Abstract
Background and Purpose:
How the Area Deprivation Index (ADI) performs compared to other measures of socioeconomic status (SES) is unknown. The study purpose is to compare the ADI and other measures of SES in their ability to predict pain severity/interference.
Methods:
Four measures of SES were compared—ADI, income, education, and subjective social status (SSS).
Results:
Pain severity/interference correlated positively with ADI (r = .396/r = .33), and negatively with income (r = −.507/r = −.428) and education (r = −.271/r = −.102). Criterion scores of the pain severity model suggest income performs best (AIC = 428.29/BIC = 436.22), followed by ADI (AIC = 437.24/BIC = 445.17), with education performing least well (AIC = 446.35/BIC = 454.29). Similar results were seen for the pain interference model.
Conclusions:
Neighborhood-level factors warrant consideration along with individual-level factors when attempting to understand the impact of SES on chronic low back pain.
Keywords: social class, residence characteristics, social environment, chronic pain
Chronic pain has been recognized as a significant cause of suffering in the world (International Association for the Study of Pain, 2017), with an estimated 11% of American adults experiencing pain every day and an annual economic cost approaching $635 billion (National Center for Complementary and Integrative Health, 2018). Chronic pain is a major cause of disability (Institute of Medicine (US) Committee on Advancing Pain Research, Care, and Education, 2011), negatively affecting a person’s quality of life and daily activities of work and family (Dueñas et al., 2016). Low back pain is one of the most common painful conditions and is the leading cause of disability worldwide (GBD 2017 Disease and Injury Incidence and Prevalence Collaborators, 2018). It is consistently among the top five reasons for health-care visits ( M. L. Ferreira et al., 2010; Maher et al., 2017). Although many individuals with acute low back pain recover, about one in five progress to chronic low back pain (CLBP), lasting more than 3 months (Maher et al., 2017). The societal cost of CLBP is very high (Dutmer et al., 2019); it is associated with decreased quality of life (Husky et al., 2018), depressive symptoms (Pinheiro et al., 2016; Robertson et al., 2017), and decreased work productivity (Amirdelfan et al., 2018; Dutmer et al., 2019; Vlaeyen et al., 2018). To date, CLBP remains a major public health problem despite concerted efforts to address it.
Prior studies have documented the relationship between socioeconomic status (SES) and pain outcomes (Dorner et al., 2011; Dorner et al., 2018; Ikeda et al., 2019; Morgan et al., 2011; Riskowski, 2014; van Hecke et al., 2013). Generally, lower SES has been associated with virtually every aspect of poor chronic pain outcomes, including pain severity (Morgan et al., 2011), pain interference (Dorner et al., 2011), and decreased quality of life (Mielck et al., 2014). This trend toward worser pain outcomes in chronic pain has also be documented in CLBP (Hartvigsen et al., 2018; Ikeda et al., 2019; Jonsdottir et al., 2019). Specifically, higher rates of CLBP correlate with low SES and low educational attainment (Ikeda et al., 2019; Jonsdottir et al., 2019).
Investigators frequently use demographic variables to define SES, but the operational measurement of SES varies between studies. Individual level SES has been operationalized using objective and subjective factors (Jackman & Jackman, 1973). Frequently used objective measures of SES include education, income, occupation, and wealth. Research suggests that an individuals’ highest attained level of education is associated with income, wealth, living conditions, and health outcomes (Galobardes et al., 2007). Subjective social status (SSS) is the internally derived perception of one’s position in society (Jackman & Jackman, 1973) and predicts various health outcomes after accounting for objective measures of SES. However, it has been suggested that SSS may differ by sex, race, and ethnicity (Shaked et al., 2016; Wolff et al., 2010). Subjective social status is frequently measured using the MacArthur Scale of Subjective Social Status (or MacArthur Ladder) (W. Ferreira et al., 2018; Hoebel et al., 2017; Stanford University Department of Psychology, n.d.; Subramanyam et al., 2012; Zell et al., 2018). Prior work from our group shows that lower SSS correlates with more severe CLBP and increased pain interference (Aroke et al., 2020).
Besides personal (objective and subjective) measures of SES, the SES of an individuals’ environment also affect their living conditions and health (Ross & Mirowsky, 2008). Living in disadvantaged neighborhoods has been associated with poor health outcomes, including cardiovascular disease, obesity, diabetes, and chronic pain (Barber et al., 2016; Brennan & Turrell, 2012; Ulirsch et al., 2014). The Area Deprivation Index (ADI) is a well-validated instrument that measures neighborhood SES. Prior studies have used the ADI to examine the effects of neighborhood SES on several health outcomes (Chamberlain et al., 2020; Durfey et al., 2019; Kind et al., 2014; Kurani et al., 2020; Oates et al., 2019). For example, low neighborhood SES has been found to be associated with multimorbidity of chronic diseases (Chamberlain et al., 2020), diabetes, and blood pressure control (Durfey et al., 2019), and the presence of methicillin-resistant Staphylococcus aureus in pediatric patients with cystic fibrosis (Oates et al., 2019). The ADI assesses SES by measuring social deprivation and neighborhood disadvantage (Kind & Buckingham, 2018). Of relevance to this study, emerging evidence suggests that the SES of the neighborhood in which a person lives (i.e., the level of neighborhood disadvantage) is an important factor in pain outcomes (Green & Hart-Johnson, 2012; Maly & Vallerand, 2018). However, little is known about the utility of various measures of SES to assess the association of SES on chronic pain outcomes. While measures of SES are meant to measure the same overarching concept, they may not be interchangeable. The specific measure chosen to examine relationships between SES and back pain outcomes may influence its predictive ability (Fliesser et al., 2017). Informed by the social determinants of health, this paper will generally examine which measure of SES better predicts CLBP outcomes. The purpose of this study was to compare the ADI with other measures of SES in predicting pain severity and interference in adults with CLBP.
BACKGROUND AND CONCEPTUAL FRAMEWORK
An individual’s SES is an essential factor for understanding the personal and societal impact of chronic pain. Chronic pain occurrence and severity increases as objective measures of SES decreases (van Hecke et al., 2013). Other investigators have reported that low SES is linked to poor pain outcomes, while high SES is associated with better results in various pain conditions, including back pain (Dorner et al., 2011; Dorner et al., 2018; Grol-Prokopczyk, 2017; Gurung et al., 2015; Hoy et al., 2010; Janevic et al., 2017; Yu et al., 2020).
