Summary
This study aimed to investigate the significance of Hill classification to predict esophagitis, Barrett’s esophagus, gastroesophageal reflux disease (GERD) symptomatology, and future prescriptions of proton pump inhibitors in clinical practice. A total of 922 patients (546 women and 376 men; mean age 54.3 [SD 18.4] years) who underwent gastroscopy between 2012 and 2015 were analyzed. Patient questionnaire regarding symptoms were compared with endoscopy findings. A medical chart review was done that focused on the prescription of PPIs, additional gastroscopies, and GERD surgery in a 3-year period before the index gastroscopy and in a 6-year period afterward. In patients naïve to PPI prescriptions (n = 466), Hill grade III was significantly associated with esophagitis (AOR 2.20; 95% CI 1.00–4.84) and > 2 PPI prescriptions 6 year after the index gastroscopy (AOR 1.95; 95% CI 1.01–3.75), whereas Hill grade IV was significantly associated with esophagitis (AOR 4.41; 95% CI 1.92–10.1), with Barrett’s esophagus (AOR 12.7; 95% CI 1.45–112), with reported heartburn (AOR 2.28; 95% CI 1.10–4.74), and with >2 PPI prescriptions (AOR 2.16; 95% CI 1.02–4.55). In patients ‘non-naïve’ to PPI prescription (n = 556), only Hill grade IV was significantly associated with esophagitis, reported heartburn, and with >2 PPI prescriptions. The gastroscopic classification in Hill grades III and IV is important in clinical practice because they are associated with esophagitis, Barrett’s esophagus, symptoms of GERD, and prescriptions of PPIs, whereas a differentiation between Hill grades I and II is not.
Keywords: esophagitis, gastroesophageal reflux disease, gastroscopy, Hill grade, proton pump inhibitor
INTRODUCTION
Gastroesophageal reflux disease (GERD) is one of the most prevalent chronic gastrointestinal (GI) diseases globally with a prevalence of ~20%.1,2,3 In clinical praxis, esophagogastroduodenoscopy (gastroscopy) is the most important medical investigation for patients with the suspicion of GERD, which enables thorough the investigation of signs of esophagitis and Barrett’s esophagus and an evaluation of the gastroesophageal valve.
The competence of the gastroesophageal flap valve is an important anatomical key to prevent reflux of gastric contents into the esophagus. Hiatal hernia is a common finding in patients with GERD and is characterized by a herniation of the stomach through the esophageal hiatus into the mediastinum.4 Hiatal hernia is often categorized using the axial length of the hiatal hernia in centimeters (cm).5 The interobserver agreement of the endoscopic length measurements during endoscopy is in general poor.6 A thorough evaluation of the gastroesophageal junction including the lower esophagus sphincter (LES), the crural fibers of the diaphragm, and the gastroesophageal flap valve is therefore important.7 The Hill classification is a validated method to evaluate the gastroesophageal flap valve in gastroscopies.7 It is simple and reproducible when evaluating patients with suspicion of GERD at gastroscopy in clinical practice.8 In the Hill classification, the gastroesophageal flap valve is graded from I to IV and a higher Hill grade has been associated with the prevalence of GERD,8,9 hiatal hernia,10 and lower pressure in the lower esophageal sphincter (LES). In addition, Hill’s classification has been shown to be a better predictor of reflux than the LES pressure7 and the Hill classification has been shown to be associated with GERD at least as strongly as the axial length of a hiatal hernia.11
Although, the Hill classification is commonly used in clinical practice, firm knowledge is lacking concern to what extent different Hill grades affect the patient symptoms, their clinical outcome, and the patients use of proton-pump inhibitors.12 The aim of this study was to see how patients with different Hill grades report upper GI symptoms, if Hill grade is associated with gastroscopy findings, and/or with the number of long-term PPI prescriptions.
PATIENTS AND METHODS
Patients
A questionnaire was given to out-patients ≥ 18 years old, between May 2012 and 2015 when attending drop-in gastroscopy at Umeå University Hospital to be answered in the waiting room. The questionnaire also included a protocol on findings during gastroscopy to be completed by the doctor. Follow-up medical chart review was done at death or 6 years after gastroscopy. Excluded at follow-up were patients with incomplete data after 6 years (Fig. 2).
Fig. 2.
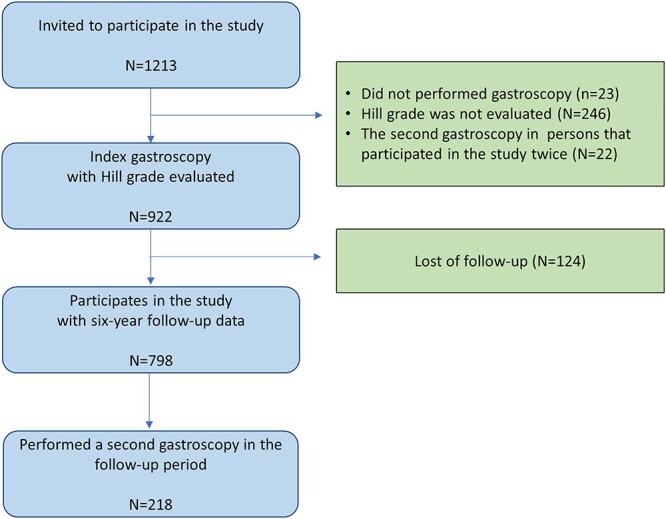
Description of included and excluded patients in the study.
