevalence of other STIs such as human papillomavirus (HPV), genital herpes, hepatitis B, and other genital infections in the DR have been small, surveillance efforts are limited, and comprehensive STI screenings are not routinely available.
As STIs carry significant morbidity and can play an important role in HIV transmission and disease progression, 8 STI surveillance among under-resourced populations in the DR is urgently needed to inform program design and public health efforts aimed at improving education, prevention, detection, and treatment of STIs. IN addition to HIV, populations that experience higher burdens of STI risk generally, when compared to the general population, are pregnant youth, MSM, trans women, people living with HIV (PLWH), batey residents, and FSW.1,6,9,10 In the DR, bateyes are geographically and socioeconomically isolated current or former sugar cane industry worker settlements inhabited primarily by people of Haitian descent. Their residents experience higher incidence of HIV and other STIs. 11
The ability of under-resourced populations to access healthcare in the DR is also limited. For instance, MSM and trans women face structural barriers such as discrimination and stigma that either limit or prohibit healthcare seeking. 10 Stigma and discrimination as a structural barrier may also limit access to education, to the job market and consequently, financial concerns among these populations are substantial. 10 These and other structural factors such as immigration status and rural dwelling place (i.e. many bateyes are isolated communities with limited access to roads/transportation to healthcare centers, schools, and/or other basic services) influence ability to access care. 12 These structural barriers (discrimination, stigma, poverty, rural dwelling place) also affect PLWH and FSW and their ability to access healthcare. Furthermore, FSWs may consistently move from one place to another, limiting their stability, ability to build and maintain social support systems, and access/maintain connections to healthcare. 10
An additional public health concern in the DR is the teen pregnancy rate, as the DR has one of the highest teen pregnancy rates in Latin America and the Caribbean. 13 Most of adolescent pregnancies are reported to be unplanned or unwanted. 10 Lack of education on pregnancy prevention and limited availability to contraception methods that fit the community’s needs are potential contributors to these high adolescent pregnancy rates.13–15 Similarly, these sexually active adolescents are less likely to take measures to prevent STIs and are affected with high prevalence of STIs including Chlamydia, Gonorrhea, and Syphilis, among others.9,16,17 As an example, globally the prevalence of chlamydia among ages 13–49 is 3.8%, but in Latin America and the Caribbean, it is estimated to be as high as 11.2%. This may be even worse in the DR. As we found in a substudy from the same sample presented in this article, pregnant adolescents in the DR had a prevalence of rectal chlamydia of 23.2%.16,17
There are also significant policies acting as barriers to access to sexual education and contraception, causing delays to the roll out of effective sexual education programs despite the obvious need for these. 13 Equally important is the lack of education on STIs and prevention. All of these factors exacerbate youth’s and adolescents’ risk for acquiring STIs.
The primary aim of this study was to address gaps in knowledge of STI prevalence among six under-resourced populations in DR: pregnant youth, MSM, trans women, PLWH, batey residents, and FSW at two sites in large urban centers: LaRomana (LR) and Santo Domingo (SD). These populations were selected based on prior studies demonstrating high burden of STI risk in the DR 14,18–21; the locations were selected because of their large regional catchment areas that enabled recruitment from both urban and rural locations. A secondary aim was to assess factors associated with STIs and HIV risk among these populations.
Methods
Study design
This multisite, cross-sectional study explored the rates and risk factors of STIs among the six target populations in two locations in the DR through a comprehensive questionnaire and STI screenings. Participants attended follow-up visits to receive the results of their STI tests and receive treatment if needed.
Study settings
In LR, the study was conducted at one of the largest clinics providing HIV care and antiretroviral treatment to adults and children with HIV in the Eastern DR. This clinic also offers general health services and STI prevention, counseling, testing, and syndromic STI treatment to surrounding communities.
In SD, the study was conducted at a large, multispecialty clinic and research institute that provides treatment for skin conditions as well as STI/HIV infections, and is a national research expert with the under-resourced populations included in this study.
Recruitment
Data collection took place from May 2015 to March 2019. Recruitment targets were 400 participants from each population of interest across both sites, 200 per population per site (Table 1), with the exception of the trans women and MSM populations, where recruitment goals were a total of 125 trans women and 275 MSM. The total sample size was limited by the available funding and resources for this study.
Table 1.
Recruitment strategies per population.
| Populations recruited | Persons living with HIV | Transactional sex workers | Pregnant adolescents | Batey residents | Men who have sex with men | Transgender women |
|---|---|---|---|---|---|---|
| Recruitment strategy in SD and LR | Clinic-based: Every third patient coming to the clinics on recruitment days. | Venue-based: Mapped venues for transactional sex work. Venues selected (criteria used for selection in methods). All transactional sex workers in the chosen venues were eligible to participate. | Clinic-based: Every third patient coming to the clinics for their first pregnancy appointment on recruitment days. | Venue-based: Mapped the Bateyes, as described in the methods section. Bateyes selected (criteria used for selection in methods). All inhabitants in the chosen Bateyes were eligible to participate. | Venue-based: Mapped venues frequented by MSM. Venues selected (criteria used for selection in methods). All MSM in the chosen venues were eligible to participate. | Venue-based: Mapped venues frequented by transgender women. Selected venues (criteria used for selection in methods). All transactional sex workers in the chosen venues were eligible to participate. |
| Target population (total in SD and LR) | 400 | 400 | 400 | 400 | 275 | 125 |
| Personnel recruitment | Study team | Peer recruiters | Study team | Peer recruiters | Peer recruiters | Peer recruiters |
LR, LaRomana; SD, Santo Domingo.
Both the LR and SD sites recruited one population at a time, and both sites recruited the same population during the same time, in the following order: PLWH, FSW, pregnant youth, batey residents, and then MSM/trans women. Some of the study populations were recruited directly from the site clinics at LR and SD (PLWH, pregnant adolescents, a number of MSM in LR); other study populations (FSW, MSM, trans women, batey residents) were recruited from the surrounding communities, with the help of the outreach programs at each of the two sites where experienced recruiters from the populations worked with the study team. Recruitment strategies included venue-based and structured convenience sampling as described below (Table 1).
PLWH recruitment
Adults with 18–60 years of age living with HIV and receiving care in the HIV treatment centers at the LR and SD clinic sites were recruited. A convenience sample offered participation to every third PLWH patient attending the clinics in LR and SD from Monday to Friday.
FSW recruitment
Women with 18–60 years of age who had engaged in sexual activity in exchange for payment or gifts within the last 6 months and who self-identified as sex workers were eligible and recruited using venue-based sampling. Members of the research team at each site partnered with staff from LR and SD site local programs serving the FSW community to map the FSW population in LR and SD by venue and type of sex work establishment. In the DR, transactional sex, or sex in exchange for payments, goods, or services, occurs independently, solicited by FSW on streets and across multiple types of establishments: beer centers (centros cerveceros), bars/cabarets, restaurants, brothels, or night clubs. 22 Independent FSW do not work in a specific establishment and mainly solicit transactional sex on the streets. Different venues for transactional sex work may convey different levels of risk, so a structured sampling method was used to ensure proportionate representation from each venue type. The proportion of FSW that worked in each establishment or independently was determined based on estimated venue totals. The number of FSW to be recruited from each type of establishment or from the streets was calculated based on the type and size of venue, geographical location, and the target sample size (N = 200 per site).
