Abstract
Purpose
To analyze the distribution of bacteria and their drug resistance changes in Intensive Care Units (ICUs) across Southwest China from 2018 to 2022 and establish the antibiogram in this region to provide a basis for early empirical antimicrobial use.
Methods
Non-repetitive pathogens isolated from 109 member units with qualified data were obtained from the Antimicrobial Resistance Surveillance System in Sichuan Province, southwest China. The results obtained were interpreted with reference to CLSI M100-31th, and analyzed with WHONET 5.6 software.
Results
A total of 46,728 clinical isolates in ICUs were collected from 2018 to 2022, of which gram-negative organisms accounted for 76.1%, and gram-positive were 23.9%. The top 5 were Klebsiella pneumoniae, Acinetobacter baumannii, Escherichia coli, Pseudomonas aeruginosa and Staphylococcus aureus, respectively. From 2018 to 2022, the resistance rates of Klebsiella pneumoniae to imipenem and meropenem changed from 14.5% and 17.8% to 14.0% and 14.4%, showing a steady downward trend. Escherichia coli was always highly sensitive to carbapenems, with a total resistance rate of 3.8%. Among non-fermented gram-negative bacteria, the resistance rates of Pseudomonas aeruginosa to imipenem and meropenem decreased significantly, changed from 25.3% and 22.9% in 2018 to 20.0% and 15.1% in 2022. However, Acinetobacter baumannii showed high resistance rates of 76.2% and 76.9% to imipenem and meropenem, respectively. MRSA and MRCNS accounted for 31.7% and 82.7%, respectively. No vancomycin and linezolid-resistant Staphylococcus aureus was isolated. Enterococcus faecalis maintained high activity to vancomycin, teicoplanin, and linezolid; no vancomycin or teicoplanin-resistant Enterococcus faecium strains were detected.
Conclusion
From 2018 to 2022, the isolated bacteria in ICU were mainly gram-negative bacteria, and the growth of some multidrug-resistant bacteria was effectively controlled. All levels of medical institutions should continue to strengthen bacterial resistance surveillance, promote the establishment of antimicrobial stewardship program, and enhance restrictions on outpatient antimicrobial use.
Keywords: intensive care unit, bacterial resistance surveillance, multidrug-resistant bacteria, change of drug-resistant rate
Introduction
Antibiotic resistance, a growing global health problem, is one of the most important determinants of outcomes in patients with severe infections.1–3 The World Health Organization (WHO) has warned that the misuse of antibiotics has resulted in a new elevation in the global antibiotic resistant rate, which further exacerbates the depletion of antibiotics.4 Due to the emergence of drug-resistant bacteria, the treatment of clinical infectious diseases has faced more severe challenges, and meanwhile, the frequency of nosocomial infections is gradually increasing. Of the more than 700,000 medical-associated infections in the United States each year, more than half were caused by drug-resistant bacteria, and nearly half of the infections caused by drug-resistant bacteria were derived from intensive care unit (ICU).5 Carbapenemase-resistant Enterobacteriaceae (CRE) bacteria has been spreading rapidly in Europe.6,7 Methicillin-resistant Staphylococcus aureus (MRSA), vancomycin-resistant Enterococci (VRE), carbapenem-resistant Acinetobacter baumannii (CRAB) and carbapenem-resistant Pseudomonas aeruginosa (CRPA) have contributed to multidrug-resistant (MDR), extensively drug-resistant (XDR), and pandrug-resistant (PDR), which has further provoked an increase in related infections within medical institutions.8 As the rate of antibiotic resistance continues to rise, so do the morbidity, mortality, and treatment costs associated with infection among patients in healthcare settings, especially in the ICU setting.9
Initial appropriate antibiotic therapy (IAAT) is a key determinant of severe infection outcome,10 and the Surviving Sepsis Guidelines highly recommended that patients receive timely and appropriate antibiotic therapy to reduce mortality.11 However, not all serious infections are caused by drug-resistant bacteria, clinicians must develop strategies to determine which patients are candidates for broad-spectrum antibiotic therapy. Antimicrobial stewardship program (ASP) has been shown to be effective in reducing unnecessary antibiotic use and improving patient outcomes,10,12 the difficulty lies in how to balance the need for IAAT to improve patient outcomes with the need to avoid unnecessary antibiotic use to reduce resistance emergence. ASP in ICU should include expected effect and feedback of antimicrobial prescription, treatment course monitoring, prescribing restriction and use of the regional antibiogram.13,14 The establishment of a regional antibiogram facilitates the improvement of the success rate of early empiric antibiotic treatment.
Therefore, we conducted a systematic analysis to the bacterial species distribution and their drug resistance rates in ICU across 109 medical institutions of Southwest China from 2018 to 2022, hoping to provide data support for the early empirical antibiotic use in intensive care units of this region, effectively control the epidemic of multidrug-resistant bacteria, and further improve the application of antimicrobial drugs and the construction of bacterial resistance surveillance network in medical institutions.
Materials and Methods
Bacterial Origin
After data review, isolated strains of ICUs (including respiratory and internal medicine intensive care units, emergency intensive care units, geriatric intensive care units, etc) from 109 medical institutions in member units of Sichuan Bacterial Resistance Monitoring Network from 2018 to 2022 were included in the final analysis, and duplicate strains were eliminated in principle of retaining the first strain of the same bacteria in the same patient.
Bacterial Identification and Susceptibility Testing
BIOMERIEUX VITEK 2 drug susceptibility system, BD Phoenix 100 automatic analysis system, DL96 detection system, Beckman Coulter MicroScan Autoscan-4 semi-automatic microbial system, TDR identification drug susceptibility system, Meihua Medical MA120 microbial identification drug susceptibility analysis system and BIOMERIEUX MOLDI-TOF mass spectrometry system were used for bacterial identification. Antibiotic susceptibility testing was performed with reference to the minimum inhibitory concentration (MIC) test, Kirby–Bauer method (K-B) and E-test method recommended by the 2022 Clinical Laboratory Standard Institute (CLSI) guidelines.15,16 The medicinal paper pieces came from Binhe Hangzhou, Kangtai Wenzhou and Oxoid, etc.
