ABSTRACT
Aim and objective
To assess and compare children's anxiety level and pain perception during cavity preparation using an erbium-doped yttrium aluminum garnet (Er:YAG) laser vs traditional rotational treatment.
Materials and methods
A randomized, controlled, split-mouth clinical trial was carried out in 35 healthy children with 70 carious primary molars. Teeth were divided equally into two groups according to the method of treatment. A bur was used to prepare the cavity in one quadrant, while an Er:YAG laser was used to prepare the cavity in the other quadrant. Anxiety was assessed using Venham's dental anxiety scale and a fingertip pulse oximeter. The pain was assessed using the Wong–Baker Face Pain Rating Scale, and the number of local anesthesia (LA) needed during both procedures was also considered.
Results
The mean age was 9.4 ± 1.29. Males accounted for 51.4% of the participants. There were no statistically significant variations in pulse rate at the baseline between Er:YAG laser and the conventional treatments. The mean pulse rate was higher during the conventional intervention than during the laser intervention; this difference was statistically significant vs the baseline pulse rate. The mean pulse rate with the conventional method was significantly higher during and after cavity formation than with the laser method. The Er:YAG laser and the conventional groups showed statistically significant differences in the Venham's and Wong–Baker scores. The scores of both scales were much higher in the conventional group. The number of participants who requested LA during the conventional technique was significantly higher than during the laser procedure.
Conclusion
Using Er:YAG lasers to remove caries produces minimal pain and anxiety and reduces the requirement for LA.
Clinical significance
During cavity preparation, the Er:YAG laser helps children stay calm.
How to cite this article
Abdrabuh RE, El Meligy OAES, Felemban OM, et al. Evaluation of the Erbium-doped Yttrium Aluminum Garnet Laser and the Conventional Method on Pain Perception and Anxiety Level in Children during Caries Removal: A Randomized Split-mouth Study. Int J Clin Pediatr Dent 2023;16(S-1):S39–S44.
Keywords: Dental anxiety, Erbium-doped yttrium aluminum garnet laser, Pain, Randomized controlled clinical trial, Split-mouth
Introduction
Anxiety and avoidance of dental care are prevalent problems in dentistry, particularly among pediatric patients. It takes a substantial amount of time for a pediatric dentist and dental clinic staff member to convince pediatric patients to undergo treatment and assure them that the pain will be minimal. Pain, fear, and anxiety are common side effects of conventional procedures to remove dental carious and prepare cavities. The dental handpiece's sound, look, and vibration all contribute to patient anxiety. As a result, dental checkups may be skipped, which might increase the incidence of caries and oral diseases.1,2
Lasers have a variety of applications in dentistry as in other fields. Laser therapy of the mouth's hard and soft tissues can make going to the dentist more pleasant. Laser tissue ablation is a desirable technique for dental treatment because it causes minimal discomfort. Treatments such as caries removal need far less local anesthesia (LA) than they would with conventional procedures; in certain circumstances, cavity preparation with lasers requires no LA at all. In general, dental laser treatments are painless, bloodless, minimally invasive, and effective at preventing infections.3 Researchers have tested the suitability of many different types of lasers for almost every conceivable dental procedure, and some of them have become widely used in clinical practice. The erbium-doped yttrium aluminum garnet (Er:YAG) laser is the most versatile laser for use in dentistry.4,5 The Er:YAG laser (2940 nm) is a good tool for ablating enamel and dentine. It is potentially applicable to many other pediatric dental applications. Pediatric dentists have embraced the Er:YAG laser for caries removal and cavity preparation in enamel and dentin in clinical practice. A precise incision through the hard tissue is achieved when the laser interacts with water at the tissue interface. The laser beam's predilection for carious structures removes only a small amount of healthy tooth structure. There is a risk of producing heat injury to the underlying tissues while attaining an efficient ablation. The laser's noncontact mode produces less vibration, which encourages cooperation from children. Contamination is not a possibility when a suitable isolation strategy is used. Tissue ablation is induced by the so called “popcorn effect” and laser noise in which water molecules break cells.6,7