In 2010, the World Health Organization published the social determinants of health (SDOH) framework that systematically maps out determinants of health to structural intermediary and health system levels (Solar & Irwin, 2010). SDOH include the conditions in which people live, work, play, and grow. Many SDOH factors tend to cluster among individuals living in underprivileged circumstances and tend to interact with each other. As such, personal factors influence an individual’s health and the environment. In turn, their environment affects both personal factors (e.g., health behaviors) and health outcomes (Artiga & Hinton, 2018). The SDOH framework has been used to explore how various chronic conditions are affected by social (personal and environmental) factors. For instance, in 2000, hundreds of thousands of deaths were attributable to negative SDOH, including low education, individual-level poverty, and area-level poverty (Galea et al., 2011).
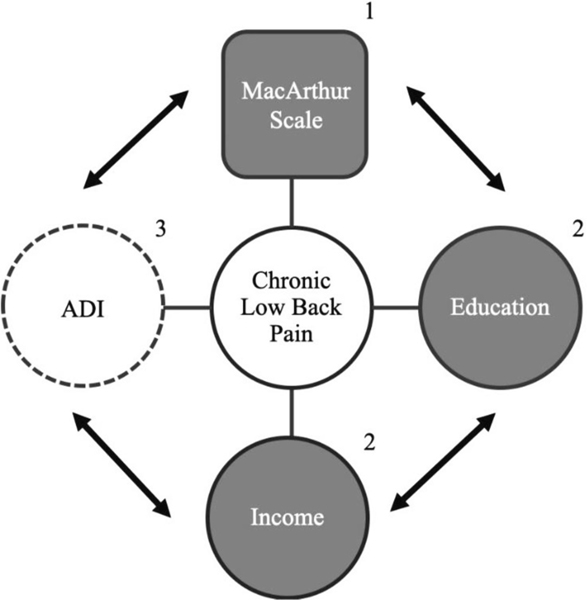
As depicted in Figure 1, an individual’s SES (objective and subjective measures of SES) influences CLBP outcomes. Conceptually, objective measures of SES include individual (income and education) and environmental (ADI) factors (Galobardes et al., 2007; Krieger et al., 1997; Ross & Mirowsky, 2008; Singh, 2003). These objective measures of SES influence and are influenced by SSS (MacArthur’s social status ladder).
Figure 1.
Relationship of objective and subjective SES measures and chronic low back pain.
Note. ADI = Area Deprivation Index; 1 = Individual-Level, Subjective; 2 = Individual-Level, Objective; 3 = Area-Level, Objective.
METHODS
Study Design and Participants
This methodological study employed a secondary analysis of data collected for an ongoing study: Examining Racial and Socioeconomic Disparities in Chronic Low Back Pain (ERASED) (R01MD010441). The goal of the ERASED study is to characterize racial differences in CLBP outcomes using a socioeconomic framework. Details of the ERASED study have previously been published (Aroke et al., 2020; Penn et al., 2020). Briefly, adults between the ages of 19 and 85 years were recruited. Respondents were included if they had nonspecific low back pain lasting more than 12 weeks. Exclusion criteria included the presence of other conditions that may confound result interpretation, such as pain conditions (e.g., ankylosing spondylitis, cancer pain, fibromyalgia), neurological diseases (e.g., Parkinson’s, epilepsy), or medical conditions (e.g., uncontrolled hypertension or poorly controlled diabetes). Participants included in the current study were recruited between November 2017 and November 2019. Only participants with data for all four measures (ADI, income, education and SSS) of SES being examined in this study were included for analysis. The Institutional Review Board at the University of Alabama at Birmingham reviewed and approved the ERASED study. All procedures were carried out following guidelines for the ethical conduct of research.
Measures
Demographic data included age, sex (male vs. female), and self-identified race (non-Hispanic Black, non-Hispanic White, and other). Measures were chosen to represent both area-level and individual SES, as well as objective and subjective SES. The goal was to capture a broad range of aspects of SES with which to compare the ADI. Income and education—measured as self-reported annual household income after taxes and the highest level of education, respectively—served as objective measures of SES at the individual level. Several valid and reliable instruments were used to assess neighborhood disadvantage, SSS, pain severity, and pain interference—the ADI, MacArthur Ladder of Subjective Social Status, and Brief Pain Inventory (BPI) respectively.
Area Deprivation Index.
The ADI is a validated objective measure of SES at the area level, using neighborhood disadvantage (Kind & Buckingham, 2018; Singh, 2003). Each participant’s address was linked to its respective census block, which is publicly available data. The ADI score is created using 17 census indicators of SES using domains such as income, housing, employment, and education (Kind & Buckingham, 2018; Kind et al., 2014). For each participants’ census block, we used the 2015 ADI v.2.0 (available at www.neighborhoodatlas.medicine.wisc.edu) that assigns a decile (i.e., 1–10) ADI score at the state level. For analysis, the Alabama state-level ADI decile scores were stratified into quintile rankings (i.e., 1–5), whereby the highest ranking “5” represented the greatest level of neighborhood disadvantage and “1” represented the lowest level of neighborhood disadvantage. The ADI has demonstrated high internal consistency (i.e., Cronbach’s alpha .94) (Singh, 2003; Singh et al., 2002; Singh & Siahpush, 2002) and a high test-retest reliability of 0.89 (Singh et al., 2002)
MacArthur Ladder of SSS.
The MacArthur ladder is a commonly used instrument that measures SSS at the individual level using a visual analog of a ladder (Adler & Stewart, 2007). Participants compare their self-perceived social status relative to others based on the following instructions:
Think of this ladder as representing where people stand in the United States. At the top of the ladder are the people who are the best off – those who have the most money, the most education and the most respected jobs. At the bottom are the people who are the worst off – who have the least money, least education, and the least respected jobs, or no job. The higher up you are on the ladder, the closer you are to people at the very top; the lower you are, the closer you are to the people at the very bottom. Please place a large “X” on the rung of the ladder for where you think you stand at this time in your life, relative to other people in the United States.
Participants ranked their position on the rungs of the ladder 0 to 10 corresponding with their subjective impression of their level of social status. The MacArthur ladder is a widely used instrument and has been translated into many languages (W. Ferreira et al., 2018). It has a moderate test-retest reliability (ρ = 0.62) (Operario et al., 2004), face validity, moderate concurrent validity (Kappa = 0.55–0.67) (W. Ferreira et al., 2018) and strong construct validity (Cundiff et al., 2013).
Brief Pain Inventory—Short Form.
