Abstract
OBJECTIVE:
Annual influenza vaccination rates for children remain well below the Healthy People 2030 target of 70%. We aimed to compare influenza vaccination rates for children with asthma by insurance type and to identify associated factors.
METHODS:
This cross-sectional study examined influenza vaccination rates for children with asthma by insurance type, age, year, and disease status using the Massachusetts All Payer Claims Database (2014–2018). We used multivariable logistic regression to estimate the probability of vaccination accounting for child and insurance characteristics.
RESULTS:
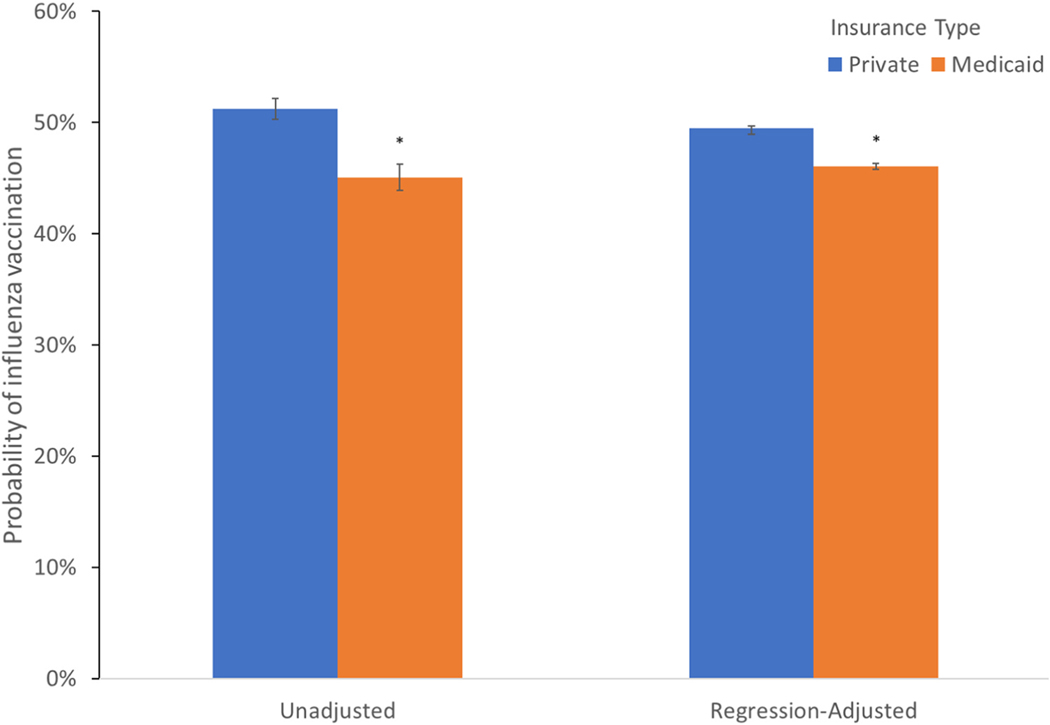
The sample included 317,596 child-year observations for children with asthma in 2015–18. Fewer than half of children with asthma received influenza vaccinations; 51.3% among privately insured and 45.1% among Medicaid insured. Risk modeling reduced, but did not eliminate, this gap; privately insured children were 3.7 percentage points (pp) more likely to receive an influenza vaccination than Medicaid-insured children (95% confidence interval [CI]: 2.9–4.5pp). Risk modeling also found persistent asthma was associated with more vaccinations (6.7pp higher; 95% CI: 6.2–7.2pp), as was younger age. The regression-adjusted probability of influenza vaccination in a non-office setting was 3.2pp higher in 2018 than 2015 (95% CI: 2.2–4.2pp), and significantly lower for children with Medicaid.
CONCLUSIONS:
Despite clear recommendations for annual influenza vaccinations for children with asthma, low rates persist, particularly for children with Medicaid. Offering vaccines in non-office settings such as retail pharmacies may reduce barriers, but we did not observe increased vaccination rates in the first years after this policy change.
