Abstract
Background:
Ineffective surgical fluid waste management in operating rooms (OR) creates a significant environmental burden, reduces OR efficiency, and adds physical challenges for surgical staff. There is a need for waste management systems that improve OR efficiency, safety, and sustainability. The GREEN study (Greening operating Rooms in EuropE comparing Neptune vs. canisters) was conducted to compare the impact of two fluid waste management systems.
Materials and methods:
This 2-arm, nonrandomized, prospective service evaluation of fluid waste extraction was conducted using observational time series and surveys. Fluid waste-related data were collected from routine urologic and orthopedic surgeries across three European hospital sites. The primary endpoint of waste disposal impact was the volume of treated waste after surgery (kilograms) using Stryker’s Neptune device (n=43) or canisters (n=41). The authors hypothesized that the surgical waste volume related to Neptune is less than the waste volume related to canisters. Secondary endpoints included time efficiency, user satisfaction, and staff ergonomics.
Results:
The total weight of device-related treated waste products was reduced by 98.5% when using Neptune (0.2±0.7 kg) compared with traditional canisters (13.2±16.6 kg; P<0.001). Decreased waste weight also translated to enhanced ergonomic safety for surgical staff, as Neptune reduced surgical fluid weight handled by staff by an average of 34 kg per procedure, a 96% reduction compared to canisters. Furthermore, the use of the Neptune system improved OR efficiency by reducing the number of staff required to manage the fluid suction device (P<0.001) and the time spent disposing of fluid waste (P<0.001).
Conclusion:
Stryker’s Neptune waste management system significantly reduces the volume of treated waste per surgery and improves OR efficiency, staff safety, and user satisfaction over the traditional canister system. This is a more eco-responsible approach to OR fluid waste management and could be considered in any healthcare establishment that generates fluid waste.
Keywords: environmental burden, fluid waste management, operating room, sustainability
Introduction
Highlights
Ineffective surgical fluid waste management in operating rooms (OR) creates a significant environmental burden, reduces OR efficiency, and adds physical challenges for surgical site staff, highlighting the need for waste management systems that improve OR efficiency and enhance sustainability.
The GREEN study (Greening operating Rooms in EuropE comparing Neptune vs. canisters) was conducted to compare the surgical waste disposal impact of two systems across three European hospital sites.
The Neptune waste management system significantly reduces the volume of treated waste per surgery in kilograms and improves OR efficiency, staff safety, and user satisfaction over the traditional canister system.
Results from this study will help inform healthcare decisionmakers to make ORs greener, more efficient, and safer for staff. Given the environmental burden caused by surgical waste, this is highly needed and relevant.
Operating rooms (ORs) generate as much as 70% of the total waste produced in hospitals1. Waste from the OR requires segregation into waste streams, with normal solid waste (requiring landfilling) and regulated medical waste (requiring high energy processing) comprising the major streams. The disposal cost of regulated medical waste is estimated to be eight times that of normal solid waste. Expert opinion suggests that regulated medical waste should constitute no more than 15% of an institution’s total waste stream2, which can be achieved through comprehensive waste segregation processes. These practices not only result in cost savings but are also critical for reducing a hospital’s ecological footprint3.
In many procedures, fluids are introduced to the surgical site to irrigate or cool tissues or to improve visibility of the surgical site. In some surgical specialties such as orthopedics and urology, large amounts of fluid are used and captured by fluid waste management systems in the OR4. This fluid, combined with fluids derived from the patient, needs to be captured during surgery so as not to pose a danger to OR staff. A single surgery may produce upwards of 50 l of fluid waste, and a typical OR can generate two tons of fluid waste each month2,5. This waste stream is typically collected in disposable plastic suction canisters. Surgical suction canisters, estimated to include up to 25% of regulated medical waste from ORs, have historically been disposed of in one of two ways2. The first involves clinical staff manually opening the canisters and pouring the contents down the drain. This can pose a significant risk of splashing or aerosolization of blood-borne pathogens6. A second option involves opening the container and adding chemical solidifiers (or isolyzers) to the contents. Once the solidifier has made the canister contents immoveable, the canister is then placed in the regulated medical waste stream for treatment and disposal. However, this can also lead to staff exposure as well as requiring significant staff time6. Furthermore, medical waste disposal is often performed via incineration, which has significant environmental impacts7.
