Summary
Background
Clinical practice guidelines (CPGs) predominantly prioritise treatment and cost-effectiveness, which encourages a universal approach that may not address the circumstances of disadvantaged groups. We aimed to advance equity and quality of care for individuals experiencing homelessness and traumatic brain injury (TBI) by assessing the extent to which homelessness and TBI are integrated in CPGs for TBI and CPGs for homelessness, respectively, and the extent to which equity, including consideration of disadvantaged populations and the PROGRESS-Plus framework, is considered in these CPGs.
Methods
For this systematic review, CPGs for TBI or homelessness were identified from electronic databases (MEDLINE, Embase, CINAHL, PsycINFO), targeted websites, Google Search, and reference lists of eligible CPGs on November 16, 2021 and March 16, 2023. The proportion of CPGs that integrated evidence regarding TBI and homelessness was identified and qualitative content analysis was conducted to understand how homelessness is integrated in CPGs for TBI and vice versa. Equity assessment tools were utilised to understand the extent to which equity was considered in these CPGs. This review is registered with PROSPERO (CRD42021287696).
Findings
Fifty-eight CPGs for TBI and two CPGs for homelessness met inclusion criteria. Only three CPGs for TBI integrated evidence regarding homelessness by recognizing the prevalence of TBI in individuals experiencing homelessness and identifying housing as a consideration in the assessment and management of TBI. The two CPGs for homelessness acknowledged TBI as prevalent and recognised individuals experiencing TBI and homelessness as a disadvantaged population that should be prioritised in guideline development. Equity was rarely considered in the content and development of CPGs for TBI.
Interpretation
Considerations for equity in CPGs for homelessness and TBI are lacking. To ensure that CPGs reflect and address the needs of individuals experiencing homelessness and TBI, we have identified several guideline development priorities. Namely, there is a need to integrate evidence regarding homelessness and TBI in CPGs for TBI and CPGs for homelessness, respectively and engage disadvantaged populations in all stages of guideline development. Further, this review highlights an urgent need to conduct research focused on and with disadvantaged populations.
Funding
Canada Research Chairs Program (2019-00019) and the Ontario Ministry of Health and Long-Term Care (Grant #725A).
Keywords: Clinical practice guideline, Concussion, Disadvantaged populations, Evidence-based practice, Health inequity, Homeless, Knowledge synthesis, Traumatic brain injury
Research in context.
Evidence before this study
Adherence to clinical practice guidelines (CPGs) for traumatic brain injury (TBI) leads to lower mortality, reduced length of stay in hospital, and improved functional outcomes. However, the extent to which disadvantaged populations and health equity is considered in these guidelines is unclear. We systematically searched for CPGs for TBI and homelessness in electronic databases (MEDLINE, Embase, CINAHL, PsycINFO on November 16, 2021 and March 16, 2023), targeted websites, Google Search, and reference lists of eligible CPGs using search terms outlined in the appendix; 58 CPGs for TBI and 2 CPGs for homelessness met predetermined eligibility criteria and were included in this review.
Added value of this study
To our knowledge, this is the first systematic review that assessed equity in CPGs for TBI and CPGs for homelessness. Our review shows that only 5.2% of the CPGs for TBI integrated evidence regarding homelessness, and while all CPGs for homelessness integrated evidence regarding TBI, they only acknowledged that TBI is prevalent among individuals experiencing homelessness. Results also showed that equity is rarely considered in the content and development of TBI CPGs, as disadvantaged populations are seldom involved among members of the working group and no plans to assess and monitor guideline uptake were included.
Implications of all the available evidence
The findings from our systematic review demonstrate the need to prioritise equity in CPG development, particularly given the increasing calls for inclusion, diversity, equity, and accessibility in healthcare and the high prevalence of TBI among individuals experiencing homelessness. We urge guideline developers to seek and consider evidence regarding TBI and homelessness in CPGs for homelessness and TBI, respectively, to develop recommendations that are appropriate and implementable for individuals experiencing homelessness and TBI, involve disadvantaged populations in all stages of guideline development, and conduct equity-driven research focused on disadvantaged populations. Action in these areas will ensure that the needs of disadvantaged groups, such as individuals experiencing homelessness and TBI are taken into account in future CPG recommendations.
Introduction
Globally, traumatic brain injury (TBI) affects more than fifty million individuals every year and costs the economy approximately $400 billion USD annually.1 While TBI does not discriminate against sociodemographic factors,1 it has been found to be more prevalent among individuals experiencing homelessness than the general population.2 According to a recent systematic review and meta-analysis, 53.1% of individuals who experienced or were experiencing homelessness had a lifetime history of TBI.2
Individuals experiencing homelessness and TBI are a disadvantaged group requiring urgent attention. TBI in persons experiencing homelessness is associated with life-altering impairments, including poorer self-reported physical and mental health,2 increased likelihood of subsequent psychiatric and neurological conditions,3 higher risk of suicide and involvement with the criminal justice system, and greater use of health services than the general population.2 Individuals experiencing homelessness are also impacted by a vast number of health inequities (i.e., avoidable, unjust, and unfair differences in health within or between populations)4 that are not limited to poorer health (e.g., infectious diseases, serious mental illness, and substance use disorders) and increased morbidity,5,6 reduced probability of accessing primary and preventive healthcare,5 food insecurity, violence and victimization,6 and increased mortality.5,6 These inequities are worsened by adverse social determinants of health, such as poverty, trauma, unemployment, and social disconnection.5 Combined, TBI and the health inequities encountered by individuals experiencing homelessness increase the likelihood of long-term homelessness,7 repeated TBIs,8 and significant socio-economic consequences.9
Clinical practice guidelines (CPGs) are tools used to translate research evidence to clinical practice.10 They are defined as recommendations based on a rigorous review of evidence and an evaluation of alternative care options.10 There is evidence that adherence to TBI CPGs leads to lower mortality, reduced length of stay in hospital, and improved functional outcomes, particularly among adults and children with severe TBI.11 CPGs are often developed with a focus on treatment effectiveness and cost-effectiveness,12 without regard for equity (i.e., “the absence of unfair and avoidable or remediable differences on health amongst social groups12,13”) or health inequities.4,12 Thus, recommendations in CPGs may not always be applicable or beneficial to disadvantaged groups who encounter health inequities, including individuals experiencing homelessness. Without considering equity or health inequities, CPGs would continue to promote a one-size-fits-all approach to care1 that fails to address the needs of disadvantaged groups.12
The objectives of this systematic review were to assess: (1) the extent to which evidence about homelessness is integrated in CPGs for TBI, (2) the extent to which evidence about TBI is integrated in CPGs for homelessness, and (3) equity considerations in CPGs for TBI and CPGs homelessness. Findings from this review provide the foundation to advance equity and promote quality of care for individuals with lived experience of TBI and homelessness. We recognise the possible stigma that accompany the term disadvantaged, along with other terms such as marginalised or underserved. However, we used the term disadvantaged group to communicate the lack of opportunities experienced by individuals that ultimately positioned them in a disadvantaged state. We also used this term to remain consistent with the language used by the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) Working Group who developed the rationale and methods for considering health equity in CPGs and whose appraisal tool we adapted for this review.
