Abstract
Purpose.
The purpose of this study was to assess differences in COVID-19 vaccine willingness and uptake between rural and nonrural adults, and within rural racial-ethnic groups.
Methods.
We utilized data from the COVID-19’s Unequal Racial Burden online survey, which included 1,500 Black/African American, Latino, and White rural adults (n=500 each). Baseline (12/2020-2/2021) and 6-month follow-up (8/2021-9/2021) surveys were administered. A cohort of nonrural Black/African American, Latino, and White adults (n=2,277) was created to compare differences between rural and nonrural communities. Multinomial logistic regression was used to assess associations between rurality, race-ethnicity, and vaccine willingness and uptake.
Findings.
At baseline, only 24.9% of rural adults were extremely willing to be vaccinated and 28.4% were not at all willing. Rural White adults were least willing to be vaccinated, compared to nonrural White adults (extremely willing: aOR=0.44, 95% CI=0.30-0.64). At follow-up, 69.3% of rural adults were vaccinated; however, only 25.3% of rural adults who reported being unwilling to vaccinate were vaccinated at follow-up, compared to 95.6% of adults who were extremely willing to be vaccinated and 76.3% who were unsure. Among those unwilling to vaccinate at follow-up, almost half reported distrust in the government (52.3%) and drug companies (46.2%); 80% reported that nothing would change their minds regarding vaccination.
Conclusions.
By August 2021 almost 70% of rural adults were vaccinated. However, distrust and misinformation were prevalent among those unwilling to vaccinate at follow-up. To continue to effectively combat COVID-19 in rural communities, we need to address misinformation to increase COVID-19 vaccination rates.
Keywords: COVID-19 vaccine, rural disparities, race/ethnicity, racial-ethnic disparities
Introduction
Vaccination remains one of the most effective measures against COVID-19 infection and mortality,1,2 yet COVID-19 vaccine hesitancy and uptake remains a concern in the United States3,4 as boosters continue to be recommended.5 As of November 30, 2022, 78.6% of adults ≥18 years old have been fully immunized in the United States (1 dose of the Johnson and Johnson vaccine or 2 doses of Pfizer or Moderna), and 13.9% adults have received an updated (bivalent) booster dose.6 While these numbers reflect that a majority of Americans have at least some protection from COVID-19, disparities in vaccination willingness and uptake have been observed within rural communities and racial-ethnic minorities,3,7-9 despite these groups being at higher risk for COVID-19 infection, hospitalization, and death.10-12 These disparities have been shown to be a result of both structural racism and social determinants of health which place racial-ethnic minorities at higher risk for both contracting COVID-19 and having worse outcomes once infected.11,13,14 Rural adults are also at increased risk for COVID-related morbidity and mortality because they are more likely to have comorbid conditions,15,16 less likely to have access to health facilities,17,18 and are on average older than those living in urban areas.19 These risk factors, among others, make rural adults more susceptible to COVID-19, particularly without the protection afforded with vaccination.20-22
We have previously reported notable differences by race-ethnicity in intent to be vaccinated using data from the nationally representative COVID-19’s Unequal Racial Burden (CURB) survey. Overall, we found that Black/African American adults were significantly less likely than White adults to report being extremely willing to be vaccinated, while English-speaking and Spanish-speaking Latino adults were as likely and more likely, respectively, than White adults to report being extremely willing to be vaccinated in early 2021.3 However, despite our study and others, it remains unclear how rural locale may intersect with race-ethnicity to impact vaccination willingness and uptake, which could provide important information to help tailor vaccination campaigns and community outreach. There are also relatively few studies which have assessed how initial COVID-19 vaccine willingness correlates with vaccination uptake,23,24 and none have been conducted among US adults. Thus, the purpose of this study was to 1) measure differences in vaccination willingness and uptake between rural and nonrural adults, 2) assess how vaccine willingness is associated with vaccination uptake among rural adults, and 3) identify the primary concerns surrounding vaccination, both before and after the vaccine was widely available to adults in the United States, among rural adults using data from a nationally representative sample of rural Black/African American, Latino (English- and Spanish-speaking), and White adults.
Methods
Survey Design and Study Populations
For this study, we utilized baseline and 6-month follow-up data from the COVID-19’s Unequal Racial Burden (CURB) online survey, which was conducted to measure the social, behavioral, and economic impact of the COVID-19 pandemic among diverse populations.3,25 Baseline surveys were completed between December 17, 2020 and February 17, 2021 and 6-month follow-up surveys were completed between August 16, 2021 and September 9, 2021. Of note, the Pfizer-BioNTech and Moderna COVID-19 vaccines were approved for emergency use authorization at the time of the baseline survey (December 11-18, 2020); however, the initial rollout was slow and vaccines were prioritized for individuals with in high-risk settings (e.g., healthcare providers, adults living in long-term care facilities)26 or adults with high-risk conditions (e.g., heart disease, cancer)27. Vaccines became available to all individuals ≥16 years old in all 50 states and Washington, D.C by April 19, 2021 (some states expanded eligibility earlier that month).28
The baseline CURB survey consisted of three separate cohorts: a nationally representative sample of all adults living in the U.S. (main sample, n=5,500), a nationally representative sample of rural Black/African American, Latino, and White rural adults (n=1,500), and a nationally representative sample of low-income Black/African American, Latino, and White low-income adults (n=1,500). The main, rural, and low-income samples were mutually exclusive; thus, in total, 8,500 adults were surveyed as part of the CURB study.