Patient questionnaire
The questionnaire included the GerdQ13 with questions of heartburn, regurgitation of stomach contents, nausea, and epigastric pain. The questions in GerdQ are constructed as a four-graded Likert scale with no symptoms, symptoms on 1, 2–3, or 4–7 days the last week. In addition, a question on smoking was included in the questionnaire.
Endoscopic findings
Blinded from the answers from the patient’s questionnaires, an experienced endoscopist filled in a questionnaire that included findings on the gastroscopy. Images showing the Hill grade and the Los Angeles classification14 were available to the endoscopist at the room where the gastroscopy was performed. To be classified with Hill grade I, the prominent fold of tissue along with the lesser curvature encloses the gastroscope. In Hill grade II, the fold is present, but there are periods of opening and rapid closing around the gastroscope. In Hill grade III, the fold is barely present, and there is failure to close around the gastroscope, and in Hill grade IV, the fold is absent and there is an open space around the gastroscope, and a hiatus hernia is always present (Fig. 1).7 The endoscopist filled in a standardized questionnaire that included, among other things, Hill’s classification with grades from I to IV, the presence of macroscopic Barrett’s esophagus (defined by Prague classification C > 3 cm),15 and esophagitis (according to the Los Angeles classification system, with grades from A through D).
Fig 1.
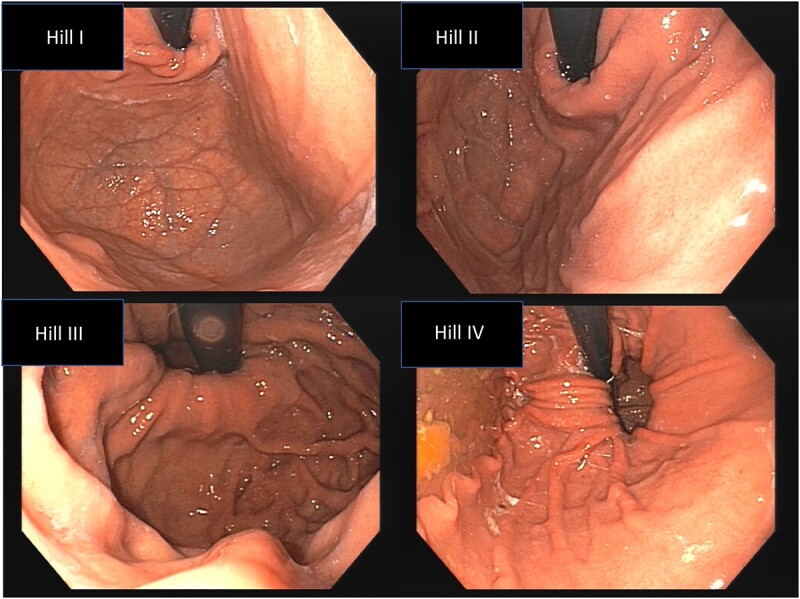
Endoscopic images of Hill grade I (A), Hill grade II (B), Hill grade III (C), and Hill grade IV (D).
Medical chart review
The Region of Västerbotten uses a single and cohesive medical chart computerized system in which all notes on patient health-related contacts including endoscopy, surgery, and all prescriptions of medications are recorded. Blinded from the data from the questionnaires, a medical chart review was performed that focuses on the prescription of PPIs, the presence and outcome of additional gastroscopies, and referral for GERD surgery in a 3-year period before, and a 6-year period after the index gastroscopy. We recorded the number of prescription of PPIs 3 years before and 6 years after the gastroscopy. We also recorded the prescribed cumulative dose (in omeprazole equivalents)16 in the 6-year follow-up period.
Statistical analysis
Statistical Package for the Social Sciences, version 26.0, has been used for the statistics. Pearson’s chi2 test (or Fisher’s Exact test when appropriate) was used to compare categorical data. Student’s t-test and Mann–Whitney test were used to compare means and medians. Bivariate correlations were tested using Spearman’s test. The significance level was set at a P-value of 0.05. To adjust for possible confounding of factors associated with GERD, we used logistic regression with dependent variables for PPI prescription (> median prescriptions), findings of any esophagitis or Barrett’s esophagus on gastroscopy, and any reported GERD symptom on the patient questionnaire. The independent variables were age, female gender, BMI > 30 kg/m,2 and Hill grade (reference Hill grade I).