Pediatric dentists prefer procedures and strategies that aid in improving pediatric patient behavior. Pediatric treatment effectiveness is determined not only by the quality of the treatment but also by developing in children a positive attitude toward dental care and regular dental checkups. The use of scales to determine early detection and assessment of requirements, for children's dental anxiety is crucial. To date, behavioral scoring, psychometric evaluations, psychological exams, and projective procedures have been employed to identify dental pain and anxiety. In psychometric procedures, direct inquiries demonstrate patients’ pain and anxiety. Physiological assessment methods are used in physiological approaches. These tests assess dental phobia in a roundabout way (e.g., heart rate, pulse rate, and the response of the dorsal skin). Projective approaches allow the researcher to form an opinion on the subconscious's hidden feelings. They also ask the subjects to remark on some of the photographs. Researchers are thus attempting to uncover the link between children's emotions and the images that they create in their minds.8
Pain is subjective, and thus it is better to elicit a reaction from the child's own experience. The Wong–Baker Face Pain Rating Scale has numerous advantages: It is a self-assessment tool that consists of a row of six sample visuals (icons) ranging from “no discomfort” to “hurts the most” each with a 0–10 score. It is simple to use, takes a short amount of time to complete, and may be used with both children and teenagers. Anxiety results in a rise in sweat, blood pressure, heart rate, and pulse rate. Stress hormones such as cortisol, adrenaline, and norepinephrine are released into the system causing these alterations. In addition, Venham's behavior rating scale can assess the child's situational anxiety. It is an interval rating scale with a stable and valid rating technique that may simply be implemented into clinical or research activity. It's a six-point scale with scale points based on objective, specific, and easily identifiable behavior.9 Finally, pulse oximetry can track physiological alterations. It enables the monitoring of physiological markers such as blood pressure, heart rate, and oxygen saturation in real-time.10 Here, we evaluated and compared the pain perception, and anxiety level of laser cavity preparation vs a rotary approach in children. This study hypothesized that there would be no difference between the conventional and the Er:YAG laser methods of caries removal in pain perception and in reducing the anxiety level.
Materials and Methods
Study Design
A randomized, single-blinded, and split-mouth study was performed.
Ethical Approval
The Research Ethics Committee of the Faculty of Dentistry at King Abdulaziz University (KAU) in Jeddah, Saudi Arabia, provided ethical permission (approval number 063–02–19).
Sample Size
The clinical trial was carried out in 35 healthy children with 70 carious primary molars. Teeth were randomly and equally divided into two groups (I and II) according to the method of treatment.
Randomization
The randomization was done with a sealed envelope system used to choose which procedure for cavity preparation should be performed first.
Study Subjects
Patients aged 9–12 years old who came for a dental visit and met the inclusion criteria were chosen from the outpatient Department of Pediatric Dentistry at King Abdulaziz University Dental Hospital (KAUDH) in Jeddah, Saudi Arabia, during the period from 2019 to 2020. The patients were clinically and radiographically assessed.
Inclusion criteria were—(1) healthy patients, (2) the patients ranged in age from 9 to 12, (3) each patient had at least two active occlusal cavities reaching into the dentine in a primary molar without pulpal involvement (D3 threshold, WHO system), (4) no spontaneous pain, (5) no dental developmental problems, and (6) no abscesses, sinuses, or fistulae. Before the laser and conventional treatment procedures, the parents signed informed consent.