Additional information on the development of the baseline CURB survey has been detailed elsewhere.3,25 Briefly, all CURB survey participants were recruited from the YouGov proprietary, opt-in survey panel comprised of over 1.8 million US residents. To obtain nationally representative estimates of rural adults, YouGov first generated a theoretical cohort (target sample) of 1,500 rural adults from the 2016 Current Population Survey. Panel members who self-reported living in a rural residence (small town or rural area) were then proximity matched to the rural target sample until quotas were met, using race-ethnicity, gender, age, education, language preference (Latino sample only).
After quotas were met, survey weights for each racial-ethnic group were calculated using multivariable logistic regression, adjusting for age, gender, education, and Census region. Overall, this combination of weighting and matching allowed us to generate nationally representative cohorts of rural adults within each racial-ethnic group (e.g., rural White participants represent all rural White adults in the U.S.).
We created a nonrural comparison group by selecting the nonrural Black/African American, Latino, and White participants from the main sample. Of the 3,000 Black/African American, Latino, and White participants in the CURB main sample, we identified 840 nonrural Black/African American, 874 nonrural Latino, and 563 nonrural White adults (n=2,277). Additional weights for the nonrural comparison group were calculated to generate nationally representative estimates for these populations (e.g., nonrural Black/African American participants represent all nonrural Black/African American adults in the U.S.).
Vaccine Willingness, Concerns, and Uptake
Vaccine willingness and concerns were measured using two questions from the baseline survey. First, all participants were asked “If a COVID-19 vaccine becomes available, how likely are you to get vaccinated?” with response options including: not at all likely, slightly likely, moderately likely, very likely, and extremely likely. Responses were then collapsed into a 3-level variable for analysis (not at all, slightly likely/moderately likely/very likely [unsure], and extremely likely). This definition has been used previously.3 Vaccine concerns were assessed by asking, “Would any of the following concerns keep you from getting the vaccine?” Concerns included: concerns about the cost, not knowing where to get the vaccine, concerns about its safety, concerns about how effective it will be, concerns about side effects, other (specify), and I have no concerns about getting the vaccine. Written responses for “other concerns” that would keep them from getting a COVID-19 vaccine were independently coded by two coders to identify salient themes, create theme definitions, and select illustrative quotes. The coders then met until consensus was reached.
Vaccine uptake was measured in the 6-month follow-up survey; participants were asked “How would you describe your personal situation regarding COVID-19 vaccines?” with the following responses: I am fully vaccinated against COVID-19; I have started the vaccination process, but need another shot; I plan to get vaccinated; I will not get vaccinated; I’m not sure about getting vaccinated. Responses were again collapsed into a 3-level variable: vaccinated (fully or partially), planning to/unsure, and will not get vaccinated. Vaccination status was also dichotomized into vaccinated (fully or partially) and unvaccinated. Those who reported being fully or partially vaccinated (defined by the Centers for Disease Control and Prevention as having received the primary series at the time of the CURB surveys), were also asked which vaccine they received (Pfizer, Moderna, Johnson & Johnson, other [write-in response]), where they received their vaccine, and how difficult it was to get vaccinated (not at all difficult, slightly difficult, moderately difficult, very difficult, extremely difficult).
In the follow-up survey, individuals who reported they plan to get vaccinated, will not get vaccinated, or were unsure were again asked about their vaccination concerns. Concerns included all responses from the baseline survey, as well as: I plan to wait and see if it is safe and may get it later; I don’t believe I need a COVID-19 vaccine; I don’t like vaccines; my doctor has not recommended it; I don’t trust the government; I don’t trust the drug companies that developed the COVID-19 vaccines; I don’t trust the contents of the COVID-19 vaccines; I don’t trust the healthcare system. These responses were added after reviewing the write-in responses from all participants included in the baseline survey.3 Additionally, in the follow-up survey “concerns about how effective it will be” was expanded into two response options: 1) concerns about how effective it will be in general, and 2) concerns about how effective it will be against new variants. Finally, unvaccinated individuals were asked if there was anything that might help change their mind about being vaccinated (write-in). Participants who responded that nothing would change their mind (e.g., “No”, “Nothing. This hyped Covid pandemic is a hoax”, “Absolutely not. I am 100% against it”) were flagged and counted.
Statistical Analyses
Descriptive statistics and Chi-square tests were used to compare vaccine willingness between rural and nonrural adults, as well as across race-ethnicity, and vaccination concerns. Multinomial logistic regression was used to compare the odds of being unsure (slightly/moderately/very willing) or extremely willing, versus not at all willing, between rural and nonrural adults. Models were adjusted for race-ethnicity, age, gender, health insurance, chronic conditions associated with increased risk of COVID-19 morbidity and mortality (cancer diagnosis within the past year, chronic obstructive pulmonary disease, chronic kidney disease, diabetes, heart conditions, immunocompromised from transplant, obesity, and sickle cell anemia), self-rated physical health, education, and family annual income. Interaction terms were used to assess whether associations between rural status and vaccine willingness significantly differed by race-ethnicity (p-value only); However, race-ethnicity specific odds ratios were estimated using race-ethnicity specific models (i.e., the analysis which estimated the association between rural and nonrural White adults was restricted to only White participants). Estimates from the interaction term model and race-ethnicity specific analyses were consistent. All baseline analyses were weighted to obtain nationally representative estimates; counts were rounded for easier interpretation.