The burden of managing surgical waste during surgical procedures largely falls on OR staff, including surgical nurses, technicians, and cleaning staff. These staff members experience high rates of spills or splashes of blood or other body fluids as well as exposure to electrosurgical smoke8,9. Ergonomic risks from long periods of standing and lifting patients and heavy equipment commonly lead to lumbar pain; several studies have found incidence of lumbar pain in over 60% of OR nurses 8,10. Time-consuming cleaning protocols and the need to mitigate exposure risks can significantly slow OR workflow and negatively impact overall efficiency. The need for innovative strategies and technologies to substantiate more sustainable and safer OR practices without compromising patient care is clear.
Since the early 2000s, another fluid waste management system has become available that empty liquids directly to the sanitary sewer. Fluid management systems are either stationary and hard plumbed into the sewer or portable, utilizing a cart that employs a docking station for automated drainage to the sewer. These systems are safer for staff, better for the environment, and offer long-term cost savings. The ecological impact of implementing a movable fluid waste recovery system to replace the use of a classic canister system was calculated to significantly reduce global warming impact, environmental toxicity, landfill occupation, as well as required human resources3. Additionally, the use of a ‘constantly closed’ fluid waste management system when compared to a traditional canister-based ‘open’ system was determined to reduce OR staff exposure. The closed system also required significantly less lifting by OR staff (as the system rolls and docks for waste disposal), whereas the open system required full or partially full canisters (up to 2 kg each) to be handled at least five times in the disposal process. The closed system also increased OR efficiency and reduced landfill waste volume11.
To further quantify the specific sustainability, efficiency, safety, and staff satisfaction benefits of using a constantly closed waste management system, we conducted a study to compare these two types of fluid waste management systems in the OR setting — the traditional ‘open’ system relying on traditional canisters and the more recent ‘closed’ system, specifically Stryker’s Neptune 3 Waste Management System (Neptune). A prospective service evaluation of fluid waste extraction during routine surgical procedures was performed using observational time series and a user survey. The primary objective of the study was to compare the waste disposal impact of the Neptune and canister devices, defined as the volume of treated waste related to Neptune or canisters in kilograms after surgery. We hypothesized that the volume of treated waste related to Neptune is less than the volume of treated waste related to canisters. The secondary objectives of the study were to quantify time efficiency, user satisfaction, ergonomics as a metric of safety, and to identify any adverse events reported during device use.
Materials and methods
Study design
This was a prospective, multicenter service evaluation of fluid waste extraction during routine surgical procedures comparing two different fluid waste systems (Neptune and canisters). The use of either system was not randomized but was used 1:1 at each site. Fluid waste management systems are used for the suction of fluid from the surgical field during a variety of surgeries. For the purpose of this evaluation, Neptune and canisters were used in the following urological and orthopedic surgeries: transurethral resection of the prostate (TURP), transurethral resection of bladder tumor (TURBT), holmium laser prostate surgery (HoLEP), arthroscopic rotator cuff and/or labral repair, arthroscopic ACL reconstruction and/or meniscus repair, and total knee or hip replacement. In every surgery, the treated waste, time, user satisfaction, ergonomics, and staff safety associated with the use of the Neptune or canister were measured. The data was collected and managed by Avania. The results of this study have been reported in line with the strengthening the reporting of cohort, cross-sectional, and case–control studies in surgery (STROCSS) criteria12 (Supplemental Digital Content 1, http://links.lww.com/MS9/A204).
Objectives
The study objective was to evaluate the environmental burden, OR efficiency, and staff safety when comparing two fluid waste management systems: Neptune versus canister. The primary objective was to compare the waste disposal impact of the Neptune and canister devices, defined as the volume of treated waste related to Neptune or canisters in kilograms after surgery. The secondary objectives were to compare time efficiency, user satisfaction, and ergonomics for the Neptune and canisters, as well as to track any reported adverse events associated with use of either system.
Inclusion criteria
Inclusion criteria were established as follows: surgery should be performed by an operating team (surgeons and nurses) familiar with the use of Neptune and canisters (≥4 weeks); at least three operating team members should be trained on this service evaluation; surgery should be one of the surgical procedures defined in Section 2.1; and the physician preoperatively expects a normal course of the surgery. Emergency surgeries were excluded. Surgeries were performed by operating teams familiar (≥4 weeks) with the use of Neptune and canisters. At least three operating team members were trained on the service evaluation for this study.