Ethics
The study was approved by the Ethical Board, Umeå, Dnr 2011-160-31M. All patients that were included in the study gave their informed consent to participate.
RESULTS
Invited were 1213 patients attending the hospital for drop-in gastroscopy between May 2012 and 2015. All patients answered the questionnaire. Twenty-two patients attended twice, and the second gastroscopy was regarded as follow-up. Gastroscopy was not done in 23 patients. A Hill grade was not recorded in another 246 patients, leaving 922 patients including in the data analysis (Fig. 2). Ten experienced doctors performed the gastroscopies.
Basal characteristics of the patients referred for gastroscopy
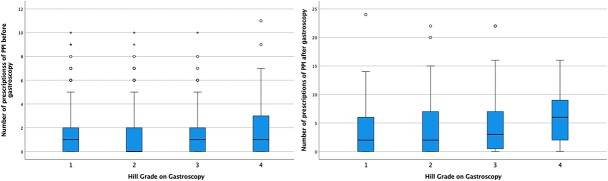
Table 1 shows the basal characteristics of the 922 patients included in the data analysis. There was a significantly higher proportion of women than men that participated in the study (P < 0.001). Approximately half of the patients had any PPI prescribed 3 years before the index gastroscopy. The median number of prescriptions of PPIs in the 3-year period before the index gastroscopy was for patients with Hill grade I, 1.0 (25th–75th percentile 0–2.0), Hill grade II, 0 (0–2.0), Hill grade III, 1.0 (0–2.0), and for patients with Hill grade IV, 1.0 (0–3.0) (Fig. 3). There were no significant differences in the number of prescriptions before gastroscopy between patients with different Hill grades except for patients with Hill grade IV versus Hill grade II (P = 0.017).
Table 1.
Basic characteristics of patients included in the study (n = 922). Proportions are presented as percent, means with standard deviation,11 and medians with 25th–75th percentile
| Gender | Women Men |
59.2% 40.8% |
|---|---|---|
| Age at index gastroscopy, years | Mean Median |
54.3 (18.4) 58.0 (38–69) |
| Body mass index, kg/m2 | ≤25 >25 >30 Mean |
50.7% 49.3% 14.5% 25.5 (4.6) |
| Current smokers (n = 916) | Yes No |
7.1% 92.9% |
| Any prescription of proton pump inhibitors 3 years before the index gastroscopy (n = 798) | Yes No |
54.3% 45.7% |
| Number of prescriptions of proton pump inhibitors 3 years before the index gastroscopy (n = 798) | Mean Median |
1.38 (1.88) 1 (0–2) |
Fig. 3.
The number of prescriptions of PPIs in the 3-year period before the index gastroscopy and in the 6-year follow-up period after the index gastroscopy.
The median number of prescriptions for PPIs 3 years before the index gastroscopy was significantly higher among women than men (1.0 vs 0.0, P < 0.001).
The association between Hill grade and findings on the index gastroscopy
Table 2 presents the prevalence of reported findings on the index gastroscopy. Approximately one-third of the patients had at least one clinically relevant pathological finding at their index gastroscopy. The proportion of patients with esophagitis and Barrett’s esophagus for Hill grades I–IV are shown in Figures 4 and 5. The patients with Hill grade IV had significantly more often esophagitis compared with the patients with Hill grade I (40.5 vs 11.9%; P < 0.001), Hill grade II (40.5 vs 18.4%; P < 0.001), and Hill grade III (40.5 vs 21.4%; P < 0.001). Patients with Hill grade II (18.4 vs 11.9%; P = 0.41) and Hill grade III (21.4 vs 11.9%; P = 0.05) had significantly more often esophagitis on the index gastroscopy than patients with Hill grade I, but there were no differences between patients with Hill grades II and III (P = 0.393).
Table 2.
Findings on the index gastroscopy
| Hill grade (n = 922) | I II III IV |
26.5% 29.5% 26.9% 17.1% |
|---|---|---|
| Any pathological findings (n = 922) | Yes No |
28.0% 72.6% |
| Esophagitis (n = 872)† | Grade A Grade B Grade C Grade D No |
8.4% 6.0% 1.8% 0.6% 83.3% |
| Barrett’s esophagus (n = 920) | Yes No |
4.3% 95.7% |
†Los Angeles classification system.
Fig. 4.