Venues in LR (n = 30) and SD (n = 20) were randomly selected based on the above characteristics, and all FSW at selected venues were eligible to participate. A team of peer FSW (current or former) conducted all recruitment activities. Program staff recruited women on weekends and made reminder visits for interested participants until the target number of women, per establishment or from the streets, was reached. Following recruitment, all study procedures (informed consent, questionnaire completion, sample collection) took place at the study sites.
Pregnant youth recruitment
Pregnant youth 15–24 years of age with capacity to consent were eligible to participate in the study and were recruited from a clinic in LR that provides pre- and post-natal care to pregnant youth in a structured convenience sample. As we were aiming to recruit youth, the age range inclusion criteria of this population is lower than in the others. Pregnant youth were systematically recruited during normally scheduled clinic visits by inviting every third pregnant patient coming for a first clinic visit to be part of the study. In SD, pregnant adolescents were recruited from two of the largest maternity hospital clinics in the DR, utilizing a similar approach to the recruitment in LR. In the DR, pregnant youth 18 and younger are considered emancipated minors and able to provide consent for research participation.
Batey resident recruitment
Eligible batey residents were 18–60 years of age and reported living in a batey at the time of recruitment. Recruitment strategies varied by site because of population characteristics. In the LR region, bateyes are rural and geographically isolated, whereas in the area surrounding SD, bateyes have become part of the SD metropolitan area but remain structurally marginalized.
Bateyes were mapped by distance to larger urban centers, those at 30 km or less from LR or two other nearby towns and by the distance of the batey from the main road. Bateyes were then divided into three groups based on: closeness to the main road, closeness to urban centers, and number of people living in the batey. Seven bateyes were chosen from the three groups to arrive at a representative sample of bateyes in the area. All adult residents in the selected bateyes were eligible for participation in the study. Recruitment, data collection, and testing occurred on site in the bateyes.
Bateyes in SD were rural in the past. Currently, because the sugar cane industry has concentrated mainly on the Southeast part of DR, and as SD has grown in size, bateyes as such have nearly disappeared and are now areas that have become part of the city. Batey residents have similar sociodemographic characteristics from bateyes in LR. In SD, batey residents were recruited by Haitian–Dominican recruiters through community outreach. Participants were recruited from four bateyes in the SD Area.
MSM and trans women recruitment
Cisgender male participants 18–60 years of age who report having had intercourse with males (MSM), and participants 18–60 years of age who identified as trans women were recruited using venue-based sampling. Peer recruiters from, or familiar with, these communities at both sites identified recruitment venues frequented by both populations. These including internet cafes, places of worship, specific bars, parks, streets, establishments, or areas where trans women or MSM congregate. Sites with similar characteristics were categorized and sites for recruitment were randomly selected from each category. Venues frequented by MSM and trans women were mapped. The target number of MSM and trans women to be recruited from each site was calculated based on visits to these venues and the target sample size. All of those present during recruitment at the selected sites were eligible to participate. In LR, a small portion of the MSM participants were recruited from the men’s health program for MSM. For the men’s clinic in LR, a structured convenience sample invited every third patient coming to the men’s clinic to participate in the study.
Enrollment and study visits
Following recruitment, all participants underwent informed consent procedures and written consent was obtained as participants enrolled in the study. They then received counseling on STIs generally, including transmission and prevention as well as what to expect and/or do if any of their results are positive. Participants then completed a questionnaire with the help of the study team and STI testing as described below. Participants were then invited to return to the study site for follow-up visits to receive their test results and treatment if necessary, 2 weeks later. At each study visit, participants received an incentive congruent with site standards for research participations and guidelines established by the Dominican ethical review committee.
Questionnaire
The questionnaire included demographic characteristics (e.g. age, sex, gender, race, ethnicity, place of birth, sexual orientation, marital status, educational attainment, languages spoken), sexual and drug use behaviors [e.g. type(s) of sex engaged in, number of partners, frequency of condom use, rates of transactional sex], history of STIs (confirmed by testing and/or by history of syndromic treatment in medical records), preventive behaviors, and an assessment of symptoms suggestive of current STI syndromes. It also included questions on self-reported stigma and discrimination. The questionnaire was developed in Spanish by our bilingual (English/Spanish) study team and were then professionally translated to Haitian Creole and verified by bilingual (Spanish/Creole) staff at the LR and SD sites. Thus, questionnaires were available in Spanish or Creole and the study team collecting data had members fluent in both languages available during data collection.
Study staff administered questionnaires in a private space in participants’ preferred language on tablets with Qualtrics software. 23 After we conducted a small pilot study, it was determined that the most effective way to administer questionnaires was to read all questions and answer choices to the participants and record their responses. Trained interviewers in LR and SD then administered questionnaires in this fashion by. If a tablet could not be used, a paper questionnaire was administered by the interviewer in the same fashion, and data were later entered into Qualtrics.
Samples collected for STI testing/laboratory analysis
Blood samples
STI testing included blood sample collection for HIV (fourth-generation antibody/antigen assay), syphilis rapid plasma reagin with reflex/confirmatory (FTA), hepatitis B surface antigen (HBV) and hepatitis C antibodies (HCV) with reflex/confirmatory viral load testing (Table 2). Columbia University Irving Medical Center CALM laboratories processed blood samples for the study. Participants already known to be living with HIV and engaged in care at either the LR or SD site were not tested for HIV.
Table 2.
STI testing and study populations.
| STI Test/brand | Population | Sample | Positive result |
|---|---|---|---|
|
Neisseria gonorrhoeae and Chlamydia trachomatis
Oral and anal: Aptima Urine: SeeGene |
All | Urine/cervical/anal/oral* | Treatment/Test of cure |
|
Trichomonas vaginalis
SeeGene |
All | Urine/cervical | Treatment/Test of cure |
|
Mycoplasma genitalium
SeeGene |
All | Urine/cervical | Treatment when indicated |
|
Ureaplasma urealyticum
SeeGene |
All | Urine/cervical | Treatment when indicated |
| HPV (liquid based) Aptima |
Biological Females | Cervical (cytology or cervical swab) | Referral for management |
|
Cytology
Thin Prep Pap Test by Hologic |
Non-pregnant biological females | Cervical/ pap smear | Referral for management |
| HIV fourth generation Ab testing | All except PLWH | Blood | Referral for management |
| Hepatitis B and C ab with reflex VL | All | Blood | Referral for management |
| Syphilis reflex to FTA absorption test | All | Blood | Treatment/ referral for management |
FTA, fluorescent treponemal antibody; HPV, human papillomavirus; STI, Sexually transmitted infections; VL, viral load.