Methods
Ethics
Data in this study were retrieved from public databases, including MEDLINE, Embase, CINAHL, PsycINFO and websites. Ethical approval and informed consent of participants were not applicable for this study.
Search strategy
The protocol for this systematic review was published in a peer-reviewed journal14 and registered on PROSPERO [CRD42021287696]. The reporting of this systematic review followed the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) extension for searching (PRISMA-S) and the PRISMA Equity Checklist.
CPGs were identified from (a) databases for peer-reviewed literature, (b) targeted websites and Google Search for grey literature, and (c) reference lists of eligible CPGs and scoping and systematic reviews that met inclusion criteria.
Peer-reviewed literature
The search strategy, developed with an Information Specialist (JB) and team members with subject-matter experience relevant to TBI and homelessness (VC, MJE), applied a validated search filter for CPGs,15 and was informed by reviews related to CPGs, TBI, and/or homelessness.16, 17, 18 The search structure was developed using concepts of (A) CPG, (B) TBI, and (C) homelessness to form the final search for each database: (A + B) OR (A + C). The search strategy was first created for MEDLINE® ALL (in Ovid, including Epub Ahead of Print, In-Process & Other Non-Indexed Citations, Ovid MEDLINE ® Daily) database and subsequently translated to Embase and Embase Classic (Ovid), CINAHL (EBSCOhost), and APA PsycInfo (Ovid). All databases were first searched on November 16, 2021 and updated on March 16, 2023 by rerunning database searches and restricting to records entered into the database on or after the last search date.19 No date or language limits were placed. However, animal studies and conference abstracts were excluded, where possible. Supplementary file 1 (Appendix) presents the search strategy for each database.
Grey literature
Guided by a methodology on applying systematic search methods to grey literature,20 we searched for grey literature, defined as CPGs outside of the peer-reviewed literature, from (1) targeted websites identified by the research team, (2) websites included in Grey Matters: A Practical Tool for Searching Health-Related Literature (herein referred to as ‘Grey Matters’),21 and (3) the first ten pages of Google Search. Supplementary file 1 (Appendix) presents the full details of these searches.
Reference list
Reference lists of scoping and systematic reviews and CPGs that met study selection criteria at full-text screening were reviewed for additional CPGs.
Study selection
Supplementary Table S1 presents the PICAR Statement outlining the eligibility criteria. Only CPGs for TBI or homelessness were included. Supplementary file 2 (Appendix) presents the list of excluded studies at full-text screening.
Peer-reviewed literature
EndNote X8 was used for reference management and de-duplication, and Covidence was used for de-duplication and study selection. We followed the screening process outlined in our protocol.14 For the search conducted in November 2021, the resulting agreement for title and abstract screening was 94.6% for English articles and 90.0% for non-English language articles. The resulting agreement for full-text screening was 95.4% for English articles and 94.9% for non-English language articles. For the search conducted in March 2023, the resulting agreement for title and abstract screening was 87.0% for English articles and 95.8% for non-English language articles. The resulting agreement for full-text screening was 80.0% for English articles and 100% for non-English language articles.
Grey literature
We followed the screening process outlined in our protocol.14 Microsoft Excel was used to document the study selection process, including the search date, the name and link of each website, and the reasons for exclusion at the full-text screening stage.
Data extraction and synthesis
The data extraction and synthesis were adapted from a systematic review that assessed sex and gender considerations in Canadian CPGs.22 The text and reference lists of all CPGs were searched for (a) keywords describing TBI and homelessness or (b) content consistent with the definitions of TBI and homelessness as presented in Supplementary Table S2 and categorised into “text-positive” or “text-negative”. Text-positive CPGs were those that contained at least one of the keywords for, or content consistent with, homelessness (in the case of CPGs for TBI) or TBI (in the case of CPGs for homelessness) in the text (i.e., body) of the guideline. Text-negative CPGs were those that did not include any of the keywords for, or content consistent with, homelessness or TBI in the body of the guideline.
Text-positive and text-negative guidelines were synthesised separately according to the definitions outlined in Supplementary Table S3. Two independent reviewers completed the data extraction and synthesis (SH, ZC), with discrepancies resolved through consensus or consultation with a third reviewer (VC). Supplementary file 3 (Appendix) presents the data extraction and synthesis for this systematic review.