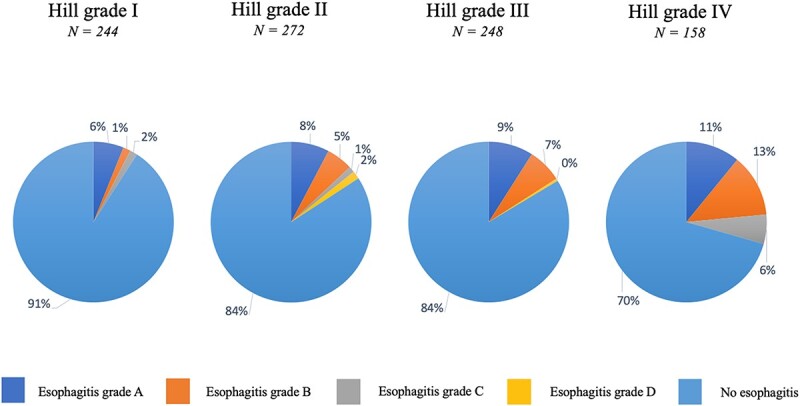
Association between Hill grade and esophagitis (Los Angeles classification) at the index gastroscopy.
Fig. 5.
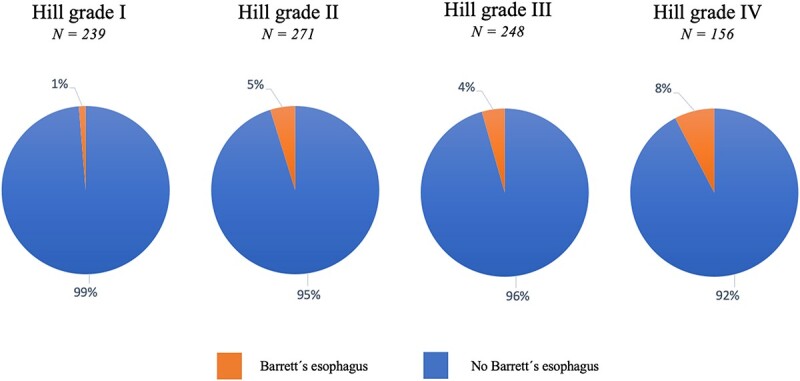
Association between Hill grade and Barrett’s esophagus at the index gastroscopy.
The proportion of patients with Barrett’s esophagus was significantly higher in the Hill IV group compared with the Hill I group (8.2 vs 1.6%; P = 0.002), but there were no significant differences between the other Hill grade groups. Correlations between Hill grade and age, body mass index, esophagitis, and Barrett’s esophagus are shown in Table 3.
Table 3.
Spearman correlations for Hill grade and age, body mass index, reported symptoms, findings on the index gastroscopy, and number of proton pump inhibitor12 prescriptions. Data are presented for all Hill grades and when Hill grade IV is excluded
| Hill grades I–IV | Hill grades I–III | |
|---|---|---|
| Age | 0.081* | 0.033 |
| Body Mass Index | 0.081* | 0.006 |
| Esophagitis† at the index gastroscopy | 0.207** | 0.093* |
| Barrett’s esophagus at the index gastroscopy | −0.009 | 0.068 |
| Reported heartburn | 0.104** | 0.023 |
| Reported regurgitation | 0.034 | 0.023 |
| Reported epigastralgia | −0.077* | −0.059 |
| Number of PPI prescriptions 3 years before the index gastroscopy | 0.062 | 0.015 |
| Number of PPI prescriptions 6 years after the index gastroscopy | 0.172** | 0.068 |
| Cumulative dose of prescribed omeprazole equivalents 6 years after the index gastroscopy | 0.216** | 0.098* |
* P < 0.05; **P < 0.01.
†Los Angeles classification system.
The association between Hill grade and reported GI symptoms
The proportions of patient-reported GI symptoms for different Hill grades are shown in Supplementary Table 1. There was a significant correlation between increasing Hill grade and the frequency of reported symptoms of heartburn (Table 3) and a weak negative correlation between increasing Hill grade and the frequency of reported epigastric pain (Table 3). When excluding patients with Hill grade IV, there were no significant correlations between Hill grade and reported symptoms (Table 3).
Referral to gastroscopy and prescription of PPI in the follow-up period
Of the 922 patients included in the data analysis, 124 patients moved to another region during the 6-year follow-up period and were excluded in the follow-up analysis (Fig. 2). Forty-four patients deceased in the 6-year observation period. The mean observation time for the 798 patients included in the follow-up analysis was 70 months (SD 10 months).
A total of 75.7% of patients received a prescription of PPIs at least once within the 6-year follow-up period. The median number of prescriptions of PPIs in the 6-year follow-up period was for all patients, 3 (25th–75th percentile 0–6), for patients with Hill grade I, 2 (0–6), Hill grade II, 2 (0–7), Hill grade III, 3 (0–7), and for patients with Hill grade IV, 6 (1.5–9) (Fig. 3).
The median number of prescriptions of PPI within the 6-year follow-up period was significantly higher among the patients with Hill grade IV compared with the other Hill groups (6 vs 2 prescriptions, P < 0.001), but there was no difference between patients with Hill grades I–III (Fig. 3). There was a significantly positive correlation between Hill grade with the number of PPI prescriptions and prescribed cumulative dose of omeprazole equivalents but when excluding patients with Hill grade IV there was no significant correlation in the number of PPI prescriptions (Table 3).