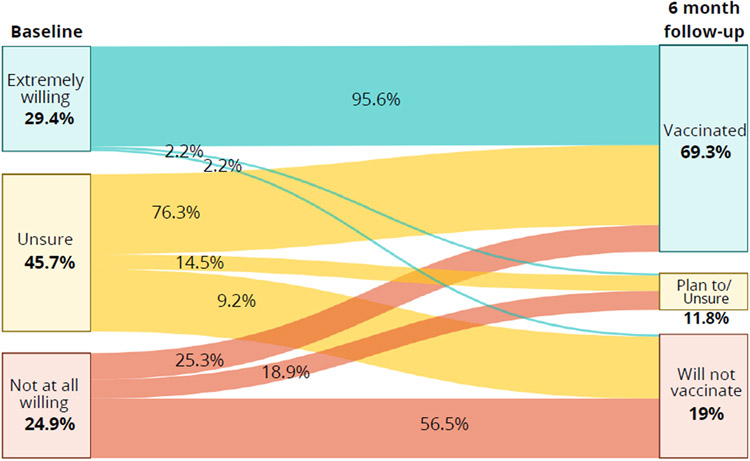
Chi-square tests were also used to compare differences in vaccination status at 6-month follow-up between rural and nonrural adults. Finally, Sankey plots were used to visualize the correlation between vaccine willingness at baseline and uptake at the 6-month follow-up among rural adults. Due to the smaller sample size at follow-up, follow-up analyses were unweighted.
Analyses were performed using SAS version 9.4 (SAS Inc., Cary, NC). The National Institutes of Health Office of IRB Operations determined that this study does not qualify as human subjects research because YouGov provided de-identified data.
Results
Demographics for the rural and nonrural samples, stratified by race-ethnicity, are reported in Supplemental Table 1.
Vaccine Willingness among Rural and Nonrural Adults
Overall, 24.9% of rural adults were extremely willing to be vaccinated, 46.7% were unsure, and 28.4% were not at all willing to be vaccinated. Compared to nonrural adults, rural adults were slightly less likely to be extremely willing (24.9% vs. 29.3%, p=0.003) and slightly more likely to be not at all willing (28.4% vs. 23.8%, p=0.002), Figure 1A. After adjusting for sociodemographics, rural adults, compared to nonrural adults, remained significantly less likely to be extremely willing to vaccinate (OR=0.71, 95% CI=0.58-0.87), Table 1.
Figure 1.
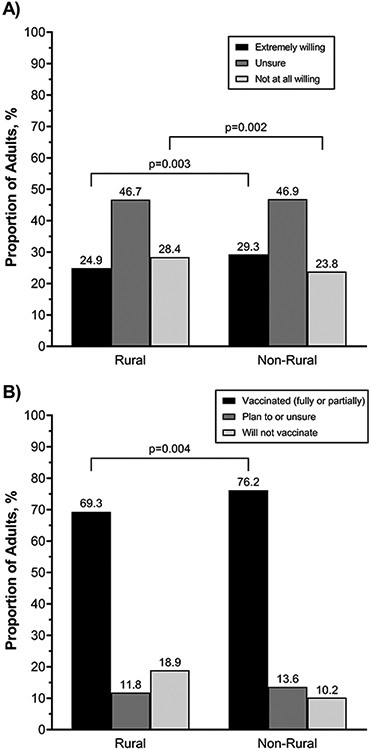
The prevalence of A) vaccine willingness between December 2020-February 2021, and B) vaccine uptake between August-September 2021 among rural and nonrural adults. Vaccine willingness analyses are weighted to be nationally representative within racial-ethnic groups; due to relatively low response rates, follow-up survey data is unweighted.
Table 1.
Adjusted association between rural status on willingness to vaccinate, overall and stratified by race-ethnicity, December 2020 – February 2021. Data is weighted to be nationally representative within racial-ethnic groups.
| Extremely Willing aOR (95% CI)a |
Unsure aOR (95% CI)a |
|
|---|---|---|
| Overall | 0.71 (0.58-0.87) | 0.88 (0.74-1.04) |
| Race-ethnicity b | ||
| Black/African American | 1.09 (0.74-1.61) | 1.65 (1.23-2.21) |
| Latino | 0.67 (0.47-0.94) | 0.59 (0.43-0.80) |
| White | 0.44 (0.30-0.64) | 0.57 (0.40-0.81) |
Abbreviations: aOR, adjusted odds ratio; CI, confidence interval
Adjusted for race/ethnicity age group, gender, insurance status, chronic conditions associated with increased risk of COVID-19 morbidity and mortality, self-reported physical health, education, and annual household income
Separate models were used to get race-ethnicity specific associations between rural status and vaccine willingness; results from model which included an interaction term between race-ethnicity and rural status produced consistent results
When results were stratified by race-ethnicity, the association between rurality and willingness differed across race-ethnicity (p<0.0001). White rural adults were substantially less likely to be extremely willing and unsure to be vaccinated, compared to not at all willing, than their nonrural counterparts (extremely willing: aOR=0.44, 95% CI=0.30-0.64; unsure: aOR=0.57, 95% CI=0.40-0.81), Table 1. Rural Latino adults were also less willing to be vaccinated compared to nonrural Latino adults (extremely willing: aOR=0.67, 95% CI=0.47-0.94; unsure: aOR=0.59, 95% CI=0.43-0.80). However, Black/African American adults were equally as likely to be extremely willing (aOR=1.09, 95% CI=0.74-1.61) and more likely to be unsure, compared to not at all willing (aOR=1.65, 95% CI=1.23-2.21) than nonrural Black/African American adults.
Vaccine Concerns among Rural Adults at Baseline
Side-effects (55.6%), safety (44.7%), and effectiveness (36.7%) were the most common vaccine concerns among rural adults at baseline. The prevalence of concerns varied substantially across baseline willingness. For example, rural adults who were extremely willing to be vaccinated were less likely to report concerns about side effects, compared to those unsure and not at all willing (28.2% vs. 64.5% and 63.6%, respectively, p<0.0001), Figure 2. Rural adults who were extremely willing to be vaccinated were also less likely to report concerns about safety (16.1% vs. 56.2% and 63.8%, p<0.0001), effectiveness (17.8% vs. 46.4% and 40.1%, p<0.0001), and more likely to report no concerns (53.5% vs. 14.5% and 15.9%, p<0.0001). Adults not at all willing to be vaccinated were more likely to report other concerns, compared to those extremely willing and unsure (12.7% vs. 1.7% and 2.7%, p<0.0001). Smaller differences were seen in vaccine concerns across race-ethnicity, with rural Black/African American adults being more likely to report most concerns, compared to Latino and White adults, Supplemental Figure 1.