Product comparison
The Stryker Neptune 3 Waste Management System (referred to as ‘Neptune’ for the remainder of this study) is a mobile unit (rover) used to collect, transport, and dispose of fluid waste and evacuate surgical smoke from a surgical site. During collection, fluid waste is removed from the surgical site through suction tubing connected to the inlet ports of the manifold(s) installed in the rover. Manifolds and suction tubing are single-use disposables and must be replaced between patients. If there is still sufficient fluid volume capacity for another surgical procedure, it may not be necessary to empty the contents of the rover’s collection canisters after each procedure. When capacity is reached, the rover is relocated and connected to the Docking Station (docker). Emptying of the fluid waste and cleaning of the device then occurs automatically; this is a constantly closed waste collection and disposal system. The Neptune is intended to be used in the OR, pathology, surgical centers, and doctor’s offices to collect and dispose of surgical fluid waste.
The canister system is designed to receive suction bags to collect and dispose of fluid waste.
The canisters included in the evaluation are provided by the standard of care of the included investigational site. As the waste management method for canisters is similar, no specific requirement on the manufacturer or canister is needed. The canisters are intended to be used in the OR, pathology, surgical centers, and doctor’s offices to collect and dispose of surgical fluid waste.
Study locations
This cohort study was conducted in three major hospitals; one in the United Kingdom (NHS Friarage) and two in Spain (Sant Pau; German Trias). The ethics committee of each hospital confirmed that, given the nature of the study in which no patient data is collected, ethics approval was not required for this analysis. Friarage (site 1) collected data for 41 total surgeries performed, including 23 with Neptune and 18 with canisters. Sant Pau (site 2) collected data for 24 total surgeries performed, including 12 with Neptune and 12 with canisters. German Trias (site 3) collected data for 19 total surgeries, including 8 with Neptune and 11 with canisters. The total collected data involved 43 surgeries using Neptune and 41 surgeries using canisters. Data were collected over the span of October 2021 to June 2022.
Endpoints
The primary endpoint was the total weight of treated waste related to the Neptune or canister in kilograms after surgery. The tested hypothesis was that the weight of treated surgical waste associated with the use of Neptune is significantly less than the weight of treated waste related to the use of canisters. Secondary sustainability endpoints include the number of device-related disposable products used during surgery (which includes the combined number of inco pads, isolyzers, waste bags, canister liners, Neptune manifolds, cable ties, incineration boxes, and tubes), and endpoints related to OR efficiency, ergonomics, adverse events, and user satisfaction.
The secondary endpoints related to efficiency included time spent intraoperatively: time to adjust or re-adjust suction levels, and time taken to replace liners (for canisters) or time to remove and replace a manifold (for Neptune). Postoperative time was also recorded for the following: time to clean the OR postsurgery (minutes) and total time to transfer waste to the appropriate location (minutes). The number of staff required to collect and dispose of liquid waste was also recorded.
The ergonomic endpoint was the combined total weight of surgical fluid handled intraoperatively and postoperatively. The number of manual lifting events associated with the collection and disposal of surgical fluid waste was also recorded. Any adverse events related to surgical fluid collection and disposal were noted.
The general satisfaction of the Neptune device compared to the canister device with the performance of the products was determined based on questionnaires for surgeons and nurses.
Statistics
All statistical analysis was performed using SAS Software version 9.4 or later. The necessary sample size was estimated via power analysis across sites, assuming approximately equal distribution across surgery types. These calculations were assessed based on the sample size required per treatment group to achieve 80% power at a two-sided alpha level of 0.05 for the difference in the volume of fluid surgical waste between treatment groups. Joint replacement as a procedure required the largest sample size (n=12/group); therefore, the plan was to enroll 24 surgeries per procedure type for a total of 120 procedures. Surgeries were enrolled in a 1:1 ratio into the Neptune or canister evaluation groups. Due to COVID-19 regulations limiting data collection, data analysis was performed after data was collected from 84 procedures (Neptune: n=43; canisters: n=41), which was deemed appropriate based on effect size for the primary outcome metric (Cohen’s d>0.8). The data for all sites were combined. Subgroup analysis by procedure was performed for the primary outcome metric to test procedure specificity. When comparing continuous variables between the Neptune and canister groups, a Shapiro–Wilks test was used to assess for normality in each group for a given variable. If normality was met for both groups (result of Shapiro–Wilks is P≥0.05), a two-sample t-test was used for comparison. If normality was not met for both treatment groups, a Wilcoxon Rank Sum test was used to compare the given variable between groups. Therefore, significant findings of the Wilcoxon Rank Sum test determine only differences in the distribution of data for each group, and do not signify differences in means/medians between the two treatment groups. Categorical variables were compared with a χ2test or Fisher’s Exact test. Significance was set at P≤0.05. Data are displayed as box plots identifying the median, quartiles 1 and 3, and maximum/minimum points shown as whiskers. Data are described in the text as mean±SD, unless stated otherwise. No data points were excluded as outliers; however, four data points were excluded from the time efficiency outcome metric due to erroneous data collection (sample size for this metric: canisters n=38; Neptune n=42).
