Abstract
Introduction:
In 2014, traumatic brain injury (TBI) caused 3 million ER visits, hospitalizations, and deaths in the US. The National Institute for Health and Care Excellence (NICE) guidelines, initially generated using data from patients presenting within 24 h of head trauma, are used to determine the need for head computed tomography (CT) scan in patients after 24 h. The authors wanted to determine the proportion of CT scans for head trauma performed at our center in late presenters (>24 h after head trauma), the incidence of intracranial pathology in early (24 h) versus late (>24 h) presenters, and the sensitivity of the NICE guidelines for TBI in these two subpopulations.
Methods:
A retrospective chart review was conducted at a tertiary care center in Karachi. All people (>16) who had a head CT for head trauma from 2010 to 2015 were included. Age, sex, primary diagnosis, comorbid disorders, mechanism-of-injury, duration (in hours) from head trauma to presentation, site, and extent of injury (injury severity scale), hospital stay, number and details of surgical procedures, CT scan findings, other injuries, and mortality were recorded. Means were compared using the Independent Sample t-test, while categorical variables were compared using χ2. Multivariate logistic regression analyses were used to identify TBI predictors.
Results:
The authors found 2009 eligible patients; seven were excluded due to incomplete medical records. The final statistical analysis comprised 2002 head trauma patients. Overall, 52% of early and late presenters had severe injuries, and 2.3% died. 32.2% of patients with head trauma had CT after 24 h. Early presenters were 46.7% traumatized, while late presenters were 63%. The NICE guidelines were 93% sensitive for early presenters and 83% for late presenters with traumatic intracranial injury.
Conclusion:
Patients coming to the emergency department after 24 h of head trauma are a large proportion of the overall head trauma population. The NICE guidelines for late-presenting head injuries are less sensitive and may overlook intracranial injuries if imaging is not performed.
Keywords: neurosurgery, NICE, patient care, TBI
Introduction
Highlights
Traumatic brain injury (TBI) caused 3 million ER visits, hospitalizations, and deaths in the US.
We wanted to determine the proportion of computed tomography scans for head trauma performed at our center in late presenters (>24 h after head trauma), the incidence of intracranial pathology in early (24 h) versus late (>24 h) presenters, and the sensitivity of the National Institute for Health and Care Excellence guidelines for traumatic brain injury in these two subpopulations.
Patients coming to the emergency department after 24 h of head trauma are a large proportion of the overall head trauma population. The National Institute for Health and Care Excellence guidelines for late-presenting head injuries are less sensitive and may overlook intracranial injuries if imaging is not performed.
According to the centers for disease control and prevention, there was ~2.87 million emergency department visits, hospitalizations, and deaths in the United States in 2014 due to traumatic brain injury (TBI)1. Head injuries account for 1.4 million emergency visits in England and Wales annually2. TBI can have both short-term and long-term negative consequences, including death and disability. Up to 15% of people with moderate TBI have a permanent disability3,4.
The National Institute for Health and Care Excellence (NICE) guidelines are widely used in clinical practice to triage patients with head trauma and establish the requirement for a head computed tomography (CT) scan. Surprisingly, this instrument was validated and built using data from patients who presented within 24 h after injury. As a result, it is uncertain if these guidelines apply to patients with head trauma who came in 24 h after the injury.
It is worth noting that there is little information comparing the use of NICE head injury guidelines with outcomes in patients who present within and after 24 h of sustaining a head injury and get a CT scan. Previous research reveals that NICE head injury guidelines are less sensitive for serious intracranial injury in individuals presenting after 24 h of injury (98% sensitivity in those presenting within 24 h versus 70% in patients presenting after 24 h)5.
The goal of this study was to determine the proportion of CT scans performed on late presenters, estimate the prevalence of significant injury in patients with early (24 h) and delayed (>24 h) presentation, compare the rate of intracranial abnormalities, and determine the sensitivity of NICE head injury guidelines for TBI in both groups.
Methods
A retrospective cross-sectional study was conducted at a tertiary care hospital in Karachi, Pakistan during between January 2010 and December 2015.
All adult patients who presented to the emergency room of a with any degree of head injury were included in our study. Patients other than head injury were excluded from our study.
Our study is fully compliant with the STROBE 2016 guidelines6. A complete STROBE 2016 checklist has been provided as a supplementary file. Our study has been registered on Research Registry with the following UIN: researchregistry8237 https://www.researchregistry.com/browse-the-registry#home/registrationdetails/630886af18e9e4002261e8ee/. Our study is in accordance with the Declaration of Helsinki. Data was obtained after ethical approval from Aga Khan University Hospital.
