Abstract
Background:
The time to emerge from anesthesia is affected by patient factors, anesthetic factors, the duration of surgery, and preoperative and intraoperative pain management.
Objective:
This study aimed to determine the prevalence and contributing factors of delayed awakening following general anesthesia.
Method:
A cross-sectional study was conducted from January to June 2022. After getting ethical approval with the permission number S/C/R 37/01/2022, willing patients participate with written informed consent. Chart reviews in the preoperative and postoperative recovery rooms were used to collect data. Frequency and percentage with cross-tabulation were used to provide the descriptive statistics. To determine the predictive variables that were associated with the outcome variable, bivariable, and multivariable logistic regression models were fitted. The statistical significance was evaluated using P-values of 0.05 for multivariable regression.
Results:
In the current study, a normal emergency occurred in 91.7% of surgical patients receiving general anesthesia, while delayed awakening, emergence with hypoactive, and emergence with delirium occurred in 2.6, 3.9, and 1.8% of cases, respectively. Patients older than 64 years [adjusted odds ratio (AOR): 1.33, 95% CI: 0.83–7.191], being diploma anesthesia providers (AOR: 2.38, 95% CI: 2.05–7.15), opioids (AOR: 2.3, 95% CI: 2.20–5.76), surgery lasting longer than 2 h (AOR: 1.91, 95% CI: 1.83–6.14), estimated blood loss of more than 1500 ml (AOR: 1.20, 95% CI: 0.62–11.30), crystalloid administration of more than 3000 ml (AOR: 3.12, 95% CI: 2.19–7.32), intraoperative hypotension (AOR: 3.37, 95% CI: 2.93–9.41) and extreme body weight, were significantly linked to delayed awakening after general anesthesia.
Conclusion:
Although delayed emergence is an uncommon condition with a number of contributing causes, it is preventable, and once it has occurred, it presents a challenge for anesthetists.
Keywords: anesthetic agents, delayed awakening, delayed emergence, delayed recovery, drug effects, general anesthesia, risk factors
Background
Highlights
Even though delayed awakening is preventable, it remains a challenge for anesthetists.
Patient-related, medication, and surgical factors have an impact on consciousness recovery.
It is crucial to accurately identify high-risk patients who have delayed awakenings.
Failure to restore consciousness after a general anesthetic within 30–60 min is known as delayed awakening1–3. This is something that some surgical patients encounter right after their anesthetic wears off, but if it persists or is delayed, it can be a diagnostic problem and pose a major risk in mental status and respiratory compromise leading to increased morbidity, and operating room delays4.
At the end of the surgical procedure, anesthesia and adjuvant medications are stopped being administered, and the patient gradually regains consciousness5. After being extubated, most patients become more fully cognizant in about 15 min and all patients should be awake and alert within 60 min of the last sedative, narcotic, or anesthetic medication being administered6.
Delayed awaking resulting from lingering anesthetics, pharmaceutical effects, surgical complications, neurologic occurrences, endocrine issues, and patient-related factors6–8. In addition, it may also be caused by underlying metabolic conditions like hypoglycemia, severe hyperglycemia, and electrolyte imbalance, especially hypernatremia. Other potential causes include chronic hypertension, liver disease, hypoalbuminemia, uremia, and severe hypothyroidism intraoperative cerebral hypoxia, hemorrhage, embolism, or thrombosis. Although maintaining the airway, breathing, and circulation should be the priorities of treatment, accurate diagnosis of the underlying cause is essential4,6,8.
Since there is no specific tool for tracking postanesthesia recovery, the clinical assessment is conducted by using glaucoma scale (GCS) scales that are frequently used to gage the level of consciousness in various situations. Although GCS was created for the examination and prognosis of traumatic brain injuries, it also offers a useful approach for determining the level of awareness after general anesthesia9.
Diagnosing the underlying cause of delayed awakening is crucial to developing appropriate treatment options, to reduce the patient’s pain and the likelihood of delayed awakening that shortens the patient’s recovery time and increases the quality of life.
Even though the prevalence of delayed awakening has been decreasing annually due to the ongoing development of anesthetics and related monitoring technology, it is still one of the major side effects of general anesthesia10. This study seeks to identify the prevalence and contributing variables of delayed awakening following general anesthesia. This topic has not yet been the subject of research or reviews in our nation, which intrigues us.
Methods
An observational study was conducted from January to June 2022. After getting ethical approval from Debre Markos University, with the permission number S/C/R 37/01/2022, willing patients participate with written informed consent.
The patient’s basic details and medical background were gathered before surgery, and information about the anesthetic and surgical-related aspects was collected from the patient’s chart with the trained data collectors, in the recovery room, since every activity in the operation room was recorded on the anesthesia and surgery recording sheet. Even though this study aimed to determine the prevalence of delayed awakening and its predictors, during data collection some cases were not categorized as either normal or delayed emergence, and so we have categorized some patients as hypoactive and emergence delirium based on the valid tools.