Keywords: asthma, Medicaid, vaccination
AN ESTIMATED 5.1 MILLION children in the United States had asthma, the most common chronic disease of childhood, in 2019.1 Half of children with asthma do not have well-controlled disease, resulting in hospitalizations, emergency department visits, missed school days, lower quality of life and missed workdays for parents.2 Children in lower-income, Black, and Puerto Rican communities who have asthma receive disproportionately lower quality of care and have worse health outcomes.3 Annual influenza vaccination has been recommended as part of a comprehensive strategy for preventing asthma-associated morbidity for more than 30 years.4,5 Although influenza vaccination rates have increased overall during this time period, rates remain well below the Healthy People 2030 target of 70%.6 These rates remain low despite interventions to address barriers to influenza vaccine uptake in this population.7,8 In addition to the suboptimal vaccination rates identified, these studies have also identified potential barriers to vaccination at multiple system levels. Examples of potential barriers identified include parent lack of awareness of recommendations, concerns about side effects, and trust in physician, continuity of care with a primary care clinician, provider lack of awareness of recommendations, and lack of systems for identifying children in need of vaccination and for tracking vaccination.9
Prior studies of influenza vaccine rates for children with asthma have largely focused on children insured by Medicaid10–13 because of the high prevalence of children with higher risk for poor asthma outcomes in the Medicaid population. However, we are aware of no recent studies that have compared vaccination rates for privately insured children with asthma to rates for Medicaid-insured children using insurance claims data for a large population, a potentially important and actionable inequity in preventive asthma care.14 Additionally, recent policy changes increasing availability of influenza vaccination have the potential to affect vaccination rates for children with asthma. Massachusetts began allowing retail pharmacies to administer vaccinations to children aged 9 years and older in May 2017.15
This study’s objective was to compare influenza vaccine rates for children insured by Medicaid to privately insured children in Massachusetts over the 2015–18 period and to identify patterns of location of care that may help to identify opportunities for improving influenza vaccination rates for children with asthma as well as potential barriers.
METHODS
Data and Analytic Sample: We used health insurance enrollment and claims data from 2014 to 2018 from the Massachusetts All-Payer Claims Database v8.0, maintained by the Massachusetts Center for Health Information and Analysis.16 This database includes claims data from many private insurers, Medicaid, and Medicaid managed care, including clinical encounters and pharmacy data. We limited the analytic18 sample to child-year observations for children aged 2–17 years in a given calendar year who met criteria for having asthma in that year.
Criteria for having asthma in a calendar year were adapted from prior studies using claims data to study asthma in children.17,18 Children with asthma were identified if they met at least one of the following five criteria (see Supplemental Appendix Table 1 for International Classification of Diseases, Ninth Revision [ICD-9] and ICD-10 codes18): 1) one or more claims in an inpatient setting with any diagnosis of asthma, 2) one or more claims in an emergency department setting with any diagnosis of asthma, 3) one or more claims in the hospital observation setting with any diagnosis of asthma, 4) two or more claims in an ambulatory care setting with any diagnosis of asthma, or 5) at least one claim in an ambulatory care setting with any diagnosis of asthma and at least one filled prescription for any asthma-related medication.19
Asthma-related prescriptions included rescue medications (short-acting β2-agonists including both aerosol inhalers, oral, and respiratory/inhalation albuterol sulfate) and controller medications (long-acting β2-agonist or inhaled corticosteroid, anti-asthmatic combinations, methylxanthines, or mast-cell stabilizers).13 Patients with diagnoses of cystic fibrosis, chronic obstructive pulmonary disease, or emphysema were excluded.13,18
We excluded child-year observations in which we did not have information on the child’s primary medical insurance, when there were technical errors in the claims or eligibility files, if they did not have at least 7 months of primary insurance in the calendar year, or they were not a Massachusetts resident for at least 6 months of the calendar year. Our analytic sample includes child-year observations in 2015–18; we used the 2014 data to determine whether children met criteria for persistent asthma as defined below.
MEASURES
Our primary outcome was a binary indicator of the receipt of at least one influenza vaccine within a calendar year, ascertained using Current Procedural Terminology (CPT) codes; ICD-9; and National Drug Codes (Supplemental Appendix Table 2).20,21 We also determined where influenza vaccine was delivered for children who had received vaccine in each year using site of service codes and pharmacy claims. We characterized vaccinations occurring in an office setting versus a non-office setting (Supplemental Appendix Table 3); the non-office setting includes settings such as emergency departments, acute care hospitals, and freestanding urgent care centers as well as influenza vaccinations that were administered in a retail pharmacy.