Using a predesigned questionnaire, information on demographics (age and sex), primary diagnosis, comorbid medical conditions, mechanism-of-injury, time from injury to presentation, site, and extent of damage using the injury severity scale, and hospital course were extracted from medical records (length of hospital stay, number and details of surgical procedures performed, findings on the CT scan, other injuries besides head injury, mortality, or morbidity). The patients were then categorized as either early (within 24 h of trauma) or late (more than 24 h after trauma).
The outcome indicators evaluated were the skull radiograph, head CT, and admission requirement. The incidence of a skull fracture influences several management issues. The fracture diagnosis was solely based on the radiologist’s report after radiologists reviewed all skull radiographs. The Royal College of Surgeons and the National Institute for Health and Care Excellence (NICE) guidelines were used to determine the management of each patient in the study and were compared to the actual management.
For continuous variables with normal and non-normal distributions, respective means with SD and medians with interquartile ranges were calculated. Categorical variables were determined using percentages and proportions. Means were compared using t-tests on independent samples, whereas categorical data were analyzed using χ2 testing. A 0.05 P-value was considered significant. For data analysis, version 21 of SPSS IBM was utilized. Multivariate regression was used to identify independent predictors by removing confounders.
Results
After excluding 22 patients due to lacking information in their medical records, there were 9227 eligible patients. The demographics and symptoms are detailed in Table 1. The average age of the patients was 39.47 years; 79% were male, and 21% were female. The most prevalent comorbid seen were diabetes and hypertension, which were present in 81.8% of the research participants (6.7% of patients). 35.5% of the patients who presented to the emergency room were involved in a car collision.
Table 1.
Showing the demographics of the included patients
| Frequency (n) | Percentage (%) | |
|---|---|---|
| Sex | ||
| Male | 4030 | 79.0 |
| Female | 1071 | 21.0 |
| Age groups | ||
| 16–20 years | 285 | 14.3 |
| 21–30 years | 601 | 30.1 |
| 31–40 years | 357 | 17.9 |
| 41–50 years | 262 | 13.1 |
| 51–60 years | 195 | 9.8 |
| 61–70 years | 141 | 7.1 |
| 71–80 years | 98 | 4.9 |
| 81–90 years | 49 | 2.5 |
| 91–100 years | 8 | 0.4 |
| ≥101 years | 1 | 0.1 |
| Mechanism-of-injury | ||
| RTA – pedestrian | 96 | 4.8 |
| RTA – motorcycle | 423 | 21.3 |
| RTA – car | 187 | 9.4 |
| Fall | 393 | 19.8 |
| Assault/nonaccidental trauma | 128 | 6.4 |
| Other | 758 | 38.2 |
| Symptoms | ||
| Vomiting | 215 | 10.8 |
| Focal deficit | 156 | 7.8 |
| Seizures | 50 | 2.5 |
| Amnesia | 172 | 8.6 |
| Irritability/altered behavior | 200 | 10.0 |
| Loss of consciousness | 435 | 21.8 |
| GCS=15 | 3480 | 37.81 |
Eighteen hundred patients were determined to have needed a CT scan by the NICE head injury guidelines’ CT scan criteria (Table 1).
Two thousand two patients underwent a CT scan; of these, 809 (40.4%) were admitted, 47 (2.3%) died after hospital admission, and 565 (28.2%) were observed in the emergency department (with 75% of these patients being followed for >3 h). However, 60% of patients were discharged within 6 h.
Figure 1 depicts why our patients require a CT scan (certain patients had multiple reasons). According to NICE recommendations, the most common indication for a CT scan in our study population would be suspected skull fractures, followed by disturbed mental status.
Figure 1.
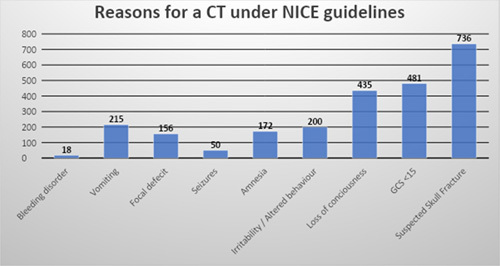
Reasons for computed tomography under the National Institute for Health and Care Excellence guidelines.
One thousand four hundred and fifty three patients (72.6%) who received CT were early presenters, while 549 patients (27.4%) presented late. TBI was diagnosed in 46.7% of early presenters and 63% of late presenters. The sensitivity of the intracranial damage NICE guidelines was 89.1, 93 in early presenters, and 83% in late presenters, as shown in Table 2.