Every patient who was scheduled for elective surgery under general anesthesia and was included while a patient refused, age younger than 18 years, known neuromuscular disease, procedures that required therapeutic hypothermia, and poor exercise tolerance on preoperative evaluation based on a 6 min walk test was excluded from the study.
Medicines in daily use were taken as usual. Onegram of paracetamol 30 min before initiation of surgery and 8 mg of dexamethasone during induction were institutional protocols for indicated elective surgical procedures as premedication. The ASA minimum standard of monitoring has been attached for all patients who entered the operation room for intraoperative monitoring. This study was reported in line with strengthening the reporting of cohort, cross-sectional and case–control studies in surgery (STROCSS) guidelines11.
Sample size determination
The sample size was calculated based on a single population proportion formula by considering the previously published article with Zhang et al.12 having the prevalence of delayed awakening 25%.
Assuming
n=the sample size, 95% confidence interval, 5% margin of error.
with a 10% none response rate, n=318.
Statistical analysis
A descriptive analysis of variables was used to summarize the data. The normality distribution was passed with the Kolmogorov–Smirnov test and normally distributed data are presented as means and SD. Both bivariable and multivariable logistic regression was performed with SPSS (Statistical Package for the Social Sciences) version 27 to identify the predictive variables, which had an association with the outcome variable. P-values <0.2 for bivariable and <0.05 for multivariable regression were used to consider the statistical significance.
Operational definitions
Delayed awakening is defined as the failure to regain consciousness within 30 min after anesthesia and adjuvant medications are stopped being administered2.
Preoperative anemia – preoperative levels of Hgb <12 g/dl in both sexes13.
Intraoperative Hypotension – A decrease in mean arterial pressure by 20%14.
Hypothermia – is defined as a core body temperature below 36°C15.
Preoperative Hypertension – Hypertension is usually defined by the presence of a chronic elevation of systemic arterial pressure above a certain threshold value16.
On the General Cognitive Scale (GCS), a score of >12 denotes a restoration of consciousness, whereas a GCS of less than 8 denotes coma17.
Hypoactive and Emergency with Delirium – Patients were assessed 10 min after being admitted to the recovery room. The Richmond Agitation and Sedation Scale (RASS) was used to assess the severity of emergency delirium/hypoactive emergence18; a 10-point scale with four levels of anxiety/agitation, one level denoting a calm and alert state patient, and five levels of sedation. Emergence delirium was defined as a RASS score ≥+1 and hypoactive emergence as a RASS score ≤2.
Results
Preoperative and sociodemographic details of patients undergoing elective surgery
A total of 318 patients were enrolled, but 5 patients declined to take part, and 2 patients with incomplete documentation, leaving 311 patients signed up with a response rate of 97.8%. In this research, women outnumbered men by a ratio of 1:1.14, and the mean and SD of the age (year) and BMI (kg/m2) of the study participants was 38.14±14.97 and 27.2±3.9, respectively. Comorbid conditions made up of asthma, chronic alcohol use, hypertension, diabetes patients, and known cardiac patients were 12.2, 22.5, 29.6, 8.7, and 2.3% of the study participants, respectively, as shown in Table 1.
Table 1.
Preoperative and sociodemographic details of elective surgical patients who underwent surgery, 2022 (N=311)
| Delayed awakening | ||||
|---|---|---|---|---|
| Characteristics | Category | Frequency (%) | Yes, n (%) | No, n (%) |
| Sex | Male | 145 (46.6) | 6 (4.14) | 139 (95.86) |
| Female | 166 (53.4) | 2 (1.2) | 164 (98.8) | |
| Age | 18–64 | 290 (93.3) | 7 (2.4) | 278 (97.6) |
| >64 | 21 (6.7) | 1 (4.8) | 25 (95.2) | |
| BMI (kg/m2) | 18.5–24.9 | 77 (24.8) | 3 (3.9) | 74 (96.1) |
| 25–24.9 | 189 (60.8) | 4 (2.1) | 185 (97.9) | |
| >30 | 45 (14.5) | 1 (2.2) | 44 (97.8) | |
| ASA status | ASA I | 169 (54.3) | 1 (0.6) | 168 (99.4) |
| ASA II | 116 (37.3) | 5 (4.3) | 111 (95.7) | |
| ASA III | 26 (8.4) | 2 (7.7) | 24 (92.3) | |
| Diagnosed cardiac disease | Yes | 7 (2.3) | 2 (28.6) | 298 (71.4) |
| No | 304 (97.7) | 6 (2.0) | 5 (98.0) | |
| Asthma | Yes | 38 (12.2) | 3 (7.9) | 35 (92.1) |
| No | 273 (87.8) | 5 (1.8) | 268 (98.2) | |
| Alcoholic history | Yes | 70 (22.5) | 3 (4.3) | 67 (98.7) |
| No | 241 (78.5) | 5 (2.1) | 236 (97.9) | |
| Smokers | Yes | 38 (12.2) | 3 (7.9) | 35 (92.1) |
| No | 273 (87.8) | 5 (1.8) | 268 (98.2) | |
| Hypertension | Yes | 92 (29.6) | 4 (4.3) | 88 (95.6) |
| No | 219 (70.4) | 4 (1.8) | 215 (98.2) | |
| Diabetes mellitus | Yes | 27 (8.7) | 4 (14.8) | 23 (85.2) |
| No | 284 (91.3) | 4 (1.4) | 280 (98.6) | |
| Preoperative fasting time | >12 h | 83 (26.7) | 6 (7.2) | 77 (92.8) |
| <12 h | 228 (73.3) | 2 (0.9) | 226 (99.1) | |
| Preoperative anemia | Yes | 53 (17.0) | 3 (5.7) | 52 (94.3) |
| No | 258 (83) | 5 (1.9) | 251 (98.1) | |
ASA, American Society of Anesthesiologist.