The BPI is a valid and reliable self-administered 11-item questionnaire to assess clinical pain with an internal consistency reliability of greater than 0.85 (W. Ferreira et al., 2018; Majedi et al., 2017; Song et al., 2016; Tan et al., 2004). It measures two dimensions of pain: pain severity (intensity) and pain interference. The construct validity has previously been reported using factor analysis (K. A. Ferreira et al., 2011; Song et al., 2016; Tan et al., 2004). Prior work by our team indicates that BPI has internal consistency α = 0.94 in our sample (Aroke et al., 2020). Participants were asked to rate their pain at its worst, least, and average for the last 24 hours and at the time of the study at a scale from 0 to 10. The mean of these 4 items correspond to the BPI-pain severity score. Using the same type of 0 to 10 scales, participants rated separately how their pain interferes with their life in the following seven domains: (a) mood, (b) relations with other people, (c) enjoyment, (d) ability to concentrate, (e) appetite, (f) general activity, and (g) walking. Both pain severity and interference items are scored from 0 to 10.
DATA ANALYSIS
The ADI and other measures of SES were compared using Spearman correlations, coefficient of multiple determination partial R2, and goodness-of-fit tests Akaike information criterion (AIC) and Bayesian information criteria (BIC). The strength of the correlation coefficients was classified as follows: negligible (ρ < 0.10), weak (0.10–0.39), moderate (0.40–0.69), strong (0.70–0.89), and very strong (0.90–1.00) (Schober et al., 2018). Linear regression modeling was used to determine the relative contributions of ADI, income, education, and SSS to pain severity/interference. For comparison, partial R2 of .02 to .14 were considered as small, .15 to .34 as medium, and .35 or greater as large (Cohen, 1992). Also, lower AIC/BIC scores were considered better, and an internal consistency Cronbach’s ɑ = .7 to .95 was considered acceptable (Tavakol & Dennick, 2011). Test-retest reliability of the ADI was assessed using a Bland-Altman plot. A power analysis using G*Power 3.1 showed that a sample size of 104 eligible was sufficient to detect a weak correlation (ρ = 0.27) and a ΔR2 of .08 with 80% statistical power and alpha level of .05 (Faul et al., 2009). Data were analyzed using R version 4.0.2 statistical software.
RESULTS
Pain severity and interference data were available for 129 participants. Of these, data for all variables of interest were available for 104 participants with CLBP, who were included in the final analyses. Participants were on average, 45 years old and tended to be women (58.7%), and African American (56.7%). The median household income was $35K–39.9K, falling below the Alabama State median income ($48K) and national median income level ($60K) (www.census.gov/quickfacts). Approximately 74% of participants received some college education, graduated from college, or attended graduate school. On average, participants rated their social status as 5.1 (SD = ±2.0) out of 10. ADI scores were available for 97% of participants representing 85 census block groups, across five counties (Jefferson, Shelby, Bibb, Walker, and Winston) in Central Alabama. Table 1 summarizes the characteristics of participants included in the study.
TABLE 1.
Characteristics of Participants (N = 104)
| Characteristic | Mean (SD) or % (n) |
|---|---|
|
| |
| Age in years | 45 ± 13 |
| Sex | |
| Female | 58.7% (61) |
| Male | 41.3% (43) |
| Ethnicity | |
| African American | 56.7% (59) |
| Caucasian | 41.3% (43) |
| Unknown | 1.9% (2) |
| Area Deprivation Index (1–5) | 2.7 (1.5) |
| Income (Median) | $35K–$39.9K |
| Education | |
| Partial High School | 3.8% (4) |
| High School Graduate | 22.1% (23) |
| Partial College | 31.7% (33) |
| College Graduate | 24% (25) |
| Graduate/Professional School | 18.2% (19) |
Correlations of Objective and SSS
As depicted in Table 2, there was a statistically significant moderate negative relationship between the objective measures of social status (income and education) and the ADI, ρ = −0.57 and −0.45, respectively. However, ADI and SSS were not significantly correlated (p = .335). In addition, both pain severity and pain interference negatively correlated with individual measures of social status and positively correlated with ADI. In contrary, the relationship between SSS and pain severity was not statistically significant (p = .11). Similarly, the relationship between pain interference and both education and SSS were not statistically significant
TABLE 2.
Spearman Correlations Between Measures
| 1. | 2. | 3. | 4. | 5. | 6. | |
|---|---|---|---|---|---|---|
|
| ||||||
| 1. ADI | – | |||||
| 2. Income | −.566** | – | ||||
| 3. Education | −.449** | .455** | – | |||
| 4. SSS | −.096 | .311** | .181 | – | ||
| 5. Pain Severity | .396** | −.507** | −.271* | −.16 | – | |
| 6. Pain Interference | .33** | −.428** | −.102 | −.152 | .627** | – |
Note. ADI = Area Deprivation Index; SSS = Subjective Social Status.
p < .05.
p ≤ .001.
Comparing Predictors of Pain Severity and Interference
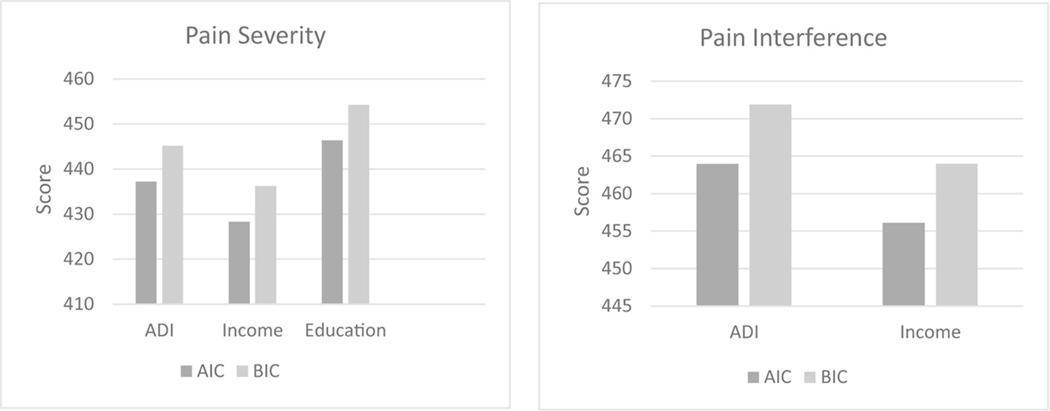
The average pain severity and interference scores were 5.1 (SD ± 2.1) and 4.1 (SD ± 2.3), respectively. The objective measures that showed significant correlations with pain outcomes were fitted into different linear models to compare their ability to predict pain severity/interference (Figure 2). For pain severity, the model’s goodness-of-fit AIC and BIC suggested that income outperforms other measures of objective SES (AIC = 428.29/ BIC = 436.22), followed by ADI (AIC = 437.24/BIC = 445.17), with education performing least well (AIC = 446.35/BIC = 454.29). Likewise, for pain interference, AIC and BIC suggested that income performs best (AIC = 456.08/BIC = 464.01), followed closely by ADI (AIC = 4 63.96/BIC = 471.90).