Figure 2.
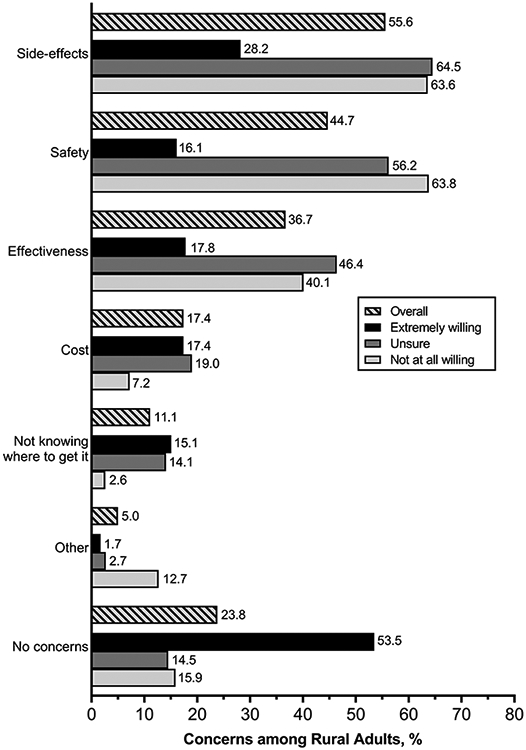
Vaccine concerns among rural adults, stratified by willingness to vaccinate, December 2020 – February 2021. Data is weighted to be nationally representative within racial-ethnic groups.
Vaccine Uptake among Rural and Nonrural Adults
Overall, 620 rural adults (41.3%) and 777 nonrural (34.1%) responded to the follow-up survey. By September 2021, over two-thirds of rural participants had received at least one dose of a COVID-19 vaccine; however, rural adults were less likely to be vaccinated compared to their nonrural counterparts (69.3% vs. 76.2%), p=0.004, Figure 1B. Rural White adults were significantly more likely to be not at all willing to vaccinate at follow-up, compared to rural Black/African American and Latino adults (23.8% vs. 12.8% and 15.6%, p=0.009); however, no significant differences were seen in vaccination rates across racial-ethnic groups (Black/African American: 69.5%, Latino: 73.3%, White: 66.8%, p=0.32), Supplemental Figure 2.
Among rural adults, half of those vaccinated (fully or partially) received Pfizer (50.1%;) and one-third received Moderna (37.5%). Three-quarters of rural vaccinated adults said it was “not at all difficult” to get vaccinated (74.6%), and <5% reported it was “very difficult” or “extremely difficult” (3.7%). Almost all rural adults who were extremely willing to be vaccinated received vaccines (95.6%), and among those who were unsure, three-fourths were vaccinated at follow-up (76.3%), Figure 3. Only 25.3% of rural adults who were not at all willing to be vaccinated had received a vaccine by late summer 2021.
Figure 3.
Vaccine willingness and uptake among rural adults. Vaccine willingness was assessed at baseline (December 2020 – February 2021) and vaccination status six months later (August – September 2021).
Vaccine Concerns at Follow-Up among Unvaccinated Rural Adults
At follow-up, rural adults who reported they would not vaccinate, compared to those who said they were unsure/plan to vaccinate, were more likely to have concerns about safety (67.5% vs. 50.7%, p=0.02), say they did not need the vaccine (43.6% vs. 15.1%, p<0.0001), and were more likely to say they did not trust the government (53.0% vs. 24.7%, p=0.0001), drug companies (46.2% vs. 21.9%, p=0.0008), vaccine contents (53.0% vs. 21.9%, p<0.0001), or the healthcare system (31.6% vs. 9.6%, p=0.0005), Figure 4. Overall, 81.7% of rural adults who said they would not get vaccinated stated in their open-text response that nothing would change their minds about getting vaccinated (data not shown).
Figure 4.
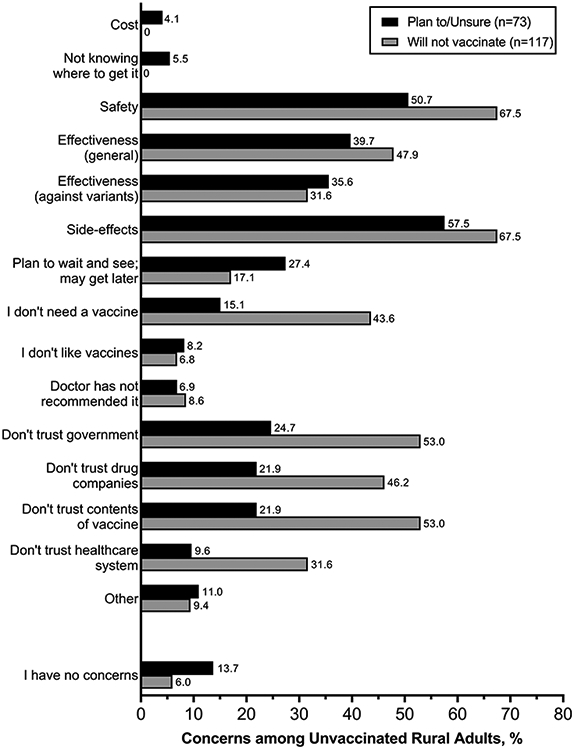
Prevalence of vaccine concerns among unvaccinated rural adults, stratified by vaccination intent at 6-month follow-up, August – September 2021.