In the study setting, 26.7% of elective procedures under general anesthesia has greater than 12 h of fasting and a significant number of patients were scheduled for elective surgery with hemoglobin of less than 12 g/dl around 17.0%, and the cross-tabulation results of variables associated with the delayed emergency was explicitly shown in Table 1.
Preoperative organ function findings of major elective surgery patients
Based on their medical history and physical examination, patients have surgery along with standard laboratory tests around 15.8% of the time if there are no symptoms of organ failure. About 80.4% of elective instances have involved one or more of the following tests, either independently or in combination: thyroid function tests, liver function tests, renal function tests, pulmonary function tests, or tests for cardiovascular problems as shown in Figure 1. Since the source of the anomaly is connected to the surgical treatment, ~3.9% of surgical cases undergo surgery with some optimization of the organ function test results as shown in Figure 1.
Figure 1.
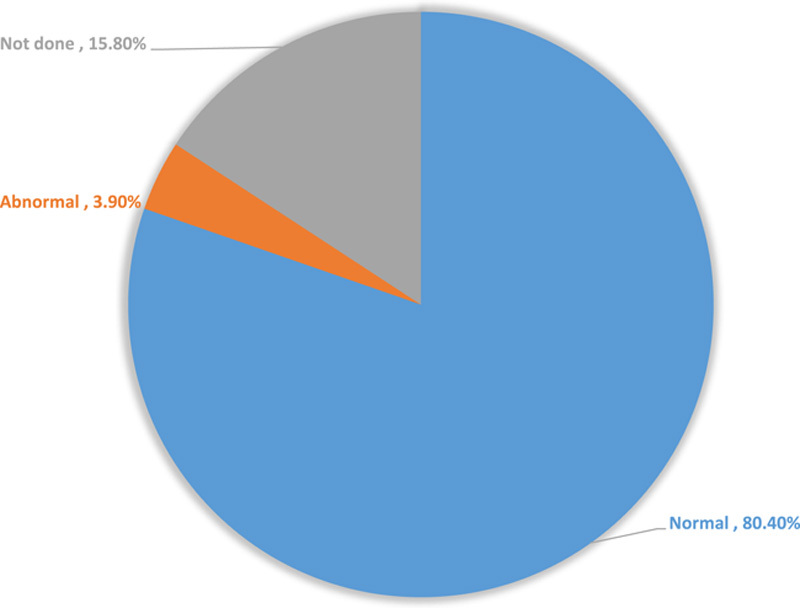
Preoperative organ function findings of major elective surgery patients, 2022 (n=311).
The pattern of surgical procedures
Regional anesthesia technology advancements have revolutionized practices and largely replaced surgeries done under general anesthesia19. Head and neck, hepatobiliary, gastrointestinal, and obstetrics and gynecology surgery made up the majority of the surgical operations covered in this study, accounting for 21.5, 17, 15.1, and 10.6%, respectively, as shown in Figure 2.
Figure 2.
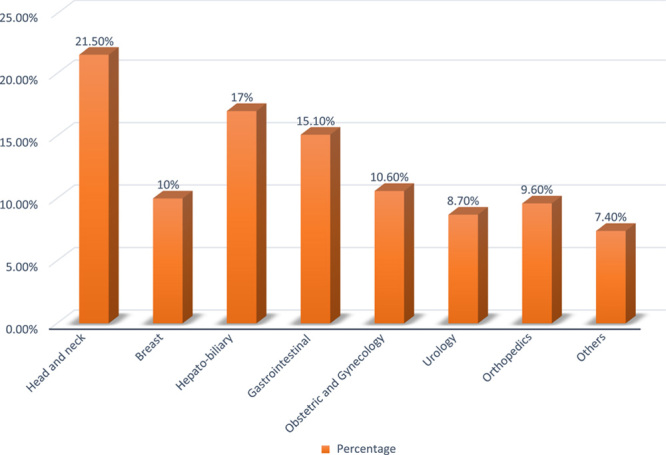
The pattern of surgical procedures for elective surgical patients, 2022 (n=311).