Analysis
A narrative synthesis23 was conducted. In addition to the categories defined above, the CPGs were also grouped based on their characteristics. Tabulation, as defined in Supplementary Table S4, was used to address the three objectives of this review, and a qualitative content analysis of text-positive guidelines was conducted to understand how homelessness is integrated in existing CPGs for TBI, how TBI is integrated in existing CPGs for homelessness, and how equity is considered in the CPGs.
Quality appraisal
Quality appraisal, using the equity lens from Dans and colleagues12 and the equity extension of the GRADE Working Group,24 was independently completed by two reviewers (MJE, JMJ or SH), with discrepancies resolved through consultation with a third reviewer (VC). Supporting documents associated with the CPGs were retrieved to inform the quality appraisal process. No CPGs were excluded following quality appraisal. Findings from the quality appraisal were synthesised to address the tertiary objective of this review. Supplementary file 4 (Appendix) presents the quality appraisal for this systematic review and supplementary file 5 (Appendix) summarises quality appraisal findings.
Role of the funding source
The funder of the study had no role in the study design, data analysis, data interpretation, or writing of the report. All authors had full access to all the data in the study. All authors accept responsibility for the decision to submit for publication.
Results
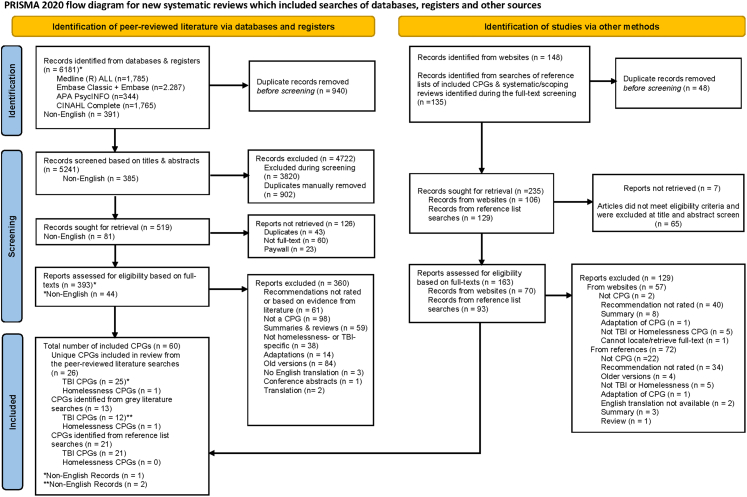
The systematic search identified 60 unique CPGs (non-English language, n = 3) that met inclusion criteria for this systematic review. Of the 60 CPGs, 58 were CPGs for TBI and two were CPGs for homelessness.16,25 Fig. 1 presents the PRISMA Flow Chart documenting the study selection process and Supplementary Table S5 presents the characteristics of included CPGs.
Fig. 1.
PRISMA flow chart. The PRISMA flow chart shows the number of studies identified, included, and excluded from each source and phase of the review, and the reasons for exclusion.
Inclusion of homelessness information in CPGs for TBI
Three (5.2%) CPGs for TBI were text-positive26, 27, 28 for homelessness. Two CPGs acknowledged or made reference to data regarding individuals experiencing homelessness or with lived experience of homelessness, without recommendations (i.e., category 2),27,28 while the other mentioned keywords consistent with individuals experiencing homelessness or with lived experience of homelessness without context related to the literature or recommendations (i.e., category 3).26 One CPG acknowledged the disproportionate prevalence of TBI among individuals experiencing homelessness,28 while the rest identified housing as an important consideration in the assessment and management of TBI.26,27 Specifically, one CPG recommended exploring issues related to housing27 in the assessment of individuals with persistent symptoms, while the other CPG identified housing as a psychosocial issue that may be addressed through case management.26 Of the text-negative CPGs, none of the articles in the reference list included keywords for homelessness (i.e., category 2). Supplementary Table S5 presents the text and relevant keywords from the three text-positive TBI CPGs.
Inclusion of TBI information in CPGs for homelessness
Both CPGs for homelessness were text-positive16,25 and acknowledged or made reference to data regarding individuals with TBI, without recommendations (i.e., category 2). These CPGs noted brain injury as prevalent among individuals experiencing homelessness25 and recognised individuals experiencing homelessness and brain injury as a marginalised population that should be prioritised in guideline development.16 One CPG recommended that communication and information provision (e.g., resources and forms, explanations, etc.) should be tailored to individuals who may have speech, language, and communication difficulties, including individuals with brain injury25 and identified individuals with brain injury as needing onsite specialist support or higher levels of wrap-around support25 in order to stay housed. Supplementary Table S5 presents the text and relevant keywords from the text-positive homelessness CPGs.
Quality appraisal
A minority of CPGs for TBI considered equity, including disadvantaged populations, in guideline development. Disadvantaged populations highlighted in CPGs for TBI and CPGs for homelessness included individuals: experiencing homelessness;16,25 of a non-white race/ethnicity;28,29 of a lower socioeconomic status or experiencing financial barriers to accessing services;27,30 living in underserved regions (remote and rural areas, limited access to care in small medical centres);31, 32, 33 with a history of incarceration or who are in correction and detention facilities;28,34 who experienced intimate partner violence;28 of cultural and ethnic groups;26,27,29,35, 36, 37, 38, 39, 40, 41 and from aboriginal communities.42, 43, 44, 45 Up to five CPGs for TBI (≤8.8%) discussed TBI burden,27,42,44, 45, 46 biology of the condition, patient adherence to intervention, baseline risks, and/or care42,44 for disadvantaged populations, and up to six CPGs for TBI (≤10.5%) dedicated part of or the entire CPG to the care of disadvantaged populations,42, 43, 44 considered their perspective42,44,45,47, 48, 49 and provided separate recommendations,35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45,49 and/or discussed barriers and strategies to implementing recommendations for disadvantaged populations.31, 32, 33,35, 36, 37, 38, 39, 40, 41, 42,44
Representatives of disadvantaged populations were rarely included in guideline development. Only two CPGs for TBI (3.5%) included representatives of disadvantaged populations in their guideline group,50,51 only one (1.7%) involved representatives in rating the importance of interventions and outcomes,50 and only one other CPG (1.7%) included disadvantaged populations as the target audience.44 No CPGs for TBI explicitly reported considering equity in their process of identifying the target audience and recruiting group members or having a chair or a methodologist who is familiar with equity issues.