Interpretation of Results and Quality Control
The MIC value and inhibition circle diameter results were interpreted according to the CLSI M100 31st edition guideline standard.17 When the results of quality control strains were under control, the results of the study strains could be included in the data analysis.
Antibiotic susceptibility testing of quality control strains was performed once a week as a routine quality control procedure. MH agar medium was used for common bacterial susceptibility testing, HTM medium was used for Haemophilus influenzae susceptibility testing, and 5% sheep blood MH agar medium was used for Streptococcus pneumoniae and Streptococcus β-hemolyticus. Quality control strains included but were not limited to Staphylococcus aureus ATCC25923, Escherichia coli ATCC25922, Klebsiella pneumoniae ATCC700603, Pseudomonas aeruginosa ATCC27853, Enterobacter cloacae ATCC700323, Streptococcus pneumoniae ATCC49619 and Haemophilus influenzae ATCC49247.
Statistical Processing
All data were statistically analyzed by WHONET 5.6 software after removing duplicate strains.
Results
Specimen Origin and Bacterial Distribution
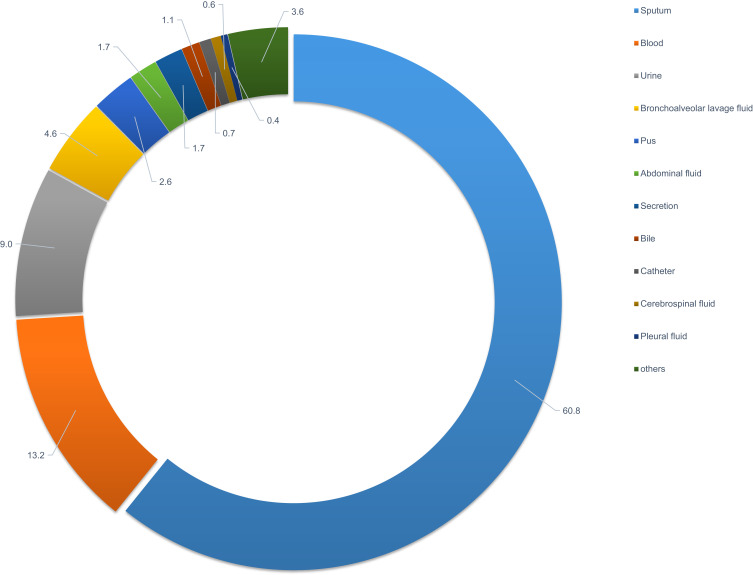
A total of 46,728 bacterial strains were isolated in Intensive Care Units from 2018 to 2022, and the top five specimen types were sputum (60.8%), blood (13.2%), urine (9.0%), bronchoalveolar lavage fluid (4.6%) and pus (2.6%), respectively (Figure 1).
Figure 1.
Percentage distribution of specimen sources.
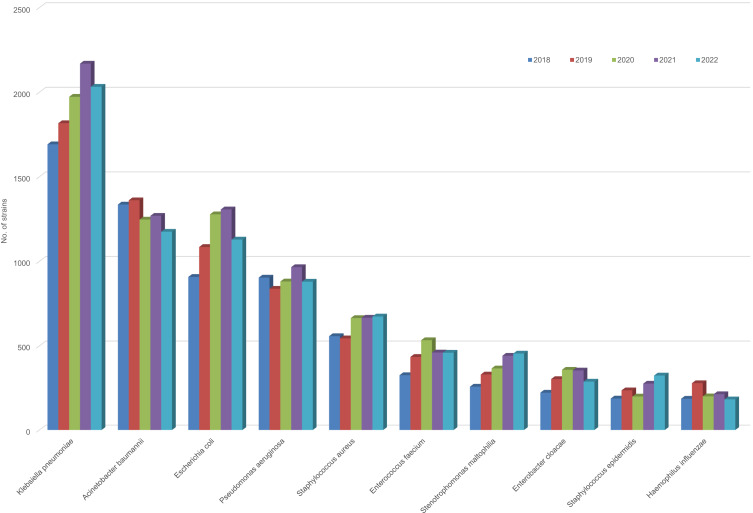
Among them, 35,549 strains of gram-negative bacteria were accounting for 76.1%, and 11,179 strains of gram-positive bacteria accounting for 23.9%. The top three isolation rates among gram-negative bacteria were Klebsiella pneumoniae (9623, 20.6%), Acinetobacter baumannii (6353, 13.6%) and Escherichia coli (5684, 12.2%), respectively. The first isolation rate among gram-positive bacteria was Staphylococcus aureus, with a total of 3099 strains accounting for 6.6%, followed by Enterococcus faecium (2210, 4.7%) and Staphylococcus epidermidis (1127, 2.6%) (Table 1). The detection trends of top 10 isolates from 2018 to 2022 are shown in Figure 2.
Table 1.
Distribution of Bacterial Species from 2018 to 2022
| Organism | No. of Strains | % |
|---|---|---|
| Klebsiella pneumoniae | 9623 | 20.6 |
| Acinetobacter baumannii | 6353 | 13.6 |
| Escherichia coli | 5684 | 12.2 |
| Pseudomonas aeruginosa | 4391 | 9.4 |
| Staphylococcus aureus | 3099 | 6.6 |
| Enterococcus faecium | 2210 | 4.7 |
| Stenotrophomonas maltophilia | 1844 | 3.9 |
| Enterobacter cloacae | 1528 | 3.3 |
| Staphylococcus epidermidis | 1227 | 2.6 |
| Haemophilus influenzae | 1065 | 2.3 |
| Streptococcus pneumoniae | 1027 | 2.2 |
| Serratia marcescens | 727 | 1.6 |
| Staphylococcus hominis ss. hominis | 701 | 1.5 |
| Staphylococcus haemolyticus | 660 | 1.4 |
| Klebsiella aerogenes | 607 | 1.3 |
| Klebsiella oxytoca | 566 | 1.2 |
| Enterococcus faecalis | 508 | 1.1 |
| Burkholderia cepacia | 403 | 0.9 |
| Others* | 4505 | 9.6 |
| Total | 46,728 | 100.0 |
Notes:*Bacteria other than the list.
Figure 2.
Detection trends of top 10 isolates from 2018 to 2022.