Anesthesia and surgery-related causes of delayed emergency following elective surgery
Despite the restricted resources, premedication was frequently used in elective surgery patients (77.5%). According to the risk and benefit analyses, dexamethasone and paracetamol were the most often recommended premeditations, with mean and SD values of 6.0±1.7 (4.3–9.6) mg and 1.0±0.5(0.4–1.3) g, respectively. Ketofol (38.8%) and inhalational drugs (55.0%) were the most widely used intraoperative procedures for induction and maintenance, respectively, as shown in Table 2. Patients undergoing elective surgery under general anesthesia made up; 61.7% of patients receive strong opioids; 28.6% experience at least one episode of unintentional hypotension; 24.8% receive an intraoperative regional block for the management of postoperative pain; 8.7% receive blood transfusions; and 20.6% experience intraoperative hypothermia (Table 2). The majority of surgical patients (70.5%) had an estimated blood loss of less than 1000 ml, 46.6% have operations that last longer than 2 h, and 76.2% get less than 3 l of intraoperative crystalloid fluids. With its cross-tabulations, the pattern of distribution of risk variables for a delayed emergence was made clear (Table 2).
Table 2.
Anesthesia and surgery-related causes of delayed emergency following elective surgery, 2022 (N=311).
| Delay awakening | ||||
|---|---|---|---|---|
| Characteristics | Category | Frequency n (%) | Yes, n (%) | No, n (%) |
| Anesthesia premedication | Yes | 241 (77.5) | 6 (2.5) | 235 (97.5) |
| No | 70 (22.5) | 2 (2.9) | 68 (97.1) | |
| Induction agent | Ketamine | 30 (23.8) | 1 (3.3) | 29 (96.7) |
| Ketofol | 131 (38.8) | 5 (3.8) | 126 (96.2) | |
| Propofol | 83 (30.1) | 2 (2.4) | 81 (97.6) | |
| Thiopental | 67 (7.3) | 0 (0.0) | 67 (100.0) | |
| Maintenance of anesthesia | Inhalational | 171 (55.0) | 7 (4.1) | 170 (95.9) |
| Combined | 140 (45.0) | 1 (0.7) | 139 (99.3) | |
| Neuromuscular blockers | Depolarizing | 26 (8.4) | 0 (0.0) | 26 (100.0) |
| Nondepolarizing | 78 (25.1) | 2 (2.6) | 76 (97.4) | |
| Combined | 207 (66.6) | 6 (2.4) | 201 (97.6) | |
| Strong intraoperative opioids given | Yes | 192 (61.7) | 5 (2.6) | 187 (97.4) |
| No | 119 (38.3) | 3 (2.5) | 116 (97.5) | |
| Hypotension | Yes | 89 (28.6) | 3 (3.4) | 86 (96.6) |
| No | 222 (71.4) | 5 (2.3) | 217 (97.7) | |
| Duration of surgery | <60 min | 44 (14.2) | 0 (0.0) | 44 (100.0) |
| 60–120 min | 122 (39.2) | 5 (4.1) | 117 (95.1) | |
| >120 min | 145 (46.6) | 3 (2.1) | 142 (97.9) | |
| Estimated blood loss | <500 | 35 (11.3) | 0 (0.0) | 35 (100.0) |
| 500–1000 | 184 (59.2) | 5 (2.7) | 179 (97.3) | |
| 1000–1500 | 69 (22.2) | 3 (4.3) | 66 (95.7) | |
| 1500–2000 | 23 (7.4) | 0 (0.0) | 23 (100.0) | |
| Intraoperatively blood transfused | Yes | 27 (8.7) | 7 (25.9) | 20 (74.1) |
| No | 284 (91.3) | 1 (0.3) | 283 (99.7) | |
| The intraoperative fluid used (ml) | 1000–2000 | 141 (45.3) | 2 (1.4) | 139 (98.6) |
| 2000–3000 | 96 (30.9) | 2 (2.0) | 94 (98.0) | |
| >3000 | 74 (23.8) | 4 (5.4) | 70 (94.6) | |
| Anesthetist specialty | Diploma | 45 (14.5) | 3 (6.7) | 42 (93.3) |
| Degree | 157 (50.5) | 4 (2.5) | 153 (97.5) | |
| Masters and above | 109 (35.0) | 1 (0.9) | 108 (99.1) | |
| Surgical specialty | IESO | 8 (2.6) | 0 (0.0) | 8 (100.0) |
| General surgeon | 155 (49.8) | 5 (3.2) | 150 (96.7) | |
| Specialized surgeon | 148 (47.6) | 3 (2.0) | 145 (98.0) | |
| Regional block | Yes | 77 (24.8) | 1 (1.3) | 76 (98.7) |
| No | 234 (75.2) | 7 (3.0) | 227 (97.0) | |
| Intraoperative hypothermia | Yes | 64 (20.6) | 6 (9.4) | 58 (90.6) |
| No | 247 (79.4) | 2 (0.8) | 245 (99.2) | |
| Reversal given | Yes | 285 (91.6) | 7 (2.5) | 278 (97.5) |
| No | 26 (9.4) | 1 (3.8) | 25 (96.2)s | |
The study subjects’ use of intraoperative analgesic medications
The majority of intraoperative painkillers administered to research participants were pethidine alone (28.90%), diclofenac with tramadol (27.30%), and pethidine with diclofenac (20.30%) (Fig. 3).