Notably, 22 CPGs for TBI (37.9%)28, 29, 30,35, 36, 37, 38, 39, 40, 41, 42,44,45,47,48,52, 53, 54, 55, 56, 57, 58, 59, 60, 61, 62, 63, 64, 65 considered one or more of the PROGRESS-plus elements when synthesizing evidence and four CPGs (6.9%)42, 43, 44, 45 sought evidence specific to disadvantaged populations and offered specific recommendations.42, 43, 44, 45 Race was considered in only six CPGs for TBI (10.3%),26,29,46,57,59,66 and sex-specific guidelines were not provided, even though sex was often highlighted as a risk factor for TBI. Two CPGs (3.4%) for TBI also explicitly excluded data from disadvantaged populations, as they did not consider them representative of the general TBI population.34,67 Finally, while five TBI CPGs (8.6%) produced tools to facilitate the implementation of CPGs among disadvantaged populations,30,32,42,49,68 no CPG included a plan for monitoring and/or auditing the implementation and use of the CPGs among disadvantaged groups.
In contrast, equity was often considered in the content and development of CPGs for homelessness. However, neither included a plan for monitoring and/or auditing the implementation and use of the CPGs among disadvantaged groups.
Discussion
This systematic review highlights the urgency to integrate evidence on homelessness and TBI in CPGs for TBI and homelessness, respectively, and to consider equity in the content and development of CPGs for TBI and homelessness. Only 3 out of 58 CPGs for TBI integrated evidence regarding homelessness, and evidence integrated in both CPG groups were limited to TBI prevalence and the importance of prioritizing TBI16,25 and considering housing during TBI assessment and management.26, 27, 28
Evidence regarding homelessness must be considered in CPGs for TBI because existing recommendations may be impracticable for this population. For example, a number of CPGs recommended diagnosis, comprehensive assessment, treatment, or follow-up care through a primary care provider or primary care team,26,27,33,58,64,69 which may not be readily accessible to or are often avoided by individuals experiencing homelessness due to negative experiences.70 Individuals with TBI who experience homelessness are more likely to be seen in the emergency department and are less likely to access or have access to other healthcare services, particularly primary care,71 which is crucial in connecting individuals to rehabilitation and community-based supports.72,73 Additionally, a history of homelessness among individuals with TBI suggests existing comorbidities, health inequities, and experiences of trauma70 that need to be managed alongside TBI sequelae.5 The latter, for example, requires clinicians to utilise a trauma-informed approach and strengthen efforts to build trust with their clients.70 CPGs must address these gaps in order to advance equity and promote quality of care for individuals with lived experience of TBI and homelessness.
Similarly, given that the relationship between homelessness and TBI has been investigated prior to the publication of CPGs for homelessness, it is critical that CPGs for homelessness go beyond acknowledging that TBI is prevalent and highlight the relationship between TBI and homelessness.7,8,74,75 In particular, homelessness may lead to recurring TBIs,8,75and individuals who sustain a TBI may be at risk of experiencing homelessness7,74,75 and adverse mental and physical health comorbidities.7,76 These findings support the need for timely and specialised services following TBI identification according to the needs of those affected.7,76 Integrating these research findings in CPGs for homelessness also serves as an avenue to educate healthcare providers about TBI and homelessness, which can help address healthcare professionals’ lack of confidence to serve individuals with TBI, their perception of TBI as an “unknown” and complex condition,77 and their need for education on TBI identification and management.77 Importantly, awareness and education on TBI and homelessness among healthcare providers builds the foundation for developing recommendations that are appropriate and achievable for this population.
Our findings also revealed that equity considerations are lacking, particularly in CPGs for TBI. For instance, disadvantaged populations are rarely involved in the development of CPGs and in rating the importance of outcomes and interventions. Co-creation of research and healthcare through the engagement of disadvantaged populations or individuals with lived experience in all stages of guideline development is critical to achieving person-centred care.78 Involving individuals with lived experience in guideline development ensures that recommendations are supported by their experiences and areas that are important to them are prioritised.79 This also aligns with the World Health Organization's vision of centring people and communities in health services and empowering and engaging individuals and families, communities, and disadvantaged populations.78
Furthermore, while PROGRESS-plus elements were identified in the content of 22 CPGs for TBI, concrete care recommendations were often absent. For example, race was rarely considered in CPGs, and sex, while often mentioned as a risk factor, was not accompanied by sex-specific guidelines or recommendations. The absence of concrete care recommendations for disadvantaged populations in CPGs may be attributed to the limited studies on such groups due to their repeated exclusion in research.80 In fact, two CPGs in this review specifically excluded disadvantaged populations, as they were not seen as representative of the larger population of individuals with TBI.34,67 More research focused on and with disadvantaged populations is needed to build the evidence base for this group. Such research should also take into account barriers for research participation.80 Finally, despite increasing calls for inclusion, diversity, equity, and accessibility considerations in healthcare,72 the proportion of CPGs that considered equity did not increase over time. Similarly, among CPGs that considered equity, the number of equity statements that were considered also did not increase over time.