The key independent variable was a binary indicator of insurance type (Medicaid vs private). To assess the independent association between insurance type and receipt of influenza vaccine, we adjusted for age category (i.e., 2–4 years, 5–9 years, 10–14 years, 15–17 years), sex, calendar year, persistent asthma (yes/no), health status, and 5-digit ZIP code of patient residence. Children in the asthma cohort were classified as having persistent asthma, consistent with the Healthcare Effectiveness Data and Information Set (HEDIS) metric,22 when they met at least one of the following criteria in the calendar year and the year prior: 1) at least one inpatient visit with a principal diagnosis of asthma, 2) at least one emergency department visit with a principal diagnosis of asthma, 3) at least four ambulatory care visits or hospital observation visits on different dates of service with any diagnosis of asthma and at least two prescriptions fills on different dates for asthma-related medications as described above, or 4) at least four prescription fills on different dates for asthma-related medications.19
To account for health status, we used binary indicators of hierarchical condition categories, calculated using the Health and Human Services-developed hierarchical condition category algorithms for each calendar year distributed by Centers for Medicare and Medicaid Services.23 We excluded the asthma category from the hierarchical condition categories to avoid collinearity in our models.
STATISTICAL ANALYSES
We first calculated descriptive statistics and used chi-squared tests to detect statistically significant differences between child-year observations in which an influenza vaccination was received versus not.
We estimated bivariate logistic regression models where the outcome was whether or not the child received an influenza vaccination. We estimated separate models for each independent variable of interest: child age, whether or not the child had persistent asthma, insurance type, and calendar year. We report the predicted probability for each category, with statistically significant observed differences across categories calculated using average marginal effects.
We then estimated a multivariable logistic regression model including the key independent variables, as well as indicators of health status (i.e., binary indicators of hierarchical condition categories) and fixed effects for patient residence 5-digit ZIP code to account for time-invariant community-level characteristics such as physician and retail pharmacy supply, socioeconomic characteristics, and population demographics. We used this model to estimate the regression adjusted predicted probability of influenza vaccination by age, insurance type, persistent asthma, and calendar year. We calculated the predicted probability of influenza vaccination for each category. For example, to examine the predicted probability of influenza vaccination by each age category, we used model estimates to calculate adjusted probabilities of the outcomes by computing the mean of predicted probabilities for the entire sample after setting the age category to be 2–4 years, and then to be 5–9 years, and so on, while keeping all other covariates at their observed values.
We additionally examined the site of care in which an influenza vaccination occurred, classifying these as office versus non-office (including retail pharmacy) settings. We report site of vaccination by calendar year in unadjusted and regression-adjusted analyses as described above for those receiving any influenza vaccination. The multivariable logistic regression model has the binary outcome of receipt of influenza vaccination in a non-office setting for those receiving influenza vaccination within a calendar year, with the same independent variables used as for our primary analysis and patient 3-digit ZIP code fixed effects. We also calculate unadjusted analyses of whether children with an influenza vaccination in a non-office setting received an influenza vaccination the year prior, for all children with asthma and for those with persistent asthma.
Vaccines provided to practices by the federal Vaccines for Children (VFC) program and the state Department of Public Health (DPH) can be administered to children with Medicaid (VFC and DPH) and with private insurance (DPH). In Massachusetts, the state Medicaid program and most private insurers pay for the administration of vaccinations under a separate CPT code with a modifier for whether vaccines were provided to the practice for free. As these CPT codes are not specific to influenza vaccination, we do not include them in the primary analysis. We conduct a sensitivity analysis in which we include these as influenza vaccinations if administered between September and January (Supplemental Appendix for details).
For each model, standard errors were clustered at the patient 5-digit ZIP code level (3-digit ZIP code for non-office setting models). The delta method was used to calculate standard errors for predicted probabilities and average marginal effects. An alpha of 0.05 was considered significant. Analyses were conducted in SAS 9.1 (SAS Corporation; Cary, North Carolina) and Stata-MP 16.0 (StataCorp; College Station, Texas).
RESULTS
The analytic sample included 317,596 child-year observations with asthma for 171,416 unique children (Table 1). Of these child-year observations, 64.4% were publicly insured (i.e., Medicaid and Medicaid managed care) and 35.6% were privately insured; 56.9% were male. Around 13% had any hierarchical condition category (excluding asthma), with the most common being autistic disorder (2.8%) and major depressive and bipolar disorders (1.9%). Less than half (47.3%) received an influenza vaccination, with 51.3% among those privately insured and 45.1% for those with Medicaid insurance. The descriptive statistics show influenza vaccination was statistically significantly more common for those with private insurance (P < 0.001), children with persistent asthma (P < 0.001), children with any hierarchical condition category (P < 0.001), and younger children (P < 0.001).