The prescribed median cumulative dose of omeprazole equivalents at 6 years after the gastroscopy was 3200 mg (0–21,850 mg) for patients with Hill grade I, 6800 mg (0–32,320 mg) for patients with Hill grade II, 7840 mg (0–43,800 mg) for patients with Hill grade III, and 30080 mg (5880–43,800 mg) for patients with Hill grade IV. The median cumulative dose of omeprazole equivalents for patients with Hill grade IV was significantly higher than for patients with Hill grade III (P < 0.001), Hill grade II (P < 0.001), and Hill grade I (P < 0.001). The median cumulative dose of omeprazole equivalents given to patients with Hill grade III was significantly higher than for patients with Hill grade I (P = 0.013), whereas there was no difference between patients with Hill grades III and II (P = 0.459) or between patients with Hill grades II and I (P = 0.051).
The median number of PPI prescriptions in the 6-year follow-up period was significantly higher among women than men (3 vs 2 prescriptions, P = 0.011), but there were no gender differences in patients who were ‘naïve’ to PPI prescriptions before the index gastroscopy (0 vs 0; P = 0.715).
In the 6-year follow-up period after the index gastroscopy, 27.8% of the patients had an additional gastroscopy. Totally, 3.6% of the patients had a new diagnosis of esophagitis and 2.3% of the patients had a new diagnosis of Barrett’s on the gastroscopy in the follow-up period. In total, six patients (0.7%) underwent surgery because of GERD in the follow-up period. Of these six patients, one patient had Hill grade I, two patients Hill grade II, two patients Hill grade III, and one patient Hill grade IV on the index gastroscopy.
Patients who at the index gastroscopy were classified to Hill grade IV significantly more often had an additional gastroscopy in the 6-year follow-up period compared with patients classified with Hill grades I–III (38.3 vs 25.0%, P = 0.001). Patients with Hill grade IV significantly more commonly were diagnosed with esophagitis (8.5 vs 2.7%, P = 0.001) and Barrett’s esophagus (5.0 vs 2.0%, P = 0.04) on gastroscopy in the follow-up period. There were no significant differences between patients with Hill grades III and I–II in for a new diagnosis of esophagitis and Barrett’s esophagus.
Patients who were ‘naïve’ to PPI prescriptions
We performed a logistic regression analyzing separately patients who were ‘naïve’ for PPI prescription and patients who were ‘non-naïve’ for PPI prescription before the index gastroscopy (Table 4). For patients who were ‘naïve’ for PPI prescriptions, BMI > 30 and Hill grades III and IV were significantly associated with esophagitis on the index gastroscopy. Hill grade IV were significantly associated to Barrett’s esophagus and to reported heartburn at the index gastroscopy. Hill grades III and IV were also significantly associated to PPI prescription in the follow-up period. BMI > 30 was significantly associated with reported regurgitation at the index gastroscopy and was significantly associated with prescriptions of PPI in the follow-up period. Females ‘naïve’ to PPI prescription had significantly more reported epigastric pain than men.
Table 4.
Logistic regression showing how age, gender, body mass index, and Hill grade effect on endoscopic findings, symptoms of GERD, and proton pump inhibitor prescriptions in patients referred to gastroscopy
| Dependent variable | Independent variable | All patients (n = 1022) Adjusted OR (CI 95%) |
Patients naïve for proton pump inhibitors prescriptions (n = 466) Adjusted OR (CI 95%) |
Patients non-naïve for proton pump inhibitors prescriptions (n = 556) Adjusted OR (CI 95%) |
|---|---|---|---|---|
| Any esophagitis at the | Age | 1.01 (0.99–1.02) | 1.00 (0.99–1.02) | 1.01 (0.99–1.03) |
| index gastroscopy | Female gender | 0.78 (0.56–1.08) | 0.62 (0.36–1.04) | 0.97 (0.58–1.61) |