Sensitivity and Resistance Rates of Gram-Negative Bacteria to Antimicrobials
Enterobacteriaceae
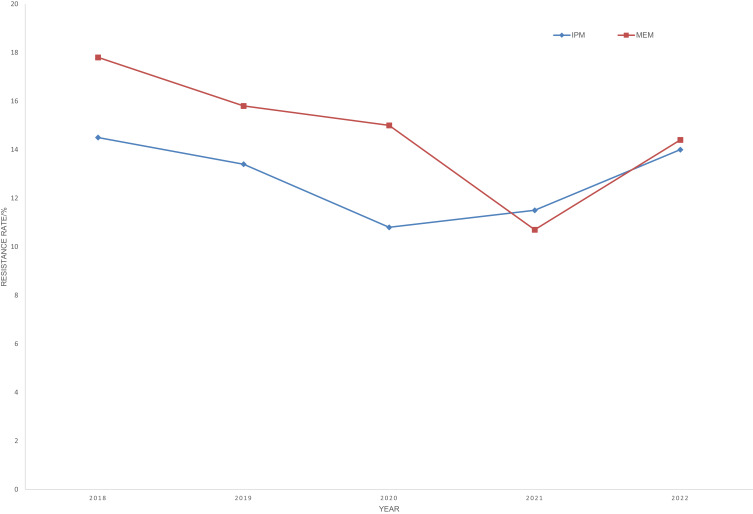
Klebsiella pneumoniae and Escherichia coli ranked first and third in the overall detection rate. From 2018 to 2022, the resistance rates of Klebsiella pneumoniae to imipenem and meropenem changed from 14.5% and 17.8% to 14.0% and 14.4%, showing a steady downward trend (Figure 3). The resistance rates of Escherichia coli to piperacillin, ceftriaxone, ciprofloxacin, levofloxacin, and trimethoprim–sulfamethoxazole were greater than 50%, while the resistance rates to carbapenems were always highly sensitive, with a total resistance rate of 3.8%. The total resistance rates of major Enterobacteriaceae to commonly used antimicrobials are shown in Table 2.
Figure 3.
Changes in the resistance rate in Klebsiella pneumoniae to imipenem and meropenem from 2018 to 2022.
Table 2.
Resistance Rates of Enterobacteriaceae Strains to Antimicrobial Agents
| Antimicrobial Agent | KPN (n=9623) | ECO (n=5684) | ECL (n=1528) | SMA (n=727) | PMI (n=383) | CFR (n=240) | MMO (n=141) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| R | S | R | S | R | S | R | S | R | S | R | S | R | S | |
| Ampicillin | –a | – | 86.7 | 11.9 | – | – | – | – | 64.9 | 32.9 | – | – | – | – |
| Piperacillin | 41.1 | 50.4 | 84.5 | 13.2 | 49.2 | 49.2 | 7.0 | 92.6 | 44.2 | 45.3 | 52.1 | 43.8 | 27.0 | 64.9 |
| Cefoperazone–sulbactam | 17.9 | 76.5 | 11.5 | 75.6 | 24.0 | 65.4 | 1.7 | 95.8 | 1.0 | 95.8 | 17.9 | 72.4 | 4.9 | 92.6 |
| Ampicillin–sulbactam | 33.3 | 61.3 | 51.2 | 28.6 | – | – | – | – | 42.2 | 49.4 | – | – | 64.8 | 9.0 |
| Piperacillin–tazobactam | 16.1 | 80.0 | 8.6 | 86.1 | 27.3 | 63.7 | 2.6 | 94.8 | 0.5 | 98.6 | 22.9 | 64.7 | 3.7 | 94.8 |
| Cefazolin | 42.1 | 45.7 | 72.5 | 17.2 | – | – | – | – | 59.3 | 25.0 | – | – | – | – |
| Cefuroxime | 33.6 | 63.5 | 60.2 | 36.1 | 63.3 | 23.6 | – | – | 46.9 | 50.2 | – | – | – | – |
| Ceftazidime | 21.8 | 76.5 | 30.4 | 66.7 | 43.4 | 55.5 | 4.3 | 95.1 | 6.8 | 91.6 | 44.2 | 54.5 | 15.2 | 78.0 |
| Ceftriaxone | 30.9 | 68.9 | 59.6 | 40.2 | 48.6 | 50.4 | 10.9 | 86.8 | 40.8 | 57.0 | 47.8 | 51.3 | 16.9 | 77.9 |
| Cefepime | 19.2 | 77.3 | 24.4 | 66.7 | 23.2 | 69.3 | 3.3 | 93.8 | 10.4 | 73.9 | 17.1 | 78.2 | 5.4 | 90.8 |
| Cefoxitin | 20.8 | 77.1 | 14.4 | 80.0 | – | – | – | – | 4.2 | 93.2 | – | – | 18.6 | 60.5 |
| Ertapenem | 9.0 | 90.9 | 2.9 | 96.9 | 15.3 | 83.1 | 2.9 | 96.8 | 1.0 | 97.9 | 7.9 | 91.5 | 2.8 | 97.2 |
| Imipenem | 12.6 | 86.7 | 3.4 | 96.4 | 16.3 | 81.5 | 5.8 | 84.1 | 25.0b | 50.0 b | 10.0 | 87.3 | NA | NA |
| Meropenem | 14.1 | 85.6 | 3.6 | 96.1 | 14.1 | 85.1 | 2.4 | 97.1 | 0.9 | 98.3 | 10.8 | 88.6 | 2.3 | 97.7 |
| Amikacin | 9.8 | 90.0 | 2.7 | 96.9 | 2.5 | 96.0 | 0.3 | 99.3 | 1.9 | 97.3 | 1.3 | 98.7 | 4.3 | 95.7 |
| Gentamicin | 18.6 | 80.3 | 34.9 | 63.3 | 18.0 | 76.9 | 2.2 | 97.2 | 20.0 | 56.0 | 17.3 | 81.0 | 21.8 | 72.2 |
| Ciprofloxacin | 21.1 | 76.6 | 52.5 | 45.1 | 20.3 | 75.0 | 1.7 | 97.7 | 42.4 | 51.0 | 25.3 | 70.6 | 20.5 | 68.2 |
| Levofloxacin | 18.7 | 78.8 | 50.3 | 46.6 | 18.3 | 77.0 | 1.0 | 98.1 | 25.2 | 64.1 | 20.1 | 75.1 | 9.0 | 81.3 |
| Trimethoprim–sulfamethoxazole | 24.5 | 75.5 | 52.7 | 47.2 | 25.9 | 74.1 | 2.8 | 97.2 | 54.9 | 45.1 | 25.0 | 75.0 | 37.0 | 63.0 |
| Polymyxin B | 0.8 | 95.1 | 2.3 | 97.7 | 0.0 | 90.9 | – | – | – | – | 0.0 | 100.0 | – | – |
| Tigecycline | 1.8 | 96.7 | 0.2 | 99.8 | 2.0 | 95.7 | 0.3 | 98.7 | – | – | 1.0 | 98.0 | – | – |
| Nitrofurantoin | 30.8 | 28.3 | 3.1 | 88.4 | 17.2 | 33.4 | – | – | – | – | 3.9 | 92.2 | – | – |
| Fosfomycin | NA | NA | 2.0c | 96.0c | NA | NA | NA | NA | NA | NA | NA | NA | NA | NA |
Notes: aIntrinsic resistance; bResults by Kirby–Bauer method only; cFor urinary tract isolates only.