Discussion
In a nationally representative cohort of 3,000 Black/African American, Latino (English- and Spanish-speaking), and White rural adults, roughly 25% were extremely willing to be vaccinated and 25% were not at all willing to be vaccinated in early 2021. Rural White adults were substantially less willing to be vaccinated for COVID-19 than their nonrural White counterparts. Relatively no differences were observed between rural and nonrural Black/African American and Latino adults. By late summer 2021, roughly 70% of rural adults had been vaccinated, which was lower than their nonrural (76%) counterparts. Again, rural White adults appeared less likely to be vaccinated than rural Black/African American and Latino adults, although differences were not statistically significant. Vaccine willingness at baseline was strongly associated with the likelihood of being vaccinated. Half of all rural adults who said they would not get vaccinated at follow-up also reported distrust in the government, drug companies, vaccine contents, and healthcare system, and over 80% said that nothing would change their minds about vaccination.
Overall, we found that 28% of rural adults were not at all willing to be vaccinated in early 2021, and that rural adults were less willing to be vaccinated than nonrural adults. These findings are consistent with prior studies on vaccine willingness during this time period.29-31 However, we found the most substantial differences in vaccination willingness were observed among rural White adults. To the best of our knowledge, this is the first study to break down COVID-19 vaccine willingness and uptake among rural adults by race-ethnicity and provides critical insight into how race-ethnicity and other social determinants of health interplay to impact health behaviors and attitudes.
In the 6-month follow-up survey, rural adults were less likely to be vaccinated compared to their nonrural (69% vs. 76%) counterparts. These findings are consistent with national vaccination data documenting lower initial uptake in rural adults.7,8,32 These trends have persisted, and even after almost a year of availability rural vaccine coverage (including boosters) continues to lag compared to nonrural communities.33 However, contrary to national trends,34 we found that that rural White adults were significantly more unwilling to vaccinate at our 6-month follow-up, compared to rural Black/African American and Latino adults. Interestingly, these differences appeared even though vaccine concerns in early 2021 among rural White adults were similar to their rural Black/African American and Latino counterparts. To date, no other reports have stratified rural vaccination willingness or uptake by race-ethnicity, which has limited our ability to create targeted vaccination campaigns in these communities.
Interestingly, we found that Latinos were the most likely to be extremely willing in our rural group, despite having similar prevalence of concerns as Black/African American and White adults. This trend was also seen among our nationally representative, main cohort in the CURB survey.3 Despite this, reports have shown that vaccination rates initially lagged for Latinos,9,34 indicating that there were disparities in initial access to the vaccinations and more barriers experienced by Latino adults, compared to other racial-ethnic groups. Similar lags in booster vaccinations are now being observed among Latinos (and Black/African Americans), suggesting that barriers may still persist.34-36 Creating more equitable access by reducing barriers37 and improving individual and health system readiness38 must remain a priority for COVID-19 vaccination programs in order to protect communities disproportionately affected by COVID-19.10,36
The correlation between vaccine willingness in early 2021, before the vaccines were even widely available, and vaccination status 6-months later provides critical insight and highlights both the successes and failures of the U.S. vaccination efforts. First, over 90% of rural adults who were extremely willing were able get at least one dose within the first 6 months of the rollout. Additionally, 75% of adults who were initially unsure, and 25% of adults who were not at all willing in early 2021 ultimately went on to receive at least one dose of the COVID-19 vaccine. Together these findings, as well as others, highlight that 1) vaccinations appeared to be available to those interested in receiving them by summer 202128,36 and 2) some minds were able to be changed regarding COVID-19 vaccination.39-42 Additional research is needed to determine what role educational campaigns, observing friends and family safely receive vaccines, work- and travel-related vaccine mandates, and other mechanisms played in getting these individuals to ultimately choose to be vaccinated.
Conversely, half of participants who were not at all willing remained unwilling to vaccinate six months later. Side-effects, safety, and effectiveness were the most common concerns among rural adults before the vaccine was available, consistent with the vaccine concerns identified in our nationally representative sample3 and with other studies.43,44 These concerns remained some of the most prevalent at our 6-month follow-up, indicating that educational campaigns did not alleviate these concerns among those unvaccinated. However, the impact of misinformation45,46 and politicization47 of COVID-19 vaccines in the U.S. cannot be understated. In our sample, half of the rural adults who said they would not get vaccinated at follow-up reported distrust in the government, drug companies, vaccine contents, and healthcare systems. Over 80% reported that nothing would change their mind about vaccination. Distrust in the government, vaccine contents and process, and belief that the vaccine and/or COVID-19 was a government conspiracy were also common concerns prior to vaccine rollout in our nationally representative CURB sample3; other studies have also found vaccine misinformation impacted vaccination willingness and uptake.45,46 While combating misinformation, particularly on social media,48,49 has proven to be incredibly challenging, it is of critical importance to continue to identify successful strategies for combating misinformation in order to reduce its impact on public health.50
This study is not without limitations. First, the survey was conducted online; however, participants were recruited through a variety of methods, and rural individuals were intentionally over-sampled to produce national estimates. We were unable to recruit enough rural Spanish-speaking Latinos to meet our enrollment goals, and thus could not conduct language-specific analyses among our rural Latino cohort. We also only conducted the survey in English and Spanish (Latinos only); other languages were excluded. Third, rural and nonrural status was determined using self-report; however, at least one study has found that self-reported rural status has relatively good concordance with ZIP-code derived Rural-Urban Category of Community (RUCA) codes (only 7% of adults living in a large rural, small rural, or isolated ZIP code incorrectly reported living in an urban area [20/280]).51 Fourth, response rates for the 6-month follow-up surveys were relatively low, 41.3% for rural adults, and we were unable to weight our follow-up analyses to be nationally representative. However, this is one of the first studies which has resampled participants, allowing us to directly link initial willingness and uptake at an individual level. Finally, our follow-up survey was conducted in August/September 2021 and these results may not represent current trends.