Figure 2.
AIC and BIC scores for SES pain severity and pain interference with SES measures.
Assessment of Independent Contribution to Pain Outcomes
We fitted each objective measure of SES into a multiple regression model to assess its independent contribution to pain outcomes assessed. Results of the model predicting pain severity indicated that income made the largest contribution (partial R2 = .098), followed by ADI (partial R2 = .021). Similar results were obtained from the model predicting pain interference. The model revealed that while the ADI (partial R2 = .029) makes a small independent contribution, the contribution of income (partial R2 = .100) was greatest. Education contributed a small amount to the interference model (partial R2 = .026) and an insignificant amount to the pain severity model (partial R2 = .0003).
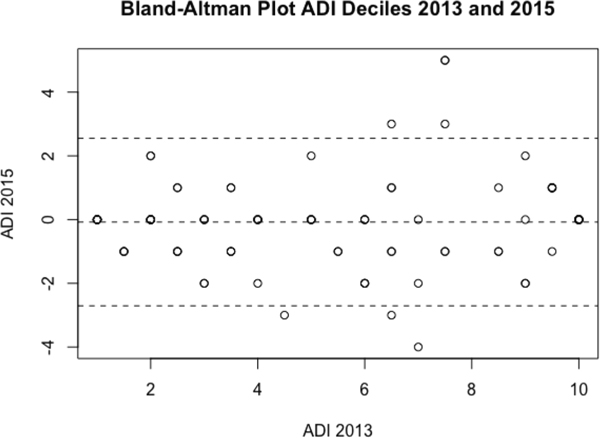
Reliability of ADI and BPI
We used ADI decile scores from 2013 and 2015 to determine its test-retest reliability. The test-retest reliability of the ADI was excellent with an intraclass correlation of 0.92 (p < .001; 95% CI: 0.89–0.94). Figure 3 displays the Bland-Altman plot for the differences between the 2013 and 2015 ADI decile scores. Most differences were clustered within two deciles, which are acceptable limits of agreement (Polit & Beck, 2017). Internal consistency of the BPI in our sample was high with a Cronbach’s alpha of 0.95 (95% CI: 0.93–0.96).
Figure 3.
Degree of agreement between ADI Deciles for 2013 and 2015.
DISCUSSION
Our study offers preliminary evidence that the ADI is an effective measure of SES and adds to the growing body of literature indicating neighborhood disadvantage is an important predictor of pain outcomes. In direct comparisons between objective and subjective measures of SES, our results showed that income performed best at predicting pain severity and interference. However, the ADI outperformed education and SSS, which are other more well-established measures of SES (Galobardes et al., 2007; Krieger et al., 1997; Singh-Manoux et al., 2005). Our findings are consistent with prior studies, which found lower neighborhood SES is associated with poorer pain outcomes. Living in a disadvantaged neighborhood is associated with increased musculoskeletal pain and increased pain interference with daily activities following motor vehicle accident (Ulirsch et al., 2014). Similarly, greater noninflammatory musculoskeletal pain interference has been reported among individuals living in low SES neighborhoods in Norway (Brekke et al., 2002). Likewise, Fuentes et al. (2007) found that high neighborhood SES is associated with lower chronic pain in adults over age 50 years. However, other investigators have shown that while low neighborhood SES is associated with new-onset chronic widespread pain, that relationship is not robust and does not hold up once psychological comorbidities are considered (Davies et al., 2009). This discrepancy may be related to the fact that the neighborhood SES measure used by Davies and colleagues (2009) did not account for income and poverty, which contribute to ADI scores. To our knowledge, this is the first study to offer evidence that suggest that neighborhood disadvantage correlates with pain severity and pain interference in CLBP. Thus, for adults with CLBP, ADI may be a good predictor of pain outcomes.
Area-Level Versus Individual-Level Measures of SES
Our findings suggest that there is a moderate relationship between individual-level versus area-level measures of SES. Also, the area-level measure of SES (i.e., ADI) performs better than some individual-level measures of SES in predicting pain severity and pain interference. The strength of the relationship in our study is slightly higher than previously reported. Buajitti and colleagues (2020) reported a low correlation between individual and area-level SES among participants in the population-based Canadian Community Health Survey. Diez-Roux et al. (2001) found weak correlations between individual and area-level measures of income in an examination of three U.S.-based cohorts. The differences in the strength of the relationship between individual and area-level measures may be related to the fact that various measures capture different dimensions of SES. Also, it may reflect the relative homogeneity of ADI in our study sample.
While the relationships between ADI and income, as well as the ADI and education were significant, the relationship between the ADI and SSS were not. Thus, supporting the view that area- and individual-level measures of SES are related and multidimensional, but not interchangeable (Galobardes et al., 2007; Geyer et al., 2006; Krieger et al., 1997). It is possible that an individual’s neighborhood may be a reflection of their income and education, which does not necessarily reflect the individual’s perception of their SES. Unfortunately, this complex relationship is under-explored among individuals living with CLBP. Fliesser and colleagues (2017), examined the relationship of chronic back pain outcomes with three different singular, individual-level measures of SES and a multidimensional, individual-level index. While the multidimensional measure predicted pain intensity best, singular measures were better at predicting disability. They concluded that the predictive ability of SES on back pain is variable based on the SES measure that is chosen (Fliesser et al., 2017). Other investigators have argued that it may not be “useful or theoretically compelling to search for a single ‘best’ indicator” of SES because different measures of SES capture different dimensions of the social hierarchy (Galobardes et al., 2007). Therefore, different SES indicators may measure different ways SES impacts health (Galobardes et al., 2007). Ultimately, our results support the inclusion of area-level indicators in addition to individual-level measures to better understand the impact of SES on CLBP.
Objective Versus Subjective Measures of SES
In our study, objective measures of SES significantly predicted pain severity and interference, while our subjective SES measure did not. These findings support the fact that objective and subjective measures of SES are not interchangeable (Shaked et al., 2016). Other studies have reported that objective measures of SES are associated with back pain outcomes. Using the objective measures income and education, Dorner et al. (2011) found lower SES to be associated with greater disability from pain. Similarly, a review by Hoy et al. (2010) found that low educational status is a common risk factor for low back pain. Jonsdottir et al. (2019) report an association between low SES and low educational attainment as risk factors for chronic back pain. Similarly, in her study using nationally representative data from the United States, Riskowski (2014) found increased odds of back pain for both men and women with the lowest SES.