Figure 3.
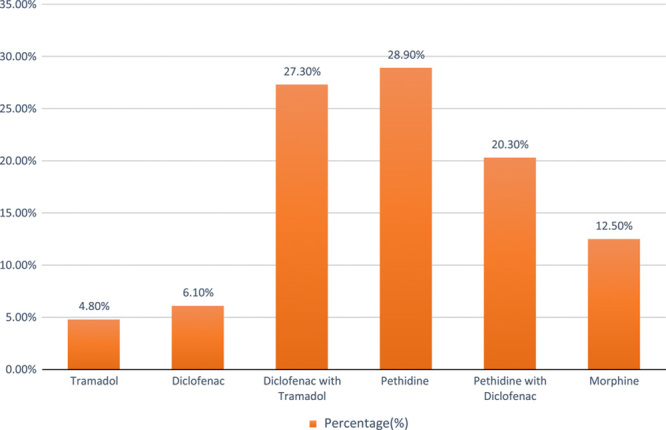
The prevalence of delayed awakening concerning opioids, 2022.
Delayed awakening after general anesthesia and its underlying causes
Patients older than 64 years who underwent elective surgery under general anesthesia were 1.33 times [adjusted odds ratio (AOR): 1.33, 95% CI: 0.83–7.19) more likely to experience delayed awakening than patients younger than 64 years. In comparison to patients with normal body weight, elective surgery patients who were underweight or obese had a 2.1 and 1.38 times higher risk of delayed awakening from general anesthesia, respectively. Strong intraoperative opioid administration (AOR: 2.3, 95% CI: 2.20–5.76), prolonged surgery lasting longer than 2 h (AOR: 1.91, 95% CI: 1.83–6.14), extended preoperative fasting (AOR: 2.72, 95% CI: 2.11–6.35), estimated blood loss of more than 1.5 l (AOR: 1.20, 95% CI: 0.62–11.30), being diploma anesthesia provider (AOR: 2.38, 95% CI: 2.05–7.15), intraoperative crystalloid administration of more than 3000 ml (AOR: 3.12, 95% CI: 2.19–7.32), intraoperative hypotension (AOR: 3.37, 95% CI: 2.93–9.41), and out of normal body weight, were significantly linked to delayed awakening after general anesthesia as shown in Table 3.
Table 3.
Delayed awakening after general anesthesia and its underlying causes, 2022 (n=311)
| Delayed awakening | ||||
|---|---|---|---|---|
| Variables | Category | COR (95% CI) | AOR (95% CI) | P |
| Age (year) | 18–64 | 1.00 | 1.00 | |
| >64 | 3.54 (0.703–7.81) | 1.33 (0.83–7.19) | 0.043* | |
| BMI (kg/m2) | 18.5–24.9 | 1.19 (0.90–4.31) | 2.1 (0.91–5.36) | 0.038* |
| 25–24.9 | 1.00 | 1.00 | ||
| >30 | 3.12 (1.24–3.67) | 1.38 (1.34–5.21) | 0.025* | |
| Preoperative anemia | Yes | 1.00 | 1.00 | |
| No | 3.12 (1.35–5.73) | 1.61 (1.17–3.14) | 0.26 | |
| MET equivalent >4 | Yes | 1.00 | 1.00 | |
| No | 2.81 (1.76–9.35) | 3.19 (1.52– 5.75) | <0.001* | |
| Preoperative hypertension | Yes | 1.00 | 1.00 | |
| No | 2.3 (0.81–5.39) | 1.01 (0.57–4.61) | 0.92 | |
| Intraoperative strong opioids given | Yes | 3.19 (1.90–6.31) | 2.3 (2.20–5.76) | 0.009* |
| No | 1.00 | 1.00 | ||
| Intraoperative hypotension | Yes | 1.00 | 1.00 | |
| No | 5.17 (2.23–11.13) | 3.37 (2.93–9.41) | 0.013* | |
| Surgical time (min) | <60 | 1.00 | 1.00 | 0.17 |
| 60–120 | 1.47 (0.73–3.65) | 1.03 (0.32–8.11) | ||
| >120 | 3.34 (2.96–7.21) | 1.91 (1.83–6.14) | 0.01* | |
| Intraoperatively blood transfused | Yes | 1.00 | 1.00 | |
| No | 1.25 (1.13–3.69) | 2.26 (1.93–7.84) | 0.17 | |
| Estimated blood loss | <500 | 1.00 | 1.00 | |
| 500–1000 | 1.10 (1.12–9.71) | 1.14 (0.90–7.13 ) | 0.53 | |
| 1000–1500 | 1.13 (0.92–4.63) | 1.65 (1.32–3.93 ) | 0.27 | |
| 1500–2000 | 1.51 (1.32–9.21) | 1.20 (0.62–11.30 ) | <0.001* | |
| Anesthesia specialty | Diploma | 1.71 (1.21–5.17) | 2.38 (2.05–7.15) | 0.015* |
| Degree | 1.32 (0.23–4.97) | 1.30 (0.65–8.95) | 0.63 | |
| Masters and above | 1.00 | 1.00 | ||
| Intraoperative hypothermia | Yes | 1.00 | 1.00 | |
| No | 1.83 (1.80–9.37) | 1.37 (1.21–4.01) | 0.86 | |
| The intraoperative fluid used (ml) | 1000–2000 | 1.00 | 1.00 | |
| 2000–3000 | 3.73 (2.67–7.38) | 1.92 (1.09–4.32) | 0.52 | |