We acknowledge the following limitations of this review. First, we did not systematically search for research studies on TBI and homelessness. As such, we cannot evaluate the extent to which research to date is integrated in existing CPGs for TBI and homelessness. Second, while we did not have restrictions on language, country, or year in our search, the number of non-English language CPGs is likely an underestimate, as our search was conducted in English. Despite the aforementioned limitations, our systematic review has the following strengths. This systematic review is the first, to our knowledge, to assess equity considerations in CPGs for TBI and homelessness. The protocol for this systematic review was published in a peer-reviewed journal.14 To further increase replicability and transparency, we utilised a rigorous search strategy using validated search filters for CPGs15 and methodological guides to grey literature searching.20 In particular, the search for grey literature, is an important strength of this review, given the low precision of searching databases for peer-reviewed CPGs.15 Finally, we presented the findings of this review to the Program Advisory Committee (PAC) of the Traumatic Brain Injury in Underserved Populations Research Program for feedback. The PAC consists of front-line staff and service providers who work with disadvantaged populations who experience TBI; organisations that represent individuals with TBI; health administrators; decision-makers and policy-makers and researchers who conduct research on TBI among disadvantaged populations.
There is an urgent need to advance equity in CPGs for TBI and homelessness. There is limited considerations for homelessness and TBI in existing CPGs for TBI and homelessness, respectively, beyond recognizing TBI prevalence and the need to prioritise TBI16,25,28 and consider housing in TBI assessment and management.26,27 Additionally, despite increasing calls for inclusion, diversity, equity, and accessibility in healthcare, equity considerations, including the engagement of disadvantaged populations, in CPGs for TBI and homelessness remain limited. Given that TBI is disproportionately prevalent among individuals who experience homelessness,2 the consideration of homelessness and TBI in CPGs for TBI and homelessness, respectively, is critical to increase awareness and education among healthcare providers and to develop recommendations that are appropriate and achievable for this population. The engagement of disadvantaged populations in all stages of guideline development and research focused on disadvantaged populations must also be prioritised to ensure that CPGs that guide healthcare reflect and address the needs of disadvantaged groups. Finally, future CPGs should be co-created with service providers, researchers, policymakers, and individuals with lived experience to ensure the CPGs are sensitive to the healthcare needs of disadvantaged populations, including individuals experiencing homelessness and TBI.
Contributors
VC and AC conceptualised the systematic review. VC, MJE, and JB developed the search strategy. VC and MJE formulated the design. VC, MJE, SH, and ZC screened the articles and extracted the data. VC, MJE, JMJ, and SH completed the quality appraisal of included CPGs. VC, MJE, SH, ZC, and JMJ completed the analyses for this review. VC and MJE drafted the manuscript and verified the underlying data. All authors critically reviewed and approved the final manuscript. All authors had full access to all the data in the study and accept responsibility for the decision to submit for publication.
Data sharing statement
All data in this systematic review are publicly available. All extracted data are available in the online supplementary files.
Declaration of interests
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgements
We would like to acknowledge Selina Rattana and Anson Li for editorial review of the data extracted and content of the manuscript. We would like to further acknowledge the PAC of the Traumatic Brain Injury in Underserved Populations Research Program for their feedback on this systematic review.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.eclinm.2023.102152.
Appendix A. Supplementary data
References
- 1.Maas A.I.R., Menon D.K., Adelson P.D., et al. Traumatic brain injury: integrated approaches to improve prevention, clinical care, and research. Lancet Neurol. 2017;16(12):987–1048. doi: 10.1016/S1474-4422(17)30371-X. [DOI] [PubMed] [Google Scholar]
- 2.Stubbs J.L., Thornton A.E., Sevick J.M., et al. Traumatic brain injury in homeless and marginally housed individuals: a systematic review and meta-analysis. Lancet Public Health. 2020;5(1):e19–e32. doi: 10.1016/S2468-2667(19)30188-4. [DOI] [PubMed] [Google Scholar]
- 3.Perry D.C., Sturm V.E., Peterson M.J., et al. Association of traumatic brain injury with subsequent neurological and psychiatric disease: a meta-analysis. J Neurosurg. 2016;124(2):511–526. doi: 10.3171/2015.2.JNS14503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Eslava-Schmalbach J., Mosquera P., Alzate J.P., et al. Considering health equity when moving from evidence-based guideline recommendations to implementation: a case study from an upper-middle income country on the GRADE approach. Health Pol Plan. 2017;32(10):1484–1490. doi: 10.1093/heapol/czx126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stafford A., Wood L. Tackling health disparities for people who are homeless? Start with social determinants. Int J Environ Res Public Health. 2017;14(12) doi: 10.3390/ijerph14121535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bowen E., Savino R., Irish A. In: Homelessness prevention and intervention in social work: policies, programs, and practices. Larkin H., Aykanian A., Streeter C.L., editors. Springer International Publishing; Cham: 2019. Homelessness and health disparities: a health equity lens; pp. 57–83. [Google Scholar]