Please see more detailed descriptions of testing approaches in the methods section.
Oral, rectal urine and cervical samples
Oral and rectal swabs were collected to test for extra-genital Neisseria gonorrhoeae and Chlamydia trachomatis in all populations. Urine samples were collected for male participants and pregnant females to test for Neisseria gonorrhoeae and Chlamydia trachomatis, Mycoplasma genitalium, Ureaplasma urealyticum, and Trichomonas vaginalis. Cervical samples were collected from biological female participants to test for Neisseria gonorrhoeae, Chlamydia trachomatis, Mycoplasma genitalium, Ureaplasma urealyticum, and Trichomonas vaginalis (please see Table 2 for brands used for each test). Ureaplasma urealyticum is a bacterium that can be passed through sexual contact although it is not considered a classic STI because of its low degree of pathogenicity. Ureaplasma urealyticum, a commensal in the genital tract, has been recognized as contributors to urogenital infection. 24 Ureaplasma urealyticum is also associated with nongonococcal urethritis. 25
Cytology/pap smear, HPV testing
Except for pregnant females, all consenting females underwent cytology/pap smear testing and liquid-based HPV testing. For females who were pregnant or nonpregnant females who declined to have a pap smear testing, a cervical sample was collected to test for HPV. Cytology testing was not conducted on pregnant females (Table 2 for brands used for testing). Bioreference Laboratories, New Jersey, USA processed the study’s urine, cervical, vaginal, oral, and anal samples.
Sample preparation and shipment
Urine, oral, rectal, vaginal, and cervical samples were shipped to and processed at Bioreference Laboratories in New Jersey, USA in accordance with all regulations and specifications regarding shipping of biological specimens by those trained in these protocols and an appropriately accredited courier. Blood samples were shipped to and processed at Columbia University Irving Medical Center-CALM lab in New York City.
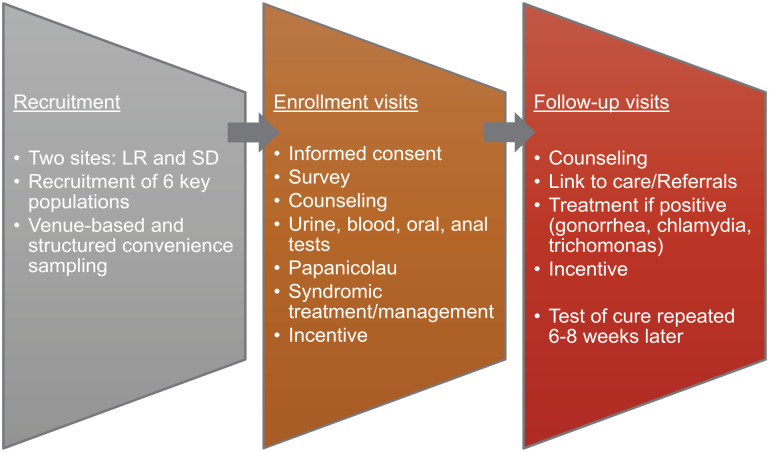
Follow-up visits
Participants were invited to return to the study site 2 weeks after participants’ baseline visit and STI testing date for results. If participants had a positive result from any of the tests conducted, they were informed and were provided appropriate treatment and counseling when indicated, following Dominican guidelines for STI treatment. Participants who tested positive for Neisseria gonorrhoeae, Chlamydia trachomatis, and/or Trichomonas vaginalis during the baseline visit came for their second visit and received treatment. Participants who tested positive for Ureaplasma urealyticus and Mycoplasma genitalium were evaluated by a physician and treated if they were symptomatic per Dominican Ministry of Health guidelines for STI treatment. Those participants who tested positive for syphilis were referred to the clinics for treatment and follow-up per DR guidelines for STI treatment. A third follow-up, test of cure visit was given to these participants who had tested positive for Neisseria gonorrhoeae, Chlamydia trachomatis, and/or Trichomonas vaginalis within 6–8 weeks to retest and confirm treatment and resolution (Figure 1). For positive results that did not have available or immediate treatment (hepatitis B, C, HIV), participants were referred to the clinics in LR and SD for further evaluation and follow-up, per DR guidelines for STI treatment.
Figure 1.
Study activities at each time point.
LR, LaRomana; SD, Santo Domingo.
Statistical analysis
We described the distributional properties of the data using standard descriptive statistics. This included the prevalence of each STI stratified by population. We evaluated bivariable associations between the social and demographic characteristics, sexual and drug use behaviors, STIs, and each population group using non-parametric tests (χ2, Wilcoxon–Mann–Whitney, Spearman Correlation, Cochran–Armitage). The statistical analysis was conducted using SPSS 27.0 (IBM Corp., Armonk, NY, USA). 26
Results
Social and demographic characteristics
A total of 1991 participants enrolled in the study. Table 3 summarizes the social and demographic characteristics of the sample. Overall, participants were rather young, with the median age of the full sample being 26 years of age (range 18–65) (Table 3). Participants were predominantly Dominican (93.3%) male or female (%) and were equally split between the LR and SD catchment areas. Participants had an average of 8.53 years of education [had completed middle school equivalent and 35.6% had formal employment at the time of enrollment. Most (58.9%) live on less than $134.11 USD per month. Of participants overall, 14.6% had ever experienced sexual violence, but when considering groups independently, 18.9% of PLWH and 25.7% of Trans women had experienced sexual violence. Overall, half of participants had participated in transactional sex at some point in their life. Among MSM and trans women, rates of participation in transactional sex were also high (91.4% and 94.1%, respectively] (Table 3).
Table 3.
Social and demographic characteristics of participants.