Treatment Procedure
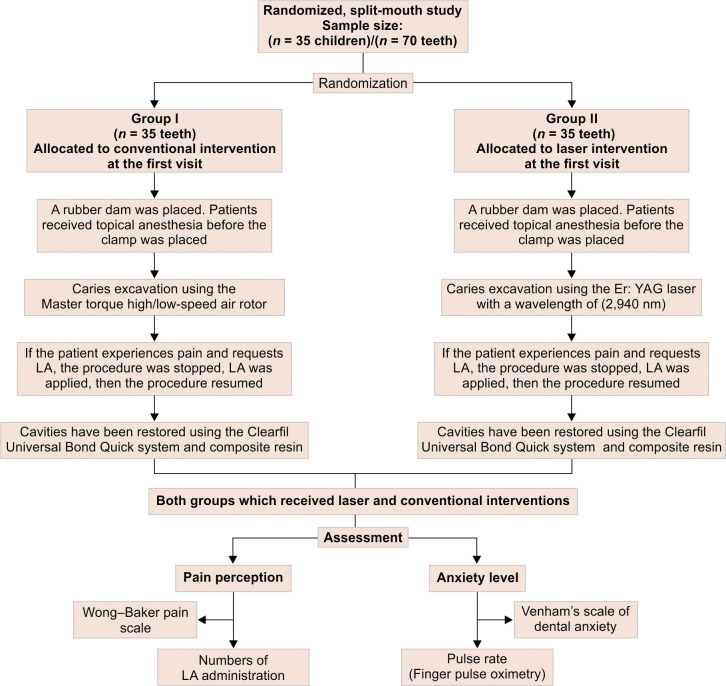
A finger pulse oximeter (ChoiceMMed MD300C2) was placed before treatment began and a baseline pulse rate was recorded. Caries-affected teeth were randomly assigned to either the conventional caries removal group (group I) or the laser caries removal group (group II). For each patient, one carious tooth was treated with the conventional method, and the contralateral carious tooth was treated using an Er:YAG laser with a split-mouth design (Fig. 1). The subjects did not know which tooth was receiving which treatment. The conventional and laser treatments occurred at two separate visits, approximately 1 week apart. The order was determined at randomization. The cavities in the conventional caries group were done using traditional rotating devices, such as high-speed and low-speed dental handpieces. The cavities in the laser caries group were done using an Er:YAG laser with a wavelength of 2940 nm. Parameters and the operative mode used for laser hard tissue therapy are 100–200 mJ/ 20 Hz with water. Complete isolation was performed using a rubber dam and saliva ejector in both groups. Patients received topical anesthesia before the clamp was placed. The procedures were performed without LA. However, the procedure was stopped for LA whenever requested, then resumed. The pulse rate was monitored during and after each cavity preparation and before beginning the restoration to evaluate the child's stimulus-induced anxiety accurately. After cavity preparation and restoration, the pain was quantified by asking the patient to indicate the face on the Wong–Baker Faces Pain Rating Scale. The treatment procedure was video recorded, and two observers other than the operator watched the video to assess the patient's behavior during the treatment procedure using Venham's scale.
Fig. 1.
Flowchart showing the study design
Statistical Analysis
Data were statistically analyzed using the Statistical Package for the Social Sciences (SPSS) version 20.0 (SPSS Inc., Chicago, Illinois). The Wilcoxon signed-rank test compared the mean difference in the pulse rate among subjects between the conventional and laser interventions; the marginal homogeneity test evaluated the difference in Venham's scale and Wong–Baker scale ratings among subjects. The number of LA requested during both interventions was evaluated by the McNemar test at the 0.05 significance level.
Results
A total of 35 out of 40 patients with 70 carious primary molars agreed to participate. The mean age was 9.4 ± 1.29. The study included both male and female patients. Males (N = 18) represented 51.4% of the subjects, while females (N = 17) represented 48.6% of the subjects.
Anxiety Level
Pulse Rate
In comparison to the mean values of pulse rate of the subjects, the mean pulse rate during and after the conventional intervention was significantly higher than the laser intervention, with a p-value of 0.001. However, there was no discernible change in pulse rate between the conventional and laser methods at the baseline (Table 1).
Table 1.