Limitations
This study has a number of limitations, including the modest number of participants, homogeneity of participants neighborhood, and idiosyncratic relationship between predictors and pain outcomes. Due to missing data on full address and income, approximately 80% of the original 129 participants were included in the final analysis. While there is no set cutoff for missing data, 5% is considered inconsequential and over 10% may be considered problematic for inference (Dong & Peng, 2013). Also, most of our participants resided in the Birmingham-Hoover, Alabama metropolitan area. The Birmingham-Hoover metropolitan area covers over 5,200 square miles and is the most populous area of the state of Alabama, with an estimated population of over 1.1 million (U.S. Census Bureau, 2018). Future studies should include participants from other geographic areas because measuring SES involves assessment of a social hierarchy, which may vary from one geographic location to another (Jackman & Jackman, 1973; Singh-Manoux et al., 2005). The use of the ADI that relies on census block data is a major limitation. This is because the reliability of the ADI score depends on the accuracy of the census data (Messer & Kaufman, 2006). However, multiple indicators are preferred when measuring SES (Messer & Kaufman, 2006). Thus, the breadth of the census data could be a strength because the ADI uses 17 indicators to assess neighborhood SES. Finally, the cross-sectional approach limited our ability to determine how long the participants had lived in the disadvantaged neighborhood.
RELEVANCE TO NURSING PRACTICE AND RESEARCH
Our findings have important implications for nursing practice and research. These findings suggest that research on SES and pain that encompasses both area-level and individual-level factors will provide valuable perspective on pain outcomes. Considering that SES may play a role in the development of pain and musculoskeletal pain severity (Maly & Vallerand, 2018; Riskowski, 2014), our findings support the adoption of neighborhood disadvantage screening for patients with, or at risk for developing chronic pain. Since the ADI allows for assessment of neighborhood disadvantage using readily available data, it may be a valuable tool in efforts to address chronic pain disparities, especially those based on geographically delineated SES inequality. An understanding of the level of neighborhood disadvantage of individuals and groups may be useful for the planning of patient care because it can help identify patients who would benefit from interventions that address area-level SDOH. Regarding research implications, nurse scientists should investigate the effect of neighborhood on chronic pain outcomes using a longitudinal approach. Also, future studies should compare individual versus area level interventions in addressing SES disparities in chronic pain.
CONCLUSION
Individual and area factors correlate with CLBP outcomes such that lower income, lower education, and living in a disadvantaged neighborhood predicts CLBP severity and interference. To better understand the impact of SES on CLBP outcomes, both area-level and individual-level aspects of SES should be considered. Results generally fit with previously established findings that different measures of SES are related but not interchangeable. Among SES measures, income appears to be the strongest predictors of CLBP outcomes.
Funding.
This study was funded in part by the National Institute on Minority Health and Health Disparities grant R01MD010441, National Institute of Arthritis and Musculoskeletal and Skin Diseases grant R01AR079178, as well as the American Association of Nurse Anesthetists grant 2018-FS-4.
Footnotes
Disclosure. The authors have no relevant financial interest or affiliations with any commercial interests related to the subjects discussed within this article.
REFERENCES
- Adler NE, & Stewart J. (2007). The MacArthur Scale of subjective social status. Retrieved August 8, 2019, from https://macses.ucsf.edu/research/psychosocial/subjective.php
- Amirdelfan K, Yu C, Doust MW, Gliner BE, Morgan DM, Kapural L, Vallejo R, Sitzman BT, Yearwood TL, Bundschu R, Yang T, Benyamin R, Burgher AH, Brooks ES, Powell AA, & Subbaroyan J. (2018). Long-term quality of life improvement for chronic intractable back and leg pain patients using spinal cord stimulation: 12-month results from the SENZA-RCT. Quality of Life Research, 27(8), 2035–2044. 10.1007/s11136-018-1890-8 [DOI] [PubMed] [Google Scholar]
- Aroke EN, Jackson P, Overstreet DS, Penn TM, Rumble DD, Kehrer CV, Michl AN, Hasan FN, Sims AM, Quinn T, Long DL, & Goodin BR. (2020). Race, social status, and depressive symptoms: A moderated mediation analysis of chronic low back pain interference and severity. The Clinical Journal of Pain, 36, 658–666. 10.1097/AJP.0000000000000849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Artiga S, & Hinton E. (2018). Beyond health care: The role of social determinants in promoting health and health equity (Issue brief). Henry J: Kaiser Family Foundation. http://files.kff.org/attachment/issue-brief-beyond-health-care [Google Scholar]
- Barber S, Hickson DA, Wang X, Sims M, Nelson C, & Diez-Roux AV. (2016). Neighborhood disadvantage, poor social conditions, and cardiovascular disease incidence among African American adults in the Jackson Heart Study. American Journal of Public Health, 106(12), 2219–2226. 10.2105/AJPH.2016.303471 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brekke M, Hjortdahl P, & Kvien TK. (2002). Severity of musculoskeletal pain: Relations to socio-economic inequality. Social Science & Medicine, 54(2), 221–228. 10.1016/s0277-9536(01)00018-1 [DOI] [PubMed] [Google Scholar]
- Brennan SL, & Turrell G. (2012). Neighborhood disadvantage, individual-level socio-economic position, and self-reported chronic arthritis: A cross-sectional multilevel study. Arthritis Care & Research, 64(5), 721–728. 10.1002/acr.21590 [DOI] [PubMed] [Google Scholar]