Results
Sustainability
The total weight of device-related treated waste was reduced by 98.5% when using Neptune (0.2±0.7 kg) compared with the use of traditional canisters (13.2±16.6 kg; Fig. 1A). When assessed by individual procedure type, waste weight was significantly reduced in the Neptune group for all procedures (Supplemental Table S1, Supplemental Digital Content 1, http://links.lww.com/MS9/A203). The use of Neptune also reduced the total number of disposable device-related products used per procedure by 87.5% (2.3±2 for the Neptune group and 18.4±17.4 for canisters group; Fig. 1B).
Figure 1.
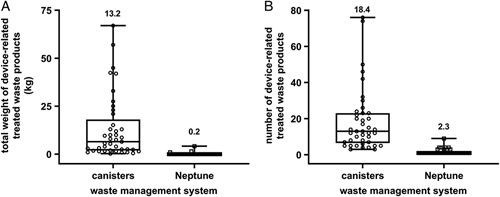
Sustainability of surgical waste management systems. (A) Distribution of the total weight of device-related treated waste products measured on a scale after each surgical procedure (kg) demonstrates a significant difference between waste weight for procedures utilizing canisters versus Neptune (P<0.001). (B) There was a similar decrease in the total number of disposable device-related products used during surgery when Neptune was used compared to canisters (P<0.001). Individual data points are shown overlaid with a box plot (quartile 1, median, and quartile 3) and max/min whiskers. Numbers above bars represent average mean. P-values are generated from Wilcoxon Rank Sum Tests due to non-normal data distributions.
OR staff efficiency
Furthermore, the use of the Neptune system improved OR staff efficiency. When considering intraoperative and postoperative time spent collecting and disposing fluid waste, the use of Neptune resulted in an 83.9% time savings (average mean difference of 11.5 min, Fig. 2).
Figure 2.
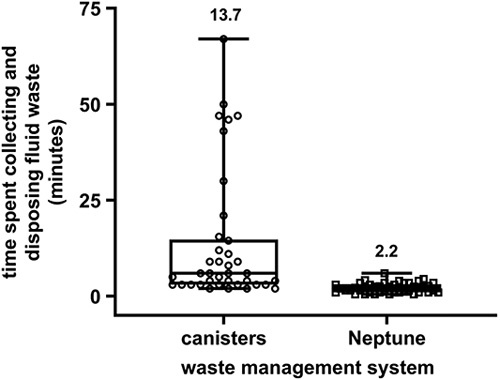
OR staff time spent collecting and disposing of surgical fluid waste. Distribution of the combined time spent collecting fluid waste intraoperatively (including adjusting suction levels, changing canister liners or Neptune manifolds, and suctioning fluids from the floor or other containers at the end of the procedure) and disposing of waste postoperatively (in minutes); data distributions are significantly different between canister (n=38) and Neptune groups (n=42, P<0.001). Individual data points are shown overlaid with a box plot (quartile 1, median, and quartile 3) and max/min whiskers. Numbers above bars represent average mean. P-values are generated from Wilcoxon Rank Sum Tests due to non-normal data distributions.
More than one staff member was required for preoperative set-up of the suction system for 44% of procedures when using canisters compared to only 2% (a single procedure) when using Neptune. Intraoperative replacement of canister liners was required in over 40% of procedures (n=17/41); Neptune manifolds, analogous to canister liners, required replacement in only 14% of procedures (n=6/43). Similarly, canister system suction levels had to be readjusted in 39% of procedures (n=16/41) and in almost half of these situations, adjusting suction required more than one OR staff (n=7/16). In procedures utilizing Neptune, suction was readjusted in only 14% of procedures (n=6/43) and never required more than one OR staff. Overall staffing requirements are detailed in Supplemental Table 2 (Supplemental Digital Content 1, http://links.lww.com/MS9/A203).
OR staff ergonomics and safety
On average, the use of Neptune reduced the total weight of surgical fluid lifted and moved by OR staff (combined intraoperative and postoperative waste handling) by 34 kg per procedure compared to canisters (95.8% decrease, Fig. 3A). Additionally, Neptune reduced the number of required manual handling/lifting events per procedure by 91% (reduced from 9.2±11.3 when using canisters to 0.8±1.5 when using Neptune), demonstrating a significant improvement in staff ergonomic safety (Fig. 3B). In 70% of procedures utilizing Neptune, the need to lift any surgical waste weight was completely eliminated (n=30/43 procedures in which there was 0 total weight handled and 0 handling events) compared to canisters for which waste weight handling and lifting was required in 100% of procedures.