- 7.Stubbs J.L., Thornton A.E., Gicas K.M., et al. Characterizing traumatic brain injury and its association with losing stable housing in a community-based sample. Can J Psychiatr. 2021;67(3):207–215. doi: 10.1177/07067437211000665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cusimano M.D., Korman M.B., Carpino M., et al. The temporal relations of traumatic brain injury, victimization, aggression, and homelessness: a developmental trajectory. Neurotrauma Rep. 2021;2(1):103–114. doi: 10.1089/neur.2020.0050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.To M.J., O'Brien K., Palepu A., et al. Healthcare utilization, legal incidents, and victimization following traumatic brain injury in homeless and vulnerably housed individuals: a prospective cohort study. J Head Trauma Rehabil. 2015;30(4):270–276. doi: 10.1097/HTR.0000000000000044. [DOI] [PubMed] [Google Scholar]
- 10.Institute of medicine (US) committee on standards for developing trustworthy clinical practice guidelines. Clinical practice guidelines we can trust. National Academies Press; Washington (DC): 2011. [PubMed] [Google Scholar]
- 11.Dheansa S., Rajwani K.M., Pang G., et al. Relationship between guideline adherence and outcomes in severe traumatic brain injury. Ann R Coll Surg Engl. 2022;105(5):400–406. doi: 10.1308/rcsann.2022.0031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dans A.M., Dans L., Oxman A.D., et al. Assessing equity in clinical practice guidelines. J Clin Epidemiol. 2007;60(6):540–546. doi: 10.1016/j.jclinepi.2006.10.008. [DOI] [PubMed] [Google Scholar]
- 13.World Health Organization Health equity. https://www.who.int/health-topics/health-equity#tab=tab_1 [cited 2022 July 12]. Available from:
- 14.Chan V., Estrella M.J., Babineau J., Colantonio A. A systematic review protocol for assessing equity in clinical practice guidelines for traumatic brain injury and homelessness. Front Med. 2022;9 doi: 10.3389/fmed.2022.815660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lunny C., Salzwedel D.M., Liu T., et al. Validation of five search filters for retrieval of clinical practice guidelines produced low precision. J Clin Epidemiol. 2020;117:109–116. doi: 10.1016/j.jclinepi.2019.09.022. [DOI] [PubMed] [Google Scholar]
- 16.Pottie K., Kendall C.E., Aubry T., et al. Clinical guideline for homeless and vulnerably housed people, and people with lived homelessness experience. CMAJ. 2020;192(10):E240. doi: 10.1503/cmaj.190777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chan V., Estrella M.J., Babineau J., Colantonio A. Protocol for a scoping review on rehabilitation among individuals who experience homelessness and traumatic brain injury. BMJ Open. 2021;11(11) doi: 10.1136/bmjopen-2021-052942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Di B.-S., Wei M., Ma W.-J., et al. A critical review to traumatic brain injury clinical practice guidelines. Medicine. 2019;98(9) doi: 10.1097/MD.0000000000014592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Library M. Systematic reviews, scoping reviews, and other knowledge syntheses. 2023. https://libraryguides.mcgill.ca/knowledge-syntheses/updating [updated May 18, 2023. Available from:
- 20.Godin K., Stapleton J., Kirkpatrick S.I., Hanning R.M., Leatherdale S.T. Applying systematic review search methods to the grey literature: a case study examining guidelines for school-based breakfast programs in Canada. Syst Rev. 2015;4(1):138. doi: 10.1186/s13643-015-0125-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.The Canadian agency for drugs and technologies in health (CADTH) 2018. GreyMatters: a practical tool for searching health-related grey literature Ottawa: CADTH.https://www.cadth.ca/grey-matters-practical-tool-searching-health-related-grey-literature Available from: [cited July 12] [Google Scholar]
- 22.Tannenbaum C., Clow B., Haworth-Brockman M., Voss P. Sex and gender considerations in Canadian clinical practice guidelines: a systematic review. CMAJ Open. 2017;5(1):E66–e73. doi: 10.9778/cmajo.20160051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Popay J., Roberts H., Sowden A., et al. 2006. Guidance on the conduct of narrative synthesis in systematic reviews: a product from the ESRC methods programme. [Google Scholar]
- 24.Welch V.A., Akl E.A., Guyatt G., et al. GRADE equity guidelines 1: considering health equity in GRADE guideline development: introduction and rationale. J Clin Epidemiol. 2017;90:59–67. doi: 10.1016/j.jclinepi.2017.01.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.National Institute for Health and Care Excellence . 2022. Integrated health and social care for people experiencing homelessness. [PubMed] [Google Scholar]
- 26.The management and rehabilitation of post-acute mild traumatic brain injury work group . 2021. VA/DoD clinical practice guideline for the management and rehabilitation of post-acute mild traumatic brain injury. [cited August 18, 2022] [Google Scholar]
- 27.The management of concussion-mild traumatic brain injury working group . Department of Veterans Affairs and Department of Defense; 2016. VA/DoD clinical practice guideline for the management of concussion-mild traumatic brain injury. [cited August 18, 2022] [Google Scholar]
- 28.Physicians ACoE . 2023. Clinical policy: critical issues in the management of adult patients presenting to the emergency department with mild traumatic brain injury. [Google Scholar]
- 29.Kennedy M.R., Coelho C., Turkstra L., et al. Intervention for executive functions after traumatic brain injury: a systematic review, meta-analysis and clinical recommendations. Neuropsychol Rehabil. 2008;18(3):257–299. doi: 10.1080/09602010701748644. [DOI] [PubMed] [Google Scholar]
- 30.Trevena L., Cameron I., Porwal M. 2004. Clinical practice guidelines for the care of people living with traumatic brain injury in the community. [cited August 18, 2022] [Google Scholar]
