Abstract
Background and Objectives
Refusals of care in dementia can be a source of distress for people with dementia and their caregivers. Informant-based measures to examine refusals of care are limited and often measure other behaviors such as agitation. We aimed to assess the validity and reliability of the newly developed, 14-item, Refusal of Care Informant Scale (RoCIS) and then use the scale to verify the most common refusal behaviors.
Research Design and Methods
Data from 129 dyads were analyzed. Dyad was defined as a person with advanced dementia either living in a care home or supported in their own home and their caregiver. Data about the person with dementia were gathered using informant-based questionnaires. The psychometric properties of the RoCIS were investigated using Rasch analysis to determine validity and reliability.
Results
Following Rasch analysis, the item “upset” was removed from the RoCIS. The reduced 13-item RoCIS is unidimensional and achieved a reliability index of 0.85 (Cronbach’s alpha 0.88). Sixty-eight percent of people with dementia had refused care in the last month, with “verbally refused” the most common type of refusal behavior. People in the “very severe/profound” stage of dementia showed more refusal behaviors than those in the “severe” stage.
Discussion and Implications
Results provide initial evidence that the RoCIS is a valid and reliable informant-based scale measuring refusals of care in advanced dementia. Results indicate a need to develop new approaches and techniques to make assistance with personal care more acceptable to people with dementia.
Keywords: Activities of daily living, Rejection, Resistance
Background and Objectives
Over 58 million people are living with dementia globally (Alzheimer’s Disease International et al., 2020). The term dementia refers to a range of progressive neurological conditions (Alzheimer’s disease being the most common subtype), which encompass a series of cognitive symptoms affecting memory, communication, thinking, and judgment, often accompanied by changes in mood, behavior, and motivation (World Health Organization, 2021). As dementia advances people living with it require physical assistance with their personal care such as with bathing, dressing, and going to the toilet (Giebel et al., 2015).
Sometimes people who are experiencing advanced stages of dementia find assistance with their care unacceptable and refuse it (Ishii et al., 2012). Refusals of care in dementia are often understandable actions from a person with dementia when their caregiver (family carers or care-home staff in this research) attempts to assist them with a personal care activity. Refusals can be related to the caregiver approach such as if they outpace the person (Hallberg et al., 1995) or use elderspeak (a patronizing, overly simple communication style) (Williams et al., 2017); unmet needs such as the person being hungry, thirsty, or uncomfortable (Ishii et al., 2012); the person not recognizing the caregiver or understanding the caregiver’s intentions (Volicer, 2021), or being in pain, depressed, or having psychotic symptoms such as hallucinations or delusions (Galindo-Garre et al., 2015; Ishii et al., 2010). A person with dementia can refuse or indicate their dissatisfaction with the care provided in many ways, including moving away, ignoring the caregiver, verbally refusing, or becoming upset or aggressive (Mahoney et al., 1999; Volicer and Hurley, 2015).
Whatever the cause/s of a particular refusal of care, prolonged uncompleted care could lead to poor hygiene, soreness, infection, and could constitute neglect (Backhouse, 2021). Distressing situations are likely to affect negatively on a person with dementia and their caregiver’s daily lives, making refusals of care in dementia important targets for intervention (Fauth et al., 2016; Ishii et al., 2012).
Reducing Refusals of Care
Relational approaches and interventions aimed at caregivers could prevent or reduce refusals (Volicer, 2021). Several caregiving interventions have been developed to prevent or reduce refusals of care (Backhouse et al., 2020). Currently, evidence on different bathing techniques such as thermal baths or strip washes and playing recorded music during care (Backhouse et al., 2020) is the strongest in reducing refusals of care. These interventions aim to make the care interaction more acceptable and pleasant for people with dementia by adjusting the sensory experience of the care.
Measuring Refusals of Care
Measures of refusals of care, and interactions leading to these, are necessary to evaluate a person with dementia’s experiences of care interactions, difficulties within care interactions, or the effectiveness of caregiver interventions to reduce refusals occurring. People in the later stages of dementia are less able to articulate their experiences and often unable to provide information about themselves. Therefore, to gain insight into the lives of people with advanced dementia researchers and clinicians turn to informants, often the person’s caregiver. Informant-based measures can be useful to elicit caregivers’ perspectives of people with dementia’s actions.
In the past, studies have framed refusals as agitation and used informant-based agitation scales such as the Cohen Mansfield Agitation Inventory (CMAI; Cohen-Mansfield, 1986) (e.g., Hicks-Moore 2005) or the Pittsburgh Agitation Scale (Rosen et al., 1994) (e.g., Sidani et al., 2011) as an indicator of refusals of care. However, refusals of care are different to general agitation and aggression, because the former always occur within an interaction as a response to caregiver communication or actions (Volicer, 2021; Volicer et al., 2007); therefore, it is likely these scales do not accurately measure refusals of care.
Many other existing measures include a refusal of care component within a scale measuring behavior more generally (Choi et al., 2020; Galik et al., 2017). For example, one study isolated six items from the 44-item Weekly Recording of Behavior scale (Son et al., 2007) to examine refusals of care through informant-based responses (Fauth et al., 2016); some of these questions arguably did not measure refusals of care, such as with the item “wore inappropriate clothes.”
The Resistiveness-to-Care Dementia of Alzheimer’s Type (RTC-DAT) scale is a specific refusal of care measure (Mahoney et al., 1999; Volicer and Hurley, 2015). It is a 13-item observational scale, often used to score video-recorded care interactions, measuring the frequency and duration of a range of refusal behaviors. This measure has been validated using Rasch analysis (Galik et al., 2017) and is particularly suitable for use with people in the advanced stages of dementia (Volicer and van der Steen, 2014). Because observational research takes considerable time resources, access to research settings can be complex, and it is not always acceptable or practical to observe personal care interactions, there is a clear need for an informant-based measure of refusals of care. A suitable refusal of care informant-based scale was not found in the literature; therefore, we used the RTC-DAT as a starting point to develop one.