Figure 3.
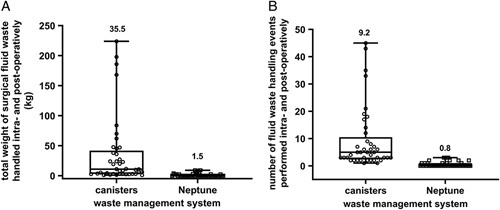
Staff ergonomics during use of surgical waste management systems. (A) Distribution of the total weight of surgical fluid waste (in kg) handled by OR staff during procedures utilizing canisters versus Neptune (P<0.001). (B) There was a similar decrease in the total number of handling events required during and after surgical procedures when Neptune was used compared to canisters (P<0.001). Individual data points are shown overlaid with a box plot (quartile 1, median, and quartile 3) and max/min whiskers. Numbers above bars represent average mean. P-values are generated from Wilcoxon Rank Sum Tests due to non-normal data distributions.
Adverse events were recorded during all procedures. Reported events are listed in Table 1. All reported events (n=7) were related to the use of canisters; no adverse events were reported during the use of Neptune. All reported events affected OR staff but did not affect patients. The severity of all adverse events was considered mild, and all resolved without sequelae.
Table 1.
List of reported adverse events related to device use
| Site | Surgery type | Treatment group | Adverse event |
|---|---|---|---|
| NHS Friarage Hospital | HOLEP | Canister | Excess fluid on floor caused staff to slip |
| Sant Pau | Knee arthroscopy | Canister | Liners opened from high pressure and splashed staff with liquid waste |
| Sant Pau | Shoulder arthroscopy | Canister | Liner opened from high pressure spilling liquid waste on staff |
| Sant Pau | Shoulder arthroscopya | Canister | Nurse tripped on canister tubing |
| Sant Pau | Shoulder arthroscopya | Canister | Anesthetist tripped over canister tower |
| Sant Pau | Shoulder arthroscopy | Canister | Nurse tripped on canister tubing |
| German Trias | HOLEP | Canister | Right arm inflammation from carrying heavy waste containers |
AEs occurred during the same procedure.
Staff satisfaction
General satisfaction regarding the use of surgical waste systems was rated by both surgeons and OR nurse staff. The nursing and operating staff rated eight performance aspects of the device used. 97.7% of nurses said they were very satisfied or satisfied with the set-up of Neptune (Fig. 4A), emptying/disposing of the waste from Neptune (Fig. 4B), the time efficiency of Neptune (Fig. 4C), and the general performance of Neptune (Fig. 4D). Additionally, 97.7% of nurse operating staff stated that Neptune device use during surgery (Fig. 4E) and overall safe use were both very easy or easy (Fig. 4F). In contrast, 63% of nurse operating staff were ‘very unsatisfied’ or ‘unsatisfied’ with the canister waste disposal process (Fig. 4B) and over 46% said safe use of the canisters was ‘very difficult’ or ‘difficult’ (Fig. 4F). With regards to surgeons, 95.3% of operating surgeons said they were very satisfied or satisfied with the use of Neptune in their working environment. 88.4% of operating surgeons said they were very satisfied or satisfied with both the general performance of the Neptune device as well as the performance of the suction during surgery. Full results are detailed in Supplemental Tables S3 (Supplemental Digital Content 1, http://links.lww.com/MS9/A203 and S4) (Supplemental Digital Content 1, http://links.lww.com/MS9/A203).
Figure 4.
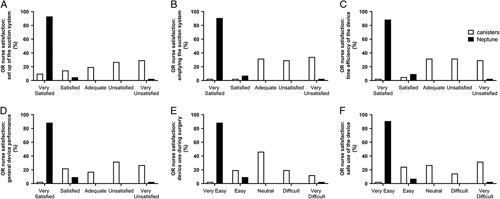
OR Nurse Responses to Satisfaction Questionnaire. Distribution of responses regarding satisfaction or dissatisfaction in (A) the set-up of the suction system, (B) the process of emptying/disposing waste from the suction device, (C) the time efficiency of the device, and (D) the general performance of the device demonstrate increased satisfaction rates for Neptune compared to canisters. Additionally, the distribution of responses regarding the ease or difficulty of (E) the use of the suction device during surgery and (F) the overall safe use of the suction device demonstrates an improved ease of use of Neptune compared to canisters. All response distributions were significantly different (P<0.001) when comparing canisters and Neptune. Data are shown as a percentage of responses for each response option by group. P-values are generated from Fisher’s Exact tests.