- 31.Da Dalt L., Parri N., Amigoni A., et al. Italian guidelines on the assessment and management of pediatric head injury in the emergency department. Ital J Pediatr. 2018;44(1):7. doi: 10.1186/s13052-017-0442-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ontario Neurotrauma Foundation . 2021. Living guideline for pediatric concussion care. [cited August 18, 2022] [Google Scholar]
- 33.Scottish Intercollegiate Guidelines Network . 2009. Early management of patients with a head injury: a national clinical guideline. Hillside Crescent, Edinburgh. [cited August 18, 2022] [Google Scholar]
- 34.Warden D.L., Gordon B., McAllister T.W., et al. Guidelines for the pharmacologic treatment of neurobehavioral sequelae of traumatic brain injury. J Neurotrauma. 2006;23(10):1468–1501. doi: 10.1089/neu.2006.23.1468. [DOI] [PubMed] [Google Scholar]
- 35.Bayley M.T., Janzen S., Harnett A., et al. INCOG 2.0 guidelines for cognitive rehabilitation following traumatic brain injury: what's changed from 2014 to now? J Head Trauma Rehabil. 2023;38(1):1–6. doi: 10.1097/HTR.0000000000000826. [DOI] [PubMed] [Google Scholar]
- 36.Bayley M.T., Janzen S., Harnett A., et al. INCOG 2.0 guidelines for cognitive rehabilitation following traumatic brain injury: methods, overview, and principles. J Head Trauma Rehabil. 2023;38(1):7–23. doi: 10.1097/HTR.0000000000000838. [DOI] [PubMed] [Google Scholar]
- 37.Jeffay E., Ponsford J., Harnett A., et al. INCOG 2.0 guidelines for cognitive rehabilitation following traumatic brain injury, Part III: executive functions. J Head Trauma Rehabil. 2023;38(1):52–64. doi: 10.1097/HTR.0000000000000834. [DOI] [PubMed] [Google Scholar]
- 38.Ponsford J., Trevena-Peters J., Janzen S., et al. INCOG 2.0 guidelines for cognitive rehabilitation following traumatic brain injury, Part I: posttraumatic amnesia. J Head Trauma Rehabil. 2023;38(1):24–37. doi: 10.1097/HTR.0000000000000840. [DOI] [PubMed] [Google Scholar]
- 39.Ponsford J., Velikonja D., Janzen S., et al. INCOG 2.0 guidelines for cognitive rehabilitation following traumatic brain injury, Part II: attention and information processing speed. J Head Trauma Rehabil. 2023;38(1):38–51. doi: 10.1097/HTR.0000000000000839. [DOI] [PubMed] [Google Scholar]
- 40.Togher L., Douglas J., Turkstra L.S., et al. INCOG 2.0 guidelines for cognitive rehabilitation following traumatic brain injury, Part IV: cognitive-communication and social cognition disorders. J Head Trauma Rehabil. 2023;38(1):65–82. doi: 10.1097/HTR.0000000000000835. [DOI] [PubMed] [Google Scholar]
- 41.Velikonja D., Ponsford J., Janzen S., et al. INCOG 2.0 guidelines for cognitive rehabilitation following traumatic brain injury, Part V: memory. J Head Trauma Rehabil. 2023;38(1):83–102. doi: 10.1097/HTR.0000000000000837. [DOI] [PubMed] [Google Scholar]
- 42.Motor Accidents Authority New South Wales . 2008. Guidelines for mild traumatic brain injury following closed head injury. [cited August 18, 2022] [Google Scholar]
- 43.Morgan A.M.C., Anderson V., Waugh M.-C., Cahill L., The TBI Guideline Expert Working Committee . 2017. Clinical practice guideline for the management of communication and swallowing disorders following paediatric traumatic brain injury. [cited August 18, 2022] [Google Scholar]
- 44.New Zealand Guidelines Group . 2006. Traumatic brain injury: diagnosis, acute management and rehabilitation. The Terrace. Wellington, New Zealand. [cited August 18, 2022] [Google Scholar]
- 45.Stergiou-Kita M., Dawson D., Rappolt S. Inter-professional clinical practice guideline for vocational evaluation following traumatic brain injury: a systematic and evidence-based approach. J Occup Rehabil. 2012;22(2):166–181. doi: 10.1007/s10926-011-9332-2. [DOI] [PubMed] [Google Scholar]
- 46.Lumba-Brown A., Yeates K.O., Sarmiento K., et al. Centers for disease control and prevention guideline on the diagnosis and management of mild traumatic brain injury among children. JAMA Pediatr. 2018;172(11) doi: 10.1001/jamapediatrics.2018.2853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Carney N., Totten A.M., O'eilly C., et al. Brain Trauma Foundation; 2016. Guidelines for the management of severe traumatic brain injury. [cited August 18, 2022] [Google Scholar]
- 48.Hawryluk G.W.J., Rubiano A.M., Totten A.M., et al. Guidelines for the management of severe traumatic brain injury: 2020 update of the decompressive craniectomy recommendations. Neurosurgery. 2020;87(3):427–434. doi: 10.1093/neuros/nyaa278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.National Institute for Health and Care Excellence . 2014. Head injury: assessment and early management. [cited August 18, 2022] [Google Scholar]
- 50.Luauté J., Hamonet J., Pradat-Diehl P. Behavioral and affective disorders after brain injury: French guidelines for prevention and community supports. Ann Phys Rehabil Med. 2016;59(1):68–73. doi: 10.1016/j.rehab.2015.10.007. [DOI] [PubMed] [Google Scholar]
- 51.Luauté J., Plantier D., Wiart L., Tell L. Care management of the agitation or aggressiveness crisis in patients with TBI. Systematic review of the literature and practice recommendations. Ann Phys Rehabil Med. 2016;59(1):58–67. doi: 10.1016/j.rehab.2015.11.001. [DOI] [PubMed] [Google Scholar]
- 52.Broglio S.P., Cantu R.C., Gioia G.A., et al. National Athletic Trainers' Association position statement: management of sport concussion. J Athl Train. 2014;49(2):245–265. doi: 10.4085/1062-6050-49.1.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Evans R., Whitlow C.T. 2022. Acute mild traumatic brain injury (concussion) in adults. [cited August 18, 2022] [Google Scholar]
- 54.Harmon K.G., Clugston J.R., Dec K., et al. American Medical Society for Sports Medicine position statement on concussion in sport. Br J Sports Med. 2019;53(4):213. doi: 10.1136/bjsports-2018-100338. [DOI] [PubMed] [Google Scholar]