Comparison of the mean difference in the pulse rate among subjects between the conventional and laser interventions (N = 35 subjects)
| Conventional method | Er:YAG laser method | p-value | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | Standard deviation | Median | Min–Max | Mean | Standard deviation | Median | Min–Max | ||
| Mean | Standard deviation | Median | Min–Max | Mean | Standard deviation | Median | Min–Max | ||
| Pulse rate before procedure | 92.2 | 10.1 | 94.0 | 75–109 | 91.3 | 10.2 | 93.0 | 74–110 | 0.094 |
| Mean pulse rate during procedure | 108.4 | 10.3 | 111.0 | 85.0–125.3 | 95.5 | 8.7 | 97.8 | 75.5–108.8 | <0.001 |
| Pulse rate during–before the procedure | 16.2 | 8.3 | 17.5 | −3.75–37.25 | 4.19 | 8.5 | 2.8 | −14.8–30.0 | <0.001 |
| Pulse rate after the procedure | 102.9 | 9.0 | 105.0 | 75–116 | 92.7 | 9.1 | 95.0 | 70–106 | <0.001 |
| Pulse rate after–before the procedure | 10.7 | 9.4 | 10.0 | −9.0–39.0 | 1.5 | 8.6 | 1.0 | −16.0–25.0 | <0.001 |
N, Number of subjects
Venham's Scale of Dental Anxiety
The subjects during the Er:YAG laser intervention scored significantly lower scores than those during the conventional method, with a p-value of 0.001 (Table 2).
Table 2.
Distribution of Venham's scores among subjects during conventional and laser interventions (N = 35)
|
Venham's scale of dental anxiety
(N = 35 subjects) |
Laser | p-value | ||||||
|---|---|---|---|---|---|---|---|---|
| Score 0–relaxed | Score 1–uneasy | Score 2–tense | Score 3–reluctant | Score 4–interference | Score 5–out of control | |||
| Conventional | Score 0–relaxed | 2 (5.7) | 2 (5.7) | 1 (2.9) | 0 | 0 | 0 | <0.001 |
| Score 1–uneasy | 9 (25.7) | 1 (2.9) | 1 (2.9) | 0 | 0 | 0 | ||
| Score 2–tense | 7 (20.0) | 11 (31.4) | 1 (2.9) | 0 | 0 | 0 | ||
| Score 3–reluctant | 0 | 0 | 0 | 0 | 0 | 0 | ||
| Score 4–interference | 0 | 0 | 0 | 0 | 0 | 0 | ||
| Score 5–out of control | 0 | 0 | 0 | 0 | 0 | 0 | ||
N, number of subjects
Pain Perception
Wong–Baker Pain Scale
When compared to the traditional technique, children after the Er:YAG laser scored significantly lower with a p-value of 0.001 (Table 3).
Table 3.
Distribution of scores on Wong–Baker Pain Scale (N = 35 subjects)
|
Wong–Baker Pain Rating Scale
(N = 35 subjects) |
Laser | p-value | ||||||
|---|---|---|---|---|---|---|---|---|
| Score 0–no hurt | Score 2–hurts little bit | Score 4–hurts little more | Score 6–hurts even more | Score 8–hurts whole lot | Score 10–hurts worst | |||
| Conventional | Score 0–no hurt | 2 (5.7) | 2 (5.7) | 1 (2.9) | 0 | 0 | 0 | <0.001 |
| Score 2–hurts little bit | 7 (20.0) | 0 | 0 | 0 | 0 | 0 | ||
| Score 4–hurts little more | 6 (17.1) | 3 (8.6) | 2 (5.7) | 2 (5.7) | 0 | 0 | ||
| Score 6–hurts even more | 0 | 6 (17.1) | 1 (2.9) | 0 | 0 | 0 | ||
| Score 8–hurts whole lot | 0 | 2 (5.7) | 1 (2.9) | 0 | 0 | 0 | ||
| Score 10–hurts worst | 0 | 0 | 0 | 0 | 0 | 0 | ||
N, number of subjects
Administration of LA
The number of subjects who asked for LA during the conventional procedure was 15 (42.9%) and was higher than that of subjects who asked for LA during the laser procedure which was three (8.6%), with a p-value of 0.008, this difference was statistically significant (Table 4).
Table 4.