| Population | |||||||
|---|---|---|---|---|---|---|---|
| Total N = 1991 No. (%) |
PA
a
N = 408 No. (%) |
MSM
b
N = 278 No. (%) |
TW
c
N = 101 No. (%) |
PLWH
d
N = 424 No. (%) |
BR
e
N = 386 No. (%) |
FSW
f
N = 394 No. (%) |
|
| Social and demographic characteristics | |||||||
| Age (median, range) | 26 (18–65) | 18 (18–24) | 23 (18–60) | 25 (17–57) | 41 (18–65) | 28 (27–60) | 27 (17–57) |
| Sexual orientation n (%) | |||||||
| Heterosexual | 1527 (76.7) | 401 (98.3) | 0 (0.0) | 0 (0.0) | 398 (93.9) | 368 (95.3) | 360 (91.4) |
| Sexual and/or Gender Minority | 464 (23.3) | 7 (1.7) | 278 (100.0) | 101 (100.0) | 26 (6.1) | 4 (4.7) | 34 (8.6) |
| Country of birth n (%) | |||||||
| Dominican Republic | 1858 (93.3) | 406 (99.5) | 272 (97.9) | 101 (100.0) | 394 (92.9) | 299 (77.7) | 386 (98.2) |
| Other g | 131 (6.6) | 2 (0.5) | 6 (2.2) | 0 (0.0) | 30 (7.1) | 86 (22.3) | 7 (1.8) |
| Nearest city of residence n (%) | |||||||
| Santo Domingo | 994 (49.9) | 204 (50.0) | 123 (44.2) | 58 (57.4) | 223 (52.6) | 195 (50.5) | 191 (48.5) |
| La Romana | 997 (50.1) | 204 (50.0) | 155 (55.8) | 43 (42.6) | 201 (47.4) | 191 (49.5) | 203 (51.5) |
| Ever lived in a batey n (%) | |||||||
| No | 1398 (70.2) | 365 (89.7) | 248 (89.9) | 95 (94.1) | 326 (77.1) | 0 (0.0) | 360 (91.4) |
| Yes | 593 (29.8) | 42 (10.3) | 28 (10.1) | 6 (5.9) | 97 (22.9) | 386 (100.0) | 34 (8.6) |
| Primary language n (%) | |||||||
| Spanish | 1877 (94.3) | 407 (99.8) | 275 (98.9) | 101 (100.0) | 395 (93.2) | 309 (80.3) | 390 (99.0) |
| Other h | 113 (5.7) | 1 (0.2) | 3 (1.1) | 0 (0.0) | 29 (6.8) | 76 (19.7) | 4 (1.0) |
| Marital status n (%) | |||||||
| Not Partnered i | 1106 (55.7) | 101 (24.8) | 205 (73.7) | 80 (79.2) | 250 (59.0) | 173 (45.4) | 297 (75.8) |
| Partnered j | 878 (44.3) | 307 (75.2) | 73 (26.3) | 21 (20.8) | 174 (41.0) | 208 (54.6) | 95 (24.2) |
| Years of education (mean, SD) | 8.56 (3.632) | 9.22 (2.60) | 9.59 (2.87) | 9.48 (3.24) | 8.01 (4.10) | 7.12 (4.27) | 8.91 (3.39) |
| Student status n (%) | |||||||
| No | 1513 (76.0) | 252 (61.8) | 213 (76.6) | 67 (66.3) | 362 (85.4) | 271 (70.2) | 340 (86.3) |
| Yes | 467 (23.5) | 147 (36.0) | 62 (22.3) | 32 (31.7) | 60 (14.2) | 109 (28.2) | 51 (12.9) |
| Employment n (%) | |||||||
| Formal work | 706 (35.6) | 75 (18.5) | 121 (43.5) | 40 (39.6) | 164 (38.7) | 144 (37.9) | 162 (41.1) |
| Informal work k | 1277 (64.4) | 331 (81.5) | 157 (56.5) | 61 (60.4) | 260 (61.3) | 236 (62.1) | 232 (58.9) |
| Monthly income (United States Dollars) l n (%) | |||||||
| <$78.23 | 716 (38.9) | 259 (73.0) | 79 (28.6) | 32 (31.7) | 160 (40.7) | 159 (43.0) | 27 (7.8) |
| $78.24–$134.11 | 369 (20.1) | 47 (13.2) | 60 (21.7) | 19 (18.8) | 82 (20.9) | 83 (22.4) | 78 (22.6) |
| $134.12–$223.51 | 387 (21.0) | 32 (9.0) | 66 (23.9) | 29 (28.7) | 81 (20.6) | 68 (18.4) | 111 (32.2) |
| $223.54–$447.03 | 281 (15.3) | 13 (3.7) | 59 (21.4) | 17 (16.8) | 47 (12.0) | 55 (14.9) | 90 (26.1) |
| ⩾$447.04 | 87 (4.7) | 4 (1.1) | 12 (4.3) | 4 (4.0) | 23 (5.9) | 5 (1.4) | 39 (11.3) |
| Housing | |||||||
| Number of people that live in residence (median, range) | 3 (0–19) | 3 (1–13) | 4 (0–19) | 3 (1–9) | 4 (0–11) | 4 (1–15) | 3 (1–11) |
| Lived in temporary residence in last 6 months n (%) | |||||||
| No | 1228 (61.7) | 357 (87.5) | 92 (33.1) | 42 (41.6) | 336 (79.2) | 281 (72.8) | 120 (30.5) |
| Yes | 763 (38.3) | 51 (12.5) | 186 (66.9) | 59 (58.4) | 88 (20.8) | 105 (27.2) | 274 (69.5) |
| Lived in prison in last 6 months n (%) | |||||||
| No | 1781 (89.5) | 406 (99.5) | 145 (52.2) | 80 (79.2) | 415 (97.9) | 358 (92.7) | 377 (95.7) |
| Yes | 210 (10.5) | 2 (0.5) | 133 (47.8) | 21 (20.8) | 9 (2.1) | 28 (7.3) | 17 (4.3) |
| Lived in an abandoned building, car, street, park in last 6 months n (%) | |||||||
| No | 1513 (76) | 390 (95.6) | 179 (64.4) | 53 (52.5) | 401 (94.6) | 334 (86.5) | 156 (39.6) |
| Yes | 478 (24.0) | 18 (4.4) | 99 (35.6) | 48 (47.5) | 23 (5.4) | 52 (13.5) | 238 (60.4) |
| Healthcare use | |||||||
| Regular doctor visits n (%) | |||||||
| Yes | 956 (48.1) | 255 (62.7) | 31 (11.2) | 40 (39.6) | 423 (99.8) | 84 (21.9) | 197 (50.3) |
| No | 1035 (51.9) | 152 (37.3) | 247 (88.8) | 61 (60.4) | 1 (0.2) | 300 (78.1) | 195 (49.7) |
| Sexual behavior | |||||||
| Unprotected vaginal sex n (%) | |||||||
| Yes | 1076 (54.0) | 346 (84.8) | 166 (59.7) | 1 (1.0) | 129 (30.4) | 246 (63.7) | 188 (47.7) |
| No | 915 (46.0) | 62 (15.2) | 112 (40.3) | 100 (99.0) | 295 (69.6) | 140 (36.3) | 199 (52.3) |
| Unprotected anal sex n (%) | |||||||
| Yes | 212 (10.6) | 19 (4.7) | 75 (27.0) | 36 (35.6) | 15 (3.5) | 24 (6.2) | 43 (10.9) |
| No | 1779 (89.4) | 389 (95.3) | 203 (73.0) | 65 (64.4) | 409 (96.5) | 362 (93.8) | 351 (89.1) |
| Sexual violence n (%) | |||||||
| Yes | 291 (14.6) | 40 (9.8) | 19 (6.8) | 26 (25.7) | 80 (18.9) | 34 (8.8) | 92 (23.4) |
| No | 1700 (85.4) | 368 (90.2) | 259 (93.2) | 75 (74.3) | 344 (81.1) | 352 (91.2) | 302 (76.6) |
| Transactional sex n (%) | |||||||
| Yes | 997 (50.1) | 53 (13.0) | 254 (91.4) | 95 (94.1) | 122 (28.8) | 81 (21.0) | 394 (100.0) |
| No | 994 (49.9) | 355 (87.0) | 24 (8.6) | 6 (5.9) | 302 (71.2) | 305 (79.0) | 0 (0.0) |