| BMI > 30 | 2.08 (1.37–3.17) | 2.21 (1.14–4.30) | 2.12 (1.17–3.83) | |
| Hill II | 1.63 (0.98–2.70) | 1.32 (0.61–2.87) | 2.05 (0.96–4.39) | |
| Hill III | 2.08 (1.26–3.43) | 2.20 (1.00–4.84) | 1.96 (0.89–4.30) | |
| Hill IV | 4.45 (2.67–7.43) | 4.41 (1.92–10.1) | 4.62 (2.18–9.82) | |
| Hill I (reference) | ||||
| Any Barrett’s | Age | 1.03 (1.01–1.05) | 1.00 (0.97–1.04) | 1.04 (1.00–1.07) |
| esophagus at the | Female gender | 1.02 (0.53–1.95) | 1.51 (0.45–5.03) | 0.67 (0.30–1.53) |
| index gastroscopy | BMI > 30 | 0.93 (0.37–2.30) | 0.34 (0.04–2.81) | 1.34 (0.47–3.82) |
| Hill II | 2.79 (0.89–8.71) | 2.96 (0.37–27.0 | 2.68 (0.70–10.3) | |
| Hill III | 2.33 (0.71–7.59) | 0.97 (0.06–15.8) | 3.16 (0.81–12.3) | |
| Hill IV | 4.59 (1.46–14.5) | 12.7 (1.45–112) | 1.81 (0.42–7.88) | |
| Hill I (reference) | ||||
| Heartburn at least | Age | 1.00 (0.99–1.01) | 1.01 (0.99–1.02) | 0.99 (0.98–1.01) |
| once a week | Female gender | 1.30 (0.99–1.73) | 1.17 (0.76–1.81) | 1.61 (1.04–2.48) |
| BMI > 30 | 1.29 (0.86–1.93) | 1.60 (0.85–3.02) | 1.15 (0.64–2.04) | |
| Hill II | 1.21 (0.84–1.73) | 1.35 (0.78–2.35) | 1.03 (0.59–1.78) | |
| Hill III | 1.33 (0.92–1.93) | 1.61 (0.88–2.94) | 1.21 (0.68–2.14) | |
| Hill IV | 2.40 (1.52–3.79 | 2.28 (1.10–4.74) | 2.16 (1.12–4.16) | |
| Hill I (reference) | ||||
| Regurgitation at least | Age | 1.00 (0.99–1.01) | 1.00 (0.99–1.02) | 1.00 (0.99–1.02) |
| once a week | Female gender | 1.52 (1.16–2.00) | 1.20 (0.77–1.84) | 1.89 (1.24–2.90) |
| BMI > 30 | 2.58 (1.69–3.96) | 3.39 (1.74–6.60) | 1.90 (1.04–3.47) | |
| Hill II | 1.02 (0.71–1.47) | 1.19 (0.68–2.09) | 1.04 (0.60–1.83) | |
| Hill III | 1.18 (0.82–1.71) | 1.77 (0.96–3.25) | 0.96 (0.54–1.69) | |
| Hill IV | 1.03 (0.67–1.58) | 0.84 (0.41–1.71) | 1.40 (0.74–2.62) | |
| Hill I (reference) | ||||
| Epigastric pain at least | Age | 1.00 (0.99–1.01) | 0.99 (0.98–1.01) | 0.99 (0.98–1.01) |
| once a week | Female gender | 1.52 (1.16–2.00) | 2.02 (1.24–3.29) | 2.59 (1.55–4.31) |
| BMI > 30 | 1.14 (0.72–1.81) | 1.27 (0.62–2.59) | 0.92 (0.47–1.80) | |
| Hill II | 0.82 (0.53–1.27) | 0.74 (0.38–1.44) | 0.70 (0.34–1.42) | |
| Hill III | 0.82 (0.52–1.28) | 0.74 (0.36–1.51) | 0.75 (0.36–1.57) | |
| Hill IV | 0.76 (0.46–1.24) | 0.48 (0.22–1.06) | 0.85 (0.39–1.85) | |
| Hill I (reference) | ||||
| Three or more | Age | 1.03 (1.01–1.05) | 1.03 (1.01–1.04) | 1.04 (1.03–1.06) |
| proton pump inhibitor | Female gender | 1.57 (1.15–2.14) | 1.04 (0.65–1.65) | 1.77 (1.12–2.82) |
| prescriptions | BMI > 30 | 1.91 (1.25–2.90) | 2.46 (1.33–4.54) | 1.58 (0.86–2.92) |
| 6 years after the index gastroscopy | Hill II | 1.21 (0.81–1.88) | 1.31 (0.70–2.46) | 1.28 (0.72–2.92) |
| Hill III | 1.48 (0.97–2.25) | 1.95 (1.01–3.78) | 1.23 (0.68–2.22) | |
| Hill IV | 2.38 (1.48–3.84) | 2.16 (1.02–4.55) | 2.56 (1.29–5.10) | |
| Hill I (reference) |
BMI, body mass index, kg/m.2 Bold text = Statistically significant
Patients who had previously been prescribed PPIs
For patients who had received at least one prescription of PPI in the 3-year period before the index gastroscopy (‘non-naïve’ to PPI), Hill grade IV was significantly associated with reported heartburn and esophagitis on the index gastroscopy and significantly associated with PPI prescription in the follow-up period (Table 4). There was no significant association between Hill grades III and II for findings on gastroscopy, reported symptoms, or PPI prescriptions in comparison patients with Hill grade I. BMI > 30 was significantly associated with esophagitis and reported regurgitation in the non-naïve for PPI patients. Female gender significantly associates with reported heartburn, reported regurgitation, reported epigastric pain, and long-term PPI prescriptions.
Increasing age was significantly associated with PPI prescription in the follow-up period independently of patients were naïve and non-naïve for PPI prescription before the index gastroscopy.
