Abstract
Background:
Microsurgical great toe-to-thumb transfer (mGTT) is a widely used procedure when immediate replantation of thumb is not feasible. The aim of this study was to investigate the alteration of plantar pressure profile of the donor foot after mGTT.
Methods:
Twenty patients receiving microsurgical great toe-to-hand transfer between 1985 to 2014, and 16 healthy subjects were recruited. Group 1 consisted of 20 feet receiving mGTT, whereas group 2 consisted of 32 normal feet as control. The flap design in this study was to preserve 1 cm of the proximal phalanx to maintain the attachment of the plantar aponeurosis and intrinsic muscles. The Taiwan Chinese version of the Foot Function Index was used for patient-reported outcome measurement. A novel Emed-X system was used for dynamic plantar pressure measurement. A total of four parameters were collected, including peak pressure, contact area, contact time, and pressure–time integral.
Results:
In group 1, the peak pressure redistributed under the first metatarsal bone and was significantly higher than group 2 (P < 0.05). There was no significant change of the contact area between the midfoot region of group 1 and group 2 (P > 0.05). Furthermore, similar foot clearance efficiency was demonstrated in group 1 and group 2 (P > 0.05).
Conclusions:
The windlass effect of the foot will not be affected when performing mGTT with preservation of 1 cm of the proximal phalanx. Therefore, this surgical procedure is highly recommended for clinical application.
Takeaways
Question: Is the windlass effect affected after microsurgical great toe-to-thumb transfer?
Findings: Peak pressure was redistributed to the first metatarsal bone and there was no increased foot contact area in the medial midfoot.
Meaning: The windlass effect of the foot can work properly after performing microsurgical great toe-to-thumb transfer with preservation of 1cm of the proximal phalanx.
INTRODUCTION
Microsurgical great toe-to-hand transfer (mGTT) has been used to reconstruct fingers of mutilated hands since the 1960s.1,2 It has become a widely used standard procedure when immediate replantation is not feasible.3,4 The outcome of the functional and sensory gain of the injured hand has been well documented, including range of motion, grip power, pinch power,5 and two-point discrimination.6 However, the effects of the biomechanics of the donor foot after mGTT were scarcely addressed in the current literature with inconclusive results.
The great toe plays an important role in the push-off phase. It also provides medial stability and balance during gait.7,8 During the aforementioned phase, the second toe is also crucial to weight-bearing and contributes to balance as well.9 Therefore, the donor site selection is important due to its potential impact on the gait pattern and levels of daily activity.10 The plantar aponeurosis is a strong sheet of connective tissue spanning from the calcaneus to the bases of the proximal phalanges. When the toes are extended, the aponeurosis slides anteriorly around the metatarsal heads, thus pulling closer the calcaneus-metatarsals distance while increasing the height of the medial longitudinal arch. This action is referred to as the “windlass mechanism,” which is an important factor for energy generation for propulsion in the push-off phase.11 Thordarson et al reported that partial plantar fasciotomy decreases the arch-supporting function of the plantar fascia in addition to weakening the structure.12
Morbidity was also reported to be the highest when the great toe was transferred, followed by the combined second and third toes, and the second toe alone.1,13 Functional impairment was reported to be as high as 23.7% in a recent systemic review.10
The peak pressure (PP), measured by the electronic pedography, is an alternative measurement of intratissue loading.14 It is used to analyze the risk of developing foot ulcers in diabetic or rheumatic patients with growing popularity.15,16 Reports have shown that the second and third metatarsal heads bear the highest PP, followed by the great toe and then the heel in normal subjects.17 According to a pilot study with piezoelectric gait analysis,18 after the great or second toe was harvested, the impact load was found to shift and would concentrate on the remaining regions of the metatarsal heads. However, in a recent cadaveric study, the distribution pattern of the PP, after free second toe transfer, remained the same as the normal weight-bearing foot.19
The current study had two aims: (1) to investigate the alteration of plantar pressure profile of the donor foot after mGTT and underlying biomechanical characteristics and (2) to investigate if the windlass effect of the foot can work properly after surgery.