- 55.Lim M., Baumann C.R. 2021. Sleep-wake disorders in patients with traumatic brain injury. [cited August 18, 2022] [Google Scholar]
- 56.Meehan W., O'Brien M.J. 2022. Concussion in children and adolescents: management. [cited August 18, 2022] [Google Scholar]
- 57.National Clinical Guideline C . National Institute for Health and Care Excellence (UK) Copyright © National Clinical Guideline Centre, 2014; London: 2014. National institute for health and clinical excellence: guidance. Head injury: triage, assessment, investigation and early management of head injury in children, young people and adults. [Google Scholar]
- 58.Ontario Neurotrauma Foundation . 2018. Guideline for concussion/mild traumatic brain injury & prolonged symptoms. [cited August 18, 2022] [Google Scholar]
- 59.Pediatric mTBI Guideline Workgroup . 2016. Systematic review and clinical recommendations for healthcare providers on the diagnosis and management of mild traumatic brain injury among children. [cited August 18, 2022] [Google Scholar]
- 60.Quatman-Yates C.C., Hunter-Giordano A., Shimamura K.K., et al. Physical therapy evaluation and treatment after concussion/mild traumatic brain injury. J Orthop Sports Phys Ther. 2020;50(4):CPG1–CPG73. doi: 10.2519/jospt.2020.0301. [DOI] [PubMed] [Google Scholar]
- 61.Ryan M.E., Pruthi S., Desai N.K., et al. ACR appropriateness Criteria® head trauma-child. J Am Coll Radiol. 2020;17(5s):S125–S137. doi: 10.1016/j.jacr.2020.01.026. [DOI] [PubMed] [Google Scholar]
- 62.Schytz H. 2021. Post-traumatic headache. [Google Scholar]
- 63.Shih R.Y., Burns J., Ajam A.A., et al. ACR appropriateness Criteria® head trauma: 2021 update. J Am Coll Radiol. 2021;18(5S):S13–S36. doi: 10.1016/j.jacr.2021.01.006. [DOI] [PubMed] [Google Scholar]
- 64.Vos P.E., Battistin L., Birbamer G., et al. EFNS guideline on mild traumatic brain injury: report of an EFNS task force. Eur J Neurology. 2002;9(3):207–219. doi: 10.1046/j.1468-1331.2002.00407.x. [DOI] [PubMed] [Google Scholar]
- 65.Giza C.C., Kutcher J.S., Ashwal S., et al. Summary of evidence-based guideline update: evaluation and management of concussion in sports. Neurology. 2013;80(24):2250. doi: 10.1212/WNL.0b013e31828d57dd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.National Institute of Excellence in Health and Social Services (INESSS) ONF . 2016. Clinical practice guideline for the rehabilitation of adults with moderate to severe TBI. [cited August 18, 2022] [Google Scholar]
- 67.Alali A.S., Mukherjee K., McCredie V.A., et al. Beta-blockers and traumatic brain injury: a systematic review, meta-analysis, and eastern association for the surgery of trauma guideline. Ann Surg. 2017;266(6):952–961. doi: 10.1097/sla.0000000000002286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.New South Wales Ministry of Health . 2011. Initial management of closed head injury in adults. [cited August 18, 2022] [Google Scholar]
- 69.Marshall S., Bayley M., McCullagh S., et al. Updated clinical practice guidelines for concussion/mild traumatic brain injury and persistent symptoms. Brain Inj. 2015;29(6):688–700. doi: 10.3109/02699052.2015.1004755. [DOI] [PubMed] [Google Scholar]
- 70.Lemsky C., Jenkins D., King B., et al. Health Care for the Homeless Council, Inc.; Nashville, TN: 2018. Adapting your practice: recommendations for the care of patients who are homeless or unstably housed living with the effects of traumatic brain injury. [cited September 14, 2022] [Google Scholar]
- 71.Vohra N., Paudyal V., Price M.J. Homelessness and the use of Emergency Department as a source of healthcare: a systematic review. Int J Emerg Med. 2022;15(1):32. doi: 10.1186/s12245-022-00435-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.National Academies of Sciences E, and Medicine . The National Academies Press; Washington, DC: 2022. Traumatic brain injury: a roadmap for accelerating progress. [PubMed] [Google Scholar]
- 73.Liu M., Hwang S.W. Health care for homeless people. Nat Rev Dis Primers. 2021;7(1):5. doi: 10.1038/s41572-020-00241-2. [DOI] [PubMed] [Google Scholar]
- 74.Topolovec-Vranic J., Ennis N., Howatt M., et al. Traumatic brain injury among men in an urban homeless shelter: observational study of rates and mechanisms of injury. CMAJ Open. 2014;2(2):E69–E76. doi: 10.9778/cmajo.20130046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Topolovec-Vranic J., Ennis N., Colantonio A., et al. Traumatic brain injury among people who are homeless: a systematic review. BMC Public Health. 2012;12(1):1059. doi: 10.1186/1471-2458-12-1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Topolovec-Vranic J., Schuler A., Gozdzik A., et al. The high burden of traumatic brain injury and comorbidities amongst homeless adults with mental illness. J Psychiatr Res. 2017;87:53–60. doi: 10.1016/j.jpsychires.2016.12.004. [DOI] [PubMed] [Google Scholar]
- 77.Estrella M.J., Kirsh B., Kontos P., et al. Critical characteristics of housing and housing supports for individuals with concurrent traumatic brain injury and mental health and/or substance use challenges: a qualitative study. Int J Environ Res Public Health. 2021;18(22) doi: 10.3390/ijerph182212211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.World Health Organization . World Health Organization; 2015. WHO global strategy on integrated people-centred health services 2016 - 2026. [cited November 23, 2022] [Google Scholar]
- 79.Lindsay M.P., Gierman N., Harris J.E., et al. People with lived experience at the centre of Canadian stroke best practice recommendations: a model for guideline developers. J Patient Exp. 2020;7(6):951–956. doi: 10.1177/2374373520956538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Finnegan M., O'Donoghue B. Rethinking vulnerable groups in clinical research. Ir J Psychol Med. 2019;36(1):63–71. doi: 10.1017/ipm.2017.73. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.