The proportions of LA requested during conventional and Er:YAG laser interventions (N = 35)
| (N = 35 subjects) | Subject asked for LA during laser | Pair-matched or (95% confidence of interval) | p-value | ||
|---|---|---|---|---|---|
| Yes | No | ||||
| Subject asked for LA during conventional | Yes | 2 (5.7) | 15 (42.9) | 0.2 (0.06–0.69) |
0.008 |
| No | 3 (8.6) | 15 (42.9) | |||
LA, local anesthesia; N, number of subjects
Discussion
Anxiety affects every child differently. As a result, their anxiety tolerance varies. Anxiety and pain have a significant relationship. General anxiety is not the same as dental anxiety—it is a reaction that can occur due to previous negative dental encounters. Pediatric patients develop conditioned reflexes when new cues are introduced to uncomfortable procedures, such as the smell in the environment and the instruments’ reverberation. Dental anxiety causes children to believe that they will experience more pain than usual and that going to the dentist will make them feel uncomfortable. As a result, they refuse to receive dental treatment.11
Dental anxiety and pain are a multifaceted notions with behavioral, cognitive, and physiological elements. The utilization of a mixture of more than one measurement approach is critical for successfully assessing youngsters with low cognitive/linguistic skills and minimal capacity to remember; using multiple metrics is a strength of this study. For example, the Wong–Baker pain scale was employed as a self-reported measure and provides an immediate state of emotional feeling regarding dental treatment when used with children. It is a reliable measure of a child's pain level.12 Venham's dental anxiety scale precisely determines the child's behavior during the dental treatment. This system has been used in previous studies and was found to have good validity.13 The pulse rate measurement determines the children's physiological arousal because its increase is attributed to stress during dental procedures.14
The current study used a split-mouth design, allowing within patient comparisons because it is a randomized, controlled single-blind trial with each participant acting as their control. The results would have been considerably more powerful if the study had utilized a double-blind methodology. However, this was not practicable because the operator who did the treatment and the observers who watched the recorded video to assess the subject's anxiety level during the treatment procedure using Venham's scale saw which excavating method was being employed. On the contrary, the subjects did not know which tooth had received which treatment. Perceived views about the two approaches may have influenced the operator's and observer's reports of treatment procedures due to the single-blind methodology. On the contrary, subjects did not know which tooth had received which treatment. Conventional and laser treatments occurred at two separate visits, approximately 1 week apart, to prevent the effect of each intervention on the patient's behavior toward the other intervention. Cavity preparations were performed by the same pediatric dentist to ensure that results were not influenced by interoperator variability. In the current study, we tried to limit the age range of the patients to achieve a more relevant spectrum of answers. All patients (N = 35) were of a similar cognitive level, 9–12-years-old. In general, children can draw on their capacity to think logically during this stage. They try to be honest, expressing their real feelings, which gives more reliability to their answers, so the evaluation of pain perception and dental anxiety level can be done accurately.
Pulse rate measurement and Venham's scale of dental anxiety were used in the current study to estimate the anxiety level of pediatric patients. When compared to the baseline pulse rate of the subjects, the pulse rate during and after the conventional approach was significantly greater than the laser approach. However, there was no discernible change in pulse rate between the conventional and laser methods at the baseline. The null hypothesis of this study was rejected after Venham's scale revealed that caries eradication using Er:YAG laser had statistically significant favorable impacts on anxiety levels when compared to the conventional approach. The probable reason for the conventional method to cause more anxiety may be due to the inevitability of high-frequency sound and vibrations that can make patients feel pain and may explain why traditional techniques generate more anxiety than laser-based methods. Erbium lasers have a noncontact mode with hard tissue and produce less vibration than the rotor, thus making dental preparations less stressful and uncomfortable. There is no odor when cavity preparation is done properly with appropriate suction. The laser's popping sound is more relaxing than the turbine's roar. Evans et al.15 reported that youngsters over the age of 10 preferred laser cavity preparation to traditional methods. They reasoned that this could be because the laser caused fewer vibrations during cavity preparation than the traditional method. Fear of the drill has been recognized as a major source of dental anxiety in children in several studies.15–18 Another study by Liu et al.19 found that laser cavity preparation reduced tooth vibration and that head or body motions were occasionally recorded during laser cavity preparations implying that it can significantly enhance a child's behavior. Our results are consistent with Eren et al.17 who discovered that patients were less anxious with an Er:YAG laser than with traditional methods. Alia et al.20 found that the sound of the dental drill has the largest impact on patients’ discomfort.