Table 2.
The sensitivity of the intracranial damage NICE guidelines
| Management of patients with head injury | ||
|---|---|---|
| CT scan | Hospital admission | |
| Actual management, n | 2002 | 809 |
| Early presenters, n (%) | 1101 | 466 |
| Late, n (%) | 901 | 343 |
| NICE guideline, n | 1800 | 661 |
| Early, n (%) | 1015 | 361 |
| Late, n (%) | 785 | 300 |
Discussion
Our study shows that TBI on CT imaging is more commonly seen in patients presenting greater than 24 h after head trauma. Further, NICE guidelines have a sensitivity of 93% for TBI among early presenters and 83% among late presenters.
Mild TBI is predicted to occur between 100 and 300 per 100 000 persons7. Traumatic brain damage can be caused by motor vehicle accidents, falls, assaults, and falls8. Mild TBI is characterized by a transient neurological impairment that typically resolves on its own. It is a functional disorder rather than a structural injury, and loss of consciousness may or may not occur. Six to 12% of patients with TBI exhibit abnormalities on CT head scans9,10. In our study, 52% of the 2002 patients who received imaging for moderate TBI had positive CT scan findings.
Prospectively, prediction or decision criteria derived from patient populations can be integrated. These recommendations are used to determine which patients with relatively modest head injuries should undergo a CT scan. It is possible to decide on the patient’s probability of developing neurocranial sequelae due to a minor head injury by applying prediction criteria. Following this, the decision rules for risk assessment are used to establish whether or not CT is advised11.
NICE recommendations aim to integrate clinical practice for managing head injuries based on a single set of guidelines based on the best available evidence. This was initially published in 2003 (NICE clinical guideline 4), revised in 2007 (NICE clinical guideline 56), and superseded in 2014 (NICE clinical guideline 176)12. While there is a considerable body of research on managing acute head trauma, there are no guidelines for individuals with moderate TBI who present after 24 h. Our study’s purpose was to externally validate the NICE guidelines for CT indications in patients with mild head trauma and a presentation delay of greater than 24 hours in Pakistan. Due to the lack of intensity of symptoms, patients with mild head injuries may not seek treatment. 15% of the population getting CT for the examination of head trauma may have a TBI, skull fractures, and delayed hemorrhage due to venous bleeding. Less intracranial injury rates have been recorded in patients with delayed presentations. At the same time, some studies indicate that the rate of TBI in patients who present after 24 h is comparable13,14. Injuries are reported in 46.7% of early presenters and 63.3% of late presenters.
All validated guidelines show a trade-off between sensitivity and specificity, as well as sensitivity and the proportion of patients who require CT scanning according to the guidelines, in identifying patients with traumatic CT findings and patients who require neurosurgical intervention for a complication after a minor head injury.
It has been observed that the NICE criteria can minimize the number of CT scans conducted while maintaining a fair sensitivity for identifying patients with TBI and those requiring neurosurgical intervention9. In our study, the sensitivity of the intracranial damage NICE criteria was 93% for early presenters and 83% for late presenters. According to our interpretation of these results, applying the NICE head injury guidelines in patients presenting after 24 h may fail to identify severe damage. This outcome is consistent with findings from a previous study5.
Among the limitations of our study are its retrospective nature and inherent biases. Our findings from a single Pakistani center may not apply to other environments. In addition, data were collected between 2010 and 2015, suggesting that the mechanism of trauma and its incidence may have evolved with time. The long-term results of hospitalized versus discharged patients were not compared.
Conclusion
Patients who present after 24 h and have suffered a head injury account for a considerable proportion of the population. For patients who present more than 24 h after sustaining a head injury, the NICE recommendations have low sensitivity. If a CT scan is not performed, injuries may go unnoticed in these patients, who comprise a significant proportion of trauma patients.
Ethical approval
Data was obtained after the ethical approval from Aga Khan University Hospital.
Consent
The informed consent from the patients was obtained considering Helsinki’s Declaration.
Sources of funding
No funding has been received.
Author contribution
F.K., M.S.K., and M.S.A.: substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; J.I., A.A., and B.G.: drafting the work or revising it critically for important intellectual content; H.M., W.A.M., and A.A.: final approval of the version to be published; S.I., N.S., and N.K.: agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Conflicts of interest disclosure
No conflict of interests declared by the authors.
Registration of research studies
Name of the registry: Research Registry.
Unique identifying number or registration ID: researchregistry8237. Register Now - Research Registry.
Guarantor
Faheemullah, Muhammad Salman Khan, and Muhammad Sami Alam.