Abbreviations: NA, not available; KPN, Klebsiella pneumonia; ECO, Escherichia coli; ECL, Enterobacter cloacae; SMA, Serratia marcescens; PMI, Proteus mirabilis; CFR, Citrobacter freundii; MMO, Morganella morganii.
Non-Fermented Gram-Negative Bacilli
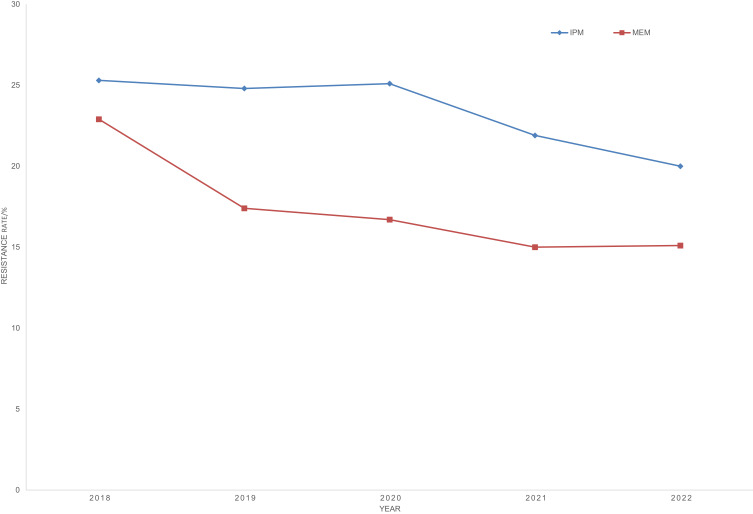
The resistance rates of Acinetobacter baumannii to most of the tested drugs were higher than 50%, and the resistance rates to imipenem and meropenem were 76.2% and 76.9%, respectively. It was highly sensitive to polymyxin B, colistin and tigecycline with resistance rates of 2.5%, 0.6% and 1.8%. The resistance rates of Pseudomonas aeruginosa to cefoperazone/sulbactam, piperacillin/tazobactam, ceftazidime, cefepime, gentamicin, ciprofloxacin, and levofloxacin were lower than 19.1%, and they were highly sensitive to polymyxin B, colistin and amikacin with resistance rates of 1.1%, 1.3% and 1.7%, respectively. The resistance rates of Pseudomonas aeruginosa to imipenem and meropenem decreased significantly, changed from 25.3% and 22.9% in 2018 to 20.0% and 15.1% in 2022 (Figure 4). The total resistance rates and susceptibility of major non-fermented gram-negative bacteria to commonly used antimicrobials are shown in Table 3.
Figure 4.
Changes in the resistance rate in Pseudomonas aeruginosa to imipenem and meropenem from 2018 to 2022.
Table 3.
Resistance Rates of Non-Fermentative Gram-Negative Bacilli to Antimicrobial Agents
| Antimicrobial Agent | ABA (n=6353) | PAE (n=4391) | PMA (n=1844) | PCE (n=403) | ||||
|---|---|---|---|---|---|---|---|---|
| R | S | R | S | R | S | R | S | |
| Piperacillin | 86.2 | 11.6 | 22.8 | 62.9 | – | – | – | – |
| Cefoperazone–sulbactam | 53.4 | 33.3 | 15.9 | 67.4 | 21.4 | 62.7 | 28.4 | 48.6 |
| Ampicillin–sulbactam | 64.9 | 28.0 | – | – | – | – | – | – |
| Piperacillin–tazobactam | 72.9 | 22.9 | 15.8 | 68.6 | – | – | 38.6 | 50.3 |
| Ceftazidime | 74.3 | 23.0 | 19.1 | 71.4 | 38.1 | 50.2 | 13.7 | 81.3 |
| Cefepime | 74.2 | 23.5 | 12.3 | 79.3 | 81.8 | 7.3 | 38.1 | 24.4 |
| Aztreonam | – * | – | 25.1 | 54.4 | – | – | 75.4 | 19.8 |
| Imipenem | 76.2 | 23.1 | 23.1 | 72.7 | – | – | 89.4 | 7.5 |
| Meropenem | 76.9 | 22.1 | 16.5 | 78.7 | – | – | 13.1 | 81.4 |
| Amikacin | 57.0 | 40.0 | 1.7 | 96.9 | – | – | NA | NA |
| Gentamicin | 67.1 | 31.1 | 5.6 | 90.3 | – | – | 83.6 | 12.1 |
| Ciprofloxacin | 76.1 | 23.5 | 13.1 | 81.5 | 23.0 | 49.2 | 14.2 | 67.6 |
| Levofloxacin | 60.6 | 26.3 | 14.1 | 77.5 | 7.9 | 88.1 | 14.0 | 77.8 |
| Trimethoprim–sulfamethoxazole | 44.7 | 55.1 | – | – | 8.5 | 91.4 | 11.6 | 88.1 |
| Colistin | 1.1 | 98.9 | 2.0 | 98.0 | 82.2 | 17.8 | – | – |
| Polymyxin B | 2.5 | 97.5 | 1.1 | 97.2 | 33.3 | 37.5 | – | – |
| Minocycline | 17.9 | 60.3 | – | – | 1.7 | 95.6 | 12.5 | 84.4 |
| Tigecycline | 1.8 | 88.9 | – | – | 7.4 | 87.0 | 16.3 | 66.3 |
Notes: *Intrinsic resistance.