Table 1.
Descriptive Statistics of Children With Asthma With and Without Influenza Vaccinations (2015–2018)
| Number of observations (%) | Influenza Vaccination |
||||||
|---|---|---|---|---|---|---|---|
| Overall |
Yes |
No |
|||||
| (N = 317,596) | (N = 150,186) | (N = 167,410) | P-value | ||||
|
| |||||||
| Influenza vaccination (binary) | 150,186 | (47.3) | 150,186 | (100.0) | 0 | (0.0) | |
| Insurance type | |||||||
| Medicaid | 204,573 | (64.4) | 92,223 | (61.4) | 112,350 | (67.1) | < 0.0001 |
| Private | 113,023 | (35.6) | 57,963 | (38.6) | 55,060 | (32.9) | |
| Child age | |||||||
| 2–4 y | 59,323 | (18.7) | 29,863 | (19.9) | 29,460 | (17.6) | < 0.0001 |
| 5–9 y | 112,876 | (35.5) | 54,449 | (36.3) | 58,427 | (34.9) | |
| 10–14 y | 100,599 | (31.7) | 47,078 | (31.4) | 53,521 | (32.0) | |
| 15–17 y | 44,798 | (14.1) | 18,796 | (12.5) | 26,002 | (15.5) | |
| Sex | |||||||
| Male | 180,628 | (56.9) | 85,939 | (57.2) | 94,689 | (56.6) | 0.0002 |
| Female | 136,968 | (43.1) | 64,247 | (42.8) | 72,721 | (43.4) | |
| Year | |||||||
| 2015 | 87,466 | (27.5) | 42,567 | (28.3) | 44,899 | (26.8) | < 0.0001 |
| 2016 | 79,243 | (25.0) | 36,780 | (24.5) | 42,463 | (25.4) | |
| 2017 | 78,827 | (24.8) | 35,901 | (23.9) | 42,926 | (25.6) | |
| 2018 | 72,060 | (22.7) | 34,938 | (23.3) | 37,122 | (22.2) | |
| Persistent asthma | 57,048 | (18.0) | 29,891 | (19.9) | 27,157 | (16.2) | < 0.0001 |
| Comorbid conditions | |||||||
| Any HCC (excluding asthma) (binary) | 40,539 | (12.8) | 19,985 | (13.3) | 20,554 | (12.3) | < 0.0001 |
| Most common HCCs (excluding asthma) | |||||||
| Autistic disorder | 8,871 | (2.8) | 4,209 | (2.8) | 4,662 | (2.8) | 0.7619 |
| Major depressive and bipolar disorders | 6,052 | (1.9) | 2,736 | (1.8) | 3,316 | (2.0) | 0.0011 |
| Seizure disorders and convulsions | 4,968 | (1.6) | 2,425 | (1.6) | 2,543 | (1.5) | 0.0301 |
| Cardio-respiratory failure and shock, including respiratory distress syndromes | 2,420 | (0.8) | 1,167 | (0.8) | 1,253 | (0.8) | 0.3552 |
| Major congenital heart/circulatory disorders | 2,077 | (0.7) | 1,170 | (0.8) | 907 | (0.5) | < 0.0001 |
P-values calculated using Chi-squared tests. HCC = Hierarchical Condition Categories.
In unadjusted and regression-adjusted models, influenza vaccinations were significantly more common among privately insured children with asthma (Fig. 1; full multivariate logistic regression results in Supplemental Appendix Table 4) than those insured by Medicaid. In regression-adjusted models, privately insured children with asthma were 3.7 percentage points (pp) more likely (95% confidence interval [CI]: 2.9–4.5pp) to receive an influenza vaccination than Medicaid-insured children with asthma (49.7% vs 46.0%). Children with persistent asthma were more likely to receive influenza vaccinations than those without (6.7pp higher in regression-adjusted models, 95% CI: 6.2–7.2pp). Influenza vaccinations were more common among younger children in both unadjusted and adjusted analyses (Fig. 2). The regression-adjusted probability of a 2- to 4-year-old child with asthma receiving vaccination was 9.8pp higher (95% CI: 8.9–10.7pp) than a 15–17 year old with asthma. There were statistically significant but small changes in unadjusted and regression-adjusted influenza vaccination rates for children with asthma over time, with lower rates in 2016 and 2017 than 2015 (Fig. 3).