| Age of sexual debut (median, range) | 15 (1–30) | 15 (2–20) | 14 (4–21) | 13 (5–22) | 16 (1–29) | 15 (6–30) | 15 (7–22) |
| Drug use | |||||||
| Marijuana n (%) | |||||||
| Yes | 290 (14.6) | 14 (3.4) | 123 (44.2) | 28 (27.7) | 8 (1.9) | 36 (9.3) | 81 (20.6) |
| No | 1701 (85.4) | 394 (96.6) | 155 (55.8) | 73 (72.3) | 416 (98.1) | 350 (90.7) | 313 (79.4) |
| Crack n (%) | |||||||
| Yes | 43 (2.2) | 1 (0.2) | 12 (4.3) | 9 (8.9) | 2 (0.5) | 1 (0.3) | 18 (4.6) |
| No | 1948 (97.8) | 407 (99.8) | 266 (95.7) | 92 (91.1) | 421 (99.5) | 385 (99.7) | 376 (95.4) |
| Cocaine n (%) | |||||||
| Yes | 101 (5.1) | 3 (0.7) | 21 (7.6) | 14 (13.9) | 10 (2.4) | 12 (3.1) | 41 (10.4) |
| No | 1890 (94.9) | 405 (99.3) | 257 (92.4) | 87 (86.1) | 414 (97.6) | 373 (96.9) | 353 (89.6) |
| Amphetamines n (%) | |||||||
| Yes | 4 (0.2) | 0 (0.0) | 1 (0.4) | 0 (0.0) | 0 (0.0) | 2 (0.5) | 1 (0.3) |
| No | 1987 (99.8) | 408 (100.0) | 277 (99.6) | 101 (100.0) | 424 (100.0) | 382 (99.5) | 393 (99.7) |
| Heroin n (%) | |||||||
| Yes | 4 (0.2) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 0 (0.0) | 2 (0.5) | 2 (0.5) |
| No | 1987 (99.8) | 408 (100.0) | 278 (100.0) | 101 (100.0) | 421 (100.0) | 383 (99.5) | 392 (99.5) |
PA, pregnant adolescent; bMSM, men who have sex with men; cTW, transgender woman; dPLWH, people living with HIV; eBR, batey resident; fFSW, female sex worker; gUSA and Haiti; hHaitian Creole and English; iSingle, divorced, separated, or widowed; jMarried and free union; kSelling items, money from spouse, temporary work, etc.; lAt the time of data collection, 1 US Dollar = 44.74 Dominican Pesos.
STI prevalence
Table 4 describes the prevalence of STIs among the key populations included in this study. Notably 24% of the full sample presented with Ureaplasma, 12.9% with HPV, and 12.8% with Chlamydia. Among FSW and Batey resident (BR), the prevalences of Ureaplasma were particularly high at 35.8% and 29.3%, respectively. FSW also had a high range of HPV at 21.4%. Other high prevalences included that 35.6% of transgender women (TWs) in our study were positive for HIV and 30.7% for syphilis. Beyond Chlamydia, PAs also had high rates of Ureaplasma (25.2%) and HPV (13.7%).
Table 4.
Presence of sexually transmitted infections of study participants stratified by population.
| Population | |||||||
|---|---|---|---|---|---|---|---|
| STI | Total N = 1991 No. (%) |
PA
a
N = 408 No. (%) |
MSM
b
N = 278 No. (%) |
TW
c
N = 101 No. (%) |
PLWH
d
N = 424 No. (%) |
BR
e
N = 386 No. (%) |
FSW
f
N = 394 No. (%) |
| None | 1006 (49.4) | 190 (46.2) | 185 (64.7) | 41 (34.7) | 239 (56.2) | 212 (52.7) | 139 (35.2) |
| Chlamydia | 254 (12.8) | 107 (26.2) | 40 (14.4) | 12 (11.9) | 10 (2.4) | 38 (9.8) | 47 (11.9) |
| Gonorrhea | 77 (3.9) | 18 (4.4) | 15 (5.4) | 10 (9.9) | 6 (1.4) | 6 (1.6) | 22 (5.6) |
| Hepatitis B | 56 (2.8) | 1 (0.2) | 6 (2.2) | 7 (6.9) | 11 (2.6) | 22 (5.7) | 9 (2.3) |
| Hepatitis C | 39 (2.0) | 7 (1.7) | 0 (0.0) | 0 (0.0) | 20 (4.7) | 7 (1.8) | 5 (1.3) |
| HIV | 506 (25.4) | 5 (1.2) | 17 (6.1) | 36 (35.6) | 424 (100.0) | 6 (1.6) | 18 (4.6) |
| HPV | 237 (11.9) | 56 (13.7) | 0 (0.0) | 0 (0.0) | 68 (16.0) | 27 (7.0) | 86 (21.8) |
| Mycoplasma | 46 (2.3) | 7 (1.7) | 14 (5.0) | 0 (0.0) | 5 (1.2) | 11 (2.8) | 9 (2.3) |
| Syphilis | 100 (5.0) | 6 (1.5) | 7 (2.5) | 31 (30.7) | 16 (3.8) | 10 (2.6) | 30 (7.6) |
| Trichomonas | 76 (3.8) | 17 (4.2) | 0 (0.0) | 0 (0.0) | 13 (3.1) | 23 (6.0) | 23 (5.8) |
| Ureaplasma | 492 (24.7) | 103 (25.2) | 24 (8.6) | 8 (7.9) | 103 (24.3) | 113 (29.3) | 141 (35.8) |
| Coinfection | 366 (17.9) | 221 (50.4) | 17 (5.9) | 30 (25.4) | 59 (13.9) | 69 (17.2) | 110 (27.8) |
HPV, human papilloma virus; STI, Sexually transmitted infections.
PA, pregnant adolescent; bMSM, men who have sex with men; cTW, transgender women; dPLWH, people living with HIV; eBR, batey resident; fFSW, female sex worker.
Discussion
This large cross-sectional study of six marginalized populations in the DR demonstrates a disproportionate burden of STIs across these populations and uncovered several structural risk factors for STI acquisition that vary by population. Participants were generally of low socioeconomic status, with almost two-thirds (64.4%) living below the poverty line, and a high prevalence of sexual risk and violence. The burden of HIV among the groups other than PLWH is elevated when compared to the estimated HIV prevalence of 0.9% among adults age 15–49 in the DR. 6 Studies on the prevalence of other STIs, such as human papilloma virus (HPV), hepatitis B, and other genital infections in this area, have been small and surveillance efforts are limited. The estimated prevalence of syphilis in the general population in the DR is 5% and the prevalence of HBV is 1.5%.27,28 Our findings, which represent one of the first comprehensive assessments of STI prevalence, including novel data on prevalence of Neisseria gonorrhoeae, Chlamydia trachomatis, and HPV, indicate that targeted programs, interventions, and policies are needed to address-specific STI risks amongst populations experiencing high burdens of poverty, violence, and mental health challenges.