The purpose of the new scale was to record if different refusal behaviors were present or absent over the last month, identifying types of behavior that occurred. A total score of refusal behaviors is created by adding all items, which describes the magnitude of refusal behaviors that occurred in the same period. RoCIS can be used as an outcome measure, and also aid in care planning, therefore enabling future targeted intervention development.
Scale Development
Drawing on the hitherto most comprehensive delineation of refusals of care, the RTC-DAT (Mahoney et al., 1999; Volicer and Hurley, 2015), we developed an informant-based measure to assess whether and which refusal of care reactions had occurred in the last month. In meetings with lay research advisors (around a table to discuss ideas with two family carers and in separate individual meetings with two care-home staff, all of whom were assisting people with dementia) and individual meetings with two expert colleagues, we assessed items from the RTC-DAT for ease of caregiver identification, recognition, and answering and explored whether other refusal behaviors also occurred. Our lay research advisors suggested they had experienced nonresponse/ignoring and not physically cooperating as refusal behaviors, so these were added to our scale. Table 1 shows the Refusal of Care Informant Scale (RoCIS) items aligned with corresponding RTC-DAT items. Because the RoCIS is an informant measure, it asks whether each refusal behavior has occurred during personal care interactions over the last month.
Table 1.
RoCIS Items Aligned With RTC-DAT Items (Mahoney et al., 1999; Volicer and Hurley, 2015)
| RTC-DAT items (n = 13) | RoCIS items (n = 14) | Shortened item description used in this article |
|---|---|---|
| Turn away | Person leaned, moved, or looked away from caregiver | Moved away |
| Pull away | ||
| Push away | Person pushed caregiver away | Pushed caregiver away |
| Person pushed care equipment away | Pushed care equipment away | |
| Push/Pull | Person tugged at things (e.g., towel, caregiver’s clothes) | Tugged items |
| Grab object | Person gripped on to items (e.g., clothes, covers, towel, toothbrush) | Gripped on to items |
| Grab person | Person gripped on to caregiver | Gripped on to caregiver |
| Adduct | Person stiffened their body | Stiffened body |
| Hit/Kick | Person was physically aggressive (e.g., nipped, pushed, slapped, spat at, hurt caregiver) | Physically aggressive |
| Say no | Person verbally refused (declined to cooperate) | Verbally refused |
| Cry | Person was visibly upset during care | Upseta |
| Threaten | Person was verbally aggressive (e.g., shouted, shrieked) | Verbally aggressive |
| Scream/Yell | ||
| Clench mouth | Person clamped their jaw | Clamped jaw |
| No equivalent item | Person became unresponsive (e.g., ignored caregivers attempts to provide assistance) | Unresponsive |
| No equivalent item | Person would not physically cooperate (e.g., person made themselves heavy, stood or leant forward) | Not physically cooperate |
Notes: RoCIS = Refusal of Care Informant Scale; RTC-DAT = The Resistiveness-to-Care Dementia of Alzheimer’s Type Scale.
aUpset item deleted for the final scale.
We adopted the assumption that all refusal behaviors would be part of a single construct “refusals of care,” with the RoCIS identifying the type of refusal behaviors occurring and the total score indicating the magnitude of refusals of care. We hypothesized that (a) different refusal behaviors (scale items) would represent different levels of complexity in refusals, with actions becoming less socially complex, (b) dementia severity would influence the type of refusal behaviors that occur (e.g., more nonverbal and aggressive behaviors used by those more impaired), and (c) that RoCIS scores would be positively associated with agitation and negatively associated with activities of daily living (ADL) function.
Objectives
To evaluate the validity and reliability of the RoCIS and then use the scale to verify the most common refusal behaviors using a sample of people with advanced dementia.
Research Design and Methods
A Rasch analysis was employed to document and evaluate the measurement functioning of different refusal of care behaviors for people with dementia on the RoCIS (Boone, 2016). Rasch analysis is appropriate when the total score of a questionnaire stems from its items summed together (Tennant and Conaghan, 2007). Rasch analysis plots the difficulty of each scale item along a linear continuum, with some items being milder (easier) for people with dementia to enact and some more intense (difficult), and considers the ability of each respondent (Linacre, 2021). We used Rasch analysis to enable learning about the intensity of different refusal behaviors (Boone, 2016).
Design and Sample
Data for this study were derived from the Pro-CARE study, funded by the Alzheimer’s Society, United Kingdom, a cross-sectional study which aimed to determine the factors associated with refusals of care in dementia. The RoCIS was developed to be the main outcome variable for the Pro-CARE study.
Participants
A sample of 130 dyads (n = 260 participants) were recruited in England (January 2019 to May 2021) comprising 106 dyads of people supported at home with a family carer, and 24 dyads of care-home residents with a care-home staff member, from eight care homes. Both participant types were included to allow learning from each setting and determine during the Pro-CARE study whether caregiver status influenced different refusal behaviors. Care homes in England provide 24-hr accommodation and personal care through qualified nursing or care without qualified nursing. One dyad had to withdraw from the study due to family circumstances before data for the RoCIS were collected; therefore, data on n = 129 dyads were used in this analysis.
People with dementia were eligible to participate if they were aged 65 or older, had advanced dementia, and were receiving physical support with their personal care; dementia stage eligibility was assessed after consent using the Frontier Dementia Rating Scale (FRS; Mioshi et al., 2010). Family carers and care-home staff (henceforward collectively termed as caregivers) were eligible to participate if they were physically assisting the person with advanced dementia with their personal care. Other eligibility criteria included: care-home staff had assisted the person with dementia with their personal care eight times over the previous month, and family carers were the primary family carer. Caregivers were informants about the person with dementia they were supporting.
Ethical approval was granted from the Queen’s Square Research Ethics Committee, London, United Kingdom (Reference: 251339). Written and verbal information was provided to all caregivers and to people with dementia where appropriate. In line with the Mental Capacity Act (2005) of England and Wales, where a person with dementia was assessed as not having the capacity to make the research decision at that time, assent from them was sought if appropriate, and a close family member or friend who knew the person well was consulted about whether they thought the person would have been likely to have wanted to take part had they have had capacity to make the decision. Written consent was obtained for all participants.
