Abstract
We reported imaging findings of arterio-venous malformation complicated by hemorrhage and venous pseudoaneurysm in a young child consulting for headache and emesis: to our knowledge venous pseudoaneurysm in association with ruptured arteriovenous malformation is a rare complication reported in the literature. We present the indications for endovascular treatment, especially with NBCA (N-butyl cyanoacrylate).
Keywords: Arterio-venous malformation, Venous pseudoaneurysm, N-butyl cyanoacrylate, Neuroradiology, Interventional radiology
Introduction
Arteriovenous malformations (AVMs) are high flow lesions formed by feeding arteries, a cluster of vessels (the nidus) and drainage veins without interposition of capillaries. The incidence of cerebral AVMs in childhood is expected to be 1 per 100,000 children [1]. The treatment consists in microsurgery, endovascular embolization, radiosurgery, and the combination of these techniques.
Case report
A 6-year-old male patient consulted for headache and emesis in the past 5 days, after à first medical imaging in another institution, he was addressed in Erasme Hospital.
Vital signs, biological results, and family history were not relevant.
Physical and neurological examination were within normal limits.
The only known antecedent is an acute right otitis media complicated by transient facial paralysis.
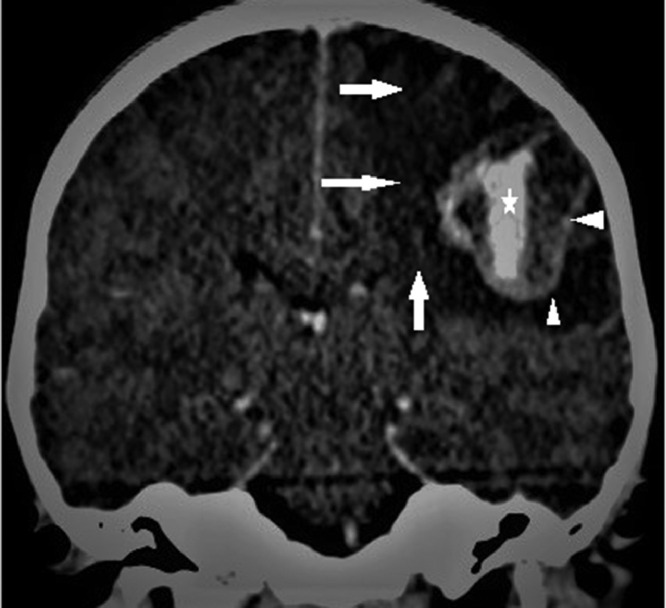
Brain-CT with contrast (Figs. 1 and 2) showed an intraparenchymal left rolandic hemorrhagic lesion of about 3 cm, perilesional oedema, peripheral enhancement, an intralesional aneurysm, and possible cortical venous drainage.
Fig. 1.
Brain enhanced CT in arterial phase: distal parietal branch of left sylvian artery (arrow) and nearby aneurismal vessel dilatation (arrowhead).
Fig. 2.
Brain enhanced CT in venous phase: perilesional oedema (arrows), peripheral enhancement (arrowheads) and an intralesional aneurysm (star).
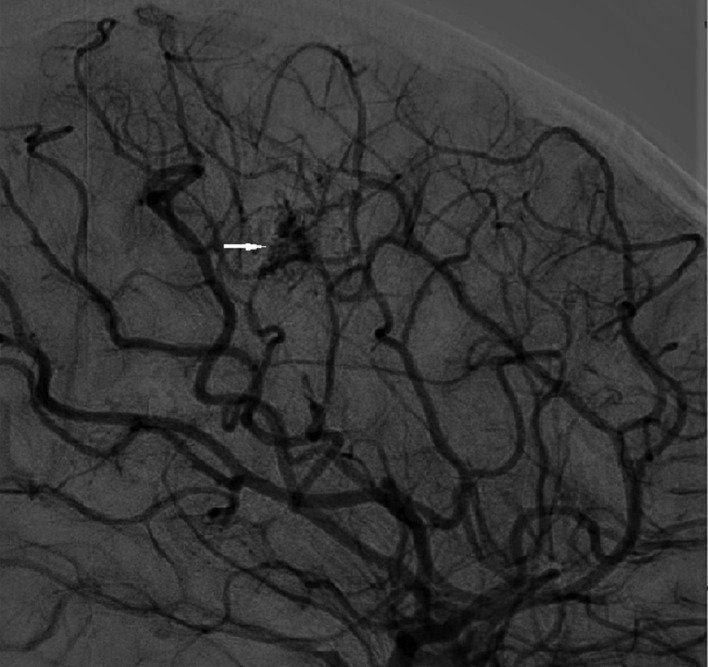
A digital subtraction angiography was performed (Fig. 3). It discovered a left parietal arterio-venous shunt with cortical drainage and venous pseudoaneurysm. After selective catheterization of the left sylvian afferent branch, a trans arterial embolization with glue (1 ml Glubran + Lipiodol ultrafluide [33%]) was performed to obtain complete occlusion of the arteriovenous shunt.
Fig. 3.
Angiogram showed venous pseudoaneurysm (arrow) in proximity of arteriovenous shunt and a small nidus (arrowhead).
The last control by digital subtraction angiography after 40 days of admission, showed complete occlusion of the AVM and a small scar residue (Fig. 4).
Fig. 4.
Forty-day control DSA, complete AVM obliteration and small scar residue (arrow). AVM, arteriovenous malformations; DSA, digital subtraction angiography.
No symptoms or clinical signs were reported in the last records.