METHOD
Subjects
Our study was approved by the institution review board of a tertiary medical center. All subjects signed an informed consent form before participation. Totally, 20 patients who underwent mGTT between 1985 to 2014 (14 men and 6 women) and were recruited as group 1. The procedures were performed by a single experienced plastic and reconstructive surgeon. The flap design in this study was to preserve 1 cm of the proximal phalanx to maintain the attachment of the plantar aponeurosis and intrinsic muscles in the foot in an attempt to preserve the windlass effect of the plantar aponeurosis. The follow-up duration after mGTT ranged between 145 and 379 months, with an average of 243.3 months. Sixteen healthy subjects (eight men and eight women) without congenital foot deformities, foot pain in the recent 6 months, previous foot surgery, or any gait disturbances were recruited as group 2. No significant difference in age, gender, or BMI was noted between group 1 and group 2 (P > 0.05) (Table 1).
Table 1.
Demographic Data
| Group 1 (Patients with mGTT) | Group 2 (Healthy Control) | P * | ||
|---|---|---|---|---|
| Age | y | 47.5 ± 9.9 | 47.6 ± 6.5 | 0.955 |
| Gender | M/F | 14/6 | 16/16 | 0.156 |
| Height | cm | 164.6 ± 7.8 | 165.8 ± 9.6 | 0.648 |
| Weight | kg | 64.3 ± 13.3 | 61.1 ± 12.5 | 0.390 |
| BMI | kg/m² | 23.7 ± 4.3 | 22.1 ± 3.2 | 0.124 |
*P<0.05 is statistically significant. Group difference in age, body height and body mass were compared using an independent t test. Gender difference between groups were determined using a chi-square test.
F, female; M, male; mGTT, microsurgical great toe-to-hand transfer.
Clinical Foot Examination
Comprehensive foot evaluation was performed by the same experienced physician for donor foot and nondonor foot pathologies including scaring, hyperkeratosis, callus formation, fissure, and ulceration.
Taiwan Chinese Version of the Foot Function Index
Budiman et al developed the Foot Function Index (FFI) to measure foot pain and disability caused by foot and ankle pathologies.20 The FFI is a self-administered index which consists of 23 items and is divided into three subscales, consisting of pain (nine items), disability (nine items), and activity limitations (ALs; five items). The patients score each question by using the visual analogue scale from 0 (no pain or difficulty) to 10 (worst pain or difficulty). The total score ranged from 0 to 230 and a higher rating suggesting a higher degree of pain, disability or ALs. Good test–retest reliability, internal consistency and criterion validity were shown in previous studies.21 It became one of the most widely used22 patient-reported outcome measurements for foot and ankle lesions and has been successfully translated into a Chinese version in Taiwan (TCv-FFI) with satisfactory reliability and validity.23 Landdorf and Redford evaluated conservative interventions for plantar fasciitis to determine minimal important differences for the FFI. For the FFI the minimal important differences were found: 12 for pain, seven for disability, and seven for total FFI.24 Therefore, FFI was used for subjective symptom reporting in this study. The TCv-FFI scores of both group 1 and group 2 were recorded.
Plantar Pressure Measurement
The novel Emed-X System (model X; Novel GmbH, Germany) was used and incorporated the Emed-X400 platform, which consisted of a 475 mm × 320 mm sensor area with 6080 sensors at a resolution of four sensors/cm2. An applied force activated the sensors on the platform, whereas the system recorded the pressure distribution and relayed the readings to a computer.
The Emed-X400 platform was assembled in the middle of a leveled 5-m walkway. The walkway enabled pressure recording during free movement, thus minimizing the effects of acceleration and deceleration of each walk. Static measurement was performed for each patient with one foot standing on the Emed platform. The accuracy of the system is ±5% when compared with the static measurement. The Emed-X system is a traditional method for collecting data using a platform system with good reliability. A study by Hafer et al shows that inter-Emed-X correlations were greater than 0.70 in 31 and 52 of parameters when looking at a 10-trail average and a five-trail average, respectively.25
Patients were asked to walk comfortably, beginning with any foot on the platform. A total of six left and six right footsteps were recorded for each patient. The pressure measurement began when the heel made contact and stopped when the toe lifted off the platform. Measurement with incomplete foot contact was excluded and the process was repeated to obtain a complete set of 12 footsteps.