Procedure
All data collection was conducted by the first author, who has prior experience of working in care homes, liaising with family carers, and assisting people with dementia with their personal care. Study measures were informant-based assessments filled in by the first author from face-to-face (n = 73), telephone (n = 41), and online (n = 15) interviews with caregivers.
Measures
Demographic details were taken including age, gender, ethnicity, and living situation.
Data on the following scales were collected.
The CMAI is a 29-item agitation measure including items such as screaming, biting, and pushing, each scored 1–7 to indicate frequency of behavior (total score range: 29–203). Higher scores indicate more agitation occurring in the previous 2 weeks (Cohen-Mansfield, 1986).
The Alzheimer’s Disease Cooperative Study Activities of Daily Living Inventory Severe Impairment Version (ADCS-ADL-Sev 19) is a 19-item questionnaire assessing ADL such as grooming, bathing, and going out (total score range: 0–54). Higher scores indicate greater function with ADL (Galesko et al., 1997, 2005).
The FRS, a well-validated, 30-item dementia severity staging tool assessing functional aspects of daily life, for example, self-care, behavior, and household chores (Mioshi et al., 2010). Total score is the percentage of applicable scores where no change in function was present compared to a participant’s premorbid function. Percentage scores are translated to logit scores for analysis. Lower scores indicate greater dementia severity (Mioshi et al., 2010).
The newly developed RoCIS, a 14-item scale asking whether particular refusal behaviors such as clamped jaw, not physically cooperate, and pushed caregiver away had occurred in the last month. Summative scores range between 0 and 14. Higher scores indicate more types of refusal behaviors had occurred.
Data Analyses
Descriptive statistics (n, percentage for categorical data and mean, standard deviation [SD] for continuous data), Cronbach’s alpha, and correlations were calculated in STATA/MP17.0 (STATA/MP, 2021). To evaluate validity and reliability of the RoCIS, Rasch analyses using the WINSTEPS statistical program version 5.1.4 (Linacre, 2015) were performed. The Rasch model is well known as the standard for modern psychometric evaluations (Tennant and Conaghan, 2007).
Separation and Reliability Indexes
Item separation verifies the item spread and item reliability verifies confidence in the replicability of the item difficulty hierarchy with other samples (Bond and Fox, 2015). A separation index of 3.0 and reliability of 0.9 reflects very good confirmation of the item-level difficulty hierarchy (Linacre, 2021). If item separation and reliability values are below the recommended levels, a larger sample may be needed to confirm the item difficulty hierarchy (Boone et al., 2014; Linacre, 2021).
Item Fit
Item fit was examined using infit and outfit statistics, to determine how well each item fits the Rasch model and to detect problem items. Mean square fit statistics show the size of misfit in the data (Bond and Fox, 2015). Mean squares were examined for both infit and outfit statistics, values between 0.6 and 1.4 are considered productive for measurement for rating scale data (Bond and Fox, 2015; Wright and Linacre, 1994), Z-distributions of mean squares should be between 2.00 and −2.00, outside of this range means items have significantly less compatibility with the model (Bond and Fox, 2015). Items outside the specified parameters should be assessed for possible removal from the scale targeting higher outfit items first (Boone et al., 2014).
Unidimensionality
Item polarity uses the point-measure correlation (PTMEA-Corr), to assess dimensionality and determine if responses to each item align with the overall construct. PTMEA-Corr statistics should be positive and not close to zero to show that they are consistent with the underlying construct—refusals of care (Bond and Fox, 2015). A principal component analysis (PCA) of the residuals from Rasch analysis was performed to assure the scale was measuring one construct only—refusals of care; eigenvalues up to 2.0 are confirmatory (Linacre, 2021).
Item Mapping of Difficulty
Wright maps plot persons and items along the Rasch unidimensional logit scale showing item difficulty (in relation to refusals of care: milder to more intense behaviors) and person ability, also denoting the mean and SD of each (Boone et al., 2014). A Wright map was used to assess distribution and location of items and to identify gaps where more items may be needed.
Differential Item Functioning
Differential item functioning (DIF) was examined for two subgroups: gender (male and female) and participant type (care-home resident or person supported at home). To learn more about the scale, DIF was used to determine if each item had the same intensity (difficulty) for both groups. DIF was defined using the Rasch–Welch (logistic regression) t test: this estimates a Rasch difficulty for each item for each person group, a significance of p ≤ .05 was used (Boone et al., 2014).
Convergent Validity
Convergent validity was assessed to determine if there were relationships between refusals of care (RoCIS) and agitation (CMAI) using bivariate correlation with a significance cutoff level of p ≤ .05. We hypothesized that higher agitation levels would correlate with higher refusal of care scores on the RoCIS.
Results
Table 2 shows the characteristics of the people with dementia and their caregivers. People with dementia were on average 80 years old, 52% male, mostly married or with a partner (74%), and predominantly White (97%). Caregivers were 65 years old on average, 71% female, mostly spouses or care workers, predominantly White 96%, and had on average been caring for the person with dementia 5 years. All participants with dementia scored severe (n = 92), very severe (n = 35), or profound (n = 2) on the FRS, with a mean of severe (range −6.66 to −0.4, mean −2.27, SD: 1.19). Due to low sample size (n = 2), the profound category was combined with the very severe category for analysis. People with dementia were reported as having moderate to severe functional dependence with 67% of participants scoring 27/54 or less on the ADCS-ADL-Sev (range 0–46, mean 20.31, SD: 12.58), and showing minimal agitation (CMAI range 29–85, mean 43.92, SD: 13.34).
Table 2.