Despite these limitations, this study is one of the first nationally representative surveys among rural Black/African American, Latino, and White adults and provides an important baseline metric at the time when vaccines were not readily available and compares it to post-deployment vaccine uptake that can inform vaccination promotion efforts. We are also one of the first to directly link individual-level willingness and vaccination status, providing critical insight into vaccination efforts and how initial willingness to vaccinate correlated to actual vaccine uptake six months later.
In conclusion, while rural White adults were least willing to be vaccinated, compared to their nonrural counterparts, these differences are not seen in Black/African American and Latino adults. Individuals who were not at all willing to vaccinate prior to the availability of COVID-19 vaccines remained unwilling to vaccinate 6 months after they were available; moreover, half of all rural adults who were unwilling to vaccinate reported distrust in the government, drug companies, vaccine contents, and healthcare system. Taken together, these findings further highlight the impact misinformation and the politization of the COVID-19 vaccination has had in the U.S. As vaccination and boosters continue to be one of the primary methods for combating the COVID-19 pandemic, increasing access to vaccination among marginalized communities and combating misinformation remains vital to improving vaccine willingness and uptake among these communities.
Supplementary Material
Acknowledgements.
Research support was provided by the NIH Medical Research Scholars Program, a public-private partnership supported jointly by the NIH and contributions to the Foundation for the NIH from the American Association for Dental Research and the Colgate-Palmolive Company.
Funding sources.
This work was supported by the Division of Intramural Research, National Institute on Minority Health and Health Disparities, National Institutes of Health. Mr. Colbert was also supported by the Division of Intramural Research, National Institute of Neurological Disorders and Stroke, National Institutes of Health. Dr. Stewart was also supported by the National Institute on Aging, National Institutes of Health [grant number 2 P30 AG015272]. The funding sources had no role in the design or conduct of the study, or in the analysis and interpretation of results.
Footnotes
Disclosures. The authors report no conflicts of interest.
Disclaimer. The opinions expressed in this article are the authors’ and do not reflect the views of the National Institutes of Health, the Department of Health and Human Services, or the United States government.
References
- 1.Christie A, Henley SJ, Mattocks L, et al. Decreases in COVID-19 Cases, Emergency Department Visits, Hospital Admissions, and Deaths Among Older Adults Following the Introduction of COVID-19 Vaccine - United States, September 6, 2020-May 1, 2021. MMWR Morb Mortal Wkly Rep. Jun 11 2021;70(23):858–864. doi: 10.15585/mmwr.mm7023e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pilishvili T, Fleming-Dutra KE, Farrar JL, et al. Interim Estimates of Vaccine Effectiveness of Pfizer-BioNTech and Moderna COVID-19 Vaccines Among Health Care Personnel - 33 U.S. Sites, January-March 2021. MMWR Morb Mortal Wkly Rep. May 21 2021;70(20):753–758. doi: 10.15585/mmwr.mm7020e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nápoles AM, Stewart AL, Strassle PD, et al. Racial/ethnic disparities in intent to obtain a COVID-19 vaccine: A nationally representative United States survey. Preventive Medicine Reports. 2021/December/01/ 2021;24:101653. doi: 10.1016/j.pmedr.2021.101653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bunch L A Tale of Two Crises: Addressing Covid-19 Vaccine Hesitancy as Promoting Racial Justice. HEC Forum. Jun 2021;33(1–2):143–154. doi: 10.1007/s10730-021-09440-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Johnson AG. COVID-19 incidence and death rates among unvaccinated and fully vaccinated adults with and without booster doses during periods of Delta and Omicron variant emergence—25 US Jurisdictions, April 4–December 25, 2021. MMWR Morbidity and mortality weekly report. 2022;71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Prevention CfDCa. COVID-19 Vaccinations in the United States. Accessed 08/13/2021, https://covid.cdc.gov/covid-data-tracker/#vaccinations_vacc-total-admin-rate-total [Google Scholar]
- 7.Barry V, Dasgupta S, Weller DL, et al. Patterns in COVID-19 Vaccination Coverage, by Social Vulnerability and Urbanicity - United States, December 14, 2020-May 1, 2021. MMWR Morb Mortal Wkly Rep. Jun 4 2021;70(22):818–824. doi: 10.15585/mmwr.mm7022e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Murthy BP, Sterrett N, Weller D, et al. Disparities in COVID-19 Vaccination Coverage Between Urban and Rural Counties - United States, December 14, 2020-April 10, 2021. MMWR Morb Mortal Wkly Rep. May 21 2021;70(20):759–764. doi: 10.15585/mmwr.mm7020e3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Pingali C, Meghani M, Razzaghi H, et al. COVID-19 Vaccination Coverage Among Insured Persons Aged ≥16 Years, by Race/Ethnicity and Other Selected Characteristics - Eight Integrated Health Care Organizations, United States, December 14, 2020-May 15, 2021. MMWR Morb Mortal Wkly Rep. Jul 16 2021;70(28):985–990. doi: 10.15585/mmwr.mm7028a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mackey K, Ayers CK, Kondo