| >3000 | 2.03 (1.95–5.15) | 3.12 (2.19–7.32) | 0.012* | |
| Preoperative fasting time | <12 h | 1.00 | 1.00 | |
| >12 h | 5.26 (4.84–9.56) | 2.72 (2.11–6.35) | <0.001* | |
AOR, adjusted odds ratio; COR, crude odds ratio.
Statistically significant.
The overall awakening state of elective surgical patients under general anesthesia
In the current study, ineffective emergence occurred in 8.3% of surgical patients receiving general anesthesia, with the composition of delayed awakening, emergence with hypoactive, and emergence with delirium occurring in 2.6, 3.9%, and 1.8% of cases, respectively, as shown in Figure 4.
Figure 4.
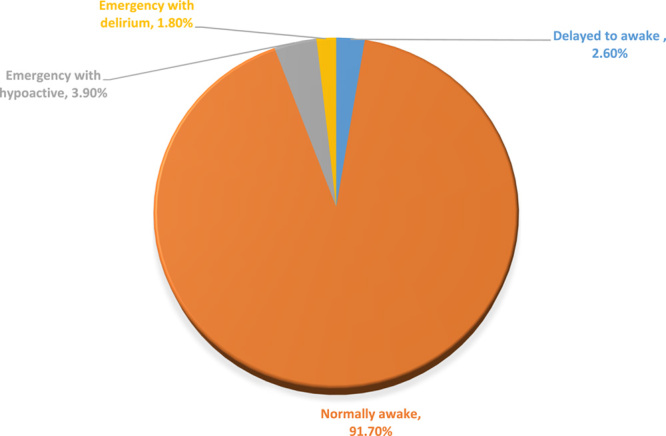
General level of arousal in patients undergoing elective surgery under general anesthesia 2022 (n=311).
Discussion
The reasons for a delayed waking after anesthesia are frequently complex and influenced by patient, medication, surgical, and metabolic factors6. This study sought to ascertain the prevalence and risk factors for delayed waking, and it found that 2.6% of people experienced it. Age greater than or equal to 64 years was found to be a risk factor in the current study for delayed awakening after anesthesia, which is comparable to other articles by Misal et al.4 and Thomas et al.3 which may be related to the fact that gradual deterioration in brain function, elderly patients are more susceptible to the benzodiazepines, opioids, and intravenous and inhalational anesthetic medications that are frequently used during general anesthesia7,20. Understanding this idea inevitably necessitates changing the dosage of anesthesia-related medications.
Similar to what Zhang et al.12 reported, fasting time was a risk factor for delayed awakening following anesthesia in this study, which may be connected to the common occurrence of hypoglycemia7. In patients with prolonged fasting hypoglycemia is one of the most terrifying side effects for patients under general anesthesia, which concealed the clinical symptoms of hypoglycemia, and prolonged hypoglycemia can have major adverse effects on the brain, delaying the need for emergence.
Being diploma has been linked to a delay in awakening, which is proven by Cascella et al.1 problems necessitate adjusting anesthetic doses to prevent late awakening. On the other hand, comorbidities cause dalliance in an emergency could be explained that lung disease, which impairs the ability to flush out inhaled substances and lengthens the duration of anesthetic effects dependent on hepatic metabolism or renal excretion. According to Cascella et al.1 Misal et al.4 and Thomas et al.3 prolonged duration of anesthesia increases recovery time from anesthesia due to tissue uptake depending on the concentration used and drug solubility1,21; which is supported by the present investigation.
Similar to Cascella et al.1 intraoperative hypotension is another decisive factor in this study that contributes to delayed awakening. This can be explained by the fact that because of the decreased cardiac output caused, blood cannot carry medications for either metabolism or excretion, it is crucial to use accurate intraoperative monitoring technology and maintain the proper amount of hypothermia.