Examining the data by population shows the variation in STI risk, with transgender women experiencing a strikingly high prevalence of HIV of 35.7%, compared to the 17.3–28.0% previously published. 29 Transgender women also had the highest rate of syphilis in our study (30% compared to the 13% published prevalence among MSM and trans women in DR) 30 and HBV rates (6.9% versus 0.65% in the general population in DR). 31 FSW were found to have high rates of HIV (4.6%), HPV (21.9%), and syphilis (7.6%). We also identified high prevalence of HIV (6.1%) among MSM. Concerningly, chlamydia was most common in pregnant youth, 9 but was also prevalent among MSM, TW, and FSW. The prevalence of HBV among BRs was high (5.7%), which may partially be a result of a lack of adult HBV vaccinations programs in the DR. There are no prior published data available for comparison for many of the STIs examined in this cohort, including Neisseria gonorrhoeae, Chlamydia trachomatis, Mycoplasma genitalium, Trichomonas vaginalis, and HPV.
Social determinants of health are linked to a lack of opportunity and resources to protect and maintain health, and likely play a large role in the inequities in STI prevalence found in our study populations. 32 An intersectional approach that considers the simultaneous and mutually constitutive effects of the multiple social categories of identity, difference, and disadvantage that individuals in each of these groups inhabit is needed. 28 Looking at the effects of gender, place of birth, neighborhood, race, class, or sexual identity independently is inadequate because these social positions are experienced simultaneously and their interplay exacerbates the conditions under which marginalized populations live. 33 Given the pervasive disadvantages affecting these populations,10,24,34 the results of our study suggest that there is a disproportionate burden of STIs across all of the study populations. While there are group differences in terms of disease burden, that is, the trans women cohort experienced the highest HIV prevalence, most of the groups in the study experienced higher burden of HIV and other STIs when compared with the general population. The intersection of identities that shape the experience of individuals in these groups, namely: poverty, low educational achievement, sexual and gender identity, stigmatization, place of birth, and gender affect health and healthcare access.
Many of the under-resourced populations included in our study experience structural violence and discrimination that affect their participation and contributions to the community at large.10,11,34 PLWH are often stigmatized and marginalized, potentially limiting their access to economic opportunities and quality healthcare. 35 Batey residents are the most economically disadvantaged of all the groups, living in precarious conditions, with limited access to most resources that would help improve their health and well-being, including education and healthcare.36,37 Batey residents are Haitian immigrants who are often undocumented, thus unprotected by the Labor Code in the DR and other legal provisions, resulting in the labor exploitation of thousands of Haitians who work in the construction sector, sugar cane plantations, and other agricultural crops. 11 A qualitative study conducted in LR with trans women and MSM found that trans women have difficulties completing their education and most drop out of school before completing high school, hindering their work opportunities. 10 This study also found that trans women experience many types of discrimination, including difficulties in accessing healthcare services and employment-based discrimination, which may limit their employment options to sex work and transactional sex. Many religious leaders and government authorities condone the violence and abuse these populations suffer. In a qualitative study conducted with female sex workers, independent female sex workers (soliciting sex work on the streets) are unprotected by law enforcement and are frequently victims of violence and abuse by clients. 34 A large number of female sex workers working in establishments are also at risk of violence; women reported having few legal protections and not having the resources or clout to assert their rights. 34
Limitations
This study has several limitations. A portion of the sample was recruited from clinics and hospitals and was comprised of healthcare-seeking participants who may not represent the broader population. Convenience sampling, which occurred for PLWH and pregnant youth, leads to limitations in generalizability; however, this was the most feasible strategy to recruit these important populations. The behavioral and demographic data were based on self-reported data, which may have led to recall and/or social desirability bias, particularly for sensitive questions related to stigmatized behaviors. Several populations sampled were recruited based on behavioral characteristics examined in the analyses. Therefore, differences across groups should be interpreted carefully. Additionally, we did not collect information on the clinical presentation of participants (i.e., symptomatic/asymptomatic) and were, therefore, unable to provide more clinical information of our participants along with our results. Regardless of limitations, this is study is the most recent, and largest, study on the epidemiology of STIs among key populations in the DR. The information we present will inform clinicians and researchers in the DR and similar settings in Latin America and the Caribbean to design programs and interventions that can begin to support these populations and ideally lead to better prevention of future infection.
Conclusion
This study confirmed suspicions of very high prevalence of STIs among key populations in the DR. This indicates that there is an urgent need for routine screening of STIs in key populations in the DR so that infections can be diagnosed and treated quickly, with the goal of reducing morbidity and mortality and preventing further transmission. It also emphasizes the need for widespread implementation of well-known HIV preventive strategies such as pre-exposure and post-exposure prophylaxis (PrEP and PEP). Understanding that the DR is a low- and middle-income country (LMIC), 38 focusing on STI prevention may be more cost-effective and efficient than other methods. More research is needed to understand how the social determinants of health and social factors such as stigma and discrimination toward key populations can be mitigated along with the risky sexual behaviors that they cause. Additionally, future studies should also determine the cost-effectiveness of widespread STI screening in the DR.
Acknowledgments
We would like to thank the Clínica de Familia La Romana staff, the Instituto Dermatológico de Cirugía y Piel staff, and the CALM laboratory at Columbia University Irving Medical Center. We would also like to thank Bioreference Laboratories for their incredibly generous donation of funds, effort, expertise, and time. In particular, we would like to acknowledge the participants in this study: without them, this study would not be possible.
Footnotes
ORCID iD: Silvia Amesty  https://orcid.org/0000-0001-5843-9655
https://orcid.org/0000-0001-5843-9655
Contributor Information
Silvia Amesty, Department of Medical Humanities and Ethics, Center for Family and Community Medicine, Mailman School of Public Health, Columbia University Irving Medical Center, 10 Ft. Washington Avenue, PH, New York, NY 10032-8300, USA.
Rafael Perez-Figueroa, Department of Urban-Global Health, Rutgers University School of Public Health, Piscataway, NJ, USA.
Samantha Stonbraker, University of Colorado College of Nursing, Anschutz Medical Campus, Aurora, CO, USA.
Mina Halpern, Clínica de Familia La Romana, La Romana, Dominican Republic.
Yeycy Donastorg, Instituto Dermatológico de Cirugía y Piel Humberto Borgart, Santo Domingo, Dominican Republic.
Martha Perez-Mencia, Instituto Dermatológico de Cirugía y Piel Humberto Borgart, Santo Domingo, Dominican Republic.
Flavia Lantigua, Instituto Dermatológico de Cirugía y Piel Humberto Borgart, Santo Domingo, Dominican Republic.