Fig. 1.
Unadjusted and adjusted rates of influenza vaccinations for children with asthma by insurance type. Note: N = 317,596 child-year observations. Regression-adjusted results control for child sex, child age, calendar year, persistent asthma, hierarchical condition categories, and patient residence 5-digit ZIP Code fixed effects. Standard errors are clustered at the 5-digit ZIP Code level. *Indicates difference in predicted probability is statistically significantly different from the reference group (private insurance) at the 5% level.
Fig. 2.
Unadjusted and adjusted rates of influenza vaccinations for children with asthma by age. Note: N = 317,596 child-year observations. Regression-adjusted results control for child sex, insurance type, calendar year, persistent asthma, hierarchical condition categories, and patient residence 5-digit ZIP Code fixed effects. Standard errors are clustered at the 5-digit ZIP Code level. *Indicates difference in predicted probability is statistically significantly different from the reference group (age 2–4 years) at the 5% level.
Fig. 3.
Unadjusted and adjusted rates of influenza vaccinations for children with asthma by calendar year. Note: N = 317,596 child-year observations. Regression-adjusted results control for child sex, child age, insurance type, persistent asthma, hierarchical condition categories, and patient residence 5-digit ZIP Code fixed effects. Standard errors are clustered at the 5-digit ZIP Code level. *Indicates difference in predicted probability is statistically significantly different from the reference group (calendar year 2015) at the 5% level.
When examining children with asthma with any influenza vaccination, we estimated the probability of these vaccinations occurring in a non-office setting as defined above by calendar year (Fig. 4). In unadjusted and regression-adjusted results, the proportion of vaccinations occurring in a non-office setting increased starting in 2017. The regression adjusted predicted probability of influenza vaccination in a non-office setting is 3.2pp higher in 2018 than in 2015 (95% CI: 2.2–4.2pp), increasing from 1.8% in 2015 to 5.0% in 2018. The probability of vaccination in a non-office setting was significantly lower for children with Medicaid and higher for older children. In 2017, 48% of vaccinations in non-office settings were in a retail pharmacy, increasing to 57% in 2018. Among those vaccinated in non-office settings in 2017 and 2018, 67.1% of those with asthma received an influenza vaccination in the prior year, and 71.3% of those with persistent asthma.
Fig. 4.
Unadjusted and adjusted rates of influenza vaccinations in non-office settings for children with asthma receiving any influenza vaccination by calendar year. Note: N = 149,340 child-year observations. Regression-adjusted results control for child sex, child age, insurance type, persistent asthma, hierarchical condition categories, and patient residence 3-digit ZIP Code fixed effects. Standard errors are clustered at the 3-digit ZIP Code level. *Indicates difference in predicted probability is statistically significantly different from the reference group (calendar year 2015) at the 5% level.
In the sensitivity analysis including additional vaccination administration codes, we found higher overall rates of influenza vaccination with larger differences between privately and Medicaid insured children (61.6% vs 53.4%; regression-adjusted difference: 8.2pp [95% CI: 7.5–8.9pp). In this sensitivity analysis, we found similar associations of higher vaccination rates for younger children as in the main analysis as well as among those with persistent asthma.
DISCUSSION
Overall, only about half of children with asthma in Massachusetts received an influenza vaccination, with little change over the 4-year period despite changes in availability of influenza vaccinations in retail pharmacies. Privately insured children were significantly more likely to receive an influenza vaccination than Medicaid-insured children.
Our study found low influenza vaccine rates for children with asthma, with Medicaid-insured children having modestly lower rates than those with commercial insurance. Influenza vaccine hesitancy and refusal differ from other childhood vaccines in part due to the comparatively low effectiveness of the vaccine in most influenza seasons, exclusion from many state’s mandated vaccine lists,24 and delivery outside of routine childhood vaccination schedules.20
Multi-level interventions (policy, community, health system, provider, patient) are likely needed to improve influenza vaccination rates for children with asthma.8 A recent study suggested that increased reimbursement to physicians for administering influenza and other vaccines may increase vaccination rates25 and a study of Medicaid reimbursement increases for childhood vaccines had similar findings.26 Patients are more likely to get vaccinated if their primary care physician strongly recommends a vaccine.27 Systems that make it easy to get the influenza vaccine even if the patient does not have a routine appointment scheduled can also increase vaccine uptake.28 Clinical trials of interventions that test these and other approaches to promoting influenza vaccine uptake for children with asthma are warranted.