- Buajitti E, Chiodo S, & Rosella LC. (2020). Agreement between area- and individual-level income measures in a population-based cohort: Implications for population health research. SSM - Population Health, 10, 1–8. 10.1016/j.ssmph.2020.100553 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chamberlain AM, Finney Rutten LJ, Wilson PM, Fan C, Boyd CM, Jacobson DJ, Rocca WA, & St Sauver JL. (2020). Neighborhood socioeconomic disadvantage is associated with multimorbidity in a geographically-defined community. BMC Public Health, 20(1), 1–10. 10.1186/s12889-019-8123-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. (1992). A power primer. Psychological Bulletin, 112(1), 155–159. 10.1037/0033-2909.112.1.155 [DOI] [PubMed] [Google Scholar]
- Cundiff JM, Smith TW, Uchino BN, & Berg CA. (2013). Subjective social status: Construct validity and associations with psychosocial vulnerability and self-rated health. International Journal of Behavioral Medicine, 20(1), 148–158. 10.1007/s12529-011-9206-1 [DOI] [PubMed] [Google Scholar]
- Davies KA, Silman AJ, Macfarlane GJ, Nicholl BI, Dickens C, Morriss R, Ray D, & McBeth J. (2009). The association between neighbourhood socio-economic status and the onset of chronic widespread pain: Results from the EPIFUND study. European Journal of Pain, 13(6), 635–640. 10.1016/j.ejpain.2008.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diez-Roux AV, Kiefe CI, Jacobs DR, Haan M, Jackson SA, Nieto FJ, Paton CC, & Schulz R. (2001). Area characteristics and individual-level socioeconomic position indicators in three population-based epidemiologic studies. Annals of Epidemiology, 11(6), 395–405. 10.1016/s1047-2797(01)00221-6 [DOI] [PubMed] [Google Scholar]
- Dong Y, & Peng C-YJ. (2013). Principled missing data methods for researchers. SpringerPlus, 2(1), 1–17. 10.1186/2193-1801-2-222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dorner TE, Muckenhuber J, Stronegger WJ, Ràsky E, Gustorff B, & Freidl W. (2011). The impact of socio-economic status on pain and the perception of disability due to pain. European Journal of Pain, 15(1), 103–109. 10.1016/j.ejpain.2010.05.013 [DOI] [PubMed] [Google Scholar]
- Dorner TE, Stein KV, Hahne J, Wepner F, Friedrich M, & Mittendorfer-Rutz E. (2018). How are socio-demographic and psycho-social factors associated with the prevalence and chronicity of severe pain in 14different body sites? A cross-sectional population-based survey. Wiener Klinische Wochenschrift, 130(1–2), 14–22. 10.1007/s00508-017-1223-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dueñas M, Ojeda B, Salazar A, Mico JA, & Failde I. (2016). A review of chronic pain impact on patients, their social environment and the health care system. Journal of Pain Research, 9, 457–467. 10.2147/JPR.S105892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durfey SNM, Kind AJH, Buckingham WR, DuGoff EH, & Trivedi AN. (2019). Neighborhood disadvantage and chronic disease management. Health Services Research, 54(Suppl. 1), 206–216. 10.1111/1475-6773.13092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dutmer AL, Schiphorst Preuper HR, Soer R, Brouwer S, Bültmann U, Dijkstra PU, Coppes MH, Stegeman P, Buskens E, vanAsselt ADI, Wolff AP, & Reneman MF. (2019). Personal and societal impact of low back pain: The Groningen Spine Cohort. Spine, 44(24), E1443–E1451. 10.1097/BRS.0000000000003174 [DOI] [PubMed] [Google Scholar]
- Faul F, Erdfelder E, Buchner A, & Lang A-G. (2009). Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behavior Research Methods, 41(4), 1149–1160. 10.3758/BRM.41.4.1149 [DOI] [PubMed] [Google Scholar]
- Ferreira KA, Teixeira MJ, Mendonza TR, & Cleeland CS. (2011). Validation of brief pain inventory to Brazilian patients with pain. Supportive Care in Cancer, 19(4), 505–511. 10.1007/s00520-010-0844-7 [DOI] [PubMed] [Google Scholar]
- Ferreira ML, Machado G, Latimer J, Maher C, Ferreira PH, & Smeets RJ. (2010). Factors defining care-seeking in low back pain: A meta-analysis of population based surveys. European Journal of Pain, 14(7), 747.e1–747.e7. 10.1016/j.ejpain.2009.11.005 [DOI] [PubMed] [Google Scholar]
- Ferreira W. de A., Giatti L, Figueiredo R. C. de., Mello H. R. de., & Barreto SM. (2018). Concurrent and face validity of the MacArthur scale for assessing subjective social status: Brazilian Longitudinal Study of Adult Health (ELSA-Brasil). Ciencia & Saude Coletiva, 23(4), 1267–1280. 10.1590/1413-81232018234.16972016 [DOI] [PubMed] [Google Scholar]
- Fliesser M, DeWitt Huberts J, & Wippert P-M. (2017). The choice that matters: The relative influence of socio-economic status indicators on chronic back pain - a longitudinal study. BMC Health Services Research, 17(1), 1–8. 10.1186/s12913-017-2735-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuentes M, Hart-Johnson T, & Green CR. (2007). The association among neighborhood socioeconomic status, race and chronic pain in black and white older adults. Journal of the National Medical Association, 99(10), 1160–1169. [PMC free article] [PubMed] [Google Scholar]
- Galea S, Tracy M, Hoggatt KJ, Dimaggio C, & Karpati A. (2011). Estimated deaths attributable to social factors in the United States. American Journal of Public Health, 101(8), 1456–1465. 10.2105/AJPH.2010.300086 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galobardes B, Lynch J, & Smith GD. (2007). Measuring socio-economic position in health research. British Medical Bulletin, 81–82, 21–37. 10.1093/bmb/ldm001 [DOI] [PubMed] [Google Scholar]
- GBD (2017). Disease and Injury Incidence and Prevalence Collaborators. (2018). Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. The Lancet, 392, 1789–1858. 10.1016/S0140-6736(18)32279-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geyer S, Hemström O, Peter R, & Vågerö D. (2006). Education, income, and occupational class cannot be used interchangeably in social epidemiology. Empirical evidence against a common practice. Journal of Epidemiology and Community Health, 60(9), 804–810. 10.1136/jech.2005.041319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green CR, & Hart-Johnson T. (2012). The association between race and neighborhood socioeconomic status in younger Black and White adults with chronic pain. The Journal of Pain, 13(2), 176–186. 10.1016/j.jpain.2011.10.008 [DOI] [PubMed] [Google Scholar]
- Grol-Prokopczyk H. (2017). Sociodemographic disparities in chronic pain, based on 12-year longitudinal data. Pain, 158(2), 313–322. 10.1097/j.pain.0000000000000762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gurung T, Ellard DR, Mistry D, Patel S, & Underwood M. (2015). Identifying potential moderators for response to treatment in low back pain: A systematic review. Physiotherapy, 101(3), 243–251. 10.1016/j.physio.2015.01.006 [DOI] [PubMed] [Google Scholar]