Abbreviations: NA, not available; ABA, Acinetobacter baumannii; PAE, Pseudomonas aeruginosa; PMA, Stenotrophomonas maltophilia; PCE, Burkholderia cepacia.
Other Gram-Negative Bacilli
A total of 1065 strains of Haemophilus influenzae were isolated, adult isolates and child isolates accounted for 59.5% and 40.5%, respectively. The resistance rate of Haemophilus influenzae to ampicillin was more than 50%. Most Haemophilus influenzae were highly sensitive to ceftriaxone, meropenem, levofloxacin and chloramphenicol, while a few non-susceptible strains had appeared to the latter three. In comparison, isolates from children were more resistant to ampicillin, cefuroxime, and trimethoprim–sulfamethoxazole than those from adults (Table 4).
Table 4.
Resistance Rates of Haemophilus influenzae to Antimicrobial Agents
| Antimicrobial Agent | Total (n=1065) | Isolates from Adults (n=431) | Isolates from Children (n=634) | |||
|---|---|---|---|---|---|---|
| R | S | R | S | R | S | |
| Ampicillin | 64.9 | 31.2 | 59.6 | 35.7 | 68.7 | 27.9 |
| Amoxicillin–clavulanic acid | 12.7 | 87.3 | 13.3 | 86.7 | 12.3 | 87.7 |
| Ampicillin–sulbactam | 27.0 | 73.0 | 22.1 | 77.9 | 30.6 | 69.4 |
| Cefuroxime | 31.0 | 66.6 | 28.4 | 68.9 | 32.5 | 65.2 |
| Ceftriaxone | 0.0* | 100.0 | 0.0* | 100.0 | 0.0* | 100.0 |
| Meropenem | 1.4* | 98.6 | 1.1* | 98.9 | 1.6* | 98.4 |
| Levofloxacin | 1.2* | 98.8 | 0.9* | 99.1 | 1.5* | 98.5 |
| Trimethoprim–sulfamethoxazole | 47.5 | 40.9 | 43.0 | 44.1 | 50.8 | 38.6 |
| Azithromycin | 28.6* | 71.4 | 29.6* | 70.4 | 27.8* | 72.2 |
| Chloramphenicol | 3.9 | 95.7 | 3.9 | 95.8 | 3.8 | 95.6 |
Notes: *Insensitivity rate, sensitive breakpoints only.
Sensitivity and Resistance Rates of Gram-Positive Bacteria to Antimicrobials
Staphylococcus spp
Staphylococcus aureus owned the highest detection rate among gram-positive bacteria, with a total of 3099 isolated. The detection rates of MRSA and methicillin-resistant coagulase-negative Staphylococcus (MRCNS) respectively were 31.7% and 82.7%, and their resistance rates to antimicrobials such as aminoglycosides, quinolones, and macrolides were significantly higher than those of methicillin-sensitive strains (MSSA and MSCNS). However, the resistance rate of MRSA to trimethoprim-sulfamethazole was below that of MSSA (10.5% versus 19.1%). No vancomycin-resistant strain had been identified in Staphylococcus species, and a very small number of linezolid-resistant MRCNS were isolated with a rate of 0.7% (Table 5).
Table 5.
Resistance Rates of Staphylococcus spp. to Antimicrobial Agents
| Antimicrobial Agent | MRSA (n=982) | MSSA (n=2117) | MRCNS (n=2717) | MSCNS (n=570) | ||||
|---|---|---|---|---|---|---|---|---|
| R | S | R | S | R | S | R | S | |
| Penicillin G | 100.0 | 0.0 | 90.0 | 10.0 | 100.0 | 0.0 | 74.5 | 25.5 |
| Oxacillin | 100.0 | 0.0 | 0.0 | 100.0 | 100.0 | 0.0 | 0.0 | 100.0 |
| Gentamicin | 26.5 | 68.6 | 14.2 | 81.8 | 31.7 | 59.2 | 3.0 | 94.0 |
| Rifampin | 16.6 | 82.8 | 0.3 | 99.2 | 16.7 | 82.9 | 1.0 | 98.8 |
| Levofloxacin | 38.8 | 60.3 | 11.3 | 88.2 | 73.7 | 23.9 | 12.5 | 86.0 |
| Trimethoprim–sulfamethoxazole | 10.5 | 89.5 | 19.1 | 80.9 | 49.3 | 50.7 | 27.9 | 72.1 |
| Clindamycin | 60.4 | 39.5 | 26.7 | 72.9 | 47.8 | 50.7 | 11.4 | 86.7 |
| Erythromycin | 79.3 | 18.7 | 48.2 | 49.3 | 85.2 | 13.2 | 55.4 | 43.1 |
| Nitrofurantoin | 1.0 | 98.5 | 0.0 | 99.4 | 0.7 | 98.8 | 0.0 | 100.0 |
| Linezolid | 0.0 | 100.0 | 0.0 | 100.0 | 0.7 | 99.3 | 0.0 | 100.0 |
| Vancomycin | 0.0 | 100.0 | 0.0 | 100.0 | 0.0 | 100.0 | 0.0 | 100.0 |
| Teicoplanin | 0.0 | 95.8 | 0.0 | 97.5 | 0.0 | 100.0 | 0.0 | 100.0 |
Abbreviations: MRSA, methicillin-resistant Staphylococcus aureus; MSSA, methicillin-sensitive Staphylococcus aureus; MRCNS, methicillin-resistant coagulase-negative Staphylococcus; MSCNS, methicillin-sensitive coagulase-negative Staphylococcus.