Strong opioids are predictor variables of this study which is comparable to previous study findings3,17,22–24. The possible reasons might be in addition to drowsiness and analgesia, opioids also cause respiratory depression, which lessens the sensitivity of the brain stem chemoreceptors to carbon dioxide.
According to the current study, either a high or low body mass index was an independent risk factor for delayed awakening, which is supported by Zhang et al.12. This finding may be because most anesthesia drugs are lipid and protein-bound23 which results in free active drugs, being present in high concentrations in the fat tissue and plasma, respectively.
Liberal intraoperative fluid infusion volumes increase the likelihood of delayed awakening following surgery (22)25, but the mechanism underlying this effect is unknown26 the potential explanation is fluid-induced hypothermia, which is consistent with our findings.
Another surgical-related risk factor identified in this study was longer surgical duration greater than 2 h, and estimated blood loss greater than 1500 ml has an association with delayed awakening following general anesthesia, which is supported by previously published articles12,23,27. The possible explanation may be the more time on surgery, the more tissue manipulation, and the more bleeding. So bleeding leads to hypotension→decrease cardiac output→anesthesia drugs not sufficiently transported for metabolism and excretion.
In general, a patient’s risk of a delayed return to consciousness can be influenced by a variety of patient-related, pharmaceutical, and surgical factors, and the majority of cases are quickly treated once they have been detected. If straightforward examination and management fail to resolve the issue, a number of uncommon and catastrophic causes should be taken into account.
Conclusion
Although delayed emergence is an uncommon condition with a number of contributing causes, it is preventable, and once it has occurred, it presents a challenge for anesthetists.
Strength and limitation
Strength: This investigation is the first to be carried out in the study setting and provides baseline data.
The study was carried out prospectively with representative sample size.
Limitation: Even if the incidence of hypoactive emergence and postoperative delirium was assessed, their predictors are not identified.
Significance of the study
This study helps clinicians to assure patient safety, perform surgery on the assumption that it would have a curative impact, precisely calculate the patient’s anesthetic dosage, and complete the procedure as quickly as possible.
Since the independent variables are identified, it is essential to precisely identify high-risk patients who have delayed awakenings and carefully monitor the patient’s vital signs.
To researchers: Since there is no proven tool for delayed awakening it is better to build a model with time to recovery from anesthesia to incorporate continuous variable, and hemodynamic changes during the intraoperative period to evaluate the influence on delayed awakening, which will provide more reliable evidence into the clinical management.
This study also gives some information that delayed awakening is not the only problem that the patient encounters but hypoactive emergence and postoperative delirium are the anesthetists’ concerns, so these two problems need further research.
Ethical approval
Ethical approval was obtained from Debre Markos University, the School of Medicine Ethical Review Board with the permission number S/C/R 37/01/2022.
Consent
Written informed consent was obtained from the patient for publication and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal on request.
Sources of funding
None.
Author contribution
S.D.B.: conceptualization, formal analysis, investigation, methodology, project administration, resources, software, supervision, validation, visualization, writing – original draft and writing – review and editing; W.D.A.: data curation, formal analysis, investigation, project administration, resources, software, validation, and writing – review and editing; M.B.F.: data curation, formal analysis, methodology, resources, software, validation, writing – original draft, and writing – review and editing.
Conflicts of interest disclosure
The authors declare that they have no conflicts of interest.
Research registration unique identifying number (UIN)
Registry used= https://www.researchregistry.com
Unique identifying number or registration ID=9020.
Hyperlink to your specific registration (must be publicly accessible and will be checked) researchregistry9020 with link address of = https://www.researchregistry.com/browse-the-registry#home/
Guarantor
Samuel Debas Bayable (Assistant professor).
Provenance and peer review
Not commissioned, externally peer-reviewed.
Data availability statement
Data is available on the corresponding author and can be presented upon request.
Acknowledgements
The authors are thankful to Debre Markos University for giving ethical clearance and Debre Markos Comprehensive Specialized Hospital stakeholders for their positive response during data collection. In addition, we highly appreciate all data collectors and volunteer study subjects, supervisors, and anesthesia and gynecologic department staff who support the data collectors.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Published online 31 July 2023
Contributor Information
Samuel D. Bayable, Email: samuel_debas@dmu.edu.et.
Wubet D. Amberbir, Email: wubetdessie19@yahoo.com.
Melaku B. Fetene, Email: bmelaku088@gmail.com.