Delivery of acute and preventive healthcare in non–office-based settings, such as pharmacies, retail clinics, and freestanding urgent care centers, has increased substantially over the past decade.29 In a study using data from 2007, 9.4% of retail clinic visits for children were for immunizations,30 although use of retail clinics for influenza vaccination (identified by a site of service code) was rare in our sample. In addition to the policy change in 2017 allowing children nine and older to receive vaccinations in pharmacies, federal and Massachusetts regulations allow for childhood vaccinations in pharmacies for children ages three years and older starting in 2020 with the public health emergency and the emergence of vaccinations for COVID-19.31 Although we found that significantly more children received their influenza vaccine in retail pharmacies following changes in state regulations that lowered the age at which retail pharmacies could administer vaccinations, there was little change overall in the percentage of children with asthma receiving influenza vaccine between 2015 and 2018. Further study is needed to understand the long-term impacts of allowing influenza and other vaccinations in pharmacies on healthcare for children with asthma.
There were several limitations of the analysis. The first is that this was a single-state study which may limit the generalizability of findings. However, our study included a large sample of privately and publicly insured children, with Medicaid-insured children overrepresented in the sample relative to coverage in the state. Additionally, despite having higher insurance coverage, Massachusetts has one of the highest rates of asthma among children in the United States.32 Uncontrolled asthma rates are similar in Massachusetts to the national rate,2 and so findings related to influenza vaccination are important to improve quality of asthma care in Massachusetts and nationally. Second, we are not able to observe the severity of asthma or confirm the diagnosis based on clinical symptoms. We identify children with asthma using a method used in previous literature that accounts for both acute care use related to asthma and more stringent methods (e.g., two visits) for outpatient care use where a rule-out diagnosis might be more likely to appear on a claim. We do additional analyses to examine whether there are differences in vaccination by whether the child is identified with persistent asthma, including having asthma claims in at least two consecutive years. Third, due to the small number of children with asthma receiving vaccinations in non-office settings and year-to-year fluctuation in influenza vaccination rates, we were unable to determine whether vaccinations in retail pharmacies are replacing vaccinations in pediatric office settings or whether they are contributing to children receiving vaccinations that would not have otherwise. Receiving an influenza vaccination in a non-office setting was less likely for those with Medicaid; increasing vaccination rates among these populations is important in improving asthma care. In the 2020–21 season, 12% of all pediatric influenza vaccinations nationally were in pharmacies,33 making understanding care patterns for chronically ill children an increasingly important area for future research. Fourth, it is possible that not all influenza vaccinations are captured in the insurance claims data, including those provided by the federal VFC program or the state DPH. We conducted a sensitivity analysis using administration codes for these vaccinations (which may capture vaccinations other than influenza) and found that the lower rates of vaccination among Medicaid-insured children with asthma persisted. Fifth, we did not have information regarding whether providers recommended or offered vaccinations, so were unable determine the extent to which the variation we observed was a result of differences in parental acceptance or other factors. Future research should explore provider and patient factors to identify effective interventions to increase vaccination rates.
CONCLUSION
Influenza vaccine rates for Medicaid-insured children with asthma were lower than those with private insurance. Current and longstanding guidelines recommend influenza vaccinations for children with asthma4,5 and most health plans are required to cover them without cost- sharing.26 However, low rates persist among both privately and publicly insured children with asthma, including for those with persistent asthma. Further research is needed to develop and test strategies to increase influenza vaccination among this vulnerable population.
Supplementary Material
WHAT’S NEW.
This study compares influenza vaccination rates for privately insured children with asthma to rates for Medicaid-insured children, addressing a potentially important and actionable inequity in preventive asthma care.
ACKNOWLEDGMENTS
The authors thank Erin DeCou (University of Massachusetts Amherst) for research assistance.
Financial statement:
This research was supported by the National Heart, Lung, and Blood Institute (grant number R01 HL149874). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Heart, Lung, and Blood Institute or the National Institutes of Health. The funding source had no involvement in study design; collection, analysis, and interpretation of data; the writing of the report; nor in the decision to submit the article for publication. Dr Ash is also supported by Biostatistics, Epidemiology & Research Design Component (BERD) awards 2UL1 TR001453-05A1 and 5UL1 TR001453-07 from the National Center for Advancing Translation Studies.