Enterococcus Genus
The detection rate of Enterococcus faecium (2210, 4.7%) was significantly higher than that of Enterococcus faecalis (508, 1.1%). The sensitivity to most of the tested antibacterial drugs of Enterococcus faecium was significantly lower than that of Enterococcus faecalis. The resistance rates of the two to high concentrations of gentamicin were 36.0% and 47.5%, respectively. No vancomycin and teicoplanin-resistant Enterococcus faecium strains was detected, while a few vancomycin and teicoplanin-resistant strains (both 1.3%) were detected in Enterococcus faecalis, and more linezolid-resistant Enterococcus faecium strains (2.1%) than Enterococcus faecalis (0.4%). The total susceptibility and resistance rates of major Enterococcus genus to commonly used antimicrobials are shown in Table 6.
Table 6.
Resistance Rates of E. faecium and E. faecalis to Antimicrobial Agents
| Antimicrobial Agent | EFM (n=2210) | EFA (n=508) | ||
|---|---|---|---|---|
| R | S | R | S | |
| Penicillin G | 95.2 | 4.8 | 13.2 | 86.6 |
| Ampicillin | 93.8 | 6.2 | 9.7 | 90.3 |
| Gentamicin-high | 47.5 | 52.5 | 36.0 | 64.0 |
| Streptomycin-high | 30.7 | 69.3 | 28.5 | 71.5 |
| Rifampin | 76.1 | 13.4 | 48.5 | 34.3 |
| Levofloxacin | 93.7 | 4.6 | 28.0 | 68.8 |
| Moxifloxacin | 96.0 | 3.0 | 25.9 | 69.1 |
| Nitrofurantoin | 53.1 | 21.1 | 8.2 | 85.8 |
| Linezolid | 0.4 | 98.6 | 2.1 | 95.3 |
| Vancomycin | 1.3 | 98.7 | 0.0 | 100.0 |
| Teicoplanin | 1.3 | 98.7 | 0.0 | 100.0 |
Abbreviations: EFM, Enterococcus faecium; EFA, Enterococcus faecalis.
Other Gram-Positive Coccus
A total of 1027 strains of Streptococcus pneumoniae were isolated. The detection rates of PSSP, PISP, and PRSP were 98.5%, 1.5%, and 0.0% for 82 strains isolated from children, and 96.4%, 2.5%, and 1.1% for 945 strains isolated from adults. The drug sensitivity test results showed that both children’s and adult strains had high resistance rates to trimethoprim–sulfamethoxazole, erythromycin and clindamycin, and no vancomycin- and linezolid-resistant strains were detected (Table 7).
Table 7.
Resistance Rates of Streptococcus pneumonia to Antimicrobial Agents
| Antimicrobial Agent | Total (n=1027) | Isolates from Adults (n=945) | Isolates from Children (n=82) | |||
|---|---|---|---|---|---|---|
| R | S | R | S | R | S | |
| Penicillin G | 1.0 | 96.7 | 1.1 | 96.4 | 0.0 | 98.5 |
| Ceftriaxone | 6.7 | 89.8 | 6.3 | 90.4 | 10.1 | 84.1 |
| Cefotaxime | 4.6 | 89.6 | 4.2 | 90.5 | 7.1 | 81.4 |
| Meropenem | 7.0 | 68.3 | 6.9 | 69.1 | 7.2 | 58.0 |
| Levofloxacin | 2.5 | 97.0 | 2.7 | 96.7 | 0.0 | 100.0 |
| Moxifloxacin | 1.5 | 98.0 | 1.4 | 98.1 | 2.9 | 97.1 |
| Trimethoprim–sulfamethoxazole | 56.6 | 30.5 | 56.0 | 30.6 | 66.2 | 27.0 |
| Clindamycin | 87.7 | 11.1 | 87.4 | 11.5 | 90.3 | 6.5 |
| Erythromycin | 93.4 | 5.3 | 93.6 | 5.2 | 92.9 | 5.7 |
| Vancomycin | 0.0 | 100.0 | 0.0 | 100.0 | 0.0 | 100.0 |
Discussion
The monitoring results showed that a total of 46,728 bacterial strains were isolated from ICU across 109 medical institutions in Western China from 2018 to 2022, and the main sources of specimens were sputum, blood, urine, bronchoalveolar lavage fluid, pus, etc. Among them, the isolation rate of gram-negative bacteria was 76.1%, and the top three were Klebsiella pneumoniae, Acinetobacter baumannii and Escherichia coli, respectively. The isolation rate of gram-positive bacteria was 23.9%, with Staphylococcus aureus being the most, followed by Enterococcus faecium and Staphylococcus epidermidis.
Klebsiella pneumoniae and Escherichia coli ranked the top 2 gram-negative bacteria, and the number of isolates displayed an upward trend from 2018 to 2022 (Figure 2). Over a five-year period, the resistance rates of Klebsiella pneumoniae to imipenem and meropenem exhibited a steady downward trend. The sensitivity of Escherichia coli to carbapenems was stable overall, with a total resistance rate of only 3.8%. Among non-fermented gram-negative bacteria, the resistance rates of Acinetobacter baumannii to most of the tested drugs were more than 50%, and the resistance rates to imipenem and meropenem respectively were 76.2% and 76.9%, which were significantly higher than those of the national level (65.8% and 66.6%).18 The overall resistance rates of Pseudomonas aeruginosa to imipenem and meropenem were 23.1% and 16.5%, performing a significant decrease trend from 2018 to 2022. The overall downward trend of the drug resistance rate is inseparable from the following two points. First of all, the national policy system has made the legalization and institutionalization of antimicrobial drug management on track, raised the awareness of medical workers on the hierarchical use of antimicrobial drugs and the public’s awareness of the drug resistance’s crisis, and greatly promoted the rational use of antimicrobial drugs. Secondly, the gradual improvement of the bacterial resistance monitoring network provides a useful reference for the administrative department to adjust management policies in a timely manner, and for medical institutions to rationally select antibacterial drugs.