In the current study, the Wong–Baker Faces Pain Rating Scale was used to assess the pain perceptions of pediatric patients according to the literature. The findings demonstrated that when compared to conventional approaches, the Er:YAG laser demonstrated statistically significant favorable benefits on pain perception, thus rejecting the null hypothesis of the study. These findings could be connected to the adverse vibration effect of rotational equipment. Eren et al.17 compared the Er:YAG laser to a mechanical caries removal approach, and Hjertton and Bagesund21 compared the Er:YAG laser to traditional procedures vs traditional techniques, the researchers discovered that using lasers on soft and hard tissues caused less or no pain. The Er:YAG laser did not create any pressure, heat, or pain, and some children wanted to continue their therapy with it.
In the present study, we found that patients during laser treatment required less LA. This finding is consistent with DenBesten et al.22 who found that patients treated with lasers were less likely to request anesthesia than those treated with spinning tools. Similar outcomes were observed when chemomechanical caries removal was compared to traditional procedures, and a Cochrane review paper came to the same conclusion.23,24 Chandras25 found opposite results to the present study, he showed that the children had a significant preference for the bur in comparison with the use of the Er:YAG laser. Our findings are consistent with Sarmadi et al.26 who found that patients require less LA during laser treatment than with traditional methods. The probable reason for the conventional method to cause more pain may be due to the process of tooth preparation could be the source of additional discomfort caused by the rotary bur. The rotary bur prepares the cavity by abrasion, which generates heat and increases the intrapulpal temperature. The spinning tool also applies pressure to the tooth surface in the second step. The pulp is thermally injured during mechanical preparation, thus resulting in pulpal inflammation, pain, and a hyperemic rise in pulpal blood flow. On the contrary, the Er:YAG laser employs extremely short pulse durations to efficiently ablate calcified tissue layers while generating minimal heat. It has the most sensitivity for hydroxyapatite and the most water absorption vs other dental laser wavelengths. Erbium lasers have a restricted penetration and result in less tooth destruction and a lower patient sense of discomfort. The pulp temperature was reduced when water and air were used with the laser.27 However, when using a conventional bur, the temperature soared to >60° C. More inflammation and pain are caused by a larger temperature rise in the pulp.20,28
In this investigation and previous studies, using lasers for cavity preparation showed positive results when it comes to reducing anxiety and pain. Regardless of positive results, the use of lasers in the present clinical practice is still debatable. Lasers are a cutting-edge technological tool and are projected to be somewhat more costly than ordinary drills for dental operations, this cost limits their use in routine clinical practice. It is necessary to use different wavelengths for different soft and hard tissue surgeries, and thus the practitioner may need more than one laser. To buy the equipment, run the technology, and complete the necessary education and training, large initial investments are required.29,30
A laser may, however, be appropriate in some circumstances such as in children with acute dental anxiety. Patients suffering from anxiety or phobias may find the laser to be a good alternative, but further research is needed to confirm this information.
Conclusion
Using Er:YAG lasers to remove caries produces minimal pain and anxiety, reduces the requirement for LA, and is a more comfortable option for pediatric patients than conventional rotary devices.
Clinical Significance
During cavity preparation, the Er:YAG laser helps children stay calm.