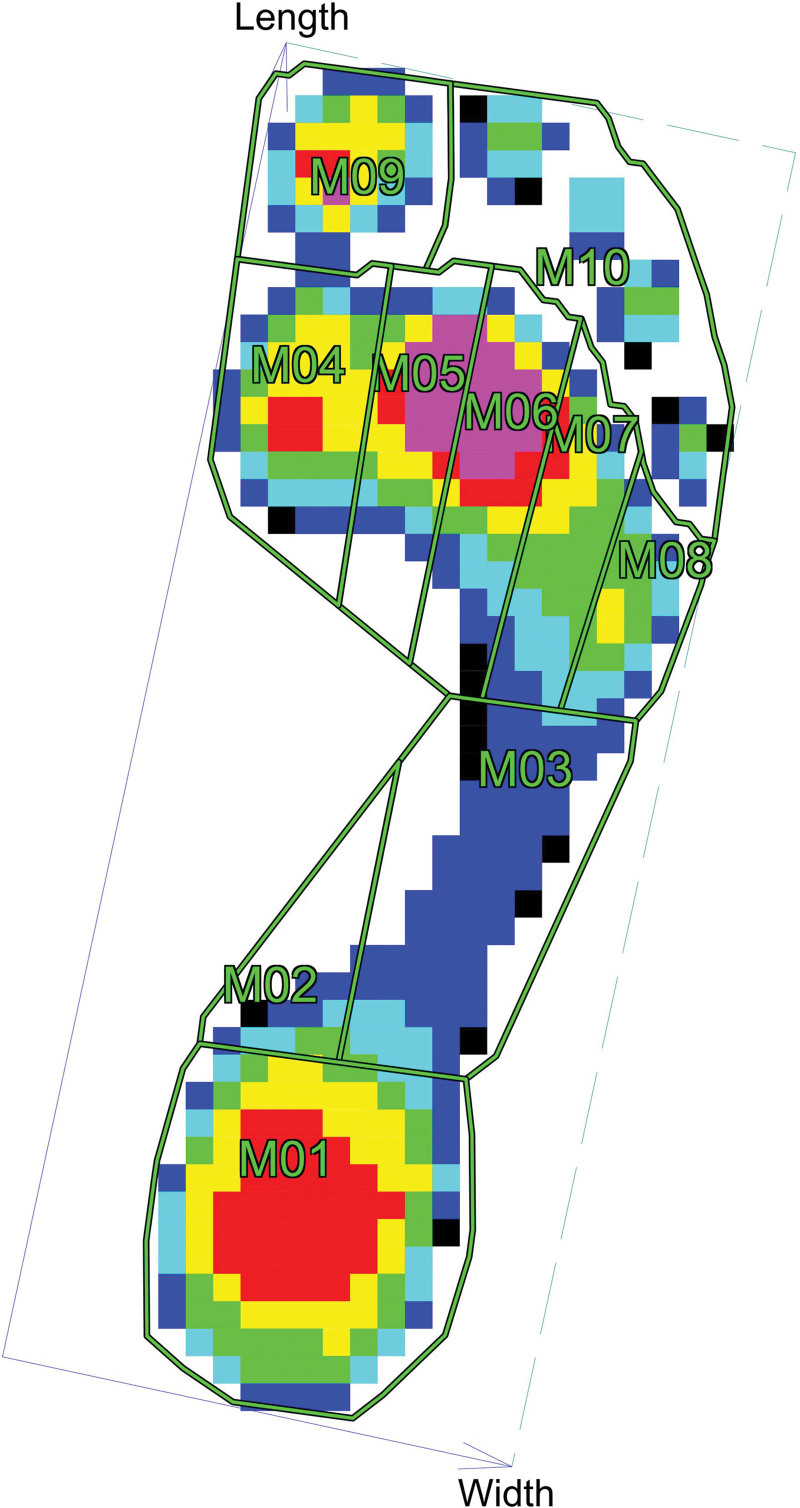
The foot was divided into 10 regions containing the heel; the medial and lateral midfoot; the first, second, third, fourth and fifth metatarsals; the great toe; and the second to fifth toes (Fig. 1). The novel Emed-X system used the software with the automasking function, where the first eight of the aforementioned regions were drawn automatically, whereas the toe regions had to be drawn manually due to deformity of the toes, especially after mGTT. Four clinically relevant parameters were investigated including the PP (kPa), contact time (CT, ms), contact area (CA, cm2), force–time integral (FTI; N s), and pressure–time integral (PTI, kPa s).
Fig. 1.