Footnotes
Authorship statement: Drs Geissler and Goff conceptualized and designed the study, drafted the initial manuscript, carried out the acquisition, analyses, or interpretation of data for the work. Drs Shieh, Lindenauer, Ash, and Krishnan and Ms Evans carried out the acquisition, analyses, or interpretation of data for the work, and review and revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
APPENDIX A. SUPPORTING INFORMATION
Supplementary data associated with this article can be found in the online version at doi:10.1016/j.acap.2023.02.010.
REFERENCES
- 1.Centers for Disease Control and Prevention. 2019 National Health Interview Survey Data. U.S. Department of Health & Human Services; 2019. 〈https://www.cdc.gov/asthma/nhis/2019/data.htm〉. [Google Scholar]
- 2.Centers for Disease Control and Prevention. AsthmaStats: Uncontrolled Asthma Among Children, 2012–2014. U.S. Department of Health and Human Services; 2019. 〈https://www.cdc.gov/asthma/asthma_stats/uncontrolled-asthma-children.htm〉. [Google Scholar]
- 3.Volerman A, Chin MH, Press VG. Solutions for asthma disparities. Pediatrics. 2017;139(3):e20162546. 10.1542/peds.2016-2546 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Centers for Disease Control and Prevention. Prevention and Control of Influenza Recommendations of the Immunization Practices Advisory Committee (ACIP). MMWR; 1990:1–15. 〈https://www.cdc.gov/mmwr/preview/mmwrhtml/00001644.htm〉. [PubMed] [Google Scholar]
- 5.Grohskopf LA, Alyanak E, Ferdinands JM, et al. Prevention and control of seasonal influenza with vaccines: recommendations of the Advisory Committee on Immunization Practices, United States, 2021–22 Influenza Season. MMWR Recomm Rep. 2021;70(5):1–28. 10.15585/mmwr.rr7005a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.U.S. Department of Health and Human Services. Increase the Proportion of People who Get the Flu Vaccine Every Year — IID-09. Healthy People 2030. 〈https://health.gov/healthypeople/objectives-and-data/browse-objectives/vaccination/increase-proportion-people-who-get-flu-vaccine-every-year-iid-09〉. Accessed June 1, 2022. [Google Scholar]
- 7.Friedman BC, Goldman RD. Influenza vaccination for children with asthma. Can Fam Physician. 2010;56(11):1137–1139. [PMC free article] [PubMed] [Google Scholar]
- 8.Norman DA, Barnes R, Pavlos R, et al. Improving influenza vaccination in children with comorbidities: a systematic review. Pediatrics. 2021;147(3):e20201433. 10.1542/peds.2020-1433 [DOI] [PubMed] [Google Scholar]
- 9.Murphy EV. Improving influenza vaccination coverage in the pediatric asthma population: the case for combined methodologies. Yale J Biol Med. 2014;87(4):439–446. [PMC free article] [PubMed] [Google Scholar]
- 10.Dombkowski KJ, Lamarand K, Dong S, et al. Using Medicaid claims to identify children with asthma. J Public Health Manag Pract. 2012;18(3):196–203. 10.1097/PHH.0b013e31821a3fa7 [DOI] [PubMed] [Google Scholar]
- 11.Simon AE, Ahrens KA, Akinbami LJ. Influenza vaccination among US children with asthma, 2005–2013. Acad Pediatr. 2016;16(1):68–74. 10.1016/j.acap.2015.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gnanasekaran SK, Finkelstein JA, Lozano P, et al. Influenza vaccination among children with asthma in Medicaid managed care. Ambul Pediatr. 2006;6(1):1–7. 10.1016/j.ambp.2005.08.004 [DOI] [PubMed] [Google Scholar]
- 13.NCQA. HEDIS 2017 Final NDC Lists. NCQA. 〈https://www.ncqa.org/hedis/measures/hedis-2017-national-drug-code-ndc-license/hedis-2017-final-ndc-lists/〉. Accessed June 1, 2022. [Google Scholar]
- 14.Schwarze J, Openshaw P, Jha A, et al. Influenza burden, prevention, and treatment in asthma – a scoping review by the EAACI Influenza in asthma task force. Allergy. 2018;73(6):1151–1181. 10.1111/all.13333 [DOI] [PubMed] [Google Scholar]
- 15.The Secretary of the Commonwealth, William Francis Galvin, Secretary. The Massachusetts Register.; 2017. [Google Scholar]
- 16.Center for Health Information and Analysis. 2014–2018 Massachusetts All-Payer Claims Database. 〈https://www.chiamass.gov/ma-apcd/〉.