DISCUSSION
The main finding was that Hill grades III and IV were associated with esophagitis and long-term PPI prescriptions at follow-up. Patients classified to Hill grade IV significantly more often had an additional gastroscopy in the 6-year follow-up period, and they more often had a new diagnosis of esophagitis and Barrett’s esophagus on the second gastroscopy. In clinical practice, our data suggest that defining Hill grades III and IV is important to prevent complications of gastroesophageal reflux and to predict the need of further PPI, whereas differentiation of Hill grade I from Hill grade II was not important.
Our study supports a previous study that patients with an abnormal gastroesophageal flap valve more often have symptoms of GERD.17 However, in our study when adjusting for age, gender, and BMI, the frequency of heartburn was only associated with Hill grade, and only with Hill grade IV, whereas regurgitation or epigastric pain was not. This finding indicates that the presence of gastroesophageal valve with Hill grades I to III is of low importance in generating symptoms typically for GERD.
Xirouchakis et al.18 found that patients with symptomatic GERD and with Hill grade IV needed significantly more prescriptions of PPI during a 3-month period with on-demand therapy compared with Hill grades II and III. In the present study, patients with Hill grades III and IV had received more prescriptions of PPIs within the follow-up period compared with the other Hill grade groups, but there was no significant difference in the number of prescriptions between the patients with Hill grades I–III in patients non-naïve to PPI.
The main strength of our study was the relatively large cohort of clinical practice. In addition, at the time of the study, all gastroscopies in the catchment area were performed at only one endoscopic unit. In the Region of Västerbotten, all patient’s prescriptions are registered in a medical record system. Data are collected from a period of 9 years with a 3-year retrospective study, a cross-sectional study, and a 6-year follow-up study, which give a long range of follow-up and more information about the patients and their possible GERD complications, symptoms, and PPI prescriptions. Furthermore, the endoscopists who performed the gastroscopy were experienced and graded the patients’ gastroesophageal flap valve by using a standardized picture on the wall in the endoscopic room showing the different Hill grades. The endoscopist was also blinded to the patient questionnaire when evaluating the gastroscopy findings.
However, there are also some limitations. First, in Sweden, PPIs and antacids are also available without a doctor prescription in small packages (20 tablets) over the counter (OTC), and in this current study, we do not have information of to what extent the participants used OTC PPIs in the follow-up period. In Sweden, PPIs on prescriptions are much cheaper than OTC PPIs. Therefore, one can assume that patients who need frequent use of PPIs contact their doctor for a prescription. Second, patients were asked about the frequency of upper GI symptoms but were not asked about the severity of symptoms. The severity and frequency of reflux play an important role in the pathophysiology of GERD; however, there is often a discrepancy between the severity of esophageal exposure to gastric content and the severity of symptoms. Patients with relatively low esophageal acid exposure can have severe symptoms and patients with high exposure to reflux can have relatively few reflux symptoms.19,20 Furthermore, there is an association between insufficient gastroesophageal flap valve with poor response to PPI treatment,21 but in our study, we did not evaluate the association between Hill grade and response to PPI treatment. Finally, the study only includes patients referred for gastroscopy in clinical practice, subjects who are highly prevalent of GI complaints and we are not able to compare symptoms, findings, and PPI prescriptions with subjects who are representative of a normal population. For example, it is possible that patients with Hill grades II and III may significantly differ from patients with Hill grade I if a cohort representative of a normal population was used.
In conclusion, the gastroscopic classification in Hill grades III and IV is important in clinical practice because they are associated with esophagitis, Barrett’s esophagus, symptoms of GERD, and prescriptions of PPIs, whereas a differentiation between Hill grades I and II is not.
Supplementary Material
ACKNOWLEDGMENT
We are grateful to the staff of the endoscopy unit at Umeå University Hospital.
FUNDING
The study was funded by Region Västerbotten, Sweden.
DATA AVAILABILITY
Unidentifed selected data may be available from the corresponding auhtor.
Contributor Information
Lisa Brännström, Department of Public Health and Clinical Medicine, Medicine, Umeå University, Umeå, Sweden.
Mårten Werner, Department of Public Health and Clinical Medicine, Medicine, Umeå University, Umeå, Sweden.
Bengt Wallner, Department of Surgical and Perioperative Sciences, Surgery, Umeå University, Umeå, Sweden.
Karl A Franklin, Department of Surgical and Perioperative Sciences, Surgery, Umeå University, Umeå, Sweden.
Pontus Karling, Department of Public Health and Clinical Medicine, Medicine, Umeå University, Umeå, Sweden.