Discussion
The natural history of cerebral AVMs is not benign and the risk factor for hemorrhage are: prior hemorrhage, deep location, exclusively deep venous drainage and associated aneurysms [2]. Children have a higher risk of bleeding and rebleeding [1,3].
The ARUBA (a randomized trial of unruptured brain arteriovenous malformations) study showed that medical management alone is superior to interventional treatment for the prevention of death or symptomatic stroke in adults patients with an uncomplicated cerebral AVM [4] but this strategy is discussed especially for the pediatric population.
Microsurgery is the treatment of choice however is limited by the localization of the lesion in the deep and eloquent regions, for which endovascular embolization is the best primary treatment [5].
The choice of endovascular treatment depends on the number and size of feeder vessels, the size of the nidus and the team's experience. The aim is the complete embolization of feeder vessel and nidus.
Embolization materials including NBCA ethylene vinyl alcohol (ONYX: EVOH COPOLYMER), dehydrated alcohol and coils [5].
The levels of evidence in the literature remain low for endovascular approaches, studies with the use of HONIX shows good effectiveness of the method [6,7].
In this case for the deep location of AMV, the endovascular NBCA treatment has been performed.
NBCA allows a decrease in operating time and gives less imaging artifacts for MRI follow-ups and possible gamma knife treatment planning.
NBCA polymerizes in contact with an anionic environment.
It is mixed with ethiodol and tantalum to transport it, to delay the polymerization and make it radiopaque, the catheter flushes is performed with dextrose 5% (D5W) in water [8].
The major risks of NBCA are: the catheter adherence to the vessel, glue migration and too distal or too proximal embolization [8]. But the complications reported are low, Li et al. [9] observed after AVMs embolization with NBCA alone a severe morbidity of 0.7% and a mortality of 0.5%.
PH, temperatures, biological catalysts, glue formulation, blood flow and lysed red blood cells influenced polymerization rate of NBCA but differences between in vitro and in vivo are reported [10]. For this reason, a training simulator or adapted preparation formulas do not exist currently.
We observed a venous pseudoaneurysm secondary to the rupture of the AVM. The nidus was not clearly visible in the first radiological investigations due to compression by hemorrhage and may re-emerge later with hemorrhage resorption.
Conclusions
We report a case of successful NBCA AVM embolization in a 6-year-old child, guidelines for the use of this technique and tailored glue preparation formulas remain to be defined.
Patient consent
Written informed consent was obtained from the patient's parent.
Footnotes
Competing Interests: The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- 1.Menovsky T, van Overbeeke JJ. Cerebral arteriovenous malformations in childhood: state of the art with special reference to treatment. Eur J Pediatr. 1997;156(10):741–746. doi: 10.1007/s004310050703. [DOI] [PubMed] [Google Scholar]
- 2.Gross BA, Du R. Natural history of cerebral arteriovenous malformations: a meta-analysis. J Neurosurg. 2013;118(2):437–443. doi: 10.3171/2012.10.JNS121280. Epub 2012 Nov 30. [DOI] [PubMed] [Google Scholar]
- 3.Qureshi AM, Muthusami P, Krings T, Amirabadi A, Radovanovic I, Dirks P, et al. Clinical and angioarchitectural features of hemorrhagic brain arterio-venous malformations in adults and children: contrasts and implications on outcome. Neurosurgery. 2021;89(4):645–652. doi: 10.1093/neuros/nyab251. [DOI] [PubMed] [Google Scholar]
- 4.Mohr JP, Overbey JR, Hartmann A, Kummer RV, Al-Shahi Salman R, Kim H, et al. ARUBA co-investigators. Medical management with interventional therapy versus medical management alone for unruptured brain arteriovenous malformations (ARUBA): final follow-up of a multicentre, non-blinded, randomised controlled trial. Lancet Neurol. 2020;19(7):573–581. doi: 10.1016/S1474-4422(20)30181-2.5. [DOI] [PubMed] [Google Scholar]
- 5.Millar C, Bissonnette B, Humphreys RP. Cerebral arteriovenous malformations in children. Can J Anaesth. 1994;41(4):321–331. doi: 10.1007/BF03009913. [DOI] [PubMed] [Google Scholar]
- 6.Baharvahdat H, Blanc R, Fahed R, Smajda S, Ciccio G, Desilles JP, et al. Endovascular treatment for low-grade (Spetzler-Martin I-II) brain arteriovenous malformations. AJNR Am J Neuroradiol. 2019;40(4):668–672. doi: 10.3174/ajnr.A5988. Epub 2019 Feb 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mounayer C, Hammami N, Piotin M, Spelle L, Benndorf G, Kessler I, et al. Nidal embolization of brain arteriovenous malformations using Onyx in 94 patients. AJNR Am J Neuroradiol. 2007;28(3):518–523. [PMC free article] [PubMed] [Google Scholar]
- 8.Vaidya S, Tozer KR, Chen J. An overview of embolic agents. Semin Intervent Radiol. 2008;25(3):204–215. doi: 10.1055/s-0028-1085930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Li TL, Fang B, He XY, Duan CZ, Wang QJ, Zhao QP, et al. Complication analysis of 469 brain arteriovenous malformations treated with N-butyl cyanoacrylate. Interv Neuroradiol. 2005;11(2):141–148. doi: 10.1177/159101990501100204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang BH, Boulton M, Lee DH, Pelz DM, Lownie SP. A systematic characterization of the factors influencing polymerization and dynamic behavior of n-butyl cyanoacrylate. J NeuroInterven Surg. 2018;10:150–155. doi: 10.1136/neurintsurg-2017-013009. [DOI] [PubMed] [Google Scholar]