- 17.Children Helping Improve Pediatric Practice, Education & Research (CHIPPER). Pediatric Asthma Emergency Department Use, ICD/CPT Codes. 〈https://chipper.ucsf.edu/studies/implement/documents〉.
- 18.Bardach NS, Neel C, Kleinman LC, et al. Depression, anxiety, and emergency department use for asthma. Pediatrics. 2019;144(4):e20190856. 10.1542/peds.2019-0856 [DOI] [PubMed] [Google Scholar]
- 19.Jacob C, Haas JS, Bechtel B, et al. Assessing asthma severity based on claims data: a systematic review. Eur J Health Econ. 2017;18(2):227–241. 10.1007/s10198-016-0769-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Worsham C, Woo J, Jena AB. Birth month and influenza vaccination in children. N Engl J Med. 2020;383(2):184–185. 10.1056/NEJMc2005928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Centers for Medicare & Medicaid Services. HCPCS/CPT Codes for Flu Shots. 〈https://www.cms.gov/medicare/preventive-services/flu-shot-coding〉.
- 22.NCQA. HEDIS Measures and Technical Resources, HEDIS Measurement Year 2021 Vol 2: Technical Specifications for Health Plans. Accessed June 1 NCQA. 2022 Accessed June 1 〈https://www.ncqa.org/hedis/measures/〉 Accessed June 1.
- 23.Centers for Medicare & Medicaid Services. Center for Consumer Information and Insurance Oversight - Regulations and Guidance. 〈https://www.cms.gov/CCIIO/Resources/Regulations-and-Guidance〉.
- 24.Immunize.org. Influenza Vaccine Mandate for Child Care and Pre-K. 〈https://www.immunize.org/laws/flu_childcare.asp〉. Accessed June 1, 2022.
- 25.Health Affairs Blog. Increased Reimbursement May Help Overcome Barriers to Administration of Seasonal and Routine Vaccines. 2020. 〈 10.1377/forefront.20201208.111539/full/〉. Accessed May 30, 2022. [DOI]
- 26.Tsai Y.Payments and utilization of immunization services among children enrolled in fee-for-service Medicaid. Med Care. 2018;56(1):54–61. 10.1097/MLR.0000000000000844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kempe A, Saville AW, Albertin C, et al. Parental hesitancy about routine childhood and influenza vaccinations: a national survey. Pediatrics. 2020;146(1):e20193852. 10.1542/peds.2019-3852 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Aigbogun NW, Hawker JI, Stewart A. Interventions to increase influenza vaccination rates in children with high-risk conditions—a systematic review. Vaccine. 2015;33(6):759–770. 10.1016/j.vaccine.2014.12.013 [DOI] [PubMed] [Google Scholar]
- 29.Lee BY, Mehrotra A, Burns RM, et al. Alternative vaccination locations: who uses them and can they increase flu vaccination rates. Vaccine. 2009;27(32):4252–4256. 10.1016/j.vaccine.2009.04.055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mehrotra A, Wang MC, Lave JR, et al. Retail clinics, primary care physicians, and emergency departments: a comparison of patients’ visits. Health Aff (Millwood). 2008;27(5):1272–1282. 10.1377/hlthaff.27.5.1272 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.The Commonwealth of Massachusetts. Board of Registration in Pharmacy Drug Control Program Immunization Program Policy 2020–11: Vaccine Administration; 2021. 〈https://www.mass.gov/doc/2020-11-vaccine-administration-0/download〉.
- 32.The Commonwealth of Massachusetts. Statistics About Asthma. 〈https://www.mass.gov/service-details/statistics-about-asthma〉. Accessed June 1, 2022.
- 33.Centers for Disease Control and Prevention. Flu Vaccination Coverage, United States, 2020–21 Influenza Season. 2021. 〈https://www.cdc.gov/flu/fluvaxview/coverage-2021estimates.htm〉. Accessed May 30, 2022.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.