Discussion
This study is one of the first head-to-head comparison studies to assess surgical waste management in Europe. Results from this study indicate that, compared with a traditional canister-based waste management system, the use of Neptune is associated with a significant decrease in the weight of treated waste products. This reduction was significant for each surgical procedure assessed, suggesting improved sustainability regardless of procedure specificity of irrigation use or the typical total fluid waste generated. Recently, the WHO issued a statement concerning the increased urgency to improve the sustainability of healthcare-related waste13. Both landfill disposal and incineration are detrimental to the environment, with the latter also having significant public health implications related to the release of a considerable number of air pollutants14. Utilizing a system that reduces the quantity of waste requiring treatment is a fundamental principle of environmental sustainability; this embodies the ‘reduce’ of the 3 R’s approach to minimizing our ecological footprint5.
Healthcare facilities produce a significant portion of the total waste generated; in France, this is estimated to comprise 3.5% of national waste production3. A pilot study was recently performed to assess the ecological impacts of sustainable actions employed within a hospital system in France. Of these, there were 13 actions directly related to waste reduction. Relevant to our study, one action was the implementation of a ‘movable irrigation fluid recovery system’ that connects directly to wastewater as opposed to the alternative ‘classic system using flexible bags’ and associated disposal of waste through infectious waste avenues. Utilization of this action significantly impacted overall global warming, environmental toxicity, and human toxicity when compared to the alternative3. Green surgical practices have also been evaluated in the United States; healthcare facilities in the US produce more than 4 billion tons of waste annually15. Kwayke et al. reviewed 43 publications detailing US healthcare sustainability initiatives. Five primary recommendations were made through the consensus of a seven-member panel, the first being ‘operating room waste reduction and segregation’16. This was the only variable of the five that could be directly controlled by the surgical team. Data from our study serves to strengthen such sustainability-related recommendations.
Reducing the overall weight of collected waste also impacts the surgical staff that manages waste collection and disposal. This study demonstrated a significant reduction in the physical demands of these tasks, as clearly seen in the complete elimination of waste handling requirements for 70% of procedures when using Neptune. Of seven reported adverse events related to the use of canisters, one was physical discomfort and pain caused by handling heavy waste containers. Previous studies also report decreased satisfaction with ‘manual handling’ aspects of the canister system (average rating of 3 out of 5) compared to the closed waste system (average rating greater than 4 out of 5)11. A cross-sectional study of Spanish nurses identified a significantly increased incidence of musculoskeletal diseases in surgical nurses compared to ward (hospitalization) nurses; while not significant, the surgical nurses also experienced increased rates of elbow and wrist or hand discomfort compared to ward nurses. Over 70% of surgical nurses reported lower back pain17, highlighting the need for ergonomic improvements in the OR. The use of the Neptune system could significantly improve working conditions.
One reported adverse event related to the use of canisters was due to OR staff slipping on a wet floor and three more were due to tripping over canister tubing. Slips, trips, and falls are reported to be the second most common cause of lost-workday injuries in hospitals. The Association of periOperative Registered Nurses (AORN) acknowledges that these are preventable and suggests both keeping floors dry and controlling the clutter as key approaches to reducing the risk of falls18. Because neither of these issues (slipping on fluids on the floor and tripping over hosing) was reported with Neptune, the use of this closed system may effectively remove these risks from the OR.
An added benefit of eliminating or significantly reducing the need for waste handling is eliminating or significantly reducing the risk of splashes. Occupational exposure to potential blood-borne exposure constitutes a significant health hazard to healthcare workers19. The remaining two of seven reported adverse events related to the use of canisters were exposure to biohazardous material after canister liners opened during handling. No exposure events were reported in the procedures using Neptune. Improved safety is also reflected in customer satisfaction feedback. 90.7% of nursing staff using Neptune reported that safe use of the device was ‘very easy’, which contrasts with only 2.4% of canister users (staff in a single procedure) reporting this level of ease to safely use canisters. This metric of user satisfaction likely reflects both reduced incidence of splashes and spills but also improved ergonomics with Neptune compared to canisters.