Leidy Soriano, Clínica de Familia La Romana, La Romana, Dominican Republic.
Pamela Baez-Caraballo, Clínica de Familia La Romana, La Romana, Dominican Republic.
Jeffrey Gilbert, BioReference Laboratories, Elmwood Park, NJ, USA.
Frank Buccini, BioReference Laboratories, Elmwood Park, NJ, USA.
James Sharp, BioReference Laboratories, Elmwood Park, NJ, USA.
Brian Hernandez, Joe R. and Teresa Lozano Long School of Medicine, University of Texas Health Science Center San Antonio, San Antonio, TX, USA.
Jonathan Gelfond, Joe R. and Teresa Lozano Long School of Medicine, University of Texas Health Science Center San Antonio, San Antonio, TX, USA.
Ethan Cardwell, Melbourne School of Global and Population Health, University of Melbourne, Melbourne, VIC, Australia.
Catherine Nicholas, University of Rochester Medical Center, Golisano Children’s Hospital, Rochester, NY, USA.
Kelsey A. Egan, Boston University School of Medicine, Boston, MA, USA
Angelina Gomes, Grossman School of Medicine, New York University, New York, NY, USA.
Elizabeth Van Dyke, Children’s Hospital Los Angeles, Los Angeles, CA, USA.
Stephen W. Nicholas, Children’s Global Health Fund, Mt Kisco, NY, USA
Marc Grodman, Vagelos College of Physicians and Surgeons, Columbia University, New York, NY, USA.
Barbara S. Taylor, Joe R. and Teresa Lozano Long School of Medicine, University of Texas Health Science Center San Antonio, San Antonio, TX, USA
Declarations
Ethics approval and consent to participate: This study was approved by the Consejo Nacional de Bioética en Salud (CONABIOS, Dominican National Institutional Review Board), protocol number 056–2014 and the Instituto Dermatológico y Cirugía de Piel Dr. Humberto Bogaert Díaz (IDCP) and Institutional Review Board at Columbia University, protocol #AAAN9650. Following recruitment, all participants underwent informed consent procedures and written consent was obtained as participants enrolled in the study.
Consent for publication: Not applicable.
Author contributions: Silvia Amesty: Conceptualization; Data curation; Formal analysis; Funding acquisition; Investigation; Methodology; Resources; Supervision; Writing – original draft; Writing – review & editing.
Rafael Perez-Figueroa: Data curation; Formal analysis; Methodology; Writing – original draft; Writing – review & editing.
Samantha Stonbraker: Investigation; Supervision; Writing – review & editing.
Mina Halpern: Methodology; Project administration; Supervision; Writing – review & editing.
Yeycy Donastorg: Investigation; Methodology; Project administration; Supervision; Writing – review & editing.
Martha Perez-Mencia: Data curation; Investigation; Methodology; Project administration; Writing – review & editing.
Flavia Lantigua: Data curation; Investigation; Methodology; Project administration; Supervision.
Leidy Soriano: Data curation; Investigation; Project administration.
Pamela Baez-Caraballo: Investigation; Project administration; Writing – review & editing.
Jeffrey Gilbert: Conceptualization; Data curation; Methodology; Supervision; Writing – review & editing.
Frank Buccini: Conceptualization; Data curation; Supervision; Writing – review & editing.
James Sharp: Data curation; Formal analysis; Software; Writing – review & editing.
Brian Hernandez: Data curation; Formal analysis; Writing – review & editing.
Jonathan Gelfond: Formal analysis; Writing – review & editing.
Ethan Cardwell: Formal analysis; Writing – review & editing.
Catherine Nicholas: Investigation; Methodology; Writing – review & editing.
Kelsey A. Egan: Investigation; Methodology; Project administration; Writing – review & editing.
Angelina Gomes: Investigation; Methodology; Supervision; Writing – review & editing.
Elizabeth Van Dyke: Investigation; Methodology; Supervision; Writing – review & editing.
Stephen W. Nicholas: Conceptualization; Funding acquisition; Writing – review & editing.
Marc Grodman: Conceptualization; Funding acquisition; Writing – review & editing.
Barbara S. Taylor: Conceptualization; Data curation; Formal analysis; Investigation; Methodology; Supervision; Writing – review & editing.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The study received private funds from Bioreference Laboratories. The author SS received funding from the National Institute of Nursing Research of the National Institutes of Health under award number K99/R00NR017829. The content is solely the responsibility of the authors and does not necessarily represent the official views of the institutions they represent.
The authors declare that there is no conflict of interest.
Availability of data and materials: Not applicable.
References
- 1. Montgomery MC, Alholm Z, Almonte A, et al. A cross-sectional evaluation of HIV testing practices among women in the rural Dominican Republic. BMC Womens Health 2020; 20: 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. World Health Organization. Global prevalence and incidence of selected curable sexually transmitted infections overview and estimates. Geneva: WHO, 2001. [Google Scholar]
- 3. Guilamo-Ramos V, Jaccard J, Lushin V, et al. HIV risk behavior among youth in the Dominican Republic: the role of alcohol and other drugs. J Int Assoc Physicians AIDS Care 2011; 10: 388–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. World Health Organization. Report on global sexually transmitted infection surveillance. Geneva: WHO, 2018. [Google Scholar]
- 5. Breslin E, Heaphy D, Dreyfus T, et al. Advancing health justice using Medicaid data: key lessons from Minnesota for the nation, https://academyhealth.org/sites/default/files/publication/%5Bfield_date%3Acustom%3AY%5D-%5Bfield_date%3Acustom%3Am%5D/advancinghealthjusticeusingmedicaiddata_jan2021.pdf (2021, accessed 10 June 2023).
- 6. Pepfar. Dominican Republic country operational plan (COP/ROP) 2019 strategic direction summary, https://www.state.gov/wp-content/uploads/2019/09/Dominican-Republic_COP19-Strategic-Directional-Summary_public.pdf (2019, accessed 22 November 2021).
- 7. PEPFAR. Strategic technical alignment for results (STAR). PROCESS Dominican Republic country operational plan COP 2017 strategic direction summary, https://www.state.gov/wp-content/uploads/2019/08/Dominican-Republic-1.pdf (2019, accessed 22 November 2021).
- 8. The National Academy of Sciences. Despite increasing rates of STIs, Federal Investment Has Been Flat; Report Recommends Approach to Address Structural Drivers of STIs While Expanding No-Cost Care Services, New Vaccines and Diagnostics, https://www.nationalacademies.org/news/2021/03/despite-increasing-rates-of-stis-federal-investment-has-been-flat-report-recommends-approach-to-address-structural-drivers-of-stis-while-expanding-no-cost-care-services-new-vaccines-and-diagnostics (2021, accessed 22 November 2021).