The foot was divided into 10 regions containing the heel; the medial and lateral midfoot; the first, second, third, fourth and fifth metatarsals; the great toe; and the second to fifth toes. The novel Emed-X system used the software with the automasking function, where the first eight of the aforementioned regions were drawn automatically, while the toe regions had to be drawn manually due to deformity of the toes, especially after microsurgical great toe-to-hand transfer. Four clinically relevant parameters were investigated including the PP (kPa), CT (ms), CA (cm2), FTI (N s), and PTI (kPa s).
Statistics
Data were summarized with the mean and SD rounded off to the first decimal point for the continuous variables and the number of counts for the categorical variables. The Levene test was used for the equality of variances. The independent samples t test was used to explore the variability of multiple biomechanical parameters between the donor feet and the control group. All statistical analyses were performed using the SPSS version 22.0 software package. Statistical significance was defined as a P value less than 0.05.
RESULTS
Clinical Foot Examination
Foot pathologies such as scaring, hyperkeratosis, callus formation, and fissure were observed in 80% of the patients on the stump end during comprehensive foot evaluation of the donor feet (Fig. 2). The nondonor feet did not have pathologic change.
Fig. 2.
Foot pathologies such as scarring, hyperkeratosis and fissure were observed in most of the patients on the stump end.
Taiwan Chinese Version of the FFI
The TCv-FFI data are shown in Table 2. There was no significant difference in the mean total score of the TCv-FFI between group 1 and group 2 (11.3 ± 26.7 and 2.2 ± 4.2, respectively, P > 0.05). Furthermore, all subscales of the TCv-FFI demonstrated no significant increases (P > 0.05).
Table 2.
Taiwan Chinese Version of the FFI
| Group 1 (Patients with mGTT) | Group 2 (Healthy Control) | P * | ||
|---|---|---|---|---|
| TCv-FFI | Total score | 11.3 ± 26.7 | 2.2 ± 4.2 | 0.146 |
| Pain | 4.8 ± 11.7 | 1.4 ± 2.9 | 0.220 | |
| Disability | 5.3 ± 11.3 | 0.8 ± 1.6 | 0.092 | |
| AL | 1.2 ± 4.6 | 0.0 ± 0.0 | 0.260 |
*P<0.05 is statistically significant. Comparison between patients with mGTT and control group by using student’s t-test.
mGTT, microsurgical great toe-to-hand transfer.
Plantar Pressure Measurement
Measurements of the biomechanical parameters of the foot are summarized in Table 3. There was significantly higher total foot PP (TFPP) comparing group 1 to group 2 (885.8 ± 270.2 and 692.8 ± 234.3 kPa, respectively, P < 0.05).
Table 3.
Foot Pressure Parameters of the 10 Foot Areas
| PP (kPa) | CA (cm2) | CT (ms) | PTI (kPa s) | |
|---|---|---|---|---|
| Heel | ||||
| Group 1 | 377.9 ± 154.7 | 30.6 ± 3.4 | 457.0 ± 92.0 | 98.3 ± 41.2 |
| Group 2 | 353.6 ± 87.2 | 29.6 ± 4.1 | 465.6 ± 74.6 | 93.8 ± 26.7 |
| MMF | ||||
| Group 1 | 131.7 ± 42.1* | 3.9 ± 2.7 | 406.3 ± 91.5 | 35.8 ± 12.8* |
| Group 2 | 96.5 ± 28.7 | 5.8 ± 6.4 | 393.4 ± 96.0 | 27.9 ± 11.0 |
| LMF | ||||
| Group 1 | 152.8 ± 57.9* | 20.2 ± 6.3 | 505.4 ± 104.5 | 52.6 ± 24.5* |
| Group 2 | 114.5 ± 30.4 | 20.0 ± 6.4 | 507.8 ± 111.4 | 40.4 ± 15.3 |
| MT1 | ||||
| Group 1 | 782.4 ± 319.0* | 10.1 ± 2.3* | 615.8 ± 94.8 | 221.9 ± 110.4* |