KK, et al. Racial and Ethnic Disparities in COVID-19-Related Infections, Hospitalizations, and Deaths : A Systematic Review. Annals of internal medicine. Mar 2021;174(3):362–373. doi: 10.7326/m20-6306 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Webb Hooper M, Nápoles AM, Pérez-Stable EJ. COVID-19 and Racial/Ethnic Disparities. Jama. Jun 23 2020;323(24):2466–2467. doi: 10.1001/jama.2020.8598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Shiels MS, Haque AT, Haozous EA, et al. Racial and Ethnic Disparities in Excess Deaths During the COVID-19 Pandemic, March to December 2020. Annals of internal medicine. Oct 5 2021;doi: 10.7326/m21-2134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Romano SD, Blackstock AJ, Taylor EV, et al. Trends in Racial and Ethnic Disparities in COVID-19 Hospitalizations, by Region - United States, March-December 2020. MMWR Morb Mortal Wkly Rep. Apr 16 2021;70(15):560–565. doi: 10.15585/mmwr.mm7015e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dasgupta S, Bowen VB, Leidner A, et al. Association Between Social Vulnerability and a County's Risk for Becoming a COVID-19 Hotspot - United States, June 1-July 25, 2020. MMWR Morb Mortal Wkly Rep. Oct 23 2020;69(42):1535–1541. doi: 10.15585/mmwr.mm6942a3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Weaver KE, Geiger AM, Lu L, Case LD. Rural-urban disparities in health status among US cancer survivors. Cancer. Mar 1 2013;119(5):1050–7. doi: 10.1002/cncr.27840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mercado CI, McKeever Bullard K, Gregg EW, Ali MK, Saydah SH, Imperatore G. Differences in U.S. Rural-Urban Trends in Diabetes ABCS, 1999-2018. Diabetes Care. Aug 2021;44(8):1766–1773. doi: 10.2337/dc20-0097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kaufman BG, Thomas SR, Randolph RK, et al. The Rising Rate of Rural Hospital Closures. J Rural Health. Winter 2016;32(1):35–43. doi: 10.1111/jrh.12128 [DOI] [PubMed] [Google Scholar]
- 18.Graves JM, Abshire DA, Alejandro AG. System- and Individual-Level Barriers to Accessing Medical Care Services Across the Rural-Urban Spectrum, Washington State. Health Serv Insights. 2022;15:11786329221104667. doi: 10.1177/11786329221104667 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Smith AS, Trevelyan E. The older population in rural America: 2012-2016. US Department of Commerce, Economics and Statistics Administration, US; …; 2019. [Google Scholar]
- 20.Anzalone AJ, Horswell R, Hendricks BM, et al. Higher hospitalization and mortality rates among SARS-CoV-2-infected persons in rural America. J Rural Health. Jun 27 2022;doi: 10.1111/jrh.12689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Denslow S, Wingert JR, Hanchate AD, et al. Rural-urban outcome differences associated with COVID-19 hospitalizations in North Carolina. PLoS One. 2022;17(8):e0271755. doi: 10.1371/journal.pone.0271755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Accorsi EK, Britton A, Fleming-Dutra KE, et al. Association Between 3 Doses of mRNA COVID-19 Vaccine and Symptomatic Infection Caused by the SARS-CoV-2 Omicron and Delta Variants. JAMA. 2022;327(7):639–651. doi: 10.1001/jama.2022.0470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nguyen LH, Joshi AD, Drew DA, et al. Self-reported COVID-19 vaccine hesitancy and uptake among participants from different racial and ethnic groups in the United States and United Kingdom. Nature Communications. 2022/February/01 2022;13(1):636. doi: 10.1038/s41467-022-28200-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Siegler AJ, Luisi N, Hall EW, et al. Trajectory of COVID-19 Vaccine Hesitancy Over Time and Association of Initial Vaccine Hesitancy With Subsequent Vaccination. JAMA Network Open. 2021;4(9):e2126882–e2126882. doi: 10.1001/jamanetworkopen.2021.26882 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Strassle PD, Stewart AL, Quintero SM, et al. COVID-19–Related Discrimination Among Racial/Ethnic Minorities and Other Marginalized Communities in the United States. American Journal of Public Health. 2022;112(3):453–466. doi: 10.2105/ajph.2021.306594 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.The COVID-19 “Vaccination Line”: An Update on State Prioritization Plans. Kaiser Family Foundation; 2021. https://www.kff.org/coronavirus-covid-19/issue-brief/the-covid-19-vaccination-line-an-update-on-state-prioritization-plans/ [Google Scholar]
- 27.States Set Different COVID-19 Vaccination Priorities for People with High-Risk Conditions. Kaiser Family Foundation; 2021. https://www.kff.org/coronavirus-covid-19/press-release/states-set-different-covid-19-vaccination-priorities-for-people-with-high-risk-conditions/ [Google Scholar]
- 28.Schumaker E All US adults now eligible for COVID-19 vaccines. ABCNews. April/19/2021. https://abcnews.go.com/Health/adults-now-eligible-covid-19-vaccines/story?id=77163212 [Google Scholar]