- 9. Bancalari P, Nicholas C, Halpern M, et al. High prevalence of rectal chlamydia among pregnant adolescents in La Romana, Dominican Republic, warrants extragenital STI testing. Int J STD AIDS 2022; 33: 31–37. [DOI] [PubMed] [Google Scholar]
- 10. Amesty S. Health needs of trans women population in La Romana, DR, (unpublished data), 2017. [Google Scholar]
- 11. López-Severino I, de Moya A. Migratory routes from Haiti to the Dominican Republic: Implications for the epidemic and the Human Rights of people living with HIV/AIDS. Revista Interamericana de Psicología/Interam J Psychol 2007; 41: 7–16. [Google Scholar]
- 12. Simmons D. Structural Violence as social practice: Haitian agricultural workers, anti-haitianism, and health in the Dominican Republic. Hum Organ 2010; 69: 10–18. [Google Scholar]
- 13. Human Rights Watch. Dominican republic: policies fuel teen pregnancy, https://www.hrw.org/news/2019/06/18/dominican-republic-policies-fuel-teen-pregnancy#:~:text=Public%20health%20data%20shows%2020.5,pregnancies%20are%20unplanned%20or%20unwanted (2019, accessed 10 October 2022).
- 14. Centro de Estudios Sociales y Demográficos (CESDEM). Encuesta Demográfica y de salud, República Dominicana, https://dominicanrepublic.unfpa.org/sites/default/files/pub-pdf/DRDHS2013-Final02-10-2013.pdf (2013, accessed 10 October 2022).
- 15. Fay CJ, Fay KE, Messina LA, et al. Factors related to subsequent adolescent pregnancy in the Dominican Republic. J Adolesc Fam Health 2020; 11: 1. [Google Scholar]
- 16. Rowley J, Vander Hoorn S, Korenromp E, et al. Chlamydia, gonorrhoea, trichomoniasis and syphilis: global prevalence and incidence estimates, 2016. Bull World Health Organ 2019; 97: 548–562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Joseph Davey DL, Shull HI, Billings JD, et al. Prevalence of curable sexually transmitted infections in pregnant women in low- and middle-income countries from 2010 to 2015: a systematic review. Sex Transm Dis 2016; 43: 450–458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Newman L, Rowley J, Vander Hoorn S, et al. Global estimates of the prevalence and incidence of four curable sexually transmitted infections in 2012 based on systematic review and Global Reporting. PLoS One 2015; 10: e0143304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Conavihsida (Consejo National para el VIH y sida). Plan Estrategico Nacional (PEN 2021-2024). Para la Respuesta a la Prevencion y el Control de las ITS, VIH y SIDA, en la Republica Dominicana 2021. [Google Scholar]
- 20. Conavihsida (Consejo National para el VIH y sida). Tercera encuentra de vigilancia de comportamiento con Vinculacion serológica en Poblaciones Clave. Republica Dominicana 2018, https://repositorio.conavihsida.gob.do/?page_id=12398 (2018, accessed January 2022).
- 21. Informe de resultados, Encuesta Nacional LGBTI 2020. AGOSTO 2021 SANTO DOMINGO, REPÚBLICA DOMINICANA, https://dominicanrepublic.un.org/sites/default/files/2021-08/Informe%20de%20Resultados%20Encuesta%20Nacional%20LGBTI%202020%20en%20la%20Republica%20Dominicana_2.pdf (2020, accessed 20 January 2021).
- 22. Richards SD, Stonbraker S, Halpern M, et al. Cervical cancer screening among transactional female sex workers in the Dominican Republic. Int J STD AIDS 2018; 29: 1204–1214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Qualtrics. Provo, UT, USA. [Google Scholar]
- 24. Liang YY, Zhai HY, Li ZJ, et al. Prevalence of Ureaplasma urealyticum, Chlamydia trachomatis, Neisseria gonorrhoeae and herpes simplex virus in Beijing, China. Epidemiol Infect 2018; 147: e59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Wetmore CM, Manhart LE, Lowens MS, et al. Ureaplasma urealyticum is associated with nongonococcal urethritis among men with fewer lifetime sexual partners: a case-control study. J Infect Dis 2011; 204: 1274–1282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. IBM Corp Released 2020. IBM SPSS Statistics for Windows, version 27.0. Armonk, NY: IBM Corp, 2020. [Google Scholar]
- 27. Miller WM. Análisis de la epidemia de VIH en la Republica Dominicana, http://conavihsida.gob.do/phocadownload/Informacion_y_Estadisticas/Analisis_e_Informes/2016_Analisis_Epi_VIH_RD_compressed.pdf (2016, accessed 27 December 2021).
- 28. Ministerio de Salud Püblica. Guía de Atención de las Hepatitis Virales y sus Comorbilidades asociadas al VIH, https://repositorio.msp.gob.do/bitstream/handle/123456789/1648/Guia-atencionhepatitis.pdf?sequence=1 (2018, accessed 27 December 2021).
- 29. Budhwani H, Hearld KR, Butame SA, et al. Transgender women in Dominican Republic: HIV, stigma, substances, and sex work. AIDS Patient Care STDS 2021; 35: 488–494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Brito MO, Hodge D, Donastorg Y, et al. Risk behaviours and prevalence of sexually transmitted infections and HIV in a group of Dominican gay men, other men who have sex with men and transgender women. BMJ Open 2015; 5: e007747–e007747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Coalition for Global Hepatitis elimination. A program of the task force for global health, https://www.globalhep.org/country-progress/dominican-republic (2021, accessed 22 November 2021).
- 32. Artiga S, Hinton E. Beyond Health Care: The Role of Social Determinants in Promoting Health and Health Equity, https://www.kff.org/racial-equity-and-health-policy/issue-brief/beyond-health-care-the-role-of-social-determinants-in-promoting-health-and-health-equity/ (2018, accessed 27 December 2021).
- 33. Crenshaw K. Mapping the margins: intersectionality, identity politics, and violence against women of color. Stanford Law Rev 1991; 43: 1241–1299. [Google Scholar]
- 34. Amesty S, Juniu S. Health needs of transactional sex workers in La Romana, DR, (unpublished data), 2018. [Google Scholar]
- 35. Valdez C, Barillas E, Cepeda I, et al. Diagnóstico de la situación de estigma y discriminación hacia poblaciones claves, en 15 Servicios de Atención Integral al VIH (SAI) priorizados, en República Dominicana. Presentado al proyecto del Fondo Mundial del Consejo Nacional del VIH y el SIDA (CONAVIHSIDA) en Santo Domingo, República Dominicana 2017. [Google Scholar]
- 36. Castel RZ. Trabajo, deuda y chantaje: Los braceros haitianos en los cañaverales de la República Dominicana. Latin American Research Review 2021; 56: 877–890. [Google Scholar]
- 37. Murphy Z, Cenziper D, Fitzgibbon W, et al. (eds). Bitter sugar, https://www.washingtonpost.com/business/interactive/2021/central-romana-tax-haven-south-dakota/ (2021, accessed 27 December 2021).
- 38. Wellcome. Low and middle income countries, https://wellcome.org/grant-funding/guidance/low-and-middle-income-countries (accessed 13 June 2022).