| Group 2 | 322.4 ± 163.1 | 12.2 ± 2.6 | 650.5 ± 100.6 | 102.0 ± 43.9 |
| MT2 | ||||
| Group 1 | 640.7 ± 210.7 | 8.6 ± 1.6 | 644.1 ± 104.9 | 182.0 ± 76.1 |
| Group 2 | 527.8 ± 227.2 | 9.5 ± 2.0 | 677.3 ± 105.9 | 160.7 ± 63.7 |
| MT3 | ||||
| Group 1 | 538.4 ± 140.5 | 9.9 ± 1.4 | 655.1 ± 100.6 | 153.6 ± 41.9 |
| Group 2 | 451.4 ± 201.7 | 10.3 ± 1.8 | 688.1 ± 109.9 | 145.4 ± 56.6 |
| MT4 | ||||
| Group 1 | 344.3 ± 116.7 | 8.5 ± 1.3 | 642.8 ± 96.4 | 107.7 ± 38.6 |
| Group 2 | 280.9 ± 121.0 | 8.3 ± 1.3 | 669.6 ± 110.7 | 92.9 ± 37.0 |
| MT5 | ||||
| Group 1 | 296.9 ± 212.8 | 5.5 ± 0.9* | 605.1 ± 101.5 | 92.1 ± 79.9 |
| Group 2 | 201.7 ± 154.9 | 4.9 ± 0.8 | 596.5 ± 140.0 | 63.0 ± 39.1 |
| GT | ||||
| Group 1 | 35.6 ± 54.6* | 0.3 ± 0.5* | 72.8 ± 95.6* | 5.0 ± 8.9* |
| Group 2 | 530.1 ± 254.8 | 9.0 ± 1.9 | 590.3 ± 149.4 | 145.6 ± 81.2 |
| Toe 2, 3, 4, 5 | ||||
| Group 1 | 201.6 ± 109.2 | 10.0 ± 3.2* | 509.5 ± 168.4 | 52.8 ± 31.2 |
| Group 2 | 169.9 ± 84.1 | 7.6 ± 3.9 | 473.1 ± 165.8 | 46.9 ± 31.5 |
| Total foot | ||||
| Group 1 | 885.8 ± 270.2* | 107.9 ± 16.8 | 748.9 ± 107.2 | 336.5 ± 120.3* |
| Group 2 | 692.8 ± 234.3 | 117.4 ± 23.2 | 789.3 ± 121.3 | 275.2 ± 82.9 |
P< 0.05.
GT, great toe; LMF, lateral midfoot; MF, maximal force; MMF, medial midfoot; MT1, the first metatarsal; MT2, the second metatarsal; MT3, the third metatarsal; MT4, the fourth metatarsal; MT5, the fifth metatarsal.
The PP distributions of group 1 and group 2 over heel and midfoot, metatarsal bone area, and toe area are further illustrated in Figure 2. PP concentration was noted on the residual stump end of the great toe in group 1. Comparing group 1 to group 2, there were significant increase (P < 0.05) of PP over the medial midfoot (131.7 ± 42.1 kPa), the lateral midfoot (152.8 ± 57.9 kPa), and the first metatarsal bone (782.4 ± 319.0 kPa), whereas significant decrease (P < 0.05) of PP was noted over the great toe (35.6 ± 54.6 kPa).
In group 1, the highest PP was found over the first metatarsal bone (782.4 ± 319.0 kPa), followed by the second metatarsal bone (640.7 ± 210.7 kPa), the third metatarsal bone (538.4 ± 140.5 kPa), and then the heel (377.9 ± 154.7 kPa). In contrast, in group 2, the highest PP was found over the great toe (530.1 ± 254.8 kPa), followed by the second metatarsal bone (527.8 ± 227.2 kPa), the third metatarsal bone (451.4 ± 201.7 kPa), the heel (353.6 ± 87.2 kPa), and then the first metatarsal bone (322.4 ± 163.1 kPa).
In both groups, the heel made contact with the platform with the largest CA, followed by the midfoot, and the first metatarsal head. There were significant increases (P < 0.05) of the CA over the fifth metatarsal head (5.5 ± 0.9 cm2) and the second to fifth toes (10.0 ± 3.2 cm2) in group 1. Significant decreases (P < 0.05) of the CA were recorded over the first metatarsal head (10.1 ± 2.3 cm2) and the great toe (0.3 ± 0.5 cm2) in group 1.
The mean total time foot made contact with the platform was 748.9 ± 107.2 and 789.3 ± 121.3 ms for groups 1 and 2, respectively, and there was no significant difference between groups (P > 0.05). In both groups, the third metatarsal head made the longest contact with the platform, closely followed by the fourth, second, first, and fifth metatarsal heads. The metatarsal heads of both groups were in contact with the platform for more than 80% of the total CT.
