Abstract
Treatment as prevention (TasP) is an effective HIV prevention strategy. Our objectives were to explore TasP attitudes and beliefs among people with HIV (PWH) who are not engaged in care and to examine attitudes and beliefs by selected characteristics. We sampled PWH who had participated in the Medical Monitoring Project (MMP), a structured interview survey, from June 2018–May 2019 to participate in 60-minute semi-structured telephone interviews. We obtained sociodemographic and behavioral quantitative data from the MMP structured interview. We used applied thematic analysis to analyze the qualitative data and integrated the qualitative and quantitative data during analysis. Negative attitudes and beliefs, especially skepticism and mistrust, about TasP were pervasive. Only one participant who identified as female, was not sexually active, and had not heard of TasP held positive attitudes and beliefs about TasP. TasP messages should use clear and unambiguous language, address mistrust, and reach people who are not engaged in medical care.
Keywords: HIV, mixed methods research, treatment as prevention, U=U
INTRODUCTION
Treatment as prevention (TasP) is an HIV prevention strategy whereby people with HIV (PWH) who take HIV medication and become virally suppressed have no risk of transmitting HIV to sexual partners without HIV (1). In 2016, the results of the HPTN052 clinical trial reported that there was no HIV transmission within heterosexual serodiscordant couples when the partner with HIV was virally suppressed (2). The PARTNER, Opposites Attract, and PARTNER2 studies reported similar results, indicating the potential of viral suppression in preventing HIV transmission (3–5).
“Undetectable=Untransmittable” or “U=U” is a messaging campaign developed in 2016 by the Prevention Access Campaign disseminating the fact that PWH who take HIV medication and have an undetectable viral load cannot transmit HIV to sexual partners (6). Although U=U and TasP are sometimes used synonymously, U=U refers to a messaging campaign that disseminates the science of TasP.
Few studies have examined TasP awareness, knowledge, attitudes, and beliefs among PWH (7). According to some stage theories of health behavior, awareness usually precedes the development of attitudes and beliefs; these constructs (awareness, attitudes, and beliefs) play a role in whether people adopt a health behavior (8). Studies have found that between 24% and 29% of sexual minority men with HIV had never heard of TasP or U=U messages (9,10). Furthermore, awareness of TasP does not equate to having accurate knowledge of it (11). People also lack knowledge of the term “undetectable” (7,12). In one study using in-depth, semi-structured interviews, some sexual minority men did not know what the term “undetectable” meant, even though they recognized the term because it is commonly used on sexual networking apps or in their communities (13). Accurate knowledge is key as the message of TasP hinges on people’s knowledge of the term “undetectable.” Knowledge of the term “undetectable viral loads” might vary by demographic characteristics or geographic areas. For instance, in a survey of men who have sex with men (MSM) in New York City, 94% knew what an undetectable viral load was (14).
People hold attitudes and beliefs about TasP that impede its HIV prevention potential. Studies show that people believe that TasP is partially or entirely inaccurate, or that it does not offer adequate or complete protection against HIV transmission (7, 13–15). For instance, one study found that one third of MSM with HIV believed TasP was inaccurate (16). In a survey conducted from 2017 to 2018, researchers found that only 51% of men with HIV believed TasP to be completely accurate (17). In one study, common beliefs included that TasP would not eliminate the risk of HIV transmission, that it was impossible to clear the virus from someone with HIV, that HIV was a threat, and that it would be difficult to trust someone who said they were undetectable (15). Another study found that 37% of men with HIV believed that even if someone had an undetectable viral load, they still had to worry about transmitting HIV to others, and 32% felt that it was “never safe” to engage in condomless anal sex (10). Data from semi-structured interviews with PWH who were not on antiretroviral therapy (ART) found that even when participants understood the public health benefit of TasP, this understanding was not enough to move them to take ART. Some of these participants viewed engaging in condomless sex while on ART as irresponsible since it could transmit other sexually transmitted infections. Others thought that TasP was irrelevant to people who are already engaging in other HIV prevention activities or people in seroconcordant relationships (18). However, not all beliefs and attitudes about TasP are negative. One study found that participants felt that TasP could reduce fears of HIV transmission, and another study found that most sexual minority men felt better about having HIV because of TasP and believed it would improve societal stigma (9,18).
Several studies have shown that people who are engaged in care viewed TasP more positively than people not engaged in care. Sexual minority men who had undetectable viral loads and had a discussion with their provider had stronger beliefs in the benefits of TasP for reducing stigma than sexual minority men without those indicators of care engagement (9). Furthermore, PWH who had undetectable viral loads were more likely to believe that U=U was accurate than did PWH who had detectable viral loads (17).
Relationship status and sexual behaviors have been associated with TasP attitudes and beliefs. In one study, sexual minority men in serodiscordant relationships viewed TasP more positively (i.e., TasP made them feel better about having HIV and they believed that TasP would reduce HIV stigma) and were more likely to talk about TasP with their providers than single sexual minority men (9). Furthermore, sexual and gender minority persons without HIV who trusted TasP were more willing to engage in condomless anal sex, regardless of their partner’s HIV status, than people who did not trust TasP (19).
Few mixed methods studies have examined PWH’s awareness, attitudes, and beliefs about TasP. Quantitative studies have called for future studies that focus on the specific reasons why someone would distrust TasP and how to foster more trust in TasP, which can be accomplished by qualitative and mixed methods studies (19). Our objectives were to fill these gaps by 1) exploring TasP awareness, attitudes, and beliefs among PWH who are not engaged in HIV care across the United States using data from in-depth, semi-structured qualitative telephone interviews and 2) examining awareness, attitudes, and beliefs about TasP by selected characteristics (i.e., gender, sexual orientation, history of sexual activity, awareness of TasP) using a mixed methods analysis.