- Hartvigsen J, Hancock MJ, Kongsted A, Louw Q, Ferreira ML, Genevay S, Hoy D, Karppinen J, Pransky G, Sieper J, Smeets RJ, & Underwood M. (2018). & Lancet Low Back Pain Series Working Group. What low back pain is and why we need to pay attention. The Lancet, 391(10137), 2356–2367. 10.1016/S0140-6736(18)30480-X [DOI] [PubMed] [Google Scholar]
- Hoebel J, Maske UE, Zeeb H, & Lampert T. (2017). Social inequalities and depressive symptoms in adults: The role of objective and subjective socioeconomic status. PLoS ONE, 12(1)e0169764. 10.1371/journal.pone.0169764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoy D, Brooks P, Blyth F, & Buchbinder R. (2010). The Epidemiology of low back pain. Best Practice & Research Clinical Rheumatology, 24(6), 769–781. 10.1016/j.berh.2010.10.002 [DOI] [PubMed] [Google Scholar]
- Husky MM, Ferdous Farin F, Compagnone P, Fermanian C, & Kovess-Masfety V. (2018). Chronic back pain and its association with quality of life in a large French population survey. Health and Quality of Life Outcomes, 16(1), 1–9. 10.1186/s12955-018-1018-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ikeda T, Sugiyama K, Aida J, Tsuboya T, Watabiki N, Kondo K, & Osaka K. (2019). Socioeconomic inequalities in low back pain among older people: The JAGES cross-sectional study. International Journal for Equity in Health, 18(1), 1–11. 10.1186/s12939-019-0918-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine (US) Committee on Advancing Pain Research, Care, and Education (2011). Relieving pain in America: A blueprint for transforming prevention, care, education, and research. National Academies Press. 10.17226/13172 [DOI] [PubMed] [Google Scholar]
- International Association for the Study of Pain. (2017, December 14). IASP terminology. Retrieved September 12, 2019, from https://www.iasp-pain.org/Education/Content.aspx?ItemNumber=1698 [Google Scholar]
- Jackman MR, & Jackman RW. (1973). An interpretation of the relation between objective and subjective social status. American Sociological Review, 38(5), 569–582. 10.2307/2094408 [DOI] [PubMed] [Google Scholar]
- Janevic MR, McLaughlin SJ, Heapy AA, Thacker C, & Piette JD. (2017). Racial and socioeconomic disparities in disabling chronic pain: Findings from the health and retirement study. The Journal of Pain, 18(12), 1459–1467. 10.1016/j.jpain.2017.07.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jonsdottir S, Ahmed H, Tómasson K, & Carter B. (2019). Factors associated with chronic and acute back pain in Wales, a cross-sectional study. BMC Musculoskeletal Disorders, 20(1), 215. 10.1186/s12891-019-2477-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kind AJH, & Buckingham WR. (2018). Making neighborhood-disadvantage metrics accessible - The Neighborhood Atlas. The New England Journal of Medicine, 378(26), 2456–2458. 10.1056/NEJMp1802313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kind AJH, Jencks S, Brock J, Yu M, Bartels C, Ehlenbach W, Greenberg C, & Smith M. (2014). Neighborhood socioeconomic disadvantage and 30-day rehospitalization: A retrospective cohort study. Annals of Internal Medicine, 161(11), 765–774. 10.7326/M13-2946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krieger N, Williams DR, & Moss NE. (1997). Measuring social class in US public health research: concepts, methodologies, and guidelines. Annual Review of Public Health, 18, 341–378. 10.1146/annurev.publhealth.18.1.341 [DOI] [PubMed] [Google Scholar]
- Kurani S, McCoy RG, Inselman J, Jeffery MM, Chawla S, Finney Rutten LJ, Giblon R, & Shah ND. (2020). Place, poverty and prescriptions: A cross-sectional study using Area Deprivation Index to assess opioid use and drug-poisoning mortality in the USA from 2012 to 2017. BMJ Open, 10(5), 1–7. 10.1136/bmjopen-2019-035376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maher C, Underwood M, & Buchbinder R. (2017). Non-specific low back pain. The Lancet, 389, 736–747. 10.1016/S0140-6736(16)30970-9 [DOI] [PubMed] [Google Scholar]
- Majedi H, Dehghani SS, Soleyman-Jahi S, Emami Meibodi SA, Mireskandari SM, Hajiaghababaei M, Tafakhori A, Mendoza TR, & Cleeland CS. (2017). Validation of the Persian Version of the Brief Pain Inventory (BPI-P) in chronic pain patients. Journal of Pain and Symptom Management, 54(1), 132–138.e2. 10.1016/j.jpainsymman.2017.02.017 [DOI] [PubMed] [Google Scholar]
- Maly A, & Vallerand AH. (2018). Neighborhood, socio-economic, and racial influence on chronic pain. Pain Management Nursing, 19(1), 14–22. 10.1016/j.pmn.2017.11.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messer LC, & Kaufman JS. (2006). Using census data to approximate neighborhood effects. In Oakes JM & Kaufman JS (Eds.), Methods in social epidemiology (1st ed., pp. 209–236). Jossey-Bass. [Google Scholar]
- Mielck A, Vogelmann M, & Leidl R. (2014). Health-related quality of life and socioeconomic status: Inequalities among adults with a chronic disease. Health and Quality of Life Outcomes, 12, 1–10. 10.1186/1477-7525-12-58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morgan CL, Conway P, & Currie CJ. (2011). The relationship between self-reported severe pain and measures of socio-economic disadvantage. European Journal of Pain, 15(10), 1107–1111. 10.1016/j.ejpain.2011.04.010 [DOI] [PubMed] [Google Scholar]
- National Center for Complementary and Integrative Health (2018). Chronic pain in depth Retrieved August 6, 2019, from https://nccih.nih.gov/health/pain/chronic.htm
- Oates GR, Harris WT, Rowe SM, Solomon GM, Dey S, Zhu A, Hoover WC, & Gutierrez HH. (2019). Area deprivation as a risk factor for methicillin-resistant Staphylococcus aureus infection in pediatric cystic fibrosis. The Pediatric Infectious Disease Journal, 38(11), 1–12. 10.1097/INF.0000000000002419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Operario D, Adler NE, & Williams DR. (2004). Subjective social status: Reliability and predictive utility for global health. Psychology & Health, 19(2), 237–246. 10.1080/08870440310001638098 [DOI] [Google Scholar]