For PTI measurements, comparing group 1 to group 2, there was significant increase (P < 0.05) of PTI over the medial midfoot (35.8 ± 12.8 kPa*s), the lateral midfoot (52.6 ± 24.5 kPa*s) and the first metatarsal bone (221.9 ± 110.4 kPa*s), while significant decrease(P < 0.05) of PTI was noted over the great toe (5.0 ± 8.9 kPa*s). The highest PTI of group 1 was measured over the first metatarsal bone (221.9 ± 110.4 kPa*s). These findings were highly consistent with PP measurements.
DISCUSSION
In our study, the morbidities related to skin reactions of donor feet were higher than the literature reported.10 In one systemic review,10 scar or callus formation was developed in 6.9% of patients 64.5 months after full great toe transfer, in 4.9% of patients 24.7 months after great toe transfer with the wrap-around technique, and in 3.8% of patients 21.6 months after trimmed great toe transfer. This might indicate that longer time was needed for the foot pathologies to occur resulting from the increasing pressure buildup on the sites with both high PP and long time integral. The survey of TCv-FFI indicated that there was little or no alteration of pain, disability or ALs after mGTT. This suggested that mGTT had little negative impact on the foot functions of the vast majority of patients.
The PP has been analyzed for different foot pathologies and is clinically applicable for the detection of foot regions with a high risk of developing ulcerations in patients with diabetes or rheumatoid arthritis.15,16 It can also be used to monitor the soft tissue strain under the metatarsal head in patients with metatarsalgia wearing high-heeled shoes.14 Gait analysis of the donor foot after pollicization of the great toe was first introduced in 1988 by Mann et al, who reported the center of pressure originally at the second metatarsal head of a normal foot would lateralize to the third metatarsal head after the amputation of the great toe.7 Unlike Mann et al,7 Barca et al,18 who concluded that the gait analysis, after extended great toe-to-thumb transfer, showed an overloading of the remaining metatarsal heads without lateralization of the center of the pressure. Furthermore, Barca et al reported that the highest PP change was to the region of the third metatarsal head after second toe-to-thumb transfer.18 Recently, a cadaveric study reported the preservation of the second metatarsal after second toe-to-hand transfer helped maintained the normal distribution of the PP and there were no significant differences of the PP before and after the operation.19
Unlike Mann et al7 and Barca et al,18 our study revealed that the highest PP was measured under the first metatarsal bone. The difference might be mainly attributed to the different surgical approaches used to harvest the great toe. No increase in CA over the medial foot and first metatarsal bone in group 1 revealed the integrity of the foot arch. Hicks’ study showed that the arch can’t raise up after being cut across the plantar fascia.11 Regarding the foot arch, flatfoot is characterized with insufficiency of the medial longitudinal arch and flexible flatfoot is the most predominant type which leads to numerous clinical problems. In Tang’s study, the Emed-X system revealed that there was significantly greater CA, PP, foot maximum force, and FTI in the medial midfoot area in flexible flatfoot patients.26 From the results on the medial foot, we found that the function of the plantar aponeurosis was well preserved in our patients. The preservation of the windlass effect of the plantar aponeurosis during walking, which provided the stabilization of the curvature of the medial longitudinal arch11 and modulated the stiffness of the foot to absorb the impact from the ground reaction force against weight.27 The extended great toe transfer with the harvest of the metatarsophalangeal joint might interfere with the windlass effect of the plantar aponeurosis, which might cause more energy expenditure during walking28 Additionally, there were significant increases of the PP under the first metatarsal head and the midfoot. Overall, the redistribution of the PP to first metatarsal bone after the mGTT with intact metatarsal bone was concluded in our study.