Orcid
Omar Abd El Sadek El Meligy https://orcid.org/0000-0003-1069-6374
Osama M Felemban https://orcid.org/0000-0002-3212-5735
Najat MA Farsi https://orcid.org/0000-0003-0860-4573
Footnotes
Source of support: Nil
Conflict of interest: None
REFERENCES
- 1.Thakkar T, Naik S, Dixit U. Assessment of dental anxiety in children between 5 and 10 years of age in the presence of a therapy dog: a randomized controlled clinical study. Eur Arch Peadiatr Dent. 2021;22(3):459–467. doi: 10.1007/s40368-020-00583-1. [DOI] [PubMed] [Google Scholar]
- 2.Armfield JM, Heaton L. Management of fear and anxiety in the dental clinic: a review. Aust Dent J. 2013;58(4):390–407. doi: 10.1111/adj.12118. [DOI] [PubMed] [Google Scholar]
- 3.Mallishery S, Dedhia S, Sawant K. An era of lasers–application of erbium lasers in pediatric dentistry. IOSR-JDMS. 2021;18(10):1–7. doi: 10.9790/0853-1810050107. [DOI] [Google Scholar]
- 4.Nazemisalman B, Farsadeghi M, Sokhansanj M. Types of lasers and their applications in pediatric dentistry. J Lasers Med Sci. 2015;6(3):96–101. doi: 10.15171/jlms.2015.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ajwa N, Alfayez H, Al–Oqab H, et al. The effect of erbium–doped yttrium aluminum garnet laser in debonding of orthodontic brackets: a systematic review of the literature. Photobiomodul Photomed Laser Surg. 2021;39(11):725–733. doi: 10.1089/photob.2020.4985. [DOI] [PubMed] [Google Scholar]
- 6.Yang K, Ge X, Zhang BZ, et al. Effects of Er:YAG laser pre–treatment on dentin structure and bonding strength of primary teeth: an in vitro study. BMC Oral Health. 2020;20(1):1–10. doi: 10.1186/s12903-020-01315-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Thomsen S, Pearce JA. Thermal damage and rate processes in biologic tissues. Optical–thermal response of laser–irradiated tissue. Springer. 2010:487–549. doi: 10.1007/978-90-481-8831-4_13. [DOI] [Google Scholar]
- 8.Porritt J, Buchanan H, Hall M, et al. Assessing children's dental anxiety: a systematic review of current measures. Community Dent Oral Epidemio. 2013;41(2):130–142. doi: 10.1111/j.1600-0528.2012.00740.x. [DOI] [PubMed] [Google Scholar]
- 9.Venham L, Bengston D, Cipes M. Children's response to sequential dental visits. J Dent Res. 1977;56(5):454–459. doi: 10.1177/00220345770560050101. [DOI] [PubMed] [Google Scholar]
- 10.Dias D, Paulo Silva Cunha J. Wearable health devices–vital sign monitoring, systems and technologies. Sensors (Basel) 2018;18(8):2414. doi: 10.3390/s18082414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Klinberg G, Raadal M, Arnup K. In: Pediatric dentistry: a clinical approach. Koch G, Poulsen S, editors. Copenhagen: Willey Blackwell; 2009. Dental fear and behavior management problems. pp. 32–43. [Google Scholar]
- 12.Birnie KA, Noel M, Chambers CT, et al. Psychological interventions for needle–related procedural pain and distress in children and adolescents. Cochrane Database Syst Rev. 2018;10(10):CD005179. doi: 10.1002/14651858.CD005179.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cademartori M, Rosa D, Oliveira L, et al. Validity of the Brazilian version of the Venham's behavior rating scale. Int J Paediatr Dent. 2017;27(2):120–127. doi: 10.1111/ipd.12231. [DOI] [PubMed] [Google Scholar]
- 14.Marwah N, Prabhakar AR, Raju OS. Music distraction––its efficacy in management of anxious pediatric dental patients. J Indian Soc Pedod Prev Dent. 2005;23(4):168–170. doi: 10.4103/0970-4388.19003. [DOI] [PubMed] [Google Scholar]
- 15.Evans D, Matthews S, Pitts N, et al. A clinical evaluation of an Erbium: YAG laser for dental cavity preparation. Br Dent J. 2000;188(12):677–679. doi: 10.1038/sj.bdj.4800575. [DOI] [PubMed] [Google Scholar]