The increasing incidence and epidemic of carbapenem-resistant gram-negative bacilli (CRGNB) has become a global public health issue, with mortality rates as high as 6.6% to 20%.19,20 WHO has classified CRE, CRAB, and CRPA as the pathogens of critical threat in the global priority list.4 CRGNB usually exhibit the characteristics of broad drug resistance or even total drug resistance due to the prevalence of resistance genes to other antibacterial drugs,21 making clinical anti-infection treatment difficult. Ceftazidime/avibactam, tigecycline, and polymyxin are considered the most effective antimicrobials for the treatment of infections caused by CRGNB.22–24 Laboratories should conduct susceptibility testing of other antimicrobials as much as possible while using mentioned above antimicrobials, and if necessary, combined susceptibility testing could be applied to screen out more effective anti-infective regimens.25 Carbapenemase-producing is the most important resistance mechanism of CRE,26 different types of carbapenemase need to be targeted with carbapenem inhibitor combinations. Therefore, it is recommended that laboratories should carry out the detection of carbapenemase phenotype or genotype as advocated27 and report to the clinical.
Among the gram-positive bacteria isolated in this surveillance, staphylococci and enterococci were the main ones. The detection rates of MRSA and MRCNS were 31.7% and 82.7%, respectively, which were higher than those of the national level (28.7% and 78.2%).18,28 During 5 years, Staphylococcus aureus has always maintained a high sensitivity to linezolid, vancomycin and teicoplanin, vancomycin still is introduced as a drug of choice for treating serious infections due to MRSA. However, due to the overuse of vancomycin, non-sensitive strains began to emerge. Vancomycin-resistant Staphylococcus aureus (VRSA) strains have been reported in the United States, Iran, and India.29–32 Increased antibiotic resistance in MRSA isolates is becoming one of the most serious health problems worldwide. The good news is that new agents such as Travancin, Dabavancin, Olitavan Cin and Tedizolid have recently been licensed to treat infections caused by MRSA. In addition, as a normal colonizing flora of human skin and mucous membranes, with the increase in invasive operations, such as indwelling catheters, endotracheal intubation and implantation of medical devices, Staphylococcus epidermis is necessary to exclude contamination caused by improper operation and define whether it is the real pathogenic bacteria.
During 5 years, Enterococcus faecium and Enterococcus faecalis remained highly sensitive to linezolid, vancomycin, and tecoplanin. Temporarily, no vancomycin-resistant Enterococcus faecium strains were detected, and a few vancomycin-resistant strains were detected in Enterococcus faecalis. Together with MRSA, WHO identified VRE as Priority 2 drug-resistant bacterium in the “Global Priority List of Antibiotic-Resistant Bacteria”.4 Although high-dose daptomycin and linezolid could be applied for the treatment of VRE infections, emerging antibiotic resistance to these agents limits potential available therapies.
Conclusion
From 2018 to 2022, the bacteria infection in intensive care units of Southwest China was mainly gram-negative bacteria, and the growth rate of major multidrug-resistant bacteria was significantly higher than that of the national level. Given the rising prevalence of MDR/XDR/PDR bacteria in ICU, the establishment and execution of ASP is particularly critical. ASP has been shown to be effective in reducing antibiotic resistance, duration of ventilation, days of antibiotic use, and healthcare costs in critically ill patients. Because of these benefits, antibiotic stewardship should be implemented in all intensive care units as a core competency of intensive care physicians. On top of ASP, rapid and accurate diagnostics play a crucial role in striking the right balance between providing timely and appropriate antibiotic therapy in the ICU while minimizing the unnecessary use of antibiotics. Advanced diagnostics empower healthcare professionals to make informed decisions promptly, ensuring optimal patient care and preserving the effectiveness of antibiotics.
Ethics Approval
The study was approved by the Ethics Committee of Sichuan Provincial People’s Hospital, University of Electronic Science and Technology of China, Chengdu, China (No. 2023324). The ethics committee waived the need for written informed consent provided by participants due to the retrospective nature of this study. Patients’ anonymous information was provided from the microbiology hospital laboratory, which isolated the strains. The study completely followed the principles outlined in the Declaration of Helsinki.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Murray CJL, Ikuta KS, Sharara F.; Antimicrobial Resistance Collaborators. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Lancet. 2022;399(10325):629–655. doi: 10.1016/S0140-6736(21)02724-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wagenlehner FME, Dittmar FR. Global burden of bacterial antimicrobial resistance in 2019: a systematic analysis. Eur Urol. 2022;82(6):658. doi: 10.1016/j.eururo.2022.08.023 [DOI] [PubMed] [Google Scholar]
- 3.Pulingam T, Parumasivam T, Gazzali AM, et al. Antimicrobial resistance: prevalence, economic burden, mechanisms of resistance and strategies to overcome. Eur J Pharm Sci. 2022;170:106103. doi: 10.1016/j.ejps.2021.106103 [DOI] [PubMed] [Google Scholar]
- 4.Tacconelli E, Carrara E, Savoldi A, et al. Discovery, research, and development of new antibiotics: the WHO priority list of antibiotic resistant bacteria and tuberculosis. Lancet Infect Dis. 2018;18(3):318–327. doi: 10.1016/S1473-3099(17)30753-3 [DOI] [PubMed] [Google Scholar]
- 5.Magill SS, Edwards JR, Bamberg W, et al. Multistate point-prevalence survey of health care-associated infections. N Engl J Med. 2022;386(24):2348. doi: 10.1056/NEJMx210023 [DOI] [PubMed] [Google Scholar]