Participant Characteristics
| Variable | Mean (SD) | Range | n (%) |
|---|---|---|---|
| Person with dementia (n = 129) | |||
| Age in years | 80.28 (7.95) | 65–99 | |
| Gender | |||
| Males | 67 (51.9) | ||
| Females | 62 (48.1) | ||
| Marital status | |||
| Married/with partner | 96 (74.4) | ||
| Widowed | 26 (20.2) | ||
| Single | 3 (2.3) | ||
| Divorced | 4 (3.1) | ||
| Ethnicity | |||
| White | 125 (96.9) | ||
| Black | 1 (0.8) | ||
| Asian | 2 (1.6) | ||
| Mixed | 1 (0.8) | ||
| Dementia severity | |||
| Severe | 92 (71.3) | ||
| Very severe | 35 (27.1) | ||
| Profound | 2 (1.6) | ||
| Frontier Dementia Rating Scale | −2.27 (1.19) | 5.39 to −6.66 | |
| Cohen Mansfield Agitation Inventorya | 43.92 (13.34) | 29–203 | |
| ADCS-ADL-Sev 19a | 20.31 (12.58) | 0–54 | |
| Caregiver (n = 129) | |||
| Age in years | 64.9 (16.40) | 19–87 | |
| Gender | |||
| Males | 37 (28.7) | ||
| Females | 92 (71.3) | ||
| Ethnicitya | |||
| White | 123 (96.1) | ||
| Black | 2 (1.6) | ||
| Asian | 3 (2.3) | ||
| Caregiver relationship to person with dementia | |||
| Spouse/partner | 85 (65.9) | ||
| Child | 15 (11.6) | ||
| Other family member | 3 (2.3) | ||
| Friend | 2 (1.6) | ||
| Care worker | 17 (13.2) | ||
| Senior care worker | 7 (5.4) | ||
| Length of time caring for the person with dementia in years | 5.26 (3.45) | 0.5–20 |
Notes: ADCS-ADL-Sev 19 = Alzheimer’s Disease Cooperative Study Activities of Daily Living Inventory Severe Impairment Version.
a n = 128.
Adapting the RoCIS
An initial Rasch analysis showed that the mean squares of infit and outfit statistics for most items were within the recommended range (0.6–1.4). However, two items, “upset” and “verbally refused,” had mean squares over 1.4 for outfit and infit and Z-scores over 2.0 (see Supplementary Table 1) indicating too much variation in the responses and that these items had less compatibility with the model. When the most misfitting item, “upset,” was removed, the whole model item separation and reliability increased from 2.22 and 0.83 to 2.39 and 0.85, respectively. When “upset” and “verbally refused” were both removed from the model, whole model item separation and reliability dropped to 1.62 and 0.72, respectively. Due to this drop in whole model reliability, and after considering the items from a clinical perspective, we decided to remove only “upset” from the RoCIS. The following analyses and results refer to the reduced 13-item RoCIS after the item “upset” was removed.
Separation and Reliability Indexes
For the reduced 13-item RoCIS whole model real item separation was 2.39 (more than two levels of separation) and item reliability was 0.85, which are acceptable, but indicate a larger sample size may be needed in future to confirm the item difficulty hierarchy. Cronbach’s alpha coefficient was 0.88, which was within the optimal range (Streiner and Norman, 2003).
Item Fit
Table 3 shows the infit and outfit statistics. The mean squares of fit statistics for all items were found to be within the recommended range (0.6–1.4), except “verbally refused,” which has a mean square of 1.58 for outfit and 2.45 for infit and Z-scores over 2.0 indicating more variation than that would be ideal in the responses for this item and less compatibility with the model. “Verbally refused” should be a target for improvement in the future.
Table 3.
Refusal of Care Informant Scale (RoCIS) Item Statistics in Order of Fit
| Item | Infit | Outfit | Item mapping order | PTMEA-Corr/item validity | ||
|---|---|---|---|---|---|---|
| mnsq | ZSTD | mnsq | ZSTD | 1 = mildest | ||
| Verbally refused | 1.58 | 4.37 | 2.45 | 3.61 | 1 | 0.52 |
| Clamped jaw | 1.27 | 1.74 | 1.34 | 1.24 | 8 | 0.53 |
| Unresponsive | 1.13 | 0.98 | 1.27 | 1.23 | 4 | 0.61 |
| Moved away | 1.20 | 1.39 | 1.25 | 1.11 | 5 | 0.59 |
| Physically aggressive | 0.98 | −0.05 | 0.72 | −0.58 | 13 | 0.57 |
| Pushed care equipment away | 0.95 | −0.30 | 0.87 | −0.37 | 9 | 0.63 |
| Verbally aggressive | 0.94 | −0.42 | 0.83 | −0.78 | 2 | 0.68 |
| Gripped on to caregiver | 0.92 | −0.57 | 0.86 | −0.55 | 6 | 0.66 |
| Gripped on to items | 0.83 | −1.31 | 0.72 | −1.41 | 3 | 0.71 |
| Not physically cooperate | 0.80 | −1.08 | 0.51 | −1.27 | 12 | 0.62 |
| Tugged items | 0.78 | −1.29 | 0.49 | −1.54 | 11 | 0.64 |
| Stiffened body | 0.77 | −1.55 | 0.52 | −1.84 | 10 | 0.68 |
| Pushed caregiver away | 0.76 | −1.83 | 0.68 | −1.44 | 7 | 0.71 |
Notes: mnsq = mean square; PTMEA-Corr = point-measure correlation.
Unidimensionality
Table 3 shows the PTMEA-Corr values for each item in the RoCIS, all are well over zero scoring 0.52 and over (range 0.52–0.71). These scores, typically termed as item-total correlation in classical test theory, indicate the correlation between the item score and the overall assessment score. In our results, all items being over 0.5 indicates very good discrimination; referring to how well each item differentiates between participants who refuse and those that do not refuse. PCA showed that eigenvalues for the five principal components of Rasch residuals ranged from 2.10 to 1.18 which indicates no obvious deviation from unidimensionality. Results seem to confirm that the RoCIS scale measures “refusals of care” as one single construct, as hypothesized.