References
- 1. El-Serag H B, Sweet S, Winchester C C et al. Update on the epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut 2014; 63: 871–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Yamasaki T, Hemond C, Eisa M et al. The changing epidemiology of gastroesophageal reflux disease: are patients getting younger? J Neurogastroenterol Motil 2018; 24: 559–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Andreasson A, Talley N J, Walker M M et al. An increasing incidence of upper gastrointestinal disorders over 23 years: a prospective population-based study in Sweden. Am J Gastroenterol 2021; 116: 210–3. [DOI] [PubMed] [Google Scholar]
- 4. Nishizawa T, Suzuki H. Hiatal hernia, vol. 74. Nihon Rinsho, 2016; 1339–42. [PubMed] [Google Scholar]
- 5. Wallner B, Bjor O, Andreasson A et al. Identifying clinically relevant sliding hiatal hernias: a population-based endoscopy study. Scand J Gastroenterol 2018; 53: 657–60. [DOI] [PubMed] [Google Scholar]
- 6. Guda N M, Partington S, Vakil N. Inter- and intra-observer variability in the measurement of length at endoscopy: implications for the measurement of Barrett’s esophagus. Gastrointest Endosc 2004; 59: 655–8. [DOI] [PubMed] [Google Scholar]
- 7. Hill L D, Kozarek R A, Kraemer S J et al. The gastroesophageal flap valve: in vitro and in vivo observations. Gastrointest Endosc 1996; 44: 541–7. [DOI] [PubMed] [Google Scholar]
- 8. Kim G H, Kang D H, Song G A et al. Gastroesophageal flap valve is associated with gastroesophageal and gastropharyngeal reflux. J Gastroenterol 2006; 41: 654–61. [DOI] [PubMed] [Google Scholar]
- 9. Koch O O, Spaun G, Antoniou S A et al. Endoscopic grading of the gastroesophageal flap valve is correlated with reflux activity and can predict the size of the esophageal hiatus in patients with gastroesophageal reflux disease. Surg Endosc 2013; 27: 4590–5. [DOI] [PubMed] [Google Scholar]
- 10. Navarathne N M, Abeysuriya V, Ileperuma A et al. Endoscopic observations around the gastroesophageal junction in patients with symptomatic gastroesophageal reflux disease in South Asia. Indian J Gastroenterol 2010; 29: 184–6. [DOI] [PubMed] [Google Scholar]
- 11. Hansdotter I, Bjor O, Andreasson A et al. Hill classification is superior to the axial length of a hiatal hernia for assessment of the mechanical anti-reflux barrier at the gastroesophageal junction. Endosc Int Open 2016; 4: E311–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. CMS Collaboration, Khachatryan V, Sirunyan A M et al. Search for heavy neutrinos and [formula: see text] bosons with right-handed couplings in proton-proton collisions at [formula: see text]. Eur Phys J C Part Fields 2014; 74: 3149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Jonasson C, Wernersson B, Hoff D A et al. Validation of the GerdQ questionnaire for the diagnosis of gastro-oesophageal reflux disease. Aliment Pharmacol Ther 2013; 37: 564–72. [DOI] [PubMed] [Google Scholar]
- 14. Armstrong D, Bennett J R, Blum A L et al. The endoscopic assessment of esophagitis: a progress report on observer agreement. Gastroenterology 1996; 111: 85–92. [DOI] [PubMed] [Google Scholar]
- 15. Sharma P, Dent J, Armstrong D et al. The development and validation of an endoscopic grading system for Barrett's esophagus: the Prague C & M criteria. Gastroenterology 2006; 131: 1392–9. [DOI] [PubMed] [Google Scholar]
- 16. Kirchheiner J, Glatt S, Fuhr U et al. Relative potency of proton-pump inhibitors-comparison of effects on intragastric pH. Eur J Clin Pharmacol 2009; 65: 19–31. [DOI] [PubMed] [Google Scholar]
- 17. Contractor Q Q, Akhtar S S, Contractor T Q. Endoscopic esophagitis and gastroesophageal flap valve. J Clin Gastroenterol 1999; 28: 233–7. [DOI] [PubMed] [Google Scholar]
- 18. Xirouchakis E, Kamberoglou D, Kalos D et al. The effect of gastroesophageal flap valve appearance on the management of patients with symptoms of gastroesophageal reflux disease. Dig Dis Sci 2009; 54: 328–32. [DOI] [PubMed] [Google Scholar]
- 19. Bredenoord A J, Weusten B L, Timmer R et al. Characteristics of gastroesophageal reflux in symptomatic patients with and without excessive esophageal acid exposure. Am J Gastroenterol 2006; 101: 2470–5. [DOI] [PubMed] [Google Scholar]
- 20. Stein H J, Hoeft S, DeMeester T R. Functional foregut abnormalities in Barrett’s esophagus. J Thorac Cardiovasc Surg 1993; 105: 107–11. [PubMed] [Google Scholar]
- 21. Cheong J H, Kim G H, Lee B E et al. Endoscopic grading of gastroesophageal flap valve helps predict proton pump inhibitor response in patients with gastroesophageal reflux disease. Scand J Gastroenterol 2011; 46: 789–96. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.