Provenance and peer review
Not commissioned, externally peer-reviewed.
Acknowledgements
Nil.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Supplemental Digital Content is available for this article. Direct URL citations are provided in the HTML and PDF versions of this article on the journal’s website, www.lww.com/annals-of-medicine-and-surgery.
Published online 17 July 2023
Contributor Information
Muhammad Salman Khan, Email: salmankhan3935@gmail.com.
Muhammad Sami Alam, Email: msami.alam@aku.edu.
Sameeha Ismail, Email: informsameeha@yahoo.com.
Bushra Ghafoor, Email: Bushra6877@gmail.com.
Nida Sajjad, Email: sajjad.nida@gmail.com.
Noman Khan, Email: noman.khan@aku.edu.
Wasim Ahmed Memon, Email: wasim.memon@aku.edu.
Abdullah Muhammad Ameen, Email: abdullah.ameen@aku.edu.
Faheemullah Khan, Email: islamianfellow@hotmail.com.
Hassan Mumtaz, Email: hassanmumtaz.dr@gmail.com.
Javed Iqbal, Email: ijaved578578@gmail.com.
Ahmer Ashraf, Email: kamboo93@yahoo.com.
References
- 1.Centers for Disease Control and Prevention. Surveillance Report of Traumatic Brain Injury-related Emergency Department Visits, Hospitalizations, and Deaths—United States, 2014. Centers for Disease Control and Prevention, U.S. Department of Health and Human Services; 2019. [Google Scholar]
- 2. Yates D, Aktar R, Hill J. Assessment, investigation, and early management of head injury: summary of NICE guidance. BMJ 2007;335:719–720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention (CDC). National Center for Injury Prevention and Control Report to Congress on mild traumatic brain injury in the United States: steps to prevent a serious public health problem. Centers for Disease Control and Prevention; 2003. [Google Scholar]
- 4. Kushner D. Mild traumatic brain injury: toward understanding manifestations and treatment. Arch Intern Med 1998;158:1617–1624. [DOI] [PubMed] [Google Scholar]
- 5. Marincowitz C, Allgar V, Townend W. CT head imaging in patients with head injury who present after 24 h of injury: a retrospective cohort study. Emerg Med J 2016;33:538–542. [DOI] [PubMed] [Google Scholar]
- 6. Mathew G, Agha R. for the STROCSS Group. STROCSS 2021: strengthening the reporting of cohort, cross-sectional and case-control studies in surgery. Int J Surg 2021;96:106165. [DOI] [PubMed] [Google Scholar]
- 7. Cassidy JD, Carroll LJ, Peloso PM, et al. Incidence, risk factors and prevention of mild traumatic brain injury: results of the WHO Collaborating Centre Task Force on Mild Traumatic Brain Injury. J Rehabil Med 2004;43(suppl):28–60. [DOI] [PubMed] [Google Scholar]
- 8. Taylor CA, Bell JM, Breiding MJ, et al. Traumatic brain injury-related emergency department visits, hospitalizations, and deaths—United States, 2007 and 2013. MMWR Surveill Summ 2017;66:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Smits M, Dippel DW, de Haan GG, et al. External validation of the Canadian CT Head Rule and the New Orleans criteria for CT scanning in patients with minor head injury. JAMA 2005;294:1519–25. [DOI] [PubMed] [Google Scholar]
- 10. Ibanez J, Arikan F, Pedraza S, et al. Reliability of clinical guidelines in the detection of patients at risk following mild head injury: results of a prospective study. J Neurosurg 2004;100:825–34. [DOI] [PubMed] [Google Scholar]
- 11. Smits M, Dippel DWJ, de Haan GG, et al. Minor head injury: guidelines for the use of CT—a multicenter validation study. Radiology 2007;245:831–838. [DOI] [PubMed] [Google Scholar]
- 12. Davis T, Ings A. Head injury: triage, assessment, investigation and early management of head injury in children, young people and adults (NICE guideline CG 176). Arch Dis Child Educ Pract Ed 2015;100:97–100. [DOI] [PubMed] [Google Scholar]
- 13. Borland ML, Dalziel SR, Phillips N, et al. Delayed presentations to emergency departments of children with head injury: a PREDICT study. Ann Emerg Med 2019;74:1–10. [DOI] [PubMed] [Google Scholar]
- 14. Gelernter R, Weiser G, Kozer E. Computed tomography findings in young children with minor head injury presenting to the emergency department greater than 24 h post injury. Injury 2018;49:82–85; Practice. 2015 Apr 1;100(2):97−100. [DOI] [PubMed] [Google Scholar]