The reference data of the biomechanical changes after mGTT regarding the CA, CT, and PTI have not been published in the previous literature. In our study, after the surgical removal of the great toe, significant decrease of the CA of the great toe was recorded. After the mGTT, the significant decrease of the CA under the first metatarsal bone resulted in a higher PP. In contrast, the significant increases of the CA of the fifth metatarsal and second to fifth toes in group 1 might indicate a higher degree of ongoing foot supination during gait. This phenomenon may be related to the nature of the patient’s foot to avoid further foot pressure concentration over the stump end. The gait asymmetry with high stance time variability was reported to be strongly correlated with falls in older patients,28 patients with ambulatory stroke29 and patients with Parkinson disease.30There was no significant difference of total foot CT between groups, which might suggest that the mGTT would not alter the foot clearance efficiency. The PTI described the cumulative plantar load over time and might play an important role in assessing the risk for developing skin trauma and underlying tissue damage.31 In this study, the PTI was the highest under the first metatarsal bone and significantly increased in the midfoot of group 1. This might suggest that more caution should be paid toward these areas after harvesting the toe flap in prevention of developing foot pathologies over time. Our study has its limitations. The broad range of the follow-up time after mGTT may increase the biomechanical variability due to the chronological adaptation of the feet. Furthermore, the sample size was relatively small; a larger sample size should be included in future study with regular follow-up.
In summary, the windlass effect of the foot will not be affected when performing mGTT with preservation of 1 cm of the proximal phalanx. The redistribution of the PP and PTI to first metatarsal bone after the mGTT was concluded in our study. The foot pathology was well correlated to the PP point. Through better understanding of the distribution pattern of the PP, proper insole design for pressure relief could be hugely facilitated.
DISCLOSURES
This study was supported by Minister of Science and Technology, Taiwan, R.O.C. (Grant number: 110WHK0510154), Chang Gung Medical Foundation (Grant number: CMRPG3G1422), and Lo Hsu Medical Foundation. The other authors have no financial interest to declare.
Footnotes
Published online 1 September 2023.
Disclosure statements are at the end of this article, following the correspondence information.
Drs Tang and Tang contributed equally to this work.
REFERENCES
- 1.Buncke HJ, Jr, Buncke CM, Schulz WP. Immediate nicoladoni procedure in the rhesus monkey, or hallux-to-hand transplantation, utilising microminiature vascular anastomoses. Br J Plast Surg. 1966;19:332–337. [DOI] [PubMed] [Google Scholar]
- 2.Cobbett JR. Free digital transfer. Report of a case of transfer of a great toe to replace an amputated thumb. J Bone Joint Surg Br. 1969;51:677–679.. [PubMed] [Google Scholar]
- 3.Ray EC, Sherman R, Stevanovic M. Immediate reconstruction of a nonreplantable thumb amputation by great toe transfer. Plast Reconstr Surg. 2009;123:259–267. [DOI] [PubMed] [Google Scholar]
- 4.Lam WL, Wei FC. Toe-to-hand transplantation. Clin Plast Surg. 2011;38:551–559. [DOI] [PubMed] [Google Scholar]
- 5.Chung KC, Wei FC. An outcome study of thumb reconstruction using microvascular toe transfer. J Hand Surg. 2000;25:651–658. [DOI] [PubMed] [Google Scholar]
- 6.Wei FC, Chen HC, Chuang CC, et al. Simultaneous multiple toe transfers in hand reconstruction. Plast Reconstr Surg. 1988;81:366–377. [DOI] [PubMed] [Google Scholar]
- 7.Mann RA, Poppen NK, O’Konski M. Amputation of the great toe. A clinical and biomechanical study. Clin Orthop Relat Res. 1988:192–205. [PubMed] [Google Scholar]
- 8.Yang XB, Gu YD. The donor foot in free toe or joint transfers. J Hand Surg (Edinburgh, Scotland). 2000;25:382–384. [DOI] [PubMed] [Google Scholar]
- 9.Bhutta MA, Chauhan D, Zubairy AI, et al. Second metatarsophalangeal joint instability and second metatarsal length association depends on the method of measurement. Foot Ankle Int. 2010;31:486–491. [DOI] [PubMed] [Google Scholar]