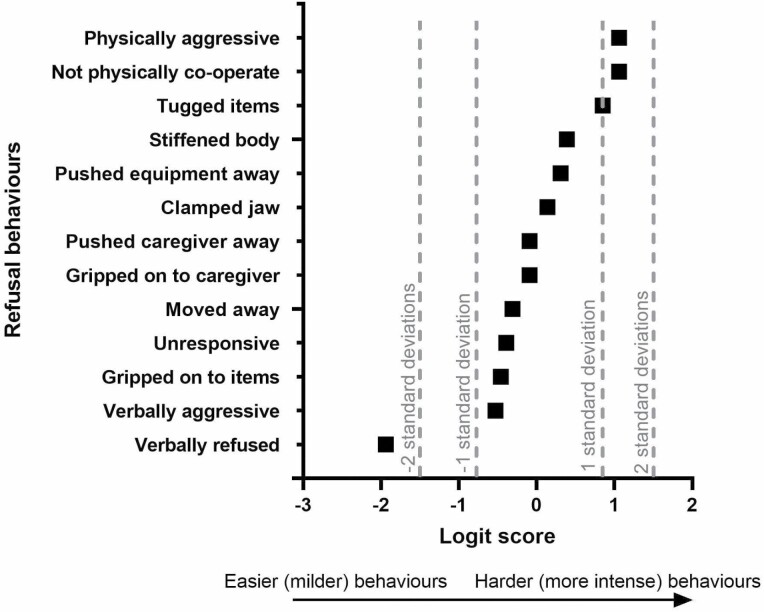
Item Mapping
Item mapping order is shown in Figure 1. “Verbally refused” was the easiest refusal behavior demonstrated by the person with dementia and detected by the scale; “physical aggression” the most intense. There was a large gap in logits between the easiest item “verbally refused” (−1.94) and the second easiest item “verbally aggressive” (−53), indicating the addition of more easy items may benefit the scale.
Figure 1.
Refusal behaviors in order of difficulty showing logits and positioning on scale.
Differential Item Functioning
DIF was assessed for gender and participant type (care-home resident and person supported at home). There were statistically significant differences for gender for two items: “moved away” (p = .04) showing this item was less likely from males and “clamped jaw” (p = .02) showing this item was less likely from females. There was a statistically significant difference for participant type for one item: “unresponsive” (p = .03) showing this item was less likely from care-home residents.
Convergent Validity
People with dementia who were more agitated on the CMAI demonstrated more refusals of care (r = 0.55, p < .01) and those with greater ability with ADLs demonstrated less refusals of care (r = −0.46, p < .01). Therefore, higher agitation levels were correlated to more refusal behaviors and greater function with ADLs to less refusal behaviors.
Are There Differences in Refusals of Care by Dementia Severity?
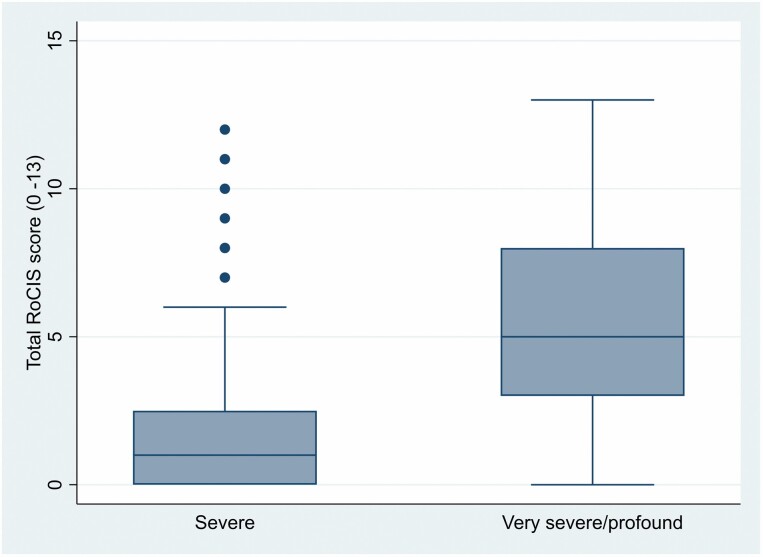
We used the newly validated 13-item RoCIS to determine the number of refusal behaviors and frequency of different refusals of care in relation to dementia severity in our sample. Sixty-eight percent of participants (88/129) had refused care in the last month (range 0–13, mean 2.97, SD: 3.44). Table 4 shows summary statistics; people with very severe/profound dementia demonstrated the highest number of different refusal behaviors (mean 5.46; SD: 3.45) compared to those with severe (mean 1.98; SD: 2.91), with over 75% in the very severe/profound stage demonstrating three or more different refusal behaviors (see Supplementary Table 2). Figure 2 shows the distribution of the overall RoCIS score by dementia severity.
Table 4.
Summary Statistics of the RoCIS by Dementia Severity
| Dementia severity | Descriptive statistics of overall RoCIS score | |||
|---|---|---|---|---|
| Mean | SD | Skewness | Kurtosis | |
| Severe | 1.98 | 2.91 | 1.84 | 5.62 |
| Very severe/profound | 5.46 | 3.45 | 0.35 | 2.32 |
Notes: RoCIS = Refusal of Care Informant Scale; SD = standard deviation.
Figure 2.
Boxplot of the overall Refusal of Care Informant Scale (RoCIS) score distribution by dementia severity.
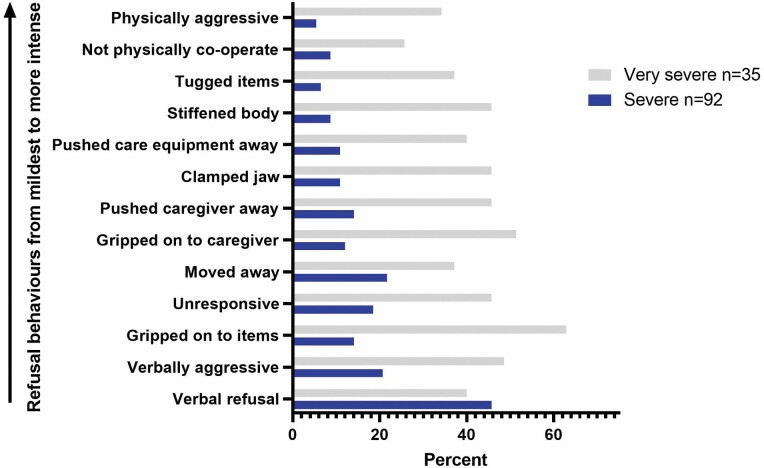
Overall, 384 refusal behaviors were reported. As shown in Table 5, “verbally refused” was the most common refusal behavior (44.2% of participants), with “verbally aggressive” (27.9%) and gripped on to items (27.1%) the next two most common. Figure 3 shows the percentage of different refusal behaviors ordered from milder to more intense by dementia stage. Milder behaviors were most common for those with severe dementia, whereas people with very severe/profound dementia demonstrated behaviors more evenly across the range of intensities.