OR efficiency is improved with the use of a closed waste management system. Maximizing OR efficiency has long been a priority for surgeons and hospital decisionmakers. OR efficiency impacts surgeon productivity and patient experience20. In a previous study, users of an open system spent 3.5 times longer for set-up, handling, and maintenance compared to Neptune11. Use of Neptune was estimated to provide a time savings of 25 h per week based on a weekly hospital average of 450 cases. Results of the current study demonstrated an even larger difference in time spent collecting and disposing of fluid surgical waste, with almost an eight times greater time requirement for canisters over Neptune. From customer feedback, it is generally accepted that the set-up of canisters requires more time than Neptune (and the data presented here indicates it requires a greater number of staff), which means this difference may be even more considerable than reported. A reduction in staffing requirements with Neptune could result in increased hospital capacity, decreased costs, and faster OR turnover times, providing hospitals with opportunities to treat patients earlier/faster and reduce waiting lists.
This study presents some limitations. Due to COVID-related restrictions, access to ORs for research staff was severely limited, which led to a decreased total sample size included in the analysis. Nonetheless, conclusions were still significantly supported by a large effect size for the primary outcome metric. Hypothesis testing was done only for the primary outcome; however, doing so for secondary outcomes could be considered in future studies. This study focused on assessing the impact of waste management systems mainly from the hospital perspective, where the largest impact is expected as such devices are used in ORs. Future assessments could adopt a broader societal perspective and capture the impact across the entire waste collection and processing cycle. As this is one of the first head-to-head comparison studies, in general, conducting future studies will strengthen the evidence base for improving surgical waste management in Europe.
In conclusion, this study demonstrates that the use of the Neptune waste management system significantly reduces the weight of treated surgical waste and improves OR efficiency, staff safety, and user satisfaction over the traditional canister system. In a setting where nurses are already experiencing a demanding environment, hazardous conditions, and ergonomically challenging tasks19, Neptune provides a simpler and more effective waste management process. This study demonstrates the clear benefits of a constantly closed waste system, Neptune, over the canister system. The use of this more eco-responsible approach to OR fluid waste management could be considered in any healthcare establishment that generates fluid waste. Results from this study will help inform healthcare decisionmakers to make ORs greener, more efficient, and safer for staff. Given the environmental burden caused by surgical waste, this is highly needed and relevant.
Ethical approval
The ethics committee of each hospital involved in this study confirmed that, given the nature of the study in which no patient data is collected, ethical approval was not required for this analysis.
Consent
The ethics committee of each hospital involved in this study confirmed that, given the nature of the study in which no patient data is collected, patient consent was not required for this analysis.
Sources of funding
Redacted for review. Funding for this study was provided by Stryker, which participated in the study design and interpretation of the results.
Author contribution
S.B., J.C., E.M.G., L.V.F., J.H., and L.T.: contributed to the study design and interpretation of results. Editorial support in the form of manuscript development, collating of author comments, copy editing, and referencing was provided by J.H., an employee of Stryker. All authors contributed to and provided approval for the submitted manuscript.
Conflicts of interest disclosure
J.H.: employee of Stryker, which funded the study; L.T.: employee of and shareholder in Stryker, which funded the study. The remaining authors declare that have no conflicts of interest.
Research registration unique identifying number (UIN)
Name of the registry: not applicable.
Unique identifying number or registration ID: not applicable.
Hyperlink to your specific registration (must be publicly accessible and will be checked): not applicable.
Guarantor
The Guarantor for this study is Luqman Tariq.
Data availability statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Provenance and peer review
This paper was not invited/commissioned.
Acknowledgements
We would like to acknowledge the participating hospital sites (Friarage Hospital, Hospital Sant Pau, and Hospital Germans Trias) and their staff for their contributions to the study, both in terms of data collection and responding to survey questionnaires. Also, we would like to thank Avania, a Clinical Research Organization, for their participation in the study design, data collection, analysis, and interpretation of the results.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Supplemental Digital Content is available for this article. Direct URL citations are provided in the HTML and PDF versions of this article on the journal's website, www.lww.com/annals-of-medicine-and-surgery.
Published online 31 July 2023
Contributor Information
Sarah Baker, Email: sarah.baker20@nhs.net.
Julie Clark, Email: juliee.clark@nhs.net.
Angels B. Pla, Email: mabarbera.germantrias@gencat.cat.
Eulalia V. Feixas, Email: EVinals@santpau.cat.
Julianne Huegel, Email: julianne.huegel@stryker.com.
Luqman Tariq, Email: Luqman.tariq@stryker.com.