- 10.Sosin M, Lin CH, Steinberg J, et al. Functional donor site morbidity after vascularized toe transfer procedures: a review of the literature and biomechanical consideration for surgical site selection. Ann Plast Surg. 2016;76:735–742. [DOI] [PubMed] [Google Scholar]
- 11.Hicks JH. The mechanics of the foot. J Anat. 1954;88:25–30. [PMC free article] [PubMed] [Google Scholar]
- 12.Thordarson DB, Kuma PJ, Hedman TP, et al. Effect of partial versus complete plantar fasciotomy on the windlass mechanism. Foot ankle Int. 1997;18:16–20. [DOI] [PubMed] [Google Scholar]
- 13.NF AL, Lin YT, Wei FC. Metacarpal-like and metacarpal hand. Hand Clin. 2016;32:549–554. [DOI] [PubMed] [Google Scholar]
- 14.Ko PH, Hsiao TY, Kang JH, et al. Relationship between plantar pressure and soft tissue strain under metatarsal heads with different heel heights. Foot Ankle Int. 2009;30:1111–1116. [DOI] [PubMed] [Google Scholar]
- 15.Driver VR, Fabbi M, Lavery LA, et al. The costs of diabetic foot: the economic case for the limb salvage team. J Vasc Surg. 2010;52:17S–22S. [DOI] [PubMed] [Google Scholar]
- 16.Scalpello A, Gatt A, Chockalingam N. A pilot comparison of forefoot plantar pressures in newly diagnosed rheumatoid arthritis patients and non-rheumatic subjects. Foot (Edinburgh, Scotland). 2013;23:120–122. [DOI] [PubMed] [Google Scholar]
- 17.Putti AB, Arnold GP, Cochrane LA, et al. Normal pressure values and repeatability of the Emed ST4 system. Gait Posture. 2008;27:501–505. [DOI] [PubMed] [Google Scholar]
- 18.Barca F, Santi A, Tartoni PL, et al. Gait analysis of the donor foot in microsurgical reconstruction of the thumb. Foot Ankle Int 1995;16:201–206. [DOI] [PubMed] [Google Scholar]
- 19.Li B, Chen DW, Yang YF, et al. Effect of second toe-to hand transfer on the plantar pressure distribution of the donor foot. Acta Orthoedica Brasileira. 2016;24:39–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Budiman-Mak E, Conrad KJ, Roach KE. The foot function index: a measure of foot pain and disability. J Clin Epidemiol. 1991;44:561–570. [DOI] [PubMed] [Google Scholar]
- 21.Saag KG, Saltzman CL, Brown CK, et al. The foot function index for measuring rheumatoid arthritis pain: evaluating side-to-side reliability. Foot Ankle Int. 1996;17:506–510. [DOI] [PubMed] [Google Scholar]
- 22.Lau JT, Mahomed NM, Schon LC. Results of an internet survey determining the most frequently used ankle scores by AOFAS members. Foot Ankle Int. 2005;26:479–482. [DOI] [PubMed] [Google Scholar]
- 23.Wu SH, Liang HW, Hou WH. Reliability and validity of the Taiwan Chinese version of the foot function index. J Formos Med Assoc. 2008;107:111–118. [DOI] [PubMed] [Google Scholar]
- 24.Landorf KB, Radford JA. Minimal important difference: values for the foot health status questionnaire, foot function index and visual analogue scale. Foot. 2008;18:15–19. [Google Scholar]
- 25.Hafer JF, Lenhoff MW, Song J, et al. Reliability of plantar pressure platforms. Gait Posture. 2013;38:544–548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Tang AC, Wu HM, Chen CK, et al. Plantar pressure distribution in patients with flexible flatfoot: measured by platform system and in-shoe system. Tw J Phys Med Rehabil. 2017;45:57–65.. [Google Scholar]
- 27.Song S, LaMontagna C, Collins SH, et al. The effect of foot compliance encoded in the windlass mechanism on the energetics of human walking. Conference proceedings: Annual International Conference of the IEEE Engineering in Medicine and Biology Society IEEE Engineering in Medicine and Biology Society Annual Conference 2013; 2013: 3179–3182. [DOI] [PubMed] [Google Scholar]
- 28.Hughes J, Clark P, Linge K, et al. A comparison of two studies of the pressure distribution under the feet of normal subjects using different equipment. Foot Ankle. 1993;14:514–519. [DOI] [PubMed] [Google Scholar]
- 29.Hutton WC, Dhanendran M. The mechanics of normal and hallux valgus feet--a quantitative study. Clin Orthop Relat Res. 1981:7–13. [PubMed] [Google Scholar]
- 30.Sauseng S, Kastenbauer T, Sokol G, et al. Estimation of risk for plantar foot ulceration in diabetic patients with neuropathy. Diabetes Nutr Metab. 1999;12:189–193. [PubMed] [Google Scholar]
- 31.Maki BE. Gait changes in older adults: predictors of falls or indicators of fear. J Am Geriatr Soc. 1997;45:313–320. [DOI] [PubMed] [Google Scholar]