Table 5.
Items Reported by Dementia Severity
| Item | Total caregivers reporting item (n = 129) | Severe (n = 92) | Very severe/profound (n = 37) |
|---|---|---|---|
| n (%) | n (%) | n (%) | |
| Verbally refused | 57 (44.2) | 42 (45.7) | 15 (40.5) |
| Verbally aggressive | 36 (27.9) | 19 (20.7) | 17 (45.9) |
| Gripped on to items | 35 (27.1) | 13 (14.1) | 22 (59.5) |
| Unresponsive | 34 (26.4) | 17 (18.5) | 17 (45.9) |
| Moved away | 33 (25.6) | 20 (21.7) | 13 (35.1) |
| Gripped on to caregiver | 30 (23.3) | 11 (12.0) | 19 (51.4) |
| Pushed caregiver away | 30 (23.3) | 13 (14.1) | 17 (45.9) |
| Clamped jaw | 27 (20.9) | 10 (10.9) | 17 (45.9) |
| Pushed care equipment away | 25 (19.4) | 10 (10.9) | 15 (40.5) |
| Stiffened body | 24 (18.6) | 8 (8.7) | 16 (43.2) |
| Tugged items | 19 (14.7) | 6 (6.5) | 13 (35.1) |
| Not physically cooperate | 17 (13.2) | 8 (8.7) | 9 (24.3) |
| Physically aggressive | 17 (13.2) | 5 (5.4) | 12 (32.4) |
Figure 3.
Refusal behaviors reported by dementia stage ordered from the mildest to the more intense items.
Discussion and Implications
The RoCIS was developed to provide a much-needed informant-based measure of refusals of care in advanced dementia. This article has described the development and content of the RoCIS and provided initial evidence for its validity and reliability while also verifying the most common refusal behaviors in a sample of care-home residents and people supported at home living with advanced dementia. One item “upset” was removed from the 14-item RoCIS due to misfitting the Rasch model. The remaining 13-item RoCIS showed good reliability and validity for measuring “refusals of care” in advanced dementia. Analyses of unidimensionality suggested that the 13 refusal behaviors were part of a single construct “refusals of care.” The RoCIS is likely to be useful for measuring the magnitude of refusals of care in research and clinical settings.
The significant correlation between agitation behaviors on the CMAI and refusals of care demonstrates convergent validity, supports our hypothesis, and aligns with previous research showing people with dementia who experience agitation are likely to also refuse care (Galik et al., 2017; Kable et al., 2012). However, the correlation was not so high as to indicate refusals of care are the same as agitation; indeed, they have different causes, with refusals being relational and created within interactions (Volicer, 2021), and they require different interventions (Kable et al., 2012). Additionally, the negative correlation with ADL function indicates a link between refusals and functional impairment, with higher support needs linked to more refusals.
Differences in item functioning were found for three items. These items could have been considered for deletion; however, the individual items fit the Rasch model and in our view their deletion would have reduced the clinical applicability of the scale. Care-home residents were less likely to be “unresponsive” than people supported at home. This could be due to personal relationships between family members being closer or taken for granted, meaning ignoring a person is easier for people supported at home than in social or formal relationships, which would be found in care-home settings. Rasch items are rated by level of difficulty and analysis showed females found “clamped jaw” more intense, and males found “moved away” more intense, which could be linked to males being more likely to engage in physically combative situations than females (Björkqvist, 2018).
The results seem to confirm our hypothesis that different refusal behaviors (scale items) would represent different levels of complexity in refusals, with actions becoming less socially complex. This was indicated by “verbally refused” and “verbally aggressive” being the mildest items for people with dementia to demonstrate and also the most socially complex to enact requiring verbal abilities. Whereas more intense refusal behaviors such as “not physically cooperate” and “physically aggressive” were the most intense to demonstrate and less socially complex, making use of the physical body to demonstrate refusal.
Our results provide some support for our hypothesis that dementia severity would influence the type of refusal behaviors that occur. Our data showed that people with very severe/profound dementia were more likely to use a range of intensities of refusal behaviors including more intense refusal behaviors (physical movements) than those with severe dementia who predominantly used “verbally refused.” Social complexity may be relevant here due to people with very severe/profound dementia having lower ability to articulate their feelings verbally meaning they may resort to more physical refusals. Alternatively, it could indicate that people with dementia who are more impaired become angrier and more physical, perhaps due to not understanding caregivers’ intentions.
A Rasch analysis of the RTC-DAT observational scale (Galik et al., 2017), which informed the development of the RoCIS, found “cry” and “say no” to be easier items in the scale and while fitting the model they had the highest mean square scores for outfit and infit. These items underpinned the RoCIS items “upset” and “verbally refused” which were the most misfitting items in our Rasch analysis. Clinically, “upset” can be viewed as a way for the person to show the caregiver that they are not happy with the care being conducted but may not be a refusal. “Verbally refused” is an important refusal behavior as a way for people with dementia to refuse without being combative such as with pushing equipment away or not physically cooperating. In this way “verbally refused” can be viewed as a more socially acceptable mode of refusing. Analysis showed more easy items would enhance the scale and “verbally refused” was the easiest refusal behavior for people with dementia to demonstrate, so was important to retain. However, the RoCIS does not enable us to determine whether people with dementia who verbally refused did so before care commenced or during care interactions.
Measuring refusal behaviors will allow the type of behaviors caregivers are encountering to be determined and enable the development of targeted interventions for adapting caregiver approaches and making care more acceptable to the person with dementia. The RoCIS allows a snapshot of refusals over the last month to be obtained quickly and easily by researchers and clinicians enabling knowledge of the scale of the phenomenon to be gained and clinical advice to be tailored to particular modes of refusal.