METHODS
The CDC Medical Monitoring Project (MMP) is an annual, cross-sectional survey designed to produce nationally representative estimates of the sociodemographic, behavioral, and clinical characteristics of adults with diagnosed HIV in the United States. MMP survey data were collected through structured telephone, or in-person interviews administered by trained staff in 23 jurisdictions and through medical records abstraction. MMP survey methods are described in detail elsewhere (20). A separate MMP Qualitative (MMP-Qual) Project was designed to collect qualitative data from a subset of MMP survey participants not engaged in HIV medical care to complement the quantitative data collected by the MMP survey. MMP-Qual Project methods are described in detail elsewhere (21). Briefly, we purposively sampled people who participated in the MMP survey from June 2018–May 2019 for the MMP-Qual Project. Some of the eligibility criteria for the MMP-Qual Project mirrored those of the MMP survey, including being ≥18 years old, having an HIV diagnosis, and living in one of 23 MMP jurisdictions on December 31, 2017. To be eligible to participate in the MMP-Qual Project, participants must also have met additional eligibility criteria, including being out of HIV care for 12 months or more or having never received HIV care based on their response to one question on the MMP structured interview survey. Persons who did not speak English or were incarcerated at the time of the interview were ineligible to participate in the MMP-Qual Project. Verbal informed consent was obtained for all participants. The Centers for Disease Control and Prevention (CDC) determined this project was public health surveillance; thus, institutional review board approval was not obtained.
Health department staff in the 23 MMP jurisdictions were responsible for recruiting, scheduling interviews, providing appointment reminders, and maintaining contact information of MMP-Qual Project sampled persons. Health department staff coordinated interview scheduling with CDC interviewers. At the end of the MMP structured interview survey, health department staff were instructed to provide HIV prevention materials to participants, including TasP materials, along with referrals to HIV care and support services. Four trained CDC interviewers conducted semi-structured 60-minute telephone interviews with 35 participants. These semi-structured interviews occurred after (typically ≥1 day) the MMP structured interview survey. One semi-structured interview was not audio recorded and another participant was never asked about TasP; thus, two transcripts were excluded from this analysis.
Qualitative data measures
Data collection lasted from August 2018 to May 2019. The qualitative interview guide contained 22 questions about barriers and facilitators to HIV care engagement, preferred method of contact for recruitment in surveys, the reason for MMP participation, and awareness, knowledge, and beliefs about TasP. For this analysis, we only analyzed questions relating to awareness (whether participants had heard of TasP or not), attitudes (feeling or opinion towards TasP) and beliefs about TasP. We did not reference or ask about the “U=U” messaging campaign in our interview questions. All interviews were audio recorded and transcribed verbatim by six trained CDC staff. Data quality checks were performed on all transcripts.
Quantitative data measures
We obtained quantitative data on participant demographic and behavioral characteristics (e.g., gender, race, sexual orientation, sexual behaviors) from the MMP structured interview survey. Sex without the use of an HIV prevention strategy was defined as condomless vaginal or anal sex with an HIV-negative or unknown-status partner not known to be on PrEP while not having sustained viral suppression during the past 12 months. In the MMP structured interview survey, we asked participants if they had heard of TasP. We categorized participants as having heard of TasP or not based on whether they answered yes or no to that question. We asked all participants to what extent they agreed or disagreed using a 5-point Likert scale with the following statement: “Having an undetectable viral load means I can worry less about using condoms.” Additionally, we asked participants if they had had conversations with 1) an outreach worker, counselor, or prevention program worker, or 2) a doctor, nurse, or other healthcare worker about HIV and STD prevention in the past 12 months.
Data analysis
We used an exploratory sequential mixed methods framework in which the initial qualitative data analysis phase was followed by a quantitative data analysis phase (22). After analyzing the qualitative and then quantitative data separately, we integrated these data.
Qualitative data
Two team members independently read two interview transcripts and constructed a list of codes. These codes were used to develop the initial codebook. The team applied the initial codebook to five additional transcripts and continued to refine the codebook until reaching consensus. Two team members coded all 33 transcripts. We performed intercoder reliability on 4 (12%) transcripts in NVivo (QSR International, Melbourne, Australia), reviewing and discussing codes until agreeing on code application. We used applied thematic analysis to analyze the data. We looked at the most frequently applied codes and placed codes into themes. Other data analysis procedures we conducted included word searches and keyword-in-context techniques.
Quantitative data
We reported frequencies of sociodemographic and behavioral data among MMP-Qual Project participants using SAS 9.4 (SAS Institute, Cary, NC). Quantitative data were obtained from the MMP structured interview survey; however, we only analyzed data from participants who had participated in the MMP structured interview survey and the MMP-Qual Project.
Mixed methods approach
We integrated the qualitative and quantitative data for the purposes of triangulation (i.e., investigating identical aspects of the same phenomenon) and complementarity (i.e., using quantitative data to elaborate the results of the qualitative data). We integrated the qualitative and quantitative data after we analyzed each separately. We used joint displays to further integrate the data to draw out insights (23).
We were interested in examining the presence of positive, neutral, and negative attitudes and beliefs about TasP by characteristics (gender, sexual orientation, sexually active, heard of TasP) associated with TasP awareness, attitudes and beliefs found in the literature. To do so, we linked the qualitative and quantitative data for each participant using the participant’s unique identifier. After linking the data, we attached the quantitative data to individual transcripts in NVivo. Then, we performed crosstabs of the qualitative and quantitative data. To use crosstabs, qualitative data were transformed into categorical variables of “positive,” “neutral,” and “negative” attitudes and beliefs about TasP. Positive statements included times when participants discussed TasP making them feel hopeful or less stigmatized, and positive statements like “great,” or “good.” Negative statements included times when participants expressed mistrust, suspicion, or cynicism about TasP. Neutral statements included statements that lacked an evaluative component; for instance, participants saying that they did not feel one way or the other about TasP. We created crosstabs of positive, neutral, and negative attitudes and beliefs about TasP (qualitative data transformed into quantitative data) by gender, sexual orientation, sexual activity, and awareness of TasP (quantitative data from the MMP structured interview survey).