References
- 1. Cascella M, Bimonte S, Di Napoli R. Delayed emergence from anesthesia: what we know and how we act. Local Reg Anesth 2020;13:195–206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Ellis TA, Edberg JL, Kumar N, et al. Delayed emergence from anesthesia: a simulation case for anesthesia learners. MedEdPORTAL 2017;13:10628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Thomas E, Martin F, Pollard B. Delayed recovery of consciousness after general anaesthesia. BJA Educ 2020;20:173–179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Misal US, Joshi SA, Shaikh MM. Delayed recovery from anesthesia: a postgraduate educational review. Anesth Essays Res 2016;10:164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Brown EN, Lydic R, Schiff ND. General anesthesia, sleep, and coma. N Engl J Med 2010;363:2638–2650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Frost E. Differential diagnosis of delayed awakening from general anesthesia: a review. Middle East J Anaesthesiol 2014;22:537–548. [PubMed] [Google Scholar]
- 7. Castillo A, Sanchez C, Bazán Y. Risk factors related to delayed post-anesthetic awakening in the elderly operated by elective video laparoscopic surgery. J Anesth Crit Care Open Access 2023;15:22–25. [Google Scholar]
- 8. Maeda S, Tomoyasu Y, Higuchi H, et al. Independent predictors of delay in emergence from general anesthesia. Anesth Prog 2015;62:8–13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wiinholdt D, Eriksen SA, Harms LB, et al. Inadequate emergence after non‐cardiac surgery—A prospective observational study in 1000 patients. Acta Anaesthesiol Scand 2019;63:1137–1142. [DOI] [PubMed] [Google Scholar]
- 10. Ohta J, Suto T, Kato D, et al. Loss of endogenous analgesia leads to delayed recovery from incisional pain in a rat model of chronic neuropathic pain. Brain Res 2020;1727:146568. [DOI] [PubMed] [Google Scholar]
- 11. Mathew G, Agha R. STROCSS 2021: strengthening the reporting of cohort, cross-sectional and case–control studies in surgery. Ann Med Surg (Lond) 2021:72 103026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Zhang G, Pan B, Tan D, et al. Risk factors of delayed recovery from general anesthesia in patients undergoing radical biliary surgery: what can we prevent. Medicine 2021;100:e26773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Punnonen K, Irjala K, Rajamäki A. Serum transferrin receptor and its ratio to serum ferritin in the diagnosis of iron deficiency.. Blood 1997;89:1052–1057. [PubMed] [Google Scholar]
- 14. KlÖHR S, Roth R, Hofmann T, et al. Definitions of hypotension after spinal anaesthesia for caesarean section: literature search and application to parturients. Acta Anaesthesiol Scand 2010;54:909–921. [DOI] [PubMed] [Google Scholar]
- 15. Simegn GD, Bayable SD, Fetene MB. Prevention and management of perioperative hypothermia in adult elective surgical patients: a systematic review. Ann Med Surg 2021;72:103059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.New definition for hypertension. J Korean Med Assoc 2018;61:485–492. [Google Scholar]
- 17. Pai S-L. Delayed emergence and emergence delirium in adults. UpToDate 2020;5:1–31. [Google Scholar]
- 18. Sessler CN, Gosnell MS, Grap MJ, et al. The Richmond Agitation–Sedation Scale: validity and reliability in adult intensive care unit patients. Am J Respir Crit Care Med 2002;166:1338–1344. [DOI] [PubMed] [Google Scholar]
- 19. Sen S, Ge M, Prabhakar A, et al. Recent technological advancements in regional anesthesia. Best Pract Res Clin Anaesthesiol 2019;33:499–505. [DOI] [PubMed] [Google Scholar]
- 20. Chemali J, Kenny J, Olutola O, et al. Ageing delays emergence from general anaesthesia in rats by increasing anaesthetic sensitivity in the brain. Br J Anaesth 2015;115(suppl_1):i58–i65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Staheli B, Rondeau B. Anesthetic Considerations in the Geriatric Population. StatPearls [Internet]. StatPearls Publishing; 2022. [PubMed] [Google Scholar]
- 22. Xará D, Silva A, Mendonça J, et al. Inadequate emergence after anesthesia: emergence delirium and hypoactive emergence in the Postanesthesia Care Unit. J Clin Anesth 2013;25:439–446. [DOI] [PubMed] [Google Scholar]
- 23. Sinclair RC, Faleiro RJ. Delayed recovery of consciousness after anaesthesia. Cont Educ Anaesthesia, Critical Care Pain 2006;6:114–118. [Google Scholar]
- 24. Takemori T, Oyama Y, Makino T, et al. Long-term delayed emergence after remimazolam-based general anesthesia: a case report. JA Clin Rep 2022;8:86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Shaikh SI, Lakshmi R. Delayed awakening after anaesthesia – a challenge for an anaesthesiologist. Int J Biomed Adv Res 2014;5:352–354. [Google Scholar]
- 26. Choi S-S, Kim S-H, Kim Y-K. Fluid management in living donor hepatectomy: recent issues and perspectives. World J Gastroenterol 2015;21:12757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Sheerin Sarah L, Kumar D, Krishnamoorthy S. Delayed Recovery.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data is available on the corresponding author and can be presented upon request.