Strengths and Limitations
The RoCIS is an informant-based measure; therefore, responses relied on caregivers’ interpretations of the questions and their interpretation of which behaviors by people with dementia were categorized as refusals. Informant-based scales may elicit biased answers, especially if the caregiver has been rejected (and perhaps insulted) by the person with dementia. Assessing interrater reliability from more than one caregiver per person with dementia would have strengthened the results. The instrument development stage could have involved further consultations and used formal methods. The sample included people from two key settings of dementia care allowing learning about both settings; however, there were less data from care-home settings. A larger sample may have increased item separation and reliability index scores. Still, the RoCIS is the first informant-based scale to support assessment of refusals of behavior in advanced dementia. It is easy and quick to complete, and cost-effective as it is a paper questionnaire.
Conclusion
This study provides initial evidence that the RoCIS is a reliable and valid scale for use with caregivers of people living with advanced dementia. The RoCIS provides an essential informant-based measure of refusals of care for use in research and clinical settings. Future work could consider: (a) adapting the item “verbally refused” for better fit, because the relatively extreme statistics for this item could indicate a second dimension, and (b) adding more refusal behaviors to the scale which are easy for people with dementia to demonstrate. Refusals of care are most common in the very severe/profound stage, with verbal refusals the most common mode of refusal overall. There is a need to develop new approaches and techniques to make assistance with personal care more acceptable to people with dementia. The RoCIS is free for academic use and available from the corresponding author.
Supplementary Material
Acknowledgments
We gratefully acknowledge the time our family carer and care-home staff participants gave to the study, the involvement of people with advanced dementia, and the insightful input from our lay advisory group members: Peter Davis, Julie Lang, and Derek Buttle.
Contributor Information
Tamara Backhouse, School of Health Sciences, University of East Anglia, Norwich, Norfolk, UK.
Mizanur Khondoker, Norwich Medical School, University of East Anglia, Norwich, Norfolk, UK.
Anne Killett, School of Health Sciences, University of East Anglia, Norwich, Norfolk, UK.
Eneida Mioshi, School of Health Sciences, University of East Anglia, Norwich, Norfolk, UK.
Funding
T. Backhouse was supported by a fellowship award from the Alzheimer’s Society, UK (372 (AS-JF-17-002)). T. Backhouse, E. Mioshi, and A. Killett are supported by the National Institute for Health Research Applied Research Collaboration East of England (ARC EoE) programme. The views expressed are those of the authors and not necessarily those of the Alzheimer’s Society, National Institute for Health Research, or the University of East Anglia.
Conflict of Interest
None declared.
References
- Alzheimer’s Disease International, Guerchet, M., Prina, M., & Prince, M. (2020). Numbers of people with dementia worldwide: An update to the estimates in the World Alzheimer Report 2015. Numbers of people with dementia worldwide | Alzheimer’s Disease International (ADI). www.alzint.org [Google Scholar]
- Backhouse, T. (2021). Understanding and reducing refusals of personal care in dementia. Nursing and Residential Care, 23(3), 1–8. doi: 10.12968/nrec.2021.23.3.8 [DOI] [Google Scholar]
- Backhouse, T., Dudzinski, E., Killett, A., & Mioshi, E. (2020). Strategies and interventions to reduce or manage refusals in personal care in dementia: A systematic review. International Journal of Nursing Studies, 109, 103640. doi: 10.1016/j.ijnurstu.2020.103640 [DOI] [PubMed] [Google Scholar]
- Björkqvist, K. (2018). Gender differences in aggression. Current Opinion in Psychology, 19, 39–42. doi: 10.1016/j.copsyc.2017.03.030 [DOI] [PubMed] [Google Scholar]
- Bond, T. G., & Fox, C. M. (2015). Applying the Rasch model fundamental measurement in the human sciences (3rd ed.). Routledge. [Google Scholar]
- Boone, W. J. (2016). Rasch analysis for instrument development: Why, when, and how? CBE Life Sciences Education, 15, 1–7. doi: 10.1187/cbe.16-04-0148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boone, W. J., Staver J. R., & Yale, M. S. (2014). Rasch analysis in the human sciences. Springer. [Google Scholar]
- Choi, S. S. W., Cajita, M. I., & Gitlin, L. N. (2020). A review of measures of three common dementia-related behaviors: Rejection of care, aggression, and agitation. Geriatric Nursing, 41, 692–708. doi: 10.1016/j.gerinurse.2020.04.003 [DOI] [PubMed] [Google Scholar]
- Cohen-Mansfield, J. (1986). Agitated behaviors in the elderly II. Preliminary results in the cognitively deteriorated. Journal of the American Geriatrics Society, 34, 722–727. doi: 10.1111/j.1532-5415.1986.tb04303.x [DOI] [PubMed] [Google Scholar]
- Fauth, E. B., Femia, E. E., & Zarit, S. H. (2016). Resistiveness to care during assistance with activities of daily living in non-institutionalized persons with dementia: Associations with informal caregivers’ stress and well-being. Aging & Mental Health, 20, 888–898. doi: 10.1080/13607863.2015.1049114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galasko, D., Bennett, D., Sano, M., Ernesto, C., Thomas, R., Grundman, M., & Ferris, S. (1997). An inventory to assess activities of daily living for clinical trials in Alzheimer’s disease. The Alzheimer’s Disease Cooperative Study. Alzheimer Disease and Associated Disorders, 11, S33–S39. doi: 10.1097/00002093-19970012-00005 [DOI] [PubMed] [Google Scholar]
- Galasko, D., Schmitt, F., Thomas, R., Jin, S., & Bennett, D. (2005). Alzheimer’s Disease Cooperative Study. Detailed assessment of activities of daily living in moderate to severe Alzheimer’s disease. Journal of the International Neuropsychological Society, 11, 446–453. doi: 10.1017/s1355617705050502 [DOI] [PubMed] [Google Scholar]