- 16.Belcheva A, Shindova M. Subjective acceptance of pediatric patients during cavity preparation with Er: YAG laser and conventional rotary instruments. J IMAB. 2014;20(5):631–633. doi: 10.5272/jimab.2014205.631. [DOI] [Google Scholar]
- 17.Eren F, Altinok B, Ertugral F, Tanboga I. The effect of erbium, chromium: yttrium–scandium–gallium–garnet (Er, Cr:YSGG) laser therapy on pain during cavity preparation in paediatric dental patients: a pilot study. Oral Health Dent Manag. 2013;12(2):80–84. [PubMed] [Google Scholar]
- 18.Santos CR, Tonetto MR, Presoto CD, et al. Application of Er: YAG and ER, Cr: YSGG lasers in cavity preparation for dental tissues: a literature review. World J Dent. 2012;3(4):340–343. doi: 10.5005/jp-journals-10015-1186. [DOI] [Google Scholar]
- 19.Liu JF, Lai YL, Shu WY, et al. Acceptance and efficiency of Er: YAG laser for cavity preparation in children. Photomed Laser Surg. 2006;24(4):489–493. doi: 10.1089/pho.2006.24.489. [DOI] [PubMed] [Google Scholar]
- 20.Alia S, Khan SA, Navit S, et al. Comparison of pain and anxiety level induced by laser vs rotary cavity preparation: an in vivo study. Int J Clin Pediatr Dent. 2020;13(6):590–594. doi: 10.5005/jp-journals-10005-1820. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mosskull Hjertton P, Bågesund M. Er:YAG laser or high–speed bur for cavity preparation in adolescents. Acta Odontol Scand. 2013;71(3–4):610–615. doi: 10.3109/00016357.2012.700064. [DOI] [PubMed] [Google Scholar]
- 22.DenBesten PK, White JM, Pelino JE, et al. The safety and effectiveness of an Er: YAG laser for caries removal and cavity preparation in children. Laser Med Sci. 2001;16(3):215–222. doi: 10.1078/1615-1615-00025. [DOI] [Google Scholar]
- 23.Lai G, Lara Capi C, Cocco F, et al. Comparison of Carisolv system vs traditional rotating instruments for caries removal in the primary dentition: a systematic review and meta–analysis. Acta Odontol Scand. 2015;73(8):569–580. doi: 10.3109/00016357.2015.1023353. [DOI] [PubMed] [Google Scholar]
- 24.Montedori A, Abraha I, Orso M, et al. Lasers for caries removal in deciduous and permanent teeth. Cochrane Database Syst Rev. 2016;9(9):CD010229. doi: 10.1002/14651858.CD010229.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chandras N. The use of Er: YAG laser in comparison with the traditional handpieces for pit and fissure sealants in children from 7 to 11 years old. A Comfort Study. Master thesis. 2017 [Google Scholar]
- 26.Sarmadi R, Andersson EV, Lingström P, et al. A randomized controlled trial comparing Er: YAG laser and rotary bur in the excavation of caries–patients’ experiences and the quality of composite restoration. Open Dent J. 2018;12:443–454. doi: 10.2174/1874210601812010443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Glockner K, Rumpler J, Ebeleseder K, et al. Intrapulpal temperature during preparation with the Er: YAG laser compared to the conventional burr: an in vitro study. J Clin Laser Med Surg. 1998;16(3):153–157. doi: 10.1089/clm.1998.16.153. [DOI] [PubMed] [Google Scholar]
- 28.Zhegova GG, Rashkova MR. Er–yag laser and dental caries treatment of permanent teeth in childhood. J IMAB. 2015;21(1):699–704. doi: 10.5272/jimab.2015211.699. [DOI] [Google Scholar]
- 29.Coluzzi DJ. Lasers in dentistry. Compend Contin Educ Dent. 2005;26(6A Suppl):429–435. [PubMed] [Google Scholar]
- 30.Olivi G, Genovese M. Laser restorative dentistry in children and adolescents. Eur Arch Paediatr Dent. 2011;12(2):68–78. doi: 10.1007/BF03262782. [DOI] [PubMed] [Google Scholar]