- 6.Grundmann H, Glasner C, Albiger B, et al. Occurrence of carbapenemase-producing Klebsiella pneumoniae and Escherichia coli in the European survey of carbapenemase-producing Enterobacteriaceae (EuSCAPE): a prospective, multinational study. Lancet Infect Dis. 2017;17(2):153–163. doi: 10.1016/S1473-3099(16)30257-2 [DOI] [PubMed] [Google Scholar]
- 7.Gorgulho A, Grilo AM, Figueiredo M, et al. Carbapenemase-producing Enterobacteriaceae in a Portuguese hospital - a five-year retrospective study. Germs. 2020;10(2):95–103. doi: 10.18683/germs.2020.1190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rafailidis PI, Kofteridis D. Proposed amendments regarding the definitions of multidrug-resistant and extensively drug-resistant bacteria. Expert Rev Anti Infect Ther. 2022;20(2):139–146. doi: 10.1080/14787210.2021.1945922 [DOI] [PubMed] [Google Scholar]
- 9.Munari M, Franzoi F, Sergi M, et al. Extensively drug-resistant and multidrug-resistant gram-negative pathogens in the neurocritical intensive care unit. Acta Neurochir. 2022;164(3):859–865. doi: 10.1007/s00701-020-04611-3 [DOI] [PubMed] [Google Scholar]
- 10.Kollef MH, Bassetti M, Francois B, et al. The intensive care medicine research agenda on multidrug-resistant bacteria antibiotics and stewardship. Intensive Care Med. 2017;43(9):1187–1197. doi: 10.1007/s00134-017-4682-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Evans L, Rhodes A, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Intensive Care Med. 2021;47(11):1181–1247. doi: 10.1007/s00134-021-06506-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Murphy CV, Reed EE, Herman DD, et al. Antimicrobial Stewardship in the ICU. Semin Respir Crit Care Med. 2022;43(1):131–140. doi: 10.1055/s-0041-1740977 [DOI] [PubMed] [Google Scholar]
- 13.Pickens CI, Wunderink RG. Principles and practice of antibiotic stewardship in the ICU. Chest. 2019;156(1):163–171. doi: 10.1016/j.chest.2019.01.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kollef MH, Torres A, Shorr AF, et al. Nosocomial Infection. Crit Care Med. 2021;49(2):169–187. doi: 10.1097/CCM.0000000000004783 [DOI] [PubMed] [Google Scholar]
- 15.Clinical and Laboratory Standards Institute. Methods for Dilution Antimicrobial Susceptibility Tests for Bacteria That Grow Aerobically. CLSI; 2018. [Google Scholar]
- 16.Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Disk Susceptibility Tests. CLSI; 2018. [Google Scholar]
- 17.Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing. CLSI; 2022. [Google Scholar]
- 18.CHINET. China's clinical strain detection distribution and drug resistance rate change data. Available from: https://www.chinets.com/Data/GermYear. Accessed March 1, 2023.
- 19.Lutgring JD. Carbapenem-resistant Enterobacteriaceae: an emerging bacterial threat. Semin Diagn Pathol. 2019;36(3):182–186. doi: 10.1053/j.semdp.2019.04.011 [DOI] [PubMed] [Google Scholar]
- 20.Livorsi DJ, Chorazy ML, Schweizer ML, et al. A systematic review of the epidemiology of carbapenem-resistant Enterobacteriaceae in the United States. Antimicrob Resist Infect Control. 2018;7(55):1–9. doi: 10.1186/s13756-018-0346-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kopotsa K, Sekyere JO, Mbelle NM. Plasmid evolution in carbapenemase-producing Enterobacteriaceae: a review. Ann N Y Acad Sci. 2019;1457(1):61–91. doi: 10.1111/nyas.14223 [DOI] [PubMed] [Google Scholar]
- 22.Duin D, Lok JJ, Earley M, et al. Colistin versus ceftazidime-avibactam in the treatment of infections due to carbapenem-resistant enterobacteriaceae. Clin Infect Dis. 2018;66(2):163–171. doi: 10.1093/cid/cix783 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Sheu CC, Chang YT, Lin SY, et al. Infections caused by carbapenem-resistant Enterobacteriaceae: an update on therapeutic options. Front Microbiol. 2019;10:80. doi: 10.3389/fmicb.2019.00080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Tian Y, Zhang QY, Wen LR, et al. Combined effect of Polymyxin B and Tigecycline to overcome heteroresistance in carbapenem-resistant Klebsiella pneumoniae. Microbiol Spectr. 2021;9(2):e0015221. doi: 10.1128/Spectrum.00152-21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang WX, Guo Y, Yang Y, et al. Study of in vitro synergistic bactericidal activity of dual β-lactam antibiotics against KPC-2-producing Klebsiella pneumonia. Microb Drug Resist. 2020;26(3):204–210. doi: 10.1089/mdr.2019.0126 [DOI] [PubMed] [Google Scholar]
- 26.Han RR, Shi QY, Wu S, et al. Dissemination of carbapenemases (KPC, NDM, OXA-48, IMP, and VIM) among carbapenem-resistant Enterobacteriaceae isolated from adult and children patients in China. Front Cell Infect Microbiol. 2020;10:314. doi: 10.3389/fcimb.2020.00314 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wei Q, Sun J, Wang Z, et al. Evaluation of Modified Rapid Carbapenem Inactivation Method (mrCIM) Combined with Rapid EDTA-modified carbapenem inactivation method (reCIM) to detect carbapenemase and distinguish metallo-carbapenemase in Enterobacteriaceae within four hours. Infect Drug Resist. 2020;13:1919–1927. doi: 10.2147/IDR.S249570 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hu F, Zhu D, Wang F, et al. Current status and trends of antibacterial resistance in China. Clin Infect Dis. 2018;67(s2):S128–S134. doi: 10.1093/cid/ciy657 [DOI] [PubMed] [Google Scholar]
- 29.Cong YG, Yang SJ, Rao XC. Vancomycin resistant Staphylococcus aureus infections: a review of case updating and clinical features. J Adv Res. 2019;21:169–176. doi: 10.1016/j.jare.2019.10.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Selvabai AP, Sattar SBA, Jayaraman P, et al. Detection and characterisation of heteroresistant vancomycin intermediate Staphylococcus aureus (hVISA) using phenotypic and genotypic methods. J Clin Diagn Res. 2019;13(5):DC01–DC05. doi: 10.7860/JCDR/2019/41127.12868 [DOI] [Google Scholar]
- 31.Wu Q, Sabokroo N, Wang Y, et al. Systematic review and meta-analysis of the epidemiology of vancomycin-resistance Staphylococcus aureus isolates. Antimicrob Resist Infect Control. 2021;10(1):101. doi: 10.1186/s13756-021-00967-y [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 32.Cascioferro S, Carbone D, Parrino B, et al. Therapeutic strategies to counteract antibiotic resistance in MRSA biofilm-associated infections. ChemMedChem. 2021;16(1):65–80. doi: 10.1002/cmdc.202000677 [DOI] [PubMed] [Google Scholar]