RESULTS
Quantitative results
We interviewed 33 PWH who were not engaged in HIV care about TasP. Seventy-six percent of participants were male, 67% were non-Hispanic Black or African American, 55% identified as straight, 64% had more than a high school education, 64% were sexually active in the past 12 months, and 16% had engaged in sex without the use of an HIV prevention strategy. The median age was 47 years (range, 29–62) and the median number of sex partners was one (range, 0–40). In the past 12 months, 9% of participants had a conversation with an outreach worker, counselor, or prevention program worker about HIV or STI prevention; and 18% had a conversation with a doctor, nurse, or other health care worker about HIV or STI prevention. Seventy-nine percent of participants strongly or somewhat disagreed with the statement, “Having an undetectable viral load means I can worry less about having to use condoms” (Table 1).
Table I.
Characteristics, behaviors, and attitudes of people with HIV who are out of care (N=33) participating in the MMP Qualitative Project, 2018–2019
| Characteristics, behaviors, and attitudesa | No.b | % |
|---|---|---|
| Gender | ||
| Male | 25 | 76% |
| Female | 8 | 24% |
| Age | ||
| Median | 47 | — |
| Range | 29–62 | — |
| Race/ethnicity | ||
| Non-Hispanic White | 6 | 18% |
| Non-Hispanic Black or African American | 22 | 67% |
| Hispanic or Latinoc | 2 | 6% |
| Another race or ethnicityd | 3 | 9% |
| Sexual orientation | ||
| Lesbian, gay, or bisexual | 14 | 42% |
| Straight | 18 | 55% |
| Another sexual orientation | 1 | 3% |
| Highest level of education completed | ||
| <High school | 5 | 15% |
| High school diploma or equivalent | 7 | 21% |
| >High school | 21 | 64% |
| Sexually active | ||
| Yes | 21 | 64% |
| No | 12 | 36% |
| Number of sex partners | ||
| Median | 1 | — |
| Range | 0–40 | — |
| Engaged in sexual behavior that increases the chance of HIV transmission e | ||
| Yes | 5 | 16% |
| No | 26 | 84% |
| Heard of Treatment as Prevention (TasP) | ||
| Yes | 18 | 55% |
| No | 15 | 45% |
| “Having an undetectable HIV viral load means I can worry less about having to use condoms.” | ||
| Strongly disagree | 21 | 64% |
| Somewhat disagree | 5 | 15% |
| Neutral | 1 | 3% |
| Somewhat agree | 4 | 12% |
| Strongly agree | 2 | 6% |
| Had a conversation with an outreach worker, counselor, or prevention program worker about HIV/STD prevention | ||
| Yes | 3 | 9% |
| No | 30 | 91% |
| Had a doctor, nurse, or other health care worker about HIV/STD prevention | ||
| Yes | 6 | 18% |
| No | 27 | 82% |
All data in this table were obtained from the MMP quantitative survey. All measures were based on the past 12 months.
Numbers might not add up to total (N=33) because of missing data.
Hispanics or Latinos might be of any race. Persons are classified in only one race/ethnicity category.
Includes American Indian/Alaska Native, Asian, Native Hawaiian/Other Pacific Islander, or multiracial.
Sexual behaviors that increase the chance of HIV transmission was defined as condomless vaginal or anal sex with an HIV-negative or unknown-status partner while not sustainably virally suppressed nor protected by PrEP in the past 12 months.
Qualitative themes
Most participants held negative beliefs and attitudes about TasP.
Many participants expressed skepticism and mistrust about TasP. Some participants noted that although science or research may demonstrate the HIV prevention benefits of HIV treatment, they don’t “think it’s the case,” and that decision making surrounding the use of TasP depends on the extent to which someone “trusts in science.” Others responded to the question by saying that while researchers might say that HIV treatment prevents HIV sexual transmission, researchers still “don’t know.” Some participants described TasP as a “lie” or “almost false information.” Sometimes, negative statements about TasP accompanied statements that TasP was not a “cure.” Participants noted that an undetectable status does not change an HIV diagnosis. Some who understood the meaning of “undetectable,” noted detectability can change, which made them skeptical of TasP. Participants also discussed that the consequences of TasP not working (transmission of HIV to a sex partner) were far too great to use TasP as HIV prevention. For instance, one participant noted, “I’m not a murderer. I don’t want anyone to die because of me.”
Participants’ individual health would be the main motivator of seeking care.
Participants were asked to what extent TasP would or would not affect their decision to seek HIV care, as all participants were out of HIV care for 12 months or more. Among participants who said that awareness of TasP would affect their decision to get care, several noted that the main reason they would get on medication was to obtain a lower viral load or to be “healthy,” and not necessarily to have sex (and sometimes condomless sex) with another person. As one participant noted, “That’s [TasP] a great thing, and that would be all more of the reason why I would want to be on medication,” followed by “the sole reason would be for me to be healthy.” Another participant noted that the HIV prevention benefit of medication is a “bonus.” One participant said that TasP was “not a strong enough reason” by itself. Another participant noted that they would prefer not take medication and continue to have “protective,” (i.e., sex with a condom to prevent HIV transmission) sex. Finally, another participant noted that getting on medication would require them to get health insurance and they would not go through the process of setting up health insurance just to be able to have condomless sex with someone who was not a steady partner, noting “I’m not about to like set up insurance for someone who’s here today and gone tomorrow.”
Participants did not view TasP as protective against HIV transmission.
When asked how TasP might affect their sex lives, several participants noted that they would not have “unprotected sex,” which indicated that TasP was not seen as protective against HIV transmission. As one participant noted, “you should protect yourself no matter what.” Protection against HIV transmission usually meant using a condom, as one participant noted that someone relying on TasP would still need to take “precautions,” (i.e., use condoms). Despite knowing or learning about TasP, participants still felt it was important to wear condoms. For instance, when asked about TasP, one participant said, “I think it’s true to a certain point… of course, you have to wear condoms.” Participants also talked about TasP as “not a guarantee.” They were not willing to “take a chance” by having condomless sex if TasP was not “100% guaranteed.” One participant noted, “I can’t imagine someone who might be on even PrEP and negative being receptive to unprotected. I don’t know, that’s risky.” Thus, TasP was not seen as protective against HIV transmission. Instead, many viewed it as “risky.”
Sexual history provided context on attitudes and beliefs about TasP.
Participants had an array of sexual histories that sometimes informed their beliefs and attitudes about TasP. For instance, two participants talked about not having sex. One of those participants noted that they no longer have sex because disclosing their HIV status is stigmatizing. Others noted that TasP was not relevant to their lives because they believed their sexual behaviors did not pose a risk for HIV transmission. For instance, one participant discussed being in a seroconcordant relationship. Another participant, who had had sex once in the past year, discussed “getting older” and not being “very [sexually] active now.” For him, TasP was not something he “really think[s] about.” For some participants, past sexual experiences affected their attitudes and beliefs about TasP. One participant reflected on his experience dating someone who had HIV while he was HIV negative, and how important it was for him to understand what his sex partner with HIV was doing to protect their health. For him, TasP requires communication. Another participant noted that he got HIV from someone who said they had an undetectable viral load. According to this participant, he confronted his sex partner after he was diagnosed with HIV and the sex partner showed paperwork demonstrating that they had an undetectable viral load when they had sex. The participant did not know his sex partner had HIV when they had sex and felt “hurt, betrayed, used.” This same participant expressed skepticism about TasP.
Few participants held positive attitudes and beliefs about TasP.
Participants who held positive attitudes and beliefs about TasP responded to our question by saying that TasP was “great” or “a good thing.” However, very few could expand on why they believed it was “great.” One person discussed the HIV prevention benefits of TasP as a positive. Two participants discussed that TasP could be destigmatizing. For instance, one participant expressed that he would “feel better about telling someone” that he was undetectable. He reflected that currently he tells people, “I am [HIV] positive” but it would “sound so much better” if he could tell a sex partner that their chances of getting HIV are “reduced” because he is undetectable. Another participant noted that learning about TasP “made [her] feel better about [herself].” When asked to expand on this, she noted that it made her “feel like less of a leper.” This participant reported feeling stigmatized in the past by health care providers because of her HIV status.
Mixed methods results
Our exploratory sequential mixed methods analysis demonstrated the number of participants who held positive, neutral, and negative attitudes and beliefs about TasP by gender, sexual orientation, sexual activity, and whether someone had heard of TasP (characteristics are not mutually exclusive). Thirteen men and four women held negative attitudes and beliefs about TasP. Ten participants who identified as straight and seven participants who identified as lesbian, gay, or bisexual held negative attitudes and beliefs about TasP. Nine participants who were sexually active and eight participants who were not sexually active held negative attitudes and beliefs about TasP. Ten participants who had heard of TasP and seven participants who had not heard of TasP held negative attitudes and beliefs about TasP.
Six men and one woman held positive attitudes and beliefs about TasP. Two participants who identified as straight and four participants who identified as lesbian, gay, or bisexual held positive attitudes and beliefs about TasP. Six participants who were sexually active and one participant who was not sexually active held positive attitudes and beliefs about TasP. Similarly, six participants who had heard of TasP and one participant who had not heard of TasP had positive attitudes and beliefs about it. To note, a single participant accounted for the positive attitudes and beliefs about TasP in females, non-sexually active participants, and participants who had not heard of TasP. The integration of the qualitative and quantitative data using a joint display signaled us to revisit the participant’s transcript to investigate whether this participant represented a negative case (i.e., a participant whose data are at odds with most of the data from other participants). Upon revisiting the transcript from this participant’s interview, we determined it to be a negative case (Figure 1; Table 2).
Figure 1.
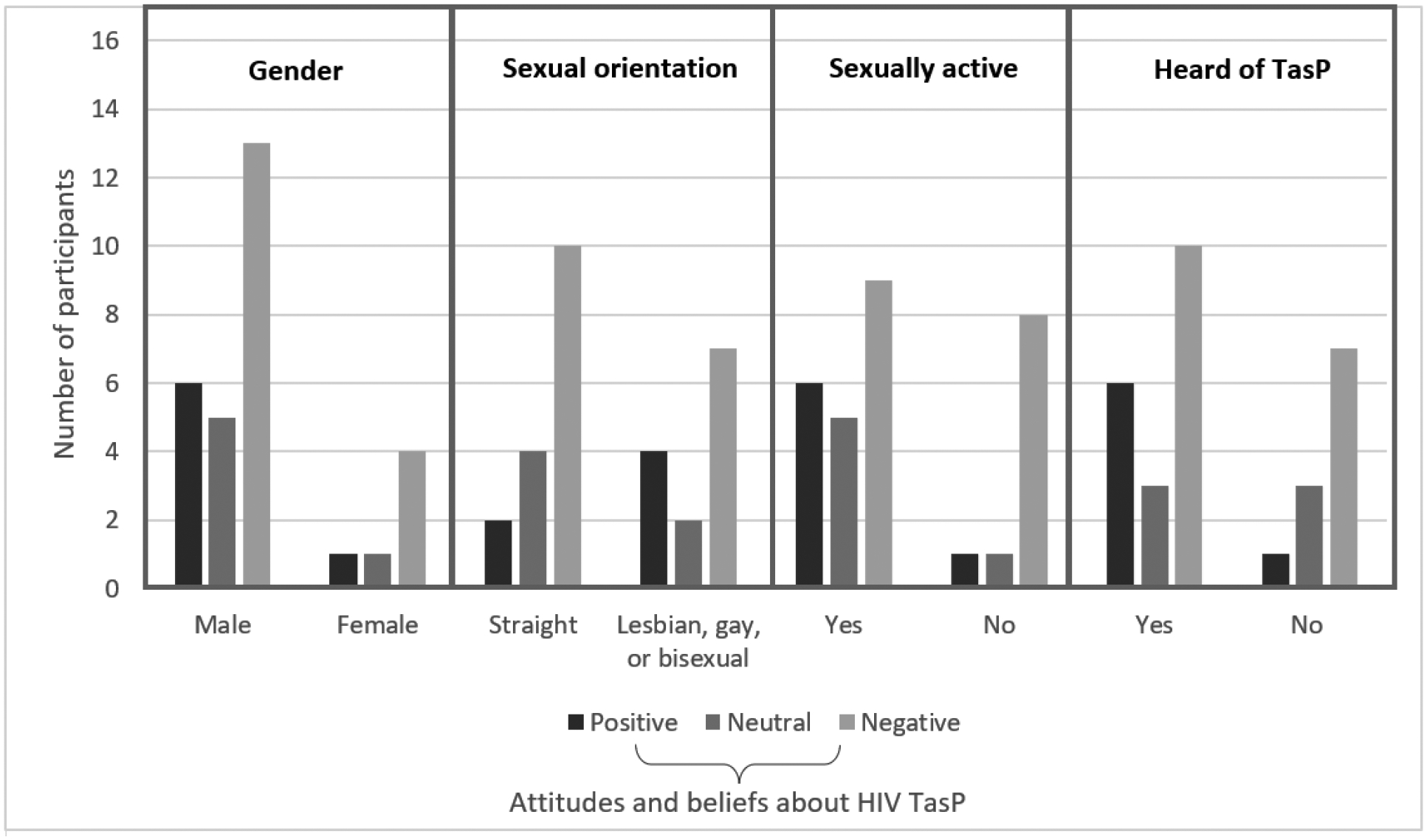
Number of participants (N=33) who expressed positive, neutral, or negative attitudes and beliefs about TasP by gender, sexual orientation, whether sexually active, and whether heard of Treatment as Prevention (TasP)
Note: Attitudes and beliefs about HIV TasP came from the qualitative data. Qualitative data were transformed into quantitative variables (positive, neutral, negative). Positive statements included times when participants discussed TasP making them feel hopeful or less stigmatized, and positive statements like “great,” or “good.” Negative statements included times when participants expressed mistrust, suspicion, or cynicism about TasP. Neutral statements included statements that lacked an evaluative component; for instance, participants saying that they did not feel one way or the other about TasP. Quantitative data from the Medical Monitoring Project (MMP) structured interview included gender, sexual orientation, whether sexually active, and whether they had heard of TasP. These data were collected separate from the qualitative data. Gender, sexual orientation, whether sexually active, and whether they had heard of TasP are not mutually exclusive categories. Categories will not add up to 33 because not all participants expressed an attitude or belief about TasP during the qualitative interview. One participant represented a negative case (i.e., their data were at odds with most of the data). This participant represented the single participant who held positive attitudes and beliefs in the female, non-sexually active, and non-TasP aware categories.
Table II.
Illustrative quotes about positive and negative attitudes and beliefs about Treatment as Prevention (TasP) by participant characteristics, behaviors, and TasP awareness
| Positive attitudes and beliefs about HIV TasP | Negative attitudes and beliefs about HIV TasP |
|---|---|
| “It’s kinda hard to describe, I think that’d give me more reason to wanna go [to an HIV health care provider], even though I haven’t ‘cus of other reasons.” – Male, gay, sexually active participant who has heard of TasP | “I’m not willing to take that chance to give anybody this. I’m not, I’m not a murderer. I don’t want anyone to die because of me”. – Female, straight, not sexually active participant and had not heard of TasP |
| “It’s a good thing because, slims the chances down of people getting it …” – Male, straight, sexually active participant who has heard of TasP | “I don’t know… It’s something to think about but it’s still scary because… you don’t really, really know that you can’t. And then what if they have something then you can catch that and then you’ll, going back over the same thing again.” – male, gay, not sexually active participant and had not heard of TasP |
| “Well, I think it’s great and I, you know, I believe that because I’ve seen that that’s true.” – male, straight, sexually active participant who has heard of TasP | “Nah. Because, you mean, there’s not, not an actually cure. You still putting someone… it’s not a cure, its treatment but it’s not a cure.” – male, straight, sexually active participant who has heard of TasP |
| “It made me feel like less of a leper” – Female participant reporting another sexual orientation, not-sexually active, and had not heard of TasP* *This participant accounts for all the positive feelings found among females, non-sexually active participants, and those who had not heard of TasP. |
“I’m a little skeptical about that because when I was infected with HIV, the person that infected me was undetectable. So even though it may be unlikely, it can happen, so I don’t necessarily think that’s something that people should be promoting, I don’t think that’s something that should be promoted.” – male, gay, sexually active participant who has heard of TasP |
| “I guess it’d be kind of, I guess you can describe it as kind of like hedging your bet. I mean they say that the thing to do and so you do it, but you don’t necessarily have full faith in it.” – male, gay, sexually active participant, who has heard of TasP | |
| “I think it’s almost false information. No matter what, you should protect yourself, especially in that situation.” – male, gay, not sexually active participant who has heard of TasP |
Note: Attitudes and beliefs about HIV TasP came from the qualitative data. Qualitative data were transformed into quantitative variables (positive, neutral, negative). Positive statements included times when participants discussed TasP making them feel hopeful or less stigmatized, and positive statements like “great,” or “good.” Negative statements included times when participants expressed mistrust, suspicion, or cynicism about TasP. Neutral statements included statements that lacked an evaluative component; for instance, participants saying that they did not feel one way or the other about TasP. Quantitative data from the Medical Monitoring Project (MMP) structured interview included gender, sexual orientation, whether sexually active, and whether they had heard of TasP. These data were collected separate from the qualitative data. Gender, sexual orientation, whether sexually active, and whether they had heard of TasP are not mutually exclusive categories. One participant represented a negative case (i.e., their data were at odds with most of the data). This participant represented the single participant who held positive attitudes and beliefs in the female, non-sexually active, and non-TasP aware categories.
DISCUSSION
Although HIV TasP is an effective HIV prevention strategy, we found that most PWH who were out of care held negative attitudes and beliefs about TasP that might impede its uptake. Participants expressed skepticism and mistrust, with some believing it to be false information. Others explained that TasP was not a cure. Many did not view TasP as protective against HIV transmission, often describing condom use as the effective HIV prevention strategy. Among participants with positive attitudes, few could articulate why they viewed TasP positively. Furthermore, positive attitudes and beliefs were expressed by few participants who identified as straight; and only one participant who identified as female, who was not sexually active, and who had not heard of TasP had positive attitudes and beliefs about TasP.
Our findings support what has been found in the literature. For instance, Siegel and Meunier (2019) also found that few participants in their study believed that TasP offered reliable and adequate protection against HIV sexual transmission (14). We also found that some people believed that TasP did not apply to them because they had few sex partners or were in seroconcordant relationships, which aligns with findings from another study (18). Thus, TasP messaging might not engage people who believe they cannot transmit HIV to others. Like the themes identified in our study, participants in other qualitative interviews believed that TasP did not eliminate the risk of HIV transmission completely, that it was impossible to eliminate HIV from someone, and that viral loads fluctuate (12,15). On the other hand, some participants in our study expressed that TasP made them feel better about themselves. One study found that TasP enabled PWH who had undetectable viral loads to feel less HIV stigma (24). Thus, TasP might play an essential role in reducing HIV stigma, which is a barrier to HIV care and treatment.
Awareness and knowledge of TasP may increase its uptake. Thus, TasP messaging should be more widely disseminated and clearly communicated. At the time of the qualitative interviews, the CDC communicated that TasP posed “effectively no risk” of HIV transmission (25). This messaging may have led people to doubt TasP as an effective HIV prevention strategy. Participants in our project often discussed how TasP was taking a risk, and that they would not rely on it because it was not “100% guaranteed,” yet they believed condoms—which are less effective at preventing HIV transmission—to be more protective against HIV transmission. Public health messaging on TasP or U=U should communicate that TasP is an HIV prevention strategy that poses no risk of HIV sexual transmission. Furthermore, the term “undetectable” should be clearly defined, especially for the U=U campaign. Messaging should also provide accurate information about the meaning of viral load and address concerns of fluctuating viral loads and notions that TasP is not a cure for HIV. Clear messaging is key as one study found that men with detectable viral loads might have had condomless sex with others because they incorrectly believed they had undetectable viral loads (26). Public health messages should also communicate the effectiveness of TasP compared with condom use by using clear and unambiguous language, since participants in our project believed condoms to be the more effective HIV prevention strategy. Last, to address the pervasive skepticism and mistrust of TasP, it is important to ensure that TasP messages are coming from trusted sources of information.
Although participants in our project were not engaged in care, all had engaged with the health care system in some capacity in the past by virtue of having an HIV diagnosis. Thus, HIV testing sites might be an important setting for disseminating TasP information. Additionally, some participants expressed interest in re-engaging in HIV care during the interview. Health care providers play an important role in disseminating information about TasP. One study found that PWH who discussed U=U with their health care providers had more favorable HIV health outcomes—including viral suppression and optimal health—than people who were unaware of TasP (27). However, a systematic review found that knowledge gaps exist among health care providers regarding TasP, which may lead to ineffective communication with patients. Further, some providers hesitate to inform patients about TasP because they believe it might lead to other STIs, an increase in condomless sex, an increase in sex partners, and HIV transmission (11). In one study, sexual minority men reported feeling stigmatized by health care providers when discussing behaviors that increase HIV risk. These participants also believed that health care providers viewed their sexual orientation as intrinsically linked to risk (28). Health care providers should receive training on TasP and on how to talk to their patients about TasP in an open, nonjudgmental, and comfortable manner. Conversations about TasP should also focus on the importance of antiretroviral therapy (ART) use and adherence. Further, the onus of initiating these conversations should be on the provider and not the patient. Health care providers should also learn about how their personal values and biases might influence their decision to misrepresent or withhold information from their patients—as doing so may perpetuate inequity and infringe on the human and sexual rights of PWH (29).
Some people in our project were not interested in re-engaging in HIV care. Thus, TasP messaging should be disseminated outside of health care facilities or AIDS service organizations, such as social networking sites, smartphone applications, or billboards. One study found that U=U tweets (posts made on Twitter) that emphasized sex and love predicted retweets and number of likes. The study researchers argued that health communication efforts that focused on the human elements of HIV—including personal narratives and messages of love and pleasure—might reach and engage more people in information-saturated environments like Twitter (30). Such messaging might also destigmatize HIV.
TasP messaging may not reach people equally, which might lead to health disparities. We found that only two people who identified as straight held positive attitudes and beliefs about TasP. This might be because TasP or U=U messaging efforts have focused on reaching gender and sexual minority (e.g., gay, lesbian, bisexual) communities. As one study found, among people who had seen or heard of “U=U,” the most common sources for finding this information included LGBTQ news media and dating or hookup apps (9). People who are not engaging with LGBTQ news media or on dating or hookup apps might not receive TasP information. In this same study, one third of participants learned about U=U through conversations with friends, medical providers, or sex partners. Thus, TasP messaging might not reach people who are not engaging with the health care system or who are not having sex (9). Additionally, one study found that awareness of TasP was moderate among heterosexual sexually active adults and lower than what has been found in other studies among gender and sexual minorities (31). Another study found that fewer men who have sex with women than MSM discussed U=U with their health care providers, indicating disparities by sexual orientation or behaviors (27). Further, our review of the literature on TasP awareness, knowledge, attitudes, and beliefs yielded only two studies that included female participants. Thus, even researchers have focused on understanding men’s awareness, knowledge, attitudes, and beliefs about TasP over those of women. TasP messaging should be expanded to reach people who are not engaging with the health care system, people who identify as heterosexual or straight, women, and people who are currently not having sex (as they might in the future).
Our findings were subject to some limitations. We only analyzed responses to questions about TasP; however, participants might have discussed attitudes and beliefs about TasP throughout the interview. To address this, we conducted keyword-in-context techniques to identify other instances when participants discussed TasP. Additionally, we asked about TasP at the end of a 60-minute semi-structured interview. Participants might have been fatigued by this point and dedicated less time to answering questions about TasP. In the MMP structured interview survey, participants were asked to what extent they agreed or disagreed with the statement “Having an undetectable HIV viral load means I can worry less about having to use condoms,” which has its limitations as this statement does not specify the purpose of the condom use (i.e., to prevent HIV transmission). Although participants were demographically comparable to the population of PWH in the United States, we had few female and Hispanic/Latino participants, and no transgender participants. Thus, we might be missing important perspectives. Although our findings are not generalizable to a larger population, they may be transferable to other settings. Additionally, we decided to keep the negative case in our data to account for differing human experiences. However, this also means those data should be interpreted with caution. Last, we cannot make statements about whether attitudes and beliefs varied by the selected characteristics.
CONCLUSIONS
We found that negative attitudes and beliefs about HIV TasP were pervasive among people with HIV who were not receiving HIV care. Participants felt that TasP did not provide guaranteed protection, that relying on TasP was taking a risk, that TasP was not a cure, that condoms were more effective than TasP, and that TasP was false information. Improving awareness and knowledge of TasP may lead to its uptake. Public health campaigns and health care providers should emphasize that TasP poses no risk of HIV sexual transmission, define TasP using clear and unambiguous language, and correct misinformation. Furthermore, TasP messaging may not be reaching people equally, which might contribute to HIV-related health disparities. Thus, public health messaging should expand to reach women, people who identify as straight, and people who are not sexually active, but might be in the future. It is also important to consider other sites and strategies for HIV prevention messaging for people who are not engaging with HIV medical care or support services.
Acknowledgments
We thank MMP-Qual participants and project area staff. We acknowledge the contributions of the Clinical Outcomes Team and Behavioral and Clinical Surveillance Branch at CDC. We also acknowledge Brittani Carter, Shana Green, Susi McGhee, Ehryn Ortega, and Ansley Lemons-Lyn for their contribution to data collection, transcription, and coding. This project was supported in part by an appointment to the Research Participation Program at the Centers for Disease Control and Prevention administered by the Oak Ridge Institute for Science and Education through an interagency agreement between the U.S. Department of Energy and the Centers for Disease Control and Prevention.
Funding:
Funding for the Medical Monitoring Project is provided by the Centers for Disease Control and Prevention.
Footnotes
Conflicts of interest: The authors declare no conflicts of interest. All authors certify that they have no affiliations with or involvement in any organization or entity with any financial interest or non-financial interest in the subject matter or materials discussed in this manuscript. The authors have no financial or proprietary interests in any material discussed in this article.
Ethics approval: MMP data collection is part of routine public health surveillance and was determined to be non-research.
Consent to participate: Informed consent was obtained for all participants.
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
REFERENCES
- 1.HIV Treatment as prevention. https://www.hiv.gov/tasp. Updated June 17, 2022. Accessed July 20, 2022.
- 2.Cohen MS, Chen YQ, McCauley M, et al. Antiretroviral therapy for the prevention of HIV-1 Transmission. N Engl J Med. 2016;375:830–839. DOI: 10.1056/NEJMoa1600693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bavinton BR, Pinto AN, Phanuphak N, et al. Viral suppression and HIV transmission in serodiscordant male couples: an international, prospective, observational, cohort study. Lancet HIV. 2018;5(8):e438–e447. doi: 10.1016/S2352-3018(18)30132-2. [DOI] [PubMed] [Google Scholar]
- 4.Rodger AJ, Cambiano V, Bruun T, et al. Sexual activity without condoms and risk of HIV transmission in serodifferent couples when the HIV-positive partner is using suppressive antiretroviral therapy. JAMA. 2016;316(2):171–181. doi: 10.1001/jama.2016.5148. [DOI] [PubMed] [Google Scholar]
- 5.Cambiano RA, Bruun T, Vernazza P, et al. Risk of HIV transmission through condomless sex in serodifferent gay couples with the HIV-positive partner taking suppressive antiretroviral therapy (PARTNER): final results of a multicentre, prospective, observational study. The Lancet.2019;393(10189):2428–2438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Prevention Access Campaign. https://preventionaccess.org/about-introduction/. Accessed January 17, 2023.
- 7.Matacotta J, Rosales-Perez F, Carillo C. HIV preexposure prophylaxis and Treatment as Prevention — beliefs and access barriers in men who have sex with men (MSM) and transgender women: a systematic review. Journal of Patient-Centered Research and Reviews. 2020;7(3): 265–274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Glan K, Rimer BK, Viswanath K, eds. Health Behavior and Health Education: Theory, Research, and Practice. 4th ed. San Francisco, Ca: Jossey-Bass; 2008. [Google Scholar]
- 9.Rendina JH, Talan AJ, Cienfuegos-Szalay J, Carter JA, Shalhav O. Treatment is more than prevention: perceived personal and social benefits of Undetectable = Untransmittable messaging among sexual minority men living with HIV. AIDS Patient Care STDS. 2020;34(10):444–451. doi: 10.1089/apc.2020.0137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Card K, Armstrong H, Lachowsky N, et al. Belief in Treatment as prevention and its relationship to HIV status and behavioral risk. J Acquir Immune Defic Syndr. 2018;77(1): 8–16. doi: 10.1097/QAI.0000000000001557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bor J, Fischer C, Modi M, et al. Changing knowledge and attitudes towards HIV Treatment-as-Prevention and “Undetectable = Untransmittable”: A systematic review. AIDS Behav. 2021;25(12): 4209–4224. doi: 10.1007/s10461-021-03296-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grace D, Nath R, Parry R, Connell J, Wong J, Grennan T. ‘… if U equals U what does the second U mean?’: sexual minority men’s accounts of HIV undetectability and untransmittable scepticism. Culture, Health, & Sexuality. 2021;23(9): 1270–1286. 10.1080/13691058.2020.1776397 [DOI] [PubMed] [Google Scholar]
- 13.Meanley S, Connochie D, Bonett S, Flores D, Bauermeister J. Awareness and perceived accuracy of Undetectable = Untransmittable: A cross-sectional analysis with implications for treatment as prevention among young men who have sex with men. Sex Transm Dis. 2019; 46(11): 733–736. doi: 10.1097/OLQ.0000000000001048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Siegel K, Meunier E. Awareness and perceived effectiveness of HIV Treatment as Prevention among men who have sex with men in New York City. AIDS Beh. 2019;23(7): 1974–1983. doi: 10.1097/QAI.0000000000001557. [DOI] [PubMed] [Google Scholar]
- 15.Meunier E, Siegel K, Sundelson A, Schrimshaw E. Stages of Adoption of “treatment as Prevention” among HIV-Negative Men Who Have Sex with Men Who Engage in Exchange Sex. AIDS Patient Care STDS. 2020;34(9): 380–391. doi: 10.1089/apc.2020.0062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rendina H, Parsons J. Factors associated with perceived accuracy of the Undetectable = Untransmittable slogan among men who have sex with men: Implications for messaging scale-up and implementation. J Int AIDS Soc. 2018;21(1): e25055. doi: 10.1002/jia2.25055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rendina JH, Cienfuegos-Szalay J, Talan A, Scott Jones S, Jimenez RH. Growing acceptability of Undetectable = Untransmittable but widespread misunderstanding of transmission risk: Findings from a very large sample of sexual minority men in the United States. J Acquir Immune Defic Syndr. 2020;83(3): 215–222. doi: 10.1097/QAI.0000000000002239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Newman C, de Wit J, Persson A, Holt M, Slavin S, Kidd M, et al. Understanding Concerns About Treatment-as-Prevention Among People with HIV who are not Using Antiretroviral Therapy. AIDS and Behav. 2015;19(5): 821–831. 10.1007/s10461-014-0959-9. [DOI] [PubMed] [Google Scholar]
- 19.Carneiro P, Westmoreland D, Patel V, Grov C. Awareness and acceptability of Undetectable = Untransmittable among a U.S. national sample of HIV-negative sexual and gender minorities. AIDS Beh. 2021;25(2): 634–644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Beer L, Johnson CH, Fagan JL, et al. A national behavioral and clinical surveillance system of adults with diagnosed HIV (The Medical Monitorign Project): Protocol for an annual cross-sectional interview and medical record abstraction survey. JMIR Rese Protoc. 2019;8(11):e15453. doi: 10.2196/15453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Padilla M, Gutierrez M, Fagan J. Using semistructured telephone interviews to collect qualitative data from people with HIV who are not in medical care: Implementation study. JMIR Res Protoc. 2022;11(11):e40041. doi: 10.2196/40041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Creswell JW, Plano Clark VL. Designing and conducting mixed methods research. 3rd ed. Thousand Oaks, CA: SAGE Publications, 2017. https://books.google.com/books?hl=en&lr=&id=BXEzDwAAQBAJ&oi=fnd&pg=PP1&ots=UkzbHnjvoz&sig=pdEZVXGw66CUfaAWTtJiYlj3JZo#v=onepage&q&f=false. Accessed August 10, 2022. [Google Scholar]
- 23.Fetters MD, Curry LA, Creswell JW. Achieving integration in mixed methods designs-principles and practices. Health Serv Res. 2013;48(6 Pt 2):2134–56. doi: 10.1111/1475-6773.12117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sauermilch D, Siegel K, Hoppe T, Roth G, Meunier E. Attitudes towards HIV-positive status disclosure among U=U-aware sexual and gender minority individuals in the USA: a consensual qualitative research approach. Sex Res Social Policy. 2022: 1–13. doi: 10.1007/s13178-022-00710-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ending the HIV Epidemic in the U.S. (EHE). Centers for Disease Control and Prevention. Updated June 13, 2022. https://www.cdc.gov/endhiv/treat.html. Accessed July 20, 2022.
- 26.Kalichman SC, Kalichman MO, Easton LA. Undisclosed HIV status to sex partners and its unintended consequences in the era of Undetectable = Untransmittable. J Acquir Immune Defic Syndr. 2021;88(2): 149–156. doi: 10.1097/QAI.0000000000002762. [DOI] [PubMed] [Google Scholar]
- 27.Okoli C, Van de Velde N, Richman B, et al. Undetectable equals Untransmittable (U = U): awareness and associations with health outcomes among people living with HIV in 25 countries. Sex Trans Infect. 2021;97(1): 18–26. doi: 10.1136/sextrans-2020-054551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hascher K, Jaiswal J, Lorenzo J, et al. ‘Why aren’t you on PrEP? You’re a gay man’: reification of HIV ‘risk’ influences perception and behavior of young sexual minority men and medical providers. Cult Health Sex. 2021:1–15. DOI: 10.1080/13691058.2021.2018501 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Calabrese SK, Mayer KH, Marcus JL. Prioritising pleasure and correcting misinformation in the era of U=U. Lancet HIV. 2021;8(3): e175–e180. doi: 10.1016/S2352-3018(20)30341-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schwartz J, Grimm J. Investigating the content of #UequalsU on Twitter. Health Commun. 2021:1–9. doi: 10.1080/10410236.2021.2006395. [DOI] [PubMed] [Google Scholar]
- 31.Rivera AV, Carillo SA, Braunstein SL. Prevalence of U=U awareness and its association with anticipated HIV stigma among low-income heterosexually active black and Latino adults in New York City, 2019. AIDS Patient Care STDS. 2021;35(9): 370–376. doi: 10.1089/apc.2021.0070. [DOI] [PMC free article] [PubMed] [Google Scholar]