References
- 1. Lee RJ, Mears SC. Greening of orthopedic surgery. Orthopedics 2012;35:e940–e944. [DOI] [PubMed] [Google Scholar]
- 2. Moyle JK, Lynn CD. The Business Case for Sustainability in Surgery. Practice Greenhealth, Nov. 2018, Accessed 25 October 2022. https://practicegreenhealth.org/about/news/business-case-sustainability-surgery
- 3. Rouvière N, Chkair S, Auger F, et al. Ecoresponsible actions in operating rooms: a health ecological and economic evaluation. Int J Surg 2022;101:106637. [DOI] [PubMed] [Google Scholar]
- 4. Alexander CE, Scullion MM, Omar MI, et al. Bipolar versus monopolar transurethral resection of the prostate for lower urinary tract symptoms secondary to benign prostatic obstruction. Cochrane Database Syst Rev 2019;12:CD009629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kagoma YK, Stall N, Rubinstein E, et al. People, planet and profits: the case for greening operating rooms. CMAJ 2012;184:1905–1911. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Burger J. 3 Golden Rules of Fluid Waste Disposal. Outpatient Surgery, July 2018, Accessed 25 October 2022. https://www.aorn.org/outpatient-surgery/articles/outpatient-surgery-magazine/2018/july/3-golden-rules-of-fluid-waste-disposal
- 7. Attrah M, Elmanadely A, Akter D, et al. A review on medical waste management: treatment, recycling, and disposal options. Environments 2022;9:146. [Google Scholar]
- 8. Uğurlu Z, Karahan A, Ünlü H, et al. The effects of workload and working conditions on operating room nurses and technicians. Workplace Health Saf 2015;63:399–407. [DOI] [PubMed] [Google Scholar]
- 9. Bree K, Barnhill S, Rundell W. The dangers of electrosurgical smoke to operating room personnel: a review. Workplace Health Saf 2017;65:517–526. [DOI] [PubMed] [Google Scholar]
- 10. Van den Berg-Dijkmeijer ML, Frings-Dresen MHW, Sluiter KJ. Risks and health effects in operating room personnel. Work 2011;39:331–344. [DOI] [PubMed] [Google Scholar]
- 11. Horn M, Patel N, MacLellan DM, et al. Traditional canister-based open waste management system versus closed system: hazardous exposure prevention and operating theatre staff satisfaction. ORNAC J 2016;34:36–50. [PubMed] [Google Scholar]
- 12. Mathew G, Agha R. for the STROCSS Group. STROCSS 2021: strengthening the reporting of cohort, cross-sectional and case–control studies in surgery. Int J of Surg 2021;96:106165. [DOI] [PubMed] [Google Scholar]
- 13.WHO. Water, Sanitation, Hygiene and Health Unit. Tonnes of COVID-19 health care waste expose urgent need to improve waste management systems. News release, 01 February 2022. Accessed 17 January 2023. https://www.who.int/news/item/01-02-2022-tonnes-of-covid-19-health-care-waste-expose-urgent-need-to-improve-waste-management-systems
- 14. Sharma R, Sharma M, Sharma R, et al. The impact of incinerators on human health and environment. Rev Environ Health 2013;28:67–72. [DOI] [PubMed] [Google Scholar]
- 15. Van Demark RE, Jr, Smith VJS, Fiegen A. Lean and green hand surgery. J Hand Surg Am 2018;43:179–181. [DOI] [PubMed] [Google Scholar]
- 16. Kwakye G, Brat GA, Makary MA. Green surgical practices for health care. Arch Surg 2011;146:131–136. [DOI] [PubMed] [Google Scholar]
- 17. Martí-Ejarque MDM, Guiu Lázaro G, Juncal RC, et al. Occupational diseases and perceived health in operating room nurses: a multicenter cross-sectional observational study. Inquiry 2021;58:469580211060774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Nichols J. Keep Your OR Free of Slipping and Tripping Hazards. Outpatient Surgery Magazine, 13 June 2022. Accessed 17 January 2023. https://www.aorn.org/outpatient-surgery/article/2022-June-slipping-tripping
- 19. Mohammadi N, Allami A, Malek Mohamadi R. Percutaneous exposure incidents in nurses: knowledge, practice and exposure to hepatitis B infection: percutaneous exposure incidents in nurses. Hepat Mon 2011;11:186–190. [PMC free article] [PubMed] [Google Scholar]
- 20. Ryan D, Rocks M, Noh K, et al. Specific factors affecting operating room efficiency: an analysis of case time estimates. J Hand Surg Am 2022;S0363-S5023:00533–0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.