- Penn TM, Overstreet DS, Aroke EN, Rumble DD, Sims AM, Kehrer CV, Michl AN, Hasan FN, Quinn TL, Long DL, Trost Z, Morris MC, & Goodin BR. (2020). Perceived injustice helps explain the association between chronic pain stigma and movement-evoked pain in adults with non-specific chronic low back pain. Pain Medicine, 21, 3161–3171. 10.1093/pm/pnaa095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinheiro MB, Ferreira ML, Refshauge K, Maher CG, Ordoñana JR, Andrade TB, Tsathas A, & Ferreira PH. (2016). Symptoms of depression as a prognostic factor for low back pain: A systematic review. The Spine Journal, 16(1), 105–116. 10.1016/j.spinee.2015.10.037 [DOI] [PubMed] [Google Scholar]
- Polit DF, & Beck CT. (2017). Nursing research: Generating and assessing evidence for nursing practice (10th.). Wolters Kluwer. [Google Scholar]
- Riskowski JL. (2014). Associations of socio-economic position and pain prevalence in the United States: Findings from the National Health and Nutrition Examination Survey. Pain Medicine, 15(9), 1508–1521. 10.1111/pme.12528 [DOI] [PubMed] [Google Scholar]
- Robertson D, Kumbhare D, Nolet P, Srbely J, & Newton G. (2017). Associations between low back pain and depression and somatization in a Canadian emerging adult population. The Journal of the Canadian Chiropractic Association, 61(2), 96–105. [PMC free article] [PubMed] [Google Scholar]
- Ross CE, & Mirowsky J. (2008). Neighborhood socio-economic status and health: Context or composition? City and Community, 7(2), 163–179. 10.1111/j.1540-6040.2008.00251.x [DOI] [Google Scholar]
- Schober P, Boer C, & Schwarte LA. (2018). Correlation coefficients: Appropriate use and interpretation. Anesthesia and Analgesia, 126(5), 1763–1768. 10.1213/ANE.0000000000002864 [DOI] [PubMed] [Google Scholar]
- Shaked D, Williams M, Evans MK, & Zonderman AB. (2016). Indicators of subjective social status: Differential associations across race and sex. SSM - Population Health, 2, 700–707. 10.1016/j.ssmph.2016.09.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh GK. (2003). Area deprivation and widening inequalities in US mortality, 1969–1998. American Journal of Public Health, 93(7), 1137–1143. 10.2105/ajph.93.7.1137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Singh GK, Miller BA, & Hankey BF. (2002). Changing area socio-economic patterns in U.S. cancer mortality, 1950–1998: Part II–Lung and colorectal cancers. Journal of the National Cancer Institute, 94(12), 916–925. 10.1093/jnci/94.12.916 [DOI] [PubMed] [Google Scholar]
- Singh GK, & Siahpush M. (2002). Increasing inequalities in all-cause and cardiovascular mortality among US adults aged 25–64 years by area socio-economic status, 1969–1998. International Journal of Epidemiology, 31(3), 600–613. 10.1093/ije/31.3.600 [DOI] [PubMed] [Google Scholar]
- Singh-Manoux A, Marmot MG, & Adler NE. (2005). Does subjective social status predict health and change in health status better than objective status? Psychosomatic Medicine, 67(6), 855–861. 10.1097/01.psy.0000188434.52941.a0 [DOI] [PubMed] [Google Scholar]
- Solar O, & Irwin AA. (2010). A conceptual framework for action on the social determinants of health: Social determinants of health discussion paper 2 (Policy and practice). World Health Organization. [Google Scholar]
- Song C-Y, Lin S-F, Huang C-Y, Wu H-C, Chen C-H, & Hsieh C-L. (2016). Validation of the brief pain inventory in patients with low back pain. Spine, 41(15), E937–E942. 10.1097/BRS.0000000000001478 [DOI] [PubMed] [Google Scholar]
- Stanford University Department of Psychology. (n.d). MacArthur Scale of subjective social status – Adult version. Stanford SPARQtools. Retrieved January 13, 2021, from https://sparqtools.org/mobility-measure/macarthur-scale-of-subjective-social-status-adult-version/ [Google Scholar]
- Subramanyam MA, Diez-Roux AV, Hickson DA, Sarpong DF, Sims M, Taylor HA, Williams DR, & Wyatt SB. (2012). Subjective social status and psychosocial and metabolic risk factors for cardiovascular disease among African Americans in the Jackson Heart Study. Social Science & Medicine, 74(8), 1146–1154. 10.1016/j.socscimed.2011.12.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tan G, Jensen MP, Thornby JI, & Shanti BF. (2004). Validation of the Brief Pain Inventory for chronic nonmalignant pain. The Journal of Pain, 5(2), 133–137. 10.1016/j.jpain.2003.12.005 [DOI] [PubMed] [Google Scholar]
- Tavakol M, & Dennick R. (2011). Making sense of Cronbach’s alpha. International Journal of Medical Education, 2, 53–55. 10.5116/ijme.4dfb.8dfd [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ulirsch JC, Weaver MA, Bortsov AV, Soward AC, Swor RA, Peak DA, Jones JS, Rathlev NK, Lee DC, Domeier RM, Hendry PL, & McLean SA. (2014). No man is an island: Living in a disadvantaged neighborhood influences chronic pain development after motor vehicle collision. Pain, 155(10), 2116–2123. 10.1016/j.pain.2014.07.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Census Bureau, U. S. (2018). American Community Survey 1-year estimates. Retrieved August 19, 2020, from https://censusreporter.org/profiles/31000US13820-birmingham-hoover-al-metro-area/
- vanHecke O, Torrance N, & Smith BH. (2013). Chronic pain epidemiology: Where do lifestyle factors fit in? British Journal of Pain, 7(4), 209–217. 10.1177/2049463713493264 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vlaeyen JWS, Maher CG, Wiech K, VanZundert J, Meloto CB, Diatchenko L, Battié MC, Goossens M, Koes B, & Linton SJ. (2018). Low back pain. Nature Reviews. Disease Primers, 4(1), 1–18. 10.1038/s41572-018-0052-1 [DOI] [PubMed] [Google Scholar]
- Wolff LS, Acevedo-Garcia D, Subramanian SV, Weber D, & Kawachi I. (2010). Subjective social status, a new measure in health disparities research: Do race/ethnicity and choice of referent group matter? Journal of Health Psychology, 15(4), 560–574. 10.1177/1359105309354345 [DOI] [PubMed] [Google Scholar]
- Yu T, Wei Z, Xu T, Gamber M, Han J, Jiang Y, Li J, Yang D, & Sun W. (2020). The association between the socioeconomic status and body pain: A nationwide survey. Medicine, 99(12) e19454. 10.1097/MD.0000000000019454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zell E, Strickhouser JE, & Krizan Z. (2018). Subjective social status and health: A meta-analysis of community and society ladders. Health Psychology, 37(10), 979–987. 10.1037/hea0000667 [DOI] [PubMed] [Google Scholar]