- Galik, E., Resnick, B., Vigne, E., Holmes, S. D., & Nalls, V. (2017). Reliability and validity of the resistiveness to care scale among cognitively impaired older adults. Journal of the American Medical Directors Association, 18, 59–64. doi: 10.1016/j.jamda.2016.08.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galindo-Garre, F., Volicer, L., & van der Steen, J. T. (2015). Factors related to rejection of care and behaviors directed towards others: A longitudinal study in nursing home residents with dementia. Dementia and Geriatric Cognitive Disorders Extra, 5, 123–134. doi: 10.1159/000369158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giebel, C. M., Sutcliffe, C., & Challis, D. (2015). Activities of daily living and quality of life across different stages of dementia: A UK study. Aging & Mental Health, 19, 63–71. doi: 10.1080/13607863.2014.915920 [DOI] [PubMed] [Google Scholar]
- Hallberg, I. R., Holst, G., Nordmark, A., & Edberg, A.-K. (1995). Cooperation during morning care between nurses and severely demented institutionalized patients. Clinical Nursing Research, 4, 78–104. doi: 10.1177/105477389500400108 [DOI] [PubMed] [Google Scholar]
- Hicks-Moore, S. L. (2005). Relaxing music at mealtime in nursing homes: Effects on agitated patients with dementia. Journal of Gerontological Nursing, 31, 26–32. doi: 10.3928/0098-9134-20051201-07 [DOI] [PubMed] [Google Scholar]
- Ishii, S., Streim, J. E., & Saliba, D. (2010). Potentially reversible resident factors associated with rejection of care behaviors. Journal of the American Geriatrics Society, 58, 1693–1700. doi: 10.1111/j.1532-5415.2010.03020.x [DOI] [PubMed] [Google Scholar]
- Ishii, S., Streim, J. E., & Saliba, D. A. (2012). Conceptual framework for rejection of care behaviors: Review of literature and analysis of role of dementia severity. Journal of the American Medical Directors Association, 13, 11–23.e2. doi: 10.1016/j.jamda.2010.11.004 [DOI] [PubMed] [Google Scholar]
- Kable, A., Guest, M., & McLeod, M. (2012). Resistance to care: Contributing factors and associated behaviours in healthcare facilities. Journal of Advanced Nursing, 69, 1747–1760. doi: 10.1111/jan.12035 [DOI] [PubMed] [Google Scholar]
- Linacre, J. M. (2015). Winsteps Rasch measurement (computer software). Winsteps. [Google Scholar]
- Linacre, J. M. (2021). WINSTEPS® MINISTEP Rasch-model computer programs. Program manual 5.1.5. Winsteps Help for Rasch Analysis 5.1.5. Winsteps. [Google Scholar]
- Mahoney, E. K., Hurley, A. C., Volicer, L., Bell, M., Gianotis, P., Hartshorn, M., Lane, P., Lesperance, R., MacDonald, S., Novakoff, L., Rheaume, Y., Timms, R., Warden, V. (1999). Development and testing of the resistiveness to care scale. Research in Nursing & Health, 22, 27–38. doi: [DOI] [PubMed] [Google Scholar]
- Mental Capacity Act. (2005). c.9. HMSO. [Google Scholar]
- Mioshi, E., Hsieh, S., Savage, S., Hornberger, M., & Hodges, J. R. (2010). Clinical staging and disease progression in frontotemporal dementia. Neurology, 74, 1591–1597. doi: 10.1212/WNL.0b013e3181e04070 [DOI] [PubMed] [Google Scholar]
- Rosen, J., Burgio, L., Kollar, M., Cain, M., Allison, M., Fogleman, M., Michael, M., & Zubenko, G. S. (1994). The Pittsburgh Agitation Scale: A user-friendly instrument for rating agitation in dementia patients. The American Journal of Geriatric Psychiatry, 2, 52–59. doi: 10.1097/00019442-199400210-00008 [DOI] [PubMed] [Google Scholar]
- Sidani, S., Streiner, D., & LeClerc, C. (2011). Evaluating the effectiveness of the abilities-focused approach to morning care of people with dementia. International Journal of Older People Nursing, 7, 37–45. doi: 10.1111/j.1748-3743.2011.00273.x [DOI] [PubMed] [Google Scholar]
- Son, J., Erno, A., Shea, D. G., Femia, E. E., Zarit, S. H., & Stephens, M. A. (2007). The caregiver stress process and health outcomes. Journal of Aging and Health, 19, 871–887. doi: 10.1177/0898264307308568 [DOI] [PubMed] [Google Scholar]
- STATA/MP17. (2021). Stata statistical software for data science. https://www.stata.com/statamp/.
- Streiner, D. L., & Norman, G. R. (2003). Health measurement scales: A practical guide to their development and use (3rd ed.). Oxford University Press. [Google Scholar]
- Tennant, A., & Conaghan, P. G. (2007). The Rasch measurement model in rheumatology: What is it and why use it? When should it be applied, and what should one look for in a Rasch paper? Arthritis and Rheumatism, 15, 1358–1362. doi: 10.1002/art.23108 [DOI] [PubMed] [Google Scholar]
- Volicer, L. (2021). Importance of distinguishing reactive and proactive aggression in dementia care. Journal of Geriatric Psychiatry and Neurology, 34, 243–247. doi: 10.1177/0891988720924706 [DOI] [PubMed] [Google Scholar]
- Volicer, L., Bass, E. A., & Luther, S. L. (2007). Agitation and resistiveness to care are two separate behavioral syndromes of dementia. Journal of the American Medical Directors Association, 8, 527–532. doi: 10.1016/j.jamda.2007.05.005 [DOI] [PubMed] [Google Scholar]
- Volicer, L., & Hurley, A. (2015). Assessment scales for advanced dementia. Health Professions Press. [Google Scholar]
- Volicer, L., & van der Steen, J. T. (2014). Outcome measures for dementia in the advanced stage and at the end of life. Advances in Geriatrics, 2014, 346485. doi: 10.1155/2014/346485 [DOI] [Google Scholar]
- Williams, K. N., Perkhounkova, Y., Herman, R., & Bossen, A. (2017). A communication intervention to reduce resistiveness in dementia care: A cluster randomized controlled trial. The Gerontologist, 57, 707–718. doi: 10.1093/geront/gnw047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2021). Dementia. https://www.who.int/news-room/fact-sheets/detail/dementia
- Wright, B. D., & Linacre, J. M. (1994). Reasonable mean-square fit values. Rasch Measurement Transactions, 8, 370–371. https://rasch.org/rmt/rmt83b.htm [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.