- 29.Fisher KA, Bloomstone SJ, Walder J, Crawford S, Fouayzi H, Mazor KM. Attitudes Toward a Potential SARS-CoV-2 Vaccine : A Survey of U.S. Adults. Annals of internal medicine. Dec 15 2020;173(12):964–973. doi: 10.7326/m20-3569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gatwood J, McKnight M, Fiscus M, Hohmeier KC, Chisholm-Burns M. Factors influencing likelihood of COVID-19 vaccination: A survey of Tennessee adults. Am J Health Syst Pharm. May 6 2021;78(10):879–889. doi: 10.1093/ajhp/zxab099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shih SF, Wagner AL, Masters NB, Prosser LA, Lu Y, Zikmund-Fisher BJ. Vaccine Hesitancy and Rejection of a Vaccine for the Novel Coronavirus in the United States. Front Immunol. 2021;12:558270. doi: 10.3389/fimmu.2021.558270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Sun Y, Monnat SM. Rural-urban and within-rural differences in COVID-19 vaccination rates. The Journal of Rural Health. n/a(n/a)doi: 10.1111/jrh.12625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Saelee R, Zell E, Murthy BP, et al. Disparities in COVID-19 Vaccination Coverage Between Urban and Rural Counties - United States, December 14, 2020-January 31, 2022. MMWR Morb Mortal Wkly Rep. Mar 4 2022;71(9):335–340. doi: 10.15585/mmwr.mm7109a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kriss JL, Hung MC, Srivastav A, et al. COVID-19 Vaccination Coverage, by Race and Ethnicity - National Immunization Survey Adult COVID Module, United States, December 2020-November 2021. MMWR Morb Mortal Wkly Rep. Jun 10 2022;71(23):757–763. doi: 10.15585/mmwr.mm7123a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fast HE, Zell E, Murthy BP, et al. Booster and Additional Primary Dose COVID-19 Vaccinations Among Adults Aged ≥65 Years - United States, August 13, 2021-November 19, 2021. MMWR Morb Mortal Wkly Rep. Dec 17 2021;70(50):1735–1739. doi: 10.15585/mmwr.mm7050e2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ndugga N, Hill L, Artiga S, Parker N. Latest Data on COVID-19 Vaccinations by Race/Ethnicity. Accessed 7/28/2021, https://www.kff.org/coronavirus-covid-19/issue-brief/latest-data-on-covid-19-vaccinations-race-ethnicity/ [Google Scholar]
- 37.Wong CA, Dowler S, Moore AF, et al. COVID-19 Vaccine Administration, by Race and Ethnicity - North Carolina, December 14, 2020-April 6, 2021. MMWR Morb Mortal Wkly Rep. Jul 16 2021;70(28):991–996. doi: 10.15585/mmwr.mm7028a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Grumbach K, Carson M, Harris OO. Achieving Racial and Ethnic Equity in COVID-19 Vaccination: From Individual Readiness to Health System Readiness. JAMA Health Forum. 2021;2(7):e211724–e211724. doi: 10.1001/jamahealthforum.2021.1724 [DOI] [PubMed] [Google Scholar]
- 39.Daly M, Jones A, Robinson E. Public Trust and Willingness to Vaccinate Against COVID-19 in the US From October 14, 2020, to March 29, 2021. JAMA. 2021;doi: 10.1001/jama.2021.8246 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lin C, Tu P, Beitsch LM. Confidence and Receptivity for COVID-19 Vaccines: A Rapid Systematic Review. Vaccines. 2020;9(1):16. doi: 10.3390/vaccines9010016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nguyen KH, Srivastav A, Razzaghi H, et al. COVID-19 Vaccination Intent, Perceptions, and Reasons for Not Vaccinating Among Groups Prioritized for Early Vaccination - United States, September and December 2020. MMWR Morb Mortal Wkly Rep. Feb 12 2021;70(6):217–222. doi: 10.15585/mmwr.mm7006e3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Rane MS, Kochhar S, Poehlein E, et al. Determinants and Trends of COVID-19 Vaccine Hesitancy and Vaccine Uptake in a National Cohort of US Adults: A Longitudinal Study. American Journal of Epidemiology. 2022;191(4):570–583. doi: 10.1093/aje/kwab293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Khubchandani J, Sharma S, Price JH, Wiblishauser MJ, Sharma M, Webb FJ. COVID-19 Vaccination Hesitancy in the United States: A Rapid National Assessment. Journal of Community Health. 2021;46(2):270–277. doi: 10.1007/s10900-020-00958-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pogue K, Jensen JL, Stancil CK, et al. Influences on Attitudes Regarding Potential COVID-19 Vaccination in the United States. Vaccines. 2020;8(4):582. doi: 10.3390/vaccines8040582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Loomba S, De Figueiredo A, Piatek SJ, De Graaf K, Larson HJ. Measuring the impact of COVID-19 vaccine misinformation on vaccination intent in the UK and USA. Nature Human Behaviour. 2021;doi: 10.1038/s41562-021-01056-1 [DOI] [PubMed] [Google Scholar]
- 46.Earnshaw VA, Eaton LA, Kalichman SC, Brousseau NM, Hill EC, Fox AB. COVID-19 conspiracy beliefs, health behaviors, and policy support. Translational Behavioral Medicine. 2020;10(4):850–856. doi: 10.1093/tbm/ibaa090 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Stroebe W, vanDellen MR, Abakoumkin G, et al. Politicization of COVID-19 health-protective behaviors in the United States: Longitudinal and cross-national evidence. PLoS One. 2021;16(10):e0256740. doi: 10.1371/journal.pone.0256740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Vosoughi S, Roy D, Aral S. The spread of true and false news online. Science. 2018;359(6380):1146–1151. doi:doi: 10.1126/science.aap9559 [DOI] [PubMed] [Google Scholar]
- 49.Ahmed S, Rasul ME, Cho J. Social Media News Use Induces COVID-19 Vaccine Hesitancy Through Skepticism Regarding Its Efficacy: A Longitudinal Study From the United States. Front Psychol. 2022;13:900386. doi: 10.3389/fpsyg.2022.900386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.van der Linden S, Dixon G, Clarke C, Cook J. Inoculating against COVID-19 vaccine misinformation. eClinicalMedicine. 2021;33doi: 10.1016/j.eclinm.2021.100772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Onega T, Weiss JE, Alford-Teaster J, Goodrich M, Eliassen MS, Kim SJ. Concordance of Rural-Urban Self-identity and ZIP Code-Derived Rural-Urban Commuting Area (RUCA) Designation. J Rural Health. Mar 2020;36(2):274–280. doi: 10.1